Abstract
National surveillance data show a sustained decline in the incidence rate of diagnosed diabetes, which has been heralded as a success in the battle against diabetes in the U.S. In this Perspective, we take a closer look at these data and provide additional insights to help interpret these trends. We examine multiple sources of data on the prevalence and incidence of diabetes in the U.S. as well as data on trends in diabetes risk factors to provide context for these national surveillance findings. Although some of the incidence decline may represent real progress against diabetes, it is likely that there are also nonbiological factors at play, especially changes in diagnostic criteria for diabetes. We present and discuss data that suggest improved detection and changes in screening and diagnostic practices may have resulted in the depletion of the “susceptible population.” Providing this context for the recent declines in new diabetes diagnoses observed in national data is critical to help avoid misinterpretation. We argue that it is premature to declare victory against the epidemic of diabetes in the U.S. and discuss how we might better focus current public health efforts, including a specific emphasis to address prediabetes.
Introduction
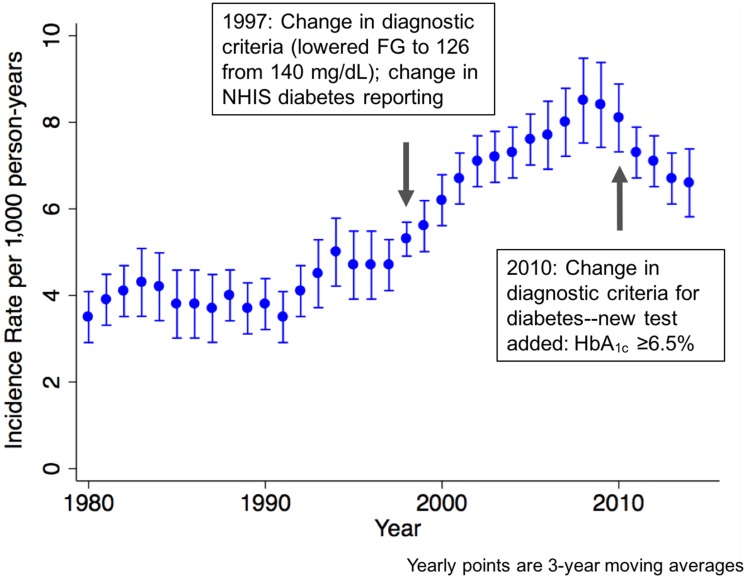
After many years of observing steady increases in diabetes in the U.S., the Centers for Disease Control and Prevention published data from the National Health Interview Survey (NHIS) in JAMA: The Journal of the American Medical Association in 2014 (1) and updates on their website in 2015 that showed substantial and sustained age-adjusted decreases in diabetes incidence from 2008 to 2014 (Fig. 1). This finding of decreases in the rate of diagnosed diabetes was covered in high-impact venues including The New York Times, CBS News, and other major media outlets (2,3). Surveillance data like those from the NHIS help us identify trends but cannot tell us what biological, behavioral, or clinical patterns are (most) responsible for the trends. Here, we provide analysis and supporting data to help contextualize the observed U.S. incidence trends and we discuss the implications for clinical practice, public health, and policy.
Figure 1.
Age-adjusted diabetes incidence rate and 95% CIs, 1980–2014, NHIS. FG, fasting glucose. Source data: http://www.cdc.gov/diabetes/statistics/incidence/fig2.htm.
