Abstract
Although radiotherapy (RT) is used for the treatment of cancers, including liver cancer, radiation-induced liver disease (RILD) has emerged as a major limitation of RT. Radiation-induced toxicities in nontumorous liver tissues are associated with the development of numerous symptoms that may limit the course of therapy or have serious chronic side effects, including late fibrosis. Although the clinical characteristics of RILD patients have been relatively well described, the understanding of RILD pathogenesis has been hampered by a lack of reliable animal models for RILD. Despite efforts to develop suitable experimental animal models for RILD, current animal models rarely present hepatic veno-occlusive disease, the pathological hallmark of human RILD patients, resulting in highly variable results in RILD-related studies. Therefore, we introduce the concept and clinical characteristics of RILD and propose a feasible explanation for RILD pathogenesis. In addition, currently available animal models of RILD are reviewed, focusing on similarities with human RILD and clues to understanding the mechanisms of RILD progression. Based on these findings from RILD research, we present potential therapeutic strategies for RILD and prospects for future RILD studies. Therefore, this review helps broaden our understanding for developing effective treatment strategies for RILD.
Introduction
Hepatocellular carcinoma (HCC) is the fifth most common cancer worldwide and the third leading cause of cancer-related deaths.1, 2 More than 700 000 people are diagnosed with this cancer each year globally, and the number of cases is expected to increase. Liver transplantation is considered the most effective therapeutic option for HCC.3 However, because of the shortage of donor livers, less than 20% of HCC patients are eligible for liver transplantation. Recently, multidisciplinary therapeutic approaches, such as surgical resection, chemotherapy, radiotherapy (RT) and combination therapy, have been proposed to treat HCC.3, 4 Among these treatments, RT has emerged as an effective treatment for intermediate-stage HCC and unresectable liver disease.5, 6 However, the application of RT is limited due to radiotoxicity in nontumorous surrounding tissue and, unfortunately, can have some negative side effects, including radiation-induced liver disease (RILD).7, 8, 9 RILD occurs as an acute response during or within a few weeks of RT or as a late-response months to years after RT. RILD is a major limitation of RT in the treatment of liver cancer and is associated with a high mortality rate in patients with liver cancer.10 Furthermore, the liver is one of the organs that is commonly irradiated during RT treatment of gastrointestinal cancers because of its proximity to the gastrointestinal tract and its large size.7, 11, 12 The liver can also be exposed to radiation during the preparation for allogeneic bone marrow or hematopoietic stem cell transplantation.13, 14 Hepatic nonparenchymal cells, such as Kupffer cells (KCs), sinusoidal endothelial cells (SECs) and hepatic stellate cells, are known to be radiosensitive. These cells release various substances that promote liver fibrosis, contributing to distorted liver structure and function during radiation.15, 16, 17 This radiation-induced hepatic fibrosis is becoming an increasingly serious problem in patients with RILD.18 Therefore, studying the pathophysiological mechanisms of RILD are very important for both preventing RILD progression and increasing the treatment efficacy of RT, eventually contributing to improving overall quality of life. However, advances in radiobiology have been slow because radiobiology relies primarily on human studies, which are heavily restricted. To overcome this limitation, well-characterized animal models of RILD are necessary. In this review, we summarize the characteristics and pathogenesis of clinical RILD and the animal models that have been reported so far. In particular, we discuss the key features of each animal model in comparison to human RILD. In the last section, we present the potential therapeutic strategies for RILD and future prospects for RILD-related studies.
Introduction and clinical characteristics of RILD
RILD, which was originally described by Ingold et al.,19 is the most significant complication of RT. Although RILD typically occurs 4–8 weeks after termination of RT, it has been reported to appear as early as 2 weeks or as late as 7 months after RT.7, 9, 10 Among the patients receiving hepatic radiation of 30–35 Gy, ~6–66% of patients present significant RILD.9, 10, 12 This broad range of RILD incidence rate is related to the volume of irradiated livers, individual hepatic functional reserve and medical history. There are two types of RILD: classic RILD and non-classic RILD. Patients with classic RILD usually have symptoms of fatigue, abdominal pain, increased abdominal girth, hepatomegaly and anicteric ascites 1–3 months after liver RT.8 In addition, the level of alkaline phosphatase (ALP) increases by more than twofold that of normal levels, whereas levels of transaminase and bilirubin remain normal.20 The pathological hallmark of classic RILD is hepatic veno-occlusive disease (VOD), which is characterized by complete obliteration of the central vein lumina by erythrocytes trapped in a network of reticulin and collagen fibers.21, 22 The trapped erythrocytes create vascular congestion, leading to decreased oxygen delivery to the central zone. This hypoxic environment results in both the death of centrilobular hepatocytes (HCs) and atrophy of the inner hepatic plate, leading to hepatic dysfunction. In addition, HSC activation contributing to hepatic fibrosis is a common characteristic in patients with classic RILD.23 Patients who develop non-classic RILD have underlying chronic hepatic diseases, such as cirrhosis and viral hepatitis, and show more dysregulated hepatic functions with jaundice and/or remarkably elevated serum transaminases (a more than fivefold increase compared to normal levels) rather than ALP.12, 24 For example, patients with the hepatitis B virus are reportedly more vulnerable to developing RILD compared to non-carrier groups.25 In addition, hepatocellular loss, hepatic dysfunction, hepatic sinusoidal endothelial death and HSC activation have been detected in non-classic RILD. Hepatic irradiation in these particular patients impairs their hepatocellular regeneration capacity and induces irreversible hepatic failure.26
Although the pathophysiological characteristics of RILD in human patients have been relatively well characterized, the precise mechanisms of RILD development remain largely unknown. As a result, there are no effective therapeutic measures to prevent or cure the progression of RILD.10 Radioprotectors, which are used in combination therapy with RT, have been recently reported to protect nontumorous liver tissue from radiation-induced damage. Amifostine, a radioprotective drug, is clinically used to treat head and neck cancer in combination therapy with RT.27 Amifostine has also been shown to protect HCs from radiation-induced damage without compromising the killing effect of RT in tumor cells in the livers of rats.28 In a phase I clinical study, amifostine demonstrated radioprotective effects in the nontumorous liver tissues of RT patients with primary or metastatic intrahepatic cancer.29 In addition, melatonin, a hormone in the pineal gland, has been shown to exert a radioprotective effect in the radiation-treated liver by decreasing oxidative stress in rats.30 However, the use of such radioprotectors in routine clinical practice is still being investigated. Evidence for their safety and effectiveness is lacking because amifostine has been reported to cause side effects, such as vomiting, nausea and hypotension, and the efficacy of melatonin has only been tested in an experimental rat model. In the treatment of patients with RILD, supportive drugs, such as diuretics for fluid retention, paracentesis for ascites and steroids for reducing hepatic congestion, are currently used,10 but they are mainly directed at alleviating symptoms rather than providing a cure. The use of anticoagulants and thrombolytics may be helpful in relieving hepatic vein thrombosis. However, there are no specific therapeutic agents for the management and cure of RILD, and RILD patients are managed in the same way as non-irradiated patients. Therefore, the underlying mechanism of RILD should be investigated and understood to provide specific management and treatment to RILD patients.
