Abstract
Prostate-specific membrane antigen (PSMA) is an attractive target for both diagnosis and therapy because of its high expression in the vast majority of prostate cancers. Development of small molecules for targeting PSMA is important for molecular imaging and radionuclide therapy of prostate cancer. Recent evidence implies that androgen-deprivation therapy increase PSMA-ligand uptake in some cases. The reported upregulations in PSMA-ligand uptake after exposure to second-generation antiandrogens such as enzalutamide and abiraterone might disturb PSMA-targeted imaging for staging and response monitoring of patients undergoing treatment with antiandrogen-based drugs. On the other hand, second-generation antiandrogens are emerging as potential endoradio-/chemosensitizers. Therefore, the enhancement of the therapeutic efficiency of PSMA-targeted theranostic methods can be listed as a new capability of antiandrogens. In this manuscript, we will present what is currently known about the mechanism of increasing PSMA uptake following exposure to antiandrogens. In addition, we will discuss whether these above-mentioned antiandrogens could play the role of endoradio-/chemosensitizers in combination with the well-established PSMA-targeted methods for pre-targeting of prostate cancer.
Keywords: Prostate-specific membrane antigen, Positron emission tomography, Antiandrogens, Prostate cancer, Molecular imaging
Introduction
Prostate cancer (PCa) is one of the most commonly diagnosed cancers among men in western industrialized nations and is a leading cause of cancer-related deaths [1]. Men with advanced PCa are usually treated with androgen-deprivation therapy (ADT) [2]. Most patients with metastatic disease treated with ADT eventually relapse with castration-resistant prostate cancer (CRPC). CRPC can be managed with the second-generation inhibitors of the androgen receptor (AR), such as enzalutamide and abiraterone [3]. These medications provide significant survival benefits, but are not curative [4], and ultimately the patients die of the disease.
Prostate-specific membrane antigen (PSMA), a transmembrane protein, is a promising target for imaging and therapy of PCa [5, 6]. First, PSMA is overexpressed in more than 85 % of primary PCa tumors and metastatic lesions in lymph nodes and bone [7–9]. Second, from the technical point of view, targeting PSMA by either by antibodies or small molecules is feasible [10–13]. Particularly, a new class of functional ligands including Glu-NH-CO-NH-Lys-[68Ga-(HBED-CC)] or 68Ga-PSMA-11 [14–17], PSMA-DKFZ-617 [18–20], 18F-DCFPyL [21] and EuK-Subkff-68GaDOTAGA [22] demonstrated their outstanding affinity to PSMA, therefore making possible the imaging of both local PCa tumors and distant metastatic lesions. These PSMA ligands can also be labeled with therapeutic radionuclides such as lutetium-177 [11]. Overall, it is anticipated that this new class of PSMA-binding radioligands will lead to a significant improvement in the diagnosis of recurrent PCa and endoradiotherapy of PCa [23].
In contrast to the normal prostate cells, fatty acid synthesis plays a crucial role in the rapid proliferation of prostate cancer cells since malignant cells need higher amounts of fatty acid for their new membrane biogenesis. Particularly choline is utilized for biosynthesis of phosphatidylcholine, and it is the basis for imaging with 18F-fluorocholine (18F-FCH) for the visualization of prostate cancer and bone, lymph nodes and visceral metastasis. Currently, for staging and monitoring treatment response, choline PET/CT using either 11C or 18F can be performed. It is generally assumed that ADT does not significantly affect choline PET/CT uptake in PCa cells considering the biological mechanism of choline-based nuclear imaging procedures [24]. However, a tendency of reduction in choline uptake following ADT is documented, particularly in hormone-naïve patients [25]. Recent in vitro and in vivo evidence and a recent clinical pilot study indicate that PSMA is regulated by androgens and suggest that ADT could considerably increase PSMA-ligand uptake [13, 26–29]. Therefore, despite the apparent clinical value of PSMA-based imaging and therapy, for those patients who are undergoing treatment with antiandrogens, evaluations of PSMA-targeted scans must account for this upregulation phenomenon.
In this manuscript we will briefly review the existing evidence regarding upregulation of PSMA expression as a result of ADT and its consequence on diagnostic images and therapeutic outcomes. In addition, the molecular background and possible mechanism of alterations in PSMA levels will also be examined. Finally, the emerging opportunities and challenges for PSMA radioligand imaging and therapy will be discussed.
Alteration in PSMA Expression by Antiandrogens
Molecular Biology of PSMA Expression
Folate hydrolase 1 (FOLH1) gene encodes PSMA protein, and it is located at the short arm of chromosome 11 in a region that is not normally omitted in PCa (11p11-p12) [30, 31]. It has been well documented that FOLH1 gene expression is suppressed by androgens [32–34]. By using an enhancer trap approach, Watt et al. [35] discovered an enhancer region as a major regulatory element for PSMA expression that considerably activates the FOLH1 core promoter region. Additionally, they reported that similar to the repression of the FOLH1 gene, PSMA expression is also inhibited in the existence of androgens. Subsequently, Noss et al. [36] sequenced and analyzed the capability of the FOLH1 promoter region to promote the transcription of PSMA mRNA. They reported that in their established PCa model cell line, the FOLH1 promoter region shaped a 21 % downregulation in response to androgens. However, activation of the enhancer region caused a 45 % downregulation in response to androgens. Furthermore, by using chromatin immunoprecipitation together with massively parallel sequencing, Yu et al. [37] recorded four peaks of AR binding in introns of the FOLH1 gene [26].
