Abstract
Study Objectives:
We aimed to compare 2-year-old children born preterm with children born full term regarding: (1) sleep characteristics, (2) temperament, and (3) relations between sleep pattern and habits and temperament.
Methods:
The study included 51 preterm children with normal cognitive, language, and motor development (mean = 20.94 months, standard deviation [SD] = 4.08) and 57 full-term children (mean = 21.19, SD = 4.32). To assess sleep-related difficulties and habits and child temperament, mothers completed the following questionnaires: the (1) Sleep Disturbance Scale for Children—adapted (SDSC); (2) Brief Infant Sleep Questionnaire (BISQ); and (3) Italian Temperament Questionnaires—version 12-36 months (QUIT).
Results:
Preterm children needed less support to fall asleep and fell asleep more often alone in their own bed compared to those born at full term; however, preterm children showed more frequent sleep difficulties, such as restlessness and breathing problems during the night. In addition, preterm children had lower scores in the temperamental dimension of attention and higher scores in negative emotionality than full-term children. Finally, sleep problems were correlated with higher motor activity, lower social orientation and attention, and increased negative emotionality; a shorter nocturnal sleep duration was related to higher motor activity and lower inhibition to novelty whereas an earlier rise time was associated with lower attention and social orientation.
Conclusions:
Preterm children showed sleep pattern problems and disturbance, predominance of attention problems, and negative emotionality related to sleep disruption.
Citation:
Caravale B, Sette S, Cannoni E, Marano A, Riolo E, Devescovi A, De Curtis M, Bruni O. Sleep characteristics and temperament in preterm children at two years of age. J Clin Sleep Med. 2017;13(9):1081–1088.
Keywords: preterm children, sleep, temperament
INTRODUCTION
Children born preterm are at increased risk for neurodevelopmental problems in various areas, such as language, motor skills, behavior, and self-regulation.1,2 Some studies have indicated that preterm children may also have sleep disturbances such as shorter daytime rest and nighttime sleep duration, as well as decreased sleep quality in the first and second year of life,3,4 showing that sleep is significantly less restful than that of full-term children. Also later in life, at 3 years of age, sleep disturbances have been described in preterm children, although a reduction of sleep problems was reported at 5 years.5 Furthermore, it has been observed that children with very low birth weight are at risk for reduced sleep efficiency at 8 years and advanced sleep onset times in adulthood.6,7 Preterm children may also present sleep-disordered breathing more frequently than full-term children during middle childhood.8 All these sleep disturbances have been associated with subsequent developmental disturbances, suggesting that adequate sleep is a fundamental requisite for an optimal infant development. Several researchers showed that sleep is particularly important during the early development phases. Sleep deprivation could determine cellular damage,9 hippocampal oxidative stress,10,11 and suppression of neurogenesis.12 It may also influence brain areas such as frontal lobes involved in motivation, goal direction, and attentional abilities.13 Therefore, in the developing brain, sleep deprivation during critical periods may result in morbid and potentially irreversible changes in neural organization of these brain structures.14
BRIEF SUMMARY
Current Knowledge/Study Rationale: Preterm birth is a risk factor for many areas of neurological and psychological development. Little is known about sleep quality and habits of preterm children beyond the neonatal period and research findings, to date, have been inconclusive. Very few studies have analyzed the relationship between sleep patterns and temperament in preterm children compared to children born full term.
Study Impact: Our findings show that preterm children with no deficit in cognitive, language, and motor areas, in the second year of life, have relatively more frequent sleep difficulties during the night and different sleep habits compared to full-term children. The temperament of preterm children seems to be characterized by a lower level of attention and more negative emotionality compared to full-term children. We observed a link between sleep pattern and temperament in preterm children and found that sleep problems were related to increased negative emotionality and decreased attention.
Conversely, other studies have found that preterm children do not differ in their sleep features, such as sleep duration, bed sharing, night waking or time of sleep onset, from full-term children.3,15 Researchers have attempted to identify the etiology of sleep difficulties in preterm children in terms of exposure to early neonatal stressors, such as nonphysiological nutrition, hypoxia, repeated painful experiences, abnormal light, and noise.16–18
The persistent attitude of parents of preterm children in the perception of their children as fragile and vulnerable and their reaction to the child's waking could be an important factor in the development of sleep problems.19 In fact, preterm infants are generally less able to provide clear distress signals, are more easily stressed, and may not show the same rich variety of interactional capacities seen in those born at term.20 Such difficulties may contribute to less adequate parenting, which may play a role in sleep development.21 Moreover, lack of constant physical bonding and challenging breastfeeding in pre-term children may also contribute to higher stress response, less organized sleep, and difficult maternal–infant interactions.22–24 Finally, melatonin rhythmicity may develop more slowly in preterm than in full-term children.17,25
It is known that sleep in children is likely to be influenced not only by environmental and biological factors but also by individual characteristics such as child temperament.26 Temperament has been variously defined27–29; for the current study, we used the temperamental model developed by Thomas and Chess, which focuses on the goodness of fit between child and environment. The model includes different cognitive, emotional, and relational processes such as attention, negative and positive emotionality, motor control activity, social orientation, and inhibition to novelty.28
Overall, recent studies have reported that during the first months of life, preterm children may manifest a higher degree of negative reactivity,30,31 a limited capacity to modulate arousal, and lower thresholds to negative emotionality.32 In addition, preterm children may present a greater use of distancing during dyadic play compared to their full-term counterparts, indicating a lower capacity for self-regulation even in routine interactions.33 There is also evidence that a history of painful procedures in the neonatal intensive care unit (NICU) is associated with poor sustained attention and with a higher basal level of cortisol during the first years of life.18,34 Neonatal pain has also been linked to the internalization of behavioral problems in preterm children at 18 months of age35 and a higher reactivity to pain was related to negative affectivity temperament in toddlerhood among preterm children.36
It is known that a difficult child temperament, such as being irritable, fussy, or hypersensitive, may interfere with sleep consolidation in the first months of life and is associated with sleep problems in general during childhood. Moreover, parental behavior in response to awakenings is highly related to the child's sleep rhythmicity and with the endurance of sleep problems.37,38 Longitudinal studies have confirmed a positive association between difficult temperament profile and sleep problems over the first 2 years of life.39
However, to the best of our knowledge only 1 study has analyzed the association between temperament and sleep in preterm children.40 In this study, 21 preterm children were assessed at 3 time points: during the neonatal period, during toddlerhood, and during the preschool age period. During toddlerhood, low birth weight and low scores in sociability were significant predictors of sleep problems. Nevertheless, the study lacked a control group and sleep was assessed only considering a global measure of sleep problems using the Child Behavior Checklist (CBCL).
