Abstract
IMPORTANCE
Panretinal photocoagulation (PRP) is standard treatment for reducing severe visual loss from proliferative diabetic retinopathy (PDR). However, PRP can damage the retina, resulting in peripheral vision loss or worsening diabetic macular edema (DME).
OBJECTIVE
Compare ranibizumab versus PRP for PDR.
DESIGN, SETTING, AND PARTICIPANTS
Randomized clinical trial (55 U.S. sites) assessing non-inferiority of ranibizumab compared with PRP for vision outcomes; 305 adults with PDR enrolled February-December 2012 (mean age 52, 44% female, 52% white). Both eyes enrolled for 89 participants totaling 394 study eyes. The final 2-year visit was completed January 2015.
INTERVENTIONS
Ranibizumab group (N=191 eyes): intravitreous 0.5-mg ranibizumab and, PRP if treatment failed; ranibizumab as needed for DME. PRP group (N=203 eyes): PRP; ranibizumab as needed for DME.
MAIN OUTCOMES AND MEASURES
Primary: mean visual acuity change at 2 years (5-letter non-inferiority margin; intention-to-treat analysis). Secondary: visual acuity area under the curve, peripheral visual field loss, DME development, neovascularization, vitrectomy, and safety.
RESULTS
Mean visual acuity letter improvement at 2 years was +2.8 in the ranibizumab group versus +0.2 in the PRP group (difference +2.2, 95% confidence interval [CI]: −0.5 to +5.0, non-inferiority P<0.001). Mean treatment group difference in visual acuity area under the curve over 2 years was +4.2 (95% CI: +3.0 to +5.4, P<0.001). Visual field sensitivity loss was worse (mean dB difference 372; 95% CI: 213 to 531, P<0.001), vitrectomy more frequent (15% versus 4%, difference 9%, 95% CI: 4% to 15%, P<0.001), and DME development more frequent (28% versus 9%, difference 19%, 95% CI: 10% to 28%, P<0.001) in the PRP versus ranibizumab group, respectively. Eyes with neither active nor regressed neovascularization at 2 years was similar (35% [ranibizumab group] versus 30% [PRP group], difference 3%, 95% CI: −7% to 12%, P=0.58). One eye (ranibizumab group) developed endophthalmitis. No significant differences between groups in rates of major cardiovascular events were identified.
CONCLUSION
Among eyes with PDR, treatment with ranibizumab resulted in visual acuity that was non-inferior to (not worse than) PRP treatment at two years. Although longer term follow-up is needed, ranibizumab may be a reasonable treatment alternative, at least through 2 years, for patients with PDR.
Proliferative diabetic retinopathy (PDR) is a leading cause of vision loss in patients with diabetes mellitus,1, 2 resulting in 12,000 to 24,000 new cases of blindness each year in the United States.3 Without treatment, nearly 50% of patients with high-risk PDR experience severe vision loss within five years.4
Panretinal photocoagulation (PRP) has been the standard treatment for PDR since the Diabetic Retinopathy Study demonstrated its benefit nearly 40 years ago.4 PRP is effective, in part, because it reduces vascular endothelial growth factor (VEGF).5 In a 2014 survey, 98% of retina specialists reported using PRP for initial PDR management in the absence of DME.6 However, it can cause permanent peripheral visual field loss, decreased night vision, and may exacerbate diabetic macular edema (DME), which makes alternative treatments desirable.7–9 Even with timely PRP, about 5% of eyes develop severe vision loss4, 7
When used for diabetic macular edema (DME) treatment, intravitreous anti-VEGF agents reduce the risk of diabetic retinopathy worsening and increase the chance of improvement10–12, making these agents a potentially viable PDR treatment. Therefore, we conducted a randomized trial evaluating the non-inferiority of intravitreous ranibizumab compared with PRP for visual acuity outcomes in patients with PDR.
METHODS
This multi-center randomized clinical trial was conducted by the Diabetic Retinopathy Clinical Research Network (DRCR.net) at 55 clinical sites in the United States. The study adhered to the tenets of the Declaration of Helsinki13 and was approved by multiple institutional review boards. Study participants provided written informed consent. An independent data and safety monitoring committee provided oversight. The study protocol is available in the supplemental material.
Study Population
Study participants were at least 18 years old, had type 1 or type 2 diabetes, at least one eye with PDR, no previous PRP, and a best corrected visual acuity letter score ≥24 (approximate Snellen equivalent 20/320 or better). Eyes with or without DME were eligible. All eligibility criteria are in Table S1. Baseline demographics (Table 1) demonstrated balance among treatment groups. Age was patient reported, gender was determined by study staff, and race/ethnicity (based on fixed categories) were either patient reported or determined by study staff.
Table 1.
Baseline Characteristics
| Ranibizumab Group (N = 191 eyes; 191 Participants) | PRP Group (N = 203 eyes; 203 participants) | |
|---|---|---|
| Participant Characteristics | ||
| Gender: Women - N (%) | 83 (43%) | 92 (45%) |
|
| ||
| Age (yrs) - Median (25th, 75th percentile) | 52 (44, 59) | 51 (44, 59) |
|
| ||
| Participants with two study eyes (i.e. participants included in both study groups)- N (%) | 89 (47%) | 89 (44%) |
|
| ||
| Race/Ethnicity - N (%) | ||
|
| ||
| White | 100 (52%) | 101 (50%) |
|
| ||
| Hispanic | 48 (25%) | 51 (25%) |
|
| ||
| Black/African-American | 38 (20%) | 43 (21%) |
|
| ||
| Asian | 2 (1%) | 3 (1%) |
|
| ||
| American Indian/Alaskan Native | 1 (<1%) | 0 (0%) |
|
| ||
| More than one race | 0 (0%) | 2 (<1%) |
|
| ||
| Unknown/not reported | 2 (1%) | 3 (1%) |
|
| ||
| Diabetes Type - N (%) | ||
|
| ||
| Type 1 | 43 (23%) | 41 (20%) |
|
| ||
| Type 2 | 140 (73%) | 155 (76%) |
|
| ||
| Uncertain | 8 (4%) | 7 (3%) |
|
| ||
| Duration of Diabetes (yrs) - Median (25th, 75th percentile) | 18 (12, 24) | 17 (11, 23) |
|
| ||
| Hemoglobin A1c* (%) - Median (25th, 75th percentile) | 8.6 (7.5, 10.4) | 8.9 (7.5, 10.4) |
|
| ||
| Prior Myocardial Infarction - N (%) | 3 (2%) | 4 (2%) |
|
| ||
| Prior Stroke - N (%) | 4 (2%) | 3 (1%) |
|
| ||
| Mean Arterial Blood Pressure‡ (mmHg) - Median (25th, 75th percentile) | 99 (88, 108) | 99 (88, 107) |
|
| ||
