Abstract
Background
Myocardial necrosis in the perioperative period of non-cardiac surgery is associated with short-term mortality, but the effect on long-term outcomes has not been characterized. We investigated the association between perioperative troponin elevation and long-term mortality in a retrospective study of subjects undergoing major orthopedic surgery.
Methods
We performed a long-term follow-up study of consecutive subjects undergoing hip, knee, and spine surgery between November 1, 2008 and December 31, 2009. Patient demographics and comorbidities were ascertained using a hospital administrative dataset. Perioperative myocardial necrosis and ICD-9 coded myocardial infarction (MI) were recorded. Long-term survival was assessed using the Social Security Death Index (SSDI) database. Logistic regression models were used to identify independent predictors of long-term mortality.
Results
A total of 3,075 subjects underwent orthopedic surgery. Mean age was 60.7 years and a majority of subjects (59%) were female. Post-operative troponin was measured in 1060 (34.5%) subjects. Myocardial necrosis occurred in 179 (5.3%%) subjects and MI was coded in 20 (0.7%). Over 9,096 patient-years of follow up, 111 (3.6%) deaths occurred. Long-term mortality was 16.8% among subjects with myocardial necrosis, 5.8% with a troponin in the normal range, and 1.5% when a perioperative troponin was not measured. Perioperative troponin elevation (HR 2.33, CI 1.33 – 4.10) and coded post-operative MI (adjusted HR 3.51, CI 1.44 – 8.53) were significantly associated with long-term mortality after multivariable adjustment.
Conclusions
Post-operative myocardial necrosis is common following orthopedic surgery. Myocardial necrosis is independently associated with long-term mortality and may be used to identify subjects at higher risk for cardiovascular events who may benefit from aggressive management of cardiovascular risk factors.
Background
Cardiovascular risks of orthopedic surgery impose a significant burden of morbidity and mortality in the United States. More than 110 million adults report a musculoskeletal condition, leading to more than 1.5 million hip, knee, and spine surgeries each year.1,2 In 2011, musculoskeletal surgeries represented nearly 24% of all inpatient operating room procedures, with steady increases in volume over the preceding decade.3 Although orthopedic procedures have historically been considered to confer only an intermediate risk of death and non-fatal myocardial infarction (MI),4 cardiovascular events are not uncommon. Perioperative myocardial necrosis and infarction, detected by post-operative elevations in serum cardiac troponin isoforms, occur with an incidence that ranges anywhere from 1% to 17% following orthopedic surgery.5–14
The short-term prognostic significance of perioperative myocardial necrosis in non-cardiac surgery is well established. In large prospective registries, peak perioperative troponin elevations correlate with 30-day mortality, and numerous smaller studies of non-cardiac surgery support these findings.15–17 Although the association between perioperative troponin elevation and short-term outcomes is clear, long-term consequences of post-operative myocardial necrosis remain uncertain. Few studies of subjects undergoing orthopedic surgery have examined long-term outcomes following myocardial necrosis.10,12 We therefore investigated the association between perioperative troponin elevation and long-term mortality in a large, retrospective, single-center study of subjects undergoing major orthopedic surgery.
Methods
Study Design
We performed long-term follow-up to a retrospective cohort analysis of consecutive adults undergoing orthopedic surgery. A full description of the methods has been described elsewhere.8 Briefly, consecutive adults undergoing knee, hip, or spine surgery between November 1, 2008 and December 31, 2009 at a large tertiary care academic medical center were eligible. Clinical data were obtained from hospital administrative database (Decision Support System), hospital laboratory database, and from retrospective record review. Data quality was assessed by reviewing a random sample of 10% of all medical and laboratory records. Long-term survival was assessed using the Social Security Death Index (SSDI) database, with the query performed on July 13, 2012. This study was approved by the Institutional Review Board with an informed consent waiver.