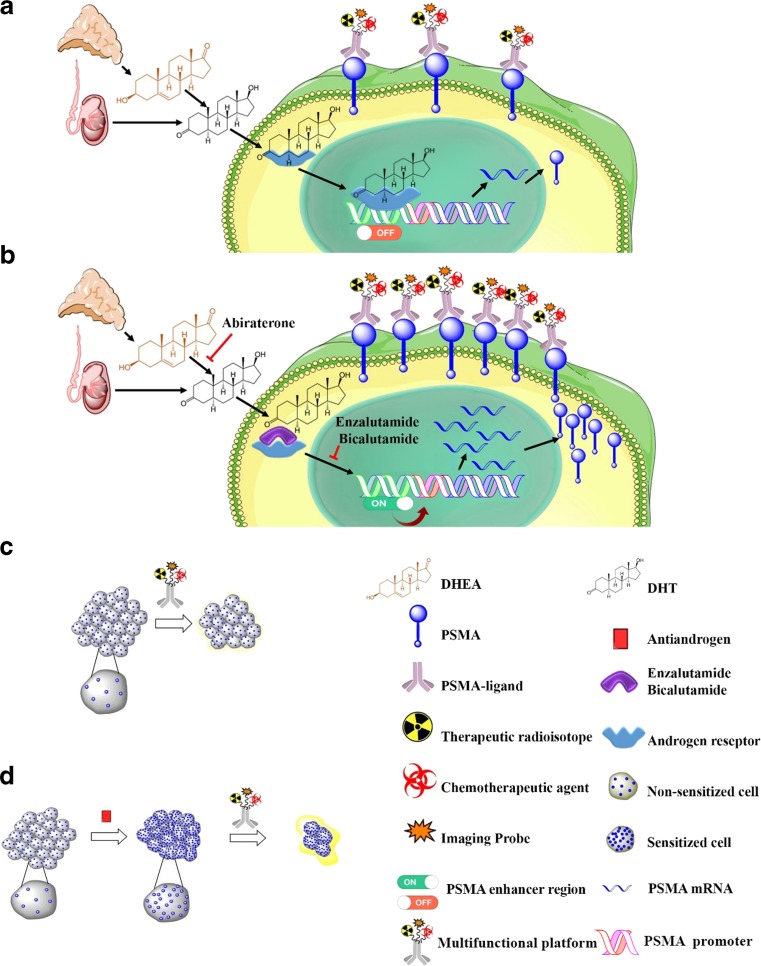
Very recent evidence substantiates the claim that we can take advantage of upregulation of PSMA expression for enhancing the efficiency of PSMA-based approaches of endoradio-/chemotherapy [13, 27–29]. However, the molecular biology of this phenomenon is unclear, and the underlying molecular mechanism needs more studies. Figure 1 illustrates PSMA-targeted endoradio-/chemotherapy using a multifunctional theranostic agent with and without pre-targeting enzalutamide, bicalutamide and abiraterone. Figure 1a illustrates that a complex including androgen and AR turns off the PSMA enhancer region of the FOLH1 gene. This complex might be responsible for androgen-mediated downregulation of FOLH1 gene transcription. Consequently, the low level of PSMA mRNA leads to a low level of PSMA on the cell membrane.
Fig. 1.
The schematic of a multifunctional PSMA-targeted endoradio-/chemotherapy with and without pre-targeting antiandrogen. (a) The androgen binds to AR, and this complex inactivates the PSMA enhancer region of the FOLH1 gene. (b) Enzalutamide competitively inhibits androgen binding to AR, and the PSMA enhancer region of the FOLH1 gene is activated. (c) Common PSMA-targeted therapy. (d) PSMA-targeted therapy with prior pre-targeting by antiandrogens
On the other hand, antiandrogens such as enzalutamide, abiraterone and bicalutamide competitively inhibit androgen binding to AR, and the PSMA enhancer region of the FOLH1 gene is switched on. Therefore, ADT leads to an antiandrogen-mediated upregulation of FOLH1 gene transcription. Finally, a high level of PSMA on the cell membrane can be observed because of the high level of PSMA mRNA (Fig. 1b). It can be inferred that common PSMA-targeted therapy without pre-targeting by antiandrogens could be less effective than PSMA-targeted therapy with prior pre-targeting by antiandrogens since increasing the level of PSMA leads to an increasing endoradio-/chemotherapeutic payload to PCa cells (Fig. 1c, d). The multifunctional platform illustrated on Fig. 1 contains an imaging probe such as 68Ga [6], a therapeutic radioisotope such as 177Lu [6] and a chemotherapeutic agent such as microtubule-disrupting agent E (MMAE) [38]. However, the biological mechanism of sensitizing PCa cells for treatment with a single function PSMA-targeted therapeutic agent containing either a radioisotope or chemotherapeutic could be similar.
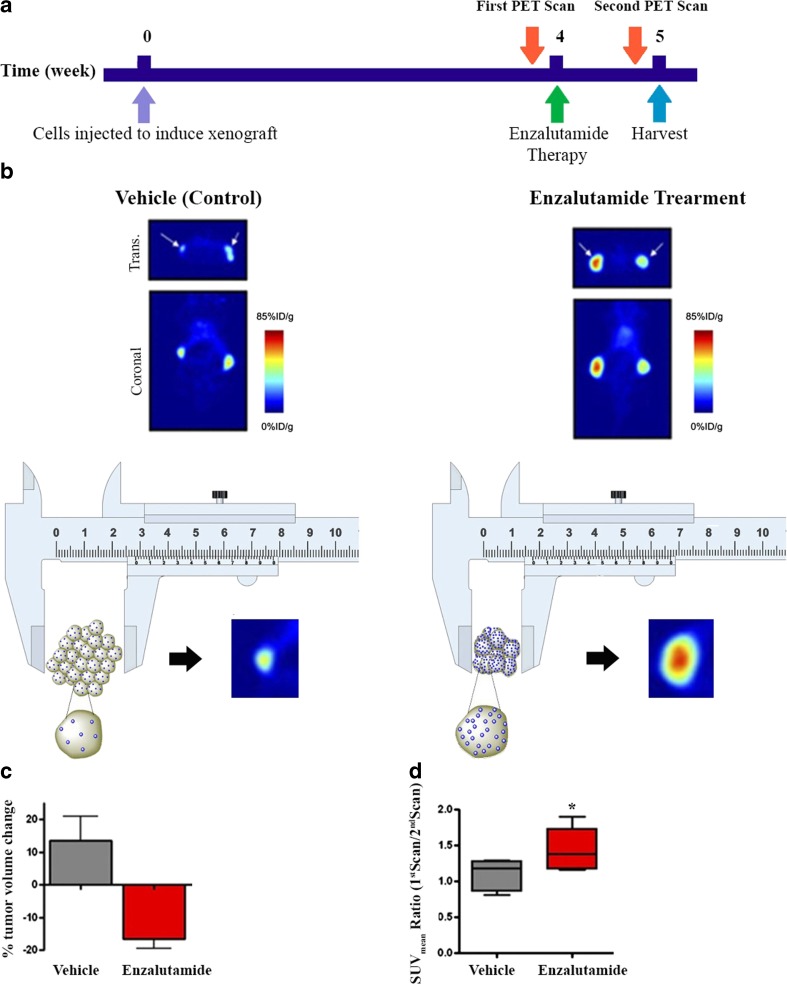
Antiandrogens as endoradiotherapy sensitizers
In 2011, Evans et al. [26] reported upregulation of PSMA expression as a result of ADT in a PCa animal model. They discovered that the AR is a prerequisite for androgen control of the expression of PSMA. Using 64Cu-J591 radiolabeled antibody, they presented that ADT either by castration of mice or via treatment with enzalutamide increases 64Cu-J591 uptake in xenografts of AR-positive and hormone-sensitive PCa cell lines including LNCaP and 22Rv1. However, exposing these androgen-sensitive cell lines to dihydrotestosterone (DHT) reduced the PSMA expression. Figure 2 illustrates the impact of enzalutamide therapy on both tumor volume and intratumoral uptake of 64Cu-J591. Figure 2b shows that 64Cu-J591 PET delineates increasing levels of PSMA expression in both LNCaP xenograft in the left thigh and 22Rv1 xenograft in the right thigh of male mice. It should be highlighted that as a result of enzalutamide therapy, the amount of PSMA per cell increased. However, the tumor size is reduced because of the inhibitory effect of enzalutamide. Therefore, uptake of the PSMA-imaging agent does not agree with tumor size measurements by caliper because the cells have been exposed to ADT (Fig. 2b, c, d).