Design of the NHIS
In interpreting these trends, it is critical to understand the design of the NHIS, its approach to data collection, and the diabetes case definition used. The NHIS is an annual nationally representative cross-sectional survey conducted by the National Center for Health Statistics of the Centers for Disease Control and Prevention. Interviews are conducted with approximately 40,000 households across the country. Participants answer about 1 h of questions. Included are the following queries: “Other than during pregnancy, have you EVER been told by a doctor or other health professional that you have diabetes or sugar diabetes?” and “How old were you when a doctor or other health professional FIRST told you that you had diabetes or sugar diabetes?” (4). Newly occurring (incident) cases of diabetes are defined as those diagnosed at the person’s current age plus half of those diagnosed at the person’s current age minus 1 (since the exact date of diagnosis of diabetes is unknown). The denominator for the incidence rate is the number of people without a previous history of diagnosed diabetes. It is worth noting that the NHIS diabetes questions changed in 1997. Prior to 1997, identification of diabetes diagnoses in NHIS involved proxy reporting, which may have resulted in underascertainment of the condition (5).
Interpreting Diabetes Incidence Trends
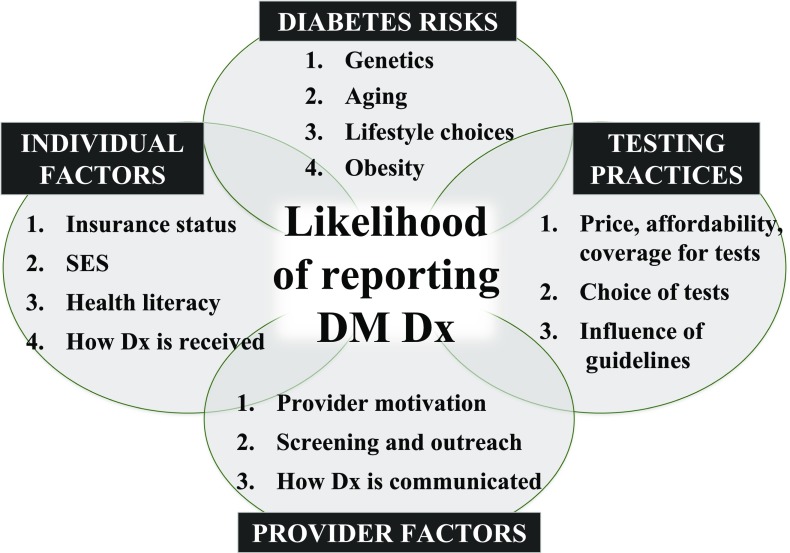
Because the NHIS survey is cross-sectional in nature and data are captured via questionnaires only, it is not possible to determine what underlies the changes observed (6). Routinely, other data are examined to corroborate and/or inform surveillance data. One approach to corroborate incidence trends is to examine incidence trends in parallel data sources—for example, claims data. Another approach involves examining changes in prevalence and mortality. A third approach is to examine trends in the specific factors that are related to incidence. In the case of diabetes, the number and rate of new diagnoses are not only related to changes in risk factors in the population but also to changes in the test(s) and diagnostic criteria used to determine diabetes status and the practices of providers offering, administering, interpreting, and conveying results of the test (Fig. 2). Although not an exhaustive list, increases and decreases in any of these factors could impact the frequency of diabetes testing, probability of diagnosis, and awareness of status and could therefore influence how participants respond to national survey questions. Of note, the changing demography of the U.S. may be playing a role in the trends observed. Specifically, minority race/ethnic groups appear to have higher physiological susceptibility to diabetes than non-Hispanic whites, although they also tend to be of lower socioeconomic status and have less access to health care. However, the balance of these influences remains unclear, as NHIS trend data also suggest recent diabetes incidence declines in Hispanics and non-Hispanic blacks.
Figure 2.
Conceptual model depicting factors associated with likelihood of self-reporting diabetes in national surveys. DM, diabetes mellitus; Dx, diagnosis; SES, socioeconomic status.
To contextualize the overall NHIS incidence trends, we examined trends in prevalence, mortality, and diabetes diagnostic criteria and screening practices, drawing from national data and published literature.