Current knowledge of RILD pathogenesis
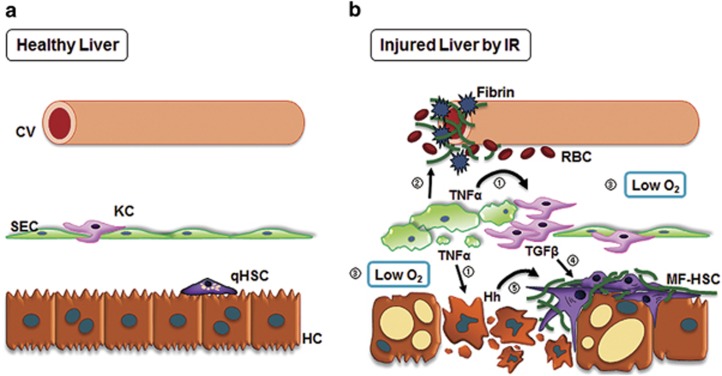
Although our knowledge of RILD pathogenesis has improved in recent years, the molecular pathogenic mechanisms of RILD remain unclear. RILD pathogenesis includes complex and multicellular responses associated with vascular changes, increased collagen synthesis and sequential activation of key growth factors and cytokines, such as tumor necrosis factor alpha (TNF-α), transforming growth factor beta (TGF-β) and hedgehog (Hh), which are important regulators in repair responses to liver damage.31 Radiation causes acute or chronic injury in the liver. The early effects of irradiation include DNA damage, oxidative stress and reactive oxygen species production leading to hepatocellular apoptosis and acute inflammatory responses in irradiated regions.32 Although HCs are considered more radioresistant than nonparenchymal cells, the radiation-induced release of TNF-α by KCs increases the susceptibility of HCs to radiation-induced apoptosis and ultimately induces hepatocellular death.15, 33 Christiansen et al.15 showed that direct irradiation of cultured rat HCs did not lead to cytotoxicity. However, irradiated KCs released TNF-α into the culture medium, and irradiated HCs treated with this culture medium containing TNF-α showed significantly increased apoptosis, suggesting that KCs secrete TNF-α, which promotes hepatocyte apoptosis and contributes to acute liver injury with dysregulated function in the irradiated liver. Massive hepatocyte death caused by repetitive or severe injury is associated with the compensatory proliferation of myofibroblastic (MF)-HSCs.31 The activation of HSCs is a key cellular event underlying hepatic fibrosis. Upon liver injury, HSCs are transdifferentiated from quiescent HSCs into activated/MF-HSCs, the main collagen-producing cells in the liver. This HSC activation is also suggested to be an essential process in RILD development because these cells are highly radiosensitive and accumulate in the livers of patients with RILD.23 Consistent with this observation in human liver samples, radiation increases the expression of alpha-smooth muscle actin, a well-known marker of MF-HSCs, in the livers of irradiated rats and mice.34, 35, 36, 37 In addition, SEC apoptosis is considered the primary event in radiation-induced liver damage. Yamanouchi et al.17 reported that the number of apoptotic SECs, not HCs, was elevated in the livers of irradiated rats. SEC injury resulted in microcirculatory blood flow disturbances, which damaged HCs. The injured SECs and central vein endothelium also activated the coagulation cascade and led to the deposition of fibrin and the formation of clots in the central veins and hepatic sinusoids. The ensuing hypoxic environment resulted in the death of centrilobular HCs and atrophy of the inner hepatic plate, promoting hepatic congestion and liver dysfunction.21, 38 At later stages, a fibrotic reaction in the sinusoids can lead to the obliteration of central venules, leading to VOD. Therefore, a complex and dynamic interaction among different types of hepatic cells occurs in RILD, and a simplified model of this event is depicted in Figure 1.
Figure 1.
Simplified model of liver-specific cellular events in radiation-induced liver injury. (a) In the normal liver, liver sinusoids are lined with SECs and KCs. Quiescent hepatic stellate cells (qHSCs) are located in the space of Disse and are in close contact with HCs and SECs. (b) In the irradiated liver, ① injured SECs undergo apoptosis and release TNF-α, which promotes HC apoptosis and KC activation. ② In addition, injured SECs induce the penetration of red blood cells (RBCs) and activate fibrin deposition in central veins (CVs), leading to sinusoidal obstruction. ③ The ensuing hypoxic environment leads to the death of HCs and the activation of KCs. ④ Activated KCs release TGF-β, the major profibrogenic cytokine, which promotes the transdifferentiation of qHSCs into MF-HSCs. ⑤ Apoptotic HCs produce Hh ligands, which trigger the proliferation of Hh-responsive cells, such as HSCs. MF-HSCs accumulate and promote the deposition of extracellular matrix proteins, leading to liver fibrosis in the late stage of RILD.
