Abstract
The Botswana workplace wellness program (WWP) for health care workers (HCWs) was initiated in 2007. WWP implementation was assessed using a sequential, explanatory, mixed methods design including a national implementation assessment (27 health districts) and in-depth interviews (n = 38). Level of implementation varied across districts with health screening, therapeutic recreation, and health promotion implemented more frequently than occupational health activities and psychosocial services. Facilitators to WWP implementation included establishment of a dedicated, diverse WWP committee; provision of administrative support, and integration of activities into organizational culture. Barriers included competing priorities related to delivery of health services to clients, limited technical ability to deliver occupation health activities and psychosocial support, receipt of health services from colleagues, and limited appreciation for personal wellness by some HCWs. Ensuring the well-being of HCWs is critical in reaching international health goals.
It is widely accepted that health professionals are particularly vulnerable to high levels of occupational stress,1,2 which has been defined as the harmful physical and emotional responses that occur when job requirements do not match the capabilities, resources, or needs of the worker.3 Contributing factors include long hours, heavy workload, and the mental and physical demands of providing care for ill patients.4 Data suggest that health workers responding to the HIV/AIDS epidemic are especially susceptible to occupational stress.5,6 The HIV/AIDS epidemic continues to pose public health and health systems challenges for many countries, particularly in sub-Saharan Africa where it is estimated that 24.7 million people are infected with the disease.7
Several unique stressors have been identified related to providing HIV/AIDS treatment and care, including risk of contagion, high mortality rate among patients, ethical concerns about confidentiality and stigma, and coping with ongoing loss.6 Before comprehensive treatment programs, in-patient death rates and limited possibilities of effective care contributed to professional frustration and stress for health workers.8 While levels of work-related stress may have decreased in countries with large-scale antiretroviral treatment programs due to improved patient survival, stress in the workplace remains a reality for many health workers involved in HIV treatment, care, and support. This is particularly relevant, given the ambitious HIV care and treatment targets recently released by UNAIDS. The targets aim to have 90% of HIV-positive individuals know their status, have 90% of HIV-positive individuals on antiretroviral treatment, and have 90% of those on treatment virally suppressed.9
In an effort to ensure that health workers are equipped to cope with the physical and emotional demands of their job, the Botswana Ministry of Health (MOH) initiated a comprehensive workplace wellness program for health workers in 2007. Workplace wellness programs are employer initiatives, such as health promotion activities or organization-wide policies, directed at improving the health and well-being of workers and, in some cases, their dependents.10 Data suggest that workplace wellness programs can have numerous benefits, including lower healthcare costs, reduced absenteeism, and increased productivity.11–13 The aim of the Botswana workplace wellness program is to empower health workers with knowledge and skills to manage and cope with the dynamic demands of the health care system, which had been exacerbated by the HIV/AIDS epidemic.14 The development of the program was guided by a needs assessment.15 District focal persons and committees within the District Health Management Teams implemented the workplace wellness program within the health districts and facilities. A training-of-trainers model was used to build capacity of health workers to lead wellness-related activities that focused on holistic improvement in the health and wellbeing of health workers. The recommended minimum package for the program included the following components: 1) health screening, treatment, and care; 2) health promotion; 3) stress management and team building; 4) occupational health and safety; 5) psychosocial and spiritual care; and 6) therapeutic recreation.14Table 1 provides a description of each component along with implementation guidance.
TABLE 1.