Incidence Trends From Other Data Sources
Consistent with incidence data from the NHIS, data from insured populations show flat or declining rates of new diabetes diagnoses. The Surveillance, Prevention, and Management of Diabetes Mellitus (SUPREME-DM) study, a diverse open cohort of 7 million insured adults in integrated health systems across 10 U.S. states, reported a roughly stable annual incidence rate of total diabetes of approximately 10 to 11 cases per 1,000 people between 2006 and 2011 (7). In addition, claims data from all 50 U.S. states show that the annual rate of new diabetes diagnoses declined from 2007 to 2012, from 10.1 per 1,000 people to 6.5 per 1,000 people (8).
Trends in Diabetes Prevalence and Mortality
Over the past two decades, mortality rates in people with diagnosed diabetes have declined considerably (9,10). Meanwhile, using both self-reported diagnoses and objectively measured biochemical data from the National Health and Nutrition Examination Survey (NHANES), the prevalence of total diabetes (undiagnosed plus diagnosed diabetes) has increased modestly over the decade, from ∼10–12% in 2000 to 12–14% in 2011 (11,12). National data on the prevalence of diagnosed diabetes from the NHIS and the Behavioral Risk Factor Surveillance System (BRFSS) are also consistent with a more moderate increase over this time period and a more recent flattening of prevalence since 2011 (13,14). Together, declining mortality and flatter prevalence is in keeping with the declining incidence of diabetes as observed in the NHIS data.
Trends in Major Diabetes Risk Factors
Three of the most important determinants of diabetes risk are age, adiposity, and prediabetes. The rates of diabetes shown in Fig. 1 are adjusted for age, meaning that they account for the changing age structure of the U.S. population over time. Thus, the aging of the U.S. population cannot account for the observed trends in diabetes incidence from the NHIS. The increase in overweight and obesity prevalence in the U.S. population, most commonly and reliably measured using BMI (weight in kg divided by height in m2), has been shown to explain the majority of cases of diabetes and increasing trends over time (12,15,16). Indeed, the increase in obesity (BMI exceeding 30 kg/m2) over the past half century in the U.S. is staggering: just over 10% of U.S. adults were obese in the 1960s, compared with almost 40% of adults now (17,18). The current combined prevalence of overweight and obesity is over 70% (18). Compared with decades past, the rate of increase in obesity prevalence has slowed; however, there have not been any overall decreases in obesity in U.S. adults and, in fact, the most recent data show a small increase (17).
By definition, people with prediabetes are at high risk for subsequent development of diabetes. Prediabetes is a condition defined by the same biochemical measures used to screen and diagnose diabetes (19). The term “prediabetes” serves to identify those individuals with glucose or glycated hemoglobin (HbA1c) values below the threshold for a diagnosis of diabetes but high enough to consider them at significant risk for development of diabetes and related cardiometabolic conditions in the future. The burden of prediabetes in the U.S. is at epidemic proportions. Unlike the diabetes data from the NHIS, national estimates of number of people with and prevalence of prediabetes are not from self-reports, but rather are based on biochemical determinations (typically, fasting glucose or HbA1c levels). Current estimates for prediabetes, depending on the definition used, range from 13% to almost 40% of U.S. adults (11,12). Consecutive waves of national surveys from 1999 to 2010 show that prediabetes prevalence has grown in the U.S. (11,12,20).
There have been some promising national data showing recent population-level decreases in sedentary behaviors, 20–30% lower beverage purchases, and 8–14% lower food calorie purchases (21). However, actual reductions in calorie consumption only amount to 7–20 fewer calories per person per day and are unlikely to account for major changes in the occurrence of diabetes. Furthermore, these reductions are fairly recent—between 2003 and 2010—and one might expect a longer lag time between changes in risk factors and in national diabetes incidence patterns.
Taken together, current evidence does not support the likelihood that the major diabetes risk factors are declining, nor can declining risk factors explain the reduction in new annual diabetes cases in the U.S. population.
