Abstract
Background
Performance of thyroid surgery as a same day surgery procedure has been a controversial topic. This study aimed to compare the safety and efficacy of outpatient thyroid surgery with inpatient thyroid surgery by meta-analysis of current literature.
Methods
Articles were identified from the following keyword searches: outpatient thyroidectomy/thyroid surgery, same day thyroidectomy/thyroid surgery. Outcomes included perioperative complications including recurrent laryngeal nerve (RLN) injury, hypocalcemia, and readmissions. Data were extracted following review of appropriate studies by authors and random effects models were used.
Results
34 potentially relevant publications were identified and 14 studies fulfilled the predetermined inclusion criteria, totaling 10,478 patients, 4,565 of whom were discharged the same day following thyroid surgery. There was no difference in malignancy rate between the two groups (95% CI, 0.84–2.31; P=0.196). Inpatient group were 2.23 times (95% CI, 1.36–3.36; P=0.001) more likely to develop transient RLN injury and 2.32 times (95% CI, 1.06–5.06; P=0.034) more likely to have documented transient hypocalcemia compared to outpatients. Inpatient groups were 2.10 times (95% CI, 1.33–3.33; P=0.002) more likely to have documented other complications. The two groups also had similar readmission rates (95% CI, 0.71–1.41; P=1.000).
Conclusions
Our meta-analysis suggests that discharging selective patients the same day after a thyroid surgery is as safe, feasible, and efficacious as admitting them for observation. Admitting patients after thyroid surgery is associated with higher reported risk of complications.
Keywords: Outpatient thyroid surgery, same day thyroid surgery, outpatient thyroidectomy, same day thyroidectomy
Introduction
The United States healthcare system is under increased scrutiny to reduce cost without undermining the quality of patient care. Patient comfort and economic considerations have made a significant impact on the evolving trend towards ambulatory surgery. Along with the advancements in postoperative care and anesthesia, more procedures are performed on an outpatient same-day basis (1).
Recently, the American Thyroid Association published an interdisciplinary consensus statement on ambulatory thyroid surgery. The committee concluded that outpatient thyroidectomy may be undertaken safely in a carefully selected patient population provided that certain precautionary measures are taken to maximize communication and minimize the likelihood of complications (2). However, surgeons have been less adaptive with this trend due to its feared complications related to thyroid surgery. Physicians are more comfortable with the notion that postoperative care is safer in the hospital where close-monitoring for potential life threatening complications, particularly, bilateral vocal fold paresis, expanding neck hematoma, and hypocalcemia can be conducted. Nevertheless, the incidence of complications resulting from thyroid surgery is relatively low ranging from 1.9% to 11.5% (1-8), and mortality rates are less than 1% (2). Additionally, circumventing the need for patient admission has been shown to diminish a number of iatrogenic postoperative complications, as well as decreasing the incidence of hospital acquired infections (9,10). These findings, along with an effort to limit unnecessary hospital stays and conserve valuable healthcare resources, has prompted the current meta-analysis and systematic review, which evaluates the outcomes and safety related to same-day outpatient thyroid surgery.
Methods
Identification of trials and data extraction
Articles published through June 2014 on PubMed, EMBASE, and the Cochrane Database of Systematic Review was systematically searched by two independent reviewers using the following medical subject headings (MeSH): “outpatient thyroidectomy”, “outpatient thyroid surgery”, “same-day thyroid surgery”, and “same-day thyroidectomy”. Additionally, all articles included in the analysis underwent reference review for other potential articles. The inclusion criteria for eligibility were as follows: (I) articles comparing outpatients who underwent same-day thyroid surgery with inpatients who underwent thyroid surgery; (II) controlled clinical trials, multicenter studies, or randomized controlled trials; (III) studies that reported intraoperative and postoperative outcomes, including total operative time, estimated blood loss, length of hospitalization, and intraoperative and postoperative complications; and (IV) studies that reported a measure of variance (standard error, standard deviation, or confidence interval). Articles not reported in English were excluded. For research groups with redundant patient populations, the latest study on that patient population was included for analysis. Results from the two independent reviews were compared for accuracy, with disagreement resolved by consensus.
Statistical analysis
Primary outcomes of this study were: total operative time, estimated blood loss, length of hospitalization, and intraoperative and/or postoperative complications. Odds ratios were calculated for categorical outcomes, while mean net changes were calculated for continuous variables. DerSimonian and Laird random-effects models were used to pool mean net changes or odds ratios across the studies (11). The presence of heterogeneity was assessed with Cochran’s Q test and its extent quantified with the I-square index. Funnel plots were constructed in order to assess publication bias and Begg’s rank correlation test was used to examine the asymmetry of these plots. Egger’s weighted linear regression test was used to examine the association between the mean effect estimate and its variance. Additionally, sensitivity analyses were conducted by excluding each study in turn, to evaluate their relative influence on the pooled estimates. All analyses were conducted in STATA (version 10; College Station, Texas, USA).
