Abstract
Background:
A departmental audit in March 2015 revealed significant mortality rate of 40% in blunt chest trauma patients (much greater than the global 25%). A study was thus planned to study morbidity and predictors of mortality in blunt chest trauma patients admitted to our hospital.
Methods:
This study was a prospective observational study of 139 patients with a history of blunt chest trauma between June 2015 and November 2015 after the Institutional Ethics Committee approval in April 2015. The sample size was calculated from the prevalence rate in our institute from the past medical records.
Results:
The morbidity factors following blunt chest injuries apart from pain were need for Intensive Care Unit stay, mechanical ventilation, and pneumonia/acute respiratory distress syndrome. Significant predictors of mortality in our study were SpO2 <80 at the time of presentation, Glasgow coma scale ≤ 8, patients with four or more rib fractures, presence of associated head injury, Injury Severity Score >16, and need for mechanical ventilation. By calculating the likelihood ratios of each respiratory sign, a clinical score was devised.
Conclusion:
The modifiable factors affecting morbidity and mortality were identified. Mild to moderate chest injury due to blunt trauma is difficult to diagnose. The restoration of respiratory physiology has not only significant implications on recovery from chest injury but also all other injuries. It is our sincere hope that the score we have formulated will help reduce mortality and morbidity after further trials.
Keywords: Blunt chest trauma, clinical score, likelihood ratios, morbidity, mortality
INTRODUCTION
A departmental audit of trauma patients revealed a mortality rate of 40% in blunt chest trauma patients far above the global 25%. The mortality in patients with missed chest injuries was 15.1% as compared to 7.6% in patients who had their injuries diagnosed during primary survey. An observational study was planned, so that we could identify modifiable causes of morbidity and mortality. The second objective was to assess the importance of specific respiratory signs that would help suspect, investigate, diagnose, and decide intervention in patients of blunt trauma by devising a clinical score. It was hypothesized this score would help reduce missed injuries and hence morbidity and mortality brought on due to the delay in their diagnosis. The score would have to be validated by a randomized controlled trial (RCT), which would be the second step of our endeavor to reduce current mortality rates.
METHODS
The study was designed as a prospective observational study. All cases with blunt chest trauma either as a sole presentation or as a part of polytraumatic insults were included in the study as patients. All patients above 12 years of age were included in the study. Informed consent was taken from all who were included. Consent was taken from legal guardians of patients between 12 and 18 years of age. Penetrating chest injuries were excluded from the study. Patients were followed throughout their course in the ward. The data were entered into the Microsoft Excel spreadsheet and statistical analysis was done using measures of central tendencies. Incidence of pneumonia, need for mechanical ventilation, and need for intensive care were calculated. Chi-square test was used to assess significant predictors of mortality. For this, patients were divided into two groups depending on the presence or absence of parameters determining mortality. These parameters were selected from historical studies. Sensitivity and specificity of each respiratory clinical sign was calculated and likelihood ratio (LR) of each sign was derived. The LRs were used to formulate a clinical score.
RESULTS
The most common mechanism of injury in blunt chest trauma patients was road traffic accidents. Seventy-seven of the 139 patients were injured in road traffic accidents, 38 by accidental fall. Sixteen patients were assault victims and eight sustained chest injuries by being victims of railway accidents.
All patients sustained rib fractures, but 77.6% (108) patients were found to have pneumothorax (68), hemothorax (34), and flail segment (6). One patient had a diaphragmatic injury. The remaining 22.4% had isolated rib fractures only. When the number of rib fractures in a patient of chest trauma was ≥4, there was a statistically significant increase in mortality (P = 0.002).
No esophageal, tracheobronchial, cardiac, or aortic injuries were seen during this period. One patient had a thoracic vertebral fracture with paraplegia and another had a scapular fracture. Some patients of chest trauma also had injury to other systems. Head injuries were found in 22.3% (31) patients. Ten (7.1%) patients had concomitant blunt abdominal injury and 9.3% (13) patients suffered musculoskeletal trauma to the extremities. The presence of concomitant head injury significantly contributed to mortality in patients of blunt chest trauma [Table 1].
Table 1.
Glasgow coma scale ≤8 and mortality

Morbidity
Morbidity was studied in terms of pneumonia, need for mechanical ventilation, and intensive care. The incidence of pneumonia was high at 17.2% (24), 9.4% (41) patients needed intensive care, and 22.3% (31) needed mechanical ventilation. Overall, the incidence of morbidity was 30.2%. Pain is an unavoidable complication of any trauma. However, it is modifiable cause of morbidity. Pain was studied from the purview of the most effective method of pain relief in blunt chest trauma as all patients would experience it.