Subjects & Outcomes
Patient baseline demographics, clinical history, and comorbidities were ascertained using a hospital administrative dataset. International Classification of Disease (ICD)-9 procedure codes extremity (81.5x), other procedures on spine (81.6x). ICD-9 diagnosis codes were used to ascertain comorbidities present on admission, including a history of diabetes mellitus (250.x), heart failure (HF) (402.01, 402.11, 402.91, 428, 428.1, 428.2, 428.22, 428.23, 428.3, 428.32, 428.33, 428.4, 428.42, 428.43, 428.9), and stroke (V12.54, 438.0–438.9). Coronary artery disease (CAD) was determined by an ICD-9 diagnosis code indicating previous MI (412.x), previous cardiac revascularization procedure (coronary artery bypass graft surgery or percutaneous coronary intervention, 36.x), or coronary artery disease (412, 414.x).
Subjects were stratified by whether or not troponin measurement was performed in the post-operative period, as previous analyses suggest that subjects in whom post-operative troponins are not measured have fewer cardiovascular risk factors and may be at a lower risk for cardiovascular events.18 Post-operative myocardial necrosis and MI were recorded. Myocardial necrosis was defined by an elevation in troponin level greater than the 99th percentile upper reference limit of the assay. Myocardial infarction was defined by ICD-9 diagnosis code 410.x, not present on admission.
The primary study outcome was long-term mortality based on the Social Security Death Index (SSDI) database. Long-term survival was not available for 32 (1.0%) subjects; 25 lacked social security numbers and were censored at the time of the SSDI query. Seven subjects from the original cohort had birth dates that were incongruent with information from the SSDI and were excluded from this analysis.
Statistical Analysis
Normally distributed continuous variables were displayed as means ± standard deviation (SD) and were compared using the Student’s t test. Categorical variables were displayed as frequencies and percentages and were compared by Chi-square and Fisher exact tests. Baseline characteristics associated with outcomes were estimated with univariate logistic regression models and reported as hazard ratios (HR) with 95% confidence intervals (CI). Time-to-event Cox proportional hazards analyses were used to examine the association between dichotomized myocardial necrosis and mortality, while controlling for potential demographic, clinical, and procedural confounders. Kaplan-Meier plots were generated to illustrate long-term survival by post-operative troponin. Statistics were calculated using SPSS 20 (IBM SPSS Statistics, Armonk, NY). Two-tailed p-values < 0.05 were considered to be statistically significant for all tests.
Results
A total of 3,075 subjects underwent orthopedic surgery of the spine, hip, or knee and were included in the analysis. Mean age was 60.7 years and a majority of subjects (59%) were female. Baseline patient characteristics, cardiovascular comorbidities, and procedural characteristics are displayed in Table 1. Troponin was measured in 1060 subjects (34.5%). Myocardial necrosis occurred in 179 cases (16.9% of subjects who had a troponin measured and 5.3% overall). Mean follow-up was 3.0 ± 0.5 years following surgery. Over 9,096 patient-years of follow up, 111 (3.6%) deaths occurred, with 53 (1.7%) and 90 (2.9%) deaths by 12 months and 24 months, respectively. Subjects who died during follow up were older, more likely to be male, and to have undergone emergent orthopedic surgery. Univariate predictors of long-term mortality are displayed in Table 2. The incidence of perioperative myocardial necrosis was significantly higher in subjects who died during long-term follow up overall (27.0% vs. 5.0%, p <.0001). The incidence of coded perioperative MI was also significantly higher among subjects who died during long-term follow-up in comparison to surviving subjects (6.3% vs. 0.4%, p<0.001).
Table 1.