| Ocular Characteristics | ||
|
| ||
| Visual Acuity | ||
|
| ||
| Letter Score – Mean | 75.0 ± 12.8 | 75.2 ± 12.5 |
|
| ||
| Letter Score - Median (75th, 25th percentile) | 77 (70, 84) | 78 (70, 85) |
|
| ||
| ~ Snellen Equivalent - Median (75th, 25th percentile) |
20/32 (20/40, 20/20) |
20/32 (20/40, 20/20) |
|
| ||
| ≥ 84 letter score (20/20 or better) | 52 (27%) | 58 (29%) |
|
| ||
| 83–79 letter score (20/25) | 35 (18%) | 35 (17%) |
|
| ||
| 78 – 69 letter score (20/32 to 20/40) | 64 (34%) | 67 (33%) |
|
| ||
| 68- 49 letter score (20/50 to 20/100) | 31 (16%) | 35 (17%) |
|
| ||
| 48–24 letter score (20/125 to 20/320) | 9 (5%) | 8 (4%) |
|
| ||
| OCT Central Subfield Thickness†* (Stratus equivalence, μm) - | ||
|
| ||
| Median (25th, 75th percentile) | 223 (196, 271) | 230 (203, 265) |
|
| ||
| Mean ± Standard Deviation | 262 ± 109 | 249 ± 86 |
|
| ||
| < 225 μm | 96 (51%) | 87 (43%) |
|
| ||
| 225–249 μm | 29 (15%) | 47 (23%) |
|
| ||
| 250–349 μm | 35 (19%) | 52 (26%) |
|
| ||
| 350–449 μm | 12 (6%) | 7 (3%) |
|
| ||
| ≥ 450 μm | 17 (9%) | 8 (4%) |
|
| ||
| Presence of CI-DME with Visual Acuity Impairment§‡ | 42 (22%) | 46 (23%) |
|
| ||
| Presence of CI-DME Regardless of Visual Acuityǁ‡ | 55 (29%) | 62 (31%) |
|
| ||
| OCT Retinal Volume (Stratus equivalence, mm3)†¶ - Median (25th, 75th percentile) | 7.6 (6.9, 8.2) | 7.5 (6.9, 8.2) |
|
| ||
| Neovascularization on Clinical Exam | ||
|
| ||
| Neovascularization of the disc | 96 (50%) | 103 (51%) |
|
| ||
| Neovascularization elsewhere | 166 (87%) | 174 (86%) |
|
| ||
| Lens Status (clinical exam) - N (%) | ||
|
| ||
| Phakic | 170 (89%) | 187 (92%) |
|
| ||
| Diabetic Retinopathy Severity** (ETDRS level) | ||
|
| ||
| Microaneurysms only (level 20) | 0 (0%) | 1 (<1%) |
|
| ||
| Mild NPDR (level 35) | 6 (3%) | 4 (2%) |
|
| ||
| Moderate NPDR (level 43) | 2 (1%) | 5 (3%) |
|
| ||
| Moderately severe NPDR (level 47) | 10 (5%) | 15 (8%) |
|
| ||
| Severe NPDR (level 53) | 1 (<1%) | 1 (<1%) |
|
| ||
| Prior PRP; without active PDR (level 60) | 0 (0%) | 1 (<1%) |
|
| ||
| Mild PDR (level 61) | 30 (16%) | 31 (16%) |
|
| ||
| Moderate PDR (level 65) | 68 (36%) | 67 (34%) |
|
| ||
| High-risk PDR (level 71 and 75) | 69 (37%) | 73 (37%) |
|
| ||
| Advanced PDR, macula center attached (level 81) | 2 (1%) | 0 (0%) |
|
| ||
| Advanced PDR, macula center detached (level 85) | 1 (<1%) | 1 (<1%) |
|
| ||
| Prior Treatment for DME - N (%) | 43 (23%) | 36 (18%) |
|
| ||
| Prior Focal/Grid Laser for DME - N (%) | 30 (16%) | 29 (14%) |
|
| ||
| Prior Anti-VEGF for DME - N (%) | 21 (11%) | 13 (6%) |
PRP = panretinal photocoagulation, OCT = optical coherence tomography, CI-DME = center-involved diabetic macular edema, ETDRS = Early Treatment Diabetic Retinopathy Study, anti-VEGF = anti- vascular endothelial growth factor.
Hemoglobin A1c missing for 7 in the ranibizumab group and 5 in the PRP group.
Assessments from OCT machines other than Zeiss Stratus were converted to equivalent on Zeiss Stratus.
OCT CST measurements missing for 2 in the ranibizumab group and 2 in the PRP group.
For Heidelberg Spectralis defined as CST ≥305 for women and ≥320 for men with visual acuity letter score 78 or less (approximate Snellen equivalent 20/32 or worse). For Zeiss Cirrus and Optovue RTVue, defined as CST ≥290 for women and ≥305 for men with visual acuity letter score 78 or less (20/32 or worse). For Zeiss Stratus defined as CST ≥250 with visual acuity letter score 78 or less (20/32 or worse).
For Heidelberg Spectralis defined as CST ≥305 for women and ≥320 for men. For Zeiss Cirrus and Optovue RTVue, defined as CST ≥290 for women and ≥305 for men. For Zeiss Stratus defined as central subfield thickness ≥250.
Missing OCT retinal volume measurements for 35 in the ranibizumab group and 40 in the PRP group.
Missing diabetic retinopathy level for 2 in the ranibizumab group and 4 in the PRP group. Proliferative diabetic retinopathy could not be identified by the reading center in 46 (12%) eyes; however was subsequently confirmed on other imaging modalities in 29 (63%) of the 46 eyes.
Synopsis of Study Design
A participant could have one or two eyes included in the study. Using the DRCR.net study website to conceal the next treatment allocation, using a permuted block design, participants with one study eye were randomly assigned with equal probability to either PRP with ranibizumab as needed for DME treatment (PRP group) or intravitreous-0.5 mg ranibizumab with PRP for treatment failure (ranibizumab group) (injection procedure: http://drcrnet.jaeb.org/ViewPage.aspx?PageName=Investig_Info). Participants with two study eyes had one eye assigned randomly to PRP and the other to ranibizumab (Table S1).
The primary outcome visit was at 2 years, with follow-up planned through 5 years. Only data through 2 years are reported. In both groups, visits occurred every 16 weeks. Ranibizumab group participants had additional visits every 4 weeks during the first year and every 4 to 16 weeks during the second year depending on treatment (eFigure S1).
At baseline and each follow-up visit, certified personnel obtained best corrected visual acuity using the Electronic-Early Treatment Diabetic Retinopathy Study (e-ETDRS) Visual Acuity Test14. Spectral (96% of scans), or time-domain ocular coherence tomography (OCT), was performed at baseline, annually and as needed for DME treatment assessment. Humphrey visual field testing (at select sites) on 30-2 and 60-4 patterns and digital fundus photographs were obtained at baseline and annually (Table S1). Images and visual fields were graded by centralized reading centers when applicable (Table S1). At baseline and annually, participants with one study eye completed visual function questionnaires and binocular visual acuity testing with everyday correction (Table S1). Adverse events were coded using the Medical Dictionary for Regulatory Activities (MedDRA).
Reading center graders and the medical monitor who reviewed all adverse events were masked to treatment assignments. Visual acuity and OCT technicians were masked to treatment group assignments at annual visits. Study participants, investigators and study coordinators were not masked due to the nature of the treatments.