TGF-β is produced by many types of hepatic cells, including HSC, and promotes the accumulation of MF-HSC during liver fibrosis.31 In the livers of irradiated rats, the level of TGF-β1 increased as the dose of radiation increased, and this expression pattern of TGF-β1 was correlated with the degree of hepatic fibrosis.39 In addition, TGF-β1 stimulated the prolonged production of reactive oxygen species in HCs.40 This increased oxidative stress was shown to be involved in the development and pathogenesis of late radiation-induced fibrosis. TGF-β activated by radiation promotes the production of profibrotic cytokines and stimulates collagen deposition.31 These fibrogenic effects of TGF-β are mediated by the overproduction of plasminogen activator inhibitor-1, one of the downstream targets of TGF-β, which inhibits plasminogen activators, thereby preventing the breakdown of fibrin and promoting its accumulation.41 In addition, connective tissue growth factor, a fibrogenic cytokine, is a downstream mediator of the effect of TGF-β on extracellular matrix deposition, including collagen synthesis.41 Thus, TGF-β1 plays an important role in RILD by mediating multicellular interactions and promoting fibrosis. Increasing evidence suggests that Hh signaling plays a pivotal role in the development of RILD. Hh signaling influences the functions of HSCs, SECs and HCs. In the injured liver, apoptotic or ballooned HCs produce Hh ligands, which stimulate Hh-responsive cells, such as progenitors, HSCs and SECs.42, 43 These cells, in turn, activate Hh signaling and are involved in the remodeling responses to liver injury. Wang et al.35, 37 demonstrated that Hh signaling was activated and involved in both acute and late liver responses to irradiation. In these studies, Wang et al.35, 37 showed that Hh signaling was associated with the activation of HSCs and that Hh suppression reduced the response of these cells, alleviating radiation-induced liver fibrosis. Therefore, the Hh pathway is suggested to be a potential player in the pathogenesis of RILD.
Animal models of RILD: the experimental approach
Our understanding of RILD is mostly based on clinical observations and patient-derived histopathology. Reed and Cox22 were the first to characterize the histological changes of RILD resembling VOD. A liver biopsy of a patient with RILD may show endothelium swelling, terminal hepatic venule narrowing, sinusoidal congestion, parenchymal atrophy and fibrosis.44 These pathologic observations are predominantly evident around the central vein and are similar to those of VOD.8 Based on these clinical observations, experimental models of RILD, ranging from small rodents to nonhuman primates, have been developed to investigate the mechanism responsible for the development of the equivalent RILD seen in human patients. The establishment of animal models is essential to better understand the pathogenesis and molecular mechanisms of RILD. A number of animal models have been used to examine RILD, and the effects of hepatic irradiation have been studied in several experimental animals. The preferred animal model is the rat. Along with rats, mice, monkeys, dogs and rabbits are also used as models for experimental RILD. However, animal models in most studies have not shown similar pathological characteristics to human RILD. In addition, animal models for RILD are yet to be established because the treatment methods used in RILD research, such as radiation dose, single or fractionated irradiation, combining radiation with other chemicals, employing mouse/rat strains and genders, follow-up times and so on, are diverse. These undefined treatments lead to variable results in RILD research, and this variability impedes the understanding of the mechanism of RILD. Therefore, it is necessary to determine the characteristics of each model and compare the results obtained from these animal models with human RILD to identify the advantages and disadvantages of each currently available animal model (Table 1) to develop an appropriate animal model for RILD.
Table 1. Currently available animal models of RILD.
| Animal | Gender | Fractionation/Irradiated area | Dose (Gy) | Follow-up times | Pathological properties | Reference |
|---|---|---|---|---|---|---|
| Rat | ||||||
| Wistar | Male | Single/Whole body | 6 Gy | 2 h | • Increased oxidative stress and lipid peroxidation | 30 |
| Male | Single/Liver | 25 Gy | 24 and 48 h | • Mild hepatocellular damage • Mild steatosis | 49 | |
| Male | Fractionation/Liver | Total 60 Gy (2 Gy per fraction) | 3 mo | • Upregulated ALP levels • No necroinflammation and fibrosis | 36 | |
| SD | Not indicated | Single/Abdomen | 8 Gy | 36 h | • Sinusoidal congestion • Hemorrhage • Dilation of the central vein • Degenerated Hepatocyte • Kupffer cell activation | 48 |
| Male | Single/Liver | 30 Gy | 6 mo | • Liver fibrosis | 50 | |
| Male | Single/Liver | 60 Gy | 8 wk | • Hepatic sinus congestion • Hepatocyte apoptosis • Liver fibrosis | 34 | |
| Mouse | ||||||
| C57BL/6 | Female | Single/Whole body | 20 Gy | 1 wk | • Accumulation of fatty hepatocyte and apoptotic hepatocyte • Expansion of progenitors and • MF-HSC • Liver fibrosis | 37 |
| Female | Single/Whole body | 6 Gy | 1 wk | • Accumulation of fatty hepatocytes and apoptotic cells • Liver fibrosis | 51 | |
| Male | Single/Abdomen | 6 Gy | 6 and 10 wk | • Upregulated ALT/AST levels • Apopotsis • Fat accumulation • Liver fibrosis | 35 | |
| Male | Fractionation/Liver | Total 30 Gy (6 Gy per fraction) | 6 and 10 wk | • Upregulated ALT/AST levels • Hepatic congestion • Liver fibrosis | 52 | |
| NHP | ||||||
| Rhesus monkey | Female | Fractionation/Liver | Total 36 Gy (4.5 Gy per fraction) or Total 50 Gy (2.5 Gy per fraction) | 9 mo | • No clinical or biochemical signs of liver dysfunction | 61 |
| Cynomolgus monkey | Male | Fractionation/Liver | Total 40 Gy | 10 wk | • VOD • Hemorrhage • Upregulated ALP levels • Hepatic congestion • Liver fibrosis | 62 |
| Rabbit | Not indicated | Single/Liver | 24–28 Gy or 36 Gy | 1, 2 and 6 mo | • No macroscopic and microscopic changes | 56 |
| Dog | Not indicated | Single/Liver | 20 Gy | 1 to 2 yr | • Liver fibrosis • Liver cell atrophy | 57 |
Abbreviations: ALP, alkaline phosphatase; ALT, alanine transaminase; AP, alkaline phosphatase; AST, aspartate transaminase; F, female; hr, hour(s); M, male; MF-HSC, myofibroblastic hepatic stellate cell; mo, month(s); NHP, nonhuman primate; SD, Sprague–Dawley; VOD, veno-occlusive disease; wk, week(s); yr, year(s).
