Abstract
Colorectal cancer screening has clear benefits in terms of mortality reduction, however it is still underutilized and especially among medically underserved populations including African Americans, who also suffer a disproportionate colorectal cancer burden. This study consisted of a theory-driven (Health Belief Model) spiritually-based intervention aimed at increasing screening among African Americans through a community health advisor-led educational series in 16 churches. Using a randomized design, churches were assigned to receive either the spiritually-based intervention or a non-spiritual comparison, which was the same in every way except that it did not contain spiritual/religious content and themes. Trained and certified peer Community Health Advisors in each church led a series of two group educational sessions on colorectal cancer and screening. Study enrollees completed a baseline, 1-month, and 12-month follow-up survey at their churches. The interventions had significant pre-post impact on awareness of all four screening modalities, and self-report receipt of fecal occult blood test, flexible sigmoidoscopy, and colonoscopy. There were no significant study group differences in study outcomes, with the exception of fecal occult blood test utilization, where those in the non-spiritual intervention reported significantly greater pre-post change. Both of these community-engaged, theory-driven, culturally-relevant approaches to increasing colorectal cancer awareness and screening appeared to have an impact on study outcomes. While adding spiritual/religious themes to the intervention was appealing to the audience, it may not result in increased intervention efficacy.
Keywords: colorectal cancer, church-based, cancer screening, African American, health disparities, spiritually-based intervention
Colorectal cancer (CRC) is the third leading cause of cancer mortality in the US (American Cancer Society [ACS], 2011a). African Americans suffer a disproportionate burden of CRC relative to other racial/ethnic groups (ACS, 2011b). CRC is third in both incidence (7,940; 8,710) and mortality (3,520; 3,530) among African Americans in both men and women, respectively (ACS, 2011b). Though it is accepted that CRC reduces mortality rates (Mandel et al., 1993; Hardcastle et al., 1996; Kronberg, Fenger, Olsen, & Sondergaard, 1996; Faivre, et al., 1999; Cuzick, 2006), screening, particularly among African Americans, is underutilized (ACS, 2011b). Screening recommendations include for average risk patients age 50–75, one of the following: annual fecal occult blood test or fecal immunochemical test; flexible sigmoidoscopy every 5 years; barium enema every 5 years; or colonoscopy every 10 years (American Cancer Society, 2012; Agency for Healthcare Research and Quality, 2008; Rex, et al., 2000). Though some view colonoscopy as the “gold standard”, the yearly fecal immunochemical test has recently, and since this intervention has been conducted, gained recognition. This is due to increased accuracy over fecal occult blood test, accessibility, and similar results in detecting cancer compared to colonoscopy (Quintero, et al., 2012). Screening rates among non-Hispanic African Americans are 48.9% compared to 56.0% for non-Hispanic Whites (flexible sigmoidoscopy within 5 years or colonoscopy within 10 years; or fecal occult blood test); (ACS, 2011b).
Church-based approaches to CRC control
Faith-based organizations have historically played a central role in the African American community (Lincoln & Mamiya, 1990). Given the important role of religiosity in African American culture, the church has been and continues to be a viable access point for reaching African American community members. Members have looked to the church for leadership in areas other than spirituality and religion. As the most stable community organization, the church has played a significant role in such areas as the civil rights movement, economic development, and politics (Thomas, Quinn, Billingsley, & Caldwell, 1994). Many churches are also addressing health issues through health ministries, which vary from informal educational activities such as blood pressure screening, to health fairs and structured activities, to large or “mega churches” which may even have their own health centers to serve members. The church is also a place to reach individuals who may not otherwise report to a doctor’s office for screening.
Several CRC interventions have targeted faith-based venues when attempting to reach this population. The Wellness for African Americans Through Churches (WATCH) Project used lay heath advisors and tailored intervention materials to promote CRC prevention behaviors among African American church members in rural North Carolina (Campbell, et al., 2004). The WATCH project increased participants’ fruit and vegetable consumption and physical activity. The “F.A.I.T.H. study” used a faith-based educational intervention to increase CRC knowledge and colonoscopy among African Americans in church and community-based organizations (Morgan, Fogel, Tyler, & Jones, 2010). More than 25% of participants received a colonoscopy within three months compared to only 4% of participants in the delayed intervention group.
The “Your Body is the Temple” project was conducted in African American and White churches (Holt, et al., 2011). Using a community health advisor approach resulted in significant increases in CRC knowledge, perceived benefits of CRC screening, awareness of the screening modalities, and decreases in perceived barriers to screening. This intervention utilized a “spiritually-based” approach, meaning that the community health advisors provided spiritual themes and scripture to support the core health content, and the study print materials also contained spiritual themes to support the CRC screening cue to action. However, the screening data in this preliminary pre-post study was inconclusive, in some cases with self-report screening rates decreasing from pre- to post-test, reflecting participant confusion between the multiple screening modalities. This suggested that a randomized controlled trial was needed to determine whether a spiritually-based approach is effective for increasing CRC screening in African American churches.
Community health advisors
Community health advisors (CHAs) have played and continue to play a fundamental role in the community empowerment process in under-served communities. Community lay persons have fostered a trusting relationship between healthcare agencies and the community. CHAs have consistently demonstrated their effectiveness in promoting health among groups lacking access to adequate care (Witmer, Seifer, Finocchio, Leslie, O’Neil, 1995; U.S. Department of Health and Human Services, 1994a; U.S. Department of Health and Human Services, 1994b; Fendall, 1984). Ethnically, linguistically, socio-economically, and experientially indigenous to the community in which they work, these trusted “insiders” serve as cost-effective conduits of information, resources, and services often to lower-income populations (Witmer, Seifer, Finocchio, Leslie, O’Neil, 1995; Walt, 1990; Indian Health Service, 1991; Giblin, 1989). As vital links between health care consumers and providers, CHAs have addressed a broad range of community health issues in various settings (U.S. Department of Health and Human Services, 1994a; U.S. Department of Health and Human Services, 1994b). Numerous studies have shown the ability of CHAs to do effective preventive work, reduce cultural and linguistic barriers to care, help patients successfully navigate in complex health systems, and improve the quality and cost-effectiveness of care (Witmer, Seifer, Finocchio, Leslie, O’Neil, 1995).