Treatment Protocol
PDR
In the ranibizumab group, study eyes received an injection for PDR at baseline and every 4 weeks through 12 weeks. Thereafter, retreatment was based on investigator assessment of neovascularization (NV) on extended ophthalmoscopy and any available retinal images. Injections at 16 and 20 weeks were required unless all NV resolved. Starting at the 24-week visit, an injection was required every 4 weeks unless NV resolved or was stable (not improved or worsened) following 2-consectuive injections. Injections resumed if NV worsened. Injections for PDR could be performed at investigator discretion if not required. PRP for PDR was permitted (eFigure S1) in the ranibizumab group for “failure” or “futility”.
In the PRP group, PRP for PDR was initiated at baseline (see Table S1 for PRP procedure). If the NV size or amount increased following completion of PRP, additional PRP could be given. In both groups, vitrectomy for vitreous hemorrhage or retinal detachment was at investigator discretion, and could include intraoperative PRP.
DME
DME was defined for the protocol as a thickened OCT central subfield (Table S1) at least 2 standard deviations beyond the gender-specific and instrument-specific norm for the population and a visual acuity letter score ≤78 (~Snellen equivalent 20/32 or worse). Eyes not meeting both criteria were considered not to have DME for purposes of the protocol. Eyes in both treatment groups with DME could receive ranibizumab provided by the study. At randomization, ranibizumab was required for eyes with DME. Otherwise, initiation and retreatment with ranibizumab for DME and application of focal/grid photocoagulation for DME was at investigator discretion. A follow-up visit and retreatment regimen for DME was provided as a guideline, melded with protocol retreatment and follow-up visits for PDR.15
Outcomes
The primary outcome was mean change in visual acuity letter score from baseline to 2 years. Secondary efficacy outcomes included visual acuity area under the curve, change in visual field total point score, central subfield thickness change, DME development, and proportion of eyes without PDR on fundus photographs. Pre-specified adverse events related to diabetic retinopathy included vitreous hemorrhage, retinal detachment, vitrectomy, neovascular glaucoma, and iris neovascularization. Pre-specified additional safety outcomes assessed included endophthalmitis, ocular inflammation, cataract surgery, serious adverse events, hospitalizations, death, Antiplatelet Trialists’ Collaboration events, and events in each MedDRA system organ class.
Statistical Methods
Sample size estimate for the primary outcome, change in visual acuity, was 380 eyes for a non-inferiority margin of 5 letters, type I error of 2.5% and 85% power (Table S1). The non-inferiority hypothesis was tested by determining whether the one end of a 2-sided 95% confidence interval excluded the non-inferiority margin. If ranibizumab was found non-inferior to prompt PRP, the same 2-sided 95% confidence interval would be used to test ranibizumab superiority. The non-inferiority margin was selected, in part, because it was the same margin used in a prior trial evaluating anti-VEGF agents for neovascular age-related macular degeneration.16 The Protocol Development Committee (see Acknowledgments) believed a true difference exceeding 5.0 letters represented a clinically important difference.17
The primary analysis for comparison between treatments of mean change in visual acuity followed the intention-to-treat principle and included all randomly assigned eyes with multiple imputation by the Markov chain Monte Carlo method to impute missing 2-year visual acuities. Imputation for 2-year visual acuities was based on treatment group, baseline visual acuity, baseline central subfield thickness, and all visual acuity data from the 16-weekly visits. Within group means were based on observed data unless otherwise specified. Treatment group differences, confidence intervals, and p-values were estimated using analysis of covariance (ANCOVA), adjusting for baseline visual acuity and randomization stratification factors (baseline central subfield thickness and number of study eyes), with generalized estimating equations (GEE) used to account for correlation between eyes of participants contributing 2 eyes. Outlying visual acuity changes were truncated to ±3 standard deviations from the mean. A per-protocol analysis was conducted excluding eyes not completing the 2-year visit, eyes without PDR on baseline fundus photographs, and eyes receiving alternate PDR treatment. Model assumptions were evaluated and satisfied. Sensitivity analyses using transformations, including nonparametric Van der Waerden normal scores, were conducted.
Pre-planned subgroup analyses repeated the primary ANCOVA, adding subgroup and subgroup by treatment interactions. Safety analyses and secondary efficacy analyses used binomial regression, ANCOVA, or the marginal Cox proportional hazards model as appropriate.18, 19 Within group means for secondary outcomes were based on observed data unless otherwise specified. Treatment group differences, confidence intervals, and p-values for secondary outcomes were based on the intention-to-treat cohort. P values and confidence intervals are two-sided unless otherwise specified. For the primary non-inferiority and superiority analyses, P values <0.025 (one-sided) or <0.05 (two-sided) were considered statistically significant. Analyses were performed using SAS, version 9.4 (SAS Institute).
RESULTS
Between February and December 2012, 394 study eyes of 305 participants were assigned randomly to the ranibizumab group (N=191) or the PRP group (N=203). In the ranibizumab and PRP groups respectively, the median age was 52 (44, 59) and 51 (44, 59) years, 43% and 45% were women, and 52% and 50% were white. Among the eyes in the ranibizumab and the PRP groups, respectively, mean baseline visual acuity letter score was 75.0 (approximate Snellen equivalent 20/32) ±12.8 and 75.2 (approximate Snellen equivalent 20/32) ±12.5. DME at baseline was present in 22% and 23%. Baseline characteristics of the 2 groups appeared similar (Table 1).
Excluding 14 deaths (including 4 participants with two study eyes), the 2-year visit completion rate was 88% and 86% in the ranibizumab and PRP groups, respectively (Figure 1). The median (quartiles) number of visits was 22 (18, 24) in the ranibizumab group and 16 (9, 22) in the PRP group. Table S2 reports baseline characteristics by 2-year visit completion status.
Figure 1. Completion of Follow-up for Study Eyes.
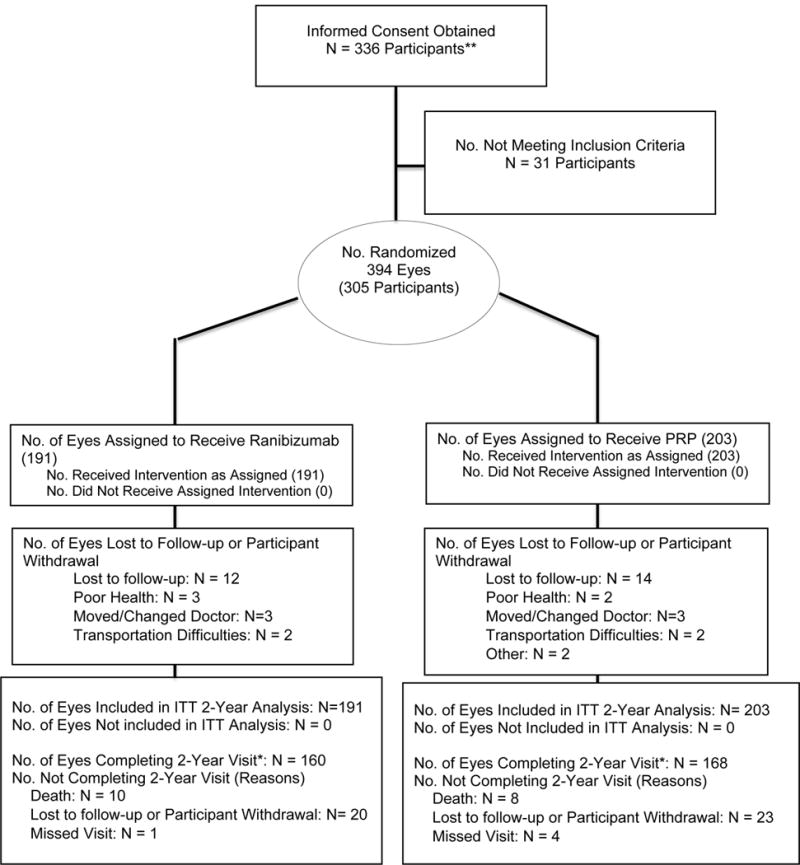
*Two-year completed visits include those that occurred between 644 and 812 days (between 92 and 116 weeks).