Therefore, because very few studies have been carried out in order to evaluate the relation between sleep quality and habits and temperament in preterm children, the aims of this study were to investigate: (1) the characteristics of sleep (in terms of sleep-related difficulties and habits), (2) the temperamental dimensions, and (3) the relations between sleep pattern and temperament in a group of preterm children.
METHODS
Participants
The current study is part of a larger investigation on the neurodevelopment of preterm children. The study group is composed of 51 preterm children recruited from the NICU of a public hospital in Rome, Italy (Umberto I General Hospital). The sample was composed of 5 extremely preterm children (< 28 weeks of gestational age), 17 very preterm children (28 to < 32 weeks gestational age), and 29 moderate to late pre-term children (32 to < 37 weeks gestational age). Data collected from the hospital medical charts revealed that among them, 2 (4%) had sepsis, 4 (7.9%) had intraventricular hemorrhage grade I-II, 4 (7.9%) had intraventricular hemorrhage grade IIIIV, 1 (2%) had periventricular leukomalacia, and 11 (21.6%) had neonatal respiratory distress syndrome (RDS). The length of stay in the NICU ranged from 9 to 88 days (mean = 36.21, standard deviation [SD] = 21.12).
As a part of their follow-up evaluation, during the first year of life, children were assessed for cognitive, language, and motor development by the Bayley Scales of Infant and Toddler Development-Third Edition (BSID-III).41 In the current study, we included only preterm children who did not have a delay in cognitive, language, and motor areas, defined as a BSIDIII scaled score in each scale of less than 2 SD relative to the mean.
The control group consists of 57 healthy full-term children recruited from 3 daycare centers in the same geographic area as the preterm group. For both groups, children with a genetic syndrome, major congenital anomalies, and neurosensory or motor disabilities, as well as mothers who did not possess an adequate Italian language level, were excluded from the study.
This study was approved by the Ethics Committee of the Department of Developmental and Social Psychology, Sapienza, University of Rome.
Procedure
Mothers of preterm children were approached by doctors or psychologists in the course of the second year of life of their children during one of their hospital follow-up visits and solicited for participation in the study. For each daycare center, the director of the center contacted the mothers of the control group to explain the aims of the study. A written parental consent was obtained from all participants before inclusion in the study. Two research assistants trained in child assessment explained the questionnaires on temperament and sleep to each parent, administered the questionnaires, and remained available for any clarification during completion. The completion of the questionnaires was checked as soon as parents returned them.
Measures
Assessment of infant sleep
To assess the infant sleep-related difficulties and habits, all mothers completed the following measures:
The Sleep Disturbance Scale for Children—adapted (SDSC).42 A revised version of the SDSC questionnaire was used and adapted for use with toddlers in order to identify the presence of sleep disturbances. From the original scale, we selected 12 items (removing 14 items deemed to be inappropriate for age). An exploratory factor analysis on the 12 items yielded 2 correlated factors named (a) bedtime difficulties (composed of 3 items, eg, a child's difficulty or refusal to fall asleep) with factor loadings ranging from 0.40 to 0.93 and a good internal consistency (α = .72) and (b) sleep difficulties (composed of 9 items, eg, nocturnal movement, restlessness during the night, or breathing problems) with factor loadings ranging from 0.37 to 0.68 and a good internal consistency (α = .76). Responses were given on a 3-point Likert scale with higher values reflecting a greater difficulty with bedtime and sleep.
Brief Infant Sleep Questionnaire (BISQ).43 The BISQ aims to evaluate sleep pattern and habits and it is composed of questions related to the following areas: (a) bedtime, (b) rise time, (c) nocturnal sleep duration, (d) daytime sleep duration, (e) number of nighttime awakenings, (f) nocturnal wakefulness, (g) latency to falling asleep during the night (or settling time), (h) method of falling asleep, and (i) location of sleep.
Assessment of infant temperament
To evaluate the infant temperament, we used the Italian Temperament Questionnaires—version 12-36 months (QUIT).44 The questionnaire is composed of 56 items rated on a 6-point Likert scale (1 = almost never to 6 = almost always) describing infant behavior in 3 different contexts: (1) child interaction with others, (2) child during play, and (3) child during an activity or a task. In total, 6 temperamental dimensions were assessed: (1) Social Orientation (9 items; infant interest and attention towards others); (2) Inhibition to Novelty (12 items; infant emotional reactivity toward contextual stimuli); (3) Motor Activity (11 items; infant physical activity); (4) Positive Emotionality (10 items; infant expression of positive emotions); (5) Negative Emotionality (6 items; infant expression of negative emotions); and (6) Attention (8 items; infant ability to keep the focus of his/her attention). The scores of each dimension were averaged to create Social Orientation, Inhibition to Novelty, Motor Activity, Positive Emotionality, Negative Emotionality, and Attention rates for each infant. Overall, each dimension of the QUIT showed an acceptable internal consistency.44,45
Statistical Analysis
Analyses of variance were conducted to analyze differences in sleep difficulties, sleep habits, and temperamental dimensions between preterm and control groups. Then, we ran a series of chi square tests (χ2) and Fisher exact tests to compare preterm and control groups for their method of falling asleep, location of sleep, and settling time. Finally, Pearson correlations were performed in preterm children to examine the associations among temperamental dimensions, sleep difficulties, and sleep habits.
