Abstract
The government of India has done remarkable work on commissioning a government funded prehospital emergency ambulance service in India. This has both public health implications and an economic impact on the nation. With the establishment of these services, there is an acute need for standardization of education and quality assurance regarding prehospital care provided. The International Joint Working Group has been actively involved in designing guidelines and establishing a comprehensive framework for ensuring high-quality education and clinical standards of care for prehospital services in India. This paper provides an independent expert opinion and a proposed framework for general operations and administration of a standardized, national prehospital emergency medical systems program. Program implementation, operational details, and regulations will require close collaboration between key stakeholders, including local, regional, and national governmental agencies of India.
Keywords: Emergency medicine, emergency medical systems, India, prehospital emergency ambulance
INTRODUCTION
The rapid progress and continued development in India over the recent years has resulted in increased expectations of its citizens regarding the prevailing quality of health care services, especially in the area of acute and emergency setting. This dynamic has placed the responsibility on local, regional, and national leaders and service providers to meet or exceed current international standards.[1] The opportunity exists to successfully achieve this goal through an enabling legislative framework, with the help of suitable organizations and experts available.[2] To that end, we must ask the question, “Why is a legislative framework necessary to oversee and regulate prehospital service providers?”
The answer to the above question is complex and requires a very close examination of the dynamic interplay between the health system, the community being served, and the patient being treated. Survival in cases of trauma, emergency, and critical illnesses (such as stroke, myocardial infarctions, diabetic complications, asthma, sepsis, meningitis, and snakebite) depends on the speed of access to high-quality health care. Critical components in this vital chain include the universal notification system, properly trained prehospital emergency care provider (emergency medical technician [EMT] and/or paramedic), and a well-equipped ambulance. The “chain of survival” in India must be expanded to embrace more than just cardiac arrests. It should also be streamlined and simplified to include three fundamental pillars supported by correct and timely actions: “Bring the patients alive, keep them alive, and make them better.”[3]
The objective of this position paper is to draw attention to the urgent need for a national regulatory framework of licensing, governance, standardization, benchmarking, and audit of prehospital service providers and ambulances.
JUSTIFICATION
There is general agreement that tremendous value is provided to the society by the high quality of prehospital services. Supporting evidence is plentiful, including well-documented, substantially higher survival rates for cardiac arrests in places with advanced paramedical care, even among developed nations.[4] Prompt and correct ambulance dispatch and response in cases of heart attacks, strokes, and traumas literally make the difference between life, disability, and death. The impact on patients, families, communities, and the nation is substantial. It is therefore within the scope of responsibilities of high-level decision makers to devote their full effort and prompt attention to improving the quality of prehospital ambulance services in India by establishing and organizing the national regulatory body for this purpose – to mirror the current international norm.
THE BACKGROUND
Without standardization, constant risk exists of the emergence and/or the continued presence of significant disparities in the delivery of emergency care and ambulance service coverage, even within the same region. The ambulance should not be merely a motorized vehicle to deliver patients to a hospital but rather a well-equipped and technologically advanced platform that safely and quickly transports patients in the best possible condition to an appropriate hospital.
The overall process of designing national standards and their implementation is dependent on defining goals and objectives and ensuring that essential elements including trained, registered, properly licensed, and supervised employees, as well as the required equipment, are all synergistically present to ensure a timely response and to optimize the chances of survival and successful outcome for the patient. The prevailing quality standards for all ambulance services should be modified to ensure uniform, high-quality delivery of emergency care on par with the best services currently provided in India.
THE CURRENT SITUATION AND NEEDS ASSESSMENT
In India, critical need exists for a nationally valid legal definition of an “ambulance.” In addition, national guidelines are required to effectively educate, certify, and monitor various prehospital care providers and services in a standardized, benchmark-driven fashion. Steps are currently underway to address the above issues at the national level through various committees, but it is important to note that the Indian health system is based on a shared responsibility model, featuring a hybrid (independent and autonomous) operations model between the central government and various state governments. therefore, definitions put forward by the central ministries may not universally apply at the local level in some states.[4]
The situation is further complicated by the lack of clarity about the designation of ministry-specific tasks and responsibilities within the central government. thus, it is not always clear which authority is ultimately responsible for establishing the policy framework for ambulances. Currently, the burden is shared between several ministries which include the Health and Family Welfare, the Department of Ayurveda, Yoga and Naturopathy, Unani, Siddha, and Homeopathy (AYUSH), human resource development (HRD), education, road, and transport. Due to a large number of governmental agencies involved and the complexity of the problem, the potential exists for bureaucratic delays and confusion.[5]
With reference to ambulances, the regulatory oversight is similarly fragmented. The mechanical, engineering, roadworthiness, and vehicular specifications are under the aegis of the road and transport ministry. However, the medical aspects are specified by the Health Department. HRD and AYUSH ministries are also closely concerned with the development and delivery of provider skills and competency-based training for prehospital service personnel. Further oversight in this area exists from the apex court which has given important judicial directives about prehospital care.