Baseline characteristics
| Overall Population (n=3075) | |
|---|---|
| Age (yr), mean | 60.74 ± 13.29 |
| Female | 1816 (59.1) |
| Race | |
| White | 1999 (65.0) |
| Black | 439 (14.3) |
| Hispanic | 415 (13.5) |
| Other | 222 (7.2) |
| BMI (kg/m2), mean | 29.60 ± 6.63 |
| Admission Type | |
| Elective | 2895 (94.1) |
| Emergency or Urgent | 180 (5 9) |
| Surgery | |
| Procedure | |
| Spine | 1161 (37.8) |
| Knee | 996 (32.4) |
| Hip | 918 (29.9) |
| RCRI Score (Lee et. al, 1999) | |
| CAD | 326 (10.6) |
| HF | 86 (2.8) |
| Stroke/TIA | 18 (0.6) |
| Creatinine > 2 mg/dL | 15 (0.5) |
| Diabetes Mellitus | 446 (14.5) |
BMI: body mass index; CAD: coronary artery disease; HF: heart failure, RCRI: Revised Cardiac Risk Index, TIA: Transient ischemic attack
Table 2.
Univariate analysis of baseline characteristics and long-term mortality
| Death (n=111) | No Death (n=2964) | Univariate Analysis | ||
|---|---|---|---|---|
| Hazard Ratio (95% CI) | P value | |||
| Age (yr), mean | 69.7 ± 15.4 | 60.41 ± 13.1 | 1.06 (1.04,1.08) | <0.001 |
| Female | 54 (48.6) | 1762 (59.4) | 0.65 (0.45,0.94) | 0.02 |
| Race | ||||
| White | 82 (73.9) | 1917 (64.7) | 1.00 (0. 51,2.0) | 0.99 |
| Black | 8(7.2) | 4 31 (14.5) | 0.44 (0.17,1.14) | 0.09 |
| Hispanic | 12 (10.8) | 403 (13.6) | 0.70 (0.30,1.67) | 0.42 |
| Other | 9 (8.1) | 213 (7.2) | 1 | 1 |
| BMI (kg/m2), mean | 26.4 ± 4.7 | 29.8 ± 6.7 | 0.91 (0.87,0.95) | <0.001 |
| Admission Type | ||||
| Elective | 65 (58.6) | 2830 (95.5) | 1 | 1 |
| Emergency or Urgent | ||||
| Surgery | 46 (41.4) | 134 (4.5) | 13.37 (9.16,19.51) | <0.001 |
| Procedure | ||||
| Spine | 50 (45. 0) | 1111 (37.5) | 0.94 (0.62,1.42) | 0.76 |
| Knee | 19 (17.1) | 977 (33) | 0.41 (0.24,0.71) | 0.001 |
| Hip | 42 (37.8) | 876 (29.6) | 1 | 1 |
| RCRI Score | ||||
| CAD | 27 (24.3) | 299 (10.1) | 2.79 (1.81,4.30) | <0.001 |
| HF | 18 (16.2) | 68 (2.3) | 7.6 (4.59,12.6) | <0.001 |
| Stroke/TIA | 2 (1.8) | 16 (0.5) | 3.26 (0.81,13.2) | 0.1 |
| Creatinine > 2 mg/dL | 3 (2.7) | 12 (0.4) | 6.19 (1.97,19.5) | 0.002 |
| Diabetes Mellitus | 26 (23.4) | 420 (14.2) | 1.84 (1.18,2.85) | 0.01 |
The 179 subjects who developed perioperative myocardial necrosis had significantly higher long-term mortality (16.8% vs. 2.8%, p<.0001) following orthopedic surgery. In multivariable models adjusting for demographic and clinical variables, perioperative troponin elevation was associated with long-term mortality (HR 2.33, CI 1.33 – 4.10) (Table 3). Associations between positive post-operative troponin and long-term mortality persisted in landmark analyses of events up to 12 months (adjusted HR 2.45, CI 1.12 – 5.34), between 12–24 months (adjusted HR 2.90 CI 1.13 – 7.42), but not after 24 months (adjusted HR 0.97 CI 0.17 – 5.39). Among subjects with myocardial necrosis, 20 had an ICD-9 coded post-operative MI. Subjects with coded post-operative MI had significantly higher mortality over study follow up (35.0% vs. 3.4%, p <.0001). Post-operative MI was also strongly associated with mortality in multivariable analysis (adjusted HR 3.51, CI 1.44 – 8.53).