RESULTS
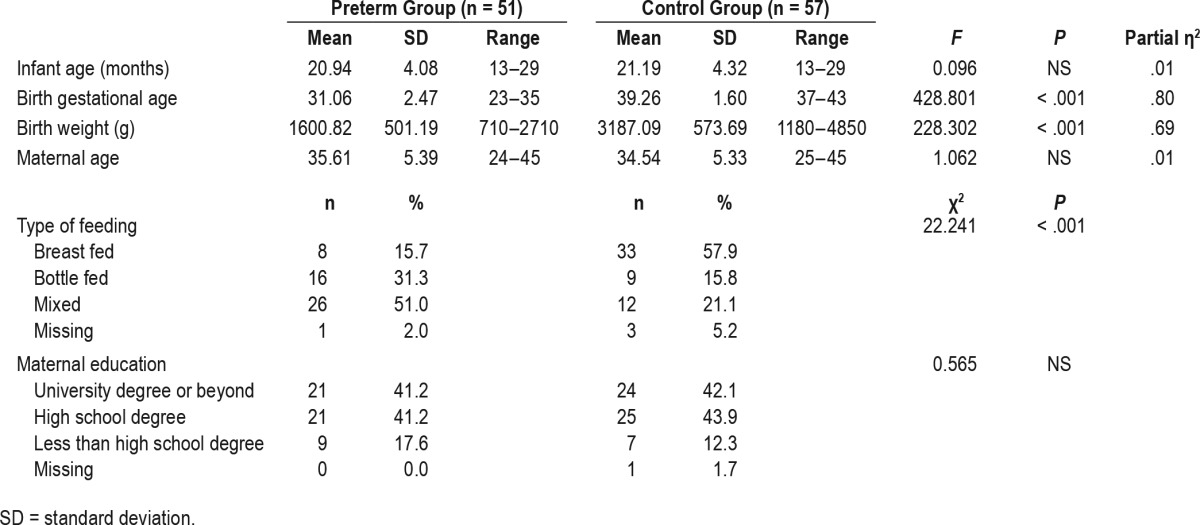
Demographic characteristics (ie, infant mean age, birth gestational age, and birth weight) and the type of feeding for the pre-term and control groups are displayed in Table 1. Table 1 also shows the maternal age and education for both groups. Preterm children had a gestational age and weight at birth lower than that of full-term children. In addition, we found that preterm children were less frequently breastfed than full-term children. No differences have been found for maternal education and maternal age.
Table 1.
Demographic characteristics of preterm and control groups.
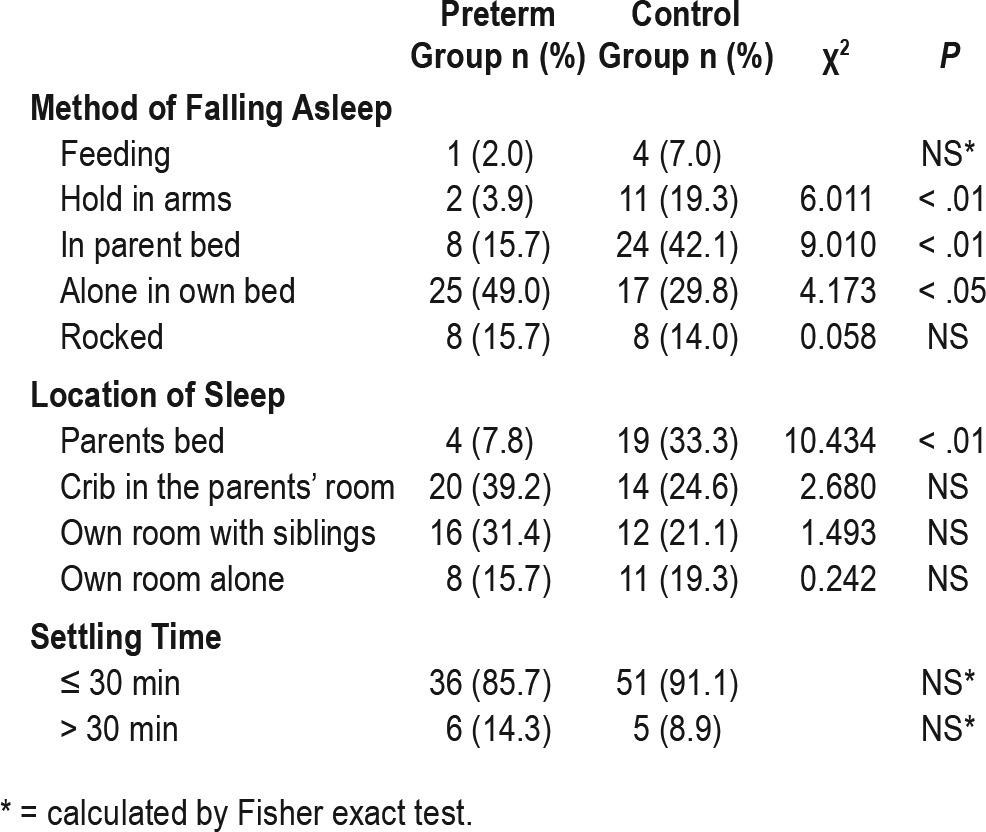
Preterm children displayed more medical sleep problems (eg, nocturnal movement, restlessness during the night and breathing problems, as assessed by the SDSC questionnaire) than the control group (Table 2) whereas behavioral sleep problems as assessed by the BISQ were less frequent. Indeed, preterm children needed less support to fall asleep (hold in arms or in parent bed), fell asleep more often alone in their own bed, and slept less often in the parent bed than the full-term children. No other significant differences were found (Table 3).
Table 2.
Sleep difficulties and habits for preterm and control groups.