Components of the Botswana Workplace Wellness Program for Health Workers
| Workplace Wellness Program Component | Description |
| 1) Health screening, treatment, and care | Encompass comprehensive health services, from clinical assessments to identify disease before symptoms show to providing necessary medical consultations and treatment interventions as well as referral for care.The minimum standard includes screening related to the following areas: 1. Blood pressure 2. Blood glucose 3. Body mass index 4. Breast cancer 5. Cervical cancer 6. Cholesterol 7. Ears, nose, and throat 8. Eye health 9. HIV 10. Oral Health 11. Prostate cancer 12. Psychosocial stress and anxiety 13. Tuberculosis-Services are to be operationalized through the implementation of a Staff Clinic, designation of clinician to see staff, or prioritizing staff for consultation |
| 2) Health promotion | Address health and lifestyle issues through commemorations, health talks, and targeted seminars focused on empowering health workers to be in control of all dimensions of their lives. The minimum standard includes the following activities:Commemorations • Month of Prayer against HIV/AIDS • Month of Breast Cancer Awareness • World Diabetes Day • World TB Day • Month of Youth Against AIDS • World AIDS DayHealth talks • Personal finance • Diet and nutrition • Exercise • Alcohol use • Tobacco useTargeted seminars • Men • Women • Youth |
| 3) Stress management and team building | Includes trainings, workshops, and other activities to reduce stress and strengthen teamwork in order to enhance the physical, psychological, emotional, and occupational well-being of health workers. |
| 4) Occupational health and safety | Address issues of safety in the workplace, focusing on identification of health hazards and prevention, control, and management of the health hazards. It also addresses occupational exposure, injury, and postexposure prophylaxis (PEP) services. The minimum standard includes provision of PEP of HIV for health workers, conducting safety talks, and providing screening for occupational infection. |
| 5) Psychosocial and spiritual care | Involves support groups of health workers led by a trained group facilitator. It also includes activities such as counseling, prayer, Holy Communion, and scripture reading. |
| 6) Therapeutic recreation | Focuses on improving the physical, psychological, emotional, and occupational well being of health workers through activities such as, physical fitness, social recreation, and “edutainment.” |
Although data suggest that workplace wellness programs can be beneficial from both the employer and employee perspective,11–13 the implementation of such programs across a national health system is not well documented. A recent review article highlighted the need for research focusing on the programmatic aspects of implementing these initiatives.16 The purpose of this study was to assess the level of implementation of the national Workplace Wellness Program in Botswana and identify barriers to and facilitators of implementation.
METHODS
A sequential, explanatory, mixed methods design was used to collect quantitative and qualitative data in two phases. The first phase was a quantitative national implementation assessment of workplace wellness activities throughout the country. The second phase encompassed qualitative in-depth interviews with program implementers at national-, district-, and facility-levels to contextualize findings from the implementation assessment. This allowed for the in-depth interviews to be tailored to explain findings from the implementation assessment. The evaluation was approved by the MOH Health Research and Development Committee and a nonresearch determination was received by the University of Washington's Internal Review Board. It was conducted by the International Training and Education Center for Health (I-TECH), which is a collaboration between the University of Washington and University of California, San Francisco under the guidance of a reference group composed of healthcare stakeholders. The reference group included representation from the Botswana MOH Departments of Corporate Services, HIV/AIDS Prevention and Care, Clinical Services, and Public Health; the Seventh Day Adventist Mission Hospital in Kanye; Directorate of Public Service Management, Office of the President; the World Health Organization; and CDC Botswana.
The Implementation Assessment implementation assessment was conducted to determine how the workplace wellness program had been executed throughout Botswana. The assessment was administered via a telephone interview with the focal person overseeing the workplace wellness program in each of the 27 health districts in the country. A quantitative interview guide was developed from the program implementation guide and operational guidelines to assess level of implementation of the program. This structured interview guide contained close-ended questions related to each of the six components of the workplace wellness program. After completion of the interviews, a numeric Implementation Assessment Summary Score implementation assessment summary score was calculated to quantify the level of program implementation in each district. Specifically, each district was assigned a rating between 0 and 10 for each of the six components of the program. Summary scores were then constructed as the sum of each of the six ratings.
In-depth interviews were conducted at national-, district-, and facility-levels with individuals involved in the development and/or implementation of the program to identify facilitators of and barriers to implementation of the workplace wellness program. A total of 38 in-depth interviews were conducted. This included 17 national-level interviews, 10 district-level interviews, and 11 facility-level interviews. District and facility-level interviews were conducted in six purposely selected health districts within Botswana, which represents 22% of the health districts in the country. These districts were selected using the Implementation Assessment Summary Score assigned to each health district. Specifically, the three districts with the highest scores and the three with the lowest scores related to program implementation were included to enable variability of the data and yield the most relevant information related to facilitators and barriers. Interviewees for the in-depth interviews were identified using a snowball technique, which involved the district-level workplace wellness focal person identifying other interviewees having knowledge of program implementation in their health district at district- and facility-level. A semi-structured interview guide with open-ended questions was administered during the interviews. These were conducted face-to-face, with a rapporteur present to take notes, and informed consent was obtained. With permission, the interviewers also captured the interviews with a digital voice recorder. After the interviews, the voice recordings were transcribed and translated from Setswana to English, as necessary.
