Abstract
Background
We determined the proportions of patients with chronic hepatitis C (CHC) in association with possible prioritized indications for interferon-free regimens and the use of co-medications with potential drug-drug interactions (DDIs).
Methods
Five hundred consecutive mono-infected CHC patients seen in 2015 at 5 Greek centers were included. Priorities for interferon-free regimens were based on liver disease severity, contraindication(s) for interferon and prior interferon-treatment failure. All co-medications were classified into those with no DDIs/no clear data for DDIs, potential DDIs, and contraindication due to DDI for each agent, according to the HEP Drug Interaction Checker.
Results
Of the 500 patients, 1% had undergone liver transplantation, whereas 6.6% had decompensated cirrhosis, 21.8% F4, 17.1% F3, 10.4% F2, and 34.8% F0-1 fibrosis. Contraindications for interferon were present in 38.5% of non-transplant patients with compensated liver disease. The probability of contraindications/potential DDIs was greater for boceprevir/telaprevir and ombitasvir/paritaprevir/ritonavir±dasabuvir, compared to all other agents (P<0.001), and least for sofosbuvir (P<0.05). Contraindications/potential DDIs were more frequently present in patients ≥50 than <50 years old (P≤0.034), and more common in F3-4 than F0-2, and F4 than F0-3 fibrosis (P≤0.019) for all direct-acting antivirals (DAAs).
Conclusions
The expansion of the criteria for prioritization of interferon-free regimens from cirrhosis to F3 and perhaps F2 fibrosis will increase the proportion of patients with DAA access by only 10-15% and 10%, respectively. A potential for DDIs is frequently present with protease inhibitors, but also exists with other DAAs. The probability of DDIs is higher in patients with priority for DAAs, including those who have advanced liver disease and are usually of older age.
Keywords: Keywords Antiviral, hepatitis C, interaction, priority
Introduction
The advent of direct-acting antivirals (DAAs) in the market has heralded a new era in the field of hepatitis C virus (HCV) treatment, offering excellent rates of sustained virological response (SVR) that nearly equate to a universal cure [1,2]. Current DAAs belong to three different classes — NS3/4A protease inhibitors, NS5B polymerase inhibitors, and NS5A inhibitors — and target distinct steps in the HCV replication cycle [1,2]. Compared to pegylated-interferon (PEG-IFN) and ribavirin (RBV), given for up to 48 weeks, which were the standard of care for all genotypes of HCV during the last two decades [3], DAAs have been proven to be not only more efficacious but also markedly safer [1,2,4]. Thus, IFN-free DAA-containing regimens represent the scientifically recommended treatment options [4].
Despite current recommendations for the use of IFN-free regimens in all chronic HCV patients (4), the current high cost of DAAs and the limited availability of resources in many countries necessitate the prioritization of IFN-free treatment in patients with advanced liver disease and/or severe extrahepatic HCV complications [5,6]. On the other hand, HCV patients, who were once excluded from IFN-based regimens because of their serious comorbidities, are now candidates for IFN-free regimens [2,5,6]. Hence, IFN contraindications may be also taken into consideration in the development of prioritization strategies.
Besides cost, one of the few limitations of the current DAAs is the risk of drug-drug interactions (DDIs) with concomitant medications [4]. DAAs are shown to act as substrates, inhibitors and/or inducers of enzymes and transporters in the liver metabolism that affect the pharmacokinetics and pharmacodynamics of the coadministered drugs, and vice versa [7,8]. Hence, routinely prescribed non-HCV medications with DDI potential for DAAs may influence the choice of DAA-containing regimen and necessitate particular caution in patient management [7,8]. In Greece, a country severely affected by an economic crisis, the prevalence of HCV infection is considered moderate according to recent studies (approximately 1.5%) [9], but there are no epidemiological data to show the patient proportions who may have priority for IFN-free treatment. To date, for economic reasons, our national insurance organization restricts the administration of IFN-free regimens to patients with HCV recurrence after liver transplantation, decompensated or compensated cirrhosis, and prior failures after (PEG-)IFN-based regimens with advanced liver fibrosis (F3). Knowledge of the profile of patients with chronic hepatitis C (CHC) in Greece would add important insight to our understanding of the prioritization needed for IFN-free regimens, as well as the possible limitations of DAA use due to potential DDIs with co-medications.
The objective of this cross-sectional study was to investigate the proportions of CHC patients in Greece in relation to: a) possible prioritized indications for IFN-free regimens, and b) the use of co-medications with DDI potential.
Patients and methods
Study population
We retrospectively evaluated the records of 500 consecutive patients with CHC infection who sought care from the outpatient liver clinics of five tertiary Greek centers. In particular, we included the first 100 patients visiting each center within 2015 who had a complete evaluation, including determination of serum HCV RNA levels. The diagnosis of CHC infection was based on positive anti-HCV for at least 6 months and detectable serum HCV RNA. All patients had to be naïve to the current DAAs at study evaluation, while patients who were co-infected with human immunodeficiency virus (HIV) were excluded from this study. The study was approved by the hospitals’ Ethics Review Board and conforms to the principles outlined in the Declaration of Helsinki.