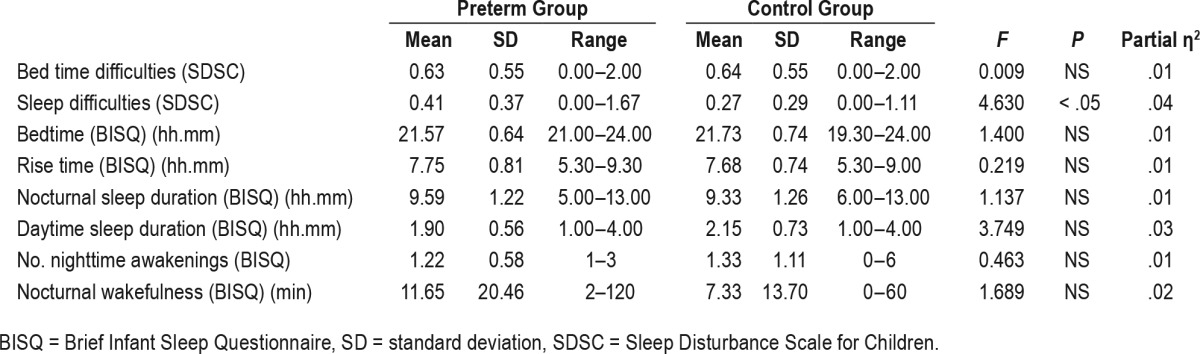
Table 3.
Prevalence of method of falling asleep, location of sleep, and settling time for preterm and control groups.
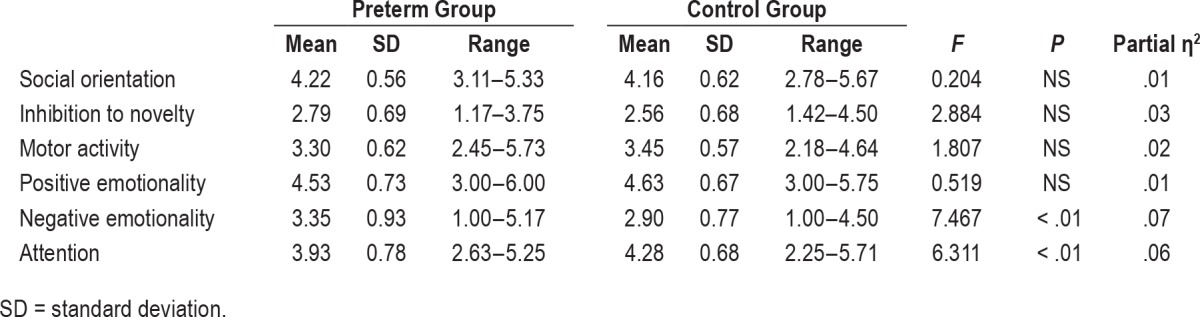
Regarding temperament, the preterm group reported lower scores in attention and higher scores in negative emotionality than the control group (Table 4).
Table 4.
Temperamental dimensions for preterm and control groups.
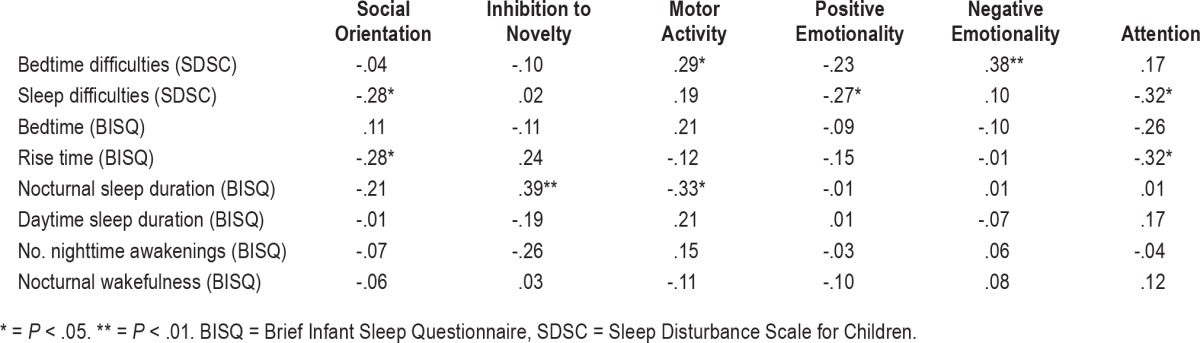
Significant and positive correlations in preterm children were found between bedtime difficulties and both motor activity and negative emotionality and between nocturnal sleep duration and inhibition to novelty. Negative correlations were observed between sleep difficulties and social orientation, positive emotionality, and attention; between the rise time and both social orientation and attention dimensions; and between nocturnal sleep duration and motor activity (Table 5).
Table 5.
Correlations between the temperamental dimensions and infant sleep difficulties and habits for preterm group.
DISCUSSION
Our findings show that preterm children have a relatively high degree of medical sleep problems during the night and a lower degree of behavioral sleep problems, such as lower need of support from parents to fall asleep, compared to full-term children, whereas no differences were found between the 2 groups on sleep patterns such as bedtime, rise time, and nocturnal and daytime sleep durations.