Results
Search results
We identified a total of 34 potentially relevant articles. Of the original 34 articles, 1 was removed due to the article not being in English. After further screening, we excluded a total of 15 articles because they did not specify the length of outpatient stay or allowed patients to spend the night and were still labeled as same-day surgery subjects. Furthermore, four articles were excluded due to utilization of data on the same subjects as in previous studies by the same authors. A total of 14 articles were included in our analysis. The flow chart diagram for the selection of publications included in this meta-analysis is shown in Figure 1.
Figure 1.
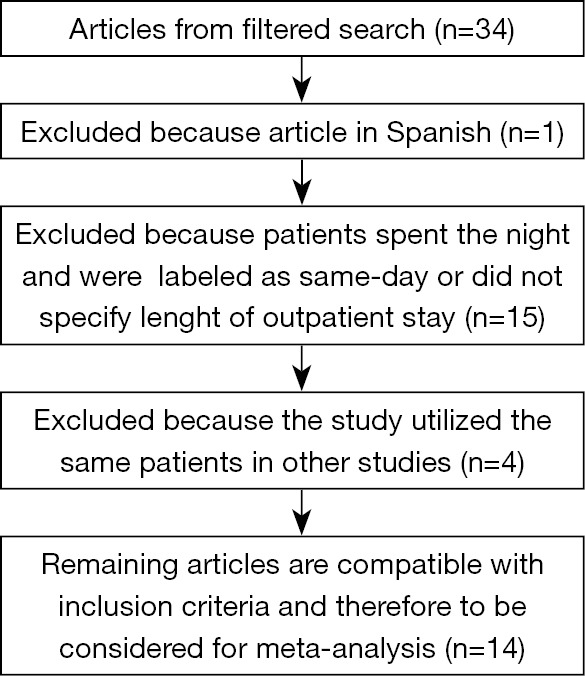
Descriptive flowchart of included studies.
Description of the included studies
A total of 10,526 patients were included in the study, of which 3,787 were discharged the same day following thyroid surgery and 6,739 were admitted as inpatients following thyroid surgery. The main characteristics of the included studies are summarized in Table 1.
Table 1. Descriptive characteristics of included studies.
| Authors/Reference | Year | Study type | Sample (n) | Inpatient (n) | Outpatient (n) |
|---|---|---|---|---|---|
| Almeida et al. (12) | 2010 | Retrospective review of prospective data | 100 | 50 | 50 |
| Seybt and Terris (5) | 2010 | Retrospective review of prospective data | 418 | 210 | 208 |
| Snyder et al. (6) | 2010 | Retrospective review of prospective data | 1,242 | 178 | 1,064 |
| Mazeh et al. (13) | 2012 | Retrospective review of prospective data | 608 | 310 | 298 |
| Chin et al. (3) | 2007 | Retrospective case control | 114 | 64 | 50 |
| Tuggle et al. (14) | 2011 | Retrospective | 6,762 | 5,594 | 1168 |
| Lo Gerfo et al. (15) | 1991 | Retrospective | 134 | 58 | 76 |
| Mowschenson and Hodin (16) | 1995 | Retrospective | 100 | 39 | 61 |
| Inabnet et al. (17) | 2008 | Retrospective | 224 | 44 | 180 |
| Teoh et al. (18) | 2008 | Retrospective | 50 | 1 | 49 |
| Champault et al. (19) | 2009 | Retrospective | 95 | 13 | 82 |
| Trottier et al. (8) | 2009 | Retrospective | 232 | 1 | 231 |
| Sklar et al. (20) | 2011 | Retrospective | 247 | 153 | 94 |
| Sahmkow et al. (21) | 2012 | Prospective | 200 | 24 | 176 |
Total complications
12 studies reported on overall complication rates related to outpatient surgery (OPS). Complication rates ranged from 0–26% (6,20). When meta-analysis was performed to compare inpatient vs. outpatient complications, five studies were identified including 2,482 patients (3-6,12,13). There was a trend towards an increased likelihood of overall complications in the inpatient group (Figure 2).
Figure 2.
