Abstract
The purposes of this study were to review historical changes in the classification of spinal arteriovenous (AV) shunts and to propose a practical classification system. The associated literature regarding the classification of spinal AV shunts was reviewed in the angiography era between 1967 and 2015. The classification systems of spinal AV shunts and a proposed classification system were presented with neuroradiological imaging and medical illustrations. There have been seven major classification systems based on the evolution of diagnostic methods as well as treatments for spinal AV shunts: the first description of spinal AV shunts diagnosed and classified using spinal angiography in 1971; the second classification based on a case report of intradural direct perimedullary arteriovenous fistulas (AVFs) treated by microsurgery in 1987; the third classification based on a case series of intradural perimedullary AVFs treated by endovascular interventions in 1993; the fourth and fifth classification systems based on a case series of spinal AVFs and arteriovenous malformations (AVMs) treated by microsurgery or endovascular interventions in 2002; the sixth classification based on a case series of cranio-spinal dural AV shunts in 2009; and the seventh classification based on a case series of extradural AVFs treated by microsurgery and endovascular interventions in 2011. Based on historical reports, the author proposed a classification system according to the sites (dural, intradural, and extradural) and types (AVF and AVM) of AV shunts. By learning the historical background, we may obtain a clearer understanding of the complex and confusing classification system of spinal AV shunts.
Keywords: spinal vascular malformation, spinal arteriovenous malformation, spinal arteriovenous fistula, pial arteriovenous fistula, epidural arteriovenous fistula
Introduction
Spinal arteriovenous (AV) shunts are abnormal connections between arteries and veins of the spine with the passage of blood from arteries to veins without going through the capillary network. The precise diagnosis of spinal AV shunts is more difficult than that of cerebral arteriovenous malformations (AVM): the sizes of the lesions are very small; spinal angiography is technically challenging; and their angioarchitecture differs according to their site, type, and spinal level. Many classification systems have been reported and have changed over time in the literature. The purposes of this study were 1) to review historical changes in the classification of spinal AV shunts after the introduction of spinal angiography, 2) to present representative neuroradiological imaging of spinal AV shunts, and 3) to propose a practical and easy-to-follow classification system.
Materials and Methods
The PubMed database was searched for English literature regarding the classification of spinal AV shunts published after the introduction of spinal angiography (1967–2015). The classification systems of spinal AV shunts were tabulated in systematic order. The proposed classification system was described and representative angiographic and magnetic resonance images of spinal AV shunts were presented.
Results
The first description of a classification (1971)
In 1967, Di chiro G (a neuroradiologist at the National Institute of Health, USA) and colleagues reported selective angiography of spinal AV shunts for the first time.1) In 1971, Di chiro G described the first classification of spinal AV shunts based on angiographic findings2): single coiled vessel type I, glomus type II, and juvenile type III (Table 1). The majority of single coiled vessel type I corresponded to dural arteriovenous fistulas (AVFs), while the glomus type and juvenile type both corresponded to intradural AVMs. Although a photographic subtraction method was used in their angiographic procedure, the spatial resolution of the images was very low. Representative angiograms of dural AVF as well as intradural glomus and juvenile AVM are presented in Figs. 1 and 2.
Table 1.
Classification of spinal AV shunts reported by Di chiro (1971)
| Type | Academic name |
|---|---|
| I | Single coiled vessel type |
| II | Glomus type |
| III | Juvenile type |
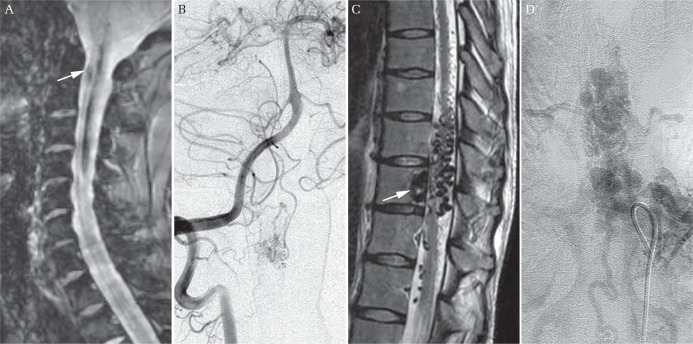
Fig. 1.

Dural arteriovenous fistula (AVF). (A) Sagittal thoracic image using T2-weighted MR imaging showing congestion of the spinal cord (asterisk). (B) An antero-posterior angiogram of the thoracic intercostal artery showing feeding meningeal arteries (white arrow), the fistula (white arrowhead), and draining vein (black arrow).
Fig. 2.
Intradural arteriovenous malformation (AVM). (A) A sagittal cervical image using gradient-echo MR imaging showing spinal intramedullary hemorrhage (white arrow). (B) An antero-posterior angiogram showing intramedullary glomus AVM. (C) A sagittal thoracic image using T2-weighted MR imaging showing intradural and vertebral flow voids (white arrow). (D) An antero-posterior angiogram of the thoracic intercostal artery showing intramedullary juvenile AVM.