** Participants are not formally screened prior to obtaining an informed consent
ITT = Intention-to-treat
PDR and DME Treatment
Ranibizumab Group
Ninety-seven percent of protocol-required injections based on clinician interpretation of NV were given. Eyes without DME at baseline (N=133) received a median (quartiles) of 7 (5, 9) injections through 1 year; eyes without DME at baseline (N=126) received a median of 10 (6, 13) injections through 2 years (Table S3). Eyes with DME at baseline (N=36) received 9 (7, 11) injections through 1 year; eyes with DME at baseline (N=33) received 14 (10, 17) injections through 2 years. Focal/grid laser was performed in 15 eyes (8%). Through 2 years, 12 eyes (6%) received PRP including 8 during vitrectomy.
PRP Group
All eyes received initial PRP, 98% received protocol-defined complete PRP (Table S4). After the completion of PRP, 92 (45%) eyes received additional PRP (median [quartiles] time from baseline to additional PRP was 221 [116, 386] days).
In addition to PRP, 72 (35%) eyes received ranibizumab for DME at baseline; an additional 36 (18%) received ranibizumab for DME prior to 2 years (Table S5). Among eyes with baseline DME (N = 46), median (quartiles) number of injections for DME was 5 (3, 9) prior to 1 year and 9 (4, 15) prior to 2 years. Among eyes without baseline DME (N = 155) that were later treated for DME, median (quartiles) number of injections was 3 (1, 6) and 4 (2, 7) prior to 1 and 2 years, respectively. Focal/grid laser was performed in 21 eyes (10%).
Effect of Treatment
Visual Acuity
At 2 years, mean visual acuity letter score improvement from baseline was +2.8 in the ranibizumab group and +0.2 in the PRP group. The mean treatment group difference was +2.2 (95% confidence interval [CI]: −0.5 to +5.0, non-inferiority P<0.001, Table 2). This result met the pre-specified non-inferiority criterion (the lower bounds of the 95% CI of −0.5 letter was greater than the non-inferiority limit of −5.0 letters). Mean change in visual acuity letter score over 2 years (area under the curve) was +4.5 compared with −0.3 for the ranibizumab and PRP groups, respectively (mean difference= 4.2 ([95% CI: 3.0 to 5.4]; P< 0.001, Table 2, Figure 2). The difference between groups was greater at 1 year than at 2 years. Results were similar in per-protocol analyses limited to participants who completed 2-years (Figure S2, Table S6, treatment group difference +2.1 [95% CI: −0.5, +4.6]) or eyes with definite baseline PDR on fundus photographs (Table S6). Results were similar when limiting analyses to participants with two study eyes (Table S7). Sensitivity analyses using cube transformation (one-sided test for superiority =0.006) and a nonparametric approach (one-sided test for superiority P =0.013) were similar to overall results (one-sided test for superiority P=0.053, Table S8). Slight differences in P-values likely were a result of transformations reducing skewness and thus increasing precision, however, a priori, the untransformed analysis was designated as primary. Percentages of eyes with ≥15 letter (Table S9) improvement or worsening (judged clinically relevant when visual acuity is moderately impaired17) at 2 years and over time (Figure S3 and S4) were similar between the groups. Percentages of eyes with ≥10 letter worsening (similarly judged clinically relevant when visual acuity is minimally impaired) also were similar. No significant interaction of treatment with pre-planned subgroups (Table S10) was identified except for a possible interaction of visual acuity and prior DME treatment (P=0.02).
Table 2.
Main Study Outcomes
| Visual Acuity Letter Score* | ||||
|---|---|---|---|---|
| Ranibizumab Group N = 160 Eyes |
PRP Group N = 168 Eyes |
Adjusted Difference 95% CI | P-value | |
| Visual Acuity at 2-Years | ||||
| Mean letter score ± SD | 78.7 ± 16.3 | 76.2 ± 14.1 | ||
| Mean Snellen equivalent | 20/32 | 20/32 | ||
| Change from Baseline in letter score | Observed Data | Intention-to-Treat Analysis with Multiple Imputation | ||
| Median letter score | 5 (−2, 11) | 2 (−4, 7) | ||
| Mean letter score (95% CI) | 2.8 (0.4, 5.2) | 0.2 (−1.9, +2.3) | +2.2 (−0.5, +5.0) |
0.11 |
| Visual Acuity Area Under the Curve – letter score£ | Observed Data | Observed Data | ||
| Mean (95% CI) | 4.5 (3.4, 5.5) | −0.3 (−1.5, +1.0) | +4.2 (+3.0, +5.4) |
< 0.001 |
| Central Subfield Thickness (CST) †‡ | ||||
|
Ranibizumab Group N = 149 Eyes |
PRP Group N = 161 Eyes |
Adjusted Difference 95% CI | P-value | |
| Observed Data | Intention-to-Treat Analysis with LOCF | |||
| Mean CST at 2 years - μm (95% CI) | 210 (201, 218) | 243 (231, 255) | ||
| Mean CST change from baseline to 2 years (95% CI) | −47 (−61, −33) | −3 (−15 −9) | −45 (−57, −33) |
< 0.001 |
| Changes in Diabetic Retinopathy§¶ | ||||
|
Ranibizumab Group N = 191 Eyes |
PRP Group N = 203 Eyes |
Adjusted Difference 95% CI | P-value | |
| Intention-to-Treat Analysis | ||||
| Retinal Detachment | ||||
| Traction retinal detachment | 10 (5%) | 16 (8%) | ||
| Rhegmatogenous retinal detachment | 1 (<1%) | 1 (<1%) | ||
| Unspecified retinal detachment | 3 (2%) | 4 (2%) | ||
| Any retinal detachmentβ | 12 (6%) | 21 (10%) | −4% (−9%, +1%) | 0.08 |
| Neovascular glaucoma | 3 (2%) | 6 (3%) | −1% (−4%, +2%) | 0.50 |
| Neovascularization of the Iris | 2(1%) | 2(1%) | 0% (−2%, +2%) | 0.96 |
| Vitreous Hemorrhage | 52 (27%) | 69(34%) | −7% (−15%, +1%) | 0.09 |
| Vitrectomy | 8 (4%) | 30 (15%) | −9% (−15%, −4%) | < 0.001 |
| Diabetic Retinopathy on Fundus Photographs at 2 Yearsǁ | N = 142 Eyes | N = 148 Eyes | 0.41 | |
| Percentage of eyes without PDR (level 60 or lower) | 49 (35%) | 44 (30%) | ||
| Percentage of eyes with regressed NV (level 61A) | 33 (23%) | 36 (24%) | ||
| Percentage of eyes with active NV (level 61B or higher) | 60 (42%) | 68 (46%) | ||
| Percentage of Eyes Improving 2 or More Steps in Diabetic Retinopathy Severity on Fundus Photos at 2 Yearsǁ¥ | 67 (47%) | – | ||
Visual acuity is measured as a continuous integer letter score from 100 to 0 with higher numbers meaning better visual acuity. A letter score of 85 is approximately 20/20 and 70 is approximately 20/40, the legal unrestricted driving limit in most states. A letter score of 35 is approximately 20/200, considered legal blindness when it is the visual acuity in the better-seeing eye. A 5-letter change for an individual is approximately equal to a 1-line change on an eye vision chart. Treatment group means are calculated from observed 2-year data (N= 31 and N = 35 missing 2-year visual acuity in ranibizumab and PRP groups respectively). Treatment group differences, confidence intervals, and P-values were obtained using of analysis of covariance, with adjustment for baseline visual acuity, number of study eyes, baseline central subfield thickness, and correlation between 2 study eyes of the same participant, with multiple imputation for missing data when indicated. Visual acuity change was truncated to ± 3 standard deviation from the mean (−47, +49) to minimize the effect of outliers (5 and 3 eyes for ranibizumab and PRP groups respectively, all on the negative end at the 2-year visit).
