Abstract
A gene therapeutic approach to treat osteoarthritis (OA) appears to be on the horizon for millions of people who suffer from this disease. Previously we described optimization of a scAAVIL-1ra gene therapeutic vector and initially tested this in an equine model verifying long-term intrasynovial IL-1ra protein at therapeutic levels. Using this vector, we carried out a dosing trial in six horses to verify protein levels and establish a dose that would express relevant levels of therapeutic protein for extended periods of time (8 months). A novel arthroscopic procedure used to detect green fluorescence protein (GFP) fluorescence intrasynovially confirmed successful transduction of the scAAVGFP vector in both the synovial and cartilage tissues. No evidence of intra-articular toxicity was detected. Immune responses to vector revealed development of neutralizing antibodies (Nabs) within 2 weeks of administration, which persisted for the duration of the study but did not lower protein expression intra-articularly. Re-dosing with a different serotype to attain therapeutic levels of protein confirmed establishment of successful transduction. This is the first study in an equine model to establish a dosing/redosing protocol, as well as examine the Nab response to capsid and supports further clinical investigation to determine the clinical efficacy of scAAVIL-1ra to treat OA.
INTRODUCTION
Osteoarthritis (OA) continues to plague both the aging as well as active younger generations around the world. Current drug therapies that exist have mainly symptom-modifying effects and consist of analgesics, nonsteroidal anti-inflammatory drugs, glucosamine and chondroitin sulfate, and intra-articular injections of corticosteroids or hyaluronan.1,2 Disease-modifying effects of corticosteroids and/or corticosteroids combined with hyaluronan have been reported in animal studies,3,4 but in humans the efficacy remains controversial as this treatment is known to be short-acting, prone to potential detrimental cartilage changes and has questionable effects on modifying the course of OA.5,6
One specific disease-modifying drug that has shown promise is interleukin receptor antagonist protein (IL-1ra).7–10 IL-1ra is a naturally occurring inhibitor, which, through its binding ability to the IL-1β receptor, inhibits the catabolic cytokine IL-1β.11 IL-1β is considered to be one of the most important pro-inflammatory cytokines in inflamed joints.12 A myriad of publications have revealed significant correlations of increased levels of IL-1β with biochemical and histologic evidence of OA.12–17 There have also been incremental increases of the IL-1ra/IL-β ratios associated with escalating grades of OA.15 Chondrocytes are the major cellular targets of IL-1β and have been found to have more receptors for IL-1β in sites of osteoarthritic cartilage compared with OA cartilage.12 There continues to be mounting clinical evidence that proves efficacy of products containing high levels of IL-1ra especially in the high motion joints that have the highest occurrence of OA such as the hip and the knee.9,10,18
Gene delivery of various therapeutic genes for arthritis is now well-established.19,20 Adeno-associated virus (AAV) has repeatedly been found to deliver long-term protein production with minimal detrimental effects to the joint tissues compared with the other viral vectors.21 Early studies utilized single stranded AAV with good success; however, with the development of self complementary AAV (scAAV), higher levels of protein could be produced more quickly (1 week with double stranded compared with 3–4 weeks with single stranded) suggesting that this vector is the preferred choice with respect to gene therapy trials.22
Although proof-of-principle was established for arthritis gene therapy using retro and adenoviral vectors to deliver anti-catabolic and anabolic vectors to treat OA, we and others pursued more efficient, enhanced production through testing of various AAV (2 and 2.5) serotypes both in vitro and in vivo, which revealed superior efficiency.22–26 Further, specific genetic alterations of the therapeutic transgene such as codon optimization as well as testing various promoters in joint tissues, revealed that the scAAVoptimizedequineIL-1ra vector produced significant and therapeutic protein production within the middle carpal and metacarpophalangeal joints of horses.24 Horses have now been used for decades as animal models to mimic osteoarthritic conditions of human joint disease and are considered a highly relevant animal model due to the size of their joints, the thickness of their cartilage and the character of their subchondral bone.27,28 Thus, we further pursued a scAAVIL-1ra dosing protocol to determine proper dosing of vector genomes to be injected into joints that have similar size and synovial volumes to the human knee. Proper dosing of scAAVIL-1ra is important as the efficacy of IL-1ra gene therapy is determined by levels of the protein in relation to levels of IL-1β.15 Conversely, the cost of vector can be prohibitive to realistic expectations of instituting this therapy in clinical patients. Further, we sought to determine whether intra-articular tissues within our horses maintained tissue transduction and protein expression by using a green fluorescence protein (GFP) encoding transgene to track protein production for up to 240 days post injection.
It has also been well-established that neutralizing antibodies (Nabs) are produced in response to AAV-mediated gene transfer.29–33 The role of Nabs is important both to establish the effects from a single intra-articular injection as well as the ability to re-inject either the same serotype vector or perhaps another serotype to ‘augment’ diminishing levels or levels that never reached therapeutic efficacy. Our objectives of this study were four fold: (1) establishment of vector dose of scAAV2equineoptIL-1ra in an equine joint that will produce therapeutic levels of protein (10–400 ng ml−1); (2) determination of longevity and location of protein expression following one injection of an optimal dose; (3) determine the NAb response to the dose administered and; (4) assess whether re-injection of an alternative serotype of AAV would result in augmented production of therapeutic levels of the IL-1ra protein in the presence of nAb levels persisting for the length of the study. Our hypotheses based on our preliminary horse study were: (1) one of the three doses tested would result in sustained therapeutic levels (10–400 ng ml−1) of protein for the duration of study (8 months); (2) the location of protein production would be only within the target tissue and most prevalent in chondrocytes verses synoviocytes as tracked using a GFP marker gene and a novel in situ arthroscopic imaging system; (3) the Nab response would occur following injection of three different doses and (4) if Nab responses persisted, injection of an alternative serotype would result in a ‘rebound’ of therapeutic protein production.