In 1975, Yaşargil MG (a neurosurgeon at the University of Zürich, Switzerland) and colleagues reported a surgical case series of spinal AV shunts.3) This report included 11 cervical lesions. All patients were diagnosed using angiography of the vertebral artery; however, the spatial resolution of angiograms was very low. These lesions presumably corresponded to intradural glomus type, juvenile type, or perimedullary AVF. In Yaşsargil’s report, AV shunts were described as “extramedullary and intramedullary vascular malformations”.
In 1977, Kendall BE (a neuroradiologist at the National Hospital for Nervous Diseases, England) and Logue V (a neurosurgeon at the same hospital) reported a surgical case series of spinal AV shunts.4) This report included eight thoracolumbar lesions and one sacral lesion. All patients were diagnosed using selective angiography of spinal segmental arteries. The spatial resolution of the images was higher in Kendall’s report than in those by Di chiro G and Yaşsargil. The angiographic findings of eight thoracolumbar lesions corresponded to single coiled vessel type (dural AVFs), while the remaining sacral lesion corresponded to an intradural perimedullary AVF at the filum terminale. In Kendall’s report, the AV shunt was described as “a spinal epidural angiomatous malformation draining into intrathecal veins”.
In 1983, Cogen P (a neurosurgeon at the Columbia-Presbyterian Medical Center, USA) reported a surgical case series of spinal AV shunts.5) This report included one cervical and five thoracolumbar lesions. The angiographic and surgical findings of these lesions corresponded to glomus AVM.
In 1983, Oldfield EH (a neurosurgeon at the National Institute of Health, USA), Di chiro G, and colleagues reported a surgical case series of spinal AV shunts.6) This report included six thoracolumbar lesions. The angiographic findings of this series corresponded to single coiled vessel type (dural AVFs). Occlusion of the proximal intradural arterialized vein was performed on five patients, whereas stripping of the intradural vein over multiple spinal segments was performed on the remaining patient. They concluded that occlusion of the proximal vein was sufficient, with more extensive removal of the vein being unnecessary.
In 1984, Symon L (a neurosurgeon at the National Hospital for Nervous Diseases, England), Kendall BE, and colleagues reported a large case series of 55 patients with dural AVF.7) Occlusion of the proximal intradural arterialized vein was performed on 50 patients, whereas decompressive laminectomy only was performed on the other five cases. Occlusion of the vein led to neurological improvements in 85% of 50 patients.
The second classification (1987)
In 1986, Hero RC (a neurosurgeon at Massachusetts General Hospital, USA) and colleagues reported a new type of spinal AV shunt that did not fit any type.8) They described a patient with a direct AV connection between the anterior spinal artery and vein that was located ventral to the spinal cord. Since this patient initially underwent spinal angiography in Belgium and was transferred to USA, Lasjaunias P (a French neuroradiologist) was listed as a co-author. Angiography revealed that the anterior spinal artery from the vertebral artery descended caudally and connected directly to the anterior spinal vein at the T3 level. The vein ascended cephalad and flowed into the vein in the posterior cranial fossa. This patient underwent direct surgery via anterior half corpectomy of the thoracic spine. The AVF was obliterated by dividing the two arterial feeders, the ascending and descending branches of the anterior spinal artery, both of which entered the vein through the fistula. On the 4th postoperative day, paraparesis deteriorated and spinal angiography revealed no filling of the ascending branch of the anterior spinal artery. In this case report, the AV shunt was described as a direct spinal AVF, Type IV.
The report by Hero was not the first case report of a direct spinal AVF. In 1977, Djindjian R (a neuroradiologist at the Lariboisière Hospital, France) and colleagues reported a series of intradural AV shunts fed by the anterior spinal artery.9) This report included six lumbosacral lesions. The angiographic findings of this case series did not fit any type of Di chiro G’s first generation classification, but corresponded to direct spinal AVF reported by Hero RC.
In 1987, Rosenblum B, Oldfield EH (neurosurgeons at the National Institute of Health, USA), Doppman JL, and Di chiro G (neuroradiologists at the same institution) reported a large case series of 81 patients with spinal AV shunts.10) In this report, spinal AV shunts were classified into four types: type I as dural AVF; type II as intradural intramedullary glomus AVM; type III as intradural intramedullary juvenile AVM; and type IV as direct AVF (Table 2). Medical illustrations were used to give a representation of these types. They compared dural AVFs and intradural AVMs in terms of clinical epidemiology, radiological imaging, and treatment outcomes.
Table 2.
