Abstract
Minority populations in the United States receive fewer effective health services than whites. Using 2006–11 Medicare administrative data, we found no consistent, corresponding protection against receipt of ineffective health services. Compared with whites, black and Hispanic beneficiaries often received more of the 11 low-value services studied. In targeting health care quality disparities, policymakers must consider both underuse and overuse.
Studies have long shown stark differences in the receipt of effective care across patient races and ethnicities in the United States; little is known, however, about whether those differences extend to receipt of low-value care (1–4). Recent and growing efforts to define low-value care permit a more comprehensive picture of the quality of health care received by minority populations in the United States (5–7). Low-value tests and treatments, as identified by the United States Preventive Services Task Force, the Choosing Wisely initiative, and other organizations, are unnecessary and economically inefficient; many are potentially harmful. Common examples include inappropriate imaging for low-back pain, cervical cancer screening, and use of antibiotics (7).
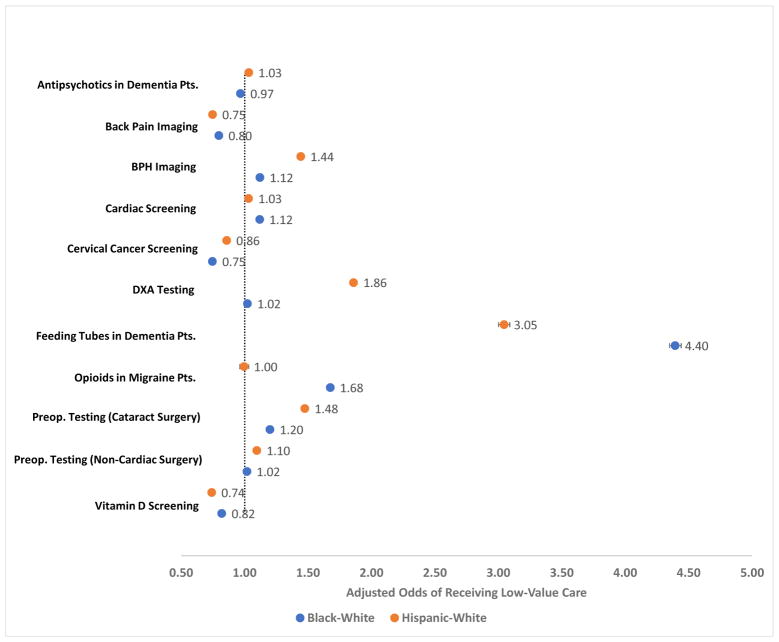
Using Medicare administrative data, we found receipt of low-value care among black and Hispanic beneficiaries was often higher than receipt among white beneficiaries (Exhibit 1). Most notably, black and Hispanic patients with dementia faced significantly greater odds of inappropriately receiving feeding tubes (black vs. white OR 4.40, CI 4.35–4.44; Hispanic vs. white OR 3.05, 95% CI 3.00–3.09). Black and Hispanic beneficiaries were also significantly more likely to receive unnecessary cardiac screening and preoperative testing, among other forms of low-value care. Our findings suggest a possible double jeopardy for minority patients: long understood to be at risk of receiving less effective care, they appear often to be at risk of receiving more ineffective care. Understanding racial and ethnic differences in the receipt of low-value care should inform policies aimed at addressing health care disparities, including the design of payer performance metrics.
Exhibit 1.
Unadjusted racial and ethnic differences in receipt of low-value care among Medicare beneficiaries, 2006–11
Sources/Notes: SOURCES Authors’ analysis of 2006–11 Medicare administrative data. NOTES Odds ratios showing the relative receipt of low-value services for black vs. white beneficiaries and Hispanic vs. white beneficiaries. 95% confidence interval indicated with bands. BPH is benign prostatic hypertrophy. DXA is dual-energy x-ray absorptiometry.
Study Data and Methods
We used 2006–11 Medicare administrative data to measure the prevalence of 11 services identified as low-value by the ABIM Foundation’s Choosing Wisely initiative among black, Hispanic, and white fee-for-service Medicare beneficiaries over age 65. We sought services reliably measurable through claims and applicable to patients of Medicare-eligible age. The 11 services included inappropriate provision of the following: imaging for lower back pain; imaging for benign prostatic hypertrophy (BPH); cardiac screening; cervical cancer screening; dual-energy x-ray absorptiometry (DXA); preoperative cardiac testing (prior to cataract surgery and, separately, other non-cardiac surgery); vitamin D screening; antipsychotics in patients with dementia; feeding tubes in patients with dementia; and opioids or butalbital in patients with migraines (Appendix Exhibit 1) (8).