The present study
The purpose of the present study was to evaluate the efficacy of a spiritually-based CHA intervention aimed at increasing CRC screening among African Americans in church settings, using a group randomized controlled design. The comparison (non-spiritual) intervention was equivalent in all other ways to the spiritually-based intervention except that it did not contain spiritual references or content. Both interventions were theory-based, utilizing Health Belief Model (Rosenstock, Strecher, & Becker, 1988) constructs in both the intervention content and evaluation. The following research questions were proposed: 1) did study participants actually perceive the spiritual nature of the spiritually-based intervention [e.g., manipulation check]; and 2) was the spiritually-based intervention more, less, or equally effective for primary CRC screening-related outcomes and secondary Health Belief Model-based outcomes, than the non-spiritual intervention. The present study actively encouraged patient informed choice among the four recommended methods of CRC screening, a gap recently identified in interventions (Vernon, et al., 2011).
It was expected that, 1) the spiritually-based intervention would be perceived as significantly more spiritual in nature than the non-spiritual comparison; and 2) the spiritually-based intervention would result in significant increases in CRC screening-related outcomes [awareness, screening behaviors] and greater pre-post changes in Health Belief Model-based outcomes [increased benefits, decreased barriers], relative to the non-spiritual comparison.
Method
Church recruitment
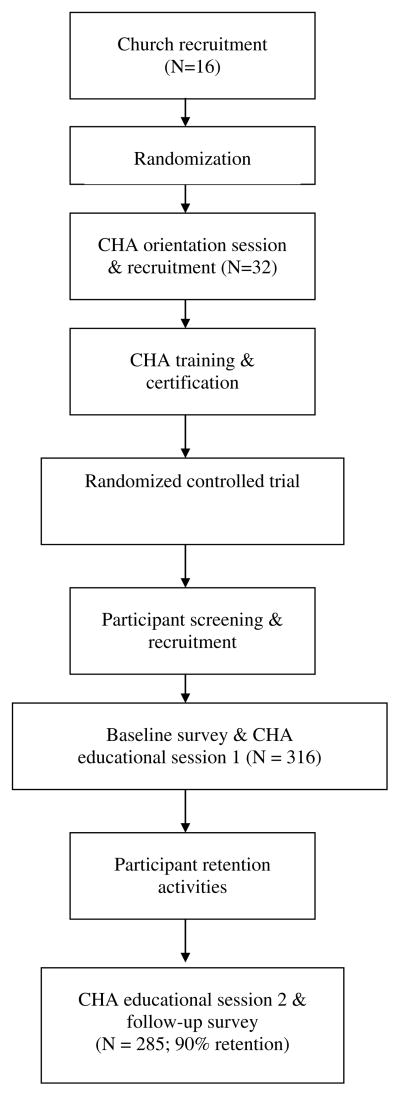
The study methodology is described in detail elsewhere (Holt, et al., In Press). All procedures were approved by the University of Alabama at Birmingham and University of Maryland Institutional Review Boards. Figure 1 provides an outline of main study procedures. A convenience sample of 16 African American churches in the Birmingham area were recruited by program staff. Each church identified two members to serve as a CHA, a lay person who receives training and can then educate their fellow community members on a health topic (Witmer, Seifer, Finocchio, Leslie, & O’Neil, 1995; US Department of Health and Human Services, 1994a, US Department of Health and Human Services, 1994b). Participating churches received an incentive in the amount of $500 to defray program costs such as space and utilities.
Figure 1.
Intervention diagram
CHA recruitment and training
Pastors or key church staff members identified 2 potential CHAs in each church. The 16 participating churches were randomly assigned to deliver either the spiritually-based or the comparison intervention. CHAs in the two study arms were trained separately to avoid intervention contamination. CHAs completed two half-days of training and then completed a mock educational session in which they practiced their delivery of the material.
Using a randomly permuted blocks technique, eight churches were randomized to conduct the spiritually-based approach and the other eight to conduct the non-spiritual intervention. The spiritually-based intervention frames core health material with spiritual themes. The non-spiritual comparison intervention covered the same CRC content but did not involve spiritually-based material. Intervention development is described in detail elsewhere (Holt, et al., 2009).
Participant recruitment and screening
Each church had a recruitment goal of 30–35 individuals age 50–74. Individuals were told about the project by the CHAs and/or in church announcements, and invited to attend a series of two educational sessions about CRC. Participants were provided with an incentive of $25 for completion of project surveys for each session they attended. Those who were interested in the project called program staff to be screened for eligibility: African American, age 50–74, no history of CRC, and able to complete a self-administered questionnaire written at 5th grade reading level. CRC screening guidelines were used to determine eligibility for the study. For individuals at average risk for CRC, screening should begin at age 50 and conclude at age 75 (Agency for Healthcare Research and Quality, 2008). Those age 75 were not included in analyses because they would become ineligible for screening during the study period.