Dedicated Expert Committees have reported on the bigger issues concerned with professions allied to medicine.[6] Efforts are underway to coordinate and collate the development and implementation of standards related to both equipment and service in this vitally important area of healthcare. However, these attempts are severely handicapped in the absence of orchestrated legislative framework and/or dedicated agency support.[7]
RESOURCE ALLOCATION FOR PREHOSPITAL CARE: FUNDING, VEHICLES, MEDICAL EQUIPMENT, AND PERSONNEL
Resource availability and total required investment are important components in ensuring the development and maintenance of a high-quality ambulance service. Insufficient number of vehicles, lack of required medical equipment, or understaffing all negatively affect both the effectiveness and the quality of service provided. In recent years, the number of claims misrepresenting a broad range of “motorized vehicles” as “ambulances” has increased substantially. This is a dangerous phenomenon that is accompanied by an expansion of institutions claiming to provide adequate prehospital care.
At the personnel level, numerous anecdotal examples have been reported of unqualified or underqualified people claiming to be either trained and/or qualified to work within the prehospital sector. The vast majority of large corporate hospitals and local nursing homes advertise their own ambulance services, with no regulatory oversight over the quality of care, equipment adequacy, or personnel competency training. Within the current, largely unregulated paradigm, the quality of services rendered is extremely difficult to ascertain in the absence of benchmarks and a legislative framework. The entire spectrum of prehospital care, from the ambulances to the staff manning these vehicles, requires urgent standardization, much like it is done in other countries with well-developed emergency medical systems (EMS) infrastructure.
The gap in the provision of ambulance services is further notable in that reliable data does not exist in India about the number of vehicles available for prehospital care and clinical outcomes (i.e. morbidity and mortality) attributable to associated treatment provided. Approximately 15,000 ambulances are registered in India under official government provision. However, reports by unofficial sources[5] suggest that the actual number of vehicles is two times larger. Various often misleading names are given to these different types of prehospital services ranging from “maternity” to “advanced life support” EMS.
Taking into account official and unofficial sources, nearly 30,000 ambulances would exceed the minimum recommended number of emergency transport vehicles for the Indian population, as outlined by the WHO experts.[2] In terms of absolute numbers, these figures are more consistent with ambulance volumes servicing mid-size European economies.[6] Yet, in the case of an emergency, the quality of the patient experience in India is not comparable to that in Europe.[5] Since significant gaps exist at multiple levels of the Indian prehospital infrastructure, there continue to be striking differences between “quantitative” and “qualitative” realities of ambulance-based service delivery.
NEED FOR STANDARDIZED TRAINING FOR EMERGENCY MEDICAL SYSTEMS PROVIDERS IN INDIA
The quality of human resources is among the most important outcome determinants in emergency healthcare situations. In other words, an ambulance without skilled personnel will likely fail to provide service as intended, or in a worst case scenario, may actually represent a danger. After all, it is the paramedic prehospital service provider, and not the vehicle, that ensures proper emergency care. Although the apparently high number of vehicles claimed to be ambulances on Indian roads, the experience of the recipients of these services is substandard compared to other countries. One reason for this discrepancy could be the lack of adequate formal training for prehospital service providers (EMTs and paramedics).
Given the reported number of ambulances in India, nearly 120,000 adequately trained front-line staff would be required to provide sufficient emergency services coverage. This field personnel estimate would be required in addition to employees already servicing emergency call centers, various administrators, educators, and support staff. First responders should be uniformed, regulated, and trained providers. In comparable countries and other emerging economies of the world, such as South Africa and Brazil, there are well-established university level courses for prehospital providers. However, in India, no similar formal educational curricula exist at the national or state level.