Fig. 2.
Monitoring treatment response using caliper measurements versus PSMA-based imaging. (a) Experiment timeline; (b) PET scans 7 days after enzalutamide therapy (10 mg/kg) versus control group. (c) Percentage change in LNCaP xenografted tumor volumes. (d) The SUVmean ratio of the first PET scan (before ADT) to the second PET scan (after ADT). (Adapted and modified from Ref. [26] with permission)
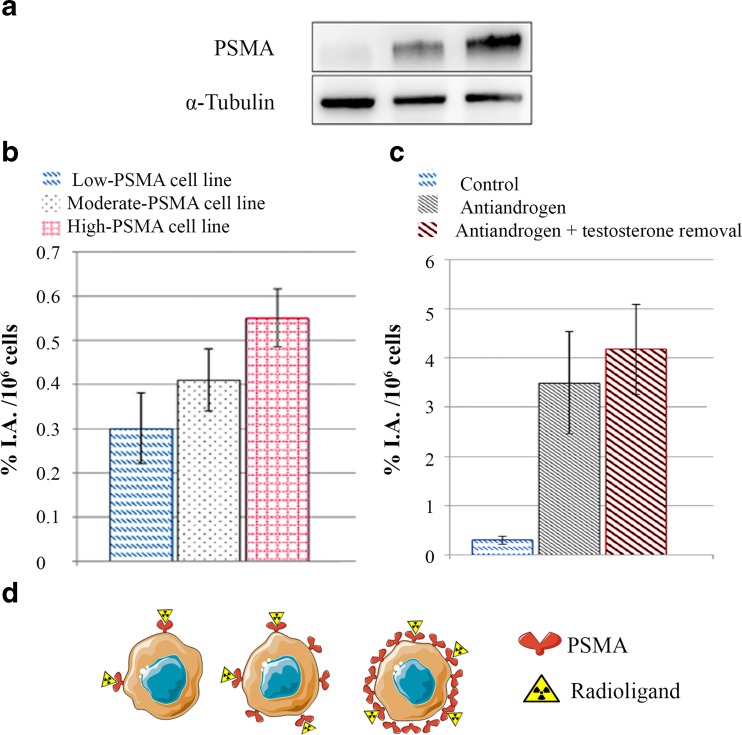
Recent data indicate that more expression of PSMA in PCa cells causes more PSMA radioligand uptake by the cells. In a very recent study, Meller et al.[29] examined binding of a 68Ga-labeled PSMA-HBED-CC to PCa cell lines to evaluate the association between alterations of PSMA expression using the antiandrogen abiraterone. They developed three different PCa model cell lines with different levels of PSMA expression. A low PSMA-expressing cell line was developed, and it was characterized with an androgen-sensitive phenotype. In addition, a high-PSMA-expressing cell line was established, and it represented the androgen-tolerant phenotype. Interestingly, a direct relationship between the level of the expression of PSMA and the uptake of PSMA radioligand was observed (Fig. 3a, b). Particularly, Fig. 3c shows that 2 days’ exposure of the androgen-sensitive phenotype model to abiraterone can significantly increase the uptake of PSMA radioligand (p < 0.001). In addition, Fig. 3d illustrates the schematics of the developed CRPC cell lines with diverse PSMA expression levels and their respective radioligand uptake. It seems that the higher level of PSMA leads to the higher capacity for radioligand uptake in a time-dependent manner.
Fig. 3.
Alteration of 68Ga-PSMA-HBED-CC uptake regarding the level of PSMA. (a) Levels of PSMA in three models of CRPC cell lines. (b) The uptake of 68Ga-PSMA-HBED-CC in different cell lines after 3 h incubation. (c) The alteration of 68Ga-PSMA-HBED-CC uptake in the low-PSMA-expressing model. (d) The schematics of the three CRPC models with different PSMA expression levels and their associated radioligand uptake. (Adapted and modified from Ref. [29])
In a very recent clinical pilot study using PSMA-targeted SPECT scans, Vallabhajosula et al. [13] monitored metastatic CRPC patients undergoing ADT. Interestingly, 2 weeks after ADT by either abiraterone or enzalutamide, the PSMA scans showed the same or more lesions with higher intensity compared to baseline. The observed higher intensity compared to baseline could be a result of upregulation of PSMA expression after ADT. However, after 12 weeks, there was a considerable reduction of the PSMA-ligand uptake in the lesions. The reported alteration in PSMA levels by Vallabhajosula et al. [13] is in accordance with the elaborated molecular biology of PSMA expression in this article.
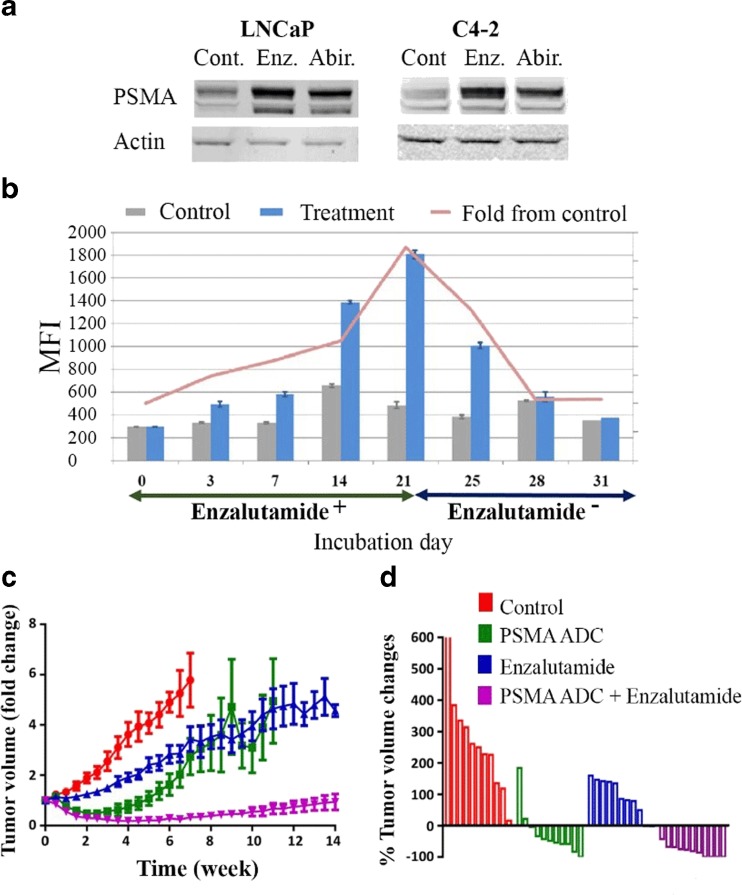
Antiandrogens as Chemosensitizers
Antibody–drug conjugates (ADCs) use the ability of monoclonal antibodies (mAbs) to specifically carry chemotherapeutic agents to malignant cells, and PSMA ADC is one of the members of this class of drugs for CRPC, which is in the clinical development state. PSMA ADC comprises a fully human IgG1 anti-PSMA mAb that is conjugated to the MMAE via a valine-citrulline (vc) linker [38]. In an in vitro study, Murga et al. [27] evaluated simultaneous application of PSMA ADC and two antiandrogens including enzalutamide and abiraterone. They documented the upregulation of PSMA in two PCa cell lines including the LNCaP and C4-2 cell lines (Fig. 4a). Interestingly, both enzalutamide and abiraterone in combination with PSMA ADC demonstrated a statistically significant synergistic antiproliferative effect on proliferation of PCa cell lines. The observed synergistic effect was related to some extent to increasing the expression of PSMA as a result of exposure of PCa cells to antiandrogens. Figure 4b illustrates that treatment with enzalutamide amplified PSMA expression gradually up to fourfold over 21 days, and the PSMA level returned to its baseline expression amount 7 days after treatment of cells with normal cell culture medium [27].