Educational sessions
Individuals eligible to participate were invited to attend the first educational session, which began with informed consent. Participants then completed the self-administered baseline questionnaire. The CHAs conducted the educational group session using standardized power point presentations. The sessions typically began with prayer, and were a combination of didactic and interaction, ending with a question and answer period. In the event that the CHA could not answer a question, study staff contributed with a response. Testimonials and stories from audience members were spontaneous and frequent occurrences. For those in the spiritually-based intervention, the slides and materials also included spiritual content. CHAs distributed print materials developed for the project (Holt, et al., 2009). These full-color materials were professionally-designed and produced, covering: an overview of cancer and CRC, incidence and prevalence statistics, risk factors, symptoms, screening tests, and barriers to screening. The materials in the spiritually-based intervention additionally included relevant scripture and spiritual themes such as:
God is such a loving God that He gave his only son so that you and I might have life. It is to Him that we give our thanks and praise. But with His gift comes a responsibility. We have a responsibility to care for our bodies in the best way that we can.
The non-spiritual intervention provided the same core colorectal cancer content, but in a non-spiritual manner, and used messages such as:
Don’t wait until you start feeling bad to get tested. Now is as good of a time as ever. An ounce of prevention is better than a pound of cure.
The second session was conducted one month later, focusing more on insurance coverage, where to receive screening, and CRC treatment. The first session lasted 1.5–2 hours due to the informed consent and baseline survey, while the educational components in each session typically lasted for 1 hour.
The intervention addressed constructs from the Health Belief Model in several ways. With perceived severity in this community, the objective is typically not to try and convince people that cancer is a significant health threat. This is because many tend to view cancer as a “death sentence”. Therefore, the intervention provided the testimony of role models who are survivors, which can serve to reduce cancer fear. The intervention addressed perceived susceptibility by providing information about the disproportionate burden of CRC incidence and mortality in the African American community, and discussing other risk factors such as age. Perceived barriers to screening such as cost, fear, transportation, access, lack of provider recommendation, pain, bowel preparation, and embarrassment, were a significant focus of the intervention. Such barriers are particularly salient in CRC screening, and therefore were given a great deal of emphasis in the intervention messaging. Perceived benefits of screening were also highlighted, including prevention of CRC through removal of pre-cancerous polyps, and being there for one’s family or to see grandchildren grow up. Self-efficacy was a focus through empowering people to talk to their doctors about screening, even if their doctor had never talked to them about it. A great deal of patient empowerment was discussed in the sessions, engendering a consumer-oriented approach. Finally, CHAs delivered the cue to action for all age-eligible participants to get screened for CRC.
Follow-up questionnaire
One year post-enrollment, study staff went to each church, providing participants with a study update, and report of baseline descriptive findings. The session began with completion of the final questionnaire. Participants were highly interested in project updates and data, so this was effective for increasing participant retention. A number of participants did not attend but completed their surveys by mail (N=72).
Measures
Perceived benefits of CRC screening
Perceived benefits of CRC screening were assessed using a previously validated instrument (Rawl, et al., 2001) (e.g., “Finding CRC early will save your life.”). Participants provided agree, disagree, or not sure responses. Benefits were summed to result in an index score with higher scores reflecting more perceived benefits. Internal reliability was reasonable in the present sample (α = .57) given its brevity (Nunnally & Bernstein, 1994).
Perceived benefits/barriers to FOBT
Perceived benefits of and barriers to the FOBT were assessed using an 11-item index (Rawl, et al., 2001). Items assessed perceived benefits such as early detection (e.g., “An FOBT will help find CRC early.”) and decreasing CRC worry (e.g., “An FOBT will help you not worry as much about CRC”). Perceived barriers included embarrassment (e.g., “An FOBT is embarrassing”), and time (e.g., “I do not have time to do an FOBT”). Participants provided responses in strongly agree, agree, neutral, disagree, or strongly disagree, format. Items were summed to yield an FOBT benefits and FOBT barriers score, with higher scores reflecting more perceived benefits and barriers. Internal reliabilities were acceptable in the present sample (α = .75 benefits; r; = .86 barriers).
Perceived benefits/barriers to colonoscopy
Perceived benefits (e.g., “The cost would keep me from having a colonoscopy.”), and barriers specific to colonoscopy such as preparation (e.g., “Having to follow a special diet and take a laxative or enema would keep me from having a colonoscopy.”) were assessed (Rawl, et al., 2001). Participants provided agree, disagree, or not sure responses. Items were summed to yield a colonoscopy benefits score and a colonoscopy barriers score, with higher scores reflecting more perceived benefits and barriers. Internal reliabilities were acceptable in the present sample (α = .82 benefits; r; = .60 barriers).
CRC screening
These items were based on the Behavioral Risk Factor and Surveillance System (Centers for Disease Control and Prevention, 2006). A definition was provided to introduce each screening method, coupled with a picture depicting the method. CRC screening awareness was assessed by asking participants if they had ever heard of the test (yes/no/not sure). In accord with screening recommendations (Agency for Healthcare Research and Quality, 2008), participants then reported when they had their last exam using the appropriate time frame categories.
Manipulation check
Participants completed a brief series of questions assessing the extent to which they perceived that the educational sessions were spiritual in nature. A series of five items with Likert-type response options (e.g., “Spirituality was discussed in the sessions.”; “The sessions ‘spoke to’ my spiritual needs.”; strongly disagree…strongly agree); (α = .94), were followed by a single item assessing the extent to which spiritual content was included in the sessions (not at all spiritual…very spiritual).
Demographics
Demographic data included sex, age, race, date of birth, marital status, health insurance coverage, educational attainment, employment status, household income before taxes, and family history of CRC.