RESULTS
Intra-articular measurement of IL-1ra levels according to dose and time
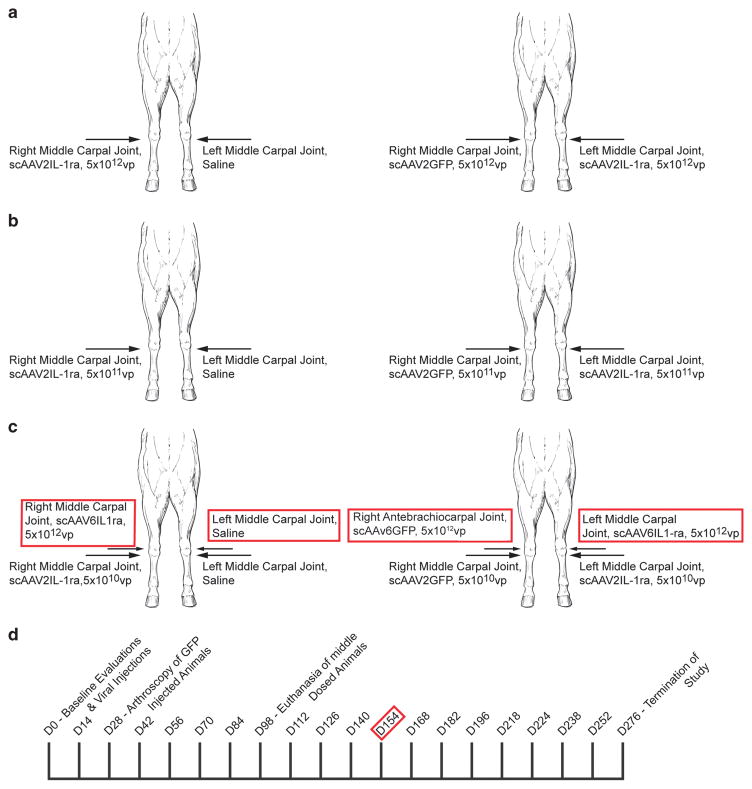
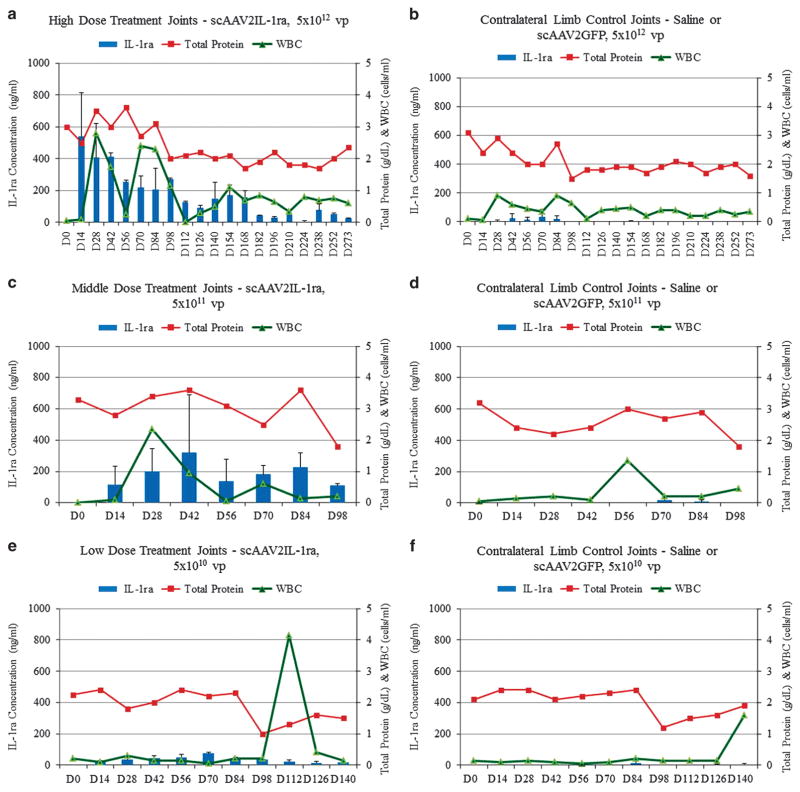
Six mature horses were dosed in the middle carpal space with scAAVIL-1ra, scAAV2GFP or saline (Figure 1). Enzyme-linked immunosorbent assay (ELISA) measurement of intra-articular protein levels revealed minimal to no IL-1ra at baseline (Day 0) for all horses (Figure 2). Fourteen days following injection, which was also the first day of synovial fluid collection, high (5 × 1012) dosed joints revealed a robust increase in IL-1ra levels of 537ng ml−1 (±195 ng ml−1 = s.d. between joints). The level of IL-1ra protein fluctuated but consistently remained between an average of 200 and 550 ng ml −1 for 98 days in the joints receiving the highest dose. Past 168 days, levels of IL-1ra gradually decreased over time but remained detectable for the duration of the study (D276). Middle dosed horses (5 × 1011) had an average of between 100 and 300 ng ml −1, an average 1.5-fold lower amount of IL-1ra concentrations in the synovial fluid than the high dosed horses. These horses were euthanized at Day 98. Low (5 × 1010) dosed horses had 10–80 ng ml −1 levels of IL-1ra in the synovial fluid, which was an average of 2.9-fold lower amount than levels of IL-1ra of the middle dosed horses. Levels of IL-1ra for the lowest dosed horses were barely detectable at Day 154, the date chosen just before redosing occurred. Re-dosing was carried out only in the low dosed horses in these studies to mimic the clinical scenario of inadequate amounts of protein produced from the first vector injection and the need to elevate those levels.
Figure 1.
Middle carpal joints were injected with saline, scAAV2GFP, scAAV6GFP, scAAV2IL-1ra and/or scAAV6IL-1ra as illustrated in panels a–c. Panel a represents the high dosed horses and the dosage of vector (or saline) and joint injected. Panel b represents the middle dosed horses and the dosage of vector (or saline) and joint injected. Panel c represents the low dosed horses and the dosage of vector (or saline) and joint injected. The red-bordered text represents what was injected on Day 154. The right antebrachiocarpal (verses the middle carpal) joint was injected with scAAV6GFP so that transduction could be determined from that particular vector and not be confused with previous GFP transduction from middle carpal joint injection. Panel d represents the time at which animals were dosed and/or redosed (red border), arthroscopically assessed and euthanized. Synovial fluid samples were collected for analysis at each time point listed.
Figure 2.
(a–f) Mean IL-1ra (ng ml−1) (left axis), total protein (g dl−1) and WBC (cells per μl) (right axis) levels in high dosed, middle dosed, low dosed and contralateral control limb synovial fluid samples (n =2). S.d. is shown for IL-1ra levels only. Time frames differ (x-axis) because the middle dosed animals were euthanized at Day 98 and the low dosed animals were given a second administration of virus at Day 154 (therefore x-axis extends up until the last time point before the second injection). High dosed joints produced an average between 200 and 550 ng ml−1 up to day 98 and then between 20 and 200 ng ml−1 thereafter. Middle dosed joints produced between an average of 100 and 300 ng ml−1 up to day 98, at which time those horses were terminated, and low dosed joints produced 10–80 ng ml−1 up to day 140, at which point they were redosed (x-axis only goes to last time point before re-injection). WBC and TP were not different between joints injected with scAAV2IL-1ra or scAAV2GFP or saline.
Contralateral joints (joints injected with saline or AAVGFP) in the high dosed horses had a mild increase in IL-1ra 28 days following injection and increased to an average of 38 ng ml −1 at day 70 and dropped to barely detectable at day 126 as described previously.24 Contralateral joints in horses receiving the middle or the low dose scAAV2IL-1ra had barely detectable levels of IL-1ra.
Synovial fluid white blood cell (WBC) counts and total protein (TP) levels ranged between 0.5 and 2 cells per ml and 1.5 and 3.5 g dl −1, respectively, for all joints close to the range of normal (0.5–2 g dl −1) (Figure 2). There were minimal differences in synovial fluid WBC counts (pre 2–3 g dl −1 and post 1–2 g dl −1) and TP between scAAV2IL-1ra injected joints and saline injected joints. An unexplained high data point was observed in one dosed horse at Day 112 in which the WBC count was 3.8–4 cells per ml.