Eyes with at least 2 follow-up visits were included in the area under the curve analyses: N = 186 and N = 196 for the ranibizumab and PRP groups respectively.
Treatment group means are calculated from observed data at the 2-year visit (N= 42 missing 2-year OCT in each group). Treatment group differences, confidence intervals, and P-values were obtained using analysis of covariance, with adjustment for number of study eyes, baseline central subfield thickness, correlation between 2 study eyes of the same participant, and imputation of missing data with last observation carried forward. Central subfield thickness changes were truncated to ± 3 standard deviations from the mean (−325, +276) to minimize the effect of outliers (4 eyes in the ranibizumab group on the large decrease end and 3 eyes in the PRP group [1 large decrease, 2 large increase] at the 2-year visit). All baseline and 2 year optical coherence tomography (OCT) scans were evaluated by the OCT reading center. In addition, a random sample of OCT images from other visits and images for which the investigator believed central grading was needed also were graded by the OCT reading center.
Optical coherence tomography values obtained by spectral-domain OCT were converted to time domain equivalent values for analysis and reporting as follows: −43.12 +1.01*Zeiss Cirrus; −72.76 + 1.03*Spectralis. (Diabetic Retinopathy Clinical Research Network. Reproducibility of spectral domain optical coherence tomography retinal thickness measurements and conversions to equivalent time domain metrics in diabetic macular edema. JAMA Ophthalmol. 2014;132(9):1113–22.)
Unless otherwise specified diabetic retinopathy outcomes were collected at any time during study follow-up through the 2-year visit. If the 2-year visit was completed, then the visit date was used to define the 2-year time point; otherwise 728 days was used.
P-values are based on binomial regression adjusting for the correlation between 2 study eyes of the same participant or multinomial regression
After database lock 4 cases of reported retinal detachment (3 in the ranibizumab group and 1 in the PRP group) were identified as macular traction and not a traction retinal detachment. Primary data reported reflects available information prior to database lock. However, excluding the 4 misclassified cases, the retinal detachment rate is 9 (5%) vs. 20 (10%) in the ranibizumab and PRP groups respectively.
Only includes eyes with baseline diabetic retinopathy level 61B or worse (active neovascularization) as graded by the reading center. Uses last observation carried forward for N = 23 and N = 25 eyes missing photographs at 2 years if 1 year fundus photographs are available.
Eyes graded by the reading center as receiving PRP (level 60) at follow-up are counted as not improving.
Figure 2.
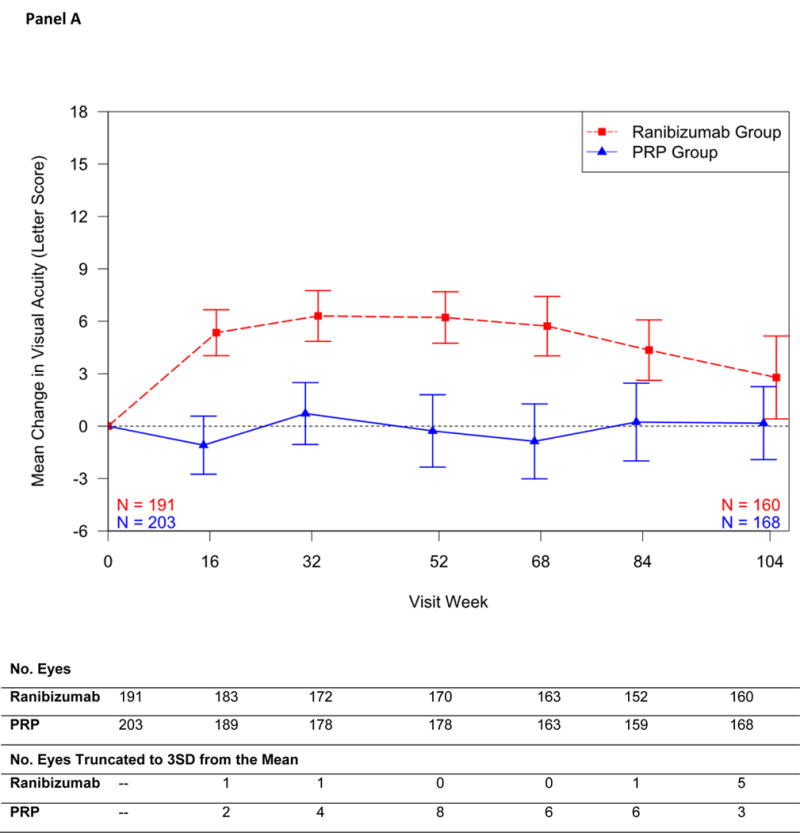
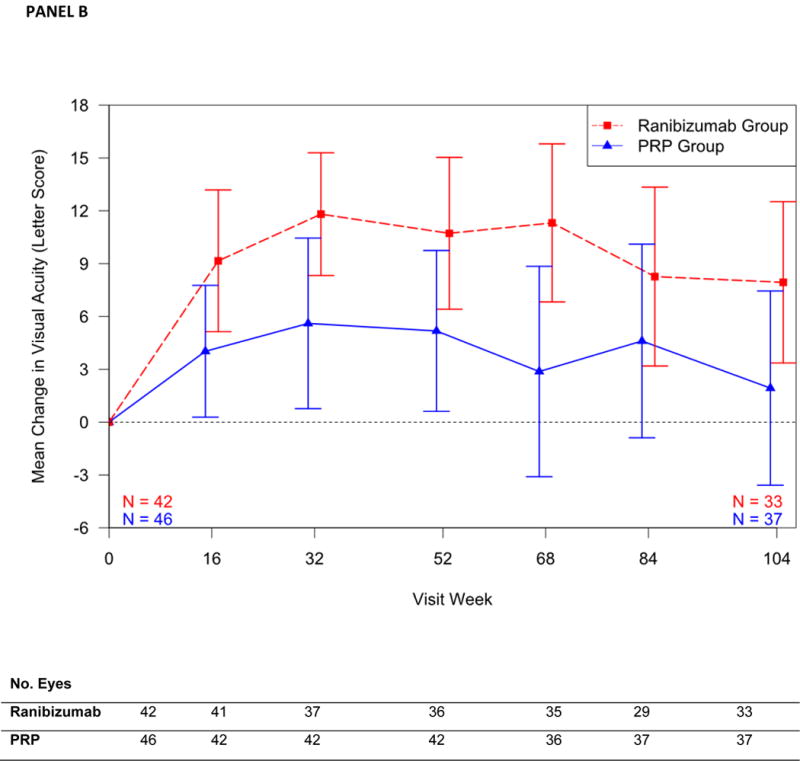
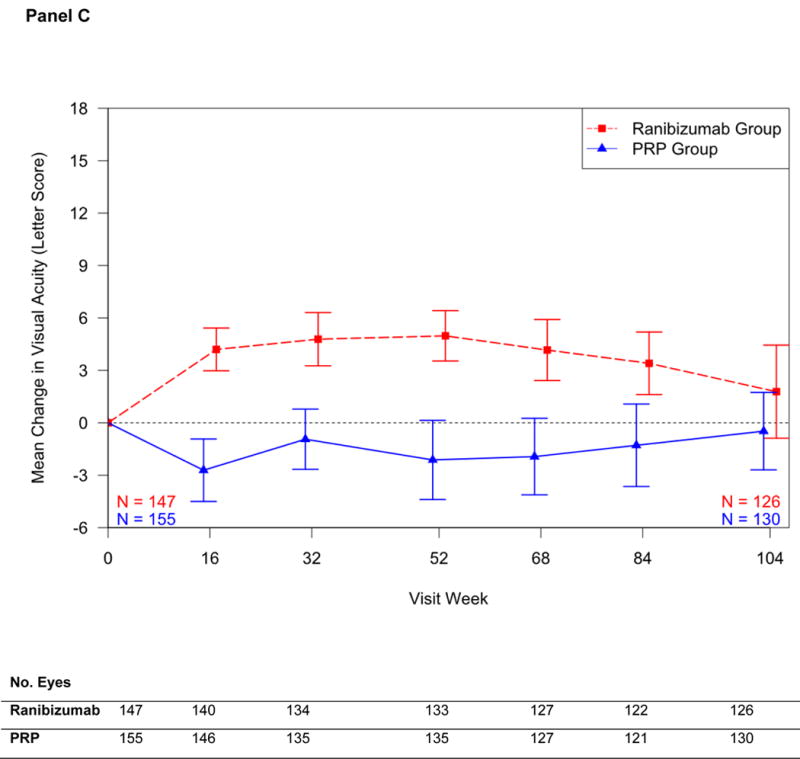
Shown are changes in visual acuity over time for the overall cohort (Panel A), for eyes with baseline DME (Panel B), and for eyes without baseline DME (Panel C). Outlying values were truncated to 3 SD from the mean. Bars represent 95% confidence interval on the mean
Among eyes with DME at baseline, mean change in visual acuity letter score differed between ranibizumab and PRP by +3.0 (95% CI: −4.2 to 10.3) and +1.4 (95% CI: −1.5 to 4.4; interaction P value = 0.84, Table S10, Table S11, Figure 2B, and Figure 2C) for eyes without baseline DME.