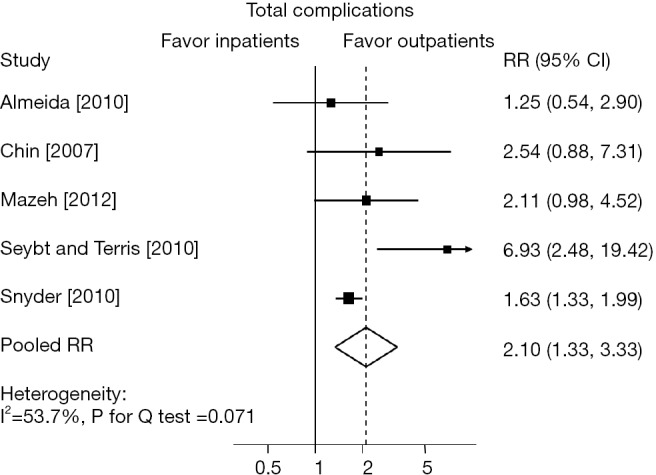
Total complications related to outpatient thyroid surgery.
Transient recurrent laryngeal nerve (RLN) injury
Five studies (6,15,17,19,21) comprising 1,717 cases identified the proportion of outpatients with a transient RLN injury and reported results ranged from 0–4% (6,15). Only one study by Snyder et al. (6) reported on inpatient and outpatient results (Figure 3).
Figure 3.
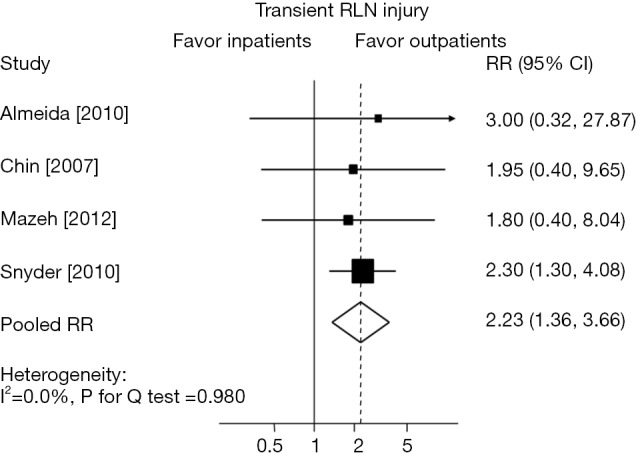
Transient recurrent laryngeal nerve (RLN) injury relations to outpatient surgery (OPS).
Permanent RLN injury
Ten studies comprising 2,505 cases reported on permanent RLN injury in OPS cases (5,6,8,13,15,17-19,21), with rates ranging from 0–2% (13,18,19). There were 11 reported cases (0.4%) of vocal cord paralysis. When meta-analysis was performed comparing inpatient and outpatient surgical cases (2,195 cases) there was no difference noted.
Hypocalcemia
There were eight studies that reported on transient hypocalcemia in OPS cases (5,6,8,13,15,17,19,21) (2,455 cases) with a reported incidence from 1–21% (6,19). Transient hypocalcemia documented by post-operative lab testing was documented in 270 cases (11%). Three studies (5,6,13) compared inpatient to outpatient hypocalcemia rates and included a total of 2,268 cases. Patients who were admitted were more likely to experience transient hypocalcemia (Figure 4).
Figure 4.
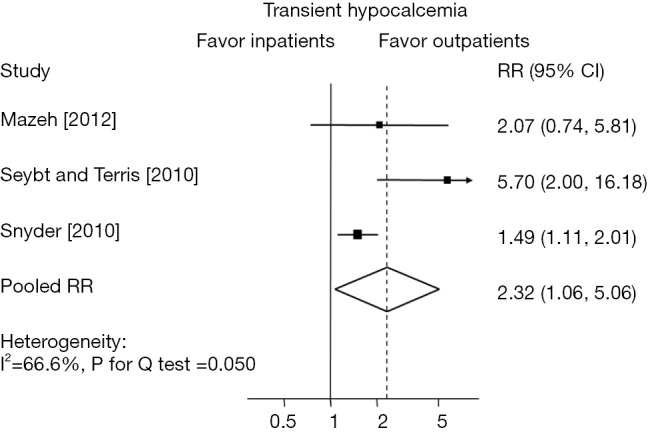
Transient postoperative hypocalcemia relations to outpatient surgery (OPS).
Hematoma
Thirteen studies (3,5,6,8,12,13,15-21) reported on the rate of hematoma formation which ranged from 0–2% (3,5,6,12,15,16,20,21). A meta-analysis of 2,760 outpatients was performed and there were 8 total cases of hematoma formation (0.02%). Of the 7 studies (3,6,8,12,17-19) that did report hematoma, three studies (6,8,12) reported hematomas that occurred after the patient had left the hospital (4 patients; 0.01%). When meta-analysis was performed to compare inpatient vs. OPS, three studies were included (8,18,19) (435 patients). Inpatients were 17.5 times more likely to develop a hematoma than outpatients (Figure 5). Champault et al. (19) reported that drains were not used in any patients; Teoh et al. (18) stated that drains were “not routinely used,” and the final study, Trottier et al. (8), did not report on drain use. It should be noted that patients who were the American Statistical Association (ASA) III or IV were largely excluded from OPS (8,18,19).
