Abstract
Cancer is a major cause of childhood death, with central nervous system (CNS) neoplasms being the second most common pediatric malignancy, following hematological cancer. Treatment of pediatric CNS malignancies requires multimodal treatment using a combination of surgery, chemotherapy, and radiotherapy, and advances in these treatments have given favorable results and longer survival. However, treatment-related toxicities have also occurred, particularly for radiotherapy, after which secondary cancer, reduced function of irradiated organs, and retarded growth are significant problems. Proton beam therapy (PBT) is a particle radiotherapy with excellent dose localization that permits treatment of liver and lung cancer by administration of a high dose to the tumor while minimizing damage to surrounding normal tissues. Thus, PBT has the potential advantages for pediatric cancer. In this context, we review the current knowledge on PBT for treatment of pediatric CNS malignancies.
Keywords: proton beam therapy, pediatric, children, brain, proton radiotherapy
Introduction
A total of 2,000 solid malignancies are newly diagnosed each year in Japan, and 800 of these tumors are indicated for radiotherapy1). Pediatric brain tumor is the most common among pediatric solid malignancies. Multimodal therapy is required for treatment of brain tumor, and radiotherapy plays an important role.2,3) Advances in multimodal therapy have improved the outcomes for pediatric brain tumor, but the long-term effects of radiotherapy have become significant problems. These effects include retardation of cognitive function, impairment of social adjustment, neuroendocrine disorder, growth impairment, acoustic disturbance, vascular disorder, and secondary cancer.4–6)
A proton beam is categorized as low linear energy transfer (LET) radiation, similarly to photon radiotherapy, and has a similar relative biological effectiveness (RBE). The LET is a measure of energy transfer to matter from an ionizing particle travelling through the matter; it is closely related to energy per unit distance and provides an indication of ion-induced damage. The RBE is defined as the ratio of the photon dose to the proton dose required to give the same biological effect under identical irradiation conditions. Proton beams used in clinical practice are normally considered to have an RBE of 1.1.7–9) That is, the biological effects of protons are similar to those of photons, with no apparent clinical advantage. Therefore, proton beam therapy (PBT) is generally thought to be applicable for most uses of photon radiotherapy. However, a proton beam has a sharp energy peak called the Bragg peak, which spreads out to cover the tumor volume (spread out of the Bragg Peak; SOBP). The energy before the peak is suppressed and the energy behind the peak is almost zero. This means that the dose to normal tissue around the tumor can be reduced in PBT compared to photon radiotherapy, and this is especially beneficial for a pediatric tumor or a tumor adjacent to normal tissue for which irradiation should be strictly avoided.10–13)
Mizumoto et al. found a low rate of late toxicity using PBT for pediatric malignancies in studies performed in Japan.14,15) In a comparison of proton and photon radiotherapy for pediatric brain tumors, including low-grade glioma, ependymoma, craniopharyngioma, and medulloblastoma, Merchant et al. suggested that proton radiotherapy has consistent advantages in reducing the low and intermediate (0–40 Gy) dose areas.16) Also, a relatively small critical normal organ, such as the cochlea and hypothalamus, can be preserved in PBT when not adjacent to the primary tumor volume. These advantages can result in preservation of intelligence, endocrine function, and hearing.16) Herein, we review the use of PBT for pediatric central nervous system (CNS) tumors. For comparison with the results of standard radiotherapy, papers were mainly selected based on three recent reviews written on pediatric brain tumor.17–19) The outcomes of standard radiotherapy and PBT in articles are shown in Tables 1–5.
Table 1.
Treatment results of radiotherapy for pediatric glioma
| Authors (year) | Number of patients | Follow-up | Radiotherapy | Additional treatment | Result | Late toxicity |
|---|---|---|---|---|---|---|
| Macdonald et al., 200520) | 76 (HGA) | - 56 died |
Photon; 59.4 Gy, 1.8 Gy / Fr | Chemo before RT Randomly assigned 3 protocols | 5y-OS 24% 5y-EFS 8% | 11 had grade 3 or 4 CNS toxicities. |
| Merchant et al., 200921) | 78 (LGG) | 89 months (28–137) | Photon; 54.0 Gy, 1.8 Gy / Fr | Chemo before RT (n = 25) Surgery (none 13, one 42, two 18, three 5) | 5y-OS 98.5%, 10y-OS 95.9% 5y-EFS 87.4%, 10y-EFS 74.3% | Vasculopathy 4.8% (7y) |
| Hug et al., 200224) | 27 (LGG) | 3.3 years (0.6–6.8) | Proton; 55.2 GyE (50.4–63.0) 1.8 GyE / Fr | 25 of 27 were unresectable or residual disease | OS 85% LC 78% | Moyamoya disease: 1 |
| Greenberger et al., 201425) | 32 (LGG) | 7.6 years (3.2–18.2) | Proton; 52.2 GyE (48.6–54.0) | Chemo before RT (n = 16) Surgery (none 5, biopsy only 6, one 17, two or more 4) | 8y-OS 100% 8y-PFS 82.8% | Vasculopathy: 2 |
Fr: fraction, HGA: high grade astrocytoma, LC: Local control, LGG: low grade glioma, 3 protocols: carboplatin/etoposide ifomide/etoposide cyclophosmide/etoposide, y-EFS: year event free survival, y-OS: year overall survival, y-PFS: year progression free survival.
Table 5.
Treatment results of radiotherapy for pediatric craniopharyngioma
| Authors (year) | Number of patients | Follow-up | Radiotherapy | Additional treatment | Result | Late toxicity |
|---|---|---|---|---|---|---|
| Merchant et al., 200679) | 28 | 36.6 months (24.4–80.0) | Photon; 54.0–55.8 Gy, 1.8 Gy / Fr | Surgery (n = 27) | 3y-PFS 90.3% | - |
| Minniti et al., 200778) | 39 | 40 months (3–88) | Photon; 50 Gy / 30Fr, 50 Gy / 33Fr, 55 Gy / 33Fr | Surgery: Complete 2, Incomplete 34, Biopsy 3 | 3y-OS 100%, 5y-OS 100% 3y-PFS 97%, 5y-PFS 92% | No second tumors |
| Klimo et al., 201580) | 97 | 9 years (0.7–19.0) | Photon; 54 Gy / 30Fr | Surgery | 5y-OS 98.9%, 10y-OS 94.5% 5y-PFS 94.1%, 10y-PFS 87.8% | Vasculopathy: 1 |
| Luu et al., 200681) | 16 | 60.2 months | Proton; 50.4–59.4 GyE, 1.8 GyE / Fr | Surgery (all) RT (n = 1) | Local control 14/15 | Panhypopituitarism: 1 Vascular accident: 1 |
| Winkfield et al., 200982) | 24 | 40.5 months (6–78) | Proton; 52.2–54.0 GyE, 1.8 GyE / Fr | Surgery (all) 4 were biopsy | No local failure | - |
| Bishop et al., 201483) | 31 | 106 months | IMRT; 50.4–54.0 GyE, 1.8 GyE / Fr | Surgery: Gross total (n = 1) Subtotal (n = 11), Other (n = 19) | 3y-OS 96.8% 3y-NFFS 96.4% | Hypothalamic obesity: 9 |
| 21 | 33 months | Proton; 50.4–54.0 GyE, 1.8 GyE / Fr | Surgery: Gross total (n = 5) Subtotal (n = 9), Other (n = 7) | 3y-OS 94.1% 3y-NFFS 91.7% | Hypothalamic obesity: 4 |
Fr: fraction, y-NFFS: year nodular failure free survival, y-OS: year overall survival, y-PFS: year progression free survival.
Glioma
Postoperative radiotherapy is essential for treatment of high-grade glioma. However, the prognosis is very poor, despite use of combined modality therapies of surgery, radiotherapy, and chemotherapy. Macdonald et al. found a 5-year overall survival (OS) of only 24% in pediatric patients with high-grade glioma treated with photon radiotherapy of 59.4 Gy in 33 fractions.20) 11 of 76 patients had Grade 3 or 4 toxicities in CNS (Seizure, motor weakness, adventitial movement and ataxia).