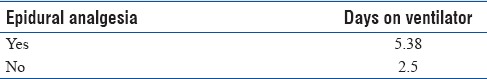
Oral analgesia, intravenous (IV) analgesia, and epidural analgesia were the methods used. Twenty-five patients were given epidural analgesia. These were patients who had persistent pain despite oral and/or IV analgesia or patients who had a flail segment. Of six patients with a flail segment, three patients were preemptively given epidural analgesia after the first bolus of IV analgesic. The epidural analgesia brought down the number of days the patients spent on the ventilator by half (2.5 vs. 5.38) [Table 2].
Table 2.
Days on ventilator
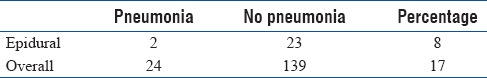
It also reduced the incidence of pneumonia significantly (8% vs. 17%) [Table 3].
Table 3.
Incidence of pneumonia in epidural versus nonepidural pain relief
Mortality
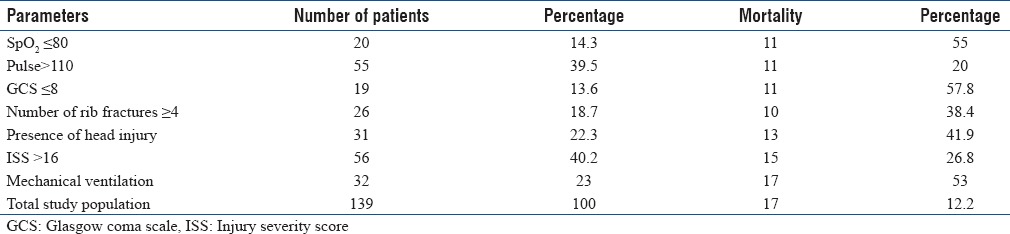
All patients who succumbed to their injuries were specifically divided into two groups on the basis of the presence or absence of certain signs (pulse >110, SpO2 >80%, Glasgow coma scale [GCS] ≤8), score (Injury Severity Score [ISS] >16), positive finding on investigations (rib #>4, presence of head injury on computed tomography [CT]), additional systemic injury, and need for mechanical ventilation. With the exception of abdominal or extremity injury, all other parameters were found to contribute significantly to mortality [Table 4].
Table 4.
Factors predicting mortality
To formulate a clinical score using established respiratory signs, the sensitivity and specificity of each sign was calculated. Thereafter, the LR of each sign was derived from sensitivity and specificity [Table 5]. An LR >1 is considered statistically significant. A sign with LR between 1 and 2 was scored as 1. Any sign with LR between 2 and 3 was scored as 2. Any LR >3 was scored as 3 [Table 5].
Table 5.
Sensitivity and specificity of respiratory signs and likelihood ratios
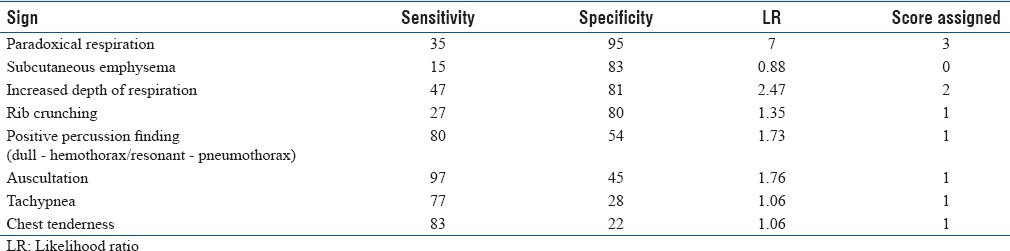
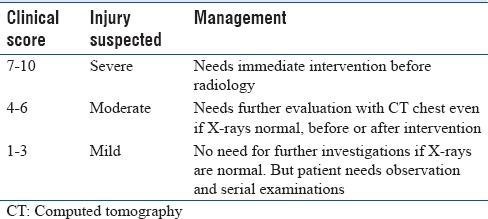
The total score derived from adding up all the individual scores was 10. Severe injury was calculated to have a score >6 as the maximum score possible by adding up the two major signs with highest score 3 and two moderate signs with highest score 2 and any one minor sign is 6. A score between 4 and 6 was assigned to signify moderate injury and a score between 1 and 3 was assigned to signify mild injury. Based on severity, the plan of management differs [Table 6].