These results are similar to those of previous studies on sleep in preterm children, although many controversial findings have been previously published in the literature. Some authors found a poorer sleep quality (in terms of restful sleep during the night) in preterm versus full-term children, at approximately 20 months of corrected age4 and an increase in the number of night awakenings and in the time spent with mouth breathing.46 However, other studies were in agreement with our findings, showing that preterm children exhibited fewer and shorter night awakenings at age 3 months and settled more quickly once awakened at 5 months of age than full-term children and no differences have been found in sleeping behavior at age 20 months and at preschool age.5,47 Furthermore, our results are also in agreement with other studies showing no differences on bedtime, rise time, nocturnal and daytime sleep durations, bed sharing, nighttime waking, bedtime resistance, and sleep onset difficulties.15,48
In our study, we only included preterm children with no deficit in cognitive, language, and motor areas, to ensure a sample as homogeneous as possible. Our criteria excluded the majority of preterm infants who had a complicated NICU course and who could present with different, and probably more severe, sleep problems often linked to the presence of a severe neurological damage.49
Despite the fact that no differences in bedtime, rise time, or sleep duration have been found in preterm versus full-term children, the sleep problems described by the parents of preterm children (restlessness, breathing problems during sleep) could have resulted in sleep disruption, which has been associated with alteration of daytime behavior, attention, and learning difficulties during childhood and adolescence as reported in the literature.50,51
Regarding temperamental characteristics, we showed that preterm children had lower levels of attention and more negative emotionality (eg, crying, stranger wariness) than full-term children. These results are consistent with previous studies demonstrating that children born preterm are at risk of attention and learning problems40 as well as emotional difficulties.52 Accordingly, a review conducted on attention development during the first 4 years of age confirmed a decrease of sustained attention and visual orientation of attention in preterm children compared to their counterparts born at full term.53 Furthermore, some authors found that preterm children at 2 months corrected age expressed more negative affect during repeated exposure to the modified still-face procedure than the full-term children, confirming, thus, the preterm children's difficulty in regulating their distress.30 Similarly, another study found that very preterm children expressed more negative emotions, in terms of fear and frustration, than full-term children in tasks assessing emotional abilities.54 The negative affectivity may represent a significant predictor of both internalizing and externalizing behaviors, as suggested by some authors with a sample of children aged from 18 to 36 months who were born preterm.55
It is noteworthy that our results support an association between sleep quality and child temperamental characteristics. Correlational analyses showed that sleep difficulties were associated with increased motor activity, lower social orientation and attention, and more negative emotionality. Furthermore, a shorter nocturnal sleep duration was related to increased motor activity and lower inhibition to novelty, whereas an earlier rise time was associated with lower attention and social orientation.
An increase in motor activity is often reported by parents of children with sleep problems and may also be related to difficulties in attention and social interactions.56 It is possible that sleep difficulties in preterm children interfere with brain maturation that, in turn, may compromise the children's cognitive and regulatory abilities.56 Previous studies also underlined the parents' role in helping children to regulate sleep and executive functions.57 Parents may have more difficulties in being external regulators for preterm children given their child's vulnerability to a range of cognitive, attentional, and behavioral problems.
Therefore, our findings also confirm a link between sleep-related difficulties and temperament in children born preterm. Most of the previous studies focused their attention on full-term children, demonstrating that sleep may be related to infant individual characteristics as well as environmental factors.26 A previous study found that a longer nocturnal sleep duration was related to infant approachability at 3, 6, and 11.5 months.58 Other authors have shown associations between infant negative temperament (in terms of distress to limitations and fear), the difficulty in putting infants to sleep, sleep problems, and longer wakefulness in the night during the first year of life.59
To the best of our knowledge, only one study analyzed the link between temperament and sleep in preterm children and reported an association between sleep problems and low sociability during toddlerhood.40 Although the authors considered a global measure of sleep problems derived from the CBCL, we found similar results confirming an association between sleep problems and difficulty in children's social orientation. In contrast, childrens' optimal sleep may be related to their adaptive functioning during the day in terms of social engagement and peer acceptance.60
Based on a transactional model of infant sleep, temperamental characteristics might directly interfere with sleep consolidation or may influence the parents' behavioral response to their children, thereby affecting their sleep.61 Infant sleep develops in dynamic and complex transactions between infant temperament and parent emotional quality. Therefore, it is important to examine both sleep and temperament and their interrelationships in order to provide a correct approach for infant sleep problems.61
Although the current study is one of the first on the relationship between different aspects of sleep (eg, duration, location of sleep) and temperament in preterm children, some limitations of this research should be considered when interpreting results. First, the cross-sectional nature of our data prevents us from analyzing possible direct relationships between infant sleep and temperament in preterm children. It is possible that infant sleep may influence the expression of temperament in terms of motor activity and less attention during the day or that infant temperamental characteristics may play a role in influencing infant sleep.62 Therefore, future studies that might analyze these associations longitudinally may help us to better understand the link between infant sleep and temperament, as well as their associations with socioemotional adjustment over time.
Furthermore, we only considered parental ratings on sleep and temperamental characteristics with no other objective sleep measures (such as actigraphy or polysomnography) or different informants (eg, teachers versus parents). The inclusion of different objective informants may be useful to better understand the effect of sleep quality on children's social behaviors in different contexts. Finally, it would be interesting to replicate the results of the current study in other cultural samples to improve our knowledge on the association between preterm children temperament and sleep in different samples/cultures.
In conclusion, we found a link between sleep and temperament in preterm children, demonstrating that sleep problems are related to more negative emotionality and lower attention. Therefore, it is important that pediatricians screen sleep more rigorously in preterm children, especially with respect to sleep-related breathing disorders and sleep-related movement disorders.
Interventions on the quality of the infant-caregiver relationship as well as environmental modification or behavioral treatment might be useful to improve sleep quality of preterm children and hopefully modify the negative temperamental characteristics of preterm children during early childhood.63
DISCLOSURE STATEMENT
Work for this study was performed at Sapienza University of Rome. All authors have read and approved the manuscript in its current form. This study was supported by University Funding ‘Ricerca di Ateneo year 2014’ from Sapienza University of Rome, Italy. The authors declare that they have no any financial interests or connections, direct or indirect, or other situations that might raise the question of bias in the work reported or the conclusions, implications, or opinions stated, including pertinent commercial or other sources of funding for the individual author(s) or for the associated department(s) or organization(s), personal relationships, or direct academic competition.
ACKNOWLEDGMENTS
The authors thank the children and the families who participated in this study. Special thanks go to Drs. Mark H. Libenson and Raffaele Ferri for proofreading the manuscript.