In contrast, standalone surgery is curative for focal resectable low-grade glioma, and use of radiotherapy for low-grade glioma is controversial. When complete resection is achieved, the 10-year OS of patients with low-grade glioma is 80–90%.21) However, unresectable tumors that develop in central locations such as the pons and optic pathways, and recurrent tumors requires multimodal therapy. In a phase II study of 78 pediatric patients with low-grade glioma treated with radiotherapy of 54 Gy in 30 fractions, Merchant et al. obtained 10-year OS and event-free survival (EFS) of 95.9% and 74.3%, respectively, and the incidence of vasculopathy was 4.79% in a median follow-up period of 89 months.21) The incidence of vasculopathy was higher for patients under 5 years old. It was concluded that these results did not compromise disease control and that radiotherapy should be delayed in patients younger than 5 years old due to concerns of late treatment failure, vasculopathy, and secondary cancer. PBT may reduce the risk of these toxicities because of dosimetric advantages22,23) and normal tissue sparing in high dose areas can be achieved using proton beams. For example, in 7 patients with optic nerve glioma treated with PBT, Fuss et al. found that doses to the contralateral optic nerve, chiasm, pituitary, temporal lobe and frontal lobe were significantly reduced compared to those with photon radiotherapy.22) Merchant et al. have shown that PBT may preserve reading ability compared to photon radiotherapy.16)
Three retrospective studies have reported treatment results using PBT for glioma. In 27 pediatric patients with low-grade glioma (mostly tumors that were unresectable or residual disease) Hug et al. found that PBT at a total dose of 50.4–63.0 GyE (median 55.2 GyE) resulted in OS of 85% and a local control rate of 78% in a follow-up period of 3.3 years.24) One patient with associated neurofibromatosis developed Moyamoya disease. Greenberger et al. showed that PBT at 48.6–54.0 GyE (median 52.2 GyE) in 32 patients with low-grade glioma gave an 8-year OS of 100% and 8-year progression-free survival (PFS) of 82.8% over a mean follow-up period of 7.6 years.25) Vasculopathy occurred in 2 patients (6.2%), but stabilization or improvement of visual acuity was achieved in 83% of patients at risk for radiation-induced injury to optic pathways. In preliminary results for PBT at a median total dose of 54 GyE in fractions of median 1.8 GyE in 13 patients with low-grade glioma, Hauswald et al. found tumor progression in only one patient and no severe acute toxicity.26) These studies indicate that PBT has advantages for unresectable low-grade glioma due to avoidance of irradiation of critical tissues and reduced toxicities. At this time, late toxicity peculiar to proton beam therapy was not happened. And in-field vasculopathy was common late toxicity of PBT and photon radiotherapy.
Medulloblastoma
Medulloblastoma is a common malignant pediatric brain tumor that arises in the posterior fossa. This tumor is characterized by its propensity for leptomeningeal spread. Therefore, medulloblastoma requires craniospinal irradiation (CSI), but this leads to late toxicities, including intelligence retardation, hormonal deficiency, short stature, and hearing loss.27) Therefore, in the 1990s, reduction of the CSI dose was encouraged, and the dose was reduced from 36 Gy to 23.4 Gy. The current commonly used dose-fractionation for medulloblastoma is CSI of 23.4 Gy in 13 fractions followed by involved-field radiation therapy (posterior fossa boost) of 30.6 Gy in 17 fractions.28–30) Packer et al showed about half patients had grade 3–4 CNS late toxicities after long term follow-up.28)
One prospective study and three retrospective studies have described treatment results using PBT for medulloblastoma. Jimenez et al. reported that 13 of 15 patients who received PBT (CSI 21.6 GyE, total 54.0 GyE) were alive without recurrence after 39 months follow-up.31) 9 of 15 patients had measurable sensorineural hearing loss, including 2 with grade 3 ototoxicity. And 3 patients had grade 2 endocriopathy requiring hormone replacement.
Sethi et al. found that 93 of 109 patients who received PBT (CSI 23.4 GyE, total 54.0 GyE) were alive without recurrence after 38.8 months follow-up.32) Both studies used a similar irradiated dose to that used in photon radiotherapy, and the outcomes were good, although the follow-up period was still short. In a recent comparison of photon radiotherapy to PBT at a median dose of 23.4 Gy CSI followed by boost to a cumulative dose of 54.0 to 55.8 Gy, Eaton et al. found no significant difference in 6-year recurrence-free survival (RFS) (PBT 78.8% vs. photon 76.5%) and 6-year OS (82.0% vs. 87.6%).33) 3 patients treated with photon radiation therapy developed a second malignancy, and no patients treated with protons developed a second malignancy.
The treatment volume of CSI is large and the risk of late toxicity and secondary cancer is higher than for other irradiation fields. Intracranial toxicities are a significant problem in whole brain irradiation and posterior fossa boost, with intelligence retardation, hormonal deficiency and ototoxicity being common after irradiation for medulloblastoma. Walter et al. found that full scale intelligence quotient (FSIQ) declines by 3.7 points per year with a CSI dose of 36 Gy,34) and Ris et al. reported an intelligence quotient (IQ) loss of 4.2 points per year with a CSI dose of 23.4 Gy,35) indicating that there may be no difference in the effects of CSI doses of 36 Gy and 23.4 Gy. However, using PBT, doses to critical intracranial structures such as the cochlea, temporal lobe, hippocampus, and hypothalamic-pituitary axis can be reduced, which preserves the function of these structures and maintains intelligence more effectively than photon radiotherapy.31,36–39) In a prospective phase II study of PBT in 59 patients with medulloblastoma, Yock et al. reported a hearing loss rate of 16% at 5 years, and an IQ loss of 1.5 points per year driven mostly by falls in processing speed and verbal comprehension.37) In a comparison of clinical outcomes of medulloblastoma between PBT and photon radiotherapy with a CSI dose of 23.4 Gy and a boost of 30.6 Gy, Eaton et al. found no significant difference in RFS or OS between patients treated with protons vs. photons (6-year RFS: 78.8% vs. 76.5%, P = 0.948; 6-year OS 82.0% vs. 87.6%, P = 0.285).33) The same group compared endocrine outcomes in 77 patients with medulloblastoma treated with chemotherapy and PBT (n = 40) or photon radiotherapy (n = 37), and found that PBT reduced the requirement for endocrine replacement therapy (55% vs. 78%, P = 0.03).36) Moeller et al. found a 1-year high-grade ototoxicity rate of 5% after PBT,40) and in 111 patients with medulloblastoma treated with PBT of ≥50 GyE, Giantsoudi et al. found 5-year incidences of CNS injury of 3.6% for any grade and 2.7% for grade 3 or more.41) In this study, 4 patients experienced symptomatic injury, but 3 of 4 received a whole posterior fossa boost. The risk of late injury in this study was similar to that reported for photon radiotherapy. Min et al evaluated the risk of alopecia after PBT for medulloblasoma.42) The skin dose was higher by proton beams compared to photon beams, because proton beams do not have a build-up effect. The threshold for alopecia treated with CSI was 21 GyE.42) Cochran et al. reported that the dose to the lens can be reduced using PBT for CSI, especially for patients under 10 years old.43)
There are many dose-volume histogram (DVH) analyses that indicate that PBT can reduce the risk of late toxicity and secondary cancer (Table 6).44–48) According to Zhang et al., the calculated total lifetime attributable risk for second cancer after PBT is much lower than that after photon radiotherapy, with a lifetime risk ratio of 0.18.48) There is a large benefit of PBT, especially for CSI, and the question can be asked: “Are protons the only ethical approach?”.49) In this article, their answer was “Yes”.49) based on there being sufficient evidence to support the argument that all children with medulloblastoma should be offered PBT.
Table 6.