Table 6.
Proposed clinical score and interpretation
DISCUSSION
Road traffic accidents were responsible for 55% of blunt chest injuries. Accidental falls (low impact) accounted for 27.3% of the cases with assault and railway accidents responsible for the rest. Similar to other recent studies,[1] most of the patients in our study were between 21 and 40 years of age. The mortality in patients >50 years was 13.25% as against 9% in those below 50 years of age. Unlike most recent studies, this difference in mortality in our study was not statistically significant.
All patients had rib fractures, of which 77.6% (108 patients) were accompanied by pneumothorax 62.9% (68 patients) or hemothorax 31.48% (34 patients). Nearly 5.5% (6) patients were found to have a flail chest. One patient (0.9%) had a diaphragmatic injury. The study by Demirhan et al. found pneumothorax (28.8%), hemothorax (24.1%), flail chest (1.7%), and diaphragmatic injuries (1.8%).[2] Similar results were also seen in other studies except with Sirmali et al., who found hemothorax was more commonly associated with rib fractures than pneumothorax.[3,4,5,6] Almost 22.4% of the patients had isolated rib fractures. Twenty-six patients had 4 or more ribs fractured which significantly increased the mortality, 38.4% versus 8.5% in those with < 4 ribs fractured (P = 0.002). Similar to findings of other studies, where mortality increased significantly if three or more ribs were fractured.[6,7,8,9] The force of impact causing multiple fractures is great. It causes underlying pulmonary contusions and is associated with injury to other systems, increasing severity of injury and mortality. Other equally important parameters that contribute to mortality are advanced age and underlying lung disease. No patients in our study were found to have underlying lung disease. One reason for this may be that young patients (21–40) constituted the majority. Hence, perhaps, chronic lung disease was not yet established. The fewer older patients may fortuitously have escaped developing chronic lung disease. In our study, the mortality in the older age group was not significantly higher than the mortality in those below fifty (13.25% vs. 9%). Curtis et al. devised an early activation protocol based on age, underlying lung disease, more than three rib fractures, response to analgesia, and respiratory signs. This protocol helped reduce the incidence of pneumonia, need for ventilation, and mortality in isolated blunt chest injury. They also found low impact injury more common in older patients.[10] In an observational study, Maher and Jayathissa also found that patients in the older age group sustained injuries with low impact chest trauma and were more likely to develop complications.[11] This group also exhibited higher mortality. A study by battle devised and validated a prognostic score considering age, underlying lung disease, number of ribs fractured, and development of pneumonia during recovery. Our score is based purely on respiratory signs and the aim was not to miss any chest injury whatever be the grade of impact, irrespective of age, and preexisting lung disease.
Other systems that were concomitantly injured in patients with chest injuries were head injury, limb injuries, and abdominal injuries. The presence of head injury and a GCS ≤8 was associated with an increase in mortality in blunt chest trauma patients (P = 0.022). A study by Jovanovic et al. found that GCS was less reliable predictor of fatal outcome. It also found that patients with coexisting chest and head injury had a higher incidence of ventilator-associated pneumonia increasing the mortality.[12] Respiratory depression secondary to raised intracranial pressure worsens hypoxia and hypoxia worsens prognosis of head injury. Hence, the respiratory system and the neurological system fed off each other, worsening prognosis in trauma. Abdominal and limb injuries did not significantly increase mortality in chest trauma patients (P = 0.707). No cardiac, aortic, esophageal, or tracheobronchial injuries were found in our patients. Thoracic vertebral fracture with paraplegia was found in one patient and another had associated scapular fracture with chest injury.
Morbidity was studied in terms of the development of pneumonia, need for mechanical ventilation, and need for intensive care. The incidence of pneumonia was 17.2% (24), which was higher than the 3.2% and 3.5%, respectively, in studies by Demirhan et al. and Veysi et al. 22.3% (31) of patients needed mechanical ventilation. Sixty-five percent of patients needed it due to the development of pneumonia. The patients that made up the remaining 35% were patients who had a flail segment 10% (3), GCS < 8 due to head injury 20% (6), and postoperative patients 5% (2). 29.4% (41) patients needed intensive care. All patients who needed mechanical ventilation (31) were a subset of the group that needed intensive care (75.6%). The remaining 24.4% (10) were patients who had epidural catheters 70% (7) and were being watched for respiratory depression and patients with pneumonia who did not require mechanical ventilation 30% (3). Since pneumonia is a proven factor contributing to mortality in multiple past studies, this study focused on assessing its contribution to morbidity only.