Table 3.
Multivariate Cox Proportional Hazards regression analysis of troponin elevation and long-term mortality
| Multivariate Analysis | ||
|---|---|---|
| Hazard Ratio (95% CI) | P value | |
| Unadjusted | 6.57 (4.32, 9.99) | <0.001 |
| Adjusted for age, sex, race | 3.76 (2.39, 5.91) | <0.001 |
| Adjusted for age, sex, race, admission type, procedure | 2.71 (1.69, 4.36) | <0.001 |
| Multivariable adjusted** | 2.33 (1.33, 4.10) | 0.003 |
Adjusted for age, sex, race, admission type (elective vs. emergency/urgent surgery), procedure, CAD,
HF, stroke/TIA, creatinine > 2 mg/dL, DM
Subjects undergoing urgent rather than elective orthopedic procedures had a higher frequency of perioperative troponin measurement (66.1% vs. 32.5%, p<.0001), myocardial necrosis (18.3% vs. 5.0%, p<.0001), and greater long-term mortality (25.6% vs. 2.2%, p<.0001). After excluding subjects who underwent urgent surgery from the analysis, perioperative troponin elevation was still significantly associated with long-term mortality (HR 3.40, CI 1.65 – 7.03).
Measurement of perioperative serum troponin, regardless of the outcome of the laboratory test, was also associated with mortality. Long-term mortality was 16.8% (30) among subjects with an abnormally elevated troponin, 5.8% (51) for those with a normal troponin measurement, and 1.5% (30) among subjects for whom perioperative troponin was not measured. In comparison to subjects without a post-operative troponin measurement, elevated (HR 5.64, CI 2.74 – 11.62) and normal (HR 2.99, CI 1.69 – 5.29) post-operative troponin measurements remained significantly associated with mortality after multivariable adjustment. Kaplan Meier curves of long-term survival associated with perioperative troponin measurement are shown in Figure 1.
Figure 1.
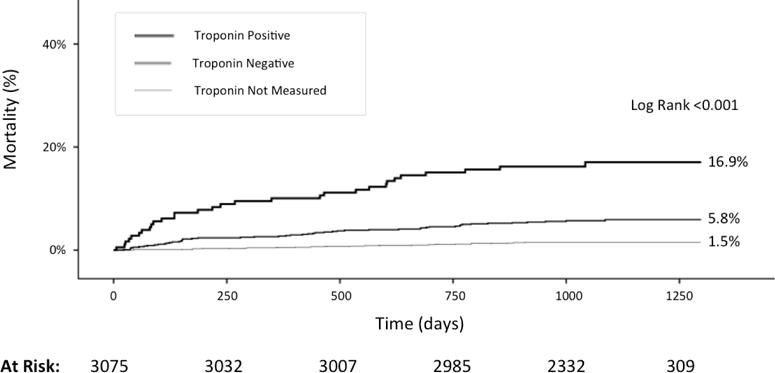
Long-term post-operative mortality by troponin measurement.
Sensitivity analyses of high-risk patient subsets with established CAD and advanced chronic kidney disease at the time of surgery revealed similar associations between troponin and mortality (Figure 2). Overall, subjects with advanced chronic kidney disease (eGFR <60 mL/min) had significantly higher mortality than subjects without renal impairment (eGFR ≥60 mL/min), (7.9% vs. 2.9%, p<.0001). After excluding xx subjects with GFR <60 mL/min, myocardial necrosis was significantly associated with long-term mortality (HR 3.27, CI 1.69– 6.31). Similarly, subjects with a history of CAD had a higher long-term mortality than those without CAD (8.3% vs. 3.1%, p<.0001). After excluding xx subjects with CAD, myocardial necrosis was independently associated with long-term mortality in 2749 without CAD (HR 3.24, CI 1.67 – 6.29).
Figure 2.