For the Implementation Assessment, a database was created using REDCap, an electronic data capture tool hosted at the Institute for Translational Health Sciences at the University of Washington.17 REDCap (Research Electronic Data Capture) is a secure, web-based application designed to support data capture for research studies, providing an intuitive interface for validated data entry. Data were exported to SPSS v 17 (Released 2008, SPSS Inc, Chicago IL) for analysis. Descriptive statistics were generated to characterize findings. Qualitative data included full transcriptions from in-depth interviews. A general inductive approach was taken for analyzing the interview data.18 This involved the manual coding of textual data and identification of common themes, in order to condense the data into a summary format and establish links with the evaluation objectives. Transcripts were reviewed to identify and code themes using ATLAS.ti v7.0 software (Released 2012, ATLAS.ti Scientific Software Development GmbH, Berlin).
RESULTS
Component 1: Health Screening, Treatment, and Care
Of the 13 health screening programs recommended for implementation by the workplace wellness program, only blood pressure monitoring and HIV testing were reported to be available in all 27 districts (Fig. 1). Screening for prostate cancer was reported in nine of the 27 districts. Across all health screening areas, the outpatient department where patients from the community are seen was the most common location for receiving these services. In some cases, health works seeking screening services were prioritized over patients from the community, but it was not uncommon to have health care workers queuing alongside patients to receive these services. Seven districts indicated that a staff clinic was available to health workers for some of the screening areas.
FIGURE 1.
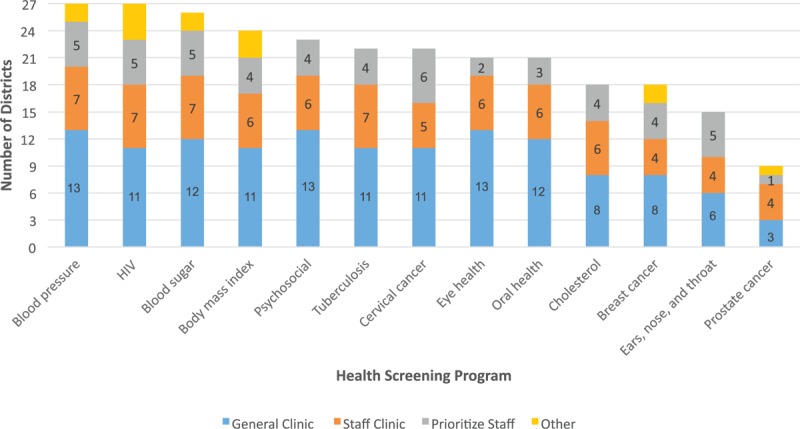
Health screenings programs offered within each district.
Component 2: Health Promotion
The minimum standard for health promotion includes health day commemorations, health talks, and targeted seminars. The recommended health commemorations were held in the majority of districts, with Breast Cancer Awareness Month and World Diabetes Day being the least observed (Fig. 2). Except for a wellness week that focused on health care workers, the majority of the commemorations targeted the community. Personal finance was the most commonly offered health talk topic. This was reported to have been offered in 18 of the districts over the past year (67%). Targeted seminars were being carried out in low numbers.
FIGURE 2.
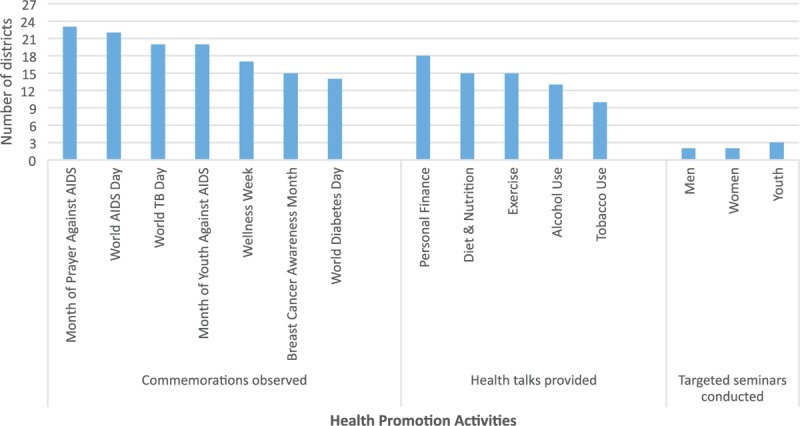
Health promotion activities at the district level.
Component 3: Stress Management and Team Building
Activities related to stress management and team building were reported by 12 districts (less than 50%) (Table 2). Generally, these were offered once (n = 5 districts) or twice (n = 3 districts) a year, with only four facilities having three or more of these activities in the previous year. In most districts, these activities were led by trainer-of-trainers and senior staff with an experience on the topic (n = 10). As expressed in the quotations below, examples of team building activities included recognition of staff and staff trips.