Pain is an unavoidable but a modifiable factor contributing to morbidity. In this study, oral (12), IV (102), and epidural analgesia (25) were used. The use of intercostal, pleural blocks was not seen in our study period. Since oral and IV analgesia is still the most commonly used method of pain relief, epidural analgesia was used if pain persisted despite the oral or IV analgesia. Epidural was also used preemptively in patients who had flail segments (3). Use of epidural analgesia brought down the number of days on ventilator by half and significantly reduced the incidence of pneumonia (8% vs. 26%). Studies by Wisner and Gage et al. have already established the advantages of epidural analgesia, but these were retrospective studies.[13,14] A systematic review by Unsworth et al. found evidence that with three or more rib fractures, epidural analgesia provides more effective pain relief in comparison with other analgesic modalities. However, these studies were limited to patients >65 years.[15] Due to the observations in our study and as per the suggestions of Unsworth et al., a randomized trial is long overdue.
SpO2 <80% at presentation was associated with a significant increase in mortality (P = 0.01). Associated neurological injury or hypovolemia may have contributed to or aggravated the hypoxia. A pulse >110 at presentation (P = 0.03) goes in favor of hemodynamic instability and hence hypoxia. A GCS ≤8 (P = 0.02) and head injury (P = 0.0001) were also statistically significant contributors to increased mortality as was the presence of four or more rib fractures (P = 0.002), ISS score >16 (P = 0.01), and need for mechanical ventilation (P = 0.01). ISS has stood the test of time in being able to predict mortality. Mortality when one system is affected is between 4% and 8%. This increases to 13%–15% when one more system is involved and 30%–40% when two more systems are involved. A potential limitation of this study was that while studying the predictors of mortality, the two groups into which patients were divided were not matched for injury severity. Parameters such as age and preexisting comorbid conditions were not matched.
Of these, factors amenable to modification are saturation, pulse, and a low GCS due to unstable hemodynamics. Özpek et al. found hemodynamic instability and need for transfusion to be reliable predictors of mortality in all trauma patients.[1] A low GCS due to underlying head injury cannot be modified except through the management of head injury.
The need for mechanical ventilation can be reduced as demonstrated by the use of epidural analgesia. Since the major indication for mechanical ventilation in our patients was pneumonia, it goes without saying that bringing down the incidence of pneumonia will also reduce mortality. Another important intervention that needs mention is the use of rib fixation techniques. Tanaka et al. and Granetzny et al. conducted RCTs describing the use of surgical rib fixation in multiple rib fractures and flail chest. These studies found a decrease in mechanical ventilation, intensive care stay, and incidence of pneumonia in the surgically treated group versus the conservatively managed group.[16,17] Surgical fixation of fractured ribs is, however, not a part of the protocol at our institute at this time and hence was not seen in this study. The principle followed by our institute is that intercostal muscles are sufficient to make the fractured ends of ribs contact and heal spontaneously. Multiple rib fractures can cause acute respiratory failure, but positive ventilation can expand the lung adequately under due analgesic cover. The prostheses used for rib fixation are anterior locking plates, intramedullary nails or wires, anterior struts, and absorbable plates, but each has its own problems. The number of ribs fractured and severity of injury cannot be modified except by preventing or dampening primary impact.
It was seen that in addition to the factors mentioned above, delayed diagnosis of chest injuries in blunt chest trauma was also contributing to morbidity and mortality. The incidence of missed injuries in blunt chest trauma patients was an unacceptable high 46% according to our audit. Severe chest injury is difficult to miss because the patient's condition is unstable enough to require immediate and undivided attention and care of the trauma unit. To salvage such a patient who is also generally hemodynamically unstable, intervention is needed before investigation. Intervention could be in the form of needle or tube thoracostomy or thoracotomy or intubation. Blunt chest injuries generally need the placement of a tube thoracostomy.[1] Higher investigations such as CT are done even if X-rays are positive because there is high suspicion of additional undiagnosed injury if patient is hemodynamically stable. A good example is aortic injury, which cannot be diagnosed by X-rays. It is patients with moderate and mild injury who have a higher incidence of missed injuries, as they do not draw immediate attention or because the injury is asymptomatic initially or there is confusion in interpreting respiratory signs, particularly percussion. This group includes but is not restricted to older patients with low impact trauma. We formulated a clinical score to help us decide if patients needed intervention first or further investigation like CT or observation alone after the mandatory chest X-ray [Table 6]. Depending on whether or not there is improvement on initial management, the patient may need further investigation. Moderate injury would need further investigation by a CT scan regardless of chest X-ray finding. Mild injury does not need CT after X-rays. Such a patient may be observed and serially reevaluated [Table 6]. It has also been demonstrated in studies that patients whose injuries are diagnosed only on CT have a better prognosis than those whose rib fractures are diagnosed on X-rays and this is particularly true when the injury is mild enough to be missed on X-rays.[18] In no patient should CT scans be used to replace clinical examination especially in patients with mild injuries. This will minimize radiation exposure in such patients.
