Abstract
Brain infarction causes tissue death by ischemia due to occlusion of the cerebral vessels and recent work has shown that post stroke inflammation contributes significantly to the development of ischemic pathology. Because secondary damage by brain inflammation may have a longer therapeutic time window compared to the rescue of primary damage following arterial occlusion, controlling inflammation would be an obvious therapeutic target. A substantial amount of experimentall progress in this area has been made in recent years. However, it is difficult to elucidate the precise mechanisms of the inflammatory responses following ischemic stroke because inflammation is a complex series of interactions between inflammatory cells and molecules, all of which could be either detrimental or beneficial. We review recent advances in neuroinflammation and the modulation of inflammatory signaling pathways in brain ischemia. Potential targets for treatment of ischemic stroke will also be covered. The roles of the immune system and brain damage versus repair will help to clarify how immune modulation may treat stroke.
Keywords: Brain ischemia, inflammation, neuroprotection, stroke
1. INTRODUCTION
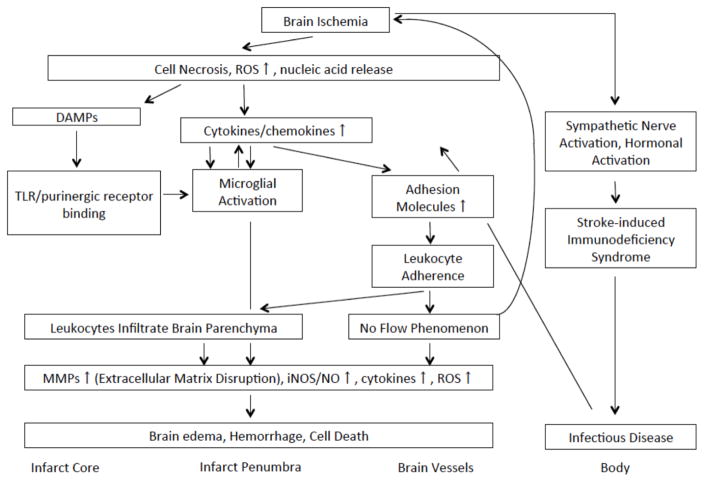
Stroke encompasses conditions caused by occlusion and/or rupture of the brain’s blood vessels. It is a leading cause of death and disability worldwide with significant clinical and socioeconomic impact. Ischemic stroke represent the majority seen in industrialized nations [1]. Besides its high incidence, approved effective therapies are limited. There are many mechanisms involved in the pathogenesis of stroke, but recent work has focused on the duality of post stroke inflammation. That is, inflammation contributes both negatively and positively to neurological outcome [2–4]. Brain inflammation leads to secondary injury following stroke (Fig. 1). Brain ischemia triggers inflammation as a response necrotic cells followed by the generation of reactive oxygen species (ROS), although many other factors have yet to be identified. Once activated, these initiators of inflammation lead to activation of microglia, the brain’s resident immune cell. Microglia then generate more pro-inflammatory cytokines which in turn leads to adhesion molecules induction in the cerebral vasculature [5–7]. These events have been documented to occur within the first 24 h of stroke onset. Chemokine upregulation leads to chemotaxis of circulating immune cells into ischemic brain especially around the penumbra. Adhesion molecules mediate leukocyte adhesion to vascular endothelia leading to microvascular occlusion and leukocyte entry into the ischemic brain parenchyma [8, 9]. Inflammatory cells release several cytotoxic agents such as matrix metalloproteinases (MMPs), nitric oxide (NO) and also are also an independent source of ROS. These molecules exacerbate brain cell damage, and lead to disruption of the extracellular matrix and blood-brain barrier (BBB) [10]. This disruption permits blood and other potentially neurotoxic serum substances to enter the Brain Res.ulting in brain edema and hemorrhagic transformation. Brain ischemia may also activate the sympathetic nervous system (SNS) and the hypothalamic-pituitary-adrenal axis (HPA) and further influence circulating immune cells to enter the brain. This in turn may lead to fewer circulating immune cells, and increase the risk of infectious complications [11]. Leukocyte plugging of the brain’s microvasculature has also been implicated in microvascular stasis leading to hypoperfusion or the so-called ‘no-reflow’ phenomenon. Blocking inflammation has shown to ameliorate injury in stroke models [12].
Fig. 1.
Post stroke inflammation pathway. Brain ischemia initiates inflammation in response to necrotic cells within the infarct. Necrotic cells then cause inflammatory cells to generate reactive oxygen species (ROS) and inflammatory cytokines. Necrotic cells lyse and release nucleic acids which can act as danger associated molecular pattern molecules (DAMPs). DAMPs and other immune molecules activate immune receptors on microglia, which in turn, leads to more cytokine production. Cytokines upregulate adhesion molecule expression on the surfaces of cells of the cerebral vasculature. The production of chemokines by cells of the immune system and brain recruit circulating immune cells to the ischemic brain. Adhesion molecules traffic circulating leukocytes to activated the endothelium where they infiltrate the brain parenchyma. After entering the brain, activated leukocytes along with activated microglia, generate inflammatory mediators, including the matrix metalloproteinases (MMPs), inducible nitric oxide synthase (iNOS) leading to nitric oxide (NO) generation, cytokines and more ROS. These pro-inflammatory molecules ultimately result in brain edema, hemorrhage and cell death. Brain infarction also affects the rest of the body, leading to a state of immunodeficiency, and is thought to be mediated through the sympathetic nervous system, resulting in lowering circulating immune cells. This can subsequently lead to infections which complicates stroke by further increasing immune activation in the brain.