Some corporate service providers in India do conduct life support and other short courses[8,9] to prepare their ambulance drivers for the work of patient rescue, transfer, and transport. Apart from the lack of funding and systemic incentives, it is likely that the lack of a legislative framework of regulation, registration, and licensing is responsible for the existing gap in the availability of training and professional certification services. In the absence of content standardization and appropriate quality benchmarks, it is difficult to assess local value and impact of the largely disjointed local initiatives.
Under the current emergency prehospital service paradigm in India, the interface between responsibility and communication between the hospital, medical ambulance control, and EMS provider is not clearly defined due to lack of a legislative framework and reliable communication systems (and/or standards). In one of its previously published white papers, INDUSEM has drawn attention to the need for a single number access to ambulances[10] such as “911” in the United States. To this day, this national priority in India is still managed locally. A considerable gap exists between the dynamic emergency needs of a critically ill patient, adequate vital signs monitoring, and the need to administer medications before arrival at definitive emergency care destination.
EMERGENCY MEDICAL SYSTEMS EDUCATION IN THE UNITED STATES: A GOOD MODEL FOR INDIA?
In the United States, there is a well-established paradigm for EMS education which is called the National Emergency Medical Services Education Standards. These standards contain objective criteria and expected achievement levels for entry-level EMS personnel. Requirements and parameters are outlined in the National EMS Scope of Practice Model. Although educational programs must adhere to the standards, this format allows for diverse implementation methods to meet local needs and evolving educational practices. The less prescriptive format of the standards also allows for ongoing revisions of content, consistent with emerging scientific evidence and community standards of care. Figure 1 displays the schematic representation of the EMS Model in the U.S.
Figure 1.
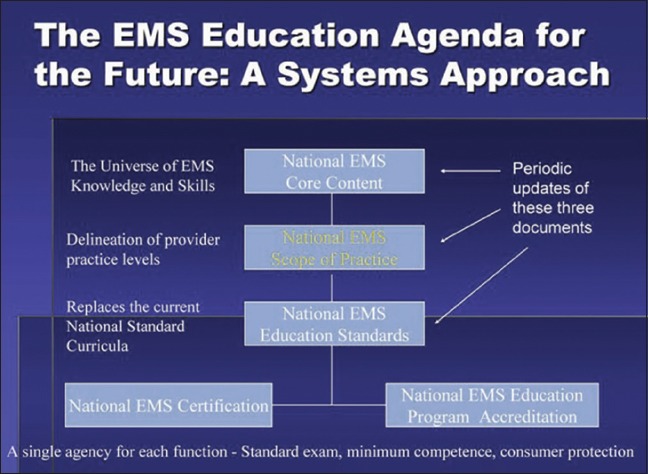
The emergency medical systems model.[11]
This is further divided into different levels of training-EMR, EMT, advanced EMT, and paramedic. Figure 2 depicts a sample of the difference in curricula.
Figure 2.
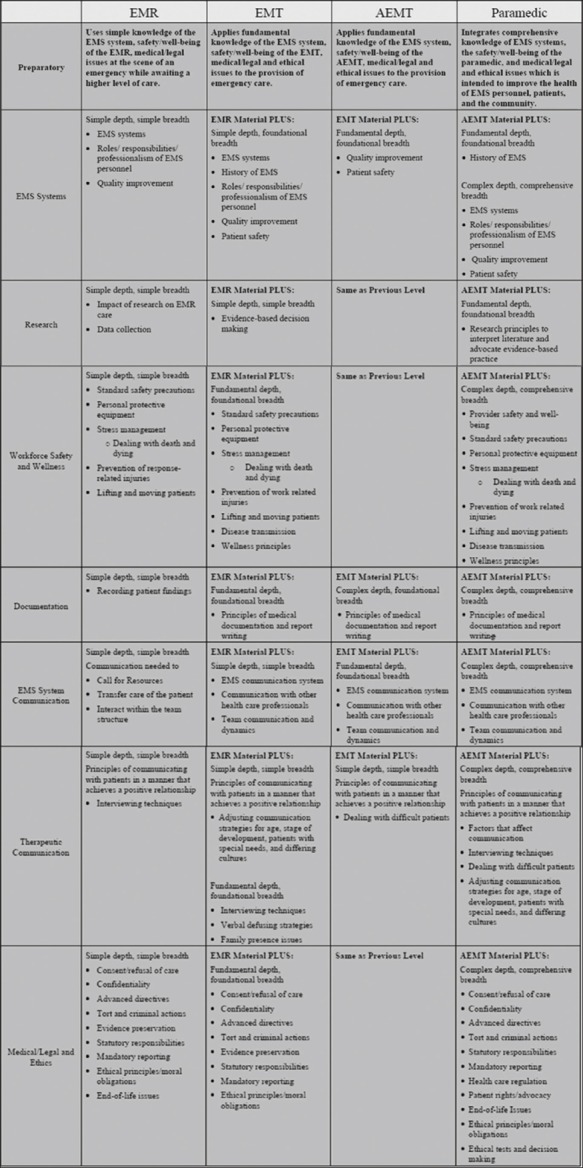
Levels of emergency medical systems training.[11]
NATIONAL PREHOSPITAL EMERGENCY MEDICAL SERVICES COUNCIL FOR INDIA: THE CRITICAL CONDUIT FOR CHANGE
In India, there is no standard certification for prehospital ambulance personnel. Consequently, anyone and everyone can claim this title, without significant repercussions. Given the absence of a legislative regulatory framework, and more importantly, since registration or licensing of the prehospital providers is not required, the current status quo is unlikely to change. As a result, there is a clear and present danger of putting the citizen at further risk during an already stressful and potentially life-threatening emergency.[7]
As previously outlined, the current state of the ambulance and prehospital services in India can be characterized as disorganized and highly fragmented.[5] Although India has a strong and proud tradition of excellence in health care,[3] this tradition has not yet been extended fully to encompass prehospital services. In an emergency situation, the challenge of quickly, efficiently, and safely transporting the patient to the hospital remains to be solved. Difficulties persist due to the systemic lack of adequate training, supervision, certification, and auditing. When the above factors are combined with insufficient standardization and lax enforcement of quality benchmarks pertaining to lifesaving equipment and the ambulance vehicle itself, the risk for critical systemic failures becomes apparent.