Classification of spinal AV shunts reported by Rosenblum (1987)
| Type | Academic name |
|---|---|
| I | Dural AVF |
| II | Intramedullary glomus AVM |
| III | Intramedullary juvenile AVM |
| IV | Intradural direct AVF |
The third classification (1993)
In 1993, Mourier KL and Merland JJ (neuroradiologists at the Lariboisière Hospital, France), and colleagues reported a series of intradural direct AVFs.11) In this report, AV shunts were described as perimedullary AVFs; thus, intradural direct AVFs were referred to as perimedullary AVFs thereafter in the literature. This study included 35 patients, 25 of whom underwent endovascular embolization. Perimedullary AVFs were classified according to the number of feeding arteries and size of AVF into the following three subtypes: Type I with a single feeder and single small AVF, Type II with multiple feeders and multiple medium AVFs, and Type III with multiple feeders and a single giant AVF (Table 3). In this report, 22 patients corresponded to type III perimedullary AVF, which is more amenable to endovascular treatment than microsurgery because of large feeders and AVFs. In contrast, type I perimedullary AVFs are amenable to microsurgery because the feeders are long and small in diameter. Anson and Spetzler proposed classifying perimedullary AVFs as Subtypes IVa, IVb, and IVc in order to avoid confusion.12) Representative angiograms of perimedullary AVFs, subtypes I-III are presented in Figs. 3–5.
Table 3.
Classification of spinal AV shunts reported by Mourier (1993)
| Academic name | Subtype | Feeder, AVF, and venous drainage |
|---|---|---|
| Perimedullary AVF | I | A single feeder and small AVF |
| II | Multiple feeders and medium AVFs | |
| III | Multiple feeders and a giant AVF |
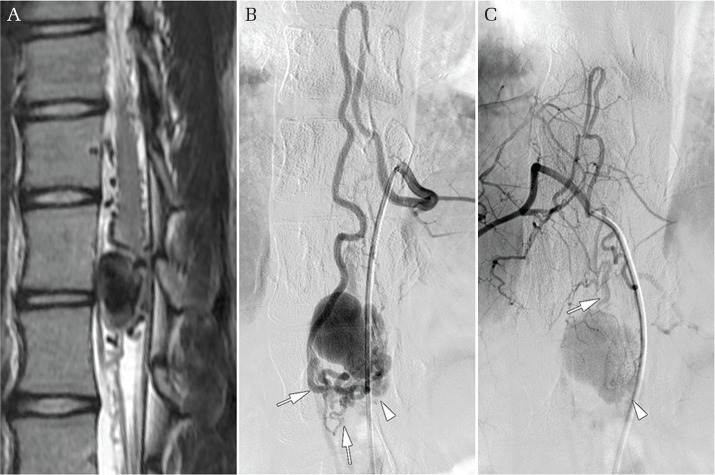
Fig. 3.
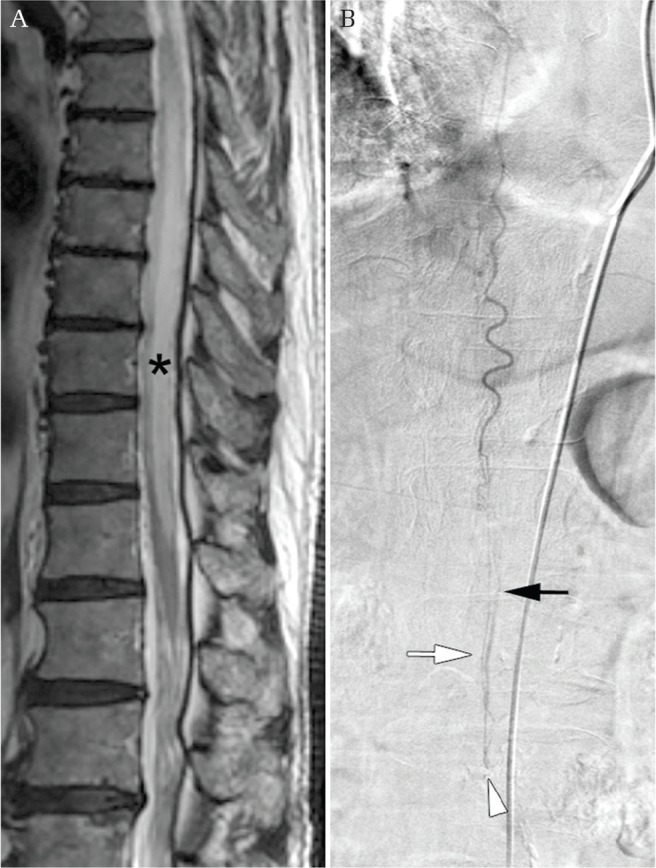
Intradural perimedullary AVF subtype I (a single feeder, a single small AVF). (A) A sagittal thoracic image using T2-weighted MR imaging showing congestion of the spinal cord (asterisk). (B) An angiogram of the thoracic intercostal artery showing intradural perimedullary AVF subtype I (arrowhead) fed by the filum artery (white arrow), and draining vein (black arrow).