What makes these inflammatory processes difficult to understand is that some of these responses may be detrimental by facilitating cell death, but also beneficial to the ischemic brain as immune cells are also capable of secreting neurotrophic factors and by scavenging necrotic debris allowing for the reorganization of a new environment for neural repair [13–16].
There has been significant progress over past years regarding inflammatory signaling pathways, cells and proteins as they pertain to post-ischemic inflammation. This review will focus on recent findings of the innate immune system and related mechanisms, and discusses ischemia-associated inflammation and possible therapeutic targets.
2. CELLS INVOLVED IN POST STROKE INFLAMMATION
The post stroke inflammatory response consists of cells intrinsic to the brain, as well as cells of the peripheral circulation which gain access through activated endothelium and/or disrupted blood brain barrier (BBB). Accumulation of circulating immune cells begins when ischemia damages and activates endothelial cells with rapid upregulation of adhesion molecules [17]. Circulating immune cells can then gain access into the injured brain and elaborate immune molecules that exacerbate ischemic cell death. Ischemic brain cells also activate endogenous immune cells such as microglia. A few studies implicate astrocytes as another brain resident immune cell which can also activate in response to ischemia.
2.1. Cerebral Endothelial Cells and the Blood Brain Barrier (BBB)
The cerebral endothelium is unique in that it contains a network of tight junctions, pericytes and astrocyte end-foot processes which make up the BBB [18, 19]. The interconnection of the cells is facilitated by integrins [20]. Endothelial cells are among the first cells which face the impact of ischemia related inflammation. When damaged by ischemic stimuli, endothelial cells swell or detach from the underlying basement membrane, leading to compromises in barrier function. This leads to increased BBB permeability causing protein extravasation and interstitial edema as well as entry of immune molecules and cells [17, 21]. Hypoxia also activates the arachidonic acid cascade leading to the generation of pro-inflammatory molecules such as prostaglandins, leukotrienes, and platelet-activating factor (PAF) [22]. These substances lead to platelet and neutrophil activation and adhesion, followed by changes in local cerebral blood flow and increases in BBB permeability [6, 22–24]. Ischemic endothelial cells are also known to express and release pro-inflammatory cytokines and chemokines. These mediators have been shown to up-regulate additional mediators in the ischemic endothelium, such as selectins and immunoglobin superfamily members leading to leukocyte adhesion and transmigration into the brain [25, 26].
2.2. Leukocytes
Leukocytes promote cerebral ischemic injury through several different mechanisms. They can adhere to the endothelium and obstruct the microvasculature. Such ‘leukocyte pluggins’ can impair local blood flow causing the ‘ no-reflow’ phenomenon and leads to additional ischemic injury [21]. Activated leukocytes near the surface of the endothelium also produce toxic ROS, proteases, gelatinases, and collagenases, and damage potentially salvageable blood vessels and brain tissues. Further, phospholipase activation in leukocytes leads to the production of leukotrienes, eicosanoids, prostaglandins, and PAF, causing vasoconstriction and increased platelet aggregation. Finally, infiltrated leukocytes elaborate proinflammatory cytokines and other immune molecules in around the penumbra surrounding the infarct core causing further neuronal injury [27–29].
2.2.1. Neutrophils
Following ischemia, neutrophils are thought to be the earliest type of leukocyte to enter the ischemic brain. Neutrophils have been observed as early as 4–6 h in models of transient focal cerebral ischemia [30, 31], and at around 12 hours after permanent focal cerebral ischemia [32]. They have been shown to exacerbate injury by producing inflammatory mediators, many of which are thought to be toxic to the injured brain [4, 33]. In transient focal cerebral ischemia, several reports have shown reduced infarct size when neutrophils are depleted or their infiltration is prevented [29, 34–38]. Many of these immune mediators appear to contribute to immune mediated damaged to adjacent viable tissue. By blocking neutrophil entry into the brain, studies have documented improved neurological outcome, thus indicating that neutrophils contribute negatively in this setting [39].