ABBREVIATIONS
- BISQ
Brief Infant Sleep Questionnaire
- BSID-III
Bayley Scales of Infant and Toddler Development-Third Edition
- CBCL
Childhood Behavior Checklist
- NICU
neonatal intensive care unit
- QUIT
Italian Temperament Questionnaires
- SD
standard deviation
- SDSC
Sleep Disturbance Scale for Children
REFERENCES
- 1.Bilgin A, Wolke D. Regulatory problems in very preterm and full-term infants over the first 18 months. J Dev Behav Pediatr. 2016;37(4):298–305. doi: 10.1097/DBP.0000000000000297. [DOI] [PubMed] [Google Scholar]
- 2.Woodward LJ, Moor S, Hood KM, et al. Very preterm children show impairments across multiple neurodevelopmental domains by age 4 years. Arch Dis Child Fetal Neonatal Ed. 2009;94(5):339–344. doi: 10.1136/adc.2008.146282. [DOI] [PubMed] [Google Scholar]
- 3.Anders TF, Keener MA. Developmental course of nighttime sleep-wake patterns in full-term and premature infants during the first year of life. I. Sleep. 1985;8(3):173–192. doi: 10.1093/sleep/8.3.173. [DOI] [PubMed] [Google Scholar]
- 4.Gössel-Symank R, Grimmer I, Korte J, Siegmund R. Actigraphic monitoring of the activity-rest behavior of preterm and full-term infants at 20 months of age. Chronobiol Int. 2004;21(4-5):661–671. doi: 10.1081/cbi-120039208. [DOI] [PubMed] [Google Scholar]
- 5.Ungerer JA, Sigman M, Beckwith L, Cohen SE, Parmelee AH. Sleep behavior of preterm children at three years of age. Dev Med Child Neurol. 1983;25(3):297–304. doi: 10.1111/j.1469-8749.1983.tb13763.x. [DOI] [PubMed] [Google Scholar]
- 6.Pesonen AK, Raikkonen K, Matthews K, et al. Prenatal origins of poor sleep in children. Sleep. 2009;32(8):1086–1092. doi: 10.1093/sleep/32.8.1086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Strang-Karlsson S, Raikkonen K, Kajantie E, et al. Sleep quality in young adults with very low birth weight--the Helsinki study of very low birth weight adults. J Pediatr Psychol. 2008;33(4):387–395. doi: 10.1093/jpepsy/jsm125. [DOI] [PubMed] [Google Scholar]
- 8.Rosen CL, Larkin EK, Kirchner HL, et al. Prevalence and risk factors for sleep-disordered breathing in 8-to 11-year-old children: association with race and prematurity. J Pediatr. 2003;142(4):383–389. doi: 10.1067/mpd.2003.28. [DOI] [PubMed] [Google Scholar]
- 9.Everson CA, Laatsch CD, Hogg N. Antioxidant defense responses to sleep loss and sleep recovery. Am J Physiol Regul Integr Comp Physiol. 2005;288(2):R374–R383. doi: 10.1152/ajpregu.00565.2004. [DOI] [PubMed] [Google Scholar]
- 10.Gopalakrishnan A, Ji LL, Cirelli C. Sleep deprivation and cellular responses to oxidative stress. Sleep. 2004;27(1):27–35. doi: 10.1093/sleep/27.1.27. [DOI] [PubMed] [Google Scholar]
- 11.Silva RH, Chehin AB, Kameda SR, et al. Effects of pre-or post-training paradoxical sleep deprivation on two animal models of learning and memory in mice. Neurobiol Learn Mem. 2004;82(2):90–98. doi: 10.1016/j.nlm.2004.04.005. [DOI] [PubMed] [Google Scholar]
- 12.Hairston IS, Little MT, Scanlon MD, et al. Sleep restriction suppresses neurogenesis induced by hippocampus-dependent learning. J Neurophysiol. 2005;94(6):4224–4233. doi: 10.1152/jn.00218.2005. [DOI] [PubMed] [Google Scholar]
- 13.Beebe DW, Gozal D. Obstructive sleep apnea and the prefrontal cortex: towards a comprehensive model linking nocturnal upper airway obstruction to daytime cognitive and behavioral deficits. J Sleep Res. 2002;11(1):1–16. doi: 10.1046/j.1365-2869.2002.00289.x. [DOI] [PubMed] [Google Scholar]
- 14.Frank MG. Sleep and synaptic plasticity in the developing and adult brain. Curr Top Behav Neurosci. 2015;25:123–149. doi: 10.1007/7854_2014_305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Iglowstein I, latal Hajnal B, Molinari L, Largo RH, Jenni OG. Sleep behaviour in preterm children from birth to age 10 years: A longitudinal study. Acta Paediatr. 2006;95(12):1691–1693. doi: 10.1080/08035250600686938. [DOI] [PubMed] [Google Scholar]
- 16.Guyer C, Huber R, Fontijn J, et al. Very preterm infants show earlier emergence of 24-hour sleep-wake rhythms compared to term infants. Early Hum Dev. 2015;91(1):37–42. doi: 10.1016/j.earlhumdev.2014.11.002. [DOI] [PubMed] [Google Scholar]
- 17.Kennaway DJ. Programming of the fetal suprachiasmatic nucleus and subsequent adult rhythmicity. Trends Endocrinol Metab. 2002;13(9):398–402. doi: 10.1016/s1043-2760(02)00692-6. [DOI] [PubMed] [Google Scholar]
- 18.Valeri BO, Holsti L, Linhares MBM. Neonatal pain and developmental outcomes in children born preterm: a systematic review. Clin J Pain. 2015;31(4):355–362. doi: 10.1097/AJP.0000000000000114. [DOI] [PubMed] [Google Scholar]
- 19.Portnoy S, Callias M, Wolke D, Gamsu H. Five year follow up study of extremely low-birthweight infants. Dev Med Child Neurol. 1988;30(5):590–598. doi: 10.1111/j.1469-8749.1988.tb04796.x. [DOI] [PubMed] [Google Scholar]
- 20.Feldman R. From biological rhythms to social rhythms: Physiological precursors of mother-infant synchrony. Dev Psychol. 2006;42(1):175–188. doi: 10.1037/0012-1649.42.1.175. [DOI] [PubMed] [Google Scholar]