Design/Analysis
The primary outcomes were the CRC screening-related variables including awareness (heard of the screening method), whether the participant had ever had the screening, and whether they had had the screening within the recommended time frame. Secondary outcomes included changes in scores for scales representing CRC knowledge, perceived benefits/barriers of CRC screening, perceived benefits/barriers to FOBT, and perceived benefits/barriers to colonoscopy. Scores were calculated by summing item responses. Since the interest was in counts of target outcome responses, missing values were treated as non-response, and were coded as negative or zero responses. A total of six change scores were calculated for the scales and subscales. Unadjusted means and standard deviations were calculated for baseline, follow-up, and changes from baseline to follow-up. Primary outcomes were compared between the intervention groups using mixed-model logistic regression analysis implemented with generalized estimating equations to account for the cluster-randomized study design. Each model included fixed effect terms for intervention group, time (baseline or follow-up), participant age, and a group by time interaction term. A term representing church was included as a random effect. The statistical test that was of primary interest was that for group by time interaction, as this evaluates equality of baseline to follow-up changes between the intervention groups. The main effect of time was also considered, in order to judge whether significant changes in mean response occurred between baseline and follow-up. The analysis of continuous measures utilized the same model structure described above, implemented as mixed-model analysis of variance. Statistical analyses were implemented using SAS® Release 9.2 software (Cary, NC). Analyses were conducted only among participants age-eligible for screening (e.g., 50–74).
Results
Participant demographic characteristics
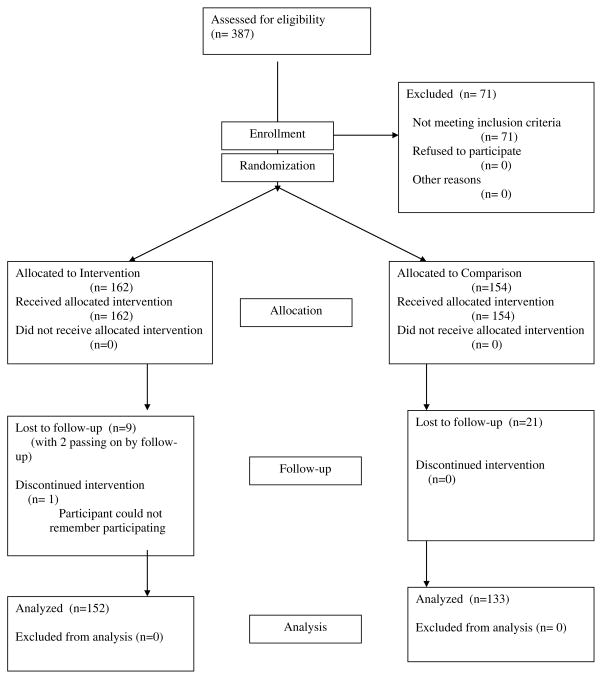
Three hundred and eighty seven individuals were assessed for eligibility and 316 met full inclusion criteria. Of the 316 enrolled participants, 285 reported both baseline and follow-up data and serve as the analytical sample for this paper. Participants retained at 12 months did not differ from those who dropped out of the study on demographic variables (all p values > .05).
Study participants had a mean age of 59.78 ± 7.15 and most were female (69.82%). Participant demographic characteristics by study group appear in Table 1. None of the demographic differences between study groups were statistically significant with the exception of age, where those in the non-spiritual group were older, on average, than those in the spiritually-based group (age controlled in subsequent analyses).
Table 1.
Participant demographic characteristics
| Spiritually-based (N=152) | Non-Spiritual (N=133) | P Value | ||
|---|---|---|---|---|
| Sex | Male | 51 (34%) | 35 (26%) | .18 |
| Female | 101 (66%) | 98 (74%) | ||
| Age mean (sd) ** | 58.56 (7.00) | 61.16 (7.10) | .01 | |
| Age median | 57 | 60 | ||
| Relationship status | Single | 15.6% | 15.2% | |
| Living w/partner | 0.7% | 0.8% | ||
| Married | 52.5% | 46.4% | .84 | |
| Separated or divorced | 18.4% | 20.8% | ||
| Widowed | 12.8% | 16.8% | ||
| Education | Grades 1–8 | 2.2% | 0.8% | |
| Grades 9–11 | 10.1% | 4.8% | ||
| Grade 12 or GED^ | 28.8% | 21.6% | .17 | |
| 1–3 yrs college | 32.4% | 40.8% | ||
| 4+ yrs college | 26.6% | 32.0% | ||
| Work status | Full time | 52.6% | 37.0% | |
| Part time | 7.0% | 10.2% | ||
| Not currently | 8.8% | 10.2% | .21 | |
| Retired | 22.8% | 28.7% | ||
| Disability | 8.8% | 13.9% | ||
| Income | < 5k | 5.3% | 3.6% | |
| 5–10k | 13.0% | 9.1% | ||
| 10–20k | 9.9% | 18.2% | ||
| 20–30k | 17.6% | 13.6% | ||
| 30–40k | 9.2% | 12.7% | ||
| 40–50k | 12.2% | 8.2% | .55 | |
| 50–60k | 13.0% | 7.3% | ||
| 60–70k | 5.3% | 5.5% | ||
| 70–80k | 2.3% | 8.2% | ||
| 80–90k | 5.3% | 4.5% | ||
| 90–100k | 1.5% | 4.5% | ||
| More than 100k | 5.3% | 4.5% |
GED = General Equivalency Diploma
Manipulation check
Independent t-tests indicated significant study group differences confirming the manipulation. Participants in the spiritually-based group perceived the sessions as significantly more spiritual (M = 20.21, SD = 4.88) than did those in the non-spiritual group (M = 18.67, SD = 5.27), t (237) = 2.33, p = .02. Similarly, participants in the spiritually-based group (M = 3.40, SD = 0.67) perceived the educational session content as significantly more spiritual in nature than did those in the non-spiritual group (M = 2.95, SD = 1.00), t (214) = 3.98, p < .001.