In the interest of maintaining a balanced discussion, it is duly acknowledged that India has indeed taken a major leap forward in terms of better defining and controlling the number of vehicles on its roads aiming and claiming to provide ambulance services. In addition, regulations are now in place to better facilitate ambulance transport within the incredibly congested urban settings. Thus, the importance and need have been recognized in this domain-perhaps more so than is currently needed, and likely out of proportion to other, more pressing issues. Increasingly, daily traffic now gives way to ambulances, and the police plays a supportive role during the transfer of acute patients. In some states of India, there has been notable progress in recruiting AYUSH doctors for providing prehospital services.
There are also several points of strength, from which further success can be built. For example, larger ambulance organizations already provide basic in-house training to their staff.[8,9,12] Some state governments in India have developed and implemented “Quick Medical Response Teams” training programs for the front line staff, but significant gaps remain.[10] These and other similar initiatives can serve as a foundation for a more broad-based implementation of critical didactic and skills training for prehospital providers.
Despite these early, optimistic achievements, critical need still exists for a robust framework that has broad systemic impact coupled with a national mandate. Significant disparities between states in India are noteworthy as some states have quite advanced prehospital systems while others have rudimentary systems or none at all. There is also a parallel need to develop efficient digital infrastructure to ensure reliable monitoring, auditing, and benchmarking of established standards across the entire country. In this context, the establishment of national governance is urgently required.
Perhaps, the most important recent development is the recognition of critical skills as the foundation for building a sustainable future of prehospital care in India. The Skills Development Council has already completed substantial work. However, much more needs to be done to complete this crucial process. The National Accreditation Board for Hospitals and Healthcare Providers (NABH)[13] has established a valuable precedence of benchmarking the inspection and certification process to include emergency departments. The existing templates, experience, and expertise can very easily be expanded and translated to assist with the accreditation process for the prehospital emergency services.
KEY RECOMMENDATIONS
International Joint Working Group (IJWG) makes evidence-based scientific recommendations for immediate review and consideration to ensure the standardization of prehospital care and harmonization of the existing framework with focus on improving the quality of prehospital emergency care services in India.
As its core mission, the National prehospital emergency medical service (PEMS) Council would be required to specify the standards of care, the governance, performance and quality improvement registry structure, as well as the license and review process to ensure that all citizens in India receive high-quality prehospital service when afflicted by serious illness or injury.
Benefiting from substantial international expertise, INDUSEM is uniquely positioned to provide a comprehensive framework for designing robust and sustainable systems necessary to oversee the training and education of prehospital service providers, the assurance of regular skills updates and verifications, competency maintenance, performance improvement, and proper supervision.