Dosimetric comparison and late toxicity of proton beam therapy
| Authors (year) | Patients | Assessment strategy | Result |
|---|---|---|---|
| Harrabi et al.,201623) | 74 (LGG) | 3D-CRT vs. PBT (RO; Optic nerve, Inner ear, Optic chiasm, Thalamus, Brain, Brain stem, etc) | PBT reduced the dose to risk organs (DVH analysis) |
| Merchant et al., 200816) | 40 (OPG/CR/MB /EP = 10/10/10/10) | Photon vs. PBT (RO; Brain, Hypothalamus, Cochlea) | PBT reduced the dose to risk organs not adjacent to tumor. Functional preservation was expected (DVH analysis). |
| Brodin et al., 201192) | 10 (MB) | 3D-CRT vs. IMPT Evaluate second cancer risk | IMPT plans compared favorably to photon radiotherapy (DVH analysis) |
| Zhang et al., 201444) | 17 (MB) | Photon vs. Proton Evaluate risk of second cancer and cardiac mortality | PBT significantly reduced the risk of second cancer and cardiac mortality (DVH analysis) |
| Cochran et al., 200843) | 39 (MB) | Photon vs. Proton Evaluate dose to the lens | PBT significantly reduced the dose to the lens (DVH analysis) |
| Brodin et al., 201438) | 17 (MB) | 3D-CRT vs. IMRT vs. Proton Evaluate the dose of Hippocampus | PBT significantly reduced the dose to the hippocampus (DVH analysis) |
| Howell et al., 201245) | 18 (MB) | Photon vs. Proton (RO; Liver, Heart, Lung, Thyroid, Kidney, Esophagus) | PBT reduced the dose to risk organs (DVH analysis) |
| Kuhlthan et al., 201293) | 142 (MB/PNET 50, EP 31, LGG 20, other 41) | Evaluate health-related quality of life (HRQoL) after PBT | CSI and chemotherapy were negatively correlated with HRQoL Comparison was not performed between photon and proton |
| Yock et al., 201637) | 59 (MB) | Evaluate late toxicity after PBT (CSI 23.4 GyE, boost dose 54.0 GyE) | 3-year incidence of Grade 3–4 hearing loss was 12% 5-year incidence rate of any neuroendocrine deficit was 55% Comparison was not performed between photon and proton |
| Pulsifer et al., 201539) | 60 (28 CSI, 32 partial brain) | Evaluate full scale IQ, verbal comprehension, perceptual reasoning, working memory | Comparison was not performed between photon and proton |
| Eaton et al., 201636) | 77 (MB) | Proton vs. Photon Evaluate endocrine outcome | proton vs photon; hypothyroidism 23% vs 69%, Sex hormone deficiency 3% vs 19%, any endocrine replacement therapy 55% vs 78%. PBT may reduce the risk of some endocrine abnormalities. |
| Moeller et al., 201140) | 23 (MB) | Evaluate early ototoxicity after PBT | 1-year grade 3 or 4 ototoxicity rate was 5% Comparison was not performed between photon and proton |
| Giantsoudi et al., 201541) | 111 (MB) | Evaluate incidence of CNS injury after PBT | 5-year incidence of grade 3 or more CNS injury was 2.7% Comparison was not performed between photon and proton |
| Min et al., 201442) | 12 (MB) | Evaluate alopecia after PBT | Permanent alopecia was associated with dose to the skin. |
| Indelicato et al., 201491) | 313 (EP 73, CR 68, LGG 66, MB 38, Other 68) | Evaluate pediatric brain stem toxicity after PBT (received 50.4 GyE or more to the brain stem) | 2-year incident of grade 3 or more brain stem toxicity was 2.1% Comparison was not performed between photon and proton |
| Park et al., 201576) | 17 (GCT) | Proton vs. IMRT (RO; brain, hippocampus, pituitary gland) | PBT significantly reduced the dose to risk organs except for the pituitary gland. (DVH analysis) |
| Beltran et al., 201284) | 14 (CR) | Proton vs. IMRT (RO; brain, cochlea, chiasm, hippocampus, optic nerve, brain stem, body) | PBT significantly reduced the dose to brain and body (DVH analysis) |
| Boehling et al., 201285) | 10 (CR) | IMPT vs. IMRT (RO; Hippocampus, carotid, brain stem, brain) | PBT reduced the dose to a variety of risk organs (DVH analysis) |
CR: craniopharyngioma, CSI: craniospinal irradiation, DVH analysis: non-clinical data: only in theory, EP: ependymoma, GCT: germ cell tumor, IMPT: intensity-modulated proton therapy, LGG: low grade glioma, MB: medulloblastoma, OPG: optic pathway glioma, RO: risk organ.
Historically, small round blue cell tumors of the cerebellum have been grouped under medulloblastoma. However, medulloblastoma is now considered to be a single entity with four molecular subgroups (wingles (WNT), sonic hedgehog (SHH), group 3, group 4) with distinct demographics, clinical features and genetics.50–56) Future treatment strategies may be customized according to these subgroups. However, considering the long life span after the treatment for pediatric patients, there is a need to minimize the dose to ensure healthy growth and to preserve normal tissue to maintain cognitive function and endocrine function, and reduce radiation therapy-related truncal organ dysfunction. PBT has robust benefits in all of these respects, even though the survival outcome is similar to that in photon radiotherapy.49,57)
Ependymoma
Ependymoma is a tumor arising from ependymal cells. More than half of cases occur in children younger than 3 years old and are located in the posterior fossa. In the treatment of ependymoma, surgical resection is the most important factor and local control is the key. Radiotherapy is applied postoperatively at doses of 50.4–59.4 GyE, except after complete resection of Grade 2 supratentorial ependymoma.58–60) The treatment volume in early studies included prophylactic CSI, but the efficacy was not been established. More recently, the clinical target volume (CTV) has generally been defined as the gross target volume (GTV) (remnant tumor or tumor bed) plus a 1.5-cm margin. However, Merchant et al. conducted radiotherapy for 153 patients with ependymoma or anaplastic ependymoma using a 1.0-cm margin and obtained favorable results of a 7-year local control rate of 88.7%, OS of 85.0%. All local recurrence was found within the 95% iso-dose irradiation area, which suggested that reduction of the irradiation field might be possible.59) The incident rate of brain stem necrosis was 2.5%, and the incident of a secondary malignancy at 7 years was 4.07%, respectively.
Reduction of the treatment field is currently an important issue under discussion in Japan.
PBT can be used as radiotherapy for ependymoma. Using pencil beam scanning PBT for 50 patients with ependymoma using 0.5- to 1-cm CTV margins to the GTV and a dose of 54–60 GyE (median, 59.4 GyE), Ares et al. obtained 5-year OS and local control rates of 84% and 78.0%, respectively.61) Severe toxicities occurred in 3 patients (6%): unilateral deafness in 2 patients and fatal brainstem necrosis in one patient.61)
A comparison of dosimetry in intensity-modulated radiotherapy (IMRT) and PBT for patients with ependymoma by MacDonald et al. showed several advantages of PBT. Thus, the mean doses to the temporal lobe were 16 Gy with IMRT, but only 4 Gy with PBT and 2 Gy with IMPT; 5% and 50% of the pituitary received 16 and 12 Gy with IMRT, respectively, but <1 cGyE with PBT and IMPT; the hypothalamus received mean doses of 10.7 Gy with IMRT and 0.2 GyE with PBT; and the mean doses to the left cochlea were 37 Gy with IMRT, but only 2 cGyE with PBT and <0.1 cGyE IMPT. The average dose to the cochlea should be kept at <32 Gy to avoid hearing loss.62) In a report of the clinical results of PBT for 70 patients with ependymoma by the same authors, gross total resection (GTR) was obtained for 66% of the patients, and the delivered dose ranged from 50.4 to 60 GyE in fractions of 1.8 GyE. The 3-years PFS and OS were 76% and 95%, respectively. The mental development index (MDI)/IQ decline was not significant, with a mean time interval of 2.21 years. The average total MDI/IQ was 108.5 at baseline and 111.3 at follow up (P = 0.475). Growth hormone replacement was required in 2 patients.63) Merchant et al. showed that PBT for ependymoma reduces the dose for organs at risk, such as the brain, hypothalamus and cochlea.16) We also found a similar tendency for reduction of the dose to normal brain tissue with PBT compared to photon radiotherapy64) (Fig. 1).
Fig. 1.
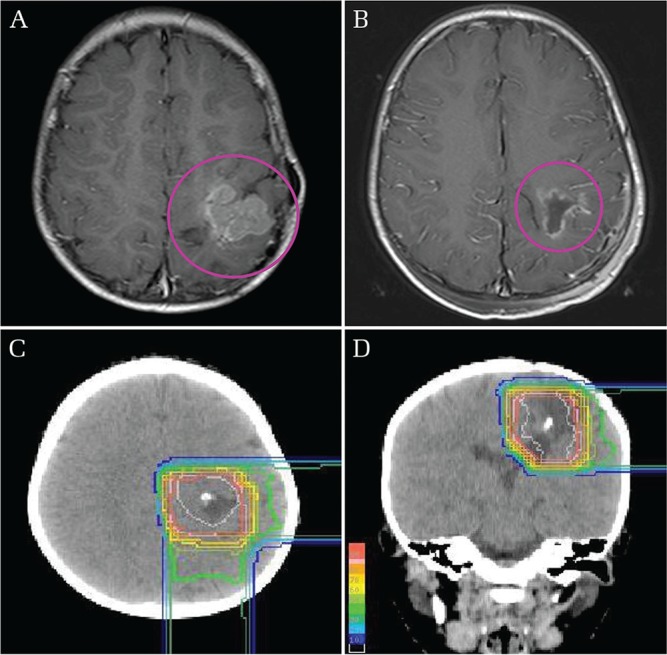
(a) 3-year-old boy had a parietal lobe tumor. (b) Tumor excision was performed and was diagnosed as an anaplastic ependymoma. Postoperative proton beam therapy was started 37 days after surgery. (c and d) A dose of 59.4 GyE in 33 fractions was initially administered to the tumor bed. Normal brain outside the blue line was completely avoided. So in theory, late toxicity and secondary cancer were prevented by PBT in the area.