Fig. 4.
Antiandrogens could play the role of chemosensitizer. (a) The estimation of PSMA protein levels in LNCaP and C4-2 cell lines using the Western blot method. (b) Time course of PSMA expression in enzalutamide-treatedC4-2 cells. Vertical bars show mean fluorescence intensity (MFI) values, and the pink color line represents the fold increase in PSMA expression in treated cells relative to untreated cells. (Adapted from Ref. [27] with permission). (c) Tumor volume (fold change); (d) the percentage of tumor volume changes at 4 weeks. (Adapted from Ref. [28] with permission)
It is possible that we can take advantage of PSMA upregulation for improvement of PSMA ADC treatments. Recently, in an in vivo study using patient-derived xenografts, DiPippo et al. [28] represented that the combination of enzalutamide with PSMA ADC could be significantly advantageous over enzalutamide monotherapy. The developed animal model showed minor responses to enzalutamide therapy and then showed resistance to enzalutamide therapy. However, Fig. 4c and d demonstrates that the combination of PSMA ADC with enzalutamide displayed more noticeable tumor size shrinkage than monotherapies by either enzalutamide or via PSMA ADC. They also reported that a maximum level of PSMA expression was observed in the combinational therapy study group, which indicates a positive role of upregulation of PMSA for CRPC therapy.
Perspective
The final ADT outcome should be determined more by the biologic aggressiveness of the residual PCa tumor than by the volume. AR variant 7 (AR-V7) is an AR isoform and encodes a shortened AR protein without the C-terminal ligand-binding domain (LBD). AR-V7 needs no androgen for activation; it is constitutively active, and the expression of AR-V7 could be augmented up to 20-fold [39]. Because antiandrogens such as enzalutamide primarily interact with the LBD of AR, it is expected that AR-V7 without LBD causes resistance to ADT and increasing AR-V7 could be indicative of increasing aggressiveness of PCa [40, 41]. The reported data by DiPippo et al. [28] represented that the combination of enzalutamide with PSMA ADC could significantly reduce AR-V7 expression, which means the residual PCa tumor is more susceptible. However, Meller et al. [29] reported two different trends in levels of AR-V7 after treatment of their models with abiraterone. In their low-PSMA-expressing model, ADT had no impact on the level of AR-V7, while in their moderate-PSMA-expressing model, PSMA and AR-V7 were increased with the same trend. It can be inferred that PSMA-targeted therapy with prior pre-targeting by antiandrogens in some models leads to the formation of tumors with a higher level of AR-V7 in the residual PCa tumor. Therefore, for clinical application of this method, we should monitor the level of AR-V7 in response to antiandrogen therapy to avoid formation of more aggressive tumors.
An increasing number of publications are now discussing the potential diagnostic usefulness of the new class of PSMA-targeted imaging such as 68Ga-PSMA-11 [14–17] and PSMA-DKFZ-617 [18–20]. However, currently these promising classes of radiopharmaceuticals are facing four main challenges, including: (1) non-specific binding uptake in salivary glands and lacrimal glands, liver, spleen and intestines [42]; (2) false-negative outcomes in PSMA-negative PCa, small size tumors and tumors situated close to areas with a high physiologic tracer uptake [43]; (3) false-positive results in the celiac ganglia [44, 45]; (4) according to the issues discussed in this review, a false-positive outcome after antiandrogen treatment, particularly in hormone-naïve patients, is predictable.
The renal uptake of therapeutic PSMA-targeted agents is a restrictive factor [46]. Some of the proposed solutions for decreasing off-target radiation to the kidneys include the small-molecule PSMA inhibitor comedication [47], the application of polyethylene glycol (PEG) polymer chains [48] and using the nanoparticle-based platforms [49, 50]. However, it should be highlighted that non-target expression of PSMA is fortunately 100- to 1000-fold less than baseline expression in most adenocarcinomas of the prostate gland. Therefore, PSMA-targeted therapy with prior pre-targeting by antiandrogens cannot considerably increase non-specific uptake. In addition, the hydrophobic patches within the molecules could be a reason for the observed considerable non-specific binding, and these patches may not be affected by antiandrogen treatment [47].
We anticipate that antiandrogens could play the role of endoradio-/chemosensitizers in CRPC management for both chemotherapy and internal radiation therapy using therapeutic radioisotopes. The significant upregulation in PSMA level in response to antiandrogens could be the main requirement and the most desirable characteristic for application of pre-targeting by antiandrogens [13, 26–29]. However, pre-clinical reports represent that that PSMA expression is not the only factor involved in treatment outcomes, and even increasing the endoradio-/chemotherapeutic payload to PCa cells cannot solely lead to higher responses [51]. Therefore, this emerging therapeutic approach is dependent on two factors including (1) the potential of PCa cells for the upregulation of the PSMA level after ADT and (2) the stability of the AR gene in response to ADT since the formed mutant AR and AR variants have the ability of independent translocation to the nucleus and DNA binding.