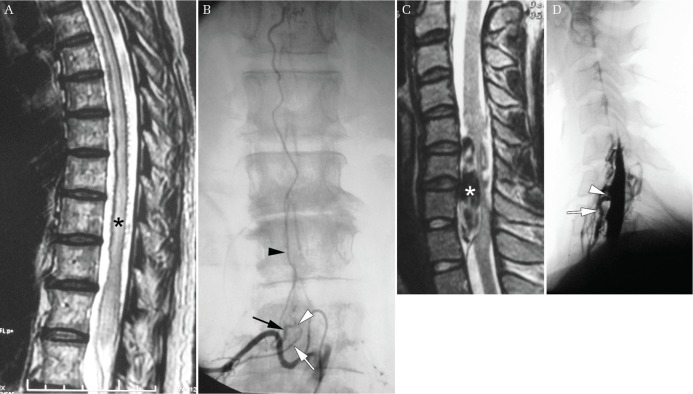
Fig. 5.
Intradural perimedullary AVF subtype III (multiple feeders, single giant AVF). (A) A sagittal thoracic image using T2-weighted MR imaging showing compression of the spinal cord by an enlarged venous varix. (B) An angiogram of the thoracic intercostal artery showing intradural perimedullary AVF subtype III (arrowhead) fed by pial branches of the anterior and posterior spinal artery (arrows). (C) An angiogram of the thoracic intercostal artery showing the same intradural perimedullary AVF (arrowhead) fed by pial branches of the posterior spinal artery (arrow).
In 1994, Barrow DL (a neurosurgeon at the Emory University School of Medicine, USA) and colleagues reported a series of intradural perimedullary AVFs treated by microsurgery.13) This report included seven patients with thoracolumbar lesions who underwent direct surgery via a posterior approach. In order to expose the ventrally positioned fistula, far lateral laminectomy with gentle rotation of the spinal cord was performed. These seven lesions corresponded to perimedullary AVF subtypes I and II.
In 2002, Hida K (a neurosurgeon at the University of Hokkaido, Japan) and colleagues reported a series of intradural perimedullary AVFs treated by microsurgery.14) This report included five patients with cervical lesions who underwent direct surgery via an anterior approach. In order to expose the ventrally positioned fistula, cervical corpectomy was performed. These five lesions corresponded to perimedullary AVF subtype I.
The Fourth and fifth classifications (2002)
In 2002, Spetzler RF (a neurosurgeon at the Barrow Neurological Institute, USA) reported a modified classification of spinal vascular malformations that changed the conventional concept of lesions (Table 4).15) He classified spinal vascular malformations including cavernous malformations and spinal AV shunts on the basis of his surgical experience of more than 130 lesions (89 spinal AV shunts). From the standpoint of a neurosurgeon, he classified spinal AV shunts based on anatomical locations between the lesion and spinal cord. Since spinal dural AVFs commonly develop at the dorsolateral portion of the dura mater, dural AVFs were defined as dorsal AVFs. In contrast, because perimedullary AVFs commonly develop at the ventral portion of the spinal cord, perimedullary AVFs were defined as ventral AVFs. Intramedullary glomus AVMs were defined as compact AVMs, and intramedullary juvenile AVMs as extradural-intradural AVMs. In addition, three new types were described: extradural AVFs, diffuse type AVMs, and conus AVMs. Extradural AVFs in the Spetzler classification were cervical lesions that were fed by the extradural branch of the vertebral artery and drained into the extradural venous plexus. In this lesion, although the spinal cord was severely compressed by the enlarged venous plexus, there was no venous congestion because there was no intradural venous drainage. Diffuse AVMs were intramedullary AVMs with subpial extensions over multiple spinal segments. Conus AVMs were complex intramedullary AVMs that developed at the conus medullaris with multiple feeders and AV shunts. Surgical procedures for these lesions differed.
Table 4.
Classification of spinal AV shunts reported by Spetzler (2002)
| Types of AV shunts | Academic name |
|---|---|
| AVF | Extradural AVF |
| Intradural ventral AVF | |
| Intradural dorsal AVF | |
| AVM | Extradural-intradural AVM |
| Intradural compact AVM | |
| Intradural diffuse AVM | |
| Intradural conus AVM |
This report resulted in controversy. Barrow DL (a neurosurgeon at Emory University, USA) criticized the modified classification via a long letter to the Editor (1500 words)16): he anticipated the likelihood of interobserver variations among intramedullary AVMs between the compact and diffuse types. He also pointed out that complex AVMs are not always located at the conus medullaris; they may develop at different spinal levels. Lasjaunias P (a neuroradiologist at the Lariboisière Hospital, France) criticized the modified classification via a longer letter to the Editor (2000 words)17): his criticism was too acerbic, but worth reading.
In 2002, the same year in which Spetzler reported the modified classification, Rodesh G and Lasjaunias P (neuroradiologists at the Lariboisière Hospital, France) reported a new classification system from the standpoint of an endovascular interventionalist.18) According to their type and size, spinal AV shunts were divided into AVMs and AVFs, with the latter being subdivided into macro and micro AVFs (Table 5). All spinal AV shunts corresponded to three categories: genetic hereditary lesions, genetic non-hereditary lesions, and single lesions.