Figure 5.
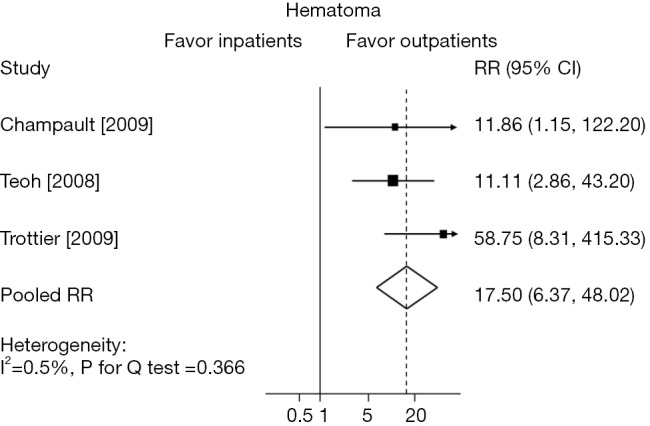
Hematoma formation relations to outpatient surgery (OPS).
Malignancy
Eight studies (5-10,13,20) identified the final pathologic diagnosis of patients undergoing outpatient thyroidectomy. Malignant pathology was identified in 322 outpatient cases (23%). When a meta-analysis was performed to compare inpatient vs. outpatient cases in these studies; two studies (5,13) were identified including 1,026 patients. There was a trend towards an increased likelihood of a malignant pathology in the inpatient group (Figure 6).
Figure 6.
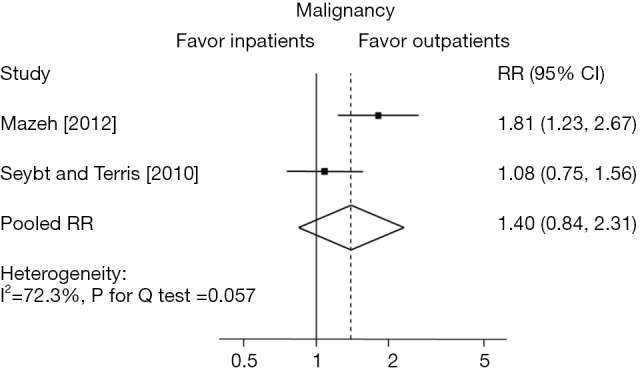
Rate of malignancy in relation to outpatient surgery (OPS).
Readmission
There were ten studies (5,6,8,14-16,18-21) that looked at readmission rates after outpatient thyroidectomy and rates ranged from 0–2.3% (4,15,16,18-20). When meta-analysis was performed on the outpatients (3,306 patients), we found a readmission rate of 1.5%. When a comparative meta-analysis was performed to compare inpatient vs. OPS, two studies (5,14) were identified (7,180 cases) and the likelihood for readmission was similar between outpatient and inpatient groups (Figure 7).
Figure 7.
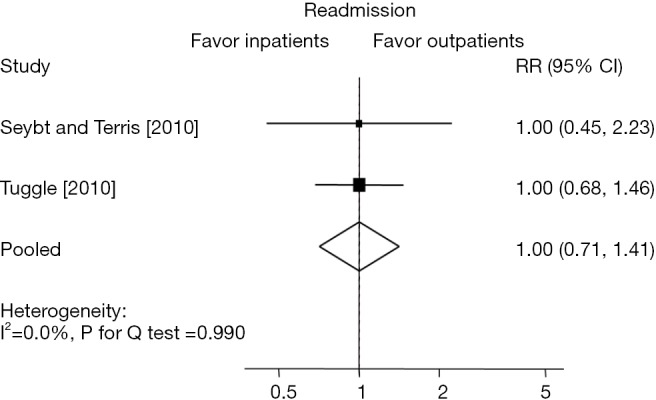
Rate of readmission in relation to outpatient surgery (OPS).
Discussion
Recently, The American Thyroid Association commissioned an interdisciplinary Task Force to develop a consensus statement to help define the eligibility criteria for outpatient thyroidectomy (2). However, despite its increasing popularity, the consensus for outpatient thyroid surgery remains far from unanimous.
The potential advantages of outpatient thyroid surgery entails three distinct categories: patient satisfaction, patient safety, and conservation of resources. Samson et al. (22) reported that of 655 patients undergoing outpatient thyroid surgery, 646 were ‘very pleased’, while the remaining nine were ‘pleased’. None expressed any displeasure with regards to early discharge. Additionally, Snyder et al. (6) and Spanknebel et al. (23) have also assessed patient satisfaction and found that very few patients expressed dissatisfaction with their experiences of outpatient thyroid surgery. Patients may prefer OPS from the comfort and convenience perspective that it affords. A restful and familiar setting surrounded by supportive and adequately prepared family and friends may be preferable to an unfamiliar and often chaotic hospital environment.