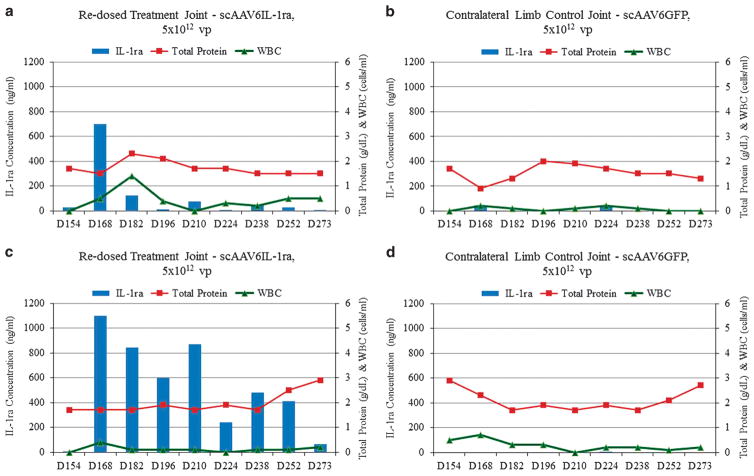
IL-1ra redosing in low dose joints
We sought to investigate whether synovial joints that were producing minimal to no IL-1ra protein due to a low dose administration would produce augmented levels of IL-1ra following a re-injection of the high dose (5 × 1012) alternative serotype (scAAV6 IL-1ra, Figure 3). Two weeks following Day 154, a robust increase of IL-1ra was detected by ELISA in two animals. One horse expressed very high levels of IL-1ra (pre 0 ng ml −1 and post 230–1000 ng ml −1) for over 100 days with a gradual decline in IL-ra at 273 days. Unexpectedly, low dosed horse #2 yielded initial levels identical to redosed horse #1 with 700 ng ml−1 at 2 weeks post injection followed by rapid diminution at 4 weeks post injection (suggestive of immune response or vector silencing yet to be determined). The WBC counts and TP for re-injected joints remained within normal range during this time and did not differ significantly from the contralateral joints injected with saline or scAAV6GFP.
Figure 3.
(a–d) IL-1ra (ng ml−1), total protein (g dl−1) and WBC (cells per μl) levels in low dosed and contralateral control limb synovial fluid samples after the second administration of virus. The x-axis begins at Day 154 when re-injection took place. One horse (a) whose joint was re-injected (scAAV6IL-1ra) had IL-1ra level rise to 675 ng ml−1 and quickly drop while the other horse (c) that was re-injected (also with scAAV6IL-1ra) rose to a high level of 1190 ng ml−1 and remained elevated until Day 273. WBC and TP were not different between any injected joints.
No lameness or pain on flexion of injected joints was noted and no increase in joint circumference was observed during the study in response to injections of scAAV2IL-1ra or scAAV6IL-1ra (re-injected joints), scAAV2GFP or saline in all test animals.
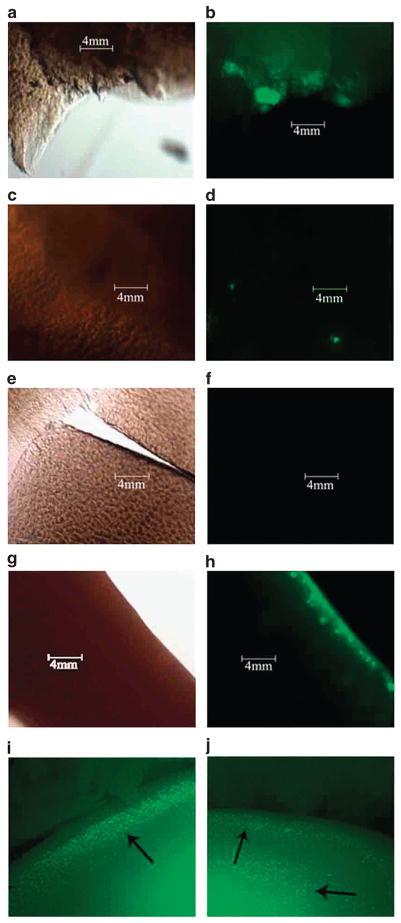
Intra-articular GFP fluorescence and intra-articular histology
Cartilage and synovial biopsies were taken from joints injected with scAAVGFP and examined under fluorescent microscopy to determine the level of tissue transduction in specific cell types (Figure 4). High and low dosed horses had cartilage and synovium removed at Day 276 and middle dosed horses had tissue harvested at Day 98 as previously described. Cartilage from the high (Figure 4b) and middle (Figure 4d) dosed horses revealed fluorescent chondrocytes at the time of harvest (Day 276 for high dosed horses and Day 98 for middle dosed horses) consistent with cell type transduction identified in a previous study24 and consistent with IL-1ra levels within this study. Cartilage from lowest dosed horses (Figure 4f) did not reveal fluorescent chondrocytes in the cartilage following injection with scAAV2GFP when analyzed at Day 276. Synovium did not reveal fluorescence from any horses injected with scAAV2GFP past Day 98 consistent with expected natural turnover of these cells.34 Arthroscopic images of the joints injected with scAAV6GFP (the antebrachiocarpal joint of re-injected horses) revealed fluorescent chondrocytes when viewed arthroscopically 122 days following GFP injection (Figure 4i and j and Supplementary Video 1 and 2).
Figure 4.
(a–j) Microscopic imaging of cartilage explants 48 h after euthanasia and collection. Explants were observed under × 100 magnification with (right image) and without (left image) a fluorescent filter (excitation of 495 nm, emission of 521 nm). High dosed (scAAV2GFP) joints are shown in panels a and b, middle dosed joints are shown in c and d, and low dosed joints are shown in panels e and f. Cartilage from the joints re-injected with scAAV6GFP are shown in panels g and h. Panels i and j represent arthroscopic images 4 months following a joint injected with scAAVGFP. The bright green dots represent transduced chondrocytes within the cartilage viewed arthroscopically following injection.
Histology (hematoxilin and eosin (H&E) and Toluidine Blue) of cartilage and H&E of synovium did not reveal any inflammation in response to vector injection. There were no pathologic changes noted in any of the tissues from either the saline, scAAVGFP or scAAVIL-1ra.
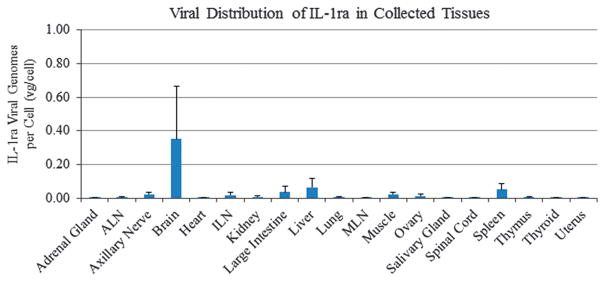
Vector distribution and joint histology
Viral distribution of IL-1ra viral genomes was tested by quantitative PCR analysis on an extensive panel of tissues harvested for all test animals (Figure 5). The vector genome levels in all nonjoint tissues were consistent with what was observed in our previous study (below 1.5 vector genomes (vg per cell).24 Viral distribution of these genomes was also examined in the capsule, cartilage, pericapsule and synovium for high, middle and low dosed joints injected with scAAV2IL-1ra as well as the control (saline) injected joints (data not shown). Inconsistent with our previous study, we were unable to detect vector genomes in joint tissues from joints injected with scAAV2IL-1ra or scAAV6IL-1ra at these extended time points, suggesting variability in tissue sampling as supported by our observed GFP transduction. This may indicate a need to adapt this protocol to conduct a broader sampling of entire organs to capture truly representative genome copy numbers per cell.
Figure 5.
Panels a–e represents the biodistribution of IL-1ra vector genomes per cell (vg per cell) in all tissues collected at the termination of the study. Standard errors are shown (n =6). Levels of vector genomes >1 vg per cell are considered significant. No samples were >0.8 vg per cell.