Rodents: rat and mouse
Rodents have many advantages as experimental models, such as their anatomical, physiological and genetic similarity to humans.45 The rat is the most frequently used animal model for RILD. The most common rat strains used are Sprague–Dawley (SD) and Wistar rats. When Wistar rats were exposed to a single dose (6 Gy) of total body irradiation, lipid peroxidation and oxidative stress were significantly elevated in the liver, showing increased levels of malondialdehyde, the main product of lipid peroxidation and cytotoxic nitric oxide in the liver.30 Although whole-body irradiation induces oxidative stress in the liver, it is inappropriate to investigate radiation-induced hepatic responses because whole-body irradiation may induce immunosuppression, endocrine dysfunction and multi-organ failure, which are risk factors for hepatic damage.46, 47 Therefore, recent studies have employed hepatic irradiation, which seems to be more suitable for investigating radiation-induced liver responses. When SD rats were exposed to an 8 Gy single dose of abdominal irradiation, severe sinusoidal congestion and hemorrhage, dilation of the central vein, degenerated HCs with perinuclear vacuolization and activated KCs were observed in the irradiated livers 36 h after exposure.48 However, when the Wistar rats were exposed to a 25 Gy single dose of hepatic irradiation, only mild hepatocellular damage and steatosis were observed 24 and 48 h after irradiation.49 These findings indicate that Wistar rats may be more radioresistant than SD rats, presenting strain disparity in responses to radiation. Therefore, a systemic comparison of strain disparity in hepatic radio-resistance is required to establish the most appropriate experimental animal model of RILD. In addition, the radiation dose influences the liver response to radiation. When the SD rats were exposed to 30 Gy of hepatic irradiation, radiation-induced liver fibrosis was detected 6 months after irradiation.50 However, when the SD rats were exposed to 60 Gy of hepatic irradiation, liver fibrosis was detected 8 weeks after irradiation.34 These observations imply that liver fibrosis increases as radiation doses increase. However, increasing radiation doses increases the chance of lethality. Therefore, Rave-Frank et al.36 employed fractionated irradiation, which is generally used in clinical RT, to minimize normal tissue toxicity. When the Wistar rats were exposed to liver-specific irradiation delivered in a fractionated dose of 2 Gy five times per week for 6 weeks (total dose 60 Gy), the irradiated livers showed upregulated ALP levels without necroinflammation and fibrosis 3 months after radiation. However, Zhang et al.34 showed that the same dose-irradiated SD rats by single irradiation presented hepatic sinus congestion, hepatocyte apoptosis and fibrosis 8 weeks after irradiation. These findings suggest that fractionated irradiation induces much less toxicity than single-dose irradiation. However, to clarify the effects of single and fractionated irradiation on the liver, strain-matched experiments following the same protocol are required.
Mice have been increasingly used to establish animal models of RILD, but they have been employed relatively less in RILD research compared to rats. Whole-body irradiation has been mainly used in past studies, but liver-specific irradiation tends to be used in more recent studies of radiation-induced liver response in mice. When female C57BL/6 mice were exposed to whole-body irradiation with a 20 Gy single dose, the livers contained accumulated fatty HCs, apoptotic cells, progenitors and MF-HSCs and demonstrated increased fibrosis 1 week after irradiation.37 Wang et al.51 also demonstrated a greater accumulation of fatty HCs and apoptotic cells in the livers of irradiated female rather than male mice after whole-body irradiation with a 6 Gy single dose. Expansion of progenitor cells and increased fibrosis were also observed in the livers of irradiated female, but not male, mice. These results suggest that female mice are more radiosensitive than males. This gender difference in radiosensitivity possibly influences the outcomes of experimental RILD in animal models. However, whole-body irradiation has several limitations, as mentioned above, in understanding radiation-induced hepatic responses. Recent studies have adopted hepatic irradiation for RILD research. Male mice that were exposed to upper region, abdomen-specific irradiation with a 6 Gy single dose presented increased levels of hepatic triglycerides, ALT/AST and apoptosis, fat accumulation in HCs, and enhanced fibrosis 6 weeks and 10 weeks after radiation; however, they showed none of the histopathological features of RILD.35 Kim et al.52 employed fractionated irradiation and, following hepatic response, conducted serial investigations. In this study, male C57BL/6 mice were exposed to liver-specific irradiation that was delivered in a fractionated dose of 6 Gy per week for 5 weeks (total dose 30 Gy). Some mice were killed 1 day after consecutive weekly irradiation to observe the acute response to radiation, and the others were killed 6 or 10 weeks after final irradiation to examine the late response to radiation. As a result, mice in the acute response model showed elevated levels of ALT/AST, apoptotic HCs and progenitor proliferation. Loss of parenchymal cells, hepatic congestion and severe fibrosis were observed in the late-response model. Liver-specific fractionated radiation-induced mild hepatic injuries in rats,36 whereas it caused severe damage in mice in the late-response model.52 However, these results cannot be compared because the species, radiation dose, frequency of fractionated radiation and follow-up intervals used are different. Relative irradiation dose by total animal volume should be considered.
Although hepatocellular injury and concomitant fibrotic response have been well established and are reproducible in irradiated rats and mice, VOD, a morphological hallmark of RILD, does not develop in them by radiation only. To cause VOD in these animals, chemicals such as monocrotaline (MCT) and 5-thiguanine are used. MCT is a toxic pyrrolizidine alkaloid and is known to induce VOD in experimental rodent models.53, 54 In the liver, MCT is metabolically activated into the toxic metabolite dehydromonocrotaline by the hepatic cytochrome P-450 enzymatic system. This toxic metabolite is converted into a stable nontoxic metabolite by glutathione (GSH) and then eliminated.55 Because centrilobular regions of the liver are rich in P-450 but poor in GSH, these areas are particularly sensitive to toxic agents.55 Therefore, MCT treatment results in the accumulation of toxic metabolites in the centrilobular areas, damaging SEC and central venular endothelial cells. This cell injury promotes severe hemorrhage, activation of the coagulation system and sinusoidal fibrin deposition, leading to VOD.38 These findings suggest that GSH is critically involved in the development of VOD. In addition, given that GSH is an important antioxidant that prevents oxidative stress and that oxidative stress is increased in the irradiated liver,32 GSH activity could be related to VOD formation in RILD. Although the detailed mechanism of radiation-induced liver injury differs from that of toxin-induced liver damage and it is unknown whether liver-specific irradiation influences the level and activity of GSH, studying the association of GSH and VOD can provide clues to understanding why VOD does not develop in small rodent models of RILD, eventually contributing to the establishment of suitable experimental rodent models for RILD.