Screening-related outcomes
For the main study outcomes of awareness of the screening methods, ever having had the screening, and having had the screening in the recommended interval, only reporting FOBT within the previous 12 months showed a significant difference between the groups (group*time p = 0.0257), with the non-spiritual group showing a 9% increase and the spiritually-based group showing a 2% decrease in reported testing. Reporting having had a barium enema within the previous 5 years showed a near-significant difference (group*time p = .06), with the spiritually-based group showing a 6% increase and the non-spiritually-based group showing a 1.5% decrease. No other study group differences were significant (see Table 2). However, the interventions may have had some significant impact for some of the screening-related outcomes from baseline to the 12-month follow-up. There were significant time effects for increases in ever heard of FOBT (p < .001), ever had FOBT (p < .05) ever heard of flexible sigmoidoscopy (p < .001), ever had flexible sigmoidoscopy (p = .05), had flexible sigmoidoscopy in previous 5 years (p < .001), ever heard of colonoscopy (p = .001), ever had colonoscopy (p = .01), had colonoscopy in previous 10 years (p < .01), and ever heard of barium enema (p < .001).
Table 2.
Analysis for screening-related outcomes1
| Spiritually-based | Non-spiritual | Time p-value2 | Time*Group p-value3 | |||
|---|---|---|---|---|---|---|
| Baseline | 12-month | Baseline | 12-month | |||
| Heard of fecal occult blood test | 92 (60.5) | 134 (88.2) | 83 (62.4) | 118 (88.7) | <.01 | .95 |
| Ever had fecal occult blood test | 51 (33.6) | 58 (38.2) | 45 (33.8) | 55 (41.4) | .03 | .55 |
| FOBT in last 12 months | 15 (9.9) | 12 (7.9) | 8 (6.0) | 20 (15.0) | .09 | .03 |
| Heard of flexible sigmoidoscopy | 59 (38.8) | 115 (75.7) | 57 (42.9) | 102 (76.7) | <.01 | .69 |
| Ever had flexible sigmoidoscopy | 30 (19.7) | 39 (25.7) | 23 (17.3) | 37 (27.8) | .05 | .52 |
| Flexible sigmoidoscopy in last 5 years | 25 (16.5) | 123 (80.9) | 16 (12.0) | 103 (77.4) | <.01 | .71 |
| Heard of colonoscopy | 108 (71.0) | 136 (89.5) | 101 (75.9) | 116 (87.2) | .001 | .16 |
| Ever had colonoscopy | 83 (54.6) | 99 (65.1) | 72 (54.1) | 91 (68.4) | .01 | .55 |
| Colonoscopy in last 10 years | 77 (50.7) | 98 (64.5) | 64 (48.1) | 84 (63.2) | .01 | .88 |
| Heard of barium enema | 59 (38.8) | 110 (72.4) | 70 (52.6) | 98 (73.7) | <.01 | .12 |
| Ever had barium enema | 22 (14.5) | 20 (13.2) | 19 (14.3) | 17 (12.8) | .08 | .32 |
| Barium enema in last 5 years | 11 (7.2) | 20 (13.2) | 19 (14.3) | 17 (12.8) | .17 | .06 |
Data shown are frequencies and percentages (in parentheses) who participants who said “yes” (missing recoded as “no” as described in the text), among study participants for whom follow-up data were available.
p-value for the time main effect, representing the difference between baseline and 12-month means, across groups
p-value for the time*group interaction effect, representing the difference in mean change between the two groups
Health Belief Model outcomes
For the outcomes including perceived barriers to and benefits of screening, no study group differences (group*time) were significant (see Table 3). However, the interventions appeared to impact some of the outcomes from baseline to the 12-month follow-up. Change was significant for increase in CRC screening benefits (p < .001), increase in FOBT perceived benefits (p < .05), increase in colonoscopy perceived benefits (p < .01), and decrease in colonoscopy perceived barriers (p < .05).
Table 3.
Comparisons of change in perceived barriers to and benefits of screening
| Spiritually-based (N = 152) | Non-spiritual (N = 133) | |||||||
|---|---|---|---|---|---|---|---|---|
| Dependent Variable (/total possible score) | Baseline Mean (SD) | 12-Month Mean (SD) | Change* | Baseline Mean (SD) | 12-Month Mean (SD) | Change* | Time p-value | Time* Group p-value** |
| CRC screening benefits (/2) | 1.66 (0.61) | 1.81 (0.52) | 0.15 (0.69) | 1.56 (0.70) | 1.85 (0.44) | 0.29 (0.74) | <.01 | .16 |
| FOBT perceived benefits (/15) | 11.42 (1.89) | 11.44 (1.65) | 0.08 (2.11) | 11.20 (2.45) | 11.18 (2.25) | 0.10 (3.23) | .04 | .20 |
| FOBT perceived barriers (/40) | 16.52 (5.89) | 14.79 (4.97) | −1.86 (5.71) | 16.11 (5.43) | 14.91 (5.50) | −1.44 (5.23) | .16 | .33 |
| CS perceived benefits (/3) | 2.35 (1.03) | 2.64 (0.66) | 0.30 (1.01) | 2.20 (1.08) | 2.45 (0.90) | 0.26 (1.16) | <.01 | .80 |
| CS perceived barriers (/10) | 0.72 (1.09) | 0.43 (1.03) | −0.29 (1.10) | 0.69 (1.23) | 0.53 (1.36) | −0.17 (1.38) | .04 | .54 |
Mean changes are the raw means, not adjusted church or age
The time*group interaction p-value is for the comparison of mean change between the groups, adjusted for the clustering effect of churches, baseline value and age
Discussion
This study evaluated the efficacy of a spiritually-based Community Health Advisor intervention to increase CRC screening among African Americans in church settings. The spiritual intervention was compared to a non-spiritual intervention that was identical in educational content, structure, and theoretical framework. This randomized controlled trial yielded mixed results. As hypothesized, the spiritually-based intervention was perceived as significantly more spiritual in nature compared to the non-spiritual intervention.