It should be noted that the level of baseline PSMA expression cannot predict the responsiveness of each model to this emerging therapeutic approach. For instance, the 22Rv1 cell line with a relatively low level of PSMA showed less alteration after enzalutamide treatment compared to the LNCaP cell line with high baseline PSMA expression (Fig. 2b) [26]. However, the low-PSMA-expressing model of Meller et al. [29] showed a maximum responsiveness to abiraterone treatment in comparison to both the moderate- and high-PSMA-expressing models. Similarly, sensitivity to androgens cannot be a predictor of PSMA alteration. For instance, both the LNCaP and C4-2 cell lines showed significant potential for modulation of their PSMA levels by antiandrogens while they have different levels of sensitivity to androgens. Therefore, the discovery of a potential predictive biomarker that can estimate the sensitivity of PSMA alteration to ADT seems essential.
Furthermore, Paximadis et al. [52] recently revealed that treatment of LNCaP cell lines with enzalutamide could lead to significant radiosensitization during exposure to external radiations with different doses. Therefore, the discussed radiosensitization capability of antiandrogen could be considered for both internal and external PCa radiation therapy.
Up to now, four radiopharmaceuticals including 18F-fluorodeoxyglucose (18F-FDG), 18F-fluoro-5-dihydrotestosterone (18F-FDHT) [53], 18F-FCH [54, 55] and 64Cu-J591 [26, 56] have been applied in the dose optimization evaluation of therapeutic pathways and assessment of the therapeutic efficacy of antiandrogen enzalutamide. However, according to Jadvar’s [57] review of the utility and limitations of 18F-FDG PET, the helpfulness of FDG PET in PCa is still evolving and FDG PET cannot be favorable in the detection of PCa in a relatively large portion of patients since FDG uptake in PCa is associated with tumor differentiation levels. Similarly, the described considerable upregulations in PSMA-ligand uptake after exposure to antiandrogens raise a question about the ability of PSMA-targeted imaging such as 68Ga-PSMA-11 [14–17] or PSMA-DKFZ-617 [18–20] for staging and response monitoring of patients undergoing treatment with antiandrogen-based drugs [26]. Therefore, we recommend the application of choline PET/CT and 18F-FDHT for antiandrogen drug development proposes.
A general trend of more PSMA expression and more ligand uptake throughout a variety of PSMA radioligands including labeled monoclonal antibodies such as ProstaScint® [58] and J591 [12, 26], nanobodies such as JVZ-007 [59], labeled small molecules such as 123I-MIP-1072 [60], 111In-PSMA I&T [61], 68Ga-labeled DOTA and [50] HBED-CC [26] has been reported. Therefore, because PSMA uptake is proportional to total PSMA protein levels, improving PSMA protein expression could improve the therapeutic efficacy of PSMA-ligand therapy.
Up to now, many research groups have suggested utilization of PSMA enhancer/promoter for application in gene therapy of PCa as a potential adjuvant therapy of CRPC [62–67]. PSMA enhancer has been an appealing candidate for expressing different cytotoxic genes accompanied by ADT since it exhibits a much higher activity at low levels or in the absence of androgens. For instance, Lee et al. [62] used PSMA enhancer to control viral E1A protein expression and achieve exclusive virus replication in the prostate. In addition, Ikegami et al. [64] suggested utilization of PSMA enhancer with Cre recombinase/LoxP system for gene therapy of PCa. Therefore, the discussed prognostic and therapeutic role of PSMA enhancer in this review could expand the role of this gene in oncology and nuclear medicine.
In the future, we might be able to use the PSMA upregulation as an adjunct to the management of PSMA-positive CRPC. However, prospective candidates for this approach should be selected based on their potential for the elevation of PSMA after ADT. According to the available literature, the PSMA-enhancer region is responsible for this alteration. Moreover, patinas with a mutant and shortened AR such as AR-7 cannot be appropriate candidates for this therapeutic approach since mutated ARs have the ability of DNA binding irrespective of the antiandrogen medication. Therefore, the use of PSMA ligand imaging to select those that are PSMA positive and are ready for PSMA ligand therapy after ADT, besides a quantitative reverse-transcriptase-polymerase-chain-reaction (PCR) assay to evaluate the PSMA-enhancer region and stability of the AR region, is essential for the selection of candidates and CRPC management.
Conclusion
Pre-targeting CRPC with second-generation antiandrogens could play a role of endoradio-/chemosensitizers in combination with the well-stablished PSMA-targeted methods because of the amplification of endoradio-/chemotherapeutic payload to PCa cells. In addition, in diagnostic PSMA-based scans a false-positive result after antiandrogen treatment, particularly in hormone-naïve patients, is predictable.
Compliance with Ethical Standards
Conflict of Interest
Martin K. Bakht, So Won Oh, Hyewon Youn, Gi jeong Cheon, Cheol Kwak and Keon Wook Kang declare that they have no conflict of interest.
Ethical Statement
This article does not contain any studies with human participants or animals performed by any of the authors. The manuscript has not been published before, is not under consideration for publication anywhere else and has been approved by all co-authors.
References
- 1.Haas GP, Delongchamps N, Brawley OW, Wang CY, de la Roza G. The worldwide epidemiology of prostate cancer: perspectives from autopsy studies. Can J Urol. 2008;15:3866–71. [PMC free article] [PubMed] [Google Scholar]
- 2.Perner S, Cronauer MV, Schrader AJ, Klocker H, Culig Z, Baniahmad A. Adaptive responses of androgen receptor signaling in castration-resistant prostate cancer. Oncotarget. 2015;29:35542–55. doi: 10.18632/oncotarget.4689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chandrasekar T, Yang JC, Gao AC, Evans CP. Targeting molecular resistance in castration-resistant prostate cancer. BMC Med. 2015 doi: 10.1186/s12916-015-0457-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Heidenreich A, Bastian PJ, Bellmunt J, Bolla M, Joniau S, van der Kwast T, et al. EAU guidelines on prostate cancer. Part II: Treatment of advanced, relapsing, and castration-resistant prostate cancer. Eur Urol. 2014;65:467–79. doi: 10.1016/j.eururo.2013.11.002. [DOI] [PubMed] [Google Scholar]
- 5.Kiess AP, Banerjee SR, Mease RC, Rowe SP, Rao A, Foss CA, et al. Prostate-specific membrane antigen as a target for cancer imaging and therapy. Q J Nucl Med Mol Imaging. 2015;59:241–68. [PMC free article] [PubMed] [Google Scholar]
- 6.Rai BP, Baum R, Patel A, Hughes R, Alonzi R, Lane T, et al. The role PET with 68Gallium (Ga)-labelled prostate-specific membrane antigen (PSMA) in the management of patient with organ confined and locally advanced prostate cancer prior to radical treatment and after radical prostatectomy. Urology. 2016 doi: 10.1016/j.urology.2015.12.048. [DOI] [PubMed] [Google Scholar]
- 7.Ananias HJ, van den Heuvel MC, Helfrich W, de Jong IJ. Expression of the gastrin‐releasing peptide receptor, the prostate stem cell antigen and the prostate‐specific membrane antigen in lymph node and bone metastases of prostate cancer. Prostate. 2009;69:1101–8. doi: 10.1002/pros.20957. [DOI] [PubMed] [Google Scholar]
- 8.Minner S, Wittmer C, Graefen M, Salomon G, Steuber T, Haese A, et al. High level PSMA expression is associated with early PSA recurrence in surgically treated prostate cancer. Prostate. 2011;71:281–8. doi: 10.1002/pros.21241. [DOI] [PubMed] [Google Scholar]
- 9.Rybalov M, Ananias HJ, Hoving HD, van der Poel HG, Rosati S, de Jong IJ. PSMA, EpCAM, VEGF and GRPR as imaging targets in locally recurrent prostate cancer after radiotherapy. Int J Mol Sci. 2014;15:6046–61. doi: 10.3390/ijms15046046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Akhtar NH, Pail O, Saran A, Tyrell L, Tagawa ST. Prostate-specific membrane antigen-based therapeutics. Adv Urol. 2011 doi: 10.1155/2012/973820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lutje S, Heskamp S, Cornelissen AS, Poeppel TD, van den Broek SA, Rosenbaum-Krumme S, et al. PSMA ligands for radionuclide imaging and therapy of prostate cancer: clinical status. Theranostics. 2015;5:1388–401. doi: 10.7150/thno.13348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vargas H, Grimm J, Donati FO, Sala E, Hricak H. Molecular imaging of prostate cancer: translating molecular biology approaches into the clinical realm. Eur Radiol. 2015;25:1294–302. doi: 10.1007/s00330-014-3539-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vallabhajosula S, Jhanwar Y, Tagawa S, Epstein J, Babich J, Youn T, et al. 99m Tc-MIP-1404 Planar and SPECT scan: Imaging biomarker of androgen receptor (AR) signaling and prostate specific membrane antigen (PSMA) expression. J Nucl Med 2016:57:1541–1.