“During morning meetings, we try to mention staff who are doing well [at their job], who have been positive influences to the community, to our patients, and to ourselves, so that other [health workers] can take an example of this.”
“We had a trip …staff traveled around Khutseto [to] see different wild animal like lions as part of the workplace wellness program.”
“We wanted to boost the morale a bit and we went into a wildlife park.”
TABLE 2.
Access to Workplace Wellness Program Components and Related Activities
| Workplace Wellness Program Component | Activities | # (%) |
| Stress management and team building | 12 (46%) | |
| Occupational health and safety | Postexposure prophylaxis | 24 (89%) |
| Health talks | 15 (56%) | |
| Screening for occupational infections | 11 (41%) | |
| Psychosocial and spiritual care | Spiritual care | 26 (96%) |
| Counseling | 18 (67%) | |
| Active support groups | 13 (48%) | |
| Assessment of stress and anxiety | 7 (26%) | |
| Therapeutic recreation | Physical fitness activities | 21 (78%) |
| Access to sporting facilities | 15 (56%) | |
| Social recreation and edutainment | 10 (37%) | |
Component 4: Occupational Health and Safety
Most districts (n = 24) reported that postexposure prophylaxis (PEP) for health workers was available. Health talks on issues of occupational health and safety were reported to be carried out in 15 districts. In eight of these 15 districts, these sessions were led by an occupational health officer. Others presenting these talks included wellness program master trainers, environmental health technicians, senior health officers, and community members. Screenings for occupational diseases that health workers are at risk of acquiring were offered in 11 districts. These were offered most often on an as-needed basis. Topics commonly mentioned in interviews included clinical waste management, hepatitis B vaccination, TB prevention, and PEP. Representative quotations are listed below.
“We tell them how to separate waste. We mostly teach the cleaners. We tell them that this one [waste] is not supposed to be in that waste bag, the red waste bag should have those materials, the yellow waste bag should have such and such rubbish and so forth.”
“TB prevention is in every ward; keeping ventilation, keeping windows open, and ensuring patients are using masks.”
“If you are exposed to HIV, if you get a needle [stick] prick…you shouldn’t keep it to yourself, you need to come immediately and get the service…the drug [PEP] is here.”
Component 5: Psychosocial and Spiritual Care
Spiritual care activities were reported to be offered to health workers in 26 of the 27 districts as part of the workplace wellness program. Morning prayer, scripture reading, motivational talks, and support groups were the main psychosocial and spiritual care activities mentioned by interviewees as being carried out at the facilities. As voiced by one health worker, “We have prayer every morning but it is a general one. We do it together with the patients. There is no day that we start our work without talking to God first. No. It is an activity that just happens.” Spiritual care activities were generally reported to be conducted daily (n = 16 districts) or weekly (n = 7 districts) and were most often led by a staff member or an outside professional such as a pastor. Counseling was reported to be available to health workers in 18 districts. It was indicated that in these 18 districts, the counseling was generally available daily or on as needed basis by a social worker during working hours. Support groups were reported to be active in 13 districts. Only seven districts reported that assessments for anxiety and stress were available.
Component 6: Therapeutic Recreation
Therapeutic recreation activities were offered in 21 districts through physical fitness activities. Access to a fitness or sporting facility at the district hospital was available in 15 of the districts, while social recreation activities and edutainment activities were present in 10 districts. In general, these activities were most often offered on a daily basis with edutainment activities being more likely to occur on an as needed basis. Therapeutic recreation activities were most often facilitated by experienced staff members. As expressed in the quotations below, the common therapeutic recreation activities included football (soccer), aerobics, and other activities such as netball, and volleyball. Clinics, in general, did not have a gym, but often could use the facility at the district hospital.
“We have aerobics, netball, and football.”
“With gentlemen, it is very easy to come together and play football…we are still working on getting females together for netball and other activities.”
“This week…we have some races: bottle races, skipping rope races, and a potato race.”
“We have aerobics in our facility. Sometimes we do something else like jogging, playing football, netball, and so forth. We have teams such as a netball and volleyball team.”
Facilitators to Workplace Wellness Program Implementation
From the in-depth interviews, having a dedicated, diverse WWP committee promoted implementation of the activities in the minimum package of wellness services. Below are statements made by health workers in the three districts with higher levels of workplace wellness program implementation.
“Each facility has a representative at [the] committee level.”
“We try as much as possible to get individuals from different locations within the district.”