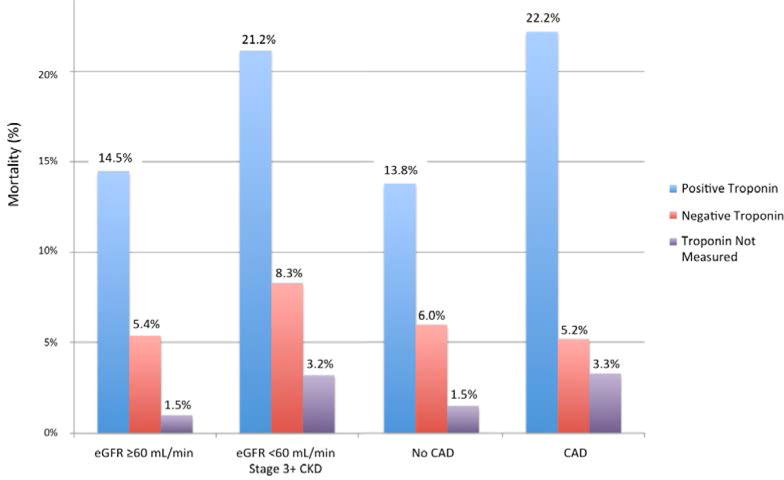
Mortality by perioperative troponin measurement: sensitivity analysis with coronary artery disease and advanced kidney disease.
Discussion
In this large, retrospective, single-center study of subjects undergoing major orthopedic surgery, post-operative myocardial necrosis occurred in 5.8% of subjects and was a significant predictor of long-term mortality, even after adjustment for baseline and procedural risk factors. The present study is the largest series of subjects undergoing major orthopedic surgery with troponin measurements and long-term follow-up. Our data support the findings of small orthopedic surgery studies,9–14,19,20 and augment the short-term results of large prospective registries of subjects undergoing non-cardiac surgery.15,16 In the large, prospective Vascular Events in Non-Cardiac Surgery Subjects Cohort Evaluation (VISION) study, elevated perioperative troponin elevations correlated with 30-day mortality.15
In this study, serum troponin elevations following orthopedic surgery were associated with increased mortality at 3 years. Although 17.1% of deaths occurred within 90 days of the post-operative myocardial necrosis, a steady accrual of events occurred over long-term follow-up (Figure 1). Even after excluding subjects with an established diagnosis of CAD, perioperative myocardial necrosis remained strongly associated with long-term mortality. Thus, myocardial necrosis is a marker of increased risk and may identify subjects who warrant aggressive reduction of cardiovascular risk factors. Routine measurements of troponin in the post-operative period may be warranted in certain subjects, even those who are asymptomatic, as perioperative ischemia causing myocardial necrosis is clinically silent in up to 96% of cases.16
The mortality risk associated with a negative post-operative troponin was another intriguing study finding. The hazard for mortality associated with negative troponins persisted after multivariable adjustment for traditional cardiovascular risk factors, suggesting that clinical parameters other than those incorporated into standard perioperative cardiovascular risk scores may identify high-risk subjects.21 Further investigation is warranted to identify non-traditional clinical factors prompting diagnostic testing for perioperative ischemia. Integrating these parameters into perioperative risk models may enhance model performance and improve perioperative management.