The patient’s safety and welfare remain imperative during recovery from thyroid surgery. Exposure to the ubiquitous nosocomial organisms that populate our hospitals such as methicillin-resistant Staphylococcus aureus, and vancomycin resistant enterococcus, is reduced because of less time spent in the hospital environment (9). Furthermore, the opportunity for serious iatrogenic events may also be reduced in the outpatient setting (10).
The United States healthcare system is under increased scrutiny to reduce cost without undermining the quality of patient care. Maximizing the efficiency of OPS serves to minimize utilization of critical hospital resources that may instead be relocated to other important needs. Studies have demonstrated that outpatient thyroid surgery provides an average savings of $2,500 per encounter compared to inpatient operations (6,7). Each day that a patient spends in the hospital will incur numerous fixed and variable expenses. The majority of health insurance plans charge patients a percentage of the expenses, or a copay, for each day spent in the hospital. Such expenses have naturally created an attitude change in some patients in favor of OPS.
Careful patient selection and clinical judgment is of paramount importance in pursuit of a successful outpatient thyroid surgery. The future of outpatient thyroid surgery lies in establishing safety outcomes comparable with traditional inpatient thyroidectomy. We found that eleven studies listed operative criteria for OPS (3,5,6,8,12,13,15-21) (Table 2). Common inclusion criteria were: absence of significant medical comorbidity, ASA I/II, adequate home support in the post-operative period, adequate patient autonomy/education, access to a telephone, close proximity to the hospital, and a motivation to have OPS. Common exclusion criteria were: significant medical co-morbidity, ASA III/IV, lack of motivation for outpatient therapy, home distance far from the hospital, anticoagulant treatment, no home support in the post-operative period, lack of patient autonomy/education, and patients undergoing concurrent operations typically performed on an inpatient basis.
Table 2. Operative criteria of OPS.
| Study name | Criteria for OPS | Observation period (hours) | Discharge criteria |
|---|---|---|---|
| Almeida et al. (12) | Exclusion criteria for OPS were: rejection of ambulatory regimen by the patient, lack of motivation for an outpatient procedure, cognitive disability or low educational level that could not permit an early recognition of the alert signs of a major complication, home distance from hospital over 20 km, and lack of adequate home facilities | 6 | Re-evaluated by surgeon before discharge |
| Seybt and Terris (5) | Cooperative patient interested in OPS, absence of significant medical comorbidities, no anticoagulant treatment or other need for drain, no concomitant procedures (e.g., lateral neck dissection), sufficient patient autonomy and social support | Not defined | Stable wound and airway with normal vital signs, ambulatory and tolerating diet, pain controlled with oral medications, able to void, availability of person to take patient home |
| Snyder et al. (6) | Patients undergoing additional operations typically performed on an outpatient basis were included in the study. Similarly, patients undergoing additional operations typically performed on an inpatient basis were excluded from the study | Not defined | Met standardized hospital criteria for discharge |
| Mazeh et al. (13) | Exclusion criteria for OPS: comorbidities that may require longer observation owing to the nature of their underlying disease, patients who live >3 hours away or with no individuals to stay with at home | 3 | Re-evaluated by the attending surgeon before discharge |
| Chin et al. (3) | Inclusion criteria: characteristics of the lesion (4 cm and below), and the patient’s fitness for surgery and postoperative family support. Exclusion criteria: large retrosternal goiters, goiters causing tracheal obstruction or deviation, patients who were ASA class 3 and above, and patients who could not meet the general criteria for same-day surgery procedures | ≥6 | Re-evaluated by surgeon before discharge |
| Tuggle et al. (14) | Not defined | Not defined | Not defined |
| Lo Gerfo et al. (15) | All patients emotionally and intellectually capable of understanding the procedure and post-operative plan | 4 | Re-evaluated by surgeon & if patient felt ready to go |
| Mowschenson and Hodin et al. (16) | Not defined | 6 | Re-evaluated by surgeon before discharge |
| Inabnet et al. (17) | Not defined | ≥5 | The patient was observed for 5–6 hours, at which time the wound was evaluated and the Prolene suture removed by a member of the surgical team. If the patient was deemed stable by the surgical team, they were then discharged |
| Teoh et al. (18) | Age <70 years, ASA grade I/II. BMI <30 kg/m2, benign unilobular thyroid disease, willingness to undergo surgery on a day case basis, responsible adult available to care for the patient postoperatively in the first 24 h, easy access to a telephone | Not defined | Reevaluated by the surgeon and anesthesiologist |