Nejati et al. calculated sensitivity and specificity of respiratory signs, but they used them to decide if X-rays would be needed.[19] As of this day, no score similar to the one we have formulated exists so that may compare it to ours. CT chest is the gold standard for diagnosis now due to its high sensitivity and specificity for entire spectrum of blunt chest injuries. However, CT is possible only when the patient is hemodynamically stable. In addition to physical examination, the current recommended basic investigation is a chest X-ray. However, chest X-rays are known to miss 50% of rib fractures.[20] This is where CT is most useful. The indications for CT at present in blunt chest trauma are mechanism of injury, clinical deterioration, mediastinal widening, presence of flail segment, diaphragmatic injury, aortic injury, spine fractures, sternal fractures, and tracheobronchial injuries.[21] Most of these injuries need to be suspected clinically to order a CT, which is difficult for a surgeon in training. It remains to be seen if the clinical score we have devised will actually help reduce the morbidity and mortality by early diagnosis of moderate and mild injury through appropriate trials in larger number of patients. We also hope that it will give surgeons in training an objective method to decide intervention, investigation, or observation in a patient of blunt chest trauma regardless of age and preexisting lung disease.
The other advantages we foresee are optimal utilization of hospital resources and reduction in hospital stay. The clearance from our Institutional Ethics Committee for a randomized controlled study of the clinical score and cost–benefit analysis is pending approval as of this day. We hope to start the second phase as soon as it is approved.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We would like to thank Dr. A. K. Gvalani, Professor and Head of Surgery, Seth G. S. Medical College and K.E.M. Hospital, Parel, Mumbai - 400 012, India, and Dr. Anuj Sharma, JR3, Department of Surgery, Seth G. S. Medical College and K.E.M. Hospital, Parel, Mumbai - 400 012, India.
REFERENCES
- 1.Özpek A, Yücel M, Atak I, Bas G, Alimoglu O. Multivariate analysis of patients with blunt trauma and possible factors affecting mortality. Ulus Travma Acil Cerrahi Derg. 2015;21:477–83. doi: 10.5505/tjtes.2015.43077. [DOI] [PubMed] [Google Scholar]
- 2.Demirhan R, Onan B, Oz K, Halezeroglu S. Comprehensive analysis of 4205 patients with chest trauma: A 10-year experience. Interact Cardiovasc Thorac Surg. 2009;9:450–3. doi: 10.1510/icvts.2009.206599. [DOI] [PubMed] [Google Scholar]
- 3.Veysi VT, Nikolaou VS, Paliobeis C, Efstathopoulos N, Giannoudis PV. Prevalence of chest trauma, associated injuries and mortality: A level I trauma centre experience. Int Orthop. 2009;33:1425–33. doi: 10.1007/s00264-009-0746-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hasbahçeci M, Ozpek A, Basak F, Caliskan M, Ener BK, Alimoglu O. Factors affecting mortality in blunt thoracic trauma. Ulus Travma Acil Cerrahi Derg. 2013;19:127–32. doi: 10.5505/tjtes.2013.54782. [DOI] [PubMed] [Google Scholar]
- 5.Management of Thoracic Trauma: Experience at Ayub Teaching Hospital, Abbottabad. [Last cited on 2016 Aug 26]. Available from: https://www.researchgate.net/publication/43019832_Hospital_Abbottabad . [PubMed]
- 6.Sirmali M, Türüt H, Topçu S, Gülhan E, Yazici U, Kaya S, et al. A comprehensive analysis of traumatic rib fractures: Morbidity, mortality and management. Eur J Cardiothorac Surg. 2003;24:133–8. doi: 10.1016/s1010-7940(03)00256-2. [DOI] [PubMed] [Google Scholar]