- 21.Schwichtenberg AJM, Poehlmann J. A transactional model of sleep-wake regulation in infants born preterm or low birthweight. J Pediatr Psychol. 2009;34(8):837–849. doi: 10.1093/jpepsy/jsn132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Baley J Committee on Fetus and Newborn. Skin-to-skin care for term and preterm infants in the neonatal ICU. Pediatrics. 2015;136(3):596–599. doi: 10.1542/peds.2015-2335. [DOI] [PubMed] [Google Scholar]
- 23.Cong X, Wu J, Vittner D, et al. The impact of cumulative pain/stress on neurobehavioral development of preterm infants in the NICU. Early Hum Dev. 2017;23:9–16. doi: 10.1016/j.earlhumdev.2017.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schwichtenberg AJ, Shah PE, Poehlmann J. Sleep and attachment in preterm infants. Infant Ment Health J. 2013;34(1):37–46. doi: 10.1002/imhj.21374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kennaway DJ, Goble FC, Stamp GE. Factors influencing the development of melatonin rhythmicity in humans. J Clin Endocrinol Metab. 1996;81(4):1525–1532. doi: 10.1210/jcem.81.4.8636362. [DOI] [PubMed] [Google Scholar]
- 26.Sadeh A, Tikotzky L, Scher A. Parenting and infant sleep. Sleep Med Rev. 2010;14(2):89–96. doi: 10.1016/j.smrv.2009.05.003. [DOI] [PubMed] [Google Scholar]
- 27.Buss AH, Plomin H. Temperament: Early Developing Personality Traits. Hillsdale, NJ: Erlbaum; 1984. [Google Scholar]
- 28.Chess S, Thomas A. Origins and Evolution of Behavior Disorders. New York, NY: Bruner/Mazel; 1984. [Google Scholar]
- 29.Shiner RL, Buss KA, McClowry SG, Putnam SP, Saudino KJ, Zentner M. What is temperament now? Assessing progress in temperament research on the twenty-fifth anniversary of Goldsmith et al. Child Dev Perspect. 2012;6(4):436–444. [Google Scholar]
- 30.Hsu HC, Jeng SF. Two-month-olds' attention and affective response to maternal still face: a comparison between term and preterm infants in Taiwan. Infant Behav Dev. 2008;31(2):194–206. doi: 10.1016/j.infbeh.2007.10.008. [DOI] [PubMed] [Google Scholar]
- 31.Langerock N, van Hanswick de Jonge L, Bickle Graz M, Hüppi PS, Borradori Tolsa C, Barisnikov K. Emotional reactivity at 12 months in very preterm infants born at < 29 weeks of gestation. Infant Behav Dev. 2013;36(3):289–297. doi: 10.1016/j.infbeh.2013.02.006. [DOI] [PubMed] [Google Scholar]
- 32.Feldman R. From biological rhythms to social rhythms: Physiological precursors of mother-infant synchrony. Dev Psychol. 2006;42(1):175–188. doi: 10.1037/0012-1649.42.1.175. [DOI] [PubMed] [Google Scholar]
- 33.Montirosso R, Borgatti R, Trojan S, Zanini R, Tronick E. A comparison of dyadic interactions and coping with still-face in healthy pre-term and full-term infants. Br J Dev Psychol. 2010;28(Pt 2):347–368. doi: 10.1348/026151009x416429. [DOI] [PubMed] [Google Scholar]
- 34.Grunau RE, Haley DW, Whitfield MF, Weinberg J, Yu W, Thiessen P. Altered basal cortisol levels at 3, 6, 8 and 18 months in infants born extremely low gestational age. J Pediatr. 2007;150(2):151–156. doi: 10.1016/j.jpeds.2006.10.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Vinall J, Miller SP, Synnes AR, Grunau RE. Parent behaviors moderate the relationship between neonatal pain and internalizing behaviors at 18 months corrected age in children born very prematurely. Pain. 2013;154(9):1831–1839. doi: 10.1016/j.pain.2013.05.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Klein VC, Gaspardo CM, Martinez FE, Grunau RE, Linhares MBM. Pain and distress reactivity and recovery as early predictors of temperament in toddlers born preterm. Early Hum Dev. 2009;85(9):569–576. doi: 10.1016/j.earlhumdev.2009.06.001. [DOI] [PubMed] [Google Scholar]
- 37.Morrell J, Steele H. The role of attachment security, temperament, maternal perception, and care-giving behavior in persistent infant sleeping problems. Infant Ment Health J. 2003;24(5):447–468. [Google Scholar]
- 38.Touchette É, Dionne G, Forget-Dubois N. Genetic and environmental influences on daytime and nighttime sleep duration in early childhood. Pediatrics. 2013;131(6):1874–1880. doi: 10.1542/peds.2012-2284. [DOI] [PubMed] [Google Scholar]
- 39.Snow ME, Jacklin CN, Maccoby EE. Crying episodes and sleep-wakefulness transitions in the first 26 months of life. Infant Behav Dev. 1980;3:387–394. [Google Scholar]
- 40.Klein VC, Gaspardo CM, Martinez FE, Linhares MBM. Neonatal characteristics and temperament predict behavior problems in children born preterm. Revista Brasileira de Crescimento e Desenvolvimento Humano. 2015;25:331–340. [Google Scholar]
- 41.Bayley N. Bayley Scales of Infant and Toddler Development. 3rd ed. San Antonio, TX: Harcourt Assessment; 2006. [Google Scholar]
- 42.Bruni O, Ottaviano S, Guidetti V, et al. The sleep disturbance scale for children (SDSC). Construction and validation of an instrument to evaluate sleep disturbances in childhood and adolescence. J Sleep Res. 1996;5(4):251–261. doi: 10.1111/j.1365-2869.1996.00251.x. [DOI] [PubMed] [Google Scholar]
- 43.Sadeh A. A brief screening questionnaire for infant sleep problems: validation and findings for an Internet sample. Pediatrics. 2004;113(6):e570–e577. doi: 10.1542/peds.113.6.e570. [DOI] [PubMed] [Google Scholar]