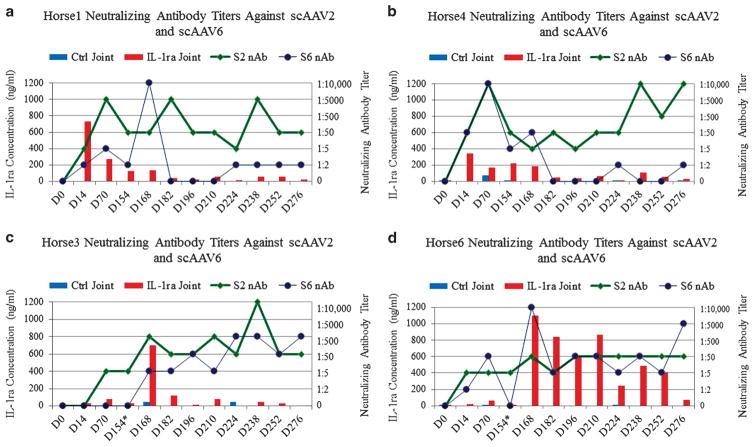
Presence of Nabs
In an attempt to determine the presence and levels of Nabs that developed to injected vector capsid, we measured levels of Nabs in the serum of all horses over the entire course of these studies. Data for the high and low dosed horses are shown in Figure 6. Figures 6a and b (high dosed horses) reveal that Nabs to serotype 2 at levels between 1:5 to 1:50 were present at Day 14 (the first time point examined following injection) and remained above 1:5 in both high dosed horses until the end of the study (Day 276). Nabs were also detected to the alternative capsid (AAV6) in the high dosed horses that only received AAV2 injections (Figures 6a and b). In both of the high dosed horses, Nabs to serotype 6 (note that AAV6 was not injected in these horses) were between 0 and 1:10 000 up until Day 182 when interestingly the levels of IL-1ra decreased to levels <20 ng ml −1. As seen in mice these cross-reactive Nabs to serotype 6 were either not detected or were below clinical significance until the end of the study.30 For lower dosed/redosed horses (Figure 6c and d) Nabs to S2 remained fairly low (0–1:50) until those horses were redosed with scAAV6IL-1ra at which time Nab’s to serotype 2 were between 1:50 and 1:10,000. When redosing with AAV6, similarly the Nabs to serotype 6 also rose from 0 to between 1:50 and 1:10,000 for the duration of the study. From the responses of Nabs to vector injection it appears responses are dose and vector dependent.
Figure 6.
(a–d) Serum neutralizing antibody titers against scAAV2IL-1ra and scAAV6IL-1ra in high (a and b) and low (c and d) dosed animals. Levels of neutralizing antibodies to S2 are highest in the high dosed horses (a and b) and are low for most of the length of the study to S6. Levels of neutralizing antibodies to S2 are also high in the low dosed horses (c and d). Neutralizing antibodies to S6 rise following injection at Day 154 and stay elevated through the termination of the study.
DISCUSSION
The majority of dosing studies for gene therapeutic approaches are done in laboratory animals or species that do not mimic the size or architecture of the human joint.22,35,36 The equine joint has been found to be most closely associated with the human joint in terms of cartilage and subchondral bone thickness, joint architecture and synovial fluid volume.27,37 While the use of the horse for dosing studies is expensive, the translational value of performing this study should provide valuable data to the human arena to suggest appropriate dosing for similarly sized joints using scAAVIL-1ra. We based our escalating vector dosage on previous work by us24 and others21,31 who established therapeutic levels of various AAV transgenes in joints similar in size to the human knee. The horse has been used extensively as a translational model to humans for OA37,38 and cartilage repair39,40 and we believe this dosing study is suggestive of levels that can be expected in a similarly sized human knee. The animal numbers and samples obtained in this study are informative albeit somewhat restricted based on expense of using the horse as a model verses rats, mice or rabbits.
We attempted to deliver clinical doses that would be relevant and translational directly to human joints based on previous studies demonstrating prolonged expression of therapeutic expression of IL-1ra transgene.24 The highest vector dose administered in the present study was 5 × 1012 vg and resulted in IL-1ra levels between 80 ng ml−1 and 750 ng ml−1 for up to 168 days and thereafter levels between 10 and 60 ng ml−1 to the end of the study. Doses of either recombinant (Anakrina) or endogenous IL-1ra (autologous conditioned serum) administered to humans with OA, juvenile OA or rheumatoid arthritis or horses with OA either systemically (anakrina) or intra-articularly (anakrina or autologous conditioned serum) have resulted in broad ranges of intra-articular levels of IL-1ra between 30 pg ml−1 and up to 30 000 pg ml−1.41,42 Levels depending on the length of time synovial fluids were taken following treatment and types of ELISA used to measure levels.
The levels of IL-1ra postulated to effectively antagonize IL-1β binding to the IL-1 receptors range from 10 fold to 1000 fold that of IL-β.11,43–46 Therefore effective levels of IL-1ra within the joint would depend on how much IL-1β is present as a result of the inflammatory process intra-articularly. In patients with joint inflammation, levels of IL-1β have been reported to be anywhere between 1 pg ml−1 and up to 600 pg ml −1.10,42 Therefore levels of synovial IL-1ra theoretically would ideally range from 10 to 6000 pg ml −1. Levels in this study far surpass this range; however, it is unknown ‘how much is enough’ and to our knowledge there are no detrimental effects associated with high levels of IL-1ra in the joint.
The drawback of direct injection of recombinant or endogenous IL-1ra is quickly diminishing levels of protein intra-articularly and even slow release formulations have only mildly prolonged levels of IL-1ra.43,47,48 The need for sustained levels of IL-1ra to protect cartilage degeneration has been highlighted by Rutgers et al.49 in which levels of proteoglycans within osteoarthritic cartilage were not ‘rescued’ by autologous conditioned serum largely due to the short half-life of the protein. A gene therapeutic approach to enhancing intra-articular IL-1ra levels circumvents the rapid decline of IL-1ra levels when administered using recombinant or endogenous IL-1ra harvested from autologous conditioned serum. Several gene therapeutic studies have revealed that IL-1ra gene therapy results in enhanced levels of intra-articular IL-1ra for sustained periods of time and provides efficacy in reducing inflammatory cytokines in induced arthritis.22,38,50–52 Further, IL-1ra gene therapy in small pilot studies performed in human joints has resulted in elevated levels of IL-1ra and a reduction of IL- β and pain.53,54 This has resulted in an intense effort within the gene therapy community to bring this approach to fruition as a potential effective treatment for OA.19
As AAV gene delivery to joints continues to show promise in animals24,31,52 and people,21,55 questions have surfaced as to whether immunity to AAV vectors would result in an inability to re-dose patients with AAV vectors that had an inadequate rise of protein to therapeutic levels. The inability to utilize AAV gene therapy following previous exposure to AAV has been well-established.56 To address these concerns, we injected all horses with AAV2 and then redosed the two lowest dosed horses (5 × 1010 vg) with AAV6 at the highest dose (5 × 1012 vg) (Figure 3) to determine if an alternative serotype could result in enhanced IL-1ra bypassing any Nabs to AAV2. Only the low dosed horses were redosed to mimic the clinical scenario of minimal levels of IL-1ra and the subsequent need to re-dose to result in therapeutic levels of IL-1ra. In both horses, we were able to induce high levels of IL-1ra intra-articularly following injection of scAAV6-IL-1ra into the same joints. In one horse, levels stayed high for the duration of the study and in the other horse levels were not sustained. It is unknown if the latter horse’s immune system recognized and blocked the IL-1ra or if levels dropped due to a less effective transduction of AAV6. Experiments are underway to clarify this. Regardless, these results are promising in that they suggest that the ability to re-dose a patient with an alternative serotype is a realistic option.