Radiotherapy is also used as a treatment modality for recurrent ependymoma. The first choice treatment for intracranial recurrent is surgical resection, and radiotherapy is also effective, even as re-irradiation. Bouffet et al. reported the results of 47 patients with recurrent ependymoma, 29 of whom were treated with surgical resection and/or chemotherapy and 18 received full dose re-irradiation of ≥54 Gy.65) The 3-year OS rates were 7% and 81% in these respective groups. During a mean follow up period of 3.7 years, 2 patients who underwent re-irradiation had endocrine dysfunction and one required special education support. Eaton et al. reported the results of PBT for re-irradiation in 20 pediatric patients with intracranial ependymoma.66) The patients were initially treated with 52.2–59.4 GyE. Fourteen of the patients received repeated PBT at a previously treated site for local failure, and most received second PBT at >50 GyE. Grade 2 toxicities occurred in 3 patients. The 3-year PFS was 28.1% (95% CI: 15.6–40.6%) and 66% of the patients had distant failure, indicating that re-irradiation with PBT is safe and effective.
In a recent study by Gunther et al., imaging changes on magnetic resonance image (MRI) were more frequent in patients with intracranial ependymoma treated with PBT compared to those treated with IMRT, with 16 of 37 patients treated with PBT and 6 of 35 patients treated with IMRT showing MRI changes.67) Brainstem toxicity is a major concern for irradiation of ependymoma located in the posterior fossa. Therefore, these results suggest that PBT is a higher risk treatment than IMRT. However, 15 of the 22 patients with MRI changes were asymptomatic, and of the 7 patients with symptoms, 3 received IMRT and 4 received PBT. Moreover, patients who received PBT had a trend for better 4-year OS. The reasons for the MRI changes are unclear, but it is clear that careful attention to brainstem toxicities are required, even though PBT is acceptable and beneficial for patients with ependymoma.
Germinoma
Germ cell tumors (GCTs) of various histologic subtypes arise from primordial germ cells of developing embryos. These tumors are divided into two histologic groups with germinoma and non-germinomatous components (NGGCT). Intracranial GCTs mainly arise in the suprasellar region or pineal gland, and are usually localized, but sometimes disseminate to the CNS. The tumors are generally sensitive to chemotherapy and radiotherapy, and the method of radiotherapy is decided based on the histologic type, age, and metastatic extent.
Germinoma is the most common type of GCT and has a favorable prognosis, with 10-year OS of 90%.68,69) Germinoma has high sensitivity to radiotherapy, and chemoradiotherapy plays an important role in treatment. However, long survival has revealed late treatment toxicities. Currently, standard radiotherapy for an intratubular GCT (ICGT) is whole ventricular irradiation (WVI) at a dose of 24 Gy in 12 fractions or 25.2 Gy in 14 fractions, followed by neoadjuvant chemotherapy.70,71) Historically, high dose irradiation of the cranio-spinal field or whole brain irradiation at 40–50 Gy had been used for germinoma, but radiation-related late toxicities were severe. Of 405 patients who survived for more than 5 years, Acharya et al. reported 20- and 30-year OS rates of 84.1% and 61.9%, respectively. There was a 59-fold increase in risk of death from stroke, and the 25-year cumulative mortality rates due to cancer and subsequent malignancy were 16% and 6%, respectively.72) In a long-term study of 111 patients with ICGT and non-IGCT, Sawamura et al. reported that 85 received radiotherapy, and that 58 of these 85 patients needed hormonal replacement therapy, 26 had a poor performance status, and only 1 patient had fathered children.73)
Based on these results, efforts have been made to reduce the irradiation dose to normal brain and preserve brain function. Bamberg et al. reduced the CSI dose to 30–36 Gy, and obtained 5-year RFS of 91%.74) As late toxicity, 23 of 60 patients had an evidence of at least one endocrine abnormality requiring hormone replacement. However, local irradiation with chemotherapy increases the risk of recurrence. In a comparison of standalone CSI and local irradiation with chemotherapy, Calaminus et al., found no significant recurrence at 5 years, but PFS was better for patients treated with CSI.70) Disease recurrence was observed in 7 of the 65 patients who received local irradiation, and was in the ventricle in 6 patients of the 7 patients. This study suggests that the ventricles should be included in the radiation field for germinoma.70)
Yang et al. used dose painting IMRT to reduce the mean dose to the whole brain, temporal lobes, hippocampus, cochlea, and optic nerves, compared to sequential IMRT.75) PBT is also advantageous for WVI, based on several comparisons with photon beams for irradiation of intracranial germinoma. Park et al. showed a dosimetric benefit of PBT over IMRT, with PBT significantly reducing the mean dose and the 10 and 15 Gy area to the normal brain.76) MacDonald et al. compared dose distributions among IMRT, three-dimensional conformal proton therapy (3D-CPT), and intensity modulated proton therapy (IMPT), and reported early clinical results for 22 patients with ICGT.77) Normal tissue was more spared using PBT, and IMPT additionally spared the brain and temporal lobe. Local control, PFS, and OS were 100, 95% and 100% for all patients. Follow-up period was still too short so it was difficult to evaluate late toxicity of PBT for germinoma.
Craniopharyngioma
Surgical resection is the most important factor in treatment of craniopharyngioma. Some authors recommend radiotherapy after conservative or maximal resection, as for gross total resection, with a total dose of 50–55 Gy.78,79) The 1- and 5-year progression-free survival does not differ between these two treatments, but neurological deficits are higher after gross total resection. However, recurrence after radiotherapy is very difficult to treat and surgical resection is the key for treatment. In 97 patients with recurrent craniopharyngeoma treated with conformal radiotherapy of 54 Gy in 30 fractions after safe resection or decompression of predominantly cystic tumors, Klimo et al. reported failure of treatment in 18 patients and 5- and 10-year treatment free-survival of 89% and 76%, respectively.80) One patient had radiation-induced vasculopathy requiring bypass surgery. Patients who received gross total resection for recurrent disease had a lower risk of subsequent recurrence, and the time interval between each treatment for new recurrence was progressively shorter. Therefore, it was concluded that craniopharyngioma progression after prior irradiation is very difficult to treat and local control is challenging, despite repeated surgical procedures.
Other reports show a 5-year PFS of about 90% after photon radiotherapy of 50–55 Gy. Three retrospective studies have examined PBT for craniopharyngioma.81–83) Luu et al. found that one of 16 patients had local recurrence after PBT of 50.4–59.4 GyE in a median follow-up period of 60.2 months.81) Long term complications were panhypopituitarism, a cerebrovascular accident and an out-of-proton field meningioma.
Winkfield et al. showed that all patients (n = 24) were well controlled in a median follow-up period of 40.5 months after PBT of 52.2–54.0 GyE.81) These studies have small numbers of patients and relatively short follow-up periods, but the results suggest that PBT can achieve similar outcomes to photon radiotherapy. In a multi-institutional comparison of PBT and conformal radiation therapy for childhood craniopharyngioma, Bishop et al. showed that survival, disease-control and toxicity were equivalent for PBT and IMRT, but it should be noted that the follow-up period for PBT was short.83) Merchant et al. showed that PBT reduced the dose to the total brain, cochlea and hypothalamus.16) and suggested that PBT may minimize intelligence diminution after radiotherapy. In dosimetric comparisons of photon radiotherapy and PBT, Beltran et al.84) and Boehling et al.85) both concluded that PBT reduced the dose to normal structures such as the brain, brainstem, optic nerve and optic chiasm. At this time, late toxicity peculiar to proton beam therapy was not happened. Vasculopathy and loss of pituitary function were common late toxicity of PBT and photon radiotherapy.