The second hypothesis, however, was not supported. The spiritually-based intervention was not superior to the non-spiritual comparison on CRC screening or pre-post changes in Health Belief Model outcomes. In fact, report of receiving an FOBT within the intervention period was greater in the non-spiritual group than in the spiritually-based group. This was a surprising finding and in fact opposite of the hypothesized direction. When such findings occur, explanations such as compensatory rivalry may be explored. This is where the control/comparison group becomes aware of the study hypothesis and overcompensates in such a way as to impact the dependent variable. However, because both interventions were nearly equivalent and of high quality, and due to the team’s high community competence and use of community-engaged research practices throughout the project, this seems unlikely. There is a possibility that while participants embraced the spiritually-based messages as being familiar in the church setting, they may have perceived greater credibility in the non-spiritual approach. The curriculum was delivered by CHAs, and even though they had been trained and certified, issues of credibility and CHA confidence sometimes arose. It is also possible that there was a greater emphasis on the core medical information in the non-spiritual group because that group did not also contain the spiritual messaging, and both sessions were equal in length.
Given the minimal differences between the interventions, the current hypothesis was an ambitious test. Examining the time main effect findings, both interventions appeared to be effective for most study outcomes. These included awareness of the tests, as well as self-report of having received them. There are of course limitations in interpretation of these findings because without an untreated group, the findings may be due to reporting bias. However, use of community-engaged research methods discourages use of control groups from a social justice perspective. A delayed treatment control group may have been a feasible alternative.
With regard to the non-significant study group differences, the most likely explanation is that the modest differences between the two interventions made it difficult to detect significant group differences. A review of the literature (Husaini et al., 2002, Paskett et al., 1999) suggests that spiritually-based interventions to promote cancer screening are superior to control groups, but in studies in which two interventions are compared (Campbell et al., 1999), consistent with our findings, the interventions are comparable. Indeed, several previous studies that have identified more robust study group differences have either utilized control groups or delayed treatment control group designs (Morgan, Fogel, Tyler, & Jones, 2010; Walsh, et al., 2010). For example, the “F.A.I.T.H.” study resulted in 25% of participants receiving colonoscopy within three months compared to 4% in the control group (Morgan, Fogel, Tyler, & Jones, 2010), while the present study saw 14% and 15% increases from baseline to 12-month follow-up in self-report colonoscopy across the spiritual and non-spiritual groups, respectively. The study reported by Walsh and colleagues (2010) indicated more robust 12-month increases in self-report FOBT in a Latino and Vietnamese population, at 7.8% in the control group, 15.1% among those who received brochures, and 25.1% for those who received culturally tailored telephone counseling with the brochures.
Another potential explanation for the lack of study group differences are that the non-spiritual intervention became “spiritualized” because of the church setting. The team gave careful consideration as to whether the non-spiritual intervention could actually be delivered in a secular fashion, and produce a difference in “spiritual-ness” between the interventions. Study group differences in CHA training around this issue, and the CHA presentations being somewhat standardized by the power point slides helped to ensure, to the extent possible, that the non-spiritual group was as secular as possible. In addition, the manipulation check revealed that there were significant differences in the level of spirituality of the intervention as perceived by participants. However, it was also evident from the data that participants even in the non-spiritual group perceived the sessions to be at least somewhat spiritual in nature.
The secondary outcomes analysis indicated that while there were some pre-post changes in the Health Belief Model constructs, again there were no study group differences. The present study was not intended as a “test” of the Health Belief Model. The idea that theories may not operate optimally in diverse samples is one that is being increasingly recognized, but has yet to become fully realized in practice. This issue was addressed in a special issue of Health Education & Behavior. Pasick and colleagues (2009) examined the meaning of constructs from individual level behavior change theories in a mixed-methods study among Filipina and Latina women. They reported that the importance of social context may play a significant role in cancer control behaviors (e.g., mammography), suggesting that individual level theories alone may not be as appropriate with this population. It was recommended that a more social ecological approach be taken, incorporating people’s social context, culture, families, and communities (Burke, Joseph, Pasick, & Barker, 2009). Another study examined behavioral constructs in predicting mammography in multiethnic populations, including African Americans (Stewart, Rakowski, & Pasick, 2009). While several perceived benefits items were associated with screening, other items were not, suggesting the need for improved measurement among diverse groups.
Strengths and limitations
The present study has several strengths. Using a group randomized controlled trial, we tested two theory-based, culturally-targeted interventions. The interventions were developed using an iterative process with community participation throughout its development and pre-testing (Holt, et al., 2009). Second, by training church members to deliver the intervention, we increased the capacity of 16 churches to deliver CRC educational programs. This model is sustainable and has public health implications for dissemination. It is currently being employed in a second generation behavioral translational research study aimed at determining an optimal dissemination/implementation method for church-based cancer control interventions. Finally, we fill an important gap in the literature. As noted by Powe and colleagues (2010), the number of intervention studies designed to increase CRC screening among African Americans are relatively few (Powe, Fauklenberry, & Harmond, 2010).