Other Vision Outcomes
At the 2-year visit, outcomes were better in the ranibizumab than the PRP group for binocular visual acuity (mean change from baseline +3.4±10.9 versus 0 ±11.8, respectively; difference 3.2 [95% CI: −0.3 to 6.1]; P = 0.03) and visual field (mean change, combining 30-2 and 60-4 total point score -23±410 dB versus −422±518 dB, respectively; mean difference 372 dB (95% CI: 213 to 531; P <0.001), Table S12. There were no statistically significant differences identified in the subscale scores for the National Eye Institute Visual Function Questionnaire-25 or University of Alabama-Birmingham Low Luminescence Questionnaire outcomes (Tables S13 and S14).
Retinal Thickening
At the 2-year visit, among eyes with baseline DME (N=68), central subfield thickness decreased, on average, by 153±129 μm in the ranibizumab group and by 48±124 μm in the PRP group receiving ranibizumab for DME (adjusted difference = −65μm; 95% CI: −126 to −4.5; P=0.035; Table S15). Among eyes without baseline DME, (N=242), mean change in central subfield thickness was −18±37 versus +10±54 (difference = −31μm; 95% CI: −41 to −21; P<0.001, Table S15) while the cumulative probability of developing central DME with vision impairment by 2 years was 9% versus 28% (adjusted difference 19% more frequently in the PRP group, 95% CI: 10% to 28%, P<0.001) in the ranibizumab and PRP groups, respectively (Figure S5). Changes in retinal volume are in Table S16.
Diabetic Retinopathy
A vitreous hemorrhage developed in 52 eyes (27%) within the ranibizumab group and 69 eyes (34%) within the PRP group (difference 7% more in the PRP group, 95% CI: 15% more in the PRP group to 1% more in the ranibizumab group, P = 0.09, Table 2) and a retinal detachment occurred in 6% versus 10%, respectively (difference 4% more in the PRP group, 95% CI: 9% more in the PRP group to 1% more in the ranibizumab group, P = 0.08). A vitrectomy was performed in 8 (4%) versus 30 (15%) eyes in the ranibizumab and PRP groups, respectively (difference 9% more in the PRP group, 95% CI: 4% to 15% more in the PRP group, P<0.001), including 2% versus 14% among the 302 eyes without baseline DME and 12% versus 17% among the 88 eyes with baseline DME. Timing of events related to complications of PDR is in Table S17. Rates of neovascular glaucoma were 2% in the ranibizumab group and 3% in the PRP group. New iris neovascularization was 1% in both groups.
Percentages of eyes without active or regressed neovascularization at the disc or elsewhere on fundus photographs (excluding PRP lesions) at 2 years was 35% among 142 eyes in the ranibizumab group and 30% among 148 eyes in the PRP group (difference 3%, 95% CI: −7% to 12%, P=0.58, Table 2). At 2 years, 48% of eyes in the ranibizumab group improved by 2 or more steps in diabetic retinopathy severity on fundus photographs, an outcome not assessable after PRP.
Adverse Events
Injection-related endophthalmitis occurred in one eye (0.5%) in the ranibizumab group and no eyes in the PRP group (0.04% of 2,581 total injections, 0.33% among the 299 eyes receiving ranibizumab). Ocular inflammation excluding endophthalmitis was reported in 2 (1%) and 9 (4%) eyes in the ranibizumab and PRP groups, respectively, (P = 0.02). Cataract extraction occurred in 4 (2%) and 12 (6%), respectively (P = 0.06). Additional ocular events are reported in Table 3.