Late toxicity/Secondary cancer
Radiotherapy plays an important role in the treatment of pediatric malignancies, especially for brain tumors, because obtaining a sufficient surgical margin is difficult for brain tumors. However, radiation sensitivity in children is higher than in adults, and even a computed tomography (CT) scan may increase cancer risk.86) Toxicities related to impairment of growth and development are also significant problems in growing children, and intelligence retardation is related to the irradiation dose, age at irradiation, time since irradiation, and the mean dose to normal brain.87–89) Growth hormone is the most susceptible to irradiation among hypothalamic-pituitary hormones.34)
PBT can safely irradiate a tumor that cannot be treated by photon radiotherapy by sparing critical organs due to the high degree of dose conformity.22,90) DVH comparisons of PBT and photon radiotherapy and toxicity data after PBT are shown in Table 6. 91–93) These studies indicated that PBT significantly reduces the dose to organs at risk and the risk of secondary cancer. Pulsifer et al. analyzed cognitive function after PBT using full scale IQ (FSIQ) and its components (verbal comprehension, perceptual reasoning/organization, working memory. and processing speed) in 60 pediatric patients with brain tumor.39) FSIQ, verbal and nonverbal intelligence, and working memory were stable at a mean of 2.5 years follow up, whereas progressive cognitive decline is evident at 1–2 years after photon radiotherapy. However, reduced scores were found for processing speed, especially for younger patients (<12 years old).39)
Brain stem toxicity is also a concern in PBT. Proton beams are regarded to have similar LET and RBE to photon radiotherapy, as discussed above. However, RBE slightly increases in the very distal part of the SOBP relative to the mid-SOBP.7,9) It has also been suggested that aggressive surgery may increase brainstem sensitivity to radiation, and this toxicity is therefore of concern in postoperative PBT. In pediatric patients who received PBT of ≥50.4 GyE to the brainstem, Indelicato et al. found a 2-year incidence of brain stem toxicity of grade 3 or more of 2.1%.91) This risk of brainstem toxicity is similar to that with photon radiotherapy, and it was recommended that no more than one-third of proton beams should reach a brainstem tissue outside the planning target volume (PTV). Other analyses of brainstem injury attributed to proton beam characteristics have also suggested a clinical incidence similar to that with photon raditotherapy.41,67) Recently, we retrospectively analyzed the 62 children who were treated by PBT and followed up 5 or more years in Japan.15) The 5 year rates for grade 2 or higher late toxicity was 18% and no malignant secondary tumors occurred within irradiated. At this time late toxicity peculiar to proton beam therapy was not occurred. The rate of late toxicity and secondary tumors looks low, and these data indicate that PBT has the potential to reduce the risk of late toxicity and secondary malignancy.
Conclusion
Current PBT is mainly administered with a similar schedule to that of photon radiotherapy. Based on studies with short follow-up and a small number of patients, PBT has an equivalent therapeutic effect to that of photon radiotherapy. Many studies showed that PBT reduces the dose to an organ at risk, compared to photon radiotherapy. Although long-term follow up is required for full evaluation of the effects, PBT is a promising treatment that reduces the risk of secondary cancer and late toxicity.
Table 2.
Treatment results of radiotherapy for pediatric medulloblastoma/primitive neuroectodermal tumors (PNET)
| Authors (year) | Number of patients | Follow-up | Radiotherapy | Additional treatment | Result | Late toxicity |
|---|---|---|---|---|---|---|
| Packer et al., 200628) | 379 (Standard-Risk) | > 5 years | Photon; CSI 23.4 Gy + Fossa 32.4 Gy 1.8Gy / Fr | Chemotherapy 2 regimens | 5y-OS 86% 5y-EFS 81% | 46–51% (Grade 3 or 4 CNS toxicity) |
| Merchant et al., 200829) | 86 (Standard-Risk) | 5.1 years (0.4–9.6) | Photon; CSI 23.4 Gy + Fossa 32.4 Gy 1.8 Gy / Fr | Cyclophosphamide Cisplatin Vincristine | 5y-EFS 83.0% 5y-LC 94.7% | - |
| Lannering et al., 201230) | 340 (Standard-Risk) | 4.8 years (0.1–8.3) | Photon; CSI 23.4 Gy + Fossa 30.6 Gy 1.8 Gy / Fr, STRT CSI 36 Gy + Fossa 32 Gy 1.0 Gy (twice per day, HFRT) | Cisplatin Lomustine Vincristine | 5y-EFS 77%(STRT), 78%(HFRT) 5y-OS 87%(STRT), 85%(HFRT) | 51 patients (Grade 3 or 4 neurotoxicities) |
| Jimenez et al., 201331) | 15 (3 were PNET) | 39 months (3–102) | Proton; CSI 21.6 GyE Total 54 GyE, 1.8 GyE / Fr | Chemotherapy | 13 of 15 alive without recurrence | Grade 3 ototoxicity; 2 Grade 2 endocriopathy; 3 |
| Sethi et al., 201432) | 109 (Standard 74, High35) | 38.8 months (1.4–119.2) | Proton; CSI 23.4 GyE (18–36) Total 54 GyE, 1.8 GyE / Fr | Chemotherapy | 16 experienced relapse | - |
| Eaton et al., 201633) | 43 (Standard-Risk) | 6.2 years | Photon; CSI 23.4 Gy Total 54–55.8 Gy | Vincristine/cisplatin/ cyclophosphamide/ lomustine | 6y-OS 87.6% 6y-RFS 76.5% | 3 second malignancy |
| 45 (Standard-Risk) | 7.0 years | Proton; CSI 23.4 Gy Total 54–55.8 Gy | Vincristine/cisplatin/ cyclophosphamide/ lomustine | 6y-OS 82.0% 6y-RFS 78.8% | No second malignancy |
CSI: craniospinal irradiation, Fr: fraction, LC: Local control, 2 regimens: lomustine/cisplatin/vincristine or cyclophosphamide/cisplatin/vincristine, y-EFS: year event free survival, y-OS: year overall survival, y-RFS: year recurrence free survival.
Table 3.
Treatment results of radiotherapy for pediatric ependymoma
| Authors (year) | Number of patients | Follow-up | Radiotherapy | Additional treatment | Result | Late toxicity |
|---|---|---|---|---|---|---|
| Massimino et al., 200458) | 63 Grade 2; 43 Grade 3; 20 | 5 years (1.5–9) | Photon; Hyperfractionated 70.4 Gy, 1.1 Gy / Fr (Twice daily) 54 Gy, 2 Gy / Fr (10 patients) | VEC for ED | 5y-OS 82% (NED) 5y-PFS 65% (NED) 5y-OS 61% (ED) 5y-PFS (ED) | - |
| Merchant et al., 200959) | 153 Anaplastic; 85 | 5.3 years (0.4–10.4) | Photon; 59.4 Gy, 1.8 Gy / Fr 54.0 Gy, 1.8 Gy / Fr (age < 18 months, with gross total resection) | Prior chemo (n = 32) | 7y-OS 81.0%, 7y-PFS 69.1%, 7y-LC 83.7% (All) 7y-OS 71.8%, 7y-PFS 61.3% (anaplastic) 7y-OS 89.4%, 7y-PFS 79.2% (differentiated) Brain stem necrosis 2.5% | 4.07% (7y secondary malignancy rate) 2.5% (Brain stem necrosis) |
| Ares et al., 201661) | 50 Anaplastic; 46 | 3.6 years (0.7–9.5) | Proton; 59.4 GyE, 1.8–2.0 GyE / Fr (54–60) | Prior chemo (n = 43) | 5y-OS 84%, 5y-LC 78% (All) | 6% (> Grade 3) Brain stem necrosis: 1 Unilateral deafness: 2 |
| Macdonald et al., 201362,63) | 70 Anaplastic; 33 | 3.8 years (1–11.7) | Proton; 55.8 GyE, 1.8 GyE / Fr (50.4–60.0) | Prior chemo (n = 21) | 3y-OS 95%, 3y-PFS 76%, 3y-LC 83% (All) 3y-OS 97%, 3y-PFS 88% (GTR) 3y-OS 90%, 3y-PFS 54% (STR) | 2 patients need growth hormone replacement. No brain stem necrosis |
ED: evidence of residual disease, Fr: fraction, NED: no evidence of residual disease, y-LC: year local control, y-OS: year overall survival, y-PFS: year progression free Survival, VEC: vincristine + etoposide + cyclophosphamide.
Table 4.