2.2.2. Lymphocytes
While the data are conflicting, lymphocytes appear to play an active role in ischemic brain pathogenesis. Like neutrophils, lymphocytes are also capable of producing pro-inflammatory cytokines and cytotoxic substances. A few studies in stroke models have shown that lymphocytes are elevated in the ischemic brain later than neutrophils (3 to 6 days post stroke) [40, 41]. Strategies to block lymphocyte entry into ischemic brain reduced injury, and like neutrophils, indicate that lymphocytes play a damaging role [42]. T, but not B lymphocytes are thought to be central to the development of inflammation in stroke models [43, 44]. Several studies have evaluated the role of T lymphocyte deficient mice in the transient focal ischemia model, and have shown reduced infarct volumes and reduced neurological deficits compared to controls [44–47]. In lymphocyte-deficient mice, protection from experimental stroke was found to be explained by the lack of T lymphocytes, rather than B lymphocytes. When investigators administered B lymphocytes to these lymphocyte deficient mice, protection from lymphocyte deficiency was not affected, whereas administration of T lymphocytes led to loss of protection [44, 46, 47]. Although, T lymphocytes appear worsen outcome in transient focal cerebral ischemia models, they do not appear to play a role in permanent focal cerebral ischemia models. In experimental permanent focal cerebral ischemia, Saino et al. [48] did not observed any change of infarct size in T and B lymphocyte deficient mice versus wildtype. The reasons for these differences are unclear.
However, not all T lymphocyte subtypes are detrimental in brain ischemia models. A recent study showed that neither γδ T lymphocytes nor natural killer (NK) cells contribute to ischemic injury [44]. There are conflicting reports concerning regulatory T (Treg) lymphocyte participation in stroke. Liesz et al. [49] showed that ischemic lesion size and neurological deficit were increased in mice treated with an antibody to neutralize Treg lymphocytes compared to controls, suggesting that they contribute positively. They also suggested that IL-10 signaling may be essential for this immunomodulatory effect. However, Ren et al. [50] could not find any effect of Treg cells in similar stroke models. There is also evidence that hepatic NK cell function is impaired due to augmented sympathetic neurotransmission after stroke. This loss of invariant NK (iNK) cell activity contributed to immunosuppression and susceptibility to infections following stroke [51].
Clinical studies suggest that increased serum lymphocytes are observed in patients with increased stroke risk and mortality [52]. However, in vitro studies have shown that while neutrophils potentiate neuronal injury due to necrotic insults, lymphocytes did not actually increase astrocyte proliferation [53].
Typically, T lymphocytes kill pathogen-infected cells through the release of cytokines, or cytotoxins [54], and similar actions probably occur at the site of ischemic injury. Alternatively, T lymphocytes may cause cell death via interaction with the Fas receptor [55], and a few groups showed that blocking T lymphocyte-derived cytokines decreased infarct volume and improved neurological outcome in experimental stroke [46, 49, 56]. Furthermore, perforin-deficient mice were protected against stroke, suggesting that perforin, which is released by T lymphocytes, potentiates ischemic damage [57]. In addition to these studies, other work indicates that T lymphocytes increase oxidative stress through superoxide produced by NADPH oxidase type 2 (Nox-2). T lymphocytes produce 7 to 15 times more super-oxide through Nox-2 following experimental stroke in mice compared to uninjured mice [58]. Thus, the role of lymphocytes in stroke may depend on the subtype involved.
2.3. Microglia/Macrophages
Microglia constitute approximately 5–10% of all of the cells of the brain, and are often considered the brain’s resident immune cell. Microglia modulate immune responses and phagocytic activity in the brain [59]. They participate in the brain’s defense against infection, and are activated under conditions of trauma, ischemia, and neurodegeneration [60]. Activated microglia undergo morphologic transformation from a resting state referred to as “ramified” to an “amoeboid” state, where they become virtually indistinguishable from circulating macrophages [59, 61]. Activated microglia are often called resident brain macrophages. Through their phagocytic properties, microglia will clear foreign organisms as well as injured neurons [30, 62–64]. Cerebral ischemia also induces microglial activation, but like the circulating immune systems, the precise mechanisms of activation following ischemia are not completely understood. Accumulating data show that CD14 receptors, followed by toll-like receptor 4 (TRL4) have been documented in microglia of the infarcted brain and could be one of the mechanisms involved in activation [65–67].
Activated macrophages have been observed as early as 2 hours following ischemia in rodents, while circulating macrophages appear in the brain after 10 hours. By 24–48 hours post insult, activated microglia and macrophages are present throughout the entire lesion and persist out to 1 week and longer [31, 68–71]. Once activated, microglia are thought to release a variety of toxic substances which lead to cell injury and death [62, 72]. Edaravone, a glutathione peroxidase mimic and free radical scavenger, appears to protect against experimental stroke by reducing microglial activation [73]. Hyperbaric oxygen treatment similarly decreased infarct volume through reduction of microglial activation [74]. Phagocytic microglia have been documented in ischemic brains following transient focal cerebral ischemia [63, 75]. Others have shown that minocycline, a tetracycline family antibiotic, protects against brain ischemia through the inhibition of microglial activation and proliferation [76, 77]. Co-culture models of microglia and neurons have mostly shown that the addition of microglia increases neuron death, and provides evidence for a damaging role of these immune cells [63, 67, 78, 79]. However, some microglial products are also neuroprotective [62, 80]. When microglial proliferation was inhibited in transgenic mice, infarct size was increased following ischemia, and suggests that proliferating microglia are also important in limiting ischemic damage [81]. There are a few explanations underlying these latter observations. Microglia are known to generate neurotrophic factors which have the potential to neurogenesis and plasticity. Microglia are known to produce TGF-β1, a growth factor. Microglia may also prevent release of toxic immune mediators by invading leukocytes by phagocytosing neutrophils [82, 83]. Phagocytic microglia/macrophages may remove necrotic debris and other potentially damaing substances [83].