Although perioperative troponin elevations are strongly linked with mortality, mechanisms of myocardial necrosis remain elusive. In some instances, myocardial necrosis may reflect coronary plaque destabilization, rupture, and thrombosis (Type 1 MI). More commonly, however, perioperative myocardial necrosis is due to imbalances in myocardial oxygen supply and demand related to anemia, hypoxia, or hypotension, often the setting of stable CAD (Type 2 MI).7 Volume overload may also precipitate increased myocardial wall tension and exacerbate supply and demand mismatch. Endothelial dysfunction, microvascular coronary disease, aberrant inflammatory pathways, and heightened platelet activity may be contributing mechanisms.22,23
Just as the pathophysiology of myocardial necrosis is uncertain, so is the optimal management of subjects who develop myocardial injury in the perioperative period.24 Antiplatelet agents and statins may yield benefits, but few trials have evaluated conventional methods of cardiovascular risk reduction in subjects with myocardial necrosis following noncardiac surgery. In one small study, 70 elderly subjects undergoing emergency orthopedic surgery with postoperative troponin elevation were randomized to standard care versus intensive cardiology monitoring and evaluation. Although aspirin and beta-blocker use was significantly higher in the group randomized to cardiology evaluation, no differences in mortality were observed at 1 year.25 In contrast, in an observational sub-analysis of the original Perioperative Ischemic Evaluation trial (POISE) of adults ≥45 years undergoing non-cardiac surgery, aspirin and statin therapy were associated with reduced risk of 30-day mortality in subjects who had a perioperative MI within 30 days of randomization.26 Given the long-term post-operative mortality we observed, prolonged durations of medical therapy might be necessary to achieve reductions in cardiovascular risk.
There are some notable limitations of this retrospective observational study. First, medical comorbidities were identified through hospital laboratory systems and ICD9 coding, and unmeasured confounders and misclassification bias may affect study findings. Second, serum troponin assays were performed at the discretion of providers in only 35% of subjects. Although troponin measurements were generally performed in subjects with the greatest burden of cardiovascular risk factors and the highest likelihood for events, the incidence of myocardial necrosis may be underestimated. Third, the schedule for troponin measurement was not standardized, which may have affected peak values, although more than half of post-operative myocardial injury following non-cardiac surgery is detected on the first post-operative day and most cases occur within three days of surgery.16 Similarly, baseline pre-operative troponin values were not measured. Subjects with pre-existing heart failure, ventricular hypertrophy, end-stage renal disease, and silent myocardial ischemia can have elevated serum troponin levels, although these levels would be expected to rise in the setting of additional ischemia in the perioperative period. Cases with troponin levels peaking prior to surgery and declining in the post-operative period cannot be excluded. However, this population is expected to be small and unlikely to have significantly biased study findings. Fourth, chest pain, ECG changes, and other clinical criteria necessary for adjudication of MI were not reliably captured and were not incorporated into the analysis. Fifth, although long-term mortality data was available for 99.2% of subjects, vital status could not be queried for 25 subjects. These subjects were censored at the time of the SSDI query. Sixth, causes of death among subjects in this study were not available. Further study into the mechanisms of death in subjects with perioperative myocardial necrosis is necessary.
In conclusion, post-operative myocardial necrosis is common following orthopedic surgery and is an independent predictor of long-term mortality. Clinically indicated measurement of serum troponin in the perioperative period, regardless of the outcome of the assay, is poor prognostic predictor. Additional trials are necessary to determine the optimal management of subjects who develop perioperative myocardial necrosis. Pending further investigation, initiation of targeted medical therapy for cardiovascular risk reduction should be strongly considered for subjects with perioperative myocardial necrosis given the substantial risks of long-term mortality in this population.