- 44.Axia G. QUIT. Questionari Italiani del Temperamento. Trento, Italy: Edizioni Erickson; 2002. [Google Scholar]
- 45.Perricone G, Morales MR. The temperament of preterm infant in preschool age. Ital J Pediatr. 2011;37:1–7. doi: 10.1186/1824-7288-37-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Huang YS, Paiva T, Hsu JF, Kuo MC, Guilleminault C. Sleep and breathing in premature infants at 6 months post-natal age. BMC Pediatr. 2014;14:1–6. doi: 10.1186/s12887-014-0303-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wolke D, Meyer R, Ohrt B, Riegel K. The incidence of sleeping problems in preterm and fullterm infants discharged from neonatal special care units: an epidemiological longitudinal study. J Child Psychol Psychiatry. 1995;36(2):203–225. doi: 10.1111/j.1469-7610.1995.tb01821.x. [DOI] [PubMed] [Google Scholar]
- 48.Asaka Y, Takada S. Activity-based assessment of the sleep behaviors of VLBW preterm infants and full-term infants at around 12 months of age. Brain Dev. 2010;32(2):150–155. doi: 10.1016/j.braindev.2008.12.006. [DOI] [PubMed] [Google Scholar]
- 49.Ding X, Cheng Z, Sun B, et al. Distinctive sleep problems in children with perinatal moderate or mild hypoxic-ischemia. Neurosci Lett. 2016;614:60–64. doi: 10.1016/j.neulet.2015.12.061. [DOI] [PubMed] [Google Scholar]
- 50.Hagmann-von Arx P, Perkinson-Gloor N, Brand S, et al. In school-age children who were born very preterm sleep efficiency is associated with cognitive function. Neuropsychobiology. 2014;70(4):244–252. doi: 10.1159/000369026. [DOI] [PubMed] [Google Scholar]
- 51.Schieve LA, Tian LH, Rankin K, et al. Population impact of preterm birth and low birth weight on developmental disabilities in US children. Ann Epidemiol. 2016;26(4):267–274. doi: 10.1016/j.annepidem.2016.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wu YC, Hsieh WS, Hsu CH, et al. Intervention effects on emotion regulation in preterm infants with very low birth weight: A randomize controlled trial. Res Dev Disabil. 2016;48:1–12. doi: 10.1016/j.ridd.2015.10.016. [DOI] [PubMed] [Google Scholar]
- 53.Van de Weijer-Bergsma E, Wijnroks L, Jongmans MJ. Attention development in infants and preschool children born preterm: a review. Infant Behav Dev. 2008;31(3):333–351. doi: 10.1016/j.infbeh.2007.12.003. [DOI] [PubMed] [Google Scholar]
- 54.Witt A, Theurel A, Borradori Tolsa C, et al. Emotional and effortful control abilities in 42-month-old very preterm and full-term children. Early Hum Dev. 2014;90(10):565–569. doi: 10.1016/j.earlhumdev.2014.07.008. [DOI] [PubMed] [Google Scholar]
- 55.Guilherme Monte Cassiano R, Gaspardo CM, Cordaro Bucker Furini G, Martinez FE, Martins Linhares MB. Impact of neonatal risk and temperament on behavioral problems in toddlers born preterm. Early Hum Dev. 2016;103:175–181. doi: 10.1016/j.earlhumdev.2016.09.015. [DOI] [PubMed] [Google Scholar]
- 56.Sadeh A, De Marcas G, Guri Y, Berger A, Tikotzky L, Bar-Haim Y. Infant sleep predicts attention regulation and behavior problems at 3-4 years of age. Dev Neuropsychol. 2015;40(3):122–137. doi: 10.1080/87565641.2014.973498. [DOI] [PubMed] [Google Scholar]
- 57.Bernier A, Carlson SM, Deschenes M, Matte-Gagne C. Social factors in the development of early executive functioning: a closer look at the caregiving environment. Dev Sci. 2012;15(1):12–24. doi: 10.1111/j.1467-7687.2011.01093.x. [DOI] [PubMed] [Google Scholar]
- 58.Spruyt K, Aitken RJ, So K, et al. Relationship between sleep/wake patterns, temperament and overall development in term infants over the first year of life. Early Hum Dev. 2008;84(5):289–296. doi: 10.1016/j.earlhumdev.2007.07.002. [DOI] [PubMed] [Google Scholar]
- 59.Sorondo BM, Reeb-Sutherland BC. Associations between infant temperament, maternal stress, and infants' sleep across the first year of life. Infant Behav Dev. 2015;39:131–135. doi: 10.1016/j.infbeh.2015.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Vaughn BE, Elmore-Staton L, Shin N, et al. Sleep as a support for social competence, peer relations, and cognitive functioning in preschool children. Behav Sleep Med. 2015;13(2):92–106. doi: 10.1080/15402002.2013.845778. [DOI] [PubMed] [Google Scholar]
- 61.Jian N, Teti DM. Emotional availability at bedtime, infant temperament, and infant sleep development from one to six months. Sleep Med. 2016;23:49–58. doi: 10.1016/j.sleep.2016.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Molfese VJ, Rudasill K, Molfese D. Sleep in preschoolers: School readiness, academics and behavior. In: Wolfson A, Montgomery-Downs H, editors. The Oxford Handbook of Infant, Child, and Adolescent Sleep and Behavior. New York, NY: Oxford University Press; 2013. pp. 397–413. [Google Scholar]
- 63.Vanderveen JA, Bassler D, Robertson CM, Kirpalani H. Early interventions involving parents to improve neurodevelopmental outcomes of premature infants: a meta-analysis. J Perinatol. 2009;29(5):343–351. doi: 10.1038/jp.2008.229. [DOI] [PubMed] [Google Scholar]