| Champault et al. (19) | Exclusion criteria were: ASA of III or IV, anticoagulation treatment, the presence of sleep apnea, age >75 years, live >50 km from the hospital, no functional telephone line, and the absence of an adult willing to accompany them home and to stay with them overnight. In addition, for the first 5 years (1999 to 2003), the following were also exclusion criteria: toxic adenoma, suspicious (indeterminate) cyto-diagnosis on preoperative fine-needle aspiration (hypercellularity and a pattern suggestive of follicular- or Hurthle-cell neoplasms or atypical features), and completion thyroidectomy after contralateral thyroid lobectomy | 6 | The decision to discharge was made by both the surgeon and an anesthesiologist before 17:30. If patients tolerated oral fluid, could walk, had passed urine spontaneously, and had no dyspnea. Pain medications given, and in cases of subsequent total thyroidectomy, thyroxin were supplied to the patients at discharge |
| Trottier et al. (8) | Patient within a 1-hour drive from the hospital for at least 48 hours and with adequate support at home. Hemi-thyroidectomies and subtotal thyroidectomies completed by 13:00 to allow adequate time to monitor | 4 | Re-evaluated by surgeon and anesthesiologist |
| Sklar et al. (20) | A partial thyroidectomy was performed and patients must live or be staying within 20 minutes of the hospital and must have a responsible adult at home the first night after the surgery and an ASA risk score of III or less with a stable medical condition | 4 | Ability to tolerate fluids, comfortable breathing and no need for supplemental oxygen, adequate pain control and a prescription for pain medication, a dry incision, and a responsible adult with them to provide transportation home. The operating surgeon had to re-evaluate before discharge |
| Sahmkow et al. (21) | Any total, lobe, or completion thyroid with or without central neck. Exclusion criteria: history of coagulation problems or current aspirin use, severe comorbidity or uncontrolled systemic disease, simultaneous surgery, lack of social support, housing >1 hour drive from hospital | 3 | Re-evaluated by a surgeon, an adult to drive patient home, and “usual discharge criteria” |
OPS, outpatient surgery; ASA, the American Statistical Association.
The 14 studies included in this analysis reported on the majority of the outcomes of interest. Twelve studies reported on overall complication rates related to OPS. Complication rates ranged from 0–26% (6,20). There was a great deal of heterogenicity in the types of complications reported and how complication rates were measured which lends to the discrepancy in the rates and makes drawing a conclusion from the overall rates difficult to interpret. Complications were found in a total of 351 cases (13%). The increased likelihood of overall complications in the inpatient group is obviously biased since most studies lateralized their patients with greater risk and co-morbidities to the inpatient group. For example, patients that may have been more likely to form a hematoma secondary to a bleeding disorder or need for anti-coagulation were largely excluded from the outpatient group.
Only one study compared transient RLN injury between the two groups (6). The remainder of the studies either did not report this complication or simply identified the number of patients with post-operative hoarseness for undefined periods of time. When fiberoptic laryngoscopy was performed to detect nerve weakness there were a total of 46 reported cases (2.6%). However, there was significant heterogenicity found between studies and inconsistency on reporting when patients underwent post-operative laryngoscopy to diagnose a nerve paralysis and the true number of transient paralysis are likely underrepresented.
Among the complications, there was a net finding of an increased incidence of transient hypocalcemia in patients who were admitted. Three studies compared inpatient to outpatient transient hypocalcemia (5,6,13). Patients who were admitted were more likely to experience transient hypocalcemia. However, there was a great deal of variance in the timing of collecting post-operative calcium samples. Some were collected as an inpatient, some as an outpatient, and some groups only measured serum calcium when the patient was symptomatic (Table 3). Thus, the true rate of hypocalcemia is most likely greatly underreported in most studies. Additionally, hypocalcemia rates were typically reported for the entire group of patients, but after closer examination, transient hypocalcemia almost exclusively occurred following total or completion thyroidectomy (5,8,13,15). Four studies reported re-admitting patients for hypocalcemia (5,6,8,21). Finally, eight studies, comprising a total of 2,305 cases, reported a lower rate of permanent hypocalcemia in patients discharged the same day (less than 1%) (3,5,6,8,12,13,15,17,19-21).