We used diagnostic and procedure codes to generate cohorts of Medicare beneficiaries at risk of and exposed to the low-value services, as described elsewhere (5,8). We examined differences in low-value service use by race and ethnicity by estimating black-white and Hispanic-white odds ratios (ORs) for service receipt. To account for individual-level factors that may confound measurement of differences in health care utilization across races and ethnicities, we adjusted the odds ratios using logistic regression models for age, income (median by residential ZIP code from the U.S. Census American Community Survey) (9), sex, disability status, Medicaid enrollment, risk score (Centers for Medicare and Medicaid Services Hierarchical Condition Categories) (10), and health care system utilization (log of the number of outpatient clinician visits and proportion of all outpatient visits — including specialty care — to primary care providers in the calendar year), as well as fixed effects for year and the beneficiary’s health care market (hospital referral region) (11). To explore the relationship between health care utilization and differential receipt of low-value care, we conducted a secondary analysis in which we included an interaction for race and utilization (as defined above) in our regression model. The study was approved by an institutional review board.
Study Results
Black, white, and Hispanic Medicare populations studied were qualitatively similar in terms of age, percent female, risk score, number of outpatient visits, and proportion of outpatient visits to primary care (Exhibit 2). Black and Hispanic beneficiaries tended to live in ZIP codes with lower median household income (black: $44,553; Hispanic: $50,079; white: $56,580), were more likely to be disabled (black: 36.4%; Hispanic: 26.3%; white: 15.3%), and more likely to be enrolled in Medicaid (black: 40.3%; Hispanic: 51.9%; white: 13.1%).
EXHIBIT 2.
Characteristics of the study population
| Black | Hispanic | White | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| Beneficiary Characteristics | Mean | SD | Mean | SD | Mean | SD |
| Age (Mean Years) | 69.3 | 4.7 | 70.7 | 3.6 | 74.0 | 2.7 |
| Female (%) | 58.1 | 6.0 | 53.7 | 7.0 | 55.8 | 5.6 |
| Income (Median Household $) | 44,553.2 | 804.7 | 50,079.4 | 982.7 | 56,580.1 | 558.5 |
| Disability (%) | 36.4 | 14.0 | 26.3 | 11.2 | 15.3 | 6.9 |
| Medicaid (%) | 40.3 | 7.8 | 51.9 | 8.3 | 13.1 | 3.6 |
| Risk Score (Mean) | 1.0 | 0.0 | 1.0 | 0.2 | 0.9 | 0.2 |
| Outpatient Visits (Mean N) | 9.8 | 2.3 | 10.6 | 2.6 | 10.8 | 1.8 |
| Outpatient Visits to Primary Care (%) | 46.9 | 2.3 | 46.3 | 2.1 | 42.8 | 2.3 |
Sources/Notes: SOURCES Authors’ analysis of 2006–11 Medicare administrative data and 2006–10 American Community Survey data. NOTES Reported values for beneficiary characteristics reflect mean across populations for each of the 11 low-value care measures, weighted by the person-years included in each measure cohort. The weighted standard deviation across the 11 measures is in parentheses. Income reflects median household income in beneficiary’s ZIP code of residence. Risk score calculated using the Centers for Medicare and Medicaid Services Hierarchical Condition Categories. Proportion female does not include sex-specific measures (BPH imaging, cervical cancer screening, and DXA testing).
We found receipt of low-value care among black and Hispanic beneficiaries was often qualitatively higher than receipt among white beneficiaries (Exhibit 3). For example, 4.6% of white Medicare patients with dementia received a feeding tube, as compared with 17.4% of black and 12.8% of Hispanic Medicare patients with dementia. Similarly, 33.8% of black beneficiaries received opioid or butalbital prescriptions for the treatment of a migraine (vs. 23.4% of white beneficiaries) and 16.2% of Hispanic beneficiaries inappropriately received bone density testing (vs. 9.4% of white beneficiaries).
EXHIBIT 3.