Table 5.
Classification of spinal AV shunts reported by Rodesh (2002)
| Types of AV shunts | Academic name |
|---|---|
| AVM | |
| AVF | Micro AVF |
| Macro AVF | |
| Genetic classification | Genetic hereditary lesions |
| Genetic non-hereditary lesions | |
| Single lesions |
Neither Spetzler’s nor Rodesh’s classification has been universally accepted because both classifications are biased toward either microsurgery or endovascular treatment.
The sixth and seventh classifications (2011)
In 2008, Geibprasert S, Lasjaunias P (a neuroradiologist at the Lariboisière Hospital, France), and colleagues reported a new classification system for cranio-spinal AV shunts in which AV shunts were divided into ventral, lateral, and dorsal epidural groups (Table 6).19) In this classification, which included intracranial and spinal AVFs, extradural AVFs corresponded to the ventral epidural group. In this report, the ventral epidural group was not associated with intradural venous drainage. These angiographic characteristics do not fit subsequent reports, as described below.20–24)
Table 6.
Classification of cranio-spinal dural AV shunts reported by Geibprasert (2008)
| Types of AV shunts | Academic name |
|---|---|
| Ventral epidural group | Ventral epidural shunts |
| Dorsal epidural group | Dorsal epidural shunts |
| Lateral epidural group | Lateral epidural shunts |
In 2009, Clarke MJ (a neurosurgeon at the Mayo Clinic, USA) reported a surgical case series of extradural AVFs.20) This report included six lumbosacral lesions that presented with venous congestion of the spinal cord because of the presence of intradural venous drainage. These six AVFs differed from Spetzler’s extradural AVFs, which did not have intradural venous drainage.
In 2011, Rangel-Castilla L (a neurosurgeon at the Methodist Hospital, USA), Diaz OM (a neuroradiologist at the same hospital), and colleagues reported an endovascular case series of extradural AVFs.21) This report included 8 lesions in 7 patients: 1 cervical, 1 thoracic, and 6 lumbar lesions. In this report, four lesions were associated with congestive myelopathy, three were compressive radiculopathy, and the remaining 1 was asymptomatic. Extradural AVFs were subdivided into three types: types A, B1, and B2 with or without intradural venous drainage and with or without neurological deficits (Table 7).
Table 7.
Classification of spinal extradural AVFs reported by Rangel-Castilla (2011)
| Types of AV shunts | Subtype | Venous drainage, neurological deficit |
|---|---|---|
| Extradural AVF | A | w intradural venous drainage |
| B1 | w/o intradural venous drainage, w neurological deficits | |
| B2 | w/o intradural venous drainage, w/o neurological deficits |
In 2012, the author conducted a systematic review on extradural AVFs in order to clarify the clinical and neuroradiological characteristics of these lesions.22) Forty-five cases were found in the PubMed database between 1990 and 2011. Type A spinal extradural AVFs were diagnosed in patients in their 6th decade of life and exhibited diffuse high signal intensity in the spinal cord on T2-weighted magnetic resonance (MR) images with no mass effect. They also commonly occurred in the thoracolumbar and lumbar regions. In contrast, type B lesions exhibited a severe mass effect due to an enlarged extradural venous plexus, and commonly occurred in the cervical and upper thoracic regions.
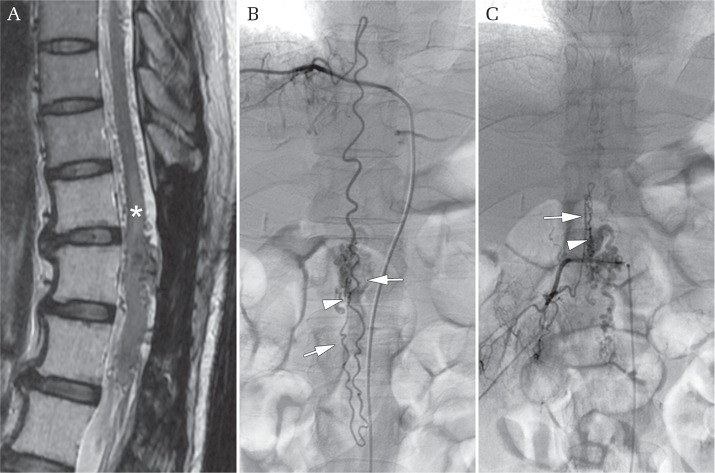
Representative cases of extradural AVFs, subtypes A and B, are shown in Fig. 6.
Fig. 6.
Extradural AVF. (A) A sagittal image using T2-weighted MR imaging showing congestion of the spinal cord (asterisk). (B)An antero-posterior angiogram of the lumbar artery showing the feeding pial arteries (white arrow), fistula (white arrowhead), venous pouch (black arrow), and draining vein (black arrowhead). (C) A sagittal image using T2-weighted MR imaging showing compression of the spinal cord by the extradural venous plexus (asterisk). (D) A lateral angiogram of the ascending cervical artery showing the feeding branch of the ascending cervical artery (white arrow) and fistula (white arrowhead).