Patient characteristics
Demographic and epidemiological characteristics, medical history, clinical and laboratory data, and treatment history were retrieved from the patients’ medical records. In particular, the parameters recorded were: age, sex, weight and height, race, year of HCV diagnosis, alcohol abuse (>30 g and >20 g daily for males and females, respectively), history of liver biopsy, Metavir score (F0-F4) and/or liver stiffness from elastography, Child-Pugh score for patients with decompensated cirrhosis, development of hepatocellular carcinoma (HCC), history of liver transplantation, prior treatment for HCV and drug allergy for anti-HCV drugs. Comorbidities were also recorded, as were all medications taken by the patients. Finally, hemoglobin, white cell blood count, platelet counts, liver function tests, blood urea, creatinine, HCV genotype and serum HCV RNA levels were recorded and included in the analysis. Creatinine clearance was calculated based on the Cockcroft-Gault equation.
The severity of liver disease was classified into the following subgroups: F0-F1 fibrosis, F2 fibrosis, F3 fibrosis, F4 fibrosis, decompensated cirrhosis, liver transplantation. The diagnosis of decompensated cirrhosis was based on the presence or history of at least one of the four major clinical signs: ascites, variceal bleeding, hepatic encephalopathy, jaundice of non-obstructive cause. The diagnosis of F0-F4 fibrosis was based on histological findings, or mainly on liver elastographic findings. In particular, patients with reliable liver stiffness measurements of <7.0, 7.0-9.0, 9.1-12.5, >12.5 kPa were considered to have F0-F1, F2, F3, and F4 fibrosis, respectively, according to the cutoffs currently set by our national insurance organization.
Definition of priorities for IFN-free regimens
The proportions of patients with the following priorities for IFN-free regimens were determined: liver decompensation, liver transplantation, F4 with IFN and/or RBV contraindications, F4 treatment-experienced, F4 naïve, F3 with IFN and/or RBV contraindications, F3 treatment-experienced, F3 naïve, F2 with IFN and/or RBV contraindications, F2 treatment-experienced, F2 naïve, F0-F1 with IFN and/or RBV contraindications, F0-F1 treatment-experienced, F0-F1 naïve. Treatment-experienced patients included those who had failed to achieve SVR after (PEG-)IFN therapy with or without RBV, including those who had received a triple combination with boceprevir or telaprevir.
Contraindications for IFN and/or RBV were assessed only in patients with compensated liver disease (F0-F4), without prior liver transplantation, and included anemia (hemoglobin <10 g/dL), neutropenia (neutrophils <1500/mm3), thrombocytopenia (platelets <90,000/mm3), pregnancy, lactation, uncontrolled autoimmune diseases, neuropsychiatric diseases (depression, psychosis, or epilepsy), cardiac diseases (severe heart failure, severe coronary artery disease), severe chronic obstructive pulmonary disease, renal impairment (creatinine clearance <50 mL/min), uncontrolled diabetes mellitus, untreated thyroid disease, and chronic hemolytic syndromes.
Potential DDIs for DAAs
The potential for DDIs between any medication used by the study subjects and IFN, RBV, boceprevir, telaprevir, simeprevir, sofosbuvir, daclatasvir, ledipasvir/sofosbuvir, ombitasvir/paritaprevir/ritonavir±dasabuvir was assessed according to the HEP Drug Interaction Checker (Liverpool University, available online at: www.hep-druginteractions.org) and the relevant prescribing information. All drugs were classified into those with no DDIs or no clear data for DDIs, potential DDIs, and contraindication due to DDI for each DAA.
Statistical analysis
All data were analyzed using the statistical package SPSS (SPSS Inc., Chicago, IL, USA). Statistical analysis was performed using the t-test or Mann-Whitney test for comparisons of continuous variables between groups and the corrected chi-squared test for comparisons of qualitative data. Multivariate analysis was performed using logistic regression models. Only variables with a P-value ≥0.10 in the univariate analysis were included in the multivariate analysis models. A two-tailed P-value <0.05 was considered to be statistically significant for all comparisons.