We also measured Nab’s to AAV2 and AAV6 throughout the duration of the study (Figure 6) to determine the level of immune stimulation to each serotype. Results suggested that AAV2 injected at the dosage of 5 × 1012 vg resulted in stimulation of Nabs to both AAV2 and AAV6. Horses injected with low dose AAV2 (5 × 1010) had Nabs to AAV2 but at a lower level than the horses injected with the high (5 × 1012) dose and Nabs to AAV6 were very low (between zero to 1:50). On redosing with AAV6IL-1ra, Nabs to AAV6 rose and remained high until the duration of the study affirming the potential to re-dose patients with alternative AAV serotypes if therapeutic levels are not reached with the initial dose. We used serum to measure Nabs as this is an accurate determination of inhibition of AAV within the syovial fluid as shown in previous studies.32,33 The Nab levels determined from this study demonstrate that once a particular AAV serotype is utilized to result in therapeutic levels of protein intra-articularly, Nabs stimulated from the original injection to that serotype rise to levels that in previous studies negate any redosing with the original serotype used.32,33
To determine the level of tissue transduction on a qualitative basis, we developed further a novel, in situ analyzation of tissues transduced by AAVGFP first described in a previous study by our group.24 This system combined with fluorescent microscopy of cartilage explants (Figure 4) revealed the superficial layer of chondrocytes in cartilage that were efficiently transduced with AAVGFP. Figures 4i and j reveal the arthroscopic confirmation that AAVGFP transduced cells are present throughout the cartilage surface and to the edges of the cartilage of the carpal bones. Supplementary Videos (S1 and S2) also reveals this throughout the joint examined arthroscopically. Synovial tissue did not reveal fluorescence when the joints were arthroscopically examined and then subsequently observed under fluorescent microscopy. As confirmed in other intra-articular gene therapy studies, synovial cells within the synovial tissue and chondrocytes within the cartilage are the principle targeted cells for initial injection; however, synovial turnover results in most transduced cells within the synovium to be absent (due to turnover) between 4 and 6 weeks following injection leaving the chondrocytes as the stable, long-term protein producing cells.24,34 Although initial gene therapy studies in laboratory animals suggested that cartilage is not successfully transduced, this and other work in the horse has shown long-term expression of AAV in this enduring population of quiescent and minimally dividing cell population19,24,31 and therefore highlight the potential for human cartilage to also result in sustained levels of protein production given its similarities to the horse.27,37 GFP expression persisting in chondrocytes rules out the possibility of immune response to GFP as a primary reason of loss of transgene expression in synoviocytes.
Biodistribution studies revealed negligible levels of vector genome within the peripheral organs collected for vector detection consistent with our previous study in which no significant levels of vector genomes were detected after assaying two horses 23 and 182 days following scAAVIL-1ra intra-articular injection.24 It also highlights the safety of AAV intra-articular gene therapy and the localization of this vector within the joint.
There are currently many studies reporting efficacy of various retro, lenti and adenoviral vectors for intra-articular gene therapy specifically to deliver IL-1ra for arthritis.22,24,38,57,58 While these studies have provided proof-of-principle, gene therapy using an AAV-delivered IL-1ra transgene appears to provide the most stable transduction and results in the shortest time to protein production following in vivo injection. Further, it is associated with the least amount of intra-articular joint inflammation.24,52,56 While efficacy of IL-1ra protein level elevation is shown in this study in normal horses, it is important to determine the proper dose of scAAVIL-1ra that results in levels of IL-1ra that will be efficacious in antagonizing the effects of IL-1β in an equine model of OA.
SUMMARY
To our knowledge, this is the first dosing study to report levels of AAVIL-1ra according to vector amounts injected. Further, it is the first study to reveal the ability to re-dose a joint with an alternative serotype that results in high levels of therapeutic protein in a large animal model that for all intents and purposes mimics the human knee. Our hypotheses were proven in that: (1) the dose of 5 × 1012 appears to result in therapeutic levels of IL-1ra for at least 8 months following injection; (2) the chondrocytes appear to be the stable, transduced cell population within the joint; (3) Nabs rise in response to various serotypes injected intra-articularly; and (4) joints can be redosed with an alternative serotype of AAV and result in high therapeutic levels of protein. Further, the dose of 5 × 1012 appears to be safe and cause minimal to no detrimental effects in joints that are similar in size to the human knee. While the joints of horses in this study were normal, levels of IL-1ra may change due to inflammation since some promoters such as CMV may enhance protein production in an inflammatory environment. With the knowledge of the appropriate dose of scAAVIL-1ra that will result in therapeutic and long-term levels of IL-1ra production, a study to determine the efficacy of this gene therapeutic approach can begin.
MATERIALS AND METHODS
Clinical trial
All animal work was approved by Colorado State University IUCAC. Six skeletally mature horses between 2 and 5 years of age were dosed in the middle carpal joint with scAAVIL-1ra, scAAV2GFP vectors (both vectors having a CMV promoter and a polyA tail) or saline. All vectors used in the study were produced by the University of North Carolina vector core facility. Two horses were given 5 × 1012 vg, two were given 5 × 1011 vg and two were given 5 × 1010 vg, corresponding to high, middle or low doses, respectively. Three animals received either scAAV2GFP or scAAV2IL-1ra in the left and right middle carpal joint, while the remaining three animals received either saline or scAAV2IL-1ra. At Day 154, animals initially receiving the lowest dose of virus 5 × 1010 vg were given a second injection of either scAAV6IL-1ra or scAAV6GFP of 5 × 1012 vg in both carpal joints. Injections were administered into the upper (antebrachiocarpal) carpal space (scAAV6GFP only) or middle carpal space based on the location of the first injection. Physical examinations (lameness evaluation, pain on flexion and joint circumference) were performed at Day 0 and weekly for the duration of the study. Serum and synovial fluid samples were collected at Day 0 to establish baseline levels. Serum and synovial fluid samples were subsequently collected 2 weeks post injection and every other week thereafter for 39 weeks, at which time the animals were killed and tissue samples were collected for histology, biodistribution and functional assays.
Arthroscopic examination
Arthroscopic assessments were performed on both carpal joints of the horses given scAAV2GFP 1 month following administration of the viral constructs. Fluorescent filters on the arthroscope were used to evaluate synovial membrane and fibrous joint capsule and cartilage for fluorescing cells. Since one carpal joint had scAAV2GFP injected and the contralateral joint had scAAV2IL-1ra injected, the joints acted as a positive and negative control (for fluorescence), respectively. Fluorescence was imaged and video recorded.
Serum and synovial fluid evaluation and viral biodistribution
Serum samples were evaluated for circulating levels of IL-1ra with a commercially available equine IL-1ra ELISA (R&D Systems, Minneapolis, MN, USA). Synovial fluid samples were evaluated for TP and fluid cytology, as well as IL-1ra with the same previously mentioned ELISA kit. Serum samples were non-diluted and synovial fluid samples were diluted 1:40 in reagent diluent (1% bovine serum albumin in phosphate buffered saline) prior to IL-1ra evaluation. Samples were evaluated as per manufacturer’s instructions.