The proposed National PEMS Council should receive the mandate and assume the responsibility for oversight, review, and resolution of the entire range of issues identified above, including the legal specifications and requirements for defining an ambulance, regardless of whether air-, land-, or water-based. In addition, oversight should encompass the human and technical resources, up to and including pertinent fee structures and enforcement penalties.
The proposed National PEMS Council will transform the quality of emergency services in India with beneficial impact throughout the entire “chain of survival.” In a previous White Paper, the international experts on behalf of INDUSEM have observed the followings:[3,14]
“Emergency medical services (EMS) are new to India even in the metropolitan cities. Ambulances from both the public and private sectors are not well equipped or staffed by well-trained personnel capable of managing prehospital care. There is an absence of a well-designed first responders system with responsibly not clearly defined between different public and private stakeholders. This inefficiency of overlap between stakeholders combined with large, unaccounted for gaps, has led to almost a third of patients succumbing to death before hospital and only one-fifth receiving any medical care within an hour.”
Further observations in another white paper by INDUSEM expert group include these comments:[3,14]
“The weak link remains: The present prehospital care set-up is largely geared for handling medical emergencies, and not traumas.”
INDUSEM believes that inattention to prehospital services creates a real risk of avoidable loss of life and worsening global burden of disease in India. This risk becomes, especially, pertinent when one considers the demographics of heart disease, hypertension, diabetes, respiratory illness, and trauma. Urgent attention to the following recommendations, through robust contextually sensitive review and targeted development, as well as the prompt delivery of concrete solutions for the following parameters will be required to bring the quality of acute care in India to the level consistent with that of other countries:[15,16]
Establishment of a National PEMS Council and state level PEMS
Establishment of a curriculum, entry qualifications, and exit competencies for prehospital and emergency/trauma care providers similar to other nations such as United States, UK, and Australia where such systems are well developed. Institutes of National Importance such as the All India Institute of Medical Sciences and their faculty could be a valuable resource to achieve these goals
Creation of a Medical Council of India [MCI]/NBE recognized postgraduate super specialty training program in prehospital EMS
Establishment of quality benchmarks and evaluation parameters for equipment, care processes, and human resources under the regulatory control of NABH
Establishment of an integrated clinical approach to the care of trauma and acutely ill or critically injured patients
Establishment of an Indian version of the chain of survival focused on “bringing the patient alive, keeping the patient alive, and making the patient better”
Establishment of a training and accreditation system for prehospital emergency and trauma care
Establishment of local, regional, and international public–private partnerships to harvest and nurture the best talents
Create a digital infrastructure to collect data on education provided and services delivered so that policies can be designed based on “big data” analytics
Prompt and proper attention to maternal and child health and safeguarding of vulnerable patients including women and the elderly age group
Defining and implementing best technical specifications for prehospital trauma and emergency care, prehospital triage to transport patients to hospitals with correct and compatible services, including inter-hospital transfers
Establishment of a unique, national emergency number to access multi-level prehospital care and response
Marketing the services and creating parameters for recruitment of skilled labor for prehospital services to improve job opportunities and ensure the best outcome for patients.
Building an education framework: Below are some urgent needs in the education system of prehospital care:
There is an acute need for standardized guidelines for EMS training institutes
A critical need exists for standardized guidelines to admit, train, evaluate, and certify EMS health care providers in the country. The various EMS service providers have diverse criteria to hire staff and lack uniformity in training leading to disparities in the provision of care
Robust safety and quality accreditation standards and benchmarks for EMS Services must be established
There is a need for a national and state level regulatory and accountability framework to exist uniformly across the nation.
PROPOSED STRUCTURE OF OPERATIONS, ROLES AND RESPONSIBILITIES
The IJWG proposes the following structure for the councils at the national level for prehospital emergency medical response service (NPEMS) and at the state level (SPEMS) which can be constituted through a special act in Parliament. The proposed NPEMS Council will cooperate, coordinate, and collaborate with the SPEMS in light of the Constitution of India that health is mainly a state, but also a central government, responsibility. the NPEMS will fall under the ministry of health and Family Welfare (MoHFW) Government of India. SPEMS will fall under the state ministry at the state level. The NPEMS Council will work closely with the SPEMS. Figure 3 summarizes the proposed Indian EMS system that is described above.
Figure 3.