Rabbit and dog
There have been additional efforts to develop experimental RILD in rabbits and dogs. When New Zealand white rabbits were exposed to a single dose (24–28 Gy or 36 Gy) of hepatic irradiation, neither changes to the portal liver architecture nor congestion of the sinusoids were evident in these animals.56 Cromheecke et al.57 reported that dogs presented macroscopic color and histopathological changes such as parenchymal fibrosis and liver cell atrophy after a single dose (20 Gy) of hepatic irradiation, although they failed to develop VOD. Shulman et al.58 showed that combined treatment with chemotherapy and RT- or MCT-induced acute VOD in dogs. However, chemotherapy alone can lead to VOD because of its cytotoxicity in humans and experimental animals, similar to MCT.58, 59 Thus, experimental animal models based on rabbits and dogs are currently limited in the study of RILD.
Nonhuman primates
Nonhuman primate models are considered the gold standard of animal models because they have a ⩾95% DNA sequence identity and very similar receptor- and pathway-related physiological responses compared to humans.60 Nonhuman primate models most closely reproduce the clinical, histopathological and pathophysiological aspects of radiation injury in humans. Several studies have used monkeys to evaluate radiation-induced hepatic injuries. When female rhesus monkeys were exposed to hepatic irradiation with 4.5 Gy per fractionated radiation for 8 fractions (total 36 Gy) or 2.5 Gy per fractionated radiation for 20 fractions (total 50 Gy), none of the monkeys developed classical VOD,61 suggesting that they might be resistant to the induction of significant hepatic injury by radiation alone. However, male cynomolgus monkeys that received fractionated hepatic radiation of more than 40 Gy showed marked veno-occlusive changes in the central veins similar to human VOD, including intimal edema, hemorrhage, elevated ALP, parenchymal congestion and a narrowed or completely obstructed lumen with mild fibrosis, 10 weeks after irradiation.62 In addition, cynomolgus monkeys presenting only mild increases in serum ALT and ALP levels with hepatic fractionated radiation of less than 36 Gy showed more severe changes in the liver and developed RILD when they received additional hepatic radiation ranging in duration from 6 months to 1 year. Because cynomolgus monkeys, not rodents, have shown hepatic venous injury, they are currently the only reproducible animal model resembling classic human RILD, suggesting that the livers of cynomolgus monkeys have a similar vascular sensitivity to the human liver in response to irradiation. This distinctive radiation sensitivity enables them to develop VOD, which is not reproduced in irradiated rodents. The reason for the difference in hepatic radiosensitivity between the monkey and the rodent is poorly understood, but elucidating this difference will provide a clue to understanding the development of VOD in RILD and establishing a small animal model of RILD.
Although various experimental animal models of RILD with pathologies similar to humans have been generated, they are still limited in RILD studies because of the absence of VOD. The use of cynomolgus monkeys enables the reproduction of experimental VOD, but their long lifespan, the high cost of studies and lower accessibility constitute a major burden for scientists.60 Therefore, if the physiological and pathological characteristics of RILD, including VOD, can be properly developed in small animal RILD models, they will have advantages over monkeys in elucidating the mechanisms of RILD. To obtain adequate rodent RILD models, experimental conditions, such as radiation dose by animal size, exposure time, single or fractionated irradiation and follow-up time to produce VOD, should be established and optimized. Furthermore, most researchers have employed an irradiated liver having neither tumors nor chronic diseases to study RILD. Therefore, these experimental models have some discrepancy in corresponding to the in vivo circumstance of patients with gastrointestinal cancers, including HCC or underlying chronic hepatic diseases, receiving RT. In particular, the liver baseline microenvironment exposed to radiation differs between human and experimental animals. Therefore, to better clarify the pathogenesis of RILD, further studies are necessary to investigate radiation-induced hepatic responses in animal models with gastrointestinal or liver cancers with or without underlying chronic disease.
Treatments of RILD and future prospects
Various strategies are being investigated to prevent or minimize radiation-induced hepatotoxicity.4, 10 There is growing interest in selective internal RT for HCC, also called radioembolization, which involves hepatic arterial infusion of yttrium-90 microspheres to deliver a higher radiation dose to the tumor vasculature relative to the surrounding normal parenchyma.63 Although the use of radioembolization may minimize the risk of serious radiation-induced hepatic toxicity, it still produces relevant toxic effects in nontumorous tissues that constitute radioembolization-induced liver disease.64 Stem cell-based therapy is a recently developed, notable treatment. Stem cell therapy aims to ameliorate the unintended side effects in normal tissues exposed to radiation by promoting the regeneration of irradiated normal tissues. The infusion of mesenchymal stem cell (MSC) or MSC-derived bioactive components was reported to prevent radiation-induced liver injury by inhibiting both apoptosis and inflammation in experimental animals,65, 66 suggesting the regenerative capability of MSCs in radiated tissues. However, the mechanism underlying the therapeutic or regenerative effects of MSCs in the damaged tissues caused by radiation remains unclear. Undesirable side effects possibly occur during the therapeutic application of MSCs in treating radiation-induced injuries. Without elucidating the microenvironment of radiation-induced damage, the application of MSCs or MSC-derived factors in the treatment of RILD is dangerous given that engrafted MSCs can differentiate into HCs as well as myofibroblasts, a major player in liver fibrosis, depending on the time frame of differentiation and the route of MSC injection.67 Therefore, further characterization of MSCs and investigations into the progression and microenvironment of RILD may be critical for ensuring the safety of MSC-based cell therapy. Given that HSC-mediated fibrogenesis is ongoing in RILD and VOD,23, 50 therapeutic strategies to control HSC function appear to have potential in the treatment of RILD. One of the cytokines-regulating HSC transdifferentiation, TGF-β, has been implicated in subendothelial and hepatic fibrosis in RILD.39, 50 TGF-β showed a radiation dose-dependent increase, and suppression of TGF-β was reported to reduce hepatic fibrosis in the irradiated livers of experimental animals.39, 50 Thus, anti-TGF-β therapy is a therapeutic strategy against RILD development. In addition, the Hh pathway is suggested to be a potential player in RILD progression.35, 37, 51, 52, 68 The expression of Hh signaling was reportedly enhanced in the livers of irradiated mice, and the blockade of Hh reduces hepatic toxicity and fibrogenic response by inhibiting myofibroblast accumulation.35 Kim et al.52 also showed that Hh signaling is activated and contributes to progressive hepatic fibrosis during both the early and late response to fractionated hepatic radiation in mice with incipient RILD. These results suggest that the Hh pathway is a potential target for novel therapeutic strategies for RILD.