- 14.Giesel FL, Fiedler H, Stefanova M, Sterzing F, Rius M, Kopka K, et al. PSMA PET/CT with Glu-urea-Lys-(Ahx)-[68Ga(HBED-CC)] versus 3D CT volumetric lymph node assessment in recurrent prostate cancer. Eur J Nucl Med Mol Imaging. 2015;42:1794–800. doi: 10.1007/s00259-015-3106-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Afshar-Oromieh A, Avtzi E, Giesel FL, Holland-Letz T, Linhart HG, Eder M, et al. The diagnostic value of PET/CT imaging with the (68)Ga-labelled PSMA ligand HBED-CC in the diagnosis of recurrent prostate cancer. Eur J Nucl Med Mol Imaging. 2015;42:197–209. doi: 10.1007/s00259-014-2949-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ebenhan T, Vorster M, Marjanovic-Painter B, Wagener J, Suthiram J, Modiselle M, et al. Development of a single vial kit solution for radiolabeling of 68Ga-DKFZ-PSMA-11 and its performance in prostate cancer patients. Molecules. 2015;20:14860–78. doi: 10.3390/molecules200814860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sterzing F, Kratochwil C, Fiedler H, Katayama S, Habl G, Kopka K, et al. (68)Ga-PSMA-11 PET/CT: a new technique with high potential for the radiotherapeutic management of prostate cancer patients. Eur J Nucl Med Mol Imaging. 2016;43:34–41. doi: 10.1007/s00259-015-3188-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kratochwil C, Giesel FL, Eder M, Afshar-Oromieh A, Benešová M, Mier W, et al. [177Lu] Lutetium-labelled PSMA ligand-induced remission in a patient with metastatic prostate cancer. Eur J Nucl Med Mol Imaging. 2015;42(6):987–8. doi: 10.1007/s00259-014-2978-1. [DOI] [PubMed] [Google Scholar]
- 19.Afshar-Oromieh A, Hetzheim H, Kratochwil C, Benesova M, Eder M, Neels OC, et al. The theranostic PSMA ligand PSMA-617 in the diagnosis of prostate cancer by PET/CT: biodistribution in humans, radiation dosimetry, and first evaluation of tumor lesions. J Nucl Med. 2015;56:1697–705. doi: 10.2967/jnumed.115.161299. [DOI] [PubMed] [Google Scholar]
- 20.Delker A, Fendler WP, Kratochwil C, Brunegraf A, Gosewisch A, Gildehaus FJ, et al. Dosimetry for 177Lu-DKFZ-PSMA-617: a new radiopharmaceutical for the treatment of metastatic prostate cancer. Eur J Nucl Med Mol Imaging. 2016;43:42–51. doi: 10.1007/s00259-015-3174-7. [DOI] [PubMed] [Google Scholar]
- 21.Szabo Z, Mena E, Rowe SP, Plyku D, Nidal R, Eisenberger MA, et al. Initial evaluation of [(18)F]DCFPyL for prostate-specific membrane antigen (PSMA)-targeted PET imaging of prostate cancer. Mol Imaging Biol. 2015;17:565–74. doi: 10.1007/s11307-015-0850-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Herrmann K, Bluemel C, Weineisen M, Schottelius M, Wester HJ, Czernin J, et al. Biodistribution and radiation dosimetry for a novel probe targeting prostate specific membrane antigen for Imaging and Therapy (68Ga-PSMA I&T) J Nucl Med. 2015;56:855–61. doi: 10.2967/jnumed.115.156133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Freitag MT, Radtke JP, Hadaschik BA, Kopp-Schneider A, Eder M, Kopka K, et al. Comparison of hybrid 68Ga-PSMA PET/MRI and 68Ga-PSMA PET/CT in the evaluation of lymph node and bone metastases of prostate cancer. Eur J Nucl Med Mol Imaging. 2016;43:70–83. doi: 10.1007/s00259-015-3206-3. [DOI] [PubMed] [Google Scholar]
- 24.Ploussard G, Almeras C, Briganti A, Giannarini G, Hennequin C, Ost P, et al. Management of node only recurrence after primary local treatment for prostate cancer: a systematic review of the literature. J Urol. 2015;194:983–8. doi: 10.1016/j.juro.2015.04.103. [DOI] [PubMed] [Google Scholar]
- 25.Dost RJ, Glaudemans AW, Breeuwsma AJ, de Jong IJ. Influence of androgen deprivation therapy on choline PET/CT in recurrent prostate cancer. Eur J Nucl Med Mol Imaging. 2013;40:41–7. doi: 10.1007/s00259-013-2398-7. [DOI] [PubMed] [Google Scholar]
- 26.Evans MJ, Smith-Jones PM, Wongvipat J, Navarro V, Kim S, Bander NH, et al. Noninvasive measurement of androgen receptor signaling with a positron-emitting radiopharmaceutical that targets prostate-specific membrane antigen. Proc Natl Acad Sci U S A. 2011;108:9578–82. doi: 10.1073/pnas.1106383108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Murga JD, Moorji SM, Han AQ, Magargal WW, DiPippo VA, Olson WC. Synergistic co-targeting of prostate-specific membrane antigen and androgen receptor in prostate cancer. Prostate. 2015;75:242–54. doi: 10.1002/pros.22910. [DOI] [PubMed] [Google Scholar]
- 28.DiPippo VA, Nguyen HM, Brown LG, Olson WC, Vessella RL, Corey E. Addition of PSMA ADC to enzalutamide therapy significantly improves survival in in vivo model of castration resistant prostate cancer. Prostate. 2016;76:325–34. doi: 10.1002/pros.23124. [DOI] [PubMed] [Google Scholar]
- 29.Meller B, Bremmer F, Sahlmann C, Hijazi S, Bouter C, Trojan L, et al. Alterations in androgen deprivation enhanced prostate-specific membrane antigen (PSMA) expression in prostate cancer cells as a target for diagnostics and therapy. EJNMMI Res. 2015;5:1–11. doi: 10.1186/s13550-015-0145-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.O’Keefe DS, Su SL, Bacich DJ, Horiguchi Y, Luo Y, Powell CT, et al. Mapping, genomic organization and promoter analysis of the human prostate-specific membrane antigen gene. Biochim Biophys Acta. 1998;1443:113–27. doi: 10.1016/S0167-4781(98)00200-0. [DOI] [PubMed] [Google Scholar]