Treatment results of radiotherapy for pediatric intracranial germinoma
| Authors (year) | Number of patients | Follow-up | Radiotherapy | Additional treatment | Result | Late toxicity |
|---|---|---|---|---|---|---|
| Bamberg et al., 199974) | 60 | 118 months (30–180) | Photon; CSI 36 Gy + Focal 14 Gy (2 Gy / Fr) CSI 30 Gy + Focal 15 Gy (1.5 Gy / Fr) | RT alone | 5y-OS 93.7% 5y-EFS 87.6% | 23 patients had endocrine abnormality requiring hormone replacement. |
| Calaminus et al., 201370) | 190 | 6 years (2.7–14) | Photon; CSI 24 Gy + Focal 16Gy (1.6 Gy / Fr) | RT alone | 5y-OS 95% 5y-PFS 97% | - |
| Photon; Focal 40 Gy (1.6 Gy / Fr) | ICE | 5y-OS 96% 5y-PFS 88% | - | |||
| Macdonald et al., 201177) | 22 | 28 months (30–180) | Proton; Total dose 30.6–57.6 GyE CSI/WVRT 19.5–35 GyE Focal 50.4 (n = 1) WVRT + Focal (n = 8) CSI + Focal (n = 13) | ICE for NGGCT (9/9) Platinum based chemo for GCT (11/13) | OS 100% PFS 95% | - |
CSI: craniospinal irradiation, Fr: fraction, ICE: ifosfamide + carboplatin + etoposide, NGGCT: nongerminomatous germ cell tumor, y-EFS: year event free survival, y-OS: year overall survival, y-PFS: year progression free survival.
Footnotes
Funding
This work was partially supported by Grants-in-Aid for Scientific Research (B) (15H04901) and Young Scientists (B) (25861064) from the Ministry of Education, Culture, Sports, Science and Technology of Japan.
Conflicts of Interest Disclosure
None.
References
- 1).Report of Brain Tumor Registry of Japan (1984–2000). Neurol Med Chir (Tokyo) 49 Suppl: PS1–PS96, 2009 [PubMed] [Google Scholar]
- 2).Ashley DM, Merchant TE, Strother D, et al. : Induction chemotherapy and conformal radiation therapy for very young children with nonmetastatic medulloblastoma: Children’s Oncology Group study P9934. J Clin Oncol 30: 3181–3186, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3).Geyer JR, Sposto R, Jennings M, et al. : Multiagent chemotherapy and deferred radiotherapy in infants with malignant brain tumors: a report from the Children’s Cancer Group. J Clin Oncol 23: 7621–7631, 2005 [DOI] [PubMed] [Google Scholar]
- 4).Oeffinger KC, Mertens AC, Sklar CA, et al. : Childhood cancer survivor study: chronic health conditions in adult survivors of childhood cancer. N Engl J Med 355: 1572–1582, 2006 [DOI] [PubMed] [Google Scholar]
- 5).Armitage G: Nursing assessment and diagnosis of respiratory distress in infants by children’s nurses. J Clin Nurs 8: 22–30, 1999 [DOI] [PubMed] [Google Scholar]
- 6).Armstrong GT, Liu Q, Yasui Y, et al. : Late mortality among 5-year survivors of childhood cancer: a summary from the Childhood Cancer Survivor Study. J Clin Oncol 27: 2328–2338, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7).Paganetti H, Niemierko A, Ancukiewicz M, et al. : Relative biological effectiveness (RBE) values for proton beam therapy. Int J Radiat Oncol Biol Phys 53: 407–421, 2002 [DOI] [PubMed] [Google Scholar]
- 8).Wambersie A: RBE, reference RBE and clinical RBE: applications of these concepts in hadron therapy. Strahlenther Onkol 175 Suppl 2: 39–43, 1999 [DOI] [PubMed] [Google Scholar]
- 9).Prescribing, recording, and reporting proton-beam therapy (ICRU Report 78). J ICRU 7, 2007 [Google Scholar]
- 10).Fukushima H, Fukushima T, Sakai A, et al. : Tailor-made treatment combined with proton beam therapy for children with genitourinary/pelvic rhabdomyosarcoma. Rep Pract Oncol Radiother 20: 217–222, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11).Oshiro Y, Mizumoto M, Okumura T, et al. : Clinical results of proton beam therapy for advanced neuroblastoma. Radiat Oncol 8: 142, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12).Oshiro Y, Sugahara S, Fukushima T, et al. : Pediatric nasopharyngeal carcinoma treated with proton beam therapy. Two case reports. Acta Oncol 50: 470–473, 2011 [DOI] [PubMed] [Google Scholar]
- 13).Mizumoto M, Oshiro Y, Ayuzawa K, et al. : Preparation of pediatric patients for treatment with proton beam therapy. Radiother Oncol 114: 245–248, 2015 [DOI] [PubMed] [Google Scholar]
- 14).Mizumoto M, Murayama S, Akimoto T, et al. : Proton beam therapy for pediatric malignancies: a retrospective observational multicenter study in Japan. Cancer Med 5: 1519–1525, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15).Mizumoto M, Murayama S, Akimoto T, et al. : Long-term follow-up after proton beam therapy for pediatric tumors: A Japanese national survey. Cancer Sci 108: 444–447, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16).Merchant TE, Hua CH, Shukla H, Ying X, Nill S, Oelfke U: Proton versus photon radiotherapy for common pediatric brain tumors: comparison of models of dose characteristics and their relationship to cognitive function. Pediatr Blood Cancer 51: 110–117, 2008 [DOI] [PubMed] [Google Scholar]
- 17).Laprie A, Hu Y, Alapetite C, et al. radiotherapy committee of SFCE and France Hadron : Paediatric brain tumours: A review of radiotherapy, state of the art and challenges for the future regarding protontherapy and carbontherapy. Cancer Radiother 19: 775–789, 2015 [DOI] [PubMed] [Google Scholar]
- 18).Leroy R, Benahmed N, Hulstaert F, Van Damme N, De Ruysscher D: Proton therapy in children: a systematic review of clinical effectiveness in 15 pediatric cancers. Int J Radiat Oncol Biol Phys 95: 267–278, 2016 [DOI] [PubMed] [Google Scholar]
- 19).Rombi B, Vennarini S, Vinante L, Ravanelli D, Amichetti M: Proton radiotherapy for pediatric tumors: review of first clinical results. Ital J Pediatr 40: 74, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20).MacDonald TJ, Arenson EB, Ater J, et al. : Phase II study of high-dose chemotherapy before radiation in children with newly diagnosed high-grade astrocytoma: final analysis of Children’s Cancer Group Study 9933. Cancer 104: 2862–2871, 2005 [DOI] [PubMed] [Google Scholar]
- 21).Merchant TE, Kun LE, Wu S, Xiong X, Sanford RA, Boop FA: Phase II trial of conformal radiation therapy for pediatric low-grade glioma. J Clin Oncol 27: 3598–3604, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22).Fuss M, Hug EB, Schaefer RA, et al. : Proton radiation therapy (PRT) for pediatric optic pathway gliomas: comparison with 3D planned conventional photons and a standard photon technique. Int J Radiat Oncol Biol Phys 45: 1117–1126, 1999 [DOI] [PubMed] [Google Scholar]
- 23).Harrabi SB, Bougatf N, Mohr A, et al. : Dosimetric advantages of proton therapy over conventional radiotherapy with photons in young patients and adults with low-grade glioma. Strahlenther Onkol 192: 759–769, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24).Hug EB, Muenter MW, Archambeau JO, et al. : Conformal proton radiation therapy for pediatric low-grade astrocytomas. Strahlenther Onkol 178: 10–17, 2002 [DOI] [PubMed] [Google Scholar]
- 25).Greenberger BA, Pulsifer MB, Ebb DH, et al. : Clinical outcomes and late endocrine, neurocognitive, and visual profiles of proton radiation for pediatric low-grade gliomas. Int J Radiat Oncol Biol Phys 89: 1060–1068, 2014 [DOI] [PubMed] [Google Scholar]
- 26).Hauswald H, Rieken S, Ecker S, et al. : First experiences in treatment of low-grade glioma grade I and II with proton therapy. Radiat Oncol 7: 189, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27).Grill J, Sainte-Rose C, Jouvet A, et al. French Society of Paediatric Oncology : Treatment of medulloblastoma with postoperative chemotherapy alone: an SFOP prospective trial in young children. Lancet Oncol 6: 573–580, 2005 [DOI] [PubMed] [Google Scholar]
- 28).Packer RJ, Gajjar A, Vezina G, et al. : Phase III study of craniospinal radiation therapy followed by adjuvant chemotherapy for newly diagnosed average-risk medulloblastoma. J Clin Oncol 24: 4202–4208, 2006 [DOI] [PubMed] [Google Scholar]