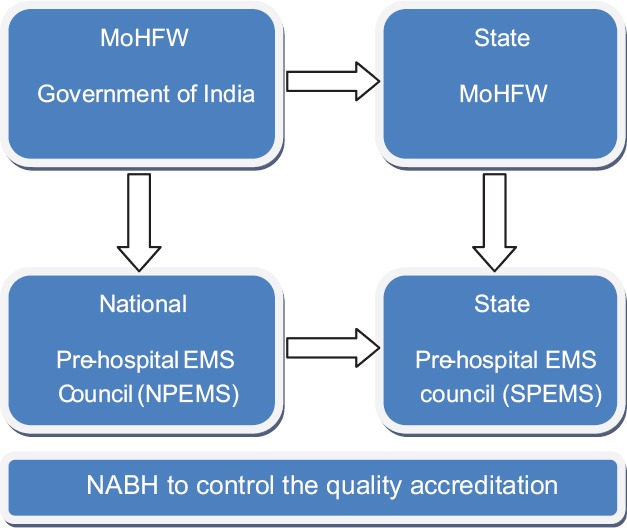
Proposed framework
Proposed roles of the NPEMS council
Commission, regulate, and accredit EMS training schools and formalize the Training Curriculum across the country
Formulate rules and regulations to mandate criteria to admit candidates to the EMS schools and administer these schools:
Address concerns and complaints in regards to violation of rules
Work with the NABH to institute a code of quality and monitor it across EMS services in the country
Create the Digital Infrastructure for collecting Data on education provided and Services delivered across the country
Make Policy Decisions based on BIG DATA gathered from Schools and PEMS providers across India.
Proposed roles of the SPEMS Council
Abide by the rules and regulations set by NPEMS Council
Provide License to Practice as EMS in the state and maintain a registry of all Licensed EMS personnel in that State
Set rules for certification and recertification examinations of EMS Personnel and conduct examinations in partnership with universities
Appoint committees to create clinical practice guidelines to manage patients across EMS Services in the nation
Address all concerns sent by the NPEMS Council and all concerns raised by citizens as regards the EMS Systems in the state
Work with NABH through NPEMS Council to institute the code of quality and monitor it across EMS services in the country
Manage, operate, and monitor the EMS services and the quality of patient care provided by the EMS services in the country
Collect Data on Education provided and Services Delivered which will enable the NPEMS to design policy and recommend bettering practices.
APPOINTMENT OF EMERGENCY MEDICAL SERVICE DIRECTORS
INDUSEM suggests that every Council should have an EMS Director who is a qualified postgraduate allopathic physician who can monitor the EMS under the council's jurisdiction. The EMS Director will appoint a Chief Executive Officer who will administer operations and clinical care across the services. The Government may consider whether the Council should be fully autonomous or work under a suitable ministry such as MoHFW, MoRHT, HRD, or AYUSH.
POSTGRADUATE TRAINING IN EMERGENCY MEDICAL SYSTEMS
As in the US, there should be a similar EMS fellowship and board certification program since being an EMS director brings with it great position of responsibility. The MCI and National Board of Examinations should consider starting an EMS specialty degree (DM/DNB) open to MD/DNB in emergency medicine, pediatrics, internal medicine, surgery, orthopedics, preventive and social medicine, and obstetrics and gynecology. EMS is a specialty, in and of itself, that encompasses administration, clinical protocol development, resource management, and disaster health.
CONCLUSIONS
There is no doubt or dispute about the need for maintaining and accelerating the evolutionary development of prehospital care in India for the benefit of the nation and its people. The above evidence-based and detailed recommendations of INDUSEM are an important milestone toward achieving the highly desirable national objectives of improving outcomes for acutely ill and injured patients in India, bringing it to a world-class level as already achieved in the treatment of cancer and heart disease.
The core focus of this INDUSEM White Paper is to build on recent achievements, to improve the skills of service providers across the entire country, and to standardize the legal framework for services through the establishment of a national and state level NPEMS and SPEMS Councils. It is important to emphasize that NPEMS is a national program that requires a coordinated approach between central and state governments.
There are lessons that can be learned from the US EMS system, but this framework suggests a progressive recommendation that NABH accredit the Indian EMS system for provision of quality healthcare. By mandating NABH to accredit and regulate the quality of prehospital care, India will be a leader in taking such a progressive step.
The specific and unique characteristics of Indian healthcare must be kept in mind when designing specific prehospital programs and interventions. The context specific design and delivery of acute emergency, trauma, and critical care services will remain a challenge unless tackled systematically with public–private partnerships.