In conclusion, RILD is a major limitation of RT in the treatment of liver cancer. Although the clinical characteristics of RILD patients have been relatively well described, understanding the pathogenesis of RILD has been hampered by the limitations of establishing a reproducible animal model for RILD, especially VOD. Therefore, the development of RILD animal models that are equivalent to human RILD is essential for understanding the underlying mechanisms of RILD and establishing novel therapeutic agents to reduce radiation-induced hepatic toxicity and improve patient survival.
Acknowledgments
This work was supported by a National Research Foundation of Korea (NRF) grant funded by the Korean government (MEST) (No 2014M2B2A9030333).
Footnotes
The authors declare no conflict of interest.
References
- Feng M, Ben-Josef E. Radiation therapy for hepatocellular carcinoma. Semin Radiat Oncol 2011; 21: 271–277. [DOI] [PubMed] [Google Scholar]
- Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin 2015; 65: 87–108. [DOI] [PubMed] [Google Scholar]
- Raza A, Sood GK. Hepatocellular carcinoma review: current treatment, and evidence-based medicine. World J Gastroenterol 2014; 20: 4115–4127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villanueva A, Hernandez-Gea V, Llovet JM. Medical therapies for hepatocellular carcinoma: a critical view of the evidence. Nat Rev Gastroenterol Hepatol 2013; 10: 34–42. [DOI] [PubMed] [Google Scholar]
- Hawkins MA, Dawson LA. Radiation therapy for hepatocellular carcinoma: from palliation to cure. Cancer 2006; 106: 1653–1663. [DOI] [PubMed] [Google Scholar]
- Delaney G, Jacob S, Featherstone C, Barton M. The role of radiotherapy in cancer treatment: estimating optimal utilization from a review of evidence-based clinical guidelines. Cancer 2005; 104: 1129–1137. [DOI] [PubMed] [Google Scholar]
- Benson R, Madan R, Kilambi R, Chander S. Radiation induced liver disease: a clinical update. J Egypt Natl Canc Inst 2016; 28: 7–11. [DOI] [PubMed] [Google Scholar]
- Lawrence TS, Robertson JM, Anscher MS, Jirtle RL, Ensminger WD, Fajardo LF. Hepatic toxicity resulting from cancer treatment. Int J Radiat Oncol Biol Phys 1995; 31: 1237–1248. [DOI] [PubMed] [Google Scholar]
- Khozouz RF, Huq SZ, Perry MC. Radiation-induced liver disease. J Clin Oncol 2008; 26: 4844–4845. [DOI] [PubMed] [Google Scholar]
- Guha C, Kavanagh BD. Hepatic radiation toxicity: avoidance and amelioration. Semin Radiat Oncol 2011; 21: 256–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li G, Wang J, Hu W, Zhang Z. Radiation-induced liver injury in three-dimensional conformal radiation therapy (3D-CRT) for postoperative or locoregional recurrent gastric cancer: risk factors and dose limitations. PLoS ONE 2015; 10: e0136288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan CC, Kavanagh BD, Dawson LA, Li XA, Das SK, Miften M et al. Radiation-associated liver injury. Int J Radiat Oncol Biol Phys 2010; 76: S94–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shulman HM, McDonald GB, Matthews D, Doney KC, Kopecky KJ, Gauvreau JM et al. An analysis of hepatic venocclusive disease and centrilobular hepatic degeneration following bone marrow transplantation. Gastroenterology 1980; 79: 1178–1191. [PubMed] [Google Scholar]
- Qiao J, Fu J, Fang T, Huang Y, Mi H, Yang N et al. Evaluation of the effects of preconditioning regimens on hepatic veno-occlusive disease in mice after hematopoietic stem cell transplantation. Exp Mol Pathol 2015; 98: 73–78. [DOI] [PubMed] [Google Scholar]
- Christiansen H, Saile B, Neubauer-Saile K, Tippelt S, Rave-Frank M, Hermann RM et al. Irradiation leads to susceptibility of hepatocytes to TNF-alpha mediated apoptosis. Radiother Oncol 2004; 72: 291–296. [DOI] [PubMed] [Google Scholar]
- Du SS, Qiang M, Zeng ZC, Ke AW, Ji Y, Zhang ZY et al. Inactivation of Kupffer cells by gadolinium chloride protects murine liver from radiation-induced apoptosis. Int J Radiat Oncol Biol Phys 2010; 76: 1225–1234. [DOI] [PubMed] [Google Scholar]
- Yamanouchi K, Zhou H, Roy-Chowdhury N, Macaluso F, Liu L, Yamamoto T et al. Hepatic irradiation augments engraftment of donor cells following hepatocyte transplantation. Hepatology 2009; 49: 258–267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee IJ, Seong J, Shim SJ, Han KH. Radiotherapeutic parameters predictive of liver complications induced by liver tumor radiotherapy. Int J Radiat Oncol Biol Phys 2009; 73: 154–158. [DOI] [PubMed] [Google Scholar]
- Ingold JA, Reed GB, Kaplan HS, Bagshaw MA. Radiation hepatitis. Am J Roentgenol Radium Ther Nucl Med 1965; 93: 200–208. [PubMed] [Google Scholar]
- Liang SX, Huang XB, Zhu XD, Zhang WD, Cai L, Huang HZ et al. Dosimetric predictor identification for radiation-induced liver disease after hypofractionated conformal radiotherapy for primary liver carcinoma patients with Child-Pugh Grade A cirrhosis. Radiother Oncol 2011; 98: 265–269. [DOI] [PubMed] [Google Scholar]
- Ogata K, Hizawa K, Yoshida M, Kitamuro T, Akagi G, Kagawa K et al. Hepatic injury following irradiation—a morphologic study. Tokushima J Exp Med 1963; 10: 240–251. [PubMed] [Google Scholar]