“We went around to all of the facilities and tried to [educate] them about wellness, what it entails, what are the components. We invited all the cadres, starting [with] the gardeners and cleaners. From there we had sensitization meetings with them to tell them about wellness, and to choose members who can represent them [on] the committee.”
“The committee structure consists of a chairperson, vice chairperson, secretary, assistant secretary and then there are focal persons responsible for either health promotion, health screening, capacity building, psychosocial support, occupational health, therapeutic recreation. There is also someone who captures activities, who is our cameraman….we also have a staff doctor and six additional members.”
“As a committee, we make decisions, produce an annual plan, come up with activities, and then these activities are followed for that particular year.”
Districts with less active workplace wellness did not report such details about the wellness committee.
Another catalyst of program implementation was administrative support from management at the national, district, and facility level. The quotations below illustrate the need to ensure that management is well aware of the program's importance.
“The national level is very supportive. We are very much supported.”
“The other reason for success is that, as it [the workplace wellness program] is a health issue, it is easy to take it up to the management, and management will just run it down through clinic supervisors. It is very easy that way.”
“Every time we have an activity here, they [the national WWP committee] get involved. They literally come and spend time with us, and give us assistance where necessary. Maybe giving us funds and gracing the occasion with their presence.”
“Now we have started to engage supervisors, because when supervisors have a sense of ownership, we hope it will trickle down to everybody at the health facilities.”
“Management has to be involved because we cannot do anything without the management.”
Another facilitator to WWP implementation was integration of the program into facility operations to ensure it is part of the organizational culture of the health facilities. A number of specific examples were given during the interviews. Several facilities reported setting aside specific times for wellness activities on a regular, recurring basis. Another example cited was the inclusion of WWP activities in institutional and district performance plans as well as in individual performance development plans.
“The program has been rolled out to facilities. They already know what the program and its mandate are all about. They have brought their workplace wellness program facility plans, which have timelines. We are going to evaluate the program in the coming year.”
“It should form part of the institutional performance plan so that they report on those areas that are used to assess performance on a monthly basis. When you discuss the strategic plan for an institution, this should form part of your plan.”
“I am planning to sit down with management to see how we can schedule my core work and wellness programme, because this thing now forms part of my PDP [Performance Development Plan] and I want them to help me schedule everything.”
“I would say workplace wellness is part of what we do here every day”
“I think everybody who comes into the health profession to practice needs to know about the wellness program. I came here around last year March and knew 6 months later that there was a workplace wellness program”
Barriers to Workplace Wellness Program Implementation
A high workload was often cited by interviewees as a barrier to implementing program activities. As discussed in some of the quotations below, this was particularly challenging in small facilities.
“Time on my part is a challenge. There is a lot of work for me as we have a serious staff shortage. So, this leaves me with little time.”
“There is poor WWP meeting attendance because most of us are held up by our core duties.”
“Mind you, we are talking about nurses. Here at [District A] we are short-staffed, so they have other responsibilities. Sometimes they are forced to prioritize…sometimes when there is a client to be attended to, they have to skip the wellness program activities.”
“Most of our WWP trainers are in health posts. If I take those in the health posts for a WWP activity, it means the health post will close—so that is a problem for us.”
“I am the only nurse here and I am overseeing all the activities under the nursing program.”
Limited technical capacity to lead activities was noted as a barrier, particularly in districts with lower levels of WWP implementation. This was more pronounced for some programmatic areas than others. Interviewees in both the high and lower implementation districts indicated that conducting stress management activities was challenging due to limited human resources skilled in the provision of these activities. As stated by one of the high implementation districts, “One of the activities we want to do is run some workshops to impart knowledge to the people we work with, thing like stress management, which we have noticed is needed in our workplace environment.” Activities related to occupational health and safety were also mentioned as being challenging to lead due to limited technical capacity in this area.
Another barrier identified was limited appreciation of wellness activities by health workers. Interviewees indicated that personal wellness was a new concept for some. Respondents from both the higher and lower implementing districts indicated that wellness activities were not necessarily perceived as being important to the health and wellbeing of health workers.
“We need to see positively the wellness program and the importance to ourselves…our attitudes should change towards wellness.”
“For this district, the WWP is a challenge because it is a new concept to them. It is not embedded in their minds and their hearts. Sometimes it is just resistance from people, not knowing how they are going to benefit from a program.”