Serum samples from each horse at Day 0, Day 14, Day 70 and Day 154–276 were analyzed for the presence of Nabs against viral serotypes, specifically serotypes 2, 2.5, 3, 5 and 6. Two-ninety-three cells were plated to 50% confluency and allowed to equilibrate for 48 h at 37 °C with 5% CO2. Serum samples from the time points listed above were diluted 1:2, 1:5, 1:50, 1:500, 1:5000 and 1:10 000 in non-supplemented Dulbecco’s Modified Eagle’s medium, and added v/v (125 μl/125 μl) to scAAVGFP viral constructs to form a neutralized complex. These complexes were incubated at 37 °C as described above for 1 h, and were added to the 293 cells for 1 h. Neutralized complexes were removed from the 293 cells, and supplemented media (10% fetal bovine serum, 10 000 U penicillin/streptomycin/amphotericinB, 1 N HEPES) for an additional 24 h. Cells were removed from plates with Accumax (Sigma-Aldrich, St Louis, MO, USA) and suspended in 0.1% bovine serum albumin/phosphate buffered saline for flow cytometry analysis.
The biodistribution of IL-1ra viral particles was investigated through collecting tissues from each animal and performing quantitative PCR for vector genome biodistribution studies. Tissue DNA was purified and the abundance of target DNA vector and reference sequences was quantified as described.59 Data is reported as the number of double-stranded IL-1ra vector DNA molecules per two copies of the equine GAPDH locus, or in other words the number of vector DNA copies per diploid equine genome. The equine GAPDH primers are as follows: forward 5′-GATTGT CAGCAATGCCTCCT-3′; reverse 5′-TGCCAAAGTGGTCATGGAT-3′. The IL-1ra primers are as follows: forward 5′-AGCTTCCCGGCAACAATTA-3′; reverse 5′-GCAGAAGTGGTCCTGCAACT-3′.
Histology and explant evaluation
Tissue samples taken from the forelimb middle carpal joints from each horse were visualized with a fluorescent microscope. Images were captured using × 100 magnification, utilizing a fluorescein isothiocyanate fluorescent filter cube with an excitation of 495 nm and emission of 521 nm. Synovium, osteochondral sections, joint capsules and joint pericapsular tissues were placed in formalin. Osteochondral samples were removed from formalin within 72 h and decalcified using an EDTA-based decalcification solution. All samples were paraffin embedded and mounted onto charged slides. Tissues were deparaffinized and stained with hematoxylin and eosin, and osteochondral samples were also stained with Toluidine Blue. Briefly, samples were hydrated with a series of ethanol incubations; followed by hematoxylin stain, blue buffer solution and eosin counterstaining. Slides were rinsed with distilled H2O between each stain. Subchondral bone was deparaffinized and hydrated as described, and were incubated in 1% Toluidine Blue solution. Slides were rinsed between stains as described above, dehydrated and cover slipped for analysis. Histological sections were observed and scored for villous architecture, subintimal fibrosis, intimal hyperplasia, vascularity and inflammatory cell infiltration (synovium), and perilesional cloning, subchondral bone attachment, Toluidine staining, surface fibrillation and tidemark (articular cartilage), as previously described.24
Supplementary Material
Acknowledgments
This study was supported by NIH1K08AR054903-01A2 and Grayson Jockey Club Foundation Award (LRG, CWM and RJS), NIHP01HL112761 (RJS and JCG), NIHR01AI072176 (RJS) and NIHR01AR064369 (RJS).
Footnotes
CONFLICT OF INTEREST
The authors declare no conflict of interest.
Supplementary Information accompanies this paper on Gene Therapy website (http://www.nature.com/gt)
References
- 1.McAlindon TE, Bannuru RR, Sullivan MC, Arden NK, Berenbaum F, Bierma-Zeinstra SM, et al. OARSI guidelines for the non-surgical management of knee osteoarthritis. Osteoarthritis Cartilage. 2014;22:363–388. doi: 10.1016/j.joca.2014.01.003. [DOI] [PubMed] [Google Scholar]
- 2.Ishijima M, Nakamura T, Shimizu K, Hayashi K, Kikuchi H, Soen S, et al. Intra-articular hyaluronic acid injection versus oral non-steroidal anti-inflammatory drug for the treatment of knee osteoarthritis: a multi-center, randomized, open-label, non-inferiority trial. Arthritis Res Ther. 2014;16:R18. doi: 10.1186/ar4446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Frisbie DD, Kawcak CE, McIlwraith CW, Werpy NM. Evaluation of polysulfated glycosaminoglycan or sodium hyaluronan administered intra-articularly for treatment of horses with experimentally induced osteoarthritis. Am J Vet Res. 2009;70:203–209. doi: 10.2460/ajvr.70.2.203. [DOI] [PubMed] [Google Scholar]
- 4.Frisbie DD, Kawcak CE, Trotter GW, Powers BE, Walton RM, McIlwraith CW. Effects of triamcinolone acetonide on an in vivo equine osteochondral fragment exercise model. Equine Vet J. 1997;29:349–359. doi: 10.1111/j.2042-3306.1997.tb03138.x. [DOI] [PubMed] [Google Scholar]
- 5.Baltzer AW, Moser C, Jansen SA, Krauspe R. Autologous conditioned serum (Orthokine) is an effective treatment for knee osteoarthritis. Osteoarthritis Cartilage. 2009;17:152–160. doi: 10.1016/j.joca.2008.06.014. [DOI] [PubMed] [Google Scholar]
- 6.Abate M, Schiavone C, Salini V. Hyaluronic acid in ankle osteoarthritis: why evidence of efficacy is still lacking? Clin Exp Rheumatol. 2012;30:277–281. [PubMed] [Google Scholar]
- 7.Nigrovic PA, Mannion M, Prince FH, Zeft A, Rabinovich CE, van Rossum MA, et al. Anakinra as first-line disease-modifying therapy in systemic juvenile idiopathic arthritis: report of forty-six patients from an international multicenter series. Arthritis Rheum. 2011;63:545–555. doi: 10.1002/art.30128. [DOI] [PubMed] [Google Scholar]
- 8.Yang KG, Raijmakers NJ, van Arkel ER, Caron JJ, Rijk PC, Willems WJ, et al. Autologous interleukin-1 receptor antagonist improves function and symptoms in osteoarthritis when compared to placebo in a prospective randomized controlled trial. Osteoarthritis Cartilage. 2008;16:498–505. doi: 10.1016/j.joca.2007.07.008. [DOI] [PubMed] [Google Scholar]
- 9.Frisbie DD, Kawcak CE, Werpy NM, Park RD, McIlwraith CW. Clinical, biochemical, and histologic effects of intra-articular administration of autologous conditioned serum in horses with experimentally induced osteoarthritis. Am J Vet Res. 2007;68:290–296. doi: 10.2460/ajvr.68.3.290. [DOI] [PubMed] [Google Scholar]
- 10.Kraus VB, Birmingham J, Stabler TV, Feng S, Taylor DC, Moorman CT, 3rd , et al. Effects of intraarticular IL1-Ra for acute anterior cruciate ligament knee injury: a randomized controlled pilot trial ( NCT00332254) Osteoarthritis Cartilage. 2012;20:271–278. doi: 10.1016/j.joca.2011.12.009. [DOI] [PubMed] [Google Scholar]