2.4. Astrocytes
In addition to the above described inflammatory cells, astrocytes have been found to produce various inflammatory molecules [84, 85]. Astrocytes activate after brain ischemia leading to increased glial fibrillary acidic protein (GFAP) expression. Astrocytes also contribute to reactive gliosis [86], which can be destructive after injury [30, 87]. An astroglial response begins in the center of the ischemic lesion beginning 4–24 hours post insult, and reaches a peak around 4 days and is persists even 28 days later [88, 89]. Activated astrocytes lead to glial scar formation which have both neurotoxic and neurotrophic properties. The scar can function as a barrier which prevents axonal ingrowth and reinnervation, thus impeding recovery. This scar isolates damaged tissue from viable tissue, and prevents additional damage to the surrounding brain [88]. Astrocytes can also directly participate in the brain’s immune response as evidenced by expression of major histocompatibility complex (MHC) and respective costimulatory molecules. Astrocytes are also capable of developing Th2 (anti-inflammatory) responses; however, this has not been shown in ischemia [90]. Astrocytes are also known to elaborate cytokines, chemokines and inducible nitric oxide synthase (iNOS) [90, 91]. iNOS was detected in reactive hippocampal astrocytes following forebrain ischemia [91]. Furthermore, astrocyte-generated iNOS may increase injury to neurons om response to ischemia-like insults [92]. Astrocytes have also been shown to signal through TWEAK (tumor necrosis factor like weak inducer of apoptosis), which is a member of the tumor necrosis factor superfamily. TWEAK is secreted by neurons, astrocytes and endothelial cells, and when it binds its Fn14 receptor which is expressed on astrocytes, leads to proinflammatory molecule production [93–95]. Expression of TWEAK and Fn14 has been documented in a murine model of stroke, and a soluble decoy to Fn14 reduced infarct volume [94]. These observations suggest that activated astrocytes may also exacerbate injury to ischemic brain in a manner that is reminiscent of traditional immune cells.
3. ADHESION MOLECULES
Adhesion molecules involved in acute inflammatory responses permit interactions between endothelial cells, platelets, leukocytes, and lymphocytes, and are important in mediating events that lead to the infiltration of immune cells into the brain parenchyma [96]. Rolling, adhesion, and transendothelial migration of immune cells are three major steps, involved in leukocyte entry into the brain [97]. Immune cells interact with the vascular endothelium via three classes of adhesion molecules: selectins (P-selectin, E-selectin, and L-selectin), the immunoglobulin superfamily (intercellular adhesion molecules, e.g. ICAM-1, 2 and vascular cell adhesion molecule-1, or VCAM-1) and integrins (CD11a-c) [98, 99]. Inhibiting leukocyte adhesion by targeting various adhesion molecules and preventing leukocytes entry into ischemic brain led to reduced neurologic injury [35, 100]. Mice lacking various adhesion molecules have reduced infarct volume after transient focal cerebral ischemia [101–103]. Although many of these adhesion molecules are upregulated in both permanent and transient middle cerebral artery occlusion (MCAO)models [104–106], blocking these targets are effective largely when reperfusion occurs (i.e., transient, rather than permanent MCAO) [100, 107, 108].
3.1. Selectins
Selectins are calcium-dependent, transmembrane glyco-proteins that bind to carbohydrate residues (sialyl-Lewisx). They mediate adhesion between cells and leukocyte rolling. The three major selectins include E-selectin, P-selectin, and L-selectin [9, 32, 109]. There is very little E-selectin [104, 106], or P-selectin [8, 110] expression in uninjured brain vessels, but are present on the outer cell membrane of activated endothelium. E- and P-selectin contribute to leukocyte rolling and recruitment to areas of injury, reaching a peak 4–24 hours post stroke, and return to baseline by 72–96 hours [8, 104, 106, 111]. In contrast, L-selectin acts to guide leukocytes to activated endothelium, and sheds from the cell surface when the leukocyte binds the endothelial cell’s surface [112].