Unadjusted prevalence of low-value care receipt by race and ethnicity
| Black | Hispanic | White | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| Measures | % | N | % | N | % | N |
| Antipsychotics in Dementia Pts. | 28.7 | 417,583 | 28.9 | 235,091 | 27.6 | 2,812,206 |
| Back Pain Imaging | 19.4 | 3,996,508 | 18.4 | 2,468,265 | 23.2 | 37,667,954 |
| BPH Imaging | 3.4 | 544,476 | 4.3 | 442,848 | 3.1 | 7,222,671 |
| Cardiac Screening | 16.6 | 1,509,836 | 15.5 | 1,291,648 | 15.1 | 14,578,573 |
| Cervical Cancer Screening | 7.4 | 5,284,232 | 8.6 | 3,089,300 | 9.7 | 74,149,624 |
| DXA Testing | 9.6 | 390,236 | 16.2 | 290,782 | 9.4 | 4,676,292 |
| Feeding Tubes in Dementia Pts. | 17.4 | 359,848 | 12.8 | 177,775 | 4.6 | 2,997,974 |
| Opioids in Migraine Pts. | 33.8 | 38,409 | 23.3 | 61,641 | 23.4 | 842,486 |
| Preop. Testing (Cataract Surgery) | 17.3 | 449,800 | 20.5 | 324,159 | 14.9 | 5,999,819 |
| Preop. Testing (Non–Cardiac Surgery) | 44.8 | 173,530 | 46.7 | 124,461 | 44.4 | 2,908,367 |
| Vitamin D Screening | 7.5 | 10,846,269 | 6.8 | 6,257,092 | 9.0 | 101,377,303 |
Sources/Notes: SOURCES Authors’ analysis of 2006–11 Medicare administrative data. NOTES N reflects person-years included in analysis.
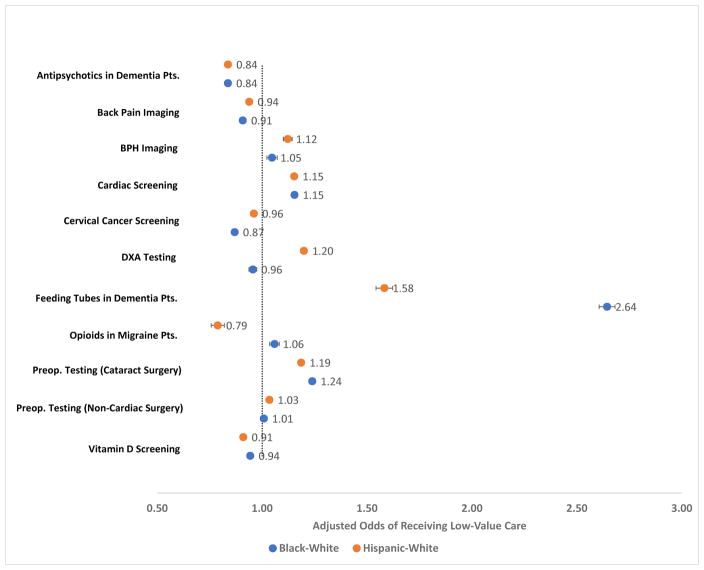
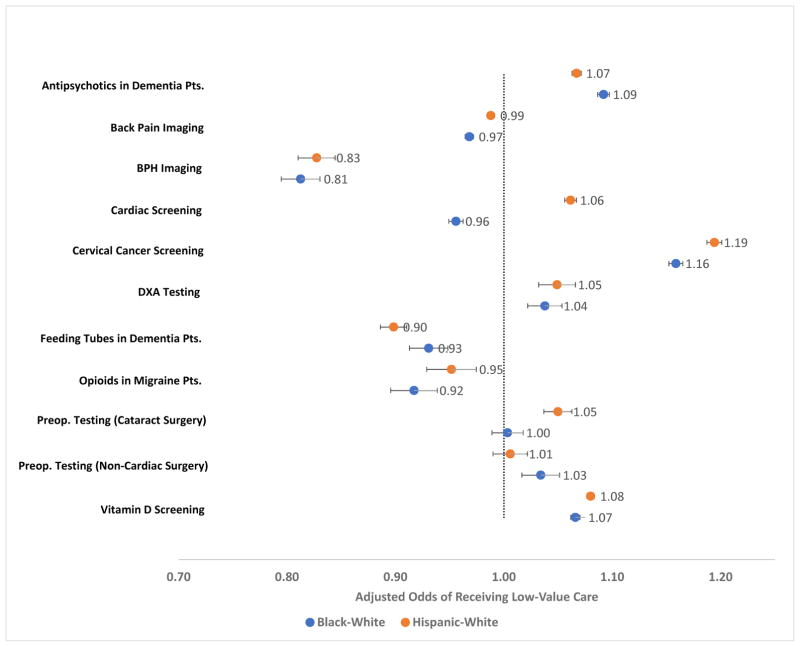
In total, receipt of low-value care among black beneficiaries was significantly higher than receipt among white beneficiaries for seven of the 11 services (Exhibit 1). After adjustment for covariates, receipt of low-value care was significantly higher among black beneficiaries for five of the 11 services (Exhibit 4). Similarly, receipt of low-value care among Hispanic beneficiaries was significantly higher than receipt among white beneficiaries for seven of the 11 services before and six services after adjustment for covariates. Adjusted relative odds of receipt were highest for inappropriate feeding tube placement in beneficiaries with dementia (black vs. white OR 2.64, CI 2.60–2.68; Hispanic vs. white OR 1.58, 95% CI 1.54–1.62). Relative receipt was lowest for inappropriate use of antipsychotics in black beneficiaries with dementia (OR 0.84, 95% CI 0.83–0.84) and for inappropriate use of opioid prescriptions for the treatment of migraines among Hispanic beneficiaries (OR 0.79, 95% CI 0.77–0.81). Greater utilization of the health care system, defined as log of the number of outpatient clinician visits, was associated with higher rates of low-value care for five measures among black beneficiaries and for six measures among Hispanic beneficiaries, relative to White beneficiaries (Exhibit 5, Appendix Exhibit 2) (8).