Finally, a key barrier involved receiving wellness services from colleagues. One of the challenges to participation in health screening activities identified during the in-depth interviews was confidentiality and trust. As one health worker stated:
“When it comes to issues like HIV and TB screening, there is still a lot of self-stigmatization among health workers. This is hindering our progress; we are not able to come together and work as a team. I remember last time when we were talking about HIV testing, they raised concerns regarding confidentiality. They said that sometimes they are not coming forward to test because they don’t want their status to be known by other health workers.”
Confidentiality and trust was also noted as a barrier related to counseling along with the Setswana culture. According to one health worker.
“Yes, counselling is available. My observation is that as staff, we do not feel comfortable receiving services from colleagues in the same hospital. Even our Setswana culture influences this nature. There are a few that come for the counselling services, especially those that understand professionalism. However, other staff can be overly inquisitive about off-duty colleagues seeking services at the facility.” This can be overcome by seeking support for these activities from external sources. In one district, social workers from outside of the health facilities are engaged in providing counseling. It was felt this “allows health workers to choose where they want to be counseled, they are allowed to go wherever they would feel free and comfortable.”
DISCUSSION
General structures for the implementation of a national workplace wellness program for health workers in Botswana have been developed across the country. To the authors’ knowledge, this is the first report of the implementation of a national workplace health promotion initiative for public health workers in middle or low income countries. Components such as health screening, therapeutic recreation, and health promotion through observation of various commemorations tended to be implemented more frequently than activities related to occupational health and safety as well as psychosocial services. Results indicate that having a dedicated and diverse WWP committee facilitated implementation of the activities in the WWP minimum package of services. Other facilitators included provision of administrative support from the national, district, and facility level, and integration of the programmatic activities into facility operations to ensure it is part of organizational culture. Barriers to implementation included competing priorities related to delivery of health services to clients, limited technical ability to deliver activities for certain components of the WWP such as psychosocial support and occupation health and safety. In addition, provision of WWP services by colleagues was cited a barrier, particularly for health screening. There was also a limited appreciation for personal wellness by some health workers.
There has been a growing interest in workplace wellness and health promotion activities, particularly in developed countries. Data from 2009 indicate that workplace wellness programs were offered by 92% of companies in the United States that had 200 or more employees.16 Although there is a large body of literature on health promotion activities in high-income countries, workplace health promotion programs in Africa have been reported less freqeuentlly,13,19,20 particularly in health care settings.21 Much of what is known about employee wellness programs in less developed counties is provided by the Healthy Company Index, which was developed by a large health insurer in South Africa to promote healthy lifestyles among insurees19,22–24 The healthy company index, which was started in 1990, provides data on 151 companies in South Africa. The 2014 index benchmarks and tracks key health issues and offers important insights to positively impact employees’ health and productivity. It also provides important information about an organization's overall health at an organizational and individual employee level.
The present study has shown that having a dedicated WWP committee and administrative support were key facilitators in the implementation of the activities in the WWP minimum package of services. This is supported by data from the Healthy Company Index that found that company commitment was directly related to employee wellness outcomes.23 A recent investigation of an WWP implemented over 3 years in nursing homes in the United States also found that administrative support was a success factor in program implementation.25
Stigma and confidentiality were found to be barriers to the health screening component of the Botswanan Workplace Wellness Program for health workers. A study from three public hospitals in South Africa also found these concerns to barriers to uptake of facility-based HIV testing and TB screening by health workers.26 Similarly, a study from Zambia reported on the hesitation of health workers to participate in HIV testing.27 Developing strategies to mitigate this barrier is critical in ensuring that health workers engage in health screening services. Campaigns to improve awareness of confidentiality provisions among health workers have been suggested as an intervention to promote health screening among this population.26 Conducting health screening campaigns led by private practitioners or clinicians based at an outside facility could also help address this challenge. There is also a growing body of literature related to self-testing, particularly for HIV,28 which could provide another alternative.
Results from this study suggest that organizational culture of health facilities in Africa may need to develop further to institutionalize workplace wellness programs. The data suggested that in some cases, there was a limited appreciation for the role of an employer on the wellness of employees. The limited availability of activities related to occupational health services may also be due to a limited appreciation of this topic. A recent review suggests there is an ethical need in Africa for stronger articulation of occupational health practice with advocacy for prevention as cultural norm in the workplace.29 There is a need to sensitize health workers on stronger advocacy of wellness and occupational health practice. However, authors found no studies or resources specifically describing effective strategies for producing cultural shifts toward the integration of health and wellness into workplace culture.