- 29).Merchant TE, Kun LE, Krasin MJ, et al. : Multi-institution prospective trial of reduced-dose craniospinal irradiation (23.4 Gy) followed by conformal posterior fossa (36 Gy) and primary site irradiation (55.8 Gy) and dose-intensive chemotherapy for average-risk medulloblastoma. Int J Radiat Oncol Biol Phys 70: 782–787, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30).Lannering B, Rutkowski S, Doz F, et al. : Hyperfractionated versus conventional radiotherapy followed by chemotherapy in standard-risk medulloblastoma: results from the randomized multicenter HIT-SIOP PNET 4 trial. J Clin Oncol 30: 3187–3193, 2012 [DOI] [PubMed] [Google Scholar]
- 31).Gordon J, Siebers J: Addressing a gap in current IMRT quality assurance. Int J Radiat Oncol Biol Phys 87: 20–21, 2013 [DOI] [PubMed] [Google Scholar]
- 32).Sethi RV, Giantsoudi D, Raiford M, et al. : Patterns of failure after proton therapy in medulloblastoma; linear energy transfer distributions and relative biological effectiveness associations for relapses. Int J Radiat Oncol Biol Phys 88: 655–663, 2014 [DOI] [PubMed] [Google Scholar]
- 33).Eaton BR, Esiashvili N, Kim S, et al. : Clinical outcomes among children with standard–risk medulloblastoma treated with proton and photon radiation therapy: a comparison of disease control and overall survival. Int J Radiat Oncol Biol Phys 94: 133–138, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34).Walter AW, Mulhern RK, Gajjar A, et al. : Survival and neurodevelopmental outcome of young children with medulloblastoma at St Jude Children’s Research Hospital. J Clin Oncol 17: 3720–3728, 1999 [DOI] [PubMed] [Google Scholar]
- 35).Ris MD, Packer R, Goldwein J, Jones-Wallace D, Boyett JM: Intellectual outcome after reduced-dose radiation therapy plus adjuvant chemotherapy for medulloblastoma: a Children’s Cancer Group study. J Clin Oncol 19: 3470–3476, 2001 [DOI] [PubMed] [Google Scholar]
- 36).Eaton BR, Esiashvili N, Kim S, et al. : Endocrine outcomes with proton and photon radiotherapy for standard risk medulloblastoma. Neuro Oncol 18: 881–887, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37).Yock TI, Yeap BY, Ebb DH, et al. : Long-term toxic effects of proton radiotherapy for paediatric medulloblastoma: a phase 2 single-arm study. Lancet Oncol 17: 287–298, 2016 [DOI] [PubMed] [Google Scholar]
- 38).Brodin NP, Munck af Rosenschöld P, Blomstrand M, et al. : Hippocampal sparing radiotherapy for pediatric medulloblastoma: impact of treatment margins and treatment technique. Neuro-oncology 16: 594–602, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39).Pulsifer MB, Sethi RV, Kuhlthau KA, MacDonald SM, Tarbell NJ, Yock TI: Early cognitive outcomes following proton radiation in pediatric patients with brain and central nervous system tumors. Int J Radiat Oncol Biol Phys 93: 400–407, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40).Moeller BJ, Chintagumpala M, Philip JJ, et al. : Low early ototoxicity rates for pediatric medulloblastoma patients treated with proton radiotherapy. Radiat Oncol 6: 58, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41).Giantsoudi D, Sethi RV, Yeap BY, et al. : Incidence of CNS injury for a cohort of 111 patients treated with proton therapy for medulloblastoma: LET and RBE associations for areas of injury. Int J Radiat Oncol Biol Phys 95: 287–296, 2016 [DOI] [PubMed] [Google Scholar]
- 42).Min CH, Paganetti H, Winey BA, et al. : Evaluation of permanent alopecia in pediatric medulloblastoma patients treated with proton radiation. Radiat Oncol 9: 220, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43).Cochran DM, Yock TI, Adams JA, Tarbell NJ: Radiation dose to the lens during craniospinal irradiation-an improvement in proton radiotherapy technique. Int J Radiat Oncol Biol Phys 70: 1336–1342, 2008 [DOI] [PubMed] [Google Scholar]
- 44).Zhang R, Howell RM, Taddei PJ, Giebeler A, Mahajan A, Newhauser WD: A comparative study on the risks of radiogenic second cancers and cardiac mortality in a set of pediatric medulloblastoma patients treated with photon or proton craniospinal irradiation. Radiother Oncol 113: 84–88, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45).Howell RM, Giebeler A, Koontz-Raisig W, et al. : Comparison of therapeutic dosimetric data from passively scattered proton and photon craniospinal irradiations for medulloblastoma. Radiat Oncol 7: 116, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46).St Clair WH, Adams JA, Bues M, et al. : Advantage of protons compared to conventional X-ray or IMRT in the treatment of a pediatric patient with medulloblastoma. Int J Radiat Oncol Biol Phys 58: 727–734, 2004 [DOI] [PubMed] [Google Scholar]
- 47).Yoon M, Shin DH, Kim J, et al. : Craniospinal irradiation techniques: a dosimetric comparison of proton beams with standard and advanced photon radiotherapy. Int J Radiat Oncol Biol Phys 81: 637–646, 2011 [DOI] [PubMed] [Google Scholar]
- 48).Zhang R, Howell RM, Giebeler A, Taddei PJ, Mahajan A, Newhauser WD: Comparison of risk of radiogenic second cancer following photon and proton craniospinal irradiation for a pediatric medulloblastoma patient. Phys Med Biol 58: 807–823, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49).Johnstone PA, McMullen KP, Buchsbaum JC, Douglas JG, Helft P: Pediatric CSI: are protons the only ethical approach? Int J Radiat Oncol Biol Phys 87: 228–230, 2013 [DOI] [PubMed] [Google Scholar]
- 50).Kool M, Korshunov A, Remke M, et al. : Molecular subgroups of medulloblastoma: an international meta–analysis of transcriptome, genetic aberrations, and clinical data of WNT, SHH, Group 3, and Group 4 medulloblastomas. Acta Neuropathol 123: 473–484, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51).Taylor MD, Northcott PA, Korshunov A, et al. : Molecular subgroups of medulloblastoma: the current consensus. Acta Neuropathol 123: 465–472, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52).Thompson MC, Fuller C, Hogg TL, et al. : Genomics identifies medulloblastoma subgroups that are enriched for specific genetic alterations. J Clin Oncol 24: 1924–1931, 2006 [DOI] [PubMed] [Google Scholar]
- 53).Northcott PA, Korshunov A, Witt H, et al. : Medulloblastoma comprises four distinct molecular variants. J Clin Oncol 29: 1408–1414, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54).Shih DJ, Northcott PA, Remke M, et al. : Cytogenetic prognostication within medulloblastoma subgroups. J Clin Oncol 32: 886–896, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55).Northcott PA, Shih DJ, Remke M, et al. : Rapid, reliable, and reproducible molecular sub-grouping of clinical medulloblastoma samples. Acta Neuropathol 123: 615–626, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56).Northcott PA, Shih DJ, Peacock J, et al. : Subgroup-specific structural variation across 1,000 medulloblastoma genomes. Nature 488: 49–56, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57).Lundkvist J, Ekman M, Ericsson SR, Jönsson B, Glimelius B: Cost-effectiveness of proton radiation in the treatment of childhood medulloblastoma. Cancer 103: 793–801, 2005 [DOI] [PubMed] [Google Scholar]
- 58).Massimino M, Gandola L, Giangaspero F, et al. AIEOP Pediatric Neuro-Oncology Group : Hyperfractionated radiotherapy and chemotherapy for childhood ependymoma: final results of the first prospective AIEOP (Associazione Italiana di Ematologia-Oncologia Pediatrica) study. Int J Radiat Oncol Biol Phys 58: 1336–1345, 2004 [DOI] [PubMed] [Google Scholar]
- 59).Merchant TE, Li C, Xiong X, Kun LE, Boop FA, Sanford RA: Conformal radiotherapy after surgery for paediatric ependymoma: a prospective study. Lancet Oncol 10: 258–266, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60).Timmermann B, Kortmann RD, Kühl J, et al. : Combined postoperative irradiation and chemotherapy for anaplastic ependymomas in childhood: results of the German prospective trials HIT 88/89 and HIT 91. Int J Radiat Oncol Biol Phys 46: 287–295, 2000 [DOI] [PubMed] [Google Scholar]
- 61).Ares C, Albertini F, Frei-Welte M, et al. : Pencil beam scanning proton therapy for pediatric intracranial ependymoma. J Neurooncol 128: 137–145, 2016 [DOI] [PubMed] [Google Scholar]