Table 3. Descriptive characteristics of postoperative calcium and PTH values.
| Study name | Post-op calcium checked | Post-op PTH checked | Post-op calcium replacement | Post-op vitamin D replacement |
|---|---|---|---|---|
| Almeida et al. (12) | Not reported | Not reported | No | Not reported |
| Seybt and Terris (5) | No | Not reported | Yes | Yes |
| Snyder et al. (6) | No | No | Yes, both in total and subtotal thyroidectomy | Yes, both in total and subtotal thyroidectomy |
| Mazeh et al. (13) | No | Yes, but only for total thyroidectomy for 1 year of the study | Yes, but only for 1 year of the study | Yes, but only for 1 year of the study |
| Chin et al. (3) | Not reported | Not reported | Not reported | Not reported |
| Tuggle et al. (14) | Not reported | Not reported | Not reported | Not reported |
| Lo Gerfo et al. (15) | No | No | No | Not reported |
| Mowschenson and Hodin (16) | No | Not reported | No | Not reported |
| Inabnet et al. (17) | Not reported | Not reported | Yes | Not reported |
| Teoh et al. (18) | No | No | Not reported | Not reported |
| Champault et al (19) | No | No | No | No |
| Trottier et al. (8) | No | Not reported | Yes, for both total and completion thyroidectomy | Not reported |
| Sklar et al. (20) | Not reported | Not reported | Not reported | Not reported |
| Sahmkow et al. (21) | No | Yes, but only for total or completion thyroidectomy | Only if PTH ≤50% of pre-op value & only in completion or total thyroidectomy | Only if PTH ≤50% of pre-op value & only in completion or total thyroidectomy |
PTH, parathyroid hormone.
No study reported performing routine in-hospital calcium measurements. Two studies reported routinely measuring parathyroid hormone (PTH) levels while in the hospital but only for total thyroidectomy patients (13,21) or completion thyroidectomy patients (21). Most studies only reported/recommended laboratory tests to detect hypocalcemia in symptomatic patients. The two studies that examined PTH levels for total thyroidectomy or completion thyroidectomy prior to discharge found in-hospital hypocalcemia rates in 7–10% of patients (13,21). As suggested before, the rates of hypocalcemia are most likely underreported in other studies. Limited publications, paired with the varying sample sizes of these studies, necessitate further investigation into this outcome before comparative inferences can be drawn.
Ten studies reported on a minimum observation period (3,8,12,13,16,17,19-21). Observation periods ranged from 3 hours (12,17) to 6 hours (3,12,16,19) (Table 2). Of the ten studies that reported on minimum observation periods, the averaged reported time was 4.7 hours. Twelve studies reported on patients that were intended to undergo OPS that required an unplanned admission (3,5,8,12,13,15-21). Unplanned admission rates ranged from 0–43% (12,15). When meta-analysis was performed of 2,439 patients, the unplanned admission rate was 10%. The reasons for overnight admission ranged widely from hypocalcemia to patient preference. Studies with unplanned admission rates less than or equal to 5% (8,12,18,20) had strict selection criteria largely including those with healthier patients, living within close proximity of the hospital, having adequate home support, and an education level that could allow for recognition of a complication; in addition, all but 16 of the patients with a 5% or less unplanned admission rate were strictly partial thyroidectomies.
Snyder et al. (6) reported on four patients who died within 30 days of thyroid surgery (0.3%). Three of these were after planned inpatient thyroidectomies; one on postoperative day 6 from pulmonary hypertension with right heart failure, one on postoperative day 8 from tracheal stenosis with respiratory arrest, and one on postoperative day 9 from cardiac failure secondary to metastatic follicular cancer with uncontrollable thyroid storm. One elderly nursing home patient in the outpatient thyroidectomy group died during sleep 2 days postoperatively from a presumed cardiac event. These deaths were the only mortalities found in our literature search.
This literature review provides the latest evidence for same-day thyroidectomy, to date. However, the small number of studies eligible for inclusion paired with a lack of randomization and clinical trials involving this approach warrant further research. Our analysis shows that discharging patients the same day following a thyroidectomy procedure is as safe and effective as admitting them for observation. Additional studies, including cost-benefit analysis and larger controlled trials, are needed to further assess cost effectiveness, clinical outcomes, and patient satisfaction with same-day thyroid surgery
Acknowledgements
This research and work was fully supported by Tulane University Medical Center.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.CDC National Center for Health Statistics Website. Available online: http://www.cdc.gov/media/pressrel/2009/r090128.htm, accessed June 5, 2014.