Health promotion programs were reported to be implemented more than occupational health activities. One explanation is that the health promotion activities of the WWP were being scheduled and planned to occur alongside key events in the health calendar such as World AIDS Day, World TB Day, Breast Cancer Awareness Month, etc. Occupational health activities are generally not scheduled to coincide with these commemorations. Another possible reason for this could be limited competence of health care workers in facilitating occupational health programs. A study in Kenya found there was a positive relationship between employee training on occupational health programs and effective implementation of occupational health activities and services.30 Given the risk of occupational exposure to HIV, TB, and other infections, focus on occupational health programs is warranted. Training and instructional aids for health workers and facility managers to lead safety talks are also necessary. Given the limited literature available on the relationship between workplace health promotion and occupational health, further research would be beneficial.
This mixed methods study was not without limitations. Although the Implementation Assessment captured information from all districts in the country, the in-depth interviews were only conducted in six (22%) of the health districts and may not be generalizable. Although efforts were made to ensure the participants felt “safe” voicing their opinions during the Implementation Assessment and the in-depth interviews, social desirability may have biased some responses. Furthermore, the WWP program in this study was implemented at public health facilities and conclusions may not be applicable to nongovernmental organizations or private sector health facilities.
The health workforce in many middle and low income countries is at a unique place. Substantive progress has been made toward the attainment of key international public health and development initiatives such as the UNDP sustainable development goals, the UNAIDS 90-90-90 HIV treatment goals, and the WHO initiatives for the elimination of mother-to-child transmission of HIV and syphilis. Reaching these and other ambitious goals will, however, lay additional burden on the most essential resource in the sector, health workers. This study has highlighted important barriers to health worker wellness in Botswana such as competing priorities related to delivery of health services to clients, limited technical ability to deliver activities, and limited appreciation for personal wellness by some health care workers. It also highlighted some facilitators such as a dedicated and diverse WWP committee; provision of administrative support from the national, district, and facility level; and integration of the programmatic activities into facility operations to the health worker wellness in Botswana. These findings could be replicated in other countries in the region where the health systems and health workers are already strained and would be extremely helpful in the attainment of key international public health and development goals.
Acknowledgments
The authors would like to gratefully acknowledge Andrea Malenya, Boyce Othulmile, and Nankie Houghton for provision of administrative support and assistance in data collection as well as Jessica Grignon for assisting in tool development.
Footnotes
This work was supported by the President's Emergency Plan for AIDS Relief (PEPFAR), through funding to the University of Washington and I-TECH from the US Department of Health and Human Services, Health Resources and Services Administration (HRSA) Global HIV/AIDS Bureau, Cooperative Agreement # U91HA06801 and the Afya Bora Consortium Fellowship in Global Health Leadership supported by NIH Office of AIDS Research and CDC/PEPFAR, grant # U91HA06801B.
The authors report no conflicts of interest.
REFERENCES
- 1.Felton JS. Burnout as a clinical entity: its importance in health care workers. Occup Med 1998; 48:237–250. [DOI] [PubMed] [Google Scholar]
- 2.Mateen FJ, Dorji C. Health-care worker burnout and the mental health imperative. Lancet 2009; 374:595–597. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. Stress at Work. NIOSH publication number 99–101. Cincinnati, Ohio: National Institute for Occupational Safety and Health; 1999.
- 4.Clegg A. Occupational stress in nursing: a review of the literature. J Nurs Manag 2001; 9:101–106. [DOI] [PubMed] [Google Scholar]
- 5.Kerr ZY, Miller KR, Galos D, Love R, Poole C. Challenges, coping strategies, and recommendations related to the HIV services field in the HAART era: a systematic literature review of qualitative studies from the United States and Canada. AIDS Pat Care STDs 2013; 27:85–95. [DOI] [PubMed] [Google Scholar]
- 6.Demmer C. Burnout: the health care worker as survivor. AIDS Reader 2004; 14:522–523. 528-530, 535-527. [PubMed] [Google Scholar]
- 7.UNAIDS. The Gap Report 2014. Geneva, Switzerland: Joint United National Programme on HIV/AIDS; 2014.
- 8.Marchal B, De Brouwere V, Kegels G. Viewpoint: HIV/AIDS and the health workforce crisis: what are the next steps? Trop Med Int Health 2005; 10:300–304. [DOI] [PubMed] [Google Scholar]
- 9.UNAIDS. 90-90-90 An Ambitious Treatment Target to Help End the AIDS Epidemic. Geneva, Switzerland: Joint United National Programme on HIV/AIDS; 2014.