P- and E-selectin upregulation have been observed in several stroke models. Their presence appears to promote inflammatory responses and increase ischemic injury [8, 92, 104, 113–115]. Mice overexpressing P-selectin had larger infarcts compared to wildtype mice, whereas P- and E-selectin inhibition led to better neurological outcomes [113, 116, 117]. P-selectin’s role appears to differ in focal versus global cerebral ischemia. In focal ischemia, neutrophils accumulated in the ischemic cortex of wild-type mice compared to P-selectin deficient mice [101]. P-selectin knockout mice also had reduced neurological deficits compared to control mice. P-selectin inhibition also improved early restoration of cerebral blood flow and this led to better stroke outcome [101]. In contrast, antibody-mediated blocking of P-selectin in models of global cerebral ischemia, paradoxically reduced survival while still reducing leukocyte rolling [118]. Reasons for these conflicting outcomes are unclear, but indicate that inflammation after focal and global ischemia may be different. It is less clear whether L-selectin plays a significant role in brain ischemia. L-selectin mediates leukocyte transmigration, but existing work in stroke models does not indicate that it influences stroke outcome. In a rabbit stroke model, L-selectin inhibition with an antibody failed to influence stroke outcome [119]. Selectins have also been studied as a target for potential vaccines against stroke. In a few studies, animals given intranasal E-selectin induced immune tolerance to subsequent exposure to brain antigens, and led to improved outcome from experimental stroke and even prevent their occurrence [120, 121]. Thus, E-selectin exposure could lead to immune tolerance, and prevent subsequent leukocyte trafficking into the brain.
3.2. Immunoglobulin Superfamily
Immunoglobulin superfamily members include intercellular adhesion molecules (ICAM-1, ICAM-2), vascular cell adhesion molecule (VCAM-1), platelet-endothelial cell adhesion molecule-1 (PECAM-1), the mucosal vascular addressing cell adhesion molecule 1 (MAdCAM-1), and activated leukocyte cell adhesion molecule (ALCAM). ICAM-1 is constitutively expressed at low levels on endothelial cells, leukocytes, epithelial cells, and fibroblasts [6]. Upon activation by immune stimuli, ICAM-1 attaches immune cells to the endothelial wall in order to facilitate diapedesis thorough the vessel wall through integrin interactions (see sectin 4.3) into the site of injury [33, 122]. Its expression is increased soon after ischemia or cytokine exposure [6, 10, 123]. TNF-alpha and IL-1 are capable of inducing VCAM-1, while PE-CAM-1 (CD31) participates in the adhesion of endothelial cells to one another, as well as leukocyte transmigration across the endothelium. MAdCAM-1, typically expressed on mucosal endothelium, is a ligand for L-selectin and the α4β7 integrin.
Of the immunoglobulin superfamily members, ICAM-1 and VCAM-1 are the most studied in stroke models [6]. ICAM-1 increases within the brain’s vasculature hours after stroke onset, peaking at about 12–48 h. Its initial expression is followed by leukocyte infiltration and returns to near base line levels by 1 week [6, 10, 23, 68, 123]. Several groups have demonstrated that antibody inhibition of ICAM-1 [29, 57, 124–126], inhibiting ICAM-1 at the mRNA level or studying ICAM-1 deficient mice all lead to reduced leukocyte infiltration into the brain and improved neurological outcome from experimental stroke [6, 36, 102]. Interestingly, other studies have shown that nitric oxide donors blocked ICAM-1 expression and also led to neuroprotection [115]. In diabetic rat models, ischemia-induced ICAM-1 elevations were higher than that seen in non-diabetic rats, and could partially explain why hyperglycemia worsens stroke outcome [127].
Reports of VCAM-1 expression in stroke are conflicting. VCAM-1 mRNA and protein have been shown to increase after cerebral ischemia [128, 129], while other reports have failed to observe significant changes [126]. Nevertheless, a study of the leukotriene receptor antagonist, ONO-1078 in a model of rat global cerebral ischemia led to improved neurological deficits and reduced neuron death by inhibiting VCAM-1 upregulation [130]. Treatment of experimental stroke with fractionated heparin decreased VCAM-1 expression and reduced infarct size [131]. Leisz et al. [57] also found that gene knockdown of VCAM-1 via small interfering RNA demonstrated reduced T lymphocyte infiltration into the brain and decrased infarct volume after the ischemic insult. However, there are other studies that did not show any change in outcome using anti-VCAM-1 antibodies treatment [57, 129].
In humans, soluable ICAM-1 and VCAM-1 (sICAM-1 and sVCAM-1, respectively) have been documented to increase in the blood and cerebral spinal fluid of patients with recent stroke, and these increases correlated to neurological severity [10, 128]. Increased VCAM-1 expression in brain blood vessels and astrocytes has been observed in autopsy specimens of stroke victims [128].
3.3. Integrins
Integrins are surface proteins involved in cell-cell binding. They are composed of heterodimeric combinations of a and b subunits, and are activated in response to signaling molecules similar to other adhesion molecules. Integrins which associate with a common β2 chain (CD18) and are thus known as β2 integrins. Along with CD18, the majority of leukocytes also express a integrin chains CD11a (also known as LFA-1) and CD11b (also known as Mac-1). α and β integrins form het-erodimers which participate in the binding of leukocytes to endothelial cells via ICAM-1 [132]. Lymphocytes and monocytes integrins include a4b1 (CD49d/CD29 also known as VLA-1, very late antigen-1) and a4b7 (CD49d/CD103 or LPAM-1, lymphocyte Peyer’s patch adhesion molecule-1). Lymphocytes bind to the endothelium through these a integrins and either VCAM-1 or MAdCAM-1 [133].