Diabetes Testing Guidelines and Practices
So, if the major diabetes risk factors in the population are not improving, what might explain the declining national rates of diagnosed diabetes shown in the NHIS? The NHIS data show major increases in the rates of diagnosed diabetes from the 1990s to the late 2000s, peaking in 2008–2010 (Fig. 1). Since 2008, we have seen a dramatic decrease in rates of newly diagnosed diabetes in the NHIS. Three key nonbiological factors may help explain these trends.
Changes in Diagnostic Criteria for Diabetes
Diabetes (and prediabetes) are clinically diagnosed and defined by elevated fasting glucose, elevated postprandial glucose, and/or elevated HbA1c. These different biochemical tests signify different pathophysiologies that are together counted as representing dysglycemia. This is relevant to our discussion of incidence because, over the years, there have been major changes to how we define diabetes that have undoubtedly affected rates of new self-reported cases.
The first major change came in 1997 when the American Diabetes Association (ADA) lowered the threshold for a diagnosis of diabetes from a fasting glucose of 140 mg/dL to 126 mg/dL. This represented a dramatic loosening of the definition of diabetes; many people not previously “eligible” for a diagnosis now met the criteria for a diagnosis of diabetes. In surveillance data, we see a corresponding and dramatic increase in rates of diagnosed diabetes after 1997 (Fig. 1). These increases peaked around 2008–2010.
There was a second major change in diagnostic criteria in 2010 when the ADA added an HbA1c of 6.5% or higher to the diagnostic criteria for diabetes (22). The use of this HbA1c cut point could be interpreted in two ways. On the one hand, it could be argued that the guideline adds HbA1c, which means that another route to diagnosis has been added to an already sensitive panel of options for testing. Indeed, the current criteria now allow for fasting glucose or postprandial glucose or HbA1c to qualify an individual as having diabetes. Also, relative to other glycemic indices, HbA1c levels tend to be higher in minorities like Latinos and non-Hispanic blacks than in non-Hispanic whites (23) and may be capturing more nonfasting hyperglycemia in these populations. On the other hand, the HbA1c cutoff of 6.5% or above is fairly specific and reflects a tightening of the definition of diabetes. Indeed, the International Expert Committee that first recommended the use of HbA1c purposely selected this cut point to “emphasize specificity rather than sensitivity” (24). As such, the balance of whether HbA1c contributes to the decline in incidence depends on which test clinicians are favoring and whether these tests are being used alone or in combination. Indeed, ADA guidelines recommend that a given diagnostic test be repeated in a new blood sample for confirmation but that two different tests (such as fasting glucose and HbA1c) can be used in combination to confirm a diagnosis. A combined approach incorporating HbA1c represents a more stringent definition of diabetes than in years past. It should also be mentioned that the sensitivity and specificity of different tests to identify diabetes vary by diabetes phenotype—i.e., whether those being tested have a predominance of elevated fasting glucose, elevated postprandial glucose levels, or both.
It is possible that widespread implementation of HbA1c testing for diagnosing diabetes (alone or in combination with glucose) after 2009 has, in part, contributed to some of the recent decline in rates of diagnosed diabetes. The SUPREME-DM study demonstrated an increase in testing with HbA1c alone and in combination with glucose in individuals without prior diabetes, especially after 2010 (7). Importantly, although postprandial glucose is a very sensitive indicator of diabetes, the high inconvenience for both patients and providers has likely led to declines in use of postprandial glucose testing. It is possible that these changes in testing practices have contributed to flattening incidence in this cohort and nationally.
Changes in Screening and Testing Practices
In addition to changes in diagnostic criteria, we have seen increased screening and diagnosis of diabetes that has potentially contributed to the recent decline. In particular, in the past few years, health reforms have been associated with more health screenings by employers, payers, and providers, as insured populations are both a source of revenue and a liability for these stakeholders. On a national level, using a confirmatory definition of diabetes of both elevated fasting glucose (≥126 mg/dL) and elevated HbA1c (≥6.5%) that closely resembles clinical practice, data from the NHANES demonstrate that the undiagnosed proportion of total cases of diabetes has decreased considerably from the late 1990s to 2010 and now seems to be fairly stable at around 11% of total cases, suggesting improvements in screening and diagnosis (12).