In summary, this white paper is an important step to ensure adequate prehospital support for more than 1.2 billion of citizens of India. This is why the Government of India should invest heavily in creating a robust system that will build, in a sustainable fashion, on synergies between foundations already in place and newly designed standardized protocols and procedures. The final framework should ensure continued quality improvement and unrelenting emphasis on patient welfare and safety.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Kobusingye OC, Hyder AA, Bishai D, Hicks ER, Mock C, Joshipura M. Emergency medical systems in low-and middle-income countries: Recommendations for action. Bull World Health Organ. 2005;83:626–31. [PMC free article] [PubMed] [Google Scholar]
- 2.Pal R, Agarwal A, Galwankar S, Swaroop M, Stawicki SP, Rajaram L, et al. The 2014 academic college of emergency experts in India's INDO-US Joint Working Group (JWG) white paper on “developing trauma sciences and injury care in India”. Int J Crit Illn Inj Sci. 2014;4:114–30. doi: 10.4103/2229-5151.134151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gautam V, Mishra M, Gupta S, Singh AR. Inter-Hospital transfer: Essential concepts for health care systems under resource constraints. Asian EMS J. 2016;2:14–8. [Google Scholar]
- 4.Rajan S, Wissenberg M, Folke F, Hansen CM, Lippert FK, Weeke P, et al. Association of bystander cardiopulmonary resuscitation and survival according to ambulance response times after out-of-hospital cardiac arrest. Circulation. 2016;134:2095–104. doi: 10.1161/CIRCULATIONAHA.116.024400. [DOI] [PubMed] [Google Scholar]
- 5.Singh A. Current Demography of Ambulance Services in India. Personal Communication. 2016 [Google Scholar]
- 6.From Paramedics to Allied Health Sciences: landscaping the journey and way forward. OWSA [Internet] [Last accessed on 2017 Jul 28]. Available from: http://southasia.oneworld.net/resources/from-paramedics-to-allied-health-sciences-landscaping-the-journey-and-way-forward .
- 7.Galwankar S. Current Status and Trends in the Delivery and Development of Pre-hospital Acute Emergency and Trauma Care Services in India. Personal Communication. 2016 [Google Scholar]
- 8.Paramedic training in India: The Fortis Emergency Medical Service Program - Emergency Live [Internet] [Last accessed on 2017 July 28]. Available from: http://www.emergency-live.com/en/equipment/paramedic-training-in-india-the-fortis-emergency-medical-service-program/
- 9.Paramedical courses, EMT Training, disaster management | IIEMS [Internet] [Last accessed on 2017 July 28]. Available from: http://iiems.org/
- 10.Gautam V. QMRT: Capacity Building in Bihar, India, to Improve First Response at the Front Line of Trauma and Emergency Care: International EMS Conference. Delhi: 2013. [Google Scholar]
- 11.NHTSA. National Emergency Medical Services Education Standards. 2016. [Last accessed on 2017 July 28]. Available from: https://www.ems.gov/pdf/811077a.pdf .
- 12.World Health Organization. Emergency Medical Services Systems in the European Union: Report of an Assessment Project Co-Ordinated by the World Health Organization. WHO Regional Office for Europe; 2008. [online] [Last accessed on 2017 July 20]. Available at: https://ec.europa.eu/digital-agenda /sites/digital-agenda /files/WHO.pdf .
- 13.National Accreditation Board for Hospitals & Healthcare Providers (NABH) [Internet] [Last accessed on 2017 July 28]. Available from: http://www.nabh.co/
- 14.Joshi A, Rajhans P, Galwankar S, Arquilla B, Swaroop M, Stawicki S, et al. Academic College of Emergency Experts in India's INDO-US Joint Working Group (JWG) White Paper on the Integrated Emergency Communication Response Service in India: Much more than just a number! J Emerg Trauma Shock. 2013;6:216–23. doi: 10.4103/0974-2700.115354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Emergency Services Review: A comparative review of international Ambulance Service best practice - aace.org.uk [Internet] [Last accessed on 2017 Jul 28]. Available from: https://aace.org.uk/resources/emergency-services-review-a-comparative-review-of-international-ambulance-service-best-practice-2/
- 16.Braun O, McCallion R, Fazackerley J. Characteristics of midsized urban EMS systems. Ann Emerg Med. 1990;19:536–46. doi: 10.1016/s0196-0644(05)82186-9. [DOI] [PubMed] [Google Scholar]