- 11.Arend WP, Welgus HG, Thompson RC, Eisenberg SP. Biological properties of recombinant human monocyte-derived interleukin 1 receptor antagonist. J Clin Investig. 1990;85:1694–1697. doi: 10.1172/JCI114622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Daheshia M, Yao JQ. The interleukin 1beta pathway in the pathogenesis of osteoarthritis. J Rheumatol. 2008;35:2306–2312. doi: 10.3899/jrheum.080346. [DOI] [PubMed] [Google Scholar]
- 13.Pelletier JP, McCollum R, Cloutier JM, Martel-Pelletier J. Synthesis of metalloproteases and interleukin 6 (IL-6) in human osteoarthritic synovial membrane is an IL-1 mediated process. J Rheumatol Suppl. 1995;43:109–114. [PubMed] [Google Scholar]
- 14.Saha N, Moldovan F, Tardif G, Pelletier JP, Cloutier JM, Martel-Pelletier J. Interleukin-1beta-converting enzyme/caspase-1 in human osteoarthritic tissues: localization and role in the maturation of interleukin-1beta and interleukin-18. Arthritis Rheum. 1999;42:1577–1587. doi: 10.1002/1529-0131(199908)42:8<1577::AID-ANR3>3.0.CO;2-Z. [DOI] [PubMed] [Google Scholar]
- 15.Smith MD, Triantafillou S, Parker A, Youssef PP, Coleman M. Synovial membrane inflammation and cytokine production in patients with early osteoarthritis. J Rheumatol. 1997;24:365–371. [PubMed] [Google Scholar]
- 16.Kubota E, Imamura H, Kubota T, Shibata T, Murakami K. Interleukin 1 beta and stromelysin (MMP3) activity of synovial fluid as possible markers of osteoarthritis in the temporomandibular joint. J Oral Maxillofac Surg. 1997;55:20–27. doi: 10.1016/s0278-2391(97)90438-9. discussion 27–28. [DOI] [PubMed] [Google Scholar]
- 17.Loeser RF, Carlson CS, Del Carlo M, Cole A. Detection of nitrotyrosine in aging and osteoarthritic cartilage: Correlation of oxidative damage with the presence of interleukin-1beta and with chondrocyte resistance to insulin-like growth factor 1. Arthritis Rheum. 2002;46:2349–2357. doi: 10.1002/art.10496. [DOI] [PubMed] [Google Scholar]
- 18.Baltzer AW, Ostapczuk MS, Stosch D, Seidel F, Granrath M. A new treatment for hip osteoarthritis: clinical evidence for the efficacy of autologous conditioned serum. Orthop Rev (Pavia) 2013;5:59–64. doi: 10.4081/or.2013.e13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Evans CH, Ghivizzani SC, Robbins PD. Arthritis gene therapy and its tortuous path into the clinic. Transl Res. 2013;161:205–216. doi: 10.1016/j.trsl.2013.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Evans CH, Ghivizzani SC, Robbins PD. Getting arthritis gene therapy into the clinic. Nat Rev Rheumatol. 2011;7:244–249. doi: 10.1038/nrrheum.2010.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mease PJ, Wei N, Fudman EJ, Kivitz AJ, Schechtman J, Trapp RG, et al. Safety, tolerability, and clinical outcomes after intraarticular injection of a recombinant adeno-associated vector containing a tumor necrosis factor antagonist gene: results of a phase 1/2 Study. J Rheumatol. 2010;37:692–703. doi: 10.3899/jrheum.090817. [DOI] [PubMed] [Google Scholar]
- 22.Kay JD, Gouze E, Oligino TJ, Gouze JN, Watson RS, Levings PP, et al. Intra-articular gene delivery and expression of interleukin-1Ra mediated by self-complementary adeno-associated virus. J Gene Med. 2009;11:605–614. doi: 10.1002/jgm.1334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Goodrich LR, Choi VW, Carbone BA, McIlwraith CW, Samulski RJ. Ex vivo serotype-specific transduction of equine joint tissue by self-complementary adeno-associated viral vectors. Hum Gene Ther. 2009;20:1697–1702. doi: 10.1089/hum.2009.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Goodrich LR, Phillips JN, McIlwraith CW, Foti SB, Grieger JC, Gray SJ, et al. Optimization of scAAVIL-1ra in vitro and in vivo to deliver high levels of therapeutic protein for treatment of osteoarthritis. Mol Ther Nucleic Acids. 2013;2:e70. doi: 10.1038/mtna.2012.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mason JB, Gurda BL, Engiles JB, Hankenson KD, Wilson JM, Richardson DW. Multiple recombinant adeno-associated viral vector serotypes display persistent in vivo gene expression in vector-transduced rat stifle joints. Hum Gene Ther Methods. 2013;24:185–194. doi: 10.1089/hgtb.2012.199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mason JB, Vandenberghe LH, Xiao R, Wilson JM, Richardson DW. Influence of serotype, cell type, tissue composition, and time after inoculation on gene expression in recombinant adeno-associated viral vector-transduced equine joint tissues. Am J Vet Res. 2012;73:1178–1185. doi: 10.2460/ajvr.73.8.1178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Frisbie DD, Cross MW, McIlwraith CW. A comparative study of articular cartilage thickness in the stifle of animal species used in human pre-clinical studies compared to articular cartilage thickness in the human knee. Vet Comp Orthop Traumatol. 2006;19:142–146. [PubMed] [Google Scholar]
- 28.McIlwraith CW, Frisbie DD, Kawcak CE. The horse as a model of naturally occurring osteoarthritis. Bone Joint Res. 2012;1:297–309. doi: 10.1302/2046-3758.111.2000132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vandenberghe LH, Wilson JM. AAV as an immunogen. Curr Gene Ther. 2007;7:325–333. doi: 10.2174/156652307782151416. [DOI] [PubMed] [Google Scholar]
- 30.Li C, Diprimio N, Bowles DE, Hirsch ML, Monahan PE, Asokan A, et al. Single amino acid modification of adeno-associated virus capsid changes transduction and humoral immune profiles. J Virol. 2012;86:7752–7759. doi: 10.1128/JVI.00675-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ishihara A, Bartlett JS, Bertone AL. Inflammation and immune response of intra-articular serotype 2 adeno-associated virus or adenovirus vectors in a large animal model. Arthritis. 2012;2012:735472. doi: 10.1155/2012/735472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cottard V, Valvason C, Falgarone G, Lutomski D, Boissier MC, Bessis N. Immune response against gene therapy vectors: influence of synovial fluid on adeno-associated virus mediated gene transfer to chondrocytes. J Clin Immunol. 2004;24:162–169. doi: 10.1023/B:JOCI.0000019781.64421.5c. [DOI] [PubMed] [Google Scholar]
- 33.Boissier MC, Lemeiter D, Clavel C, Valvason C, Laroche L, Begue T, et al. Synoviocyte infection with adeno-associated virus (AAV) is neutralized by human synovial fluid from arthritis patients and depends on AAV serotype. Hum Gene Ther. 2007;18:525–535. doi: 10.1089/hum.2006.174. [DOI] [PubMed] [Google Scholar]
- 34.Gouze E, Gouze JN, Palmer GD, Pilapil C, Evans CH, Ghivizzani SC. Transgene persistence and cell turnover in the diarthrodial joint: implications for gene therapy of chronic joint diseases. Mol Ther. 2007;15:1114–1120. doi: 10.1038/sj.mt.6300151. [DOI] [PubMed] [Google Scholar]