Results
Patient characteristics
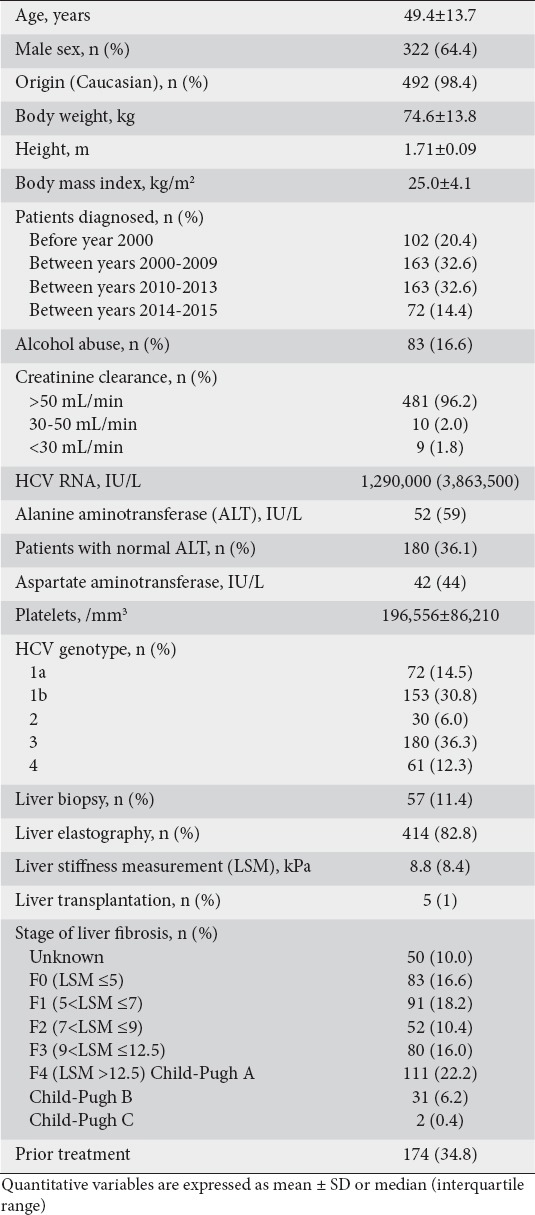
A total of 500 patients were included in the study. Their mean age was 49.4±13.7 years and 322 (64.4%) were males. Thirty-three patients (6.6%) had decompensated cirrhosis (Child class B: 31, Child class C: 2) and 5 (1.0%) patients had undergone liver transplantation. Of the remaining 462 patients, 57 (12.3%) had undergone liver biopsy and 357 (77.3%) liver elastography, while the liver disease severity could not be determined in 48 (10.4%) patients. The main characteristics of the study population are shown in Table 1.
Table 1.
Basic characteristics of 500 patients positive for hepatitis C virus
Priorities for IFN-free regimens
The proportions of patients with priorities for treatment with IFN-free regimens, according to the severity of liver disease, contraindication(s) for IFN and/or prior treatment failure, are depicted in Table 2. Decompensated cirrhosis was present in 33 (6.6%) of the study subjects and 5 (1%) had HCV recurrence after liver transplantation. Of the rest, 109 patients (21.8%) were classified as stage F4, 79 (17.1%) as F3, 52 (10.4%) as F2 and 174 (34.8%) as F0-1. The cumulative rates of patients with priorities for IFN-free regimens in relation to the severity of liver disease and patient subgroups are also shown in Fig. 1.
Table 2.
Possible priorities for interferon (IFN)-free regimens among the study population (N=500)
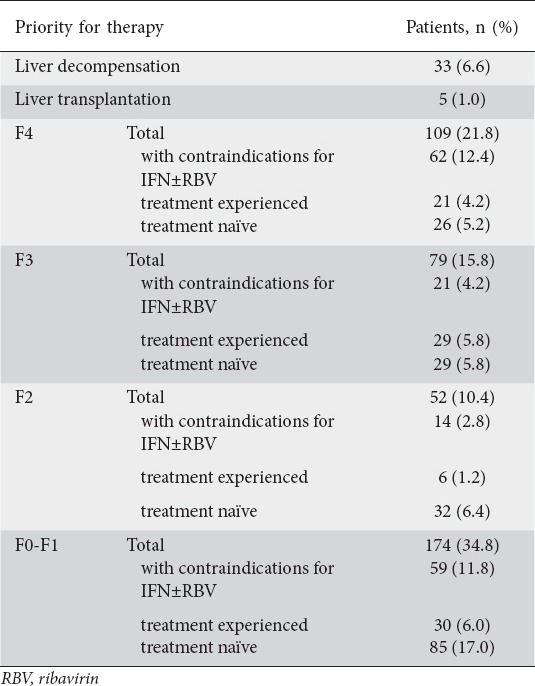
Figure 1.
Prevalence of several priorities for interferon-free regimens among study participants. Percentages on each bar are cumulative for all indications to the left
The last column does not reach 100% because there were 48 (9.6%) patients who could not be classified as the severity of liver fibrosis was not known.