- Reed GB Jr, Cox AJ Jr. The human liver after radiation injury. A form of veno-occlusive disease. Am J Pathol 1966; 48: 597–611. [PMC free article] [PubMed] [Google Scholar]
- Sempoux C, Horsmans Y, Geubel A, Fraikin J, Van Beers BE, Gigot JF et al. Severe radiation-induced liver disease following localized radiation therapy for biliopancreatic carcinoma: activation of hepatic stellate cells as an early event. Hepatology 1997; 26: 128–134. [DOI] [PubMed] [Google Scholar]
- Cheng JC, Wu JK, Lee PC, Liu HS, Jian JJ, Lin YM et al. Biologic susceptibility of hepatocellular carcinoma patients treated with radiotherapy to radiation-induced liver disease. Int J Radiat Oncol Biol Phys 2004; 60: 1502–1509. [DOI] [PubMed] [Google Scholar]
- Chou CH, Chen PJ, Lee PH, Cheng AL, Hsu HC, Cheng JC. Radiation-induced hepatitis B virus reactivation in liver mediated by the bystander effect from irradiated endothelial cells. Clin Cancer Res 2007; 13: 851–857. [DOI] [PubMed] [Google Scholar]
- Guha C, Sharma A, Gupta S, Alfieri A, Gorla GR, Gagandeep S et al. Amelioration of radiation-induced liver damage in partially hepatectomized rats by hepatocyte transplantation. Cancer Res 1999; 59: 5871–5874. [PubMed] [Google Scholar]
- Brizel DM, Wasserman TH, Henke M, Strnad V, Rudat V, Monnier A et al. Phase III randomized trial of amifostine as a radioprotector in head and neck cancer. J Clin Oncol 2000; 18: 3339–3345. [DOI] [PubMed] [Google Scholar]
- Symon Z, Levi M, Ensminger WD, Smith DE, Lawrence TS. Selective radioprotection of hepatocytes by systemic and portal vein infusions of amifostine in a rat liver tumor model. Int J Radiat Oncol Biol Phys 2001; 50: 473–478. [DOI] [PubMed] [Google Scholar]
- Feng M, Smith DE, Normolle DP, Knol JA, Pan CC, Ben-Josef E et al. A phase I clinical and pharmacology study using amifostine as a radioprotector in dose-escalated whole liver radiation therapy. Int J Radiat Oncol Biol Phys 2012; 83: 1441–1447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taysi S, Koc M, Buyukokuroglu ME, Altinkaynak K, Sahin YN. Melatonin reduces lipid peroxidation and nitric oxide during irradiation-induced oxidative injury in the rat liver. J Pineal Res 2003; 34: 173–177. [DOI] [PubMed] [Google Scholar]
- Lee UE, Friedman SL. Mechanisms of hepatic fibrogenesis. Best Pract Res Clin Gastroenterol 2011; 25: 195–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robbins ME, Zhao W. Chronic oxidative stress and radiation-induced late normal tissue injury: a review. Int J Radiat Biol 2004; 80: 251–259. [DOI] [PubMed] [Google Scholar]
- Alati T, Van Cleeff M, Strom SC, Jirtle RL. Radiation sensitivity of adult human parenchymal hepatocytes. Radiat Res 1988; 115: 152–160. [PubMed] [Google Scholar]
- Zhang J, Zhou S, Zhou Y, Feng F, Wang Q, Zhu X et al. Hepatocyte growth factor gene-modified adipose-derived mesenchymal stem cells ameliorate radiation induced liver damage in a rat model. PLoS ONE 2014; 9: e114670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang S, Lee Y, Kim J, Hyun J, Lee K, Kim Y et al. Potential role of Hedgehog pathway in liver response to radiation. PLoS ONE 2013; 8: e74141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rave-Frank M, Malik IA, Christiansen H, Naz N, Sultan S, Amanzada A et al. Rat model of fractionated (2 Gy/day) 60 Gy irradiation of the liver: long-term effects. Radiat Environ Biophys 2013; 52: 321–338. [DOI] [PubMed] [Google Scholar]
- Wang S, Hyun J, Youn B, Jung Y. Hedgehog signaling regulates the repair response in mouse liver damaged by irradiation. Radiat Res 2013; 179: 69–75. [DOI] [PubMed] [Google Scholar]
- DeLeve LD, Shulman HM, McDonald GB. Toxic injury to hepatic sinusoids: sinusoidal obstruction syndrome (veno-occlusive disease). Semin Liver Dis 2002; 22: 27–42. [DOI] [PubMed] [Google Scholar]
- Anscher MS, Crocker IR, Jirtle RL. Transforming growth factor-beta 1 expression in irradiated liver. Radiat Res 1990; 122: 77–85. [PubMed] [Google Scholar]
- Carmona-Cuenca I, Roncero C, Sancho P, Caja L, Fausto N, Fernandez M et al. Upregulation of the NADPH oxidase NOX4 by TGF-beta in hepatocytes is required for its pro-apoptotic activity. J Hepatol 2008; 49: 965–976. [DOI] [PubMed] [Google Scholar]
- Yarnold J, Brotons MC. Pathogenetic mechanisms in radiation fibrosis. Radiother Oncol 2010; 97: 149–161. [DOI] [PubMed] [Google Scholar]
- Jung Y, Witek RP, Syn WK, Choi SS, Omenetti A, Premont R et al. Signals from dying hepatocytes trigger growth of liver progenitors. Gut 2010; 59: 655–665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verdelho Machado M, Diehl AM. Role of Hedgehog signaling pathway in NASH. Int J Mol Sci 2016; 17: E857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- da Silveira EB, Jeffers L, Schiff ER. Diagnostic laparoscopy in radiation-induced liver disease. Gastrointest Endosc 2002; 55: 432–434. [DOI] [PubMed] [Google Scholar]
- Lossi L, D'Angelo L, De Girolamo P, Merighi A. Anatomical features for an adequate choice of experimental animal model in biomedicine: II. Small laboratory rodents, rabbit, and pig. Ann Anat 2016; 204: 11–28. [DOI] [PubMed] [Google Scholar]