In an in vitro model, hypoxia increased neutrophil CD11b expression, and aprotinin, which reduces CD11b expression, led to cytoprotection [134]. Reducing CD11b expression using 3-aminobenzamide (3-AB) to block poly-ADP ribose polymerase (PARP) was also protective [135]. At the in vivo level, antibodies to block CD11b and/or CD18 or studying mice lacking CD18 similarly reduced damage from MCAO, and was correlated to decreased numbers of neutrophils in the brain [34, 38, 57, 107, 136]. Blocking lymphocyte and monocyte integrins also limited damage due to ischemic injury. Treating rodents with antibodies against the α4 integrin led to smaller infarct volumes compared to control treatment [42, 137], and this was associated with reduced neurological deficit [42].
4. INFLAMMATORY MEDIATORS
Several immune mediators have been studied in stroke models, and many have been specifically studied for potential therapeutic value.
4.1. Cytokines
Cytokine expression increases in the brain after stroke, and are expressed by cells of the immune system, as well as brain cells such as glia and neurons [45, 138]. Cytokine upregulation has also been documented in blood, cerebrospinal fluid and brain of humans with stroke [139]. Interleukin-1 (IL-1α and β), TNF-α, interleukin-6 (IL-6), interleukin-10 (IL-10) and transforming growth factor-β (TGF-β) have been the most extensively studied cytokines in stroke models [12]. IL-1β appears to potentiate ischemic brain injury, while TNFα appears to contribute to and ameliorate neuronal injury. The collective literature surrounding IL-6, IL-10 and TGF-β suggest that these cytokines may be neuroprotective [140]. Many cytokines studied in stroke do not appear to be directly neurotoxic, since their administration to the uninjured brain does not lead to any obvious brain cell death. However, in the setting of injury, certain cytokines have been shown to both worsen ischemic brain damage.
4.1.1. IL-1
IL-1 is generally thought to potentiate ischemic brain damage. IL-1 exists in two isoforms, IL-1α and IL-1β. IL-1 also has an endogenous inhibitor, IL-1 receptor antagonist (IL-1ra). These three molecules have been extensively studied in stroke models [141]. IL-1β, rather than IL-1α is considered to be more engaged in ischemia pathogenesis [142]. IL-1β mRNA elevations occur within minutes following brain ischemia [123, 143], and the corresponding protein increases a few hours later starting from the infarct core and spreading to the peri-infarct area [45, 144]. In global cerebral ischemia models, IL-1β mRNA and protein expression appear biphasic, with an initial peak occurring as early as 1 h into reperfusion (following 20 minutes of forebrain ischemia), with a second peak occurring 6–24 h later [145]. Consistent with a damaging effect, IL-1β administered to rats exposed to focal cerebral ischemia led to increased infarct size [146], while mice lacking IL-1β had smaller infarcts compared to controls [142]. Reperfusion in diabetic rats also led to higher protein levels of IL-1β compared to non-diabetic rats, indicating that IL-1β may contribute to the worsening of ischemic damage by diabetes [127]. IL-1β results from conversion from its pro-form by IL-1β converting enzyme (ICE-1, a member of the caspase family) to its active form, and inhibiting ICE-1 is also protective [147]. IL-1R1 and IL-1R2 are IL-1’s two main receptors; however, only IL-1R1 appears to be involved in signal transduction [148]. IL-1R1 deficient mice suffered less brain damage due to hypoxic-ischemia (H/I) with reduced neurological deficits [149]. Overexpression of or treatment with IL-1ra, the endogenous inhibitor of the IL-1 receptor, also reduced infarct size [150, 151]. Similarly, IL-1ra deficient mice suffered worsened ischemic damage [141]. When mixed neuronal cultures from these mice were exposed to glutamate toxicity, cells from IL-1ra deficient mice experienced more death compared to wildtype cells [141].
4.1.2. TNF-α
Brain ischemia also leads to TNF-α upregulation. Like IL-1β, TNF-α expression is biphasic, with initial increases 1–3 hours post ischemia, and an initial peak at 12 h [123], followed by a second peak 24–36 h later [152, 153]. TNF-α expression has been observed in neurons [138], astrocytes [154] and in immune cells [153] in stroke models.
Although TNF-α and IL-1β often work synergistically, TNF-α seems to have both neurotoxic and neuroprotective effects in the brain, while IL-1β seems generally neurotoxic [155, 156]. Consistent with a damaging role, TNF-α inhibition reduces ischemic brain injury [157], and administration of recombinant TNF-α protein after stroke onset exacerbates damage [158]. However, TNF-α has also been shown to protect the brain in other situations. TNF-α has been implicated in ischemic tolerance [159], because mice lacking TNF receptors have larger infarcts [160]. TNF-α may also be region specific, as TNF-α in the striatum leads to neurodegeneration, while TNF-α in the hippocampus is neuroprotective [161]. TNF-α also leads to vasogenic edema as a consequence of endothelial cell death, and is involved in trafficking of circulating immune cells. However, TNF-α also activates repair processes and mediates neuronal plasticity [161]. The reasons for this disparity are still unknown, and several hypotheses have been proposed. First, TNF-α ‘s actions may depend on the timing. Acutely, TNF-α may have a detrimental effect, but may be beneficial at later time points [162], but this does not explain why TNF-α seems to underlie the phenomenon of tolerance. Other explanations for these disparate observations may have to do with the receptors to which TNF-α binds, and the fact that TNF-α is present in soluble and membrane-bound forms with potentially different functions [163]. Soluble TNF-α binds to TNF receptor 1, and potentiates damage, whereas membrane bound TNF-α binds to TNF receptor 2 (TNFR2) is associated with neuroprotection [62]. However, TNFR2 is primarily found on microglia and endothelial cells. To further complicate the picture, other studies indicate that TNF receptor 1 (TNFR1) signaling pathways are neuroprotective [164].