Liver decomp., liver decompensation; Liver Tx, liver transplantation; IFN cont, contraindications for interferon-alfa; Tx fail, prior treatment failure; Tx naïve, treatment naïve
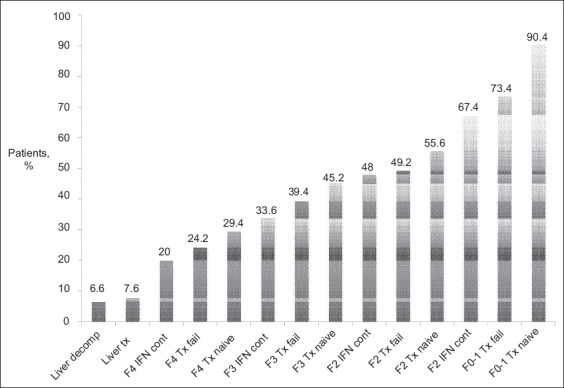
Contraindications for IFN treatment
Contraindications for IFN and/or RBV therapy were examined in the 462 non-transplant HCV patients with compensated liver disease (353 without cirrhosis and 109 with compensated cirrhosis) (Table 3). The most common contraindications for IFN and/or RBV were related to neuropsychiatric disease (73 patients, 15.8%), hematologic disorder, i.e., anemia, thrombocytopenia or neutropenia (46 patients, 10%), or cardiovascular disease (45 patients, 9.7%). Cirrhotic compared to non-cirrhotic patients presented with a higher prevalence of hematologic (32.1% vs. 3.1%, P<0.001) and cardiovascular disease (17.4% vs. 9.4%, P=0.004) and a lower prevalence of neuropsychiatric contraindications (9.2% vs. 17.8%, P<0.05).
Table 3.
Contraindications for interferon-alpha and ribavirin therapy in non-transplant chronic hepatitis C patients with compensated liver disease
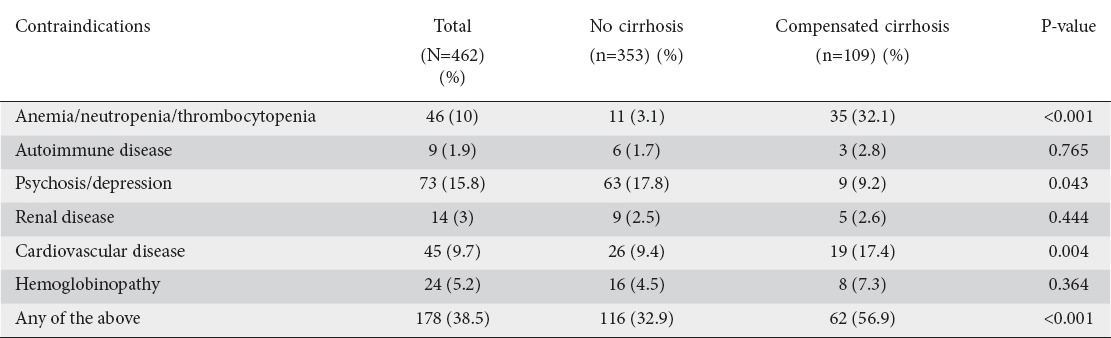
DDIs between HCV agents and non-HCV co-medications
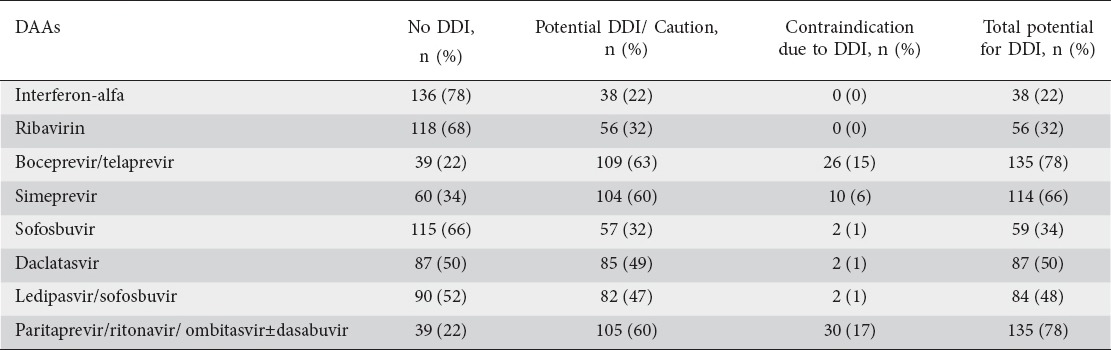
Among the 500 study participants, 174 (35%) who were on chronic co-medications were examined for potential DDIs with HCV agents. The risk for clinically significant DDIs with patient chronic co-medications varied widely among the different HCV agents. Of the 174 patients with chronic co-medications, contraindications due to DDIs were present in 30 (17%) patients for ombitasvir/paritaprevir/ritonavir±dasabuvir, 26 (15%) patients for boceprevir/telaprevir, 10 (6%) patients for simeprevir and 2 (1%) patients for sofosbuvir, daclatasvir or ledipasvir/sofosbuvir. In contrast, no contraindications due to DDIs were found for IFN and RBV. The total risk of DDIs was greater for boceprevir/telaprevir and ombitasvir/paritaprevir/ritonavir±dasabuvir (135 patients, 77.8%) compared to all other agents (P<0.001). On the other hand, the total potential for DDIs was least for the use of sofosbuvir in comparison with boceprevir/telaprevir, ledipasvir/sofosbuvir, simeprevir, daclatasvir (P<0.001) or ombitasvir/paritaprevir/ritonavir±dasabuvir (P<0.05) (Table 4).