In 2013, Niizuma K, Endo T (a neurosurgeon at Tohoku University, Japan), and colleagues reported a surgical case series of 5 type A extradural AVFs.23) In the same year, Kiyosue H (a neuroradiologist at Oita University, Japan) reported an endovascular case series of 5 type A extradural AVFs referred to as ventral epidural AVFs.24)
Discussion
Historical changes in the classification of spinal AV shunts in the angiography era were reviewed herein. There were seven major classification systems based on historical reports (Tables 1–7): the first description of spinal AV shunts diagnosed and classified using spinal angiography in 1971; the second classification system based on a case report of intradural direct perimedullary AVFs treated by microsurgery in 1987; the third classification system based on a case series of intradural perimedullary AVFs treated by endovascular interventions in 1993; the fourth and fifth classification systems based on a case series of spinal AVFs and AVMs treated by microsurgery or endovascular interventions in 2002; the sixth classification based on a case series of cranio-spinal dural AV shunts in 2009; and the seventh classification based on a case series of extradural AVFs treated by microsurgery and endovascular interventions in 2011. By learning the historical background, we may obtain a clearer understanding of the complex and confusing classification system of spinal AV shunts.
As shown in Table 8, the author proposes a practical and easy-to-follow classification system based on the historical background. Spinal AV shunts were classified into five types: type I as dural AVF; type II as intradural intramedullary glomus AVM; type III as intradural intramedullary juvenile AVM; type IV as perimedullary AVF; and type V as extradural AVF. Perimedullary AVFs were subdivided into Subtypes IVa, IVb, and IVc and extradural AVFs were subdivided into Subtypes Va and Vb (Fig. 7).
Table 8.
Proposed classification of spinal AV shunts by the author (2016)
| Type | Academic name | Subtype | Feeder, AVF, and venous drainage |
|---|---|---|---|
| I | Dural AVF | ||
| II | Intramedullary glomus AVM | ||
| III | Intramedullary juvenile AVM | ||
| IV | Perimedullary AVF | IVa | A single feeder and small AVF |
| IVb | Multiple feeders and medium AVFs | ||
| IVc | Multiple feeders and a giant AVF | ||
| V | Extradural AVF | Va | w intradural venous drainage |
| Vb | w/o intradural venous drainage |
Fig. 7.
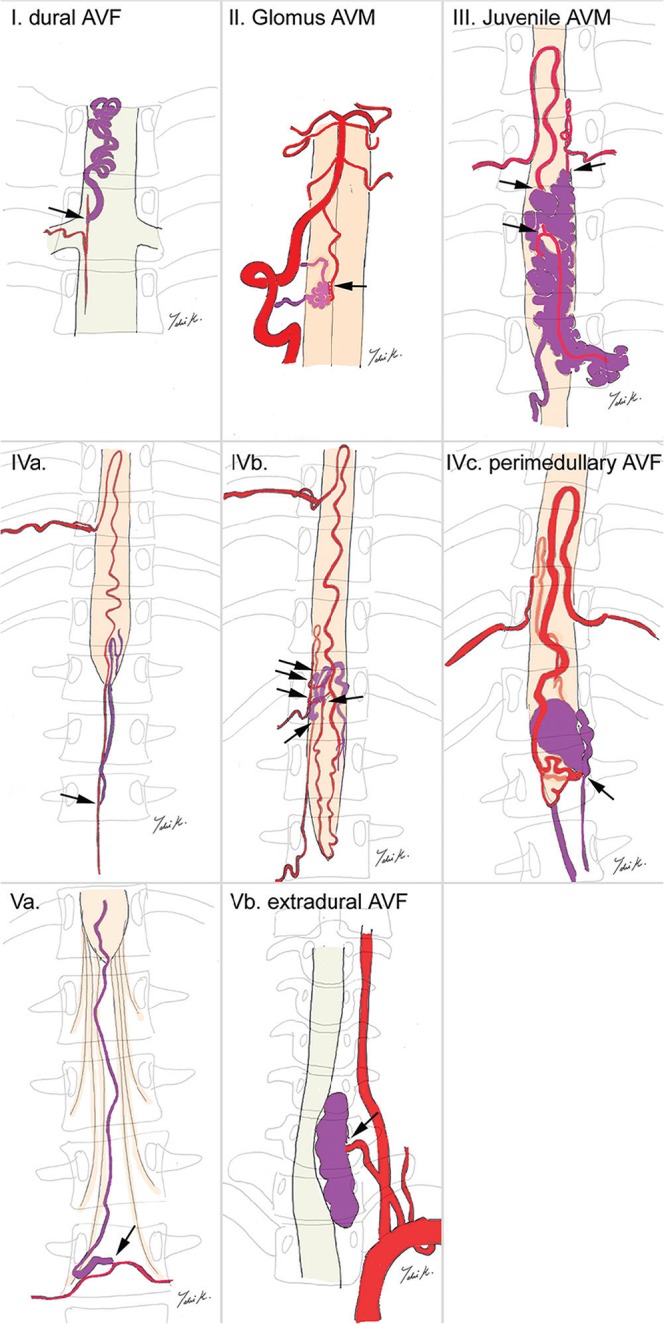
Illustration showing the different types of spinal arteriovenous shunts (Type I–V). Arrows indicates the arteriovenous connection(s).