- 62).MacDonald SM, Safai S, Trofimov A, et al. : Proton radiotherapy for childhood ependymoma: initial clinical outcomes and dose comparisons. Int J Radiat Oncol Biol Phys 71: 979–986, 2008 [DOI] [PubMed] [Google Scholar]
- 63).Macdonald SM, Sethi R, Lavally B, et al. : Proton radiotherapy for pediatric central nervous system ependymoma: clinical outcomes for 70 patients. Neuro Oncol 15: 1552–1559, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64).Mizumoto M, Oshiro Y, Takizawa D, et al. : Proton beam therapy for pediatric ependymoma. Pediatr Int 57: 567–571, 2015 [DOI] [PubMed] [Google Scholar]
- 65).Bouffet E, Hawkins CE, Ballourah W, et al. : Survival benefit for pediatric patients with recurrent ependymoma treated with reirradiation. Int J Radiat Oncol Biol Phys 83: 1541–1548, 2012 [DOI] [PubMed] [Google Scholar]
- 66).Eaton BR, Chowdhry V, Weaver K, et al. : Use of proton therapy for re-irradiation in pediatric intracranial ependymoma. Radiother Oncol 116: 301–308, 2015 [DOI] [PubMed] [Google Scholar]
- 67).Gunther JR, Sato M, Chintagumpala M, et al. : Imaging changes in pediatric intracranial ependymoma patients treated with proton beam radiation therapy compared to intensity modulated radiation therapy. Int J Radiat Oncol Biol Phys 93: 54–63, 2015 [DOI] [PubMed] [Google Scholar]
- 68).Kim JW, Kim WC, Cho JH, et al. : A multimodal approach including craniospinal irradiation improves the treatment outcome of high–risk intracranial nongerminomatous germ cell tumors. Int J Radiat Oncol Biol Phys 84: 625–631, 2012 [DOI] [PubMed] [Google Scholar]
- 69).Matsutani M, Japanese Pediatric Brain Tumor Study Group : Combined chemotherapy and radiation therapy for CNS germ cell tumors–the Japanese experience. J Neurooncol 54: 311–316, 2001 [DOI] [PubMed] [Google Scholar]
- 70).Calaminus G, Kortmann R, Worch J, et al. : SIOP CNS GCT 96: final report of outcome of a prospective, multinational nonrandomized trial for children and adults with intracranial germinoma, comparing craniospinal irradiation alone with chemotherapy followed by focal primary site irradiation for patients with localized disease. Neuro-oncology 15: 788–796, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71).Alapetite C, Brisse H, Patte C, et al. : Pattern of relapse and outcome of non-metastatic germinoma patients treated with chemotherapy and limited field radiation: the SFOP experience. Neuro-oncology 12: 1318–1325, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72).Acharya S, DeWees T, Shinohara ET, Perkins SM: Long-term outcomes and late effects for childhood and young adulthood intracranial germinomas. Neuro-oncology 17: 741–746, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73).Sawamura Y, Ikeda J, Shirato H, Tada M, Abe H: Germ cell tumours of the central nervous system: treatment consideration based on 111 cases and their long-term clinical outcomes. Eur J Cancer 34: 104–110, 1998 [DOI] [PubMed] [Google Scholar]
- 74).Bamberg M, Kortmann RD, Calaminus G, et al. : Radiation therapy for intracranial germinoma: results of the German cooperative prospective trials MAKEI 83/86/89. J Clin Oncol 17: 2585–2592, 1999 [DOI] [PubMed] [Google Scholar]
- 75).Yang JC, Terezakis SA, Dunkel IJ, Gilheeney SW, Wolden SL: Intensity-Modulated Radiation Therapy With Dose Painting: A Brain-Sparing Technique for Intracranial Germ Cell Tumors. Pediatr Blood Cancer 63: 646–651, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76).Park J, Park Y, Lee SU, Kim T, Choi YK, Kim JY: Differential dosimetric benefit of proton beam therapy over intensity modulated radiotherapy for a variety of targets in patients with intracranial germ cell tumors. Radiat Oncol 10: 135, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77).MacDonald SM, Trofimov A, Safai S, et al. : Proton radiotherapy for pediatric central nervous system germ cell tumors: early clinical outcomes. Int J Radiat Oncol Biol Phys 79: 121–129, 2011 [DOI] [PubMed] [Google Scholar]
- 78).Minniti G, Saran F, Traish D, et al. : Fractionated stereotactic conformal radiotherapy following conservative surgery in the control of craniopharyngiomas. Radiother Oncol 82: 90–95, 2007 [DOI] [PubMed] [Google Scholar]
- 79).Merchant TE, Kiehna EN, Kun LE, et al. : Phase II trial of conformal radiation therapy for pediatric patients with craniopharyngioma and correlation of surgical factors and radiation dosimetry with change in cognitive function. J Neurosurg 104: 94–102, 2006 [DOI] [PubMed] [Google Scholar]
- 80).Klimo P, Venable GT, Boop FA, Merchant TE: Recurrent craniopharyngioma after conformal radiation in children and the burden of treatment. J Neurosurg Pediatr 15: 499–505, 2015 [DOI] [PubMed] [Google Scholar]
- 81).Luu QT, Loredo LN, Archambeau JO, Yonemoto LT, Slater JM, Slater JD: Fractionated proton radiation treatment for pediatric craniopharyngioma: preliminary report. Cancer J 12: 155–159, 2006 [PubMed] [Google Scholar]
- 82).Winkfield KM, Linsenmeier C, Yock TI, et al. : Surveillance of craniopharyngioma cyst growth in children treated with proton radiotherapy. Int J Radiat Oncol Biol Phys 73: 716–721, 2009 [DOI] [PubMed] [Google Scholar]
- 83).Bishop AJ, Greenfield B, Mahajan A, et al. : Proton beam therapy versus conformal photon radiation therapy for childhood craniopharyngioma: multi-institutional analysis of outcomes, cyst dynamics, and toxicity. Int J Radiat Oncol Biol Phys 90: 354–361, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84).Beltran C, Roca M, Merchant TE: On the benefits and risks of proton therapy in pediatric craniopharyngioma. Int J Radiat Oncol Biol Phys 82: e281–e287, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85).Boehling NS, Grosshans DR, Bluett JB, et al. : Dosimetric comparison of three-dimensional conformal proton radiotherapy, intensity-modulated proton therapy, and intensity-modulated radiotherapy for treatment of pediatric craniopharyngiomas. Int J Radiat Oncol Biol Phys 82: 643–652, 2012 [DOI] [PubMed] [Google Scholar]
- 86).Pearce MS, Salotti JA, Little MP, et al. : Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study. Lancet 380: 499–505, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87).Merchant TE, Kiehna EN, Li C, et al. : Modeling radiation dosimetry to predict cognitive outcomes in pediatric patients with CNS embryonal tumors including medulloblastoma. Int J Radiat Oncol Biol Phys 65: 210–221, 2006 [DOI] [PubMed] [Google Scholar]
- 88).Grill J, Renaux VK, Bulteau C, et al. : Long-term intellectual outcome in children with posterior fossa tumors according to radiation doses and volumes. Int J Radiat Oncol Biol Phys 45: 137–145, 1999 [DOI] [PubMed] [Google Scholar]
- 89).Dennis M, Spiegler BJ, Hetherington CR, Greenberg ML: Neuropsychological sequelae of the treatment of children with medulloblastoma. J Neurooncol 29: 91–101, 1996 [DOI] [PubMed] [Google Scholar]
- 90).Takizawa D, Oshiro Y, Mizumoto M, Fukushima H, Fukushima T, Sakurai H: Proton beam therapy for a patient with large rhabdomyosarcoma of the body trunk. Ital J Pediatr 41: 90, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91).Indelicato DJ, Flampouri S, Rotondo RL, et al. : Incidence and dosimetric parameters of pediatric brainstem toxicity following proton therapy. Acta Oncol 53: 1298–1304, 2014 [DOI] [PubMed] [Google Scholar]
- 92).Brodin NP, Munck Af Rosenschöld P, Aznar MC, et al. : Radiobiological risk estimates of adverse events and secondary cancer for proton and photon radiation therapy of pediatric medulloblastoma. Acta Oncol 50: 806–816, 2011 [DOI] [PubMed] [Google Scholar]
- 93).Kuhlthau KA, Pulsifer MB, Yeap BY, et al. : Prospective study of health–related quality of life for children with brain tumors treated with proton radiotherapy. J Clin Oncol 30: 2079–2086, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]