Table 4.
Patients with contraindications due to drug-drug interactions (DDIs) or potential DDIs to hepatitis C virus (HCV) direct-acting antivirals among 174 (35%) of 500 HCV patients who were on co-medications
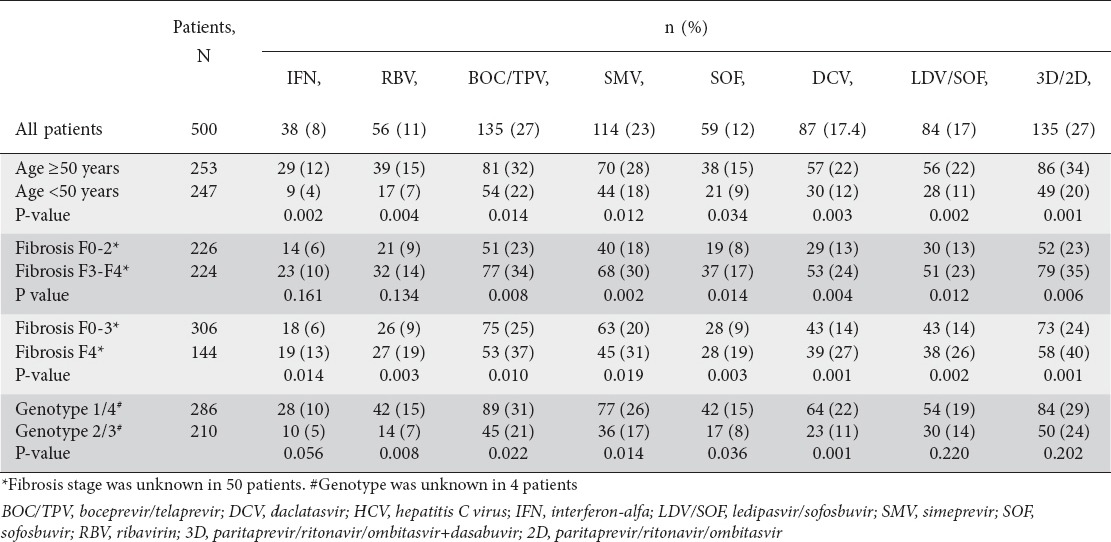
Contraindications/potential DDIs were more frequently present in patients aged ≥50 than in those <50 years (P≤0.034). Regarding fibrosis stage, the overall potential for DDIs was more prevalent in patients with F3-4 than F0-2 (P≤0.001) or in patients with F4 than F0-3 (P≤0.019) for all DAAs. Patients with HCV genotype 1 or 4 appeared to have greater total potential for DDIs than patients with genotype 2 or 3, for all DAAs (P≤0.036) except for ledipasvir/sofosbuvir and ombitasvir/paritaprevir/ritonavir±dasabuvir (Table 5). Logistic regression analyses showed that the stage of fibrosis (particularly F3) was the only factor that was independently associated with the total potential for DDIs with any of the HCV agents (data not shown).
Table 5.
Patients with contraindications due to drug-drug interactions (DDIs) or potential DDIs to HCV direct-acting antivirals in relation to patient characteristics
Discussion
This real world clinical study provides a clear overview of the HCV patient profiles at the outpatient liver clinics of Greek tertiary centers in 2015. According to our findings, almost 30% of CHC patients presented with compensated (22%) or decompensated (7%) cirrhosis. This specific patient subgroup is of particular clinical interest, as it is highly prioritized for IFN-free regimens even in health care systems with restricted access to the new therapies. Since IFN-free regimens offer for the first time exceptionally high SVR rates in such difficult-to-treat patients, the numbers of HCC and liver transplant cases and of liver-related deaths are expected to decrease in the near future [10].