- 7.Liman ST, Kuzucu A, Tastepe AI, Ulasan GN, Topcu S. Chest injury due to blunt trauma. Eur J Cardiothorac Surg. 2003;23:374–8. doi: 10.1016/s1010-7940(02)00813-8. [DOI] [PubMed] [Google Scholar]
- 8.Svennevig JL, Bugge-Asperheim B, Geiran OR, Vaage J, Pillgram-Larsen J, Fjeld NB, et al. Prognostic factors in blunt chest trauma. Analysis of 652 cases. Ann Chir Gynaecol. 1986;75:8–14. [PubMed] [Google Scholar]
- 9.Perna V, Morera R. Prognostic factors in chest traumas: A prospective study of 500 patients. Cir Esp. 2010;87:165–70. doi: 10.1016/j.ciresp.2009.11.020. [DOI] [PubMed] [Google Scholar]
- 10.Curtis K, Asha SE, Unsworth A, Lam M, Goldsmith H, Langcake M, et al. ChIP: An early activation protocol for isolated blunt chest injury improves outcomes, a retrospective cohort study. Australas Emerg Nurs J. 2016;19:127–32. doi: 10.1016/j.aenj.2016.06.002. [DOI] [PubMed] [Google Scholar]
- 11.Maher L, Jayathissa S. Blunt chest trauma in a non-specialist centre: Right treatment, right place? Emerg Med Australas. 2016;28:725–9. doi: 10.1111/1742-6723.12680. [DOI] [PubMed] [Google Scholar]
- 12.Jovanovic B, Milan Z, Djuric O, Markovic-Denic L, Karamarkovic A, Gregoric P, et al. Twenty-eight-day mortality of blunt traumatic brain injury and co-injuries requiring mechanical ventilation. Med Princ Pract. 2016;25:435–41. doi: 10.1159/000447566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wisner DH. A stepwise logistic regression analysis of factors affecting morbidity and mortality after thoracic trauma: Effect of epidural analgesia. J Trauma. 1990;30:799–804. doi: 10.1097/00005373-199007000-00006. [DOI] [PubMed] [Google Scholar]
- 14.Gage A, Rivara F, Wang J, Jurkovich GJ, Arbabi S. The effect of epidural placement in patients after blunt thoracic trauma. J Trauma Acute Care Surg. 2014;76:39–45. doi: 10.1097/TA.0b013e3182ab1b08. [DOI] [PubMed] [Google Scholar]
- 15.Unsworth A, Curtis K, Asha SE. Treatments for blunt chest trauma and their impact on patient outcomes and health service delivery. Scand J Trauma Resusc Emerg Med. 2015;23:17. doi: 10.1186/s13049-015-0091-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tanaka H, Yukioka T, Yamaguti Y, Shimizu S, Goto H, Matsuda H, et al. Surgical stabilization of internal pneumatic stabilization? A prospective randomized study of management of severe flail chest patients. J Trauma. 2002;52:727–32. doi: 10.1097/00005373-200204000-00020. [DOI] [PubMed] [Google Scholar]
- 17.Granetzny A, Abd El-Aal M, Emam E, Shalaby A, Boseila A. Surgical versus conservative treatment of flail chest. Evaluation of the pulmonary status. Interact Cardiovasc Thorac Surg. 2005;4:583–7. doi: 10.1510/icvts.2005.111807. [DOI] [PubMed] [Google Scholar]
- 18.Livingston DH, Shogan B, John P, Lavery RF. CT diagnosis of rib fractures and the prediction of acute respiratory failure. J Trauma. 2008;64:905–11. doi: 10.1097/TA.0b013e3181668ad7. [DOI] [PubMed] [Google Scholar]
- 19.Nejati A, Khalaj S, Azizkhani R, Shahryarian S, Kolahdouzan M, Hossein MS. Evaluating validity of clinical criteria for requesting chest X-rays in trauma patients referred to emergency room. Adv Biomed Res. 2012;1:22. doi: 10.4103/2277-9175.98125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bansidhar BJ, Lagares-Garcia JA, Miller SL. Clinical rib fractures: Are follow-up chest X-rays a waste of resources? Am Surg. 2002;68:449–53. [PubMed] [Google Scholar]
- 21.Van Hise ML, Primack SL, Israel RS, Müller NL. CT in blunt chest trauma: Indications and limitations. Radiographics. 1998;18:1071–84. doi: 10.1148/radiographics.18.5.9747608. [DOI] [PubMed] [Google Scholar]