4.1.3. Other Inflammation-Related Cytokines
The role of IL-6 in the ischemic stroke is even less clear than that of the previously discussed cytokines. IL-6 has been shown to increase its expression continuously up to 24 hours after ischemia onset [123]. However, IL-6 deficient mice or mice treated with an IL-6 receptor antagonist were no different than wildtype or untreated controls, and suggests that IL-6 does not actively participate in ischemia pathogenesis [165, 166]. Conflicting data on IL-6 also exists. Herrmann et al. [167] reported beneficial effects of IL-6, while Smith et al. [168] showed detrimental effects. There are also reports showing strong correlation between serum IL-6 levels and inhospital mortality rates in stroke patients[168, 169]. Further, brain derived IL-6 appears to contribute to angiogenesis and neuronal survival through STAT3 activation and manganese-superoxide dismutase [170, 171].
IL-10 is an anti-inflammatory cytokine which inhibits proinflammatory cytokines including IL-1 and TNF-α. It also suppresses cytokine receptor expression and activation. In the brain, it is mostly produced by microglia and astrocytes, and is upregulated by ischemia and related insults [172]. Studies of exogenous IL-10 administration [173] and its gene transfer [174] in cerebral ischemia models lead to improved neurological and histological outcomes. Mononuclear cells of patients with acute stroke secrete increased IL-10 compared to patients without stroke [175] and elevated IL-10 levels have been found in the cerebrospinal fluid of stroke victims [176]. Consistent with a beneficial role of IL-10, patients with decreased IL-10 levels are thought to have higher stroke risk [177].
In brain, TGF-β1 has been observed in microglia and astrocytes. Low levels have been documented in neurons [178]. Viral vector mediated TGF-β1 overexpression led to decreased ischemic lesion sizes and reduced inflammation in a mouse stroke model [179]. A study in neurons cultured with microglia were protected by microglia, and this protection was thought to be due to TGF-β1secreted by the microglia [180].
4.2. Chemokines
Chemokines, or chemotactic cytokines, and their corresponding receptors are involved in leukoctye migration and extravasation. Chemokines are expressed by injured neurons, astrocytes, microglia, and endothelial cells, and circulating immune cells [45, 85, 181, 182]. The classes of chemokines are based on their structures: CXC, CC, C, CX3C, with “Cs” refer to two cysteine residues, and the X’s referring to intervening amino acids. Members of the chemokine family tend to bind to several receptors, and individual chemokine receptors bind multiple ligands [183–185]. The CXC subfamily also includes ELR+ or ELR− subgroups, based on whether there is a glutamate–leucine–arginine sequence between the N-terminus and the first cysteine [185, 186]. The ELR+ CXC chemokine subfamily are generally attract neutrophils, whereas the CC chemokines attract monocytes and T lymphocytes [45, 187]. Several chemokines in CXC group have been shown to participate in stroke pathogenesis [43, 188] by increasing leukocyte infiltration [99]. Ischemic brain insults lead to large increases in ELR+ chemokines, along with CXCR2 and its ligands CXCL1 and CXCL2 [43]. As predicted, CXCR2 inhibition following transient focal ischemia prevented increases in these genes, and decreased leukocyte infiltration into the brain; however, this was not associated with any improvement in infarct size, brain edema or neurological outcome.
Recent data also showed that CC chemokines monocyte chemoattractant protein-1 (MCP-1, CCL2) and macrophage inflammatory protein-1α (MIP-1α, CCL-3) led to expression and secretion of chemokines RANTES and CCL5 on T cells, and macrophage inflammatory protein-3 alpha (MIP-3α) was induced in animal stroke models [85, 123, 189–191]. At baseline, MCP-1 mRNA expression was almost absent, but ischemia led to a increases in MCP-1 mRNA within the ischemic cortex after either permanent or temporary MCAO around 12 h to 2 days and remained elevated 5 days later [181, 182]. CC chemokine inhibition or deficiency led to reduced brain injury, consistent with a deleterious role [37]. Similarly, MCP-1 overexpression led to exacerbated injury and increased recruitment of inflammatory cells [189].
Fractalkine (CX3CL1), unique in that it is expressed on neurons, acts through its CX3CR receptor found on microglia. Its expression has been localized to neurons and endothelial cells following experimental stroke. The finding of fractalkine on neurons and its receptor on microglia suggests that fractalkine may be involved in signaling between these cells [192]. Fractalkine deficient mice are protected from experimental stroke, indicating that fractalkine somehow exacerbates neuron death [193].