Despite the obvious benefits from the short-term improvements in morbidity and mortality, treatment and reimbursement policies that restrict access to IFN regimens only to CHC patients with cirrhosis, as is the current situation in Greece, are not considered to be adequate in order to achieve the WHO Global Hepatitis Strategy goal for HCV elimination by 2030. A recent Greek study demonstrated that, in order to reach the WHO goals for morbidity and mortality by 2030, a significant increase is required in the treatment coverage with highly effective IFN-free regimens [10]. This increase in treatment coverage can be achieved only via a gradual expansion of the priorities for IFN-free therapies. Our findings suggest that the relatively small proportion of all patients with F3 fibrosis (16%) could be initially included among the groups with free access to current DAAs by the Greek national insurance carrier. In fact, given that patients with F3 fibrosis who have failed to respond to (PEG-)IFN-based regimens already have access to the new agents, the remaining patient population with F3 fibrosis is even smaller (approximately 10%). The criteria for DAA prioritization could gradually be expanded to include patients with moderate (F2) fibrosis and subsequently any CHC patient, as treatment of CHC patients at an early stage has been demonstrated to be a cost-effective strategy [11], leading to reductions in healthcare costs related to liver disease [11,12].
As long as strategies for prioritization to IFN-free regimens are applied, the criteria for assessment of the severity of liver fibrosis have great clinical impact. Since liver biopsy has been performed exceptionally rarely in CHC patients over the last years and the evaluation of liver fibrosis severity is usually based on noninvasive markers, and mainly on liver elastography, the liver stiffness cutoff values for the discrimination of different stages of liver fibrosis are of paramount importance. According to recent data, liver stiffness cutoff values aiming to optimize the indications for HCV treatment and sensitivity for certain stages of fibrosis are lower than those which maximize the diagnostic accuracy of the same fibrosis stage [13]. Such a redefinition of the liver stiffness cutoff values, according to improved harm/benefit ratios and available treatment options, would result in a decrease in the numbers of inappropriately untreated patients [13].
Contraindications for IFN and/or RBV combinations and prior treatment failure after (PEG)IFN-based therapy are two additional factors that may affect the priorities for IFN-free DAA regimens. Even after excluding patients with liver transplantation or decompensated cirrhosis, almost 40% of our remaining CHC patients had at least one contraindication for IFN and/or RBV therapy. The presence of such contraindications no longer precludes treatment of these patients, who can be effectively treated with IFN-free and perhaps RBV-free DAA combinations [4]. Thus, it may be considered unethical not to offer access to the only possible therapeutic option, which is therapy with DAA regimens, in all CHC patients with IFN and/or RBV contraindications, independently of the severity of their liver disease.
Besides cost, DDIs represent the main barrier to the use of DAAs, raising concerns more frequently than during the IFN era [7,8]. Consequently, at the initiation of DAA therapy, clinicians must be alert to the possibility of clinically significant DDIs with co-medications in all CHC patients. Approximately one third of our 500 patients with HCV mono-infection reported chronic use of co-medications. Among these patients, contraindications for DAAs due to DDIs were present in 1-17% and contraindications or potential DDIs for DAAs were present in 34-78% patients. Contraindications due to DDIs and total DDI risk were more frequent for ombitasvir/paritaprevir/ritonavir±dasabuvir (17% or 78%) or boceprevir/telaprevir (15% or 78%) than for any other DAA (1-6% or 34-66%), while the total DDI risk was less frequent for sofosbuvir (34%) than for any other DAA (48-78%). Our results are in line with previous reports showing that ombitasvir/paritaprevir/ritonavir±dasabuvir and the first-generation protease inhibitors (boceprevir/telaprevir) have a higher probability of DDIs [7,8,14,15]. Maasoumy et al reported that 49% of 115 consecutively treated CHC patients were exposed to at least one drug with DDI potential during treatment with HCV protease inhibitors at a German tertiary referral center [7]. The DDI concern is probably more frequent in HCV patients with HIV co-infection, as several anti-HIV agents have potential DDIs with the current HCV DAAs [4].
Our data show that the probability of DDIs with HCV DAAs is higher in CHC patients who are more likely to be prioritized for IFN-free therapies. In particular, the probability of DDIs increases with the severity of fibrosis (i.e. stages F3 and particularly F4). Older age and genotype 1 or 4 were also found to increase the risk of DDIs, but these associations did not persist in the multivariate analyses. On the other hand, it is well known that aging is typically paralleled by an increased prevalence of comorbidities and polypharmacy [16], whereas elderly patients present with physiological alterations in the liver metabolism of drugs that might potentiate DDIs [16,17]. Therefore, particular caution regarding DDIs is required in patients with advanced liver disease, particularly those of older age.