The results of the present study should also be considered in light of its limitations. First, the intervention may have been more impactful if limited to participants not up-to-date with CRC screening. Future studies should aim to balance community considerations for inclusive studies with the importance of delivering and testing interventions among those who would derive the greatest benefit. Second, while we identified and reported intriguing and significant changes on CRC screening related outcomes from baseline to follow-up, these findings cannot for certain be attributed to the interventions.
Implications for practice
In sum, both of these community-engaged, theory-driven, culturally-relevant approaches to increasing CRC awareness and screening appeared to have an impact on study outcomes. While adding spiritual/religious themes to the intervention was appealing to the audience, it may not result in increased intervention efficacy in terms of screening.
Figure 2.
CONSORT randomization diagram
Acknowledgments
This work was supported by a grant from the Centers for Disease Control and Prevention #5U48DP00046-03 and was approved by the University of Alabama at Birmingham Institutional Review Board (X051004002). The findings and conclusions in this article are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
The authors would like to acknowledge the contributions of Shereta Wiley for her assistance with data collection, Penny Southward for project management, and Dr. Steven S. Coughlin, for technical assistance from the funding agency.
References
- Agency for Healthcare Research and Quality. [Accessed January 23, 2009];US Preventive Services Task Force (USPSTF) 2008 Available at: http://www.ahrq.gov/clinic/uspstfix.htm.
- American Cancer Society. Colorectal Cancer Facts & Figures 2011–2013. American Cancer Society; Atlanta, GA: 2011a. [Google Scholar]
- American Cancer Society. Cancer Facts & Figures for African Americans 2011–2012. American Cancer Society; Atlanta, GA: 2011b. [Google Scholar]
- American Cancer Society. American Cancer Society guidelines for the early detection of cancer. American Cancer Society; 2012. [Accessed April 4, 2012]. http://www.cancer.org/Healthy/FindCancerEarly/CancerScreeningGuidelines/american-cancer-society-guidelines-for-the-early-detection-of-cancer. [Google Scholar]
- Burke NJ, Joseph G, Pasick RJ, Barker JC. Theorizing social context: Rethinking behavioral theory. Health Education & Behavior. 2009;36:55S–70S. doi: 10.1177/1090198109335338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell MK, Demark-Wahnefried W, Symons M, Kalsebeek WD, Dodds J, Cowan A, … McClelland JW. Fruit and vegetable consumption and prevention of cancer: The black churches united for better health project. American Journal of Public Health. 1999;89(9):1390–1396. doi: 10.2105/AJPH.89.9.1390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell MK, James A, Hudson MA, Carr C, Jackson E, Oates V, Demissie S. Improving multiple behaviors for colorectal cancer prevention among African American church members. Health Psychology. 2004;23(5):492–502. doi: 10.1037/0278-6133.23.5.492. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance Survey System online information. U.S. Department of Health and Human Services; 2006. [Accessed September 17, 2008]. Available at: http://cdc.gov/brfss/ [Google Scholar]
- Cuzick J. Screening for Cancer: Future Potential. Cancer Imaging. 2006;6(SpecA):S1–S8. doi: 10.1102/1470-7330.2006.9097. [DOI] [Google Scholar]
- Faivre J, Tazi MA, El Mrini T, Lejeune C, Benhamiche AM, Dassonville F. Faecal occult blood screening and reduction of colorectal cancer mortality: a case-control study. British Journal of Cancer. 1999;79(3/4):680–683. doi: 10.1038/sj.bjc.6690107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fendall R. We expect too much from community health workers. World Health Forum. 1984;5:300–303. [Google Scholar]
- Giblin PT. Effective utilization and evaluation of indigenous health care workers. Public Health Reports. 1989;104(4):361–368. [PMC free article] [PubMed] [Google Scholar]
- Hardcastle JD, Chamberlain JO, Robinson MHE, Moss SM, Amar SS, Balfour TW, … Mangham CM. Randomised controlled trial of faecal-occult-blood screening for colorectal cancer. Lancet. 1996;348(9040):1472–1477. doi: 10.1016/S0140-6736(96)03386-7. doi.org/10.1016/S0140-6736(96)03386-7. [DOI] [PubMed] [Google Scholar]
- Holt CL, Roberts C, Scarinci IC, Wiley SR, Eloubeidi M, Crowther M, Bolland J, Litaker MS, Southward V, Coughlin SS. Development of a spiritually-based educational program to increase colorectal cancer screening among African American men and women. Health Communication. 2009;24:400–412. doi: 10.1080/10410230903023451. [DOI] [PubMed] [Google Scholar]
- Holt CL, Scarinci IC, Debnam K, McDavid C, Litaker M, McNeal SF, … Martin MY. Spiritually-based intervention to increase colorectal cancer awareness among African Americans: Intermediate outcomes from a randomized trial. Journal of Health Communication. doi: 10.1080/10810730.2012.665418. (In Press) [DOI] [PubMed] [Google Scholar]
- Holt CL, Shipp M, Eloubeidi M, Fouad M, Britt K, Norena M. Your body is the temple: Impact of a spiritually-based colorectal cancer educational intervention delivered through community health advisors. Health Promotion Practice. 2011;12(4):577–588. doi: 10.1177/1524839910370421. [DOI] [PubMed] [Google Scholar]