- Strachan RD, Kane PJ, Cook S, Chambers IR, Clayton CB, Mendelow AD. Immunosuppression by whole-body irradiation and its effect on oedema in experimental cerebral ischaemia. Acta Neurol Scand 1992; 86: 256–259. [DOI] [PubMed] [Google Scholar]
- Leiper AD. Late effects of total body irradiation. Arch Dis Child 1995; 72: 382–385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ozyurt H, Ozden AS, Cevik O, Ozgen Z, Cadirci S, Elmas MA et al. Investigation into the role of the cholinergic system in radiation-induced damage in the rat liver and ileum. J Radiat Res 2014; 55: 866–875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christiansen H, Batusic D, Saile B, Hermann RM, Dudas J, Rave-Frank M et al. Identification of genes responsive to gamma radiation in rat hepatocytes and rat liver by cDNA array gene expression analysis. Radiat Res 2006; 165: 318–325. [DOI] [PubMed] [Google Scholar]
- Du SS, Qiang M, Zeng ZC, Zhou J, Tan YS, Zhang ZY et al. Radiation-induced liver fibrosis is mitigated by gene therapy inhibiting transforming growth factor-beta signaling in the rat. Int J Radiat Oncol Biol Phys 2010; 78: 1513–1523. [DOI] [PubMed] [Google Scholar]
- Wang S, Lee K, Hyun J, Lee Y, Kim Y, Jung Y. Hedgehog signaling influences gender-specific response of liver to radiation in mice. Hepatol Int 2013; 7: 1065–1074. [DOI] [PubMed] [Google Scholar]
- Kim J, Wang S, Hyun J, Guy CD, Jung Y. Hedgehog signaling is associated with liver response to fractionated irradiation in mice. Cell Physiol Biochem 2016; 40: 263–276. [DOI] [PubMed] [Google Scholar]
- Zhang J, Sheng Y, Shi L, Zheng Z, Chen M, Lu B et al. Quercetin and baicalein suppress monocrotaline-induced hepatic sinusoidal obstruction syndrome in rats. Eur J Pharmacol 2016; 795: 160–168. [DOI] [PubMed] [Google Scholar]
- DeLeve LD, McCuskey RS, Wang X, Hu L, McCuskey MK, Epstein RB et al. Characterization of a reproducible rat model of hepatic veno-occlusive disease. Hepatology 1999; 29: 1779–1791. [DOI] [PubMed] [Google Scholar]
- Vion AC, Rautou PE, Durand F, Boulanger CM, Valla DC. Interplay of inflammation and endothelial dysfunction in bone marrow transplantation: focus on hepatic veno-occlusive disease. Semin Thromb Hemost 2015; 41: 629–643. [DOI] [PubMed] [Google Scholar]
- Herfarth KK, Munter MW, Groene HJ, Delorme S, Peschke P, Debus J. Absence of tissue reaction after focal high-dose irradiation of rabbit liver. Acta Oncol 2006; 45: 865–869. [DOI] [PubMed] [Google Scholar]
- Cromheecke M, Piers BA, Beekhuis H, ter Veen H, Sluiter WJ, Grond AK et al. Tissue damage after single high-dose intraoperative irradiation of the canine liver: evaluation in time by means of radionuclide imaging and light microscopy. Radiat Res 2000; 154: 537–546. [DOI] [PubMed] [Google Scholar]
- Shulman HM, Luk K, Deeg HJ, Shuman WB, Storb R. Induction of hepatic veno-occlusive disease in dogs. Am J Pathol 1987; 126: 114–125. [PMC free article] [PubMed] [Google Scholar]
- Cefalo MG, Maurizi P, Arlotta A, Scalzone M, Attina G, Ruggiero A et al. Hepatic veno-occlusive disease: a chemotherapy-related toxicity in children with malignancies. Paediatr Drugs 2010; 12: 277–284. [DOI] [PubMed] [Google Scholar]
- VandeBerg JL, Williams-Blangero S. Advantages and limitations of nonhuman primates as animal models in genetic research on complex diseases. J Med Primatol 1997; 26: 113–119. [DOI] [PubMed] [Google Scholar]
- Stephens LC, Peters LJ, Ang KK. Tolerance of rhesus monkey liver to ionizing radiation. Radiat Oncol Investig 1993; 1: 279–284. [Google Scholar]
- Yannam GR, Han B, Setoyama K, Yamamoto T, Ito R, Brooks JM et al. A nonhuman primate model of human radiation-induced venocclusive liver disease and hepatocyte injury. Int J Radiat Oncol Biol Phys 2014; 88: 404–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salem R, Hunter RD. Yttrium-90 microspheres for the treatment of hepatocellular carcinoma: a review. Int J Radiat Oncol Biol Phys 2006; 66: S83–S88. [DOI] [PubMed] [Google Scholar]
- Gil-Alzugaray B, Chopitea A, Inarrairaegui M, Bilbao JI, Rodriguez-Fraile M, Rodriguez J et al. Prognostic factors and prevention of radioembolization-induced liver disease. Hepatology 2013; 57: 1078–1087. [DOI] [PubMed] [Google Scholar]
- Chen YX, Zeng ZC, Sun J, Zeng HY, Huang Y, Zhang ZY. Mesenchymal stem cell-conditioned medium prevents radiation-induced liver injury by inhibiting inflammation and protecting sinusoidal endothelial cells. J Radiat Res 2015; 56: 700–708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mouiseddine M, Francois S, Souidi M, Chapel A. Intravenous human mesenchymal stem cells transplantation in NOD/SCID mice preserve liver integrity of irradiation damage. Methods Mol Biol 2012; 826: 179–188. [DOI] [PubMed] [Google Scholar]
- Volarevic V, Nurkovic J, Arsenijevic N, Stojkovic M. Concise review: therapeutic potential of mesenchymal stem cells for the treatment of acute liver failure and cirrhosis. Stem Cells 2014; 32: 2818–2823. [DOI] [PubMed] [Google Scholar]
- Kabarriti R, Guha C. Hedgehog signaling and radiation induced liver injury: a delicate balance. Hepatol Int 2014; 8: 316–320. [DOI] [PMC free article] [PubMed] [Google Scholar]