Despite the careful design, our study had some limitations. The quality of the data was based on the accuracy of the patients’ records, as is always the case in almost any retrospective study. However, we think that the inclusion of outpatient liver clinics with long experience in the management of patients with viral hepatitis has minimized such a problem. The classification of the stages of fibrosis may not be so accurate in our study, as it was based not on liver biopsies but on cutoff values of liver stiffness measurements, which have variable diagnostic accuracy for differentiating stages of liver fibrosis, particularly those of intermediate severity [13]. On the other hand, the subgroup of patients with advanced liver disease may have been overrepresented in our study as a result of potential referral and/or awareness bias. The inclusion of clinics from five tertiary liver centers might have resulted in an increased prevalence of patients with more severe fibrosis or cirrhosis and underrepresentation of patients with no or mild fibrosis, compared to the overall HCV population in Greece. Moreover, patients with advanced liver disease might also have been overestimated, as a consequence of the cross-sectional design of our study and in particular the specific inclusion period. Since such patients have become increasingly aware of the approval of HCV DAAs, they might have come to the liver clinics of tertiary liver centers more frequently in 2015, which was an early DAA era just six months after the start of DAA use in Greece. Finally, HCV patients with mild fibrosis are generally less likely to be referred to large tertiary centers, particularly in a period of DAAs prioritization, but this may not be the case for Greece, where the vast majority of patients diagnosed with HCV are normally seen by tertiary liver centers.
In summary, the expansion of the criteria for prioritization of IFN-free regimens from patients with cirrhosis to patients with F3 and perhaps even F2 fibrosis will increase the proportion of patients with access to DAAs by 10-15% and 10%, but will offer significant improvements in the future morbidity and mortality rates from HCV-related liver disease. Such a careful data-driven approach, with a gradual expansion of access to DAA therapy, can be helpful in the management of the available health budget. At the same time, the increasing use of DAAs requires a good knowledge of their pharmacokinetics and a sound understanding of their DDI potential. Apart from the theoretical investigation of drug metabolism and relevant electronic databases, practitioners using HCV DAAs should be familiar with current DDI management recommendations, as this management in routine clinical practice depends upon the nature of the interaction. The probability of DDIs with non-HCV co-medications is highest for protease inhibitors and lowest for sofosbuvir, but the potential for DDIs is present for all current DAAs and is more frequent in HCV patients with advanced liver disease and/or those of older age. Since potential DDIs with current HCV DAAs might not yet have been completely evaluated, and clear DDI recommendations may not be available, vigilance is necessary in relation to any co-medication used by CHC patients under DAAs.
Summary Box.
What is already known:
Interferon-free regimens with direct-acting antivirals (DAAs) currently represent the recommended treatment options for patients with chronic hepatitis C
One of the few limitations of current DAAs is the risk of drug-drug interactions (DDIs)
The high cost of DAAs and the limited availability of resources necessitate the prioritization of such treatment in many countries
What the new findings are:
In Greece, and countries with similar DAA prioritization, the expansion of the criteria for DAA reimbursement from cirrhosis to F3 and perhaps F2 fibrosis will increase the proportion of patients with DAAs access by only 10-15% and 10%, respectively
Potential for DDIs is frequently present with protease inhibitors, but also exists with other DAAs
The probability of DDIs is higher in patients with priority for DAAs, including those with advanced liver disease, who are usually of older age
Biography
Medical School of National and Kapodistrian University of Athens, Laiko General Hospital, Athens; Thessaly University Medical School, Larissa; Medical School of Aristotle University of Thessaloniki; Medical School of National and Kapodistrian University of Athens, Hippokratio General Hospital, Athens; University Hospital of Patras; Gilead Sciences Hellas, Greece
Footnotes
Conflict of Interest: Μargarita Papatheodoridi has nothing to declare. George N. Dalekos has served as an advisor/lecturer for AbbVie, Bayer, Bristol-Myers Squibb, Gilead, Janssen, Novartis, Roche and has received grant support from Bristol-Myers Squibb, Gilead, Roche. John Goulis has served as an advisor/lecturer for Bristol-Myers Squibb, Gilead, GlaxoSmithKline, Merck Sharp & Dohme, Roche and has received grant support from Bristol-Myers Squibb. Spilios Manolakopoulos has served as an advisor/lecturer for AbbVie, Bristol-Myers Squibb, Gilead, GlaxoSmithKline, Merck Sharp & Dohme, Novartis, Roche and has received grant support from Bristol-Myers Squibb. Christos Triantos has served as an advisor/lecturer for Bristol-Myers Squibb, Gilead, Merck Sharp & Dohme. Kalliopi Zachou has nothing to declare. Argyro Koukoufiki has nothing to declare. Αnastasia Κourikou has nothing to declare. Κonstantinos Ζisimopoulos has nothing to declare. Christos Τsoulas is an employee of Gilead Science Hellas, Greece. George V. Papatheodoridis has served as an advisor/lecturer for AbbVie, Boehringer Ingelheim, Bristol-Myers Squibb, Gilead, GlaxoSmithKline, Janssen, Merck Sharp & Dohme, Novartis, Roche, has received grant support from AbbVie, Bristol-Myers Squibb, Gilead, Janssen, Roche, has served as consultant for Roche and has served as a member of Data Safety Management Board for Gilead.