The main advantage of the proposed classification system is that it is based on the classic second classification system with the type numbers I–IV, which have been the most widely used in the literature (Table 2). Extradural AVFs were added as a new type, which resulted in a type I–V classification system. Since the type numbers in the classification are consistent with those reported previously, treatment results may be easily compared among historical and current reports. In this classification system, perimedullary AVFs and extradural AVFs are subdivided into subtypes according to the feeding artery, the sizes of AV shunts, and drainage system. The advantage of this subclassification is that treatment approaches may be indicated based on the subtypes. Type IVa perimedullary AVFs are more amenable to microsurgery, and type IVc perimedullary AVFs to endovascular embolization. Type Va extradural AVFs may be treated by microsurgery and endovascular embolization, whereas type Vb extradural AVFs are more amenable to endovascular embolization. The proposed classification system is suitable for planning treatment strategies using microsurgical and/or endovascular interventions because it is based on the microvascular anatomy and hemodynamics of AV shunts.
However, this classification system also has disadvantages. We need to consider that spinal AV shunts differ not only according to the site and type of the AV shunt, but also to the spinal level at which the AV shunt develops. For example, the angioarchitecture of dural AVFs in the thoracic region differs from that in conus/lumbar lesions.25) The proposed classification system does not include anatomical differences at each spinal level. Furthermore, there may be another type of spinal AV shunt that does not fit any type of this classification. For example, the angioarchitecture of spinal AV shunts in the cervical region is complex.26) Further studies on the complex angioarchitecture of this rare disease are needed in more cases by analyzing neuroradiological imaging with high spatial and temporal resolution as well as surgical findings.
Conclusion
There were seven major classification systems based on historical reports, based on which the author proposed the current classification system according to the sites (dural, intradural, and extradural) and types (AVF and AVM) of AV shunts. By learning the historical background, we may obtain a clearer understanding of the complex and confusing classification system of spinal AV shunts.
Fig. 4.
Intradural perimedullary AVF subtype II (multiple feeders, multiple medium AVFs). (A) A sagittal thoracic image using T2-weighted MR imaging showing congestion of the spinal cord (asterisk). (B) An angiogram of the thoracic intercostal artery showing intradural perimedullary AVF subtype II (arrowhead) fed by pial branches of the anterior and posterior spinal arteries (arrows). (C) An angiogram of the lumbar artery showing the same intradural perimedullary AVF (arrowhead) fed by pial branches of the posterior spinal arteries (arrow).
Footnotes
Conflicts of Interest Disclosure
The author declares that there are no conflicts of interest.
References
- 1).Di Chiro G, Doppman JL, Ommaya AK: Selective arteriography of arteriovenous aneurysms of spinal cord. Radiology 88: 1065–1077, 1967 [DOI] [PubMed] [Google Scholar]
- 2).Di Chiro G, Doppman JL, Ommaya AK: Radiology of Spinal Cord Arteriovenous Malformations. Prog Neurol Surg 4: 329–354, 1971 [Google Scholar]
- 3).Yaşargil MG, DeLong WB, Guarnaschelli JJ: Complete microsurgical excision of cervical extramedullary and intramedullary vascular malformations. Surg Neurol 4: 211–224, 1975 [PubMed] [Google Scholar]
- 4).Kendall BE, Logue V: Spinal epidural angiomatous malformations draining into intrathecal veins. Neuroradiology 13: 181–189, 1977 [DOI] [PubMed] [Google Scholar]
- 5).Cogen P, Stein BM: Spinal cord arteriovenous malformations with significant intramedullary components. J Neurosurg 59: 471–478, 1983 [DOI] [PubMed] [Google Scholar]
- 6).Oldfield EH, Di Chiro G, Quindlen EA, Rieth KG, Doppman JL: Successful treatment of a group of spinal cord arteriovenous malformations by interruption of dural fistula. J Neurosurg 59: 1019–1030, 1983 [DOI] [PubMed] [Google Scholar]
- 7).Symon L, Kuyama H, Kendall B: Dural arteriovenous malformations of the spine. Clinical features and surgical results in 55 cases. J Neurosurg 60: 238–247, 1984 [DOI] [PubMed] [Google Scholar]