References
- 1.Steiner C, Andrews R, Barrett M, Weiss A. HCUP Projections Report # 2012–03. U.S. Agency for Healthcare Research and Quality; 2012. HCUP Projections: Mobility/Orthopedic Procedures 2003 to 2012. Online September 20, 2012. Available: http://www.hcup-us.ahrq.gov/reports/proiections/2012-03.pdf. [Google Scholar]
- 2.Haralson RH, 3rd, Zuckerman JD. Prevalence, health care expenditures, and orthopedic surgery workforce for musculoskeletal conditions. JAMA. 2009 Oct 14;302(14):1586–1587. doi: 10.1001/jama.2009.1489. [DOI] [PubMed] [Google Scholar]
- 3.Weiss AJ, Elixhauseer A. HCUP Statistical Brief #171. Agency for Healthcare Research and Quality; Rockville, MD: Mar, 2014. Trends in Operating Room Procedures in U.S. Hospitals, 2001–2011. [PubMed] [Google Scholar]
- 4.Fleisher LA, Beckman JA, Brown KA, et al. ACC/AHA 2007 guidelines on perioperative cardiovascular evaluation and care for noncardiac surgery: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines on Perioperative Cardiovascular Evaluation for Noncardiac Surgery) developed in collaboration with the American Society of Echocardiography, American Society of Nuclear Cardiology, Heart Rhythm Society, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, and Society for Vascular Surgery. J Am Coll Cardiol. 2007 Oct 23;50(17):e159–241. doi: 10.1016/j.jacc.2007.09.003. [DOI] [PubMed] [Google Scholar]
- 5.Landesberg G, Beattie WS, Mosseri M, Jaffe AS, Alpert JS. Perioperative myocardial infarction. Circulation. 2009 Jun 9;119(22):2936–2944. doi: 10.1161/CIRCULATIONAHA.108.828228. [DOI] [PubMed] [Google Scholar]
- 6.Adams JE, 3rd, Bodor GS, Davila-Roman VG, et al. Cardiac troponin I. A marker with high specificity for cardiac injury. Circulation. 1993 Jul;88(1):101–106. doi: 10.1161/01.cir.88.1.101. [DOI] [PubMed] [Google Scholar]
- 7.Thygesen K, Alpert JS, Jaffe AS, et al. Third universal definition of myocardial infarction. J Am Coll Cardiol. 2012 Oct 16;60(16):1581–1598. doi: 10.1016/j.jacc.2012.08.001. [DOI] [PubMed] [Google Scholar]
- 8.Oberweis BS, Nukala S, Rosenberg A, et al. Thrombotic and bleeding complications after orthopedic surgery. Am Heart J. 2013 Mar;165(3):427–433.e421. doi: 10.1016/j.ahj.2012.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jules-Elysee K, Urban MK, Urquhart B, Milman S. Troponin I as a diagnostic marker of a perioperative myocardial infarction in the orthopedic population. Journal of clinical anesthesia. 2001 Dec;13(8):556–560. doi: 10.1016/s0952-8180(01)00337-3. [DOI] [PubMed] [Google Scholar]
- 10.Ausset S, Auroy Y, Lambert E, et al. Cardiac troponin I release after hip surgery correlates with poor long-term cardiac outcome. European journal of anaesthesiology. 2008 Feb;25(2):158–164. doi: 10.1017/S0265021507001202. [DOI] [PubMed] [Google Scholar]
- 11.Urban MK, Jules-Elysee K, Loughlin C, Kelsey W, Flynn E. The one year incidence of postoperative myocardial infarction in an orthopedic population. HSS journal: the musculoskeletal journal of Hospital for Special Surgery. 2008 Feb;4(1):76–80. doi: 10.1007/s11420-007-9070-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chong CP, Lam QT, Ryan JE, Sinnappu RN, Lim WK. Incidence of post-operative troponin I rises and 1-year mortality after emergency orthopaedic surgery in older subjects. Age and ageing. 2009 Mar;38(2):168–174. doi: 10.1093/ageing/afn231. [DOI] [PubMed] [Google Scholar]
- 13.Ausset S, Auroy Y, Verret C, et al. Quality of postoperative care after major orthopedic surgery is correlated with both long-term cardiovascular outcome and troponin Ic elevation. Anesthesiology. 2010 Sep;113(3):529–540. doi: 10.1097/ALN.0b013e3181eaacc4. [DOI] [PubMed] [Google Scholar]