- 10.Goetzel RZ, Ozminkowski RJ. The health and cost benefits of work site health-promotion programs. Annu Rev Public Health 2008; 29:303–323. [DOI] [PubMed] [Google Scholar]
- 11.Baicker K, Cutler D, Song Z. Workplace wellness programs can generate savings. Health Aff (Millwood) 2010; 29:304–311. [DOI] [PubMed] [Google Scholar]
- 12.Goetzel RZ, Henke RM, Tabrizi M, et al. Do workplace health promotion (wellness) programs work? J Occup Environ Med 2014; 56:927–934. [DOI] [PubMed] [Google Scholar]
- 13.Kolbe-Alexander TL, Proper KI, Lambert EV, et al. Working on wellness (WOW): a worksite health promotion intervention programme. BMC Public Health 2012; 12:372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Government of Botswana. Botswana Workplace Wellness Program Operational Guidelines. Gaborone, Botswana: Ministry of Health; 2007. [Google Scholar]
- 15.Government of Botswana. Caring for Health Workers: a National Strategy for Botswana: Needs Assessment Report, Summary, and Recommendations. Gaborone, Botswana: Ministry of Health; 2006. [Google Scholar]
- 16.Mattke S, Hangsheng L, Caloyeras JP, et al. Workplace Wellness Programs Study: Final Report. Santa Monica, CA: RAND Corporation; 2013. [PMC free article] [PubMed] [Google Scholar]
- 17.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap): a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009; 42:377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Thomas DR. A general inductive approach for analyzing qualitative evaluation data. Am J Eval 2006; 27:237–246. [Google Scholar]
- 19.Patel D, Goetzel RZ, Beckowski M, et al. The Healthiest Company Index: a campaign to promote worksite wellness in South Africa. J Occup Environ Med 2013; 55:172–178. [DOI] [PubMed] [Google Scholar]
- 20.Yassi A, O’Hara LM, Lockhart K, Spiegel JM. Workplace programmes for HIV and tuberculosis: a systematic review to support development of international guidelines for the health workforce. AIDS Care 2013; 25:525–543. [DOI] [PubMed] [Google Scholar]
- 21.Basson HA, Roets L. Workplace wellness for HIV/AIDS-affected nurses in South Africa. Brit J Nurs 2013; 22:38–44. [DOI] [PubMed] [Google Scholar]
- 22.Kolbe-Alexander T, Greyling M, da Silva R, et al. The relationship between workplace environment and employee health behaviors in a South African workforce. J Occup Environ Med 2014; 56:1094–1099. [DOI] [PubMed] [Google Scholar]
- 23.Milner K, Greyling M, Goetzel R, et al. The relationship between leadership support, workplace health promotion and employee wellbeing in South Africa. Health Promot Int 2013; 30:514–522. [DOI] [PubMed] [Google Scholar]
- 24.Patel D, Lambert EV, da Silva R, et al. Participation in fitness-related activities of an incentive-based health promotion program and hospital costs: a retrospective longitudinal study. Am J Health Promot 2011; 25:341–348. [DOI] [PubMed] [Google Scholar]
- 25.Zhang Y, Flum M, Kotejoshyer R, Fleishman J, Henning R, Punnett L. Workplace participatory occupational health/health promotion program: facilitators and barriers observed in three nursing homes. J Gerontol Nurs 2016; 42:34–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Khan R, Yassi A, Engelbrecht MC, Nophale L, van Rensburg AJ, Spiegel J. Barriers to HIV counselling and testing uptake by health workers in three public hospitals in Free State Province, South Africa. AIDS Care 2015; 27:198–205. [DOI] [PubMed] [Google Scholar]
- 27.Kruse GR, Chapula BT, Ikeda S, et al. Burnout and use of HIV services among health care workers in Lusaka District, Zambia: a cross-sectional study. Hum Res Health 2009; 7:55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Napierala Mavedzenge S, Baggaley R, Corbett EL. A review of self-testing for HIV: research and policy priorities in a new era of HIV prevention. Clin Infect Dis 2013; 57:126–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.London L, Tangwa G, Matchaba-Hove R, et al. Ethics in occupational health: deliberations of an international workgroup addressing challenges in an African context. BMC Med Ethics 2014; 15:48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rotich L, Kwasira J. Assessment of success factors in the implementation of occupational health and safety programs in tea firms in Kenya: a case of Kaisugu tea factory. Int J Econ Commer Manag 2015; 3:797–812. [Google Scholar]