- 8).Heros RC, Debrun GM, Ojemann RG, Lasjaunias PL, Naessens PJ: Direct spinal arteriovenous fistula: a new type of spinal AVM. Case report. J Neurosurg 64: 134–139, 1986 [DOI] [PubMed] [Google Scholar]
- 9).Djindjian M, Djindjian R, Rey A, Hurth M, Houdart R: Intradural extramedullary spinal arterio-venous malformations fed by the anterior spinal artery. Surg Neurol 8: 85–93, 1977 [PubMed] [Google Scholar]
- 10).Rosenblum B, Oldfield EH, Doppman JL, Di Chiro G: Spinal arteriovenous malformations: a comparison of dural arteriovenous fistulas and intradural AVM’s in 81 patients. J Neurosurg 67: 795–802, 1987 [DOI] [PubMed] [Google Scholar]
- 11).Mourier KL, Gobin YP, George B, Lot G, Merland JJ: Intradural perimedullary arteriovenous fistulae: results of surgical and endovascular treatment in a series of 35 cases. Neurosurgery 32: 885–891, 1993 [DOI] [PubMed] [Google Scholar]
- 12).Anson JA, Spetzler RF: Classification of spinal arteriovenous malformations and implications for treatment. Barrow Neurol Inst Q 8: 2–8, 1992 [Google Scholar]
- 13).Barrow DL, Colohan AR, Dawson R: Intradural perimedullary arteriovenous fistulas (type IV spinal cord arteriovenous malformations). J Neurosurg 81: 221–229, 1994 [DOI] [PubMed] [Google Scholar]
- 14).Hida K, Iwasaki Y, Ushikoshi S, Fujimoto S, Seki T, Miyasaka K: Corpectomy: a direct approach to perimedullary arteriovenous fistulas of the anterior cervical spinal cord. J Neurosurg 96: 157–161, 2002 [DOI] [PubMed] [Google Scholar]
- 15).Spetzler RF, Detwiler PW, Riina HA, Porter RW: Modified classification of spinal cord vascular lesions. J Neurosurg 96(Suppl 2): 145–156, 2002 [DOI] [PubMed] [Google Scholar]
- 16).Barrow DL: Spinal cord vascular lesions. J Neurosurg 96(Suppl 2): 143–144, 2002 [DOI] [PubMed] [Google Scholar]
- 17).Lasjaunias P: Spinal cord vascular lesions. J Neurosurg 98(Suppl 1): 117–119, 2003 [DOI] [PubMed] [Google Scholar]
- 18).Rodesch G, Hurth M, Alvarez H, Tadié M, Lasjaunias P: Classification of spinal cord arteriovenous shunts: proposal for a reappraisal–the Bicêtre experience with 155 consecutive patients treated between 1981 and 1999. Neurosurgery 51: 379–380, 2002 [PubMed] [Google Scholar]
- 19).Geibprasert S, Pereira V, Krings T, Jiarakongmun P, Toulgoat F, Pongpech S, Lasjaunias P: Dural arteriovenous shunts: a new classification of craniospinal epidural venous anatomical bases and clinical correlations. Stroke 39: 2783–2794, 2008 [DOI] [PubMed] [Google Scholar]
- 20).Clarke MJ, Patrick TA, White JB, Cloft HJ, Krauss WE, Lindell EP, Piepgras DG: Spinal extradural arteriovenous malformations with parenchymal drainage: venous drainage variability and implications in clinical manifestations. Neurosurg Focus 26: E5, 2009 [DOI] [PubMed] [Google Scholar]
- 21).Rangel-Castilla L, Holman PJ, Krishna C, Trask TW, Klucznik RP, Diaz OM: Spinal extradural arteriovenous fistulas: a clinical and radiological description of different types and their novel treatment with Onyx. J Neurosurg Spine 15: 541–549, 2011 [DOI] [PubMed] [Google Scholar]
- 22).Takai K, Taniguchi M: Comparative analysis of spinal extradural arteriovenous fistulas with or without intradural venous drainage: a systematic literature review. Neurosurg Focus 32: E8, 2012 [DOI] [PubMed] [Google Scholar]
- 23).Niizuma K, Endo T, Sato K, Takada S, Sugawara T, Mikawa S, Tominaga T: Surgical treatment of spinal extradural arteriovenous fistula with parenchymal drainage: report on 5 cases. Neurosurgery 73: E287–E294, 2013 [DOI] [PubMed] [Google Scholar]
- 24).Kiyosue H, Tanoue S, Okahara M, Hori Y, Kashiwagi J, Mori H: Spinal ventral epidural arteriovenous fistulas of the lumbar spine: angioarchitecture and endovascular treatment. Neuroradiology 55: 327–336, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25).Takai K, Kin T, Oyama H, Shojima M, Saito N: Three-dimensional angioarchitecture of spinal dural arteriovenous fistulas, with special reference to the intradural retrograde venous drainage system. J Neurosurg Spine 18: 398–408, 2013 [DOI] [PubMed] [Google Scholar]
- 26).Kim DJ, Willinsky R, Geibprasert S, Krings T, Wallace C, Gentili F, Terbrugge K: Angiographic characteristics and treatment of cervical spinal dural arteriovenous shunts. AJNR Am J Neuroradiol 31: 1512–1515, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]