Abstract
Restless genital syndrome refers to excessive and persistent sensations of genital and clitoral arousal with the absence of conscious feeling of sexual desire. These sensations have been linked to symptoms of restless legs syndrome (RLS) or an overactive bladder. Restless genital syndrome may be related to small fiber sensory neuropathy of the dorsal nerve of the clitoris, so it more frequently occurs in women. The association with RLS suggests a possible dopaminergic mechanism. We report a case of a 74-year-old woman who presented restless genital symptoms every night in association with RLS symptoms. During polysomnography she reported 3 awakenings from rapid eye movement sleep with associated genital symptoms followed by a period of insomnia with RLS symptoms and sexual activity. The frequency and the intensity of the symptoms were responsive to treatment by pramipexole after 1 week of treatment and the efficacy was maintained at follow-up.
Citation:
Sforza E, Hupin D, Roche F. Restless genital syndrome: differential diagnosis and treatment with pramipexole. J Clin Sleep Med. 2017;13(9):1109–1110.
Keywords: dopamine agonists, restless genital syndrome, restless legs syndrome
INTRODUCTION
Restless genital syndrome (RGS) is an uncommon sleep disorder; most studies on its potential origin and treatment have been published in the form of case reports. The most frequent alternative diagnosis is genital arousal disorder (GAD),1 a condition more frequently found in women. GAD is characterized by unwanted genital subjective sexual arousal triggered by nonsexual stimuli or emotion, eliciting stress and lasting hours or days, occurring constantly and with little or no relief by masturbation or sexual activity. Two publications have posited that RGS should be diagnosed when a patient meets criteria for GAD and also has restless legs syndrome (RLS) symptoms or an overactive bladder.1,2 Vascular diseases (pelvic varices), stress, overactive bladder, pelvis nerve entrapment, and drugs such as lamotrigine or cessation of paroxetine intake have been theorized as causes for GAD.3 Because the disorder is not responsive to pharmacological therapies, its cause is thought to be psychological. Cognitive behavioral therapy is currently the most common treatment for GAD.4
RGS refers to an uncommon experience of unwanted and unpleasant genital sensation and excessive dysesthesia at genital and clitoris levels exaggerated by sitting and lying down during the night. It is sometimes accompanied by RLS5 and is partially relieved by sexual activity or masturbation. RGS is typically found in middle-aged and elderly women. Clinical and instrumental investigations suggest, as in GAD, a hyper-esthesia and neuropathy of the small fiber of the dorsal nerve of the clitoris, with its touching triggering hyperesthesia in the dermatome of the pudendal nerve.2,6 However, the reported similarity between RGS and restless legs,5 the presence of another variant of RLS (ie, restless abdomen syndrome7 and restless bladder syndrome), the presence of RLS during the nocturnal event, and its presence in Parkinson disease8,9 may suggest that RGS is a phenotypic variant of RLS with a common dopaminergic mechanism.
REPORT OF CASE
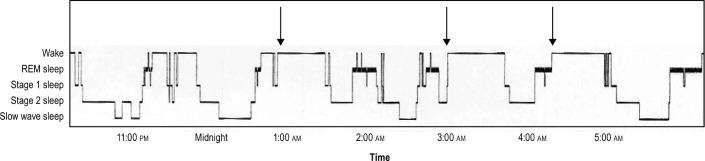
A 74-year-old woman was referred to our sleep clinic for insomnia and nocturnal experiences of spontaneous, unwanted, intrusive, excessive, and persistent sensation at the genital, clitoris, and vulvar level with partial relief by masturbation, sexual activity, and walking. The duration of these experiences were short, less than 20 minutes, but repeated 2 to 3 times during the night at approximately 1.5-hour intervals and occurred 5 times per week (Figure 1). The woman had a diagnosis of RLS 8 years prior, and her RLS was defined by urgency to move the legs frequently associated with unpleasant legs sensations; worsening of the symptoms at rest, sitting, or lying down; partial and temporary relief by activity and walking; and worsening later in the day or night. No family history of RLS was reported. The RLS symptoms were treated by clonazepam; clonazepam was not effective in managing her genital symptoms. The clinical and radiological examinations were unremarkable, except for the occurrence of occasional symptoms of RLS (twice per month) during the evening or night in the past 3 weeks. Electromyography excluded neuropathy of the pelvic nerves. No symptoms of anxiety and depression were found at the clinical interview. Three events of RGS were reported during the night of polysomnography occurring at the end of rapid eye movement sleep periods followed by awakening with masturbation and sexual activity. During the night, 4 sequences of periodic leg movements were scored, and the periodic leg movement index was 15 events/h of sleep.