Table 3.
| Systemic Adverse Events | ||||
|---|---|---|---|---|
| Participants with one study eye | ||||
| Participants with 2 Study Eyes (one in each group) | Ranibizumab Group |
PRP Group |
P-value‡ | |
| Systemic Events | N = 89 | N = 102 | N = 114 | |
| Vascular events defined by APTC occurring at least once through 2 years§ | ||||
| Non-fatal myocardial infarction | 2 (2%) | 3 (3%) | 2 (2%) | 0.89 |
| Non-fatal stroke | 1 (1%) | 2 (2%) | 4 (4%) | 0.63 |
| Death from potential vascular cause or unknown cause | 4 (4%) | 4 (4%) | 1 (<1%) | 0.22 |
| Any event | 7 (8%) | 9 (9%) | 7 (6%) | 0.80 |
| Prespecified events occurring at least once through 2 years | ||||
| Death from any cause | 4 (4%) | 6 (6%) | 4 (4%) | 0.70 |
| Hospitalization | 37 (42%) | 48 (47%) | 40 (35%) | 0.20 |
| Serious adverse event | 38 (43%) | 49 (48%) | 42 (37%) | 0.26 |
| Hypertension | 14 (16%) | 26 (25%) | 21 (18%) | 0.23 |
| Ocular Adverse Events | ||||
| Ranibizumab Group | PRP Group | P-value¶ | ||
| Ocular Events | N = 191 Eyes | N = 203 Eyes | ||
| Events occurring at least once through 2 years | ||||
| Endophthalmitis | 1 (0.5%) | 0 (0%) | – | |
| Inflammationǁ | 2 (1%) | 9 (4%) | 0.02 | |
| Retinal Tear | 0 (0%) | 0 (0%) | – | |
| Cataract surgery | 4 (2%) | 12 (6%) | 0.06 | |
| Elevation in intraocular pressure** | 17 (9%) | 27 (13%) | 0.16 | |
PRP = panretinal photocoagulation, APTC = Antiplatelet Trialists’ Collaboration
Unless otherwise specified Adverse Events were collected at any time during study follow-up.
If the 2-year visit was completed, then the visit date was used to define the 2-year time point; otherwise 728 days was used.
Systemic adverse events were classified as occurring in the group of participants with both eyes in the study (one in each treatment group), participants with one eye in the study in the PRP group, or participants with one eye in the study in the ranibizumab group. Fisher’s exact test was performed to compare the 3 groups.
Vascular events were defined according to the criteria of the Antiplatelet Trialists’ Collaboration. (Antiplatelet Trialists’ Collaboration. Collaborative overview of randomised trials of antiplatelet therapy–I: Prevention of death, myocardial infarction, and stroke by prolonged antiplatelet therapy in various categories of patients. BMJ. 1994;308(6921):81–106.)
P-values are based on binomial regression adjusting for the correlation between 2 study eyes of the same participant
Inflammation included the presence of inflammatory cells or flare in the anterior chamber, choroiditis, episcleritis, iritis, and the presence of vitreal cells.
Elevated intraocular pressure was defined as an increase in intraocular pressure of 10 mmHg or more from baseline at any visit, an intraocular pressure of 30 mmHg or more at any visit, the initiation of medication to lower intraocular pressure that was not in use at baseline, or glaucoma surgery.
There were no significant differences identified between groups in the number of participants with a serious adverse event, hospitalization, death, Antiplatelet Trialists’ Collaboration arteriothromboembolic events (Table 3),20 or events in each individual MedDRA system organ class (Table S18). However, differences with a P value slightly greater than the pre-specified cut point of P<0.01 with fewer events in the PRP group were seen in 6 of 22 system organ classes of cardiac disorders (P = 0.01), endocrine disorders (P = 0.02), infections/infestations (P = 0.02), respiratory disorders (P = 0.04), skin and subcutaneous tissue disorders (P=0.03), and surgical and medical procedures (P = 0.01). Table S19 lists all systemic adverse events.
Discussion
In this randomized clinical trial, intravitreous ranibizumab met the primary non-inferiority outcome of visual acuity change at 2 years being no worse than PRP for treatment of PDR. A statistically significant visual acuity difference between ranibizumab and PRP was not present at 2 years, recognizing that 53% of the PRP group received ranibizumab injections for DME. Ranibizumab resulted in better visual acuity when evaluated over the course of 2 years (area under the curve), although the clinical importance of this difference is unknown. More peripheral visual field loss occurred (95% CI difference: 213 dB to 531 dB), and more vitrectomies were performed in the PRP group compared with the ranibizumab group (95% CI difference: 4% to 15%). Among eyes without center-involved DME at baseline, development of DME with vision impairment was substantially more frequent in the PRP group (95% CI difference: 10% to 28%). Only 12 eyes (6%) in the ranibizumab group received PRP; more than half the eyes in the PRP group received ranibizumab for DME; thus, the protocol essentially tested ranibizumab for PDR versus PRP plus ranibizumab when needed for DME treatment.
No systemic safety concerns with ranibizumab were identified in the pre-specified major safety outcomes. Differences in MedDRA system organ classes of cardiac, endocrine, infections/infestations, respiratory, skin, or surgical disorders, while not confidently different, could be real, due to chance, or due to ascertainment bias since the ranibizumab group had more frequent visits than the PRP group. Interpreting the safety findings is difficult since a large proportion of the PRP group received ranibizumab for DME. Rates of endophthalmitis or other injection-related serious adverse events were very low, consistent with other studies.21–23
Several limitations related to the study design and conduct are important when interpreting these results. Participant retention through two years (87% of those who had not died) was lower than desired. Although participants who completed the 2-year visit had slightly better baseline visual acuities than those who did not, no visual acuity differences between treatment groups with respect to the 2-year visit completion status were apparent, limiting the possibility of differential treatment bias. Considering the final visual acuity in the PRP group, but not in the ranibizumab group, was better for those who did vs. those who did not complete the 2-year visit, if bias was present, it likely favored the PRP group. The nature of the treatments precluded masking participants and clinicians. Although DME treatment was at investigator discretion, the fixed PRP or anti-VEGF regimen for PDR limited clinician discretion, and protocol treatment adherence was high, limiting the bias of clinician unmasking except for considering vitrectomy which was at clinician discretion. Visual acuity testers were masked at the primary outcome visit and the computerized testing methods minimized acquisition bias.14
Costs, including cost-effectiveness are beyond the scope of this manuscript. It is unknown if results would have been similar with another anti-VEGF treatment. When designing this protocol, another trial evaluating ranibizumab for DME had secondary analyses supporting the potential for ranibizumab to prevent worsening of PDR.23 No such data were available for aflibercept or bevacizumab at that time. Thus, from a scientific perspective, DRCR.net investigators judged ranibizumab the best anti-VEGF agent for this trial as enrollment began.
In applying these results to clinical practice, PRP sometimes can be completed in one visit and not require additional procedures, although, in this study, 45% needed additional PRP. PRP may cost less than ranibizumab injections, and carries no risk of endophthalmitis or systemic anti-VEGF exposure. Weighing the relative benefits of PDR treatment with PRP versus ranibizumab may be influenced by whether DME is present. When DME is present for which ranibizumab treatment is planned, PRP may be unnecessary since ranibizumab will treat both the PDR and DME, assuming access to ranibizumab and patient adherence to follow-up. Regardless of presence or absence of DME, the results of this study suggest that ranibizumab is more effective than PRP for mean visual acuity outcomes over the course of 2 years with less visual field loss, and fewer eyes developing DME or undergoing vitrectomy. Nevertheless, treatment cost, adherence to and frequency of follow-up, and patient preference should be considered.