- 14.Hietala P, Strandberg M, Kiviniemi T, Strandberg N, Airaksinen KE. Usefulness of troponin T to predict short-term and long-term mortality in subjects after hip fracture. Am J Cardiol. 2014 Jul 15;114(2):193–197. doi: 10.1016/j.amjcard.2014.04.026. [DOI] [PubMed] [Google Scholar]
- 15.Vascular Events In Noncardiac Surgery Subjects Cohort Evaluation Study I. Devereaux PJ, Chan MT, et al. Association between postoperative troponin levels and 30-day mortality among subjects undergoing noncardiac surgery. JAMA. 2012 Jun 6;307(21):2295–2304. doi: 10.1001/jama.2012.5502. [DOI] [PubMed] [Google Scholar]
- 16.van Waes JA, Nathoe HM, de Graaff JC, et al. Myocardial injury after noncardiac surgery and its association with short-term mortality. Circulation. 2013 Jun 11;127(23):2264–2271. doi: 10.1161/CIRCULATIONAHA.113.002128. [DOI] [PubMed] [Google Scholar]
- 17.Levy M, Heels-Ansdell D, Hiralal R, et al. Prognostic value of troponin and creatine kinase muscle and brain isoenzyme measurement after noncardiac surgery: a systematic review and meta-analysis. Anesthesiology. 2011 Apr;114(4):796–806. doi: 10.1097/ALN.0b013e31820ad503. [DOI] [PubMed] [Google Scholar]
- 18.Oberweis BS, Berger JS. In reply to the letter to the editor by Paul et al. Am Heart J. 2013 Jun;165(6):e29. doi: 10.1016/j.ahj.2013.03.010. [DOI] [PubMed] [Google Scholar]
- 19.Dawson-Bowling S, Chettiar K, Cottam H, et al. T roponin T as a predictive marker of morbidity in subjects with fractured neck of femur. Injury. 2008 Jul;39(7):775–780. doi: 10.1016/j.injury.2008.01.025. [DOI] [PubMed] [Google Scholar]
- 20.Fisher AA, Southcott EN, Goh SL, et al. Elevated serum cardiac troponin I in older subjects with hip fracture: incidence and prognostic significance. Archives of orthopaedic and trauma surgery. 2008 Oct;128(10):1073–1079. doi: 10.1007/s00402-007-0554-x. [DOI] [PubMed] [Google Scholar]
- 21.Lee TH, Marcantonio ER, Mangione CM, et al. Derivation and prospective validation of a simple index for prediction of cardiac risk of major noncardiac surgery. Circulation. 1999 Sep 7;100(10):1043–1049. doi: 10.1161/01.cir.100.10.1043. [DOI] [PubMed] [Google Scholar]
- 22.Sandoval Y, Smith SW, Apple FS. Type 2 myocardial infarction: the next frontier. Am J Med. 2014 Jun;127(6):e19. doi: 10.1016/j.amjmed.2014.02.027. [DOI] [PubMed] [Google Scholar]
- 23.Oberweis BS, Cuff G, Rosenberg A, et al. Platelet aggregation and coagulation factors in orthopedic surgery. Journal of thrombosis and thrombolysis. 2014 Nov;38(4):430–438. doi: 10.1007/s11239-014-1078-1. [DOI] [PubMed] [Google Scholar]
- 24.Adesanya AO, de Lemos JA, Greilich NB, Whitten CW. Management of perioperative myocardial infarction in noncardiac surgical subjects. Chest. 2006 Aug;130(2):584–596. doi: 10.1016/S0012-3692(15)51881-3. [DOI] [PubMed] [Google Scholar]
- 25.Chong CP, van Gaal WJ, Ryan JE, Profitis K, Savige J, Lim WK. Does cardiology intervention improve mortality for post-operative troponin elevations after emergency orthopaedic-geriatric surgery? A randomised controlled study. Injury. 2012 Jul;43(7):1193–1198. doi: 10.1016/j.injury.2012.03.034. [DOI] [PubMed] [Google Scholar]
- 26.Devereaux PJ, Xavier D, Pogue J, et al. Characteristics and short-term prognosis of perioperative myocardial infarction in subjects undergoing noncardiac surgery: a cohort study. Ann Intern Med. 2011 Apr 19;154(8):523–528. doi: 10.7326/0003-4819-154-8-201104190-00003. [DOI] [PubMed] [Google Scholar]