Exhibit 4.
Adjusted racial and ethnic differences in receipt of low-value care among Medicare beneficiaries, 2006–11
Sources/Notes: SOURCES Authors’ analysis of 2006–11 Medicare administrative data and 2006–10 American Community Survey data.
NOTES Odds ratios showing the relative receipt of low-value services for black vs. white beneficiaries and Hispanic vs. white beneficiaries. All odds ratios have been adjusted using logistic regression for individual-level characteristics, including age, income, sex, disability status, Medicaid enrollment, risk score, log of number of outpatient clinician visits, percent of outpatient visits to primary care, and fixed effects for a given beneficiary’s hospital referral region and year. 95% confidence interval indicated with bands. BPH is benign prostatic hypertrophy. DXA is dual-energy x-ray absorptiometry.
Exhibit 5.
Adjusted racial and ethnic differences in the association between outpatient clinician visits and receipt of low-value care among Medicare Beneficiaries, 2006–11
Sources/Notes: SOURCES Authors’ analysis of 2006–11 Medicare administrative data and 2006–10 American Community Survey data. NOTES Ratio of odds ratios showing the relative receipt of low-value services for black vs. white beneficiaries and Hispanic vs. white beneficiaries given a one-point increase in the log of the number of outpatient visits (exponentiated coefficient on the interaction between the race and health care utilization variables). All results have been adjusted using logistic regression for individual-level characteristics, including age, income, sex, disability status, Medicaid enrollment, risk score, log of number of outpatient clinician visits, percent of outpatient visits to primary care, and fixed effects for a given beneficiary’s hospital referral region and year. 95% confidence interval indicated with bands. BPH is benign prostatic hypertrophy. DXA is dual-energy x-ray absorptiometry.
Discussion
For a select set of services, we find black and Hispanic Medicare beneficiaries often receive more low-value care than white beneficiaries. Despite ample evidence that minority patients generally receive fewer effective services (e.g., cancer screening and diabetes monitoring), we do not document a corresponding protective effect against receipt of low-value, potentially harmful, care. For nine of the 11 measures, we find the odds of receiving low-value care were similar for black and Hispanic beneficiaries relative to whites; this suggests differential care irrespective of specific minority race or ethnicity. Racial and ethnic differences varied considerably across the distinct low-value services studied, suggesting a singular corrective intervention is unlikely to be universally effective. The mechanisms underlying the apparent receipt of more ineffective care among minority beneficiaries for some services remains unclear, but warrant rigorous exploration and explicit targeting by quality improvement efforts.
Underuse of effective care among black and Hispanic patients in the United States has commonly been attributed to obstacles accessing the health care system (1). In our study, the relationship between health care utilization and low-value care receipt was positive for some measures. Suggestions that greater health care utilization through improved access will reduce disparities in effective care receipt might be tempered by our findings that greater utilization may similarly increase receipt of some forms of low-value care, actually widening disparities in care quality.
Reliance on administrative claims represents an important limitation of our analysis. These claims-based measures were carefully designed to conservatively measure the prevalence of low-value care and drew heavily from published and validated claims-based algorithms. Nonetheless, our estimates of low-value care may differ from the true rates. Moreover, although we believe it is unlikely, the magnitude of the measurement error may differ by race or ethnicity, leading to bias in our primary results. Our findings echo previous studies of racial and ethnic disparities in care, including inappropriate use of opioids and feeding tubes (12,13).