- 31.Chang SS. Overview of prostate-specific membrane antigen. Rev Urol. 2004;6:S13–8. [PMC free article] [PubMed] [Google Scholar]
- 32.Israeli RS, Powell CT, Corr JG, Fair WR, Heston WD. Expression of the prostate-specific membrane antigen. Cancer Res. 1994;54:1807–11. [PubMed] [Google Scholar]
- 33.Wright GL, Grob BM, Haley C, Grossman K, Newhall K, Petrylak D, et al. Upregulation of prostate-specific membrane antigen after androgen-deprivation therapy. Urol. 1996;48:326–34. doi: 10.1016/S0090-4295(96)00184-7. [DOI] [PubMed] [Google Scholar]
- 34.Good D, Schwarzenberger P, Eastham JA, Rhoads RE, Hunt JD, Collins M, et al. Cloning and characterization of the prostate-specific membrane antigen promoter. J Cell Biochem. 1999;74:395–405. doi: 10.1002/(SICI)1097-4644(19990901)74:3<395::AID-JCB8>3.0.CO;2-0. [DOI] [PubMed] [Google Scholar]
- 35.Watt F, Martorana A, Brookes DE, Ho T, Kingsley E, O’Keefe DS, et al. A tissue-specific enhancer of the prostate-specific membrane antigen gene, FOLH1. Genomics. 2001;73:243–54. doi: 10.1006/geno.2000.6446. [DOI] [PubMed] [Google Scholar]
- 36.Noss KR, Wolfe SA, Grimes SR. Upregulation of prostate specific membrane antigen/folate hydrolase transcription by an enhancer. Gene. 2002;285:247–56. doi: 10.1016/S0378-1119(02)00397-9. [DOI] [PubMed] [Google Scholar]
- 37.Yu J, Yu J, Mani RS, Cao Q, Brenner CJ, Cao X, et al. An integrated network of androgen receptor, polycomb, and TMPRSS2-ERG gene fusions in prostate cancer progression. Cancer Cell. 2010;17:443–54. doi: 10.1016/j.ccr.2010.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.DiPippo VA, Nguyen HM, Brown LG, Olson WC, Vessella RL, Corey E. In vivo efficacy of PSMA ADC in combination with enzalutamide in castration-resistant prostate cancer. Cancer Res. 2015;75:1685. doi: 10.1158/1538-7445.AM2015-1685. [DOI] [Google Scholar]
- 39.Haile S, Sadar MD. Androgen receptor and its splice variants in prostate cancer. Cell Mol Life Sci. 2011;68:3971–81. doi: 10.1007/s00018-011-0766-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ammannagari N, George S. Anti-androgen therapies for prostate cancer: a focused review. Am J Hema Oncl. 2015;11:15–9. [Google Scholar]
- 41.Antonarakis ES, Lu C, Wang H, Luber B, Nakazawa M, Roeser JC, et al. AR-V7 and resistance to enzalutamide and abiraterone in prostate cancer. N Engl J Med. 2014;371:1028–38. doi: 10.1056/NEJMoa1315815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Afshar-Oromieh A, Malcher A, Eder M, Eisenhut M, Linhart H, Hadaschik B, et al. PET imaging with a [68Ga] gallium-labelled PSMA ligand for the diagnosis of prostate cancer: biodistribution in humans and first evaluation of tumour lesions. Eur J Nucl Med Mol Imaging. 2013;40:486–95. doi: 10.1007/s00259-012-2298-2. [DOI] [PubMed] [Google Scholar]
- 43.Chakraborty PS, Tripathi M, Agarwal KK, Kumar R, Vijay MK, Bal C. Metastatic poorly differentiated prostatic carcinoma with neuroendocrine differentiation: negative on 68Ga-PSMA PET/CT. Clin Nucl Med. 2015;40:163–6. doi: 10.1097/RLU.0000000000000594. [DOI] [PubMed] [Google Scholar]
- 44.Jadvar H. PSMA PET, in prostate cancer. J Nucl Med. 2015;56:1131–2. doi: 10.2967/jnumed.115.157339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Krohn T, Verburg FA, Pufe T, Neuhuber W, Vogg A, Heinzel A, et al. [68Ga] PSMA-HBED uptake mimicking lymph node metastasis in coeliac ganglia: an important pitfall in clinical practice. Eur J Nucl Med Mol Imaging. 2015;42:210–4. doi: 10.1007/s00259-014-2915-3. [DOI] [PubMed] [Google Scholar]
- 46.Weineisen M, Schottelius M, Simecek J, Baum RP, Yildiz A, Beykan S, et al. 68Ga-and 177Lu-labeled PSMA I&T: optimization of a PSMA-targeted theranostic concept and first proof-of-concept human studies. J Nucl Med. 2015;56:1169–76. doi: 10.2967/jnumed.115.158550. [DOI] [PubMed] [Google Scholar]
- 47.Kratochwil C, Giesel FL, Leotta K, Eder M, Hoppe-Tich T, Youssoufian H, et al. PMPA for nephroprotection in PSMA-targeted radionuclide therapy of prostate cancer. J Nucl Med. 2015;56:293–8. doi: 10.2967/jnumed.114.147181. [DOI] [PubMed] [Google Scholar]
- 48.Wilbur DS, Chyan M-K, Hamlin D, Balkin E. In vivo comparison of two anti-PSMA mAb Fab’ conjugates containing branched-chain PEG derivatives with Fab’ and F(ab’)2. J Nucl Med. 2012;53:1545. [Google Scholar]
- 49.Behnam Azad B, Banerjee SR, Pullambhatla M, Lacerda S, Foss CA, Wang Y, et al. Evaluation of a PSMA-targeted BNF nanoparticle construct. Nanoscale. 2015;7:4432–42. doi: 10.1039/C4NR06069E. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Moon S-H, Yang BY, Kim YJ, Hong MK, Lee Y-S, Lee DS, et al. Development of a complementary PET/MR dual-modal imaging probe for targeting prostate-specific membrane antigen (PSMA) Nanomed Nanotech Biol Med. 2016;12:871–9. doi: 10.1016/j.nano.2015.12.368. [DOI] [PubMed] [Google Scholar]