Saturation
Together, these changes in diagnostic criteria and increases in testing have likely combined to result in “depletion of the susceptibles” in the population. More simply put, our more sensitive diabetes thresholds implemented in 1997 and increased screening efforts resulted in high case detection. Now, a decade or more later, we have likely captured most of the at-risk population and, therefore, there is nowhere for rates of diagnosis to go but down. This would then be reflected in lower numbers and rates of people with new diagnoses reporting these diagnoses annually in the NHIS and behavior risk factor surveys. Theoretically, this could also explain declining rates in claims for new diabetes diagnoses.
This is one overarching explanation for the falling incidence in diagnosed diabetes—that we have reached a saturation point. After major increases in detection from the 1990s to 2010, we are now mostly “caught up” with screening. The observed trends may largely be explained by these changes in nonbiological factors, suggesting that “real” diabetes risk has not decreased in the population.
Implications
So, is this all an academic exercise or is there relevance to practice and policy? These data and discussions have important implications. Incidence estimates help prioritize health conditions and are widely used as indicators for evaluating public health and clinical efforts to address disease.
The NHIS diabetes incidence data are actually quite limited in their ability to tell us about trends in true diabetes risk in the population. As discussed, many factors—related to patients, providers, and the larger health care system—influence the likelihood of knowing and/or reporting a diabetes diagnosis. As such, while some of the decline in rates of new diabetes diagnoses seen from the NHIS may represent real progress against diabetes, it is likely that most of the decline is an artifact of nonbiological factors, especially the combination of changing guidelines and increased diabetes testing. In particular, even though there have been some small improvements in risk behaviors, the epidemic of obesity, the main driver of the current diabetes epidemic, has done nothing but worsen.
Whatever your view on whether falling numbers and rates of reported diabetes diagnoses in national surveys are related to changing behaviors, guideline changes, or changes in testing practices and saturation in the population, the message for public health and health care is the same: the war is not yet won. Diabetes risks have not decreased in the population sufficiently to explain the trends, and it is important that we do not convey the message that we have turned the tide against the epidemic.
We believe it is premature to declare any victory. Absolute numbers of people with diabetes—both diagnosed and undiagnosed—are extremely high, as are costs per person with diabetes (25). Importantly, the current epidemic of prediabetes does not bode well for the future. Indeed, although we use a binary definition (diabetes/no diabetes), hyperglycemia exists along a continuum, and early intervention has benefits for not only reducing the risk of diabetes in the future but also improving other cardiometabolic parameters (26). Diabetes prevention efforts must therefore continue and, in fact, be scaled up to reach those people at high risk for future diabetes. Of note, focused research is needed to identify the most effective strategies to engage specific risk groups, especially racial/ethnic minority and low socioeconomic status populations in prevention programs; preventing diabetes is challenging in different contexts and one-size-fits-all interventions will likely fail.
We also need improved monitoring and surveillance efforts to help us determine what is and is not working. In particular, focused surveillance to evaluate trends in testing and diagnostic practices will help guide future efforts to improve detection, access to appropriate care, and possibly health outcomes (12,27). Continued long-term surveillance of population health efforts to lower diabetes risks in the population through regulation (the sugar-sweetened beverage tax in Berkeley, California, is just one recent example [28]) and other means will also contribute to a stronger evidence base of whether such initiatives are of value and can lower diabetes risk (29).