References
- 1.Webster DP, Klenerman P, Dusheiko GM. Hepatitis C. Lancet. 2015;385:1124–1135. doi: 10.1016/S0140-6736(14)62401-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Asselah T, Marcellin P. Interferon free therapy with direct acting antivirals for HCV. Liver Int. 2013;33 Suppl;1:93–104. doi: 10.1111/liv.12076. [DOI] [PubMed] [Google Scholar]
- 3.European Association for the Study of the Liver. EASL Clinical Practice Guidelines: management of hepatitis C virus infection. J Hepatol. 2011;55:245–264. doi: 10.1016/j.jhep.2011.02.023. [DOI] [PubMed] [Google Scholar]
- 4.European Association for the Study of the Liver. EASL recommendations on treatment of hepatitis C 2016. J Hepatol. 2017;66:153–194. doi: 10.1016/j.jhep.2022.10.006. [DOI] [PubMed] [Google Scholar]
- 5.Martin NK, Vickerman P, Dore GJ, et al. STOP-HCV Consortium Prioritization of HCV treatment in the direct-acting antiviral era: An economic evaluation. J Hepatol. 2016;65:17–25. doi: 10.1016/j.jhep.2016.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Höner Zu, Siederdissen C, Maasoumy B, Deterding K, et al. Eligibility and safety of the first interferon-free therapy against hepatitis C in a real-world setting. Liver Int. 2015;35:1845–1852. doi: 10.1111/liv.12774. [DOI] [PubMed] [Google Scholar]
- 7.Maasoumy B, Port K, Serrano Calle B, et al. The clinical significance of drug-drug interactions in the era of direct-acting anti-viral agents against chronic hepatitis C. Aliment Pharmacol Ther. 2013;38:1365–1372. doi: 10.1111/apt.12523. [DOI] [PubMed] [Google Scholar]
- 8.Höner Zu, Siederdissen C, Maasoumy B, Marra F, et al. Drug-drug interactions with novel all oral interferon-free antiviral agents in a large real-world cohort. Clin Infect Dis. 2016;62:561–567. doi: 10.1093/cid/civ973. [DOI] [PubMed] [Google Scholar]
- 9.Triantos C, Konstantakis C, Tselekouni P, Kalafateli M, Aggeletopoulou I, Manolakopoulos S. Epidemiology of hepatitis C in Greece. World J Gastroenterol. 2016;22:8094–8102. doi: 10.3748/wjg.v22.i36.8094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gountas I, Sypsa V, Papatheodoridis G, Souliotis K, Razavi H, Hatzakis A. Is elimination of HCV possible in a country with low diagnostic rate and moderate HCV prevalence?The case of Greece. J Gastroenterol Hepatol. 2017;32:466–472. doi: 10.1111/jgh.13485. [DOI] [PubMed] [Google Scholar]
- 11.Leidner AJ, Chesson HW, Xu F, Ward JW, Spradling PR, Holmberg SD. Cost-effectiveness of hepatitis C treatment for patients in early stages of liver disease. Hepatology. 2015;61:1860–1869. doi: 10.1002/hep.27736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gordon SC, Pockros PJ, Terrault NA, et al. Impact of disease severity on healthcare costs in patients with chronic hepatitis C (CHC) virus infection. Hepatology. 2012;56:1651–1660. doi: 10.1002/hep.25842. [DOI] [PubMed] [Google Scholar]
- 13.Colli A, Fraquelli M, Prati D, et al. Deciding on interferon-free treatment for chronic hepatitis C: updating liver stiffness cut-off values to maximize benefit. PLoS One. 2016;11:e0164452. doi: 10.1371/journal.pone.0164452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lauffenburger JC, Mayer CL, Hawke RL, Brouwer KL, Fried MW, Farley JF. Medication use and medical comorbidity in patients with chronic hepatitis C from a US commercial claims database: high utilization of drugs with interaction potential. Eur J Gastroenterol Hepatol. 2014;26:1073–1082. doi: 10.1097/MEG.0000000000000152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Talavera Pons S, Boyer A, Lamblin G, et al. Managing drug-drug interactions with new direct-acting antiviral agents in chronic hepatitis C. Br J Clin Pharmacol. 2017;83:269–293. doi: 10.1111/bcp.13095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Marengoni A, Nobili A, Onder G. Best practices for drug prescribing in older adults: a call for action. Drugs Aging. 2015;32:887–890. doi: 10.1007/s40266-015-0324-3. [DOI] [PubMed] [Google Scholar]
- 17.Vermehren J, Peiffer KH, Welsch C, et al. The efficacy and safety of direct acting antiviral treatment and clinical significance of drug-drug interactions in elderly patients with chronic hepatitis C virus infection. Aliment Pharmacol Ther. 2016;44:856–865. doi: 10.1111/apt.13769. [DOI] [PubMed] [Google Scholar]