- 51.DiPippo VA, Olson WC, Nguyen HM, Brown LG, Vessella RL, Corey E. Efficacy studies of an antibody‐drug conjugate PSMA‐ADC in patient‐derived prostate cancer xenografts. Prostate. 2015;75:303–13. doi: 10.1002/pros.22916. [DOI] [PubMed] [Google Scholar]
- 52.Paximadis P, Najy AJ, Snyder M, Kim HR. The interaction between androgen receptor and PDGF-D in the radiation response of prostate carcinoma. Prostate. 2016;76:534–43. doi: 10.1002/pros.23135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Scher HI, Beer TM, Higano CS, Anand A, Taplin ME, Efstathiou E, et al. Antitumour activity of MDV3100 in castration-resistant prostate cancer: a phase 1–2 study. Lancet. 2010;375:1437–46. doi: 10.1016/S0140-6736(10)60172-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Caffo O, Maines F, Donner D, Veccia A, Chierichetti F, Galligioni E. Impact of enzalutamide administration on primary prostate cancer volume: a metabolic evaluation by choline positron emission tomography in castration-resistant prostate cancer patients. Clin Genitourin Cancer. 2014;12:312–6. doi: 10.1016/j.clgc.2014.03.004. [DOI] [PubMed] [Google Scholar]
- 55.De Giorgi U, Caroli P, Scarpi E, Conteduca V, Burgio S, Menna C, et al. 18F-Fluorocholine PET/CT for early response assessment in patients with metastatic castration-resistant prostate cancer treated with enzalutamide. Eur J Nucl Med Mol Imaging. 2015;42:1276–83. doi: 10.1007/s00259-015-3042-5. [DOI] [PubMed] [Google Scholar]
- 56.Evans MJ. Measuring oncogenic signaling pathways in cancer with PET: an emerging paradigm from studies in castration-resistant prostate cancer. Cancer Discov. 2012;2:985–4. doi: 10.1158/2159-8290.CD-12-0178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Jadvar H. Imaging evaluation of prostate cancer with 18F-fluorodeoxyglucose PET/CT: utility and limitations. Eur J Nucl Med Mol Imaging. 2013;40:5–10. doi: 10.1007/s00259-013-2361-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Tolmachev V, Malmberg J, Estrada S, Eriksson O, Orlova A. Development of a 124I-labeled version of the anti-PSMA monoclonal antibody capromab for immunoPET staging of prostate cancer: Aspects of labeling chemistry and biodistribution. Int J Oncol. 2014;44:1998–2008. doi: 10.3892/ijo.2014.2376. [DOI] [PubMed] [Google Scholar]
- 59.Chatalic KL, Veldhoven-Zweistra J, Bolkestein M, Hoeben S, Koning GA, Boerman OC, et al. A Novel 111In-Labeled Anti–Prostate-Specific Membrane Antigen Nanobody for Targeted SPECT/CT Imaging of Prostate Cancer. J Nucl Med. 2015;56:1094–9. doi: 10.2967/jnumed.115.156729. [DOI] [PubMed] [Google Scholar]
- 60.Hillier SM, Kern AM, Maresca KP, Marquis JC, Eckelman WC, Joyal JL, et al. 123I-MIP-1072, a small-molecule inhibitor of prostate-specific membrane antigen, is effective at monitoring tumor response to taxane therapy. J Nucl Med. 2011;52:1087–93. doi: 10.2967/jnumed.110.086751. [DOI] [PubMed] [Google Scholar]
- 61.Chatalic KS, Heskamp S, Konijnenberg M, Molkenboer-Kuenen JM, Franssen GM, Clahsen-van Groningen MC, et al. Towards personalized treatment of prostate cancer: PSMA I&T, a promising prostate-specific membrane antigen-targeted theranostic agent. Theranostics. 2016;6:849–61. doi: 10.7150/thno.14744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Lee SJ, Zhang Y, Lee SD, Jung C, Li X, Kim HS, et al. Targeting prostate cancer with conditionally replicative adenovirus using PSMA enhancer. Mol Ther. 2004;10:1051–8. doi: 10.1016/j.ymthe.2004.08.028. [DOI] [PubMed] [Google Scholar]
- 63.Cheng WS, Kraaij R, Nilsson B, van der Weel L, de Ridder CM, Tötterman TH, et al. A novel TARP-promoter-based adenovirus against hormone-dependent and hormone-refractory prostate cancer. Mol Ther. 2004;10:355–64. doi: 10.1016/j.ymthe.2004.05.022. [DOI] [PubMed] [Google Scholar]
- 64.Ikegami S, Tadakuma T, Suzuki S, Yoshimura I, Asano T, Hayakawa M. Development of gene therapy using prostate‐specific membrane antigen promoter/enhancer with Cre recombinase/LoxP system for prostate cancer cells under androgen ablation condition. Jap J Cancer Res. 2002;93:1154–63. doi: 10.1111/j.1349-7006.2002.tb01218.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Zhao W, Xu Y, Kong D, Liu R, Zhang Z, Jin C, et al. Tissue-selective RNA interference in prostate cancer cell using prostate specific membrane antigen promoter/enhancer. Urol Oncol. 2009;27:539–66. doi: 10.1016/j.urolonc.2008.05.003. [DOI] [PubMed] [Google Scholar]
- 66.Zhao FJ, Zhang S, Yu ZM, Xia SJ, Li H. Specific targeting of prostate cancer cells in vitro by the suicide gene/prodrug system, uracil phosphoribosylltransferase/5-fluorouracil, under the control of prostate-specific membrane antigen promoter/enhancer. Prostate Cancer Prostatic Dis. 2009;12:166–71. doi: 10.1038/pcan.2008.39. [DOI] [PubMed] [Google Scholar]
- 67.Zeng H, Wei Q, Huang R, Chen N, Dong Q, Yang Y, et al. Recombinant adenovirus mediated prostate‐specific enzyme pro‐drug gene therapy regulated by prostate‐specific membrane antigen (PSMA) enhancer/promoter. J Androl. 2007;28:827–35. doi: 10.2164/jandrol.107.002519. [DOI] [PubMed] [Google Scholar]