- Husaini BA, Sherkat DE, Levine R, Bragg R, Cain V, Emerson JS, Mentes CM. The effect of a church-based breast cancer screening education program on mammography rates among African-American women. Journal of the National Medical Association. 2002;94(2):100–106. [PMC free article] [PubMed] [Google Scholar]
- Indian Health Service. Alaska community health aide program description. Washington, DC: Government Printing Office; 1991. [Google Scholar]
- Kronberg O, Fenger C, Olsen J, Jorgensen OD, Sondergaard O. Randomised study of screening for colorectal cancer with faecal-occult-blood test. Lancet. 1996;348(9040):1467–1471. doi: 10.1016/S0140-6736(96)03430-7. [DOI] [PubMed] [Google Scholar]
- Lincoln CE, Mamiya LH. The black church in the African American experience. Durham, NC: Duke University Press; 1990. [Google Scholar]
- Mandel JS, Bond JH, Church TR, Snover DC, Bradley GM, Schuman LM, Ederer F. Reducing mortality from colorectal cancer by screening for fecal occult blood. New England Journal of Medicine. 1993;328(19):1365–1371. doi: 10.1056/NEJM199305133281901. [DOI] [PubMed] [Google Scholar]
- Morgan PD, Fogel J, Tyler ID, Jones JR. Culturally targeted educational intervention to increase colorectal health awareness among African Americans. Journal of Health Care for the Poor and Underserved. 2010;21(S3):132–147. doi: 10.1353/hpu.0.0357. [DOI] [PubMed] [Google Scholar]
- Nunnally JC, Bernstein IH. Psychometric theory. 3. New York: McGraw-Hill, Inc; 1994. [Google Scholar]
- Pasick RJ, Burke NJ, Barker JC, Joseph G, Bird JA, Otero-Sabogal R, … Guerra C. Behavioral theory in a diverse population: Like a compass on Mars. Health Education & Behavior. 2009;36(Suppl 1):11S–35S. doi: 10.1177/1090198109338917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paskett ED, Tatum CM, D’Agostino RD, Rushing J, Velez R, Michielutte R, Dignan M. Community-based interventions to improve breast and cervical cancer screening: Results of the Forsyth County Cancer Screening (FoCaS) project. Cancer Epidemiology, Biomarkers & Prevention. 1999;8(5):453–459. [PubMed] [Google Scholar]
- Powe BD, Faulkenberry R, Harmond L. A review of intervention studies that seek to increase colorectal cancer screening among African Americans. American Journal of Health Promotion. 2010;25(2):92–99. doi: 10.4278/ajhp.080826-LIT-162. [DOI] [PubMed] [Google Scholar]
- Quintero E, Castells A, Bujanda L, Cubiella J, Salas D, Lanas Á, … González-Navarro A. Colonoscopy versus fecal immunochemical testing in colorectal-cancer screening. New England Journal of Medicine. 2012;366(8):697–706. doi: 10.1056/NEJMoa1108895. [DOI] [PubMed] [Google Scholar]
- Rawl S, Champion V, Menon U, Loehrer PJ, Vance GH, Skinner CS. Validation of scales to measure benefits of and barriers to colorectal cancer screening. Journal of Psychosocial Oncology. 2001;19(3–4):47–63. doi: 10.1300/J077v19n03_05. [DOI] [Google Scholar]
- Rex DK, Johnson DA, Lieberman DA, Burt RW, Sonnenberg A. Colorectal cancer prevention 2000: Screening recommendations of the American College of Gastroenterology. American College of Gastroenterology. American Journal of Gastroenterology. 2000;95(4):868–877. doi: 10.1016/S0002-9270(00)00851-0. [DOI] [PubMed] [Google Scholar]
- Rosenstock I, Strecher V, Becker M. Social learning theory and the health belief model. Health Education and Behavior. 1988;15(2):175–183. doi: 10.1177/109019818801500203. [DOI] [PubMed] [Google Scholar]
- Stewart SL, Rakowski W, Pasick RJ. Behavioral constructs and mammography in five ethnic groups. Health Education & Behavior. 2009;36(5 Suppl):36S–54S. doi: 10.1177/1090198109338918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas SB, Quinn SC, Billingsley A, Caldwell C. The characteristics of northern black churches with community health outreach programs. American Journal of Public Health. 1994;84(4):575–579. doi: 10.2105/AJPH.84.4.575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. Community health advisors: Models, research, and practice, selected annotations-United States. Vol. 1. Atlanta, Georgia: U.S. Department of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Division of Chronic Disease Control and Community Intervention; 1994a. [Google Scholar]
- U.S. Department of Health and Human Services. Community Health Advisors: Programs in the United States, Health Promotion and Disease Prevention. Atlanta, Georgia: U.S. Department of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Division of Chronic Disease Control and Community Intervention; 1994b. [Google Scholar]
- Vernon SW, Bartholomew LK, McQueen A, Bettencourt JL, Greisinger A, Coan SP, Lairson D, Chan W, Hawley ST, Myers RE. A randomized controlled trial of a tailored interactive computer-delivered intervention to promote colorectal cancer screening: Sometimes more is just the same. Annals of Behavioral Medicine. 2011;41(3):284–299. doi: 10.1007/s12160-010-9258-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsh JME, Salazar R, Nguyen TT, Kaplan C, Nguyen L, Hwang J, … Pasick RJ. Healthy colon, healthy life: A novel colorectal cancer screening intervention. American Journal of Preventive Medicine. 2010;39(1):1–14. doi: 10.1016/j.amepre.2010.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walt G, editor. Community health workers in national programmes: Just another pair of hands? Philadelphia: Open University Press; 1990. [Google Scholar]
- Witmer A, Seifer SD, Finocchio L, Leslie J, O’Neil EH. Community health workers: integral members of the health care work force. American Journal of Public Health. 1995;85(8 Pt 1):1055–1058. doi: 10.2105/AJPH.85.8_Pt_1.1055. [DOI] [PMC free article] [PubMed] [Google Scholar]