Conclusion
Among eyes with proliferative diabetic retinopathy, treatment with ranibizumab resulted in visual acuity that was non-inferior to (not worse than) panretinal photocoagulation at two years. Although longer term follow-up is needed, ranibizumab may be a reasonable treatment alternative at least through 2 years for patients with proliferative diabetic retinopathy.
Supplementary Material
Acknowledgments
A complete list of acknowledgements and funding support is available in the supplemental material.
Footnotes
A complete list of all DRCR.net investigator financial disclosures can be found at www.drcr.net.
TRIAL REGISTRATION: ClinicalTrials.gov (NCT01489189).
References
- 1.Antonetti DA, Klein R, Gardner TW. Diabetic retinopathy. N Engl J Med. 2012;366(13):1227–39. doi: 10.1056/NEJMra1005073. [DOI] [PubMed] [Google Scholar]
- 2.Aiello LP. Angiogenic pathways in diabetic retinopathy. N Engl J Med. 2005;353:839–41. doi: 10.1056/NEJMe058142. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. National diabetes fact sheet: general information and national estimates on diabetes in the United States. 2007 http://www.cdc.gov/diabetes/pubs/pdf/ndfs_2007.pdf. Accessed 10-13-09.
- 4.Photocoagulation treatment of proliferative diabetic retinopathy. Clinical application of Diabetic Retinopathy Study (DRS) findings, DRS Report Number 8. The Diabetic Retinopathy Study Research Group. Ophthalmology. 1981;88(7):583–600. [PubMed] [Google Scholar]
- 5.Silva PS, Cavallerano JD, JK S, et al. Proliferative Diabetic Retinopathy. In: Ryan SJ, editor. Retina. 5th. Elsevier; Philadelphia, PA: 2013. [Google Scholar]
- 6.American Society of Retina Specialists (ASRS) Global Trends in Retina Survey Results. https://www.asrs.org/content/documents/2014_global_trends_comprehensivepostmtg.pdf Accessed 2/18/2015.
- 7.Early Treatment Diabetic Retinopathy Study Research Group. Photocoagulation for diabetic macular edema. Early Treatment Diabetic Retinopathy Study report number 1. Arch Ophthalmol. 1985;103(12):1796–806. [PubMed] [Google Scholar]
- 8.Diabetic Retinopathy Clinical Research Network. Observational study of the development of diabetic macular edema following panretinal (scatter) photocoagulation given in 1 or 4 sittings. Arch Ophthalmol. 2009;127(2):132–40. doi: 10.1001/archophthalmol.2008.565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.The Diabetic Retinopathy Clinical Research Network. Randomized trial evaluating short-term effects of intravitreal ranibizumab or triamcinolone acetonide on macular edema following focal/grid laser for diabetic macular edema in eyes also receiving panretinal photocoagulation. Retina. 2011;31(6):1009–27. doi: 10.1097/IAE.0b013e318217d739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Diabetic Retinopathy Clinical Research Network. Randomized trial evaluating ranibizumab plus prompt or deferred laser or triamcinolone plus prompt laser for diabetic macular edema. Ophthalmology. 2010;117(6):1064–77 e35. doi: 10.1016/j.ophtha.2010.02.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Korobelnik JF, Do DV, Schmidt-Erfurth U, et al. Intravitreal aflibercept for diabetic macular edema. Ophthalmology. 2014;121(6):2247–54. doi: 10.1016/j.ophtha.2014.05.006. [DOI] [PubMed] [Google Scholar]
- 12.Ip MS, Domalpally A, Hopkins JJ, Wong P, Ehrlich JS. Long-term effects of ranibizumab on diabetic retinopathy severity and progression. Arch Ophthalmol. 2012;130(9):1145–52. doi: 10.1001/archophthalmol.2012.1043. [DOI] [PubMed] [Google Scholar]
- 13.World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191–4. doi: 10.1001/jama.2013.281053. [DOI] [PubMed] [Google Scholar]
- 14.Beck RW, Moke PS, Turpin AH, et al. A computerized method of visual acuity testing: adaptation of the early treatment of diabetic retinopathy study testing protocol. Am J Ophthalmol. 2003;135(2):194–205. doi: 10.1016/s0002-9394(02)01825-1. [DOI] [PubMed] [Google Scholar]
- 15.Aiello LP, Beck RW, Bressler NM, et al. Rationale for the diabetic retinopathy clinical research network treatment protocol for center-involved diabetic macular edema. Ophthalmology. 2011;118(12):e5–14. doi: 10.1016/j.ophtha.2011.09.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Martin DF, Maguire MG, Ying GS, Grunwald JE, Fine SL, Jaffe GJ. Ranibizumab and bevacizumab for neovascular age-related macular degeneration. N Engl J Med. 2011;364(20):1897–908. doi: 10.1056/NEJMoa1102673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Beck RW, Maguire MG, Bressler NM, Glassman AR, Lindblad AS, Ferris FL. Visual acuity as an outcome measure in clinical trials of retinal diseases. Ophthalmology. 2007;114(10):1804–9. doi: 10.1016/j.ophtha.2007.06.047. [DOI] [PubMed] [Google Scholar]
- 18.Spiegelman D, Hertzmark E. Easy SAS calculations for risk or prevalence ratios and differences. Am J Epidemiol. 2005;162(3):199–200. doi: 10.1093/aje/kwi188. [DOI] [PubMed] [Google Scholar]
- 19.SAS Institute Inc. SAS/STAT 9.3 User’s Guide. Cary, NC: SAS Institute Inc; 2011. [Google Scholar]
- 20.Antiplatelet Trialists’ Collaboration. Collaborative overview of randomised trials of antiplatelet therapy–I: Prevention of death, myocardial infarction, and stroke by prolonged antiplatelet therapy in various categories of patients. BMJ. 1994;308(6921):81–106. [PMC free article] [PubMed] [Google Scholar]
- 21.Diabetic Retinopathy Clinical Research N. Googe J, Brucker AJ, et al. Randomized trial evaluating short-term effects of intravitreal ranibizumab or triamcinolone acetonide on macular edema after focal/grid laser for diabetic macular edema in eyes also receiving panretinal photocoagulation. Retina. 2011;31(6):1009–27. doi: 10.1097/IAE.0b013e318217d739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Diabetic Retinopathy Clincical Research Network. Randomized clinical trial evaluating intravitreal ranibizumab or saline for vitreous hemorrhage from proliferative diabetic retinopathy. JAMA Ophthalmol. 2013;131(3):283–93. doi: 10.1001/jamaophthalmol.2013.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Diabetic Retinopathy Clinical Research N. Wells JA, Glassman AR, et al. Aflibercept, bevacizumab, or ranibizumab for diabetic macular edema. N Engl J Med. 2015;372(13):1193–203. doi: 10.1056/NEJMoa1414264. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