Conclusions
As described, the surveillance data may reflect a variety of ongoing (possibly parallel) trends, but it is difficult to see how true diabetes risk in the population could be decreasing without a concomitant decrease in incidence and prevalence of the major risk factors for diabetes. It is even possible that true diabetes risk in the U.S. is increasing, especially in the context of recent trends in obesity and prediabetes and changing demographics of the population. Concerted efforts to address the epidemics of obesity and diabetes are needed. We need to focus on prevention efforts that will prevent progression from prediabetes to diabetes. The lack of a clear decrease in biological risk discussed in this Perspective is concerning and suggests that diabetes will continue to have a major effect on the population and health system in the coming years.
Article Information
Acknowledgments. The authors thank Alexandra K. Lee, PhD student at Johns Hopkins Bloomberg School of Public Health, for her comments and research assistance related to this article.
Funding. E.S. is supported by grants from the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health (K24-DK-106414, R01-DK-089174, and R01-DK-108784). M.K.A. is supported by the National Institute of Diabetes and Digestive and Kidney Diseases (P30-DK-111024).
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Duality of Interest. No conflicts of interest relevant to this article were reported.
Footnotes
See accompanying article, p. 1152.
References
- 1.Geiss LS, Wang J, Cheng YJ, et al. Prevalence and incidence trends for diagnosed diabetes among adults aged 20 to 79 years, United States, 1980-2012. JAMA 2014;312:1218–1226 [DOI] [PubMed] [Google Scholar]
- 2.Tavernise S. New diabetes cases, at long last, begin to fall in the United States [article online]. The New York Times 1 Dec 2015. Available from http://www.nytimes.com/2015/12/01/health/new-diabetes-cases-at-long-last-begin-to-fall-in-the-united-states.html. Accessed 27 March 2017
- 3.Marcus MB. New diabetes cases drop for first time in decades [article online]. CBS News. 1 Dec 2015. Available from http://www.cbsnews.com/news/new-diabetes-cases-are-dropping-a-first-in-decades/. Accessed 27 March 2017
- 4.Centers for Disease Control and Prevention. NHIS Data, Questionnaires and Related Documentation [Internet]. Available from https://www.cdc.gov/nchs/nhis/data-questionnaires-documentation.htm. Accessed 14 November 2016
- 5.Geiss LS, Herman WH, Goldschmid MG, et al. Surveillance for diabetes mellitus—United States, 1980–1989. MMWR CDC Surveill Summ 1993;42:1–20 [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention. NHIS methods and limitations [Internet]. Available from http://www.cdc.gov/diabetes/statistics/incidence/methods.htm. Accessed 14 November 2016
- 7.Nichols GA, Schroeder EB, Karter AJ, et al.; SUPREME-DM Study Group . Trends in diabetes incidence among 7 million insured adults, 2006–2011: the SUPREME-DM project. Am J Epidemiol 2015;181:32–39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Weng W, Liang Y, Kimball ES, et al. Decreasing incidence of type 2 diabetes mellitus in the United States, 2007–2012: epidemiologic findings from a large US claims database. Diabetes Res Clin Pract 2016;117:111–118 [DOI] [PubMed] [Google Scholar]
- 9.Gregg EW, Cheng YJ, Saydah S, et al. Trends in death rates among U.S. adults with and without diabetes between 1997 and 2006: findings from the National Health Interview Survey. Diabetes Care 2012;35:1252–1257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gregg EW, Zhuo X, Cheng YJ, Albright AL, Narayan KM, Thompson TJ. Trends in lifetime risk and years of life lost due to diabetes in the USA, 1985–2011: a modelling study. Lancet Diabetes Endocrinol 2014;2:867–874 [DOI] [PubMed] [Google Scholar]
- 11.Menke A, Casagrande S, Geiss L, Cowie CC. Prevalence of and trends in diabetes among adults in the United States, 1988–2012. JAMA 2015;314:1021–1029 [DOI] [PubMed] [Google Scholar]