- 35.Watanabe S, Imagawa T, Boivin GP, Gao G, Wilson JM, Hirsch R. Adeno-associated virus mediates long-term gene transfer and delivery of chondroprotective IL-4 to murine synovium. Mol Ther. 2000;2:147–152. doi: 10.1006/mthe.2000.0111. [DOI] [PubMed] [Google Scholar]
- 36.Ulrich-Vinther M, Duch MR, Soballe K, O’Keefe RJ, Schwarz EM, Pedersen FS. In vivo gene delivery to articular chondrocytes mediated by an adeno-associated virus vector. J Orthop Res. 2004;22:726–734. doi: 10.1016/j.orthres.2003.12.003. [DOI] [PubMed] [Google Scholar]
- 37.McIlwraith CW, Frisbie DD, Kawcak CE. The horse as a model of naturally occurring osteoarthritis. Bone Joint Res. 2012;1:297–309. doi: 10.1302/2046-3758.111.2000132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Frisbie DD, Ghivizzani SC, Robbins PD, Evans CH, McIlwraith CW. Treatment of experimental equine osteoarthritis by in vivo delivery of the equine interleukin-1 receptor antagonist gene. Gene Ther. 2002;9:12–20. doi: 10.1038/sj.gt.3301608. [DOI] [PubMed] [Google Scholar]
- 39.Goodrich LR, Hidaka C, Robbins PD, Evans CH, Nixon AJ. Genetic modification of chondrocytes with insulin-like growth factor-1 enhances cartilage healing in an equine model. J Bone Joint Surg Br. 2007;89:672–685. doi: 10.1302/0301-620X.89B5.18343. [DOI] [PubMed] [Google Scholar]
- 40.Morisset S, Frisbie DD, Robbins PD, Nixon AJ, McIlwraith CW. IL-1ra/IGF-1 gene therapy modulates repair of microfractured chondral defects. Clin Orthop Relat Res. 2007;462:221–228. doi: 10.1097/BLO.0b013e3180dca05f. [DOI] [PubMed] [Google Scholar]
- 41.Catterall JB, Stabler TV, Flannery CR, Kraus VB. Changes in serum and synovial fluid biomarkers after acute injury ( NCT00332254) Arthritis Res Ther. 2010;12:R229. doi: 10.1186/ar3216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pascual V, Allantaz F, Arce E, Punaro M, Banchereau J. Role of interleukin-1 (IL-1) in the pathogenesis of systemic onset juvenile idiopathic arthritis and clinical response to IL-1 blockade. J Exp Med. 2005;201:1479–1486. doi: 10.1084/jem.20050473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Granowitz EV, Clark BD, Mancilla J, Dinarello CA. Interleukin-1 receptor antagonist competitively inhibits the binding of interleukin-1 to the type II interleukin-1 receptor. J Biol Chem. 1991;266:14147–14150. [PubMed] [Google Scholar]
- 44.Firestein GS, Berger AE, Tracey DE, Chosay JG, Chapman DL, Paine MM, et al. IL-1 receptor antagonist protein production and gene expression in rheumatoid arthritis and osteoarthritis synovium. J Immunol. 1992;149:1054–1062. [PubMed] [Google Scholar]
- 45.Arend WP, Malyak M, Guthridge CJ, Gabay C. Interleukin-1 receptor antagonist: role in biology. Annu Rev Immunol. 1998;16:27–55. doi: 10.1146/annurev.immunol.16.1.27. [DOI] [PubMed] [Google Scholar]
- 46.Arend WP. Interleukin-1 receptor antagonist. Adv Immunol. 1993;54:167–227. doi: 10.1016/s0065-2776(08)60535-0. [DOI] [PubMed] [Google Scholar]
- 47.Gabay C, Arend WP. Treatment of rheumatoid arthritis with IL-1 inhibitors. Springer Semin Immunopathol. 1998;20:229–246. doi: 10.1007/BF00832009. [DOI] [PubMed] [Google Scholar]
- 48.Bendele A, McAbee T, Woodward M, Scherrer J, Collins D, Frazier J, et al. Effects of interleukin-1 receptor antagonist in a slow-release hylan vehicle on rat type II collagen arthritis. Pharm Res. 1998;15:1557–1561. doi: 10.1023/a:1011903100188. [DOI] [PubMed] [Google Scholar]
- 49.Rutgers M, Saris DB, Dhert WJ, Creemers LB. Cytokine profile of autologous conditioned serum for treatment of osteoarthritis, in vitro effects on cartilage metabolism and intra-articular levels after injection. Arthritis Res Ther. 2010;12:R114. doi: 10.1186/ar3050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bandara G, Mueller GM, Galea-Lauri J, Tindal MH, Georgescu HI, Suchanek MK, et al. Intraarticular expression of biologically active interleukin 1-receptor-antagonist protein by ex vivo gene transfer. Proc Natl Acad Sci USA. 1993;90:10764–10768. doi: 10.1073/pnas.90.22.10764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zhang X, Mao Z, Yu C. Suppression of early experimental osteoarthritis by gene transfer of interleukin-1 receptor antagonist and interleukin-10. J Orthop Res. 2004;22:742–750. doi: 10.1016/j.orthres.2003.12.007. [DOI] [PubMed] [Google Scholar]
- 52.Watson RS, Broome TA, Levings PP, Rice BL, Kay JD, Smith AD, et al. scAAV-mediated gene transfer of interleukin-1-receptor antagonist to synovium and articular cartilage in large mammalian joints. Gene Ther. 2013;20:670–677. doi: 10.1038/gt.2012.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wehling P, Reinecke J, Baltzer AW, Granrath M, Schulitz KP, Schultz C, et al. Clinical responses to gene therapy in joints of two subjects with rheumatoid arthritis. Human Gene Ther. 2009;20:97–101. doi: 10.1089/hum.2008.075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Evans CH, Robbins PD, Ghivizzani SC, Wasko MC, Tomaino MM, Kang R, et al. Gene transfer to human joints: progress toward a gene therapy of arthritis. Proc Natl Acad Sci USA. 2005;102:8698–8703. doi: 10.1073/pnas.0502854102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Mease PJ, Cohen S, Gaylis NB, Chubick A, Kaell AT, Greenwald M, et al. Efficacy and safety of retreatment in patients with rheumatoid arthritis with previous inadequate response to tumor necrosis factor inhibitors: results from the SUNRISE trial. J Rheumatol. 2010;37:917–927. doi: 10.3899/jrheum.090442. [DOI] [PubMed] [Google Scholar]
- 56.Goater J, Muller R, Kollias G, Firestein GS, Sanz I, O’Keefe RJ, et al. Empirical advantages of adeno associated viral vectors in vivo gene therapy for arthritis. J Rheumatol. 2000;27:983–989. [PubMed] [Google Scholar]
- 57.Gouze E, Pawliuk R, Gouze JN, Pilapil C, Fleet C, Palmer GD, et al. Lentiviral-mediated gene delivery to synovium: potent intra-articular expression with amplification by inflammation. Mol Ther. 2003;7:460–466. doi: 10.1016/s1525-0016(03)00024-8. [DOI] [PubMed] [Google Scholar]
- 58.Evans CH, Ghivizzani SC, Kang R, Muzzonigro T, Wasko MC, Herndon JH, et al. Gene therapy for rheumatic diseases. Arthritis Rheum. 1999;42:1–16. doi: 10.1002/1529-0131(199901)42:1<1::AID-ANR1>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- 59.Gray SJ, Matagne V, Bachaboina L, Yadav S, Ojeda SR, Samulski RJ. Preclinical differences of intravascular AAV9 delivery to neurons and glia: a comparative study of adult mice and nonhuman primates. Mol Ther. 2011;19:1058–1069. doi: 10.1038/mt.2011.72. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.