- 2.Terris DJ, Snyder S, Carneiro-Pla D, et al. American thyroid association statement on outpatient thyroidectomy. Thyroid 2013;23:1193-202. 10.1089/thy.2013.0049 [DOI] [PubMed] [Google Scholar]
- 3.Chin CW, Loh KS, Tan KS. Ambulatory thyroid surgery: an audit of safety and outcomes. Singapore Med J 2007;48:720-4. [PubMed] [Google Scholar]
- 4.Hall BL, Hirbe M, Yan Y, et al. Thyroid and parathyroid operations in veterans affairs and selected university medical centers: results of the patient safety in surgery study. J Am Coll Surg 2007;204:1222-34. 10.1016/j.jamcollsurg.2007.02.073 [DOI] [PubMed] [Google Scholar]
- 5.Seybt MW, Terris DJ. Outpatient thyroidectomy: experience in over 200 patients. Laryngoscope 2010;120:959-63. [DOI] [PubMed] [Google Scholar]
- 6.Snyder SK, Hamid KS, Roberson CR, et al. Outpatient thyroidectomy is safe and reasonable: experience with more than 1,000 planned outpatient procedures. J Am Coll Surg 2010;210:575-82, 582-4. [DOI] [PubMed]
- 7.Terris DJ, Moister B, Seybt MW, et al. Outpatient thyroid surgery is safe and desirable. Otolaryngol Head Neck Surg 2007;136:556-9. 10.1016/j.otohns.2006.09.024 [DOI] [PubMed] [Google Scholar]
- 8.Trottier DC, Barron P, Moonje V, et al. Outpatient thyroid surgery: should patients be discharged on the day of their procedures? Can J Surg 2009;52:182-6. [PMC free article] [PubMed] [Google Scholar]
- 9.National Nosocomial Infections Surveillance System National Nosocomial Infections Surveillance (NNIS) System Report, data summary from January 1992 through June 2004, issued October 2004. Am J Infect Control 2004;32:470-85. 10.1016/j.ajic.2004.10.001 [DOI] [PubMed] [Google Scholar]
- 10.To err is human: Building a safer health system 1999 Institute of Medicine.
- 11.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials 1986;7:177-88. 10.1016/0197-2456(86)90046-2 [DOI] [PubMed] [Google Scholar]
- 12.Almeida C, Campos M, Leal T, et al. Outpatient hemi-thyroidectomy: is it safe? Ambulatory Surg 2010;16:17-9. [Google Scholar]
- 13.Mazeh H, Khan Q, Schneider DF, et al. Same-day thyroidectomy program: Eligiblity and safety evaluation. Surgery 2012;152:1133-41. 10.1016/j.surg.2012.08.033 [DOI] [PubMed] [Google Scholar]
- 14.Tuggle CT, Roman S, Udelsman R, et al. Same-Day Thyroidectomy: A Review of practice patterns and outcomes for 1,168 procedures in New York State. Ann Surg Oncol 2011;18:1035-40. 10.1245/s10434-010-1398-0 [DOI] [PubMed] [Google Scholar]
- 15.Lo Gerfo P, Gates R, Gazetas P. Outpatient and short-stay thyroid surgery. Head Neck 1991;13:97-101. 10.1002/hed.2880130203 [DOI] [PubMed] [Google Scholar]
- 16.Mowschenson PM, Hodin RA. Outpatient thyroid and parathyroid surgery: A prospective study of feasibility, safety, and costs. Surgery 1995;118:1051-3; discussion 1053-4. 10.1016/S0039-6060(05)80113-8 [DOI] [PubMed] [Google Scholar]
- 17.Inabnet WB, Shifrin A, Ahmed L, et al. Safety of same day discharge in patients undergoing sutureless thyroidectomy: A comparison of local and general anesthesia. Thyroid 2008:18:57-61. 10.1089/thy.2007.0148 [DOI] [PubMed] [Google Scholar]
- 18.Teoh AY, Tang YC, Leong HT. Feasibility study of day case thyroidectomy. ANZ J Surg 2008;78:864-6. 10.1111/j.1445-2197.2008.04681.x [DOI] [PubMed] [Google Scholar]
- 19.Champault A, Vons C, Zilberman S, et al. How to perform a thyroidectomy in an outpatient setting. Langenbecks Arch Surg 2009;394:897-902. 10.1007/s00423-009-0527-3 [DOI] [PubMed] [Google Scholar]
- 20.Sklar M, Ali MJ, Solomon P. Outpatient thyroid surgery in a Toronto community hospital. J Otolaryngol Head Neck Surg 2011;40:458-61. [PubMed] [Google Scholar]
- 21.Sahmkow SI, Audet N, Nadeau S, et al. Outpatient thyroidectomy: safety and patients' satisfaction. J Otolaryngol Head Neck Surg 2012;41 Suppl 1:S1-12. [PubMed] [Google Scholar]
- 22.Samson PS, Reyes FR, Saludares WN, et al. Outpatient thyroidectomy. Am J Surg 1997;173:499-503. 10.1016/S0002-9610(97)00019-6 [DOI] [PubMed] [Google Scholar]
- 23.Spanknebel K, Chabot JA, DiGiorgi M, et al. Thyroidectomy using monitored local or conventional general anesthesia: an analysis of outpatient surgery, outcome and cost in 1,194 consecutive cases. World J Surg 2006;30:813-24. 10.1007/s00268-005-0384-3 [DOI] [PubMed] [Google Scholar]