- 12.Selvin E, Parrinello CM, Sacks DB, Coresh J. Trends in prevalence and control of diabetes in the United States, 1988–1994 and 1999–2010. Ann Intern Med 2014;160:517–525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Geiss LS, Kirtland K, Lin J, et al. Changes in diagnosed diabetes, obesity, and physical inactivity prevalence in US counties, 2004-2012. PLoS ONE 2017;12:e0173428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Centers for Disease Control and Prevention. Long-term trends in diabetes [Internet], April 2016. Available from https://www.cdc.gov/diabetes/statistics/slides/long_term_trends.pdf. Accessed 14 November 2016
- 15.Hu FB, Manson JE, Stampfer MJ, et al. Diet, lifestyle, and the risk of type 2 diabetes mellitus in women. N Engl J Med 2001;345:790–797 [DOI] [PubMed] [Google Scholar]
- 16.Eckel RH, Kahn SE, Ferrannini E, et al. Obesity and type 2 diabetes: what can be unified and what needs to be individualized? Diabetes Care 2011;34:1424–1430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Flegal KM, Kruszon-Moran D, Carroll MD, Fryar CD, Ogden CL. Trends in obesity among adults in the United States, 2005 to 2014. JAMA 2016;315:2284–2291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fryar CD, Carroll MD, Ogden CL. Prevalence of overweight, obesity, and extreme obesity among adults aged 20 and over: United States, 1960–1962 through 2013–2014 [Internet], 2016. Available from http://www.cdc.gov/nchs/data/hestat/obesity_adult_13_14/obesity_adult_13_14.pdf. Accessed 14 November 14 2016
- 19.American Diabetes Association Classification and diagnosis of diabetes. Sec. 2. In Standards of Medical Care in Diabetes—2016. Diabetes Care 2016;39(Suppl. 1):S5–S88 [DOI] [PubMed] [Google Scholar]
- 20.Bullard KM, Saydah SH, Imperatore G, et al. Secular changes in U.S. prediabetes prevalence defined by hemoglobin A1c and fasting plasma glucose: National Health and Nutrition Examination Surveys, 1999–2010. Diabetes Care 2013;36:2286–2293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ng SW, Slining MM, Popkin BM. Turning point for US diets? Recessionary effects or behavioral shifts in foods purchased and consumed. Am J Clin Nutr 2014;99:609–616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.American Diabetes Association Diagnosis and classification of diabetes mellitus. Diabetes Care 2010;33(Suppl. 1):S62–S69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Selvin E. Are there clinical implications of racial differences in HbA1c? A difference, to be a difference, must make a difference. Diabetes Care 2016;39:1462–1467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.The International Expert Committee. International Expert Committee report on the role of the A1C assay in the diagnosis of diabetes. Diabetes Care 2009;32:1327–1334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhuo X, Zhang P, Kahn HS, Bardenheier BH, Li R, Gregg EW. Change in medical spending attributable to diabetes: national data from 1987 to 2011. Diabetes Care 2015;38:581–587 [DOI] [PubMed] [Google Scholar]
- 26.Mudaliar U, Zabetian A, Goodman M, et al. Cardiometabolic risk factor changes observed in diabetes prevention programs in US settings: a systematic review and meta-analysis. PLoS Med 2016;13:e1002095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ali MK, Bullard KM, Saaddine JB, Cowie CC, Imperatore G, Gregg EW. Achievement of goals in U.S. diabetes care, 1999–2010. N Engl J Med 2013;368:1613–1624 [DOI] [PubMed] [Google Scholar]
- 28.Falbe J, Rojas N, Grummon AH, Madsen KA. Higher retail prices of sugar-sweetened beverages 3 months after implementation of an excise tax in Berkeley, California. Am J Public Health 2015;105:2194–2201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ackermann RT, Kenrik Duru O, Albu JB, et al.; NEXT-D Study Group . Evaluating diabetes health policies using natural experiments: the natural experiments for translation in diabetes study. Am J Prev Med 2015;48:747–754 [DOI] [PMC free article] [PubMed] [Google Scholar]