The findings from this study of a select set of low-value services suggest a complex relationship between minority status and the U.S. health care system. Importantly, greater receipt of certain low-value services among black and Hispanic patients may crowd out receipt of effective care, compounding broader disparities in health care and health outcomes. As the health care community wrestles with new ways to incentivize quality, these findings highlight how efforts aimed at improving quality ideally would assess the experience of minority beneficiaries, addressing both health care underuse and overuse. Health care performance metrics are now beginning to specifically target disparities (14); experimentation with such metrics tied to incentive regimes may accelerate correction of the long-understood racial and ethnic differences in care that our study reveals to be multi-dimensional.
Conclusion
Black and Hispanic Medicare beneficiaries often receive more low-value care than white beneficiaries. Understanding racial and ethnic differences in the receipt of low-value care should inform the design of policies and payment models aimed at addressing health care disparities, especially importance of improving quality relative to access, as well as the complex interplay between underuse and overuse.
Supplementary Material
References
- 1.Smedley BD, Stith AY, Nelson AR, editors. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academies Press; 2003. [PubMed] [Google Scholar]
- 2.Kressin NR, Petersen LA. Racial differences in the use of invasive cardiovascular procedures: review of the literature and prescription for future research. Ann Intern Med. 2001 Sep 4;135(5):352–66. doi: 10.7326/0003-4819-135-5-200109040-00012. [DOI] [PubMed] [Google Scholar]
- 3.Mayberry RM, Mili F, Ofili E. Racial and ethnic differences in access to medical care. Med Care Res Rev. 2000;57( Suppl 1):108–45. doi: 10.1177/1077558700057001S06. [DOI] [PubMed] [Google Scholar]
- 4.Kressin NR, Groeneveld PW. Race/Ethnicity and Overuse of Care: A Systematic Review. Milbank Q. 2015;93(1):112–38. doi: 10.1111/1468-0009.12107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Colla CH, Morden NE, Sequist TD, Schpero WL, Rosenthal MB. Choosing Wisely: Prevalence and Correlates of Low-Value Health Care Services in the United States. J Gen Intern Med. 2015 Jan;1(30):221–8. doi: 10.1007/s11606-014-3070-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schwartz AL, Landon BE, Elshaug AG, Chernew ME, McWilliams JM. Measuring Low-Value Care in Medicare. JAMA Intern Med. 2014 Jan 1;2115:1–9. doi: 10.1001/jamainternmed.2014.1541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Korenstein D, Falk R, Howell Ea, Bishop T, Keyhani S. Overuse of health care services in the United States: an understudied problem. Arch Intern Med. 2012 Jan 1;172(2):171–8. doi: 10.1001/archinternmed.2011.772. [DOI] [PubMed] [Google Scholar]
- 8.To access the Appendix, click on the Appendix link in the box to the right of the article online.
- 9.American Community Survey 5-Year Data (2005–2009 to 2010–2014) [Internet] U.S. Census Bureau; 2016. [cited 2016 Oct 17]. Available from: http://www.census.gov/data/developers/data-sets/acs-survey-5-year-data.html. [Google Scholar]
- 10.Centers for Medicare and Medicaid Services; 2013. Calculating Hierarchical Condition Category (HCC) Scores Using CMS Utilization Data [Internet] [cited 2016 Oct 17]. Available from: http://www.resdac.org/resconnect/articles/173. [Google Scholar]
- 11.Geographic Crosswalks and Boundary Files [Internet] The Dartmouth Atlas of Health Care; 2016. [cited 2016 Oct 17]. Available from: http://www.dartmouthatlas.org/tools/downloads.aspx?tab=39. [Google Scholar]
- 12.Pletcher MJ, Kertesz SG, Kohn MA, Gonzales R. Trends in Opioid Prescribing by Race/Ethnicity for Patients Seeking Care in US Emergency Departments. JAMA. 2008 Jan 2;299(1) doi: 10.1001/jama.2007.64. [DOI] [PubMed] [Google Scholar]
- 13.Mitchell SL, Teno J, Roy J, Kabumoto G, Mor V. Clinical and Organizational Factors Associated With Feeding Tube Use Among Nursing Home Residents With Advanced Cognitive Impairment. JAMA. 2003 Jul 2;290(1):73–80. doi: 10.1001/jama.290.1.73. [DOI] [PubMed] [Google Scholar]
- 14.CMS Quality Strategy 2016 [Internet] Centers for Medicare and Medicaid Services; 2016. [cited 2016 Oct 17]. Available from: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/QualityInitiativesGenInfo/Downloads/CMS-Quality-Strategy.pdf. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.