Figure 1. Histogram of nocturnal sleep.
Three episodes of restless genital symptoms like those described by the patient were recorded at approximately 1:00 AM, 3:15 AM, and 4:10 AM at awakenings from rapid eye movement (REM) sleep. The events were followed by a long awakening associated with sexual activity, masturbation, and walking.
Pramipexole at a dose of 0.25 mg 1 to 2 hours before sleep reduced the frequency and the intensity of the genital discomfort with an efficacy present after 2 weeks of treatment and that persisted at 2-year follow-up.
CONCLUSIONS
To our knowledge this is the first case report of RGS confirmed by a nocturnal sleep study showing that pramipexole was an efficacious treatment. The presence of associated RLS and the successful treatment with pramipexole suggest a similar underlying dopaminergic mechanism. Physicians should be vigilant in their practice to recognize RGS, as it is probably underreported by patients to whom dopamine agonists may be prescribed.
DISCLOSURE STATEMENT
The authors report no conflicts of interest in this work.
REFERENCES
- 1.Facelle TM, Sadeghi-Nejiad H, Goldmeier D. Persistent genital arousal disorder: characterization, etiology and management. J Sex Med. 2013;10(2):1459–1558. doi: 10.1111/j.1743-6109.2012.02990.x. [DOI] [PubMed] [Google Scholar]
- 2.Waldinger MD, Venema PL, van Gils AP, Schweitzer DH. New insights into restless genital syndrome: static mechanical hyperesthesia and neuropathy of the nervus dorsalis clitoridis. J Sex Med. 2009;6(10):2778–2787. doi: 10.1111/j.1743-6109.2009.01435.x. [DOI] [PubMed] [Google Scholar]
- 3.Jackowich RA, Pink L, Gordon A, Pukall CF. Persistent genital arousal disorder: a review of its conceptualizations, potential origins impact and treatment. Sex Med Rev. 2016;4(4):329–342. doi: 10.1016/j.sxmr.2016.06.003. [DOI] [PubMed] [Google Scholar]
- 4.Aswath M, Pandit LV, Kashyap K, Ramnath R. Persistent genital arousal disorder. Indian J Psychol Med. 2016;38(4):341–343. doi: 10.4103/0253-7176.185942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Akcali A, Ferini-Strambi L, Haynak H, Karadeniz D, Akcali C. Genital restlessness (vulvodynia) events accompanying restless legs syndrome. Sleep Med. 2009;10(3):395–396. doi: 10.1016/j.sleep.2008.03.006. [DOI] [PubMed] [Google Scholar]
- 6.Waldinger MD, Venema PL, van Gils AP, de Lint GJ, Schweitzer DH. Stronger evidence for small fiber sensory neuropathy in restless genital syndrome: two case reports in males. J Sex Med. 2011;8(1):325–330. doi: 10.1111/j.1743-6109.2010.02079.x. [DOI] [PubMed] [Google Scholar]
- 7.Perez-Diaz H, Iranzo A, Santamaria J. Restless abdomen: a phenotypic variant of restless legs syndrome. Neurology. 2011;77(13):1283–1286. doi: 10.1212/WNL.0b013e318230207a. [DOI] [PubMed] [Google Scholar]
- 8.Aquino CC, Mestre T, Lang AE. Restless genital syndrome in Parkinson disease. JAMA Neurol. 2014;77(12):1559–1561. doi: 10.1001/jamaneurol.2014.1326. [DOI] [PubMed] [Google Scholar]
- 9.Suzuki K, Miyamoto T, Hirata K, Miyamoto M. Pathophysiological similarity between restless genital syndrome and restless legs syndrome in Parkinson's disease. Rinsho Shinkeigaku. 2015;55(11):848–849. doi: 10.5692/clinicalneurol.cn-000760. [DOI] [PubMed] [Google Scholar]