Chemokines also directly influence BBB permeability. MCP-1 enhanced the permeability of brain derived endothelial cells cocultured with astrocytes (a model of the BBB) and led to redictopms in tight junction (TJ) proteins, implicating MCP-1 in ‘opening’ the BBB [194].
Chemokines may also be important for stem cell migration into regions of injury, a property which could be potentially used to this advantage [195]. In fact, MCP-1 and SDF-1 and their corresponding receptors have been documented in ischemic brain and transplanted stem cells [196]. In stroke models, MCP-1 and other chemokines have been implicated in bone marrow derived stromal cell (BMSC) migration into sites of injury [197–199].
4.3. Arachidonic Acid Metabolites
Once immune cells are activated, phospholipase A2 (PLA2) is released and initiates the arachidonic acid (AA) cascade [22]. Stroke leads to cessation of blood flow and energy failure, which results calcium entry and accumulation in brain cells. Increased intracellular calcium activates PLA2 which, in turn, hydrolyses glycerophospholipids, and AA is released. PLA2 activity increases following experimental stroke [200]. AA metabolites contribute to worsening of ischemic brain injury by potentiating immune responses [201]. Consistent with this, PLA2 deficient mice exposed to experimental stroke developed less brain edema and had better outcomes compared to their wild type littermates [202]. AA undergoes metabolism through the cyclooxygenase (COX) and lipoxygenase (LOX) pathways, both of which are independently active in stroke pathogenesis.
4.3.1. Cyclooxygenase Pathways
Following arachidonic acid release, COX converts AA to prostaglandin H2 (PGH2). COX exists in two isoforms, COX-1 and COX-2. COX-1 is constitutively expressed in microglia, leukocytes and other cell types [203]. COX-1’s role in brain injury is unclear. Consistent with a beneficial role, COX-1 deficient mice have worse outcomes in brain ischemia models [204]. However, in a forebrain ischemia model, COX-1 inhibition led to increased numbers of healthy neurons in the CA1 region of the hippocampus, and would point to a damaging role of COX-1 in this model [205]. These reasons for these discrepancies are unknown, but suggest inherent differences in inflammatory responses between focal and global cerebral ischemia models.
COX-2 is induced following brain ischemia [206]. In autopsy specimens from stroke patients, COX-2 was observed within areas of ischemic brain [207], as well as regions remote from the infarct [208]. There are many COX metabolites that are biologically active, but accumulated data suggest that they are most likely deleterious in stroke. Prostaglandin E2 EP1 receptors have been identified as an effector involved in neurotoxicity [209]. Collectively, several studies now show that COX-2 inhibitor treatment or the study of COX-2 deficient mice led to improved neurological outcome after stroke [206, 210, 211], whereas COX-2 overexpression worsens outcome [212]. COX-2’s toxic effect appears to be mediated though PGE2 rather than ROS, even though COX-2 is capable of generating both [213].
4.3.2. 5-Lipoxygenase Pathway
In brain, less is known about the role of the lipoxygenase pathway, compared to that of the COX pathway. AA may alternatively be converted to 5-hydroperoxyeicosatetraenoic acid (5-HPETE) via 5-lipoxygenase (5-LOX). 5-LOX is metabolized to leukotriene A4 (LTA4), a precursor to cysteinyl leukotrienes (cysLTs). LTA4 is converted to leukotriene C4 (LTC4), which is a potent chemoattractant thought to contribute to BBB disruption, as well as tissue edema and cell death. In the setting of stroke, AA and LTC4 increases are biphasic, and correlate to BBB disruption [214]. 5-LOX has also been documented in autopsy specimens from stroke victims, and its expression localized to perivascular monocytes [215]. In a stroke model, the 5-LOX inhibitor AA861 led to decreased LTC4 levels and reduction in brain edema and cell death [216]. Furthermore, exposure of a neuron cell line to oxygen glucose deprivation led to attenuated cell death with treatment by 5-LOX inhibitor caffeic acid [217]. In contrast, at the in vivo level, 5-LOX deficiency failed to have any effect on stroke outcome in both permanent and temporary MCAO [218]. The reasons for this disparity might be due to an unforeseen phenotype in lifelong 5-LOX deficient mice, but further studies are needed to more precisely clarify.
AA may also be converted to other biologically active leukotrienes via 12-LOX. 12-LOX is found in platelets, but nevertheless leads to oxidative stress which can be toxic to brain tissue. In a rabbit model of multiple small embolic infarcts, baicalein, an inhibitor of 12/12-LOX, was found to improve neurological outcomes when administered as late as 2 h post insult [219]. However, there are known interspecies differences within 12/15-LOX making drug development challenging. Yet, a recent study showed that novel compound ML351 which blocked 12/15-LOX in both humans and rodents, was protective in a murine stroke model [220]. Thus, there is a clear need for more work in the area of the lipoxygenase pathways.
4.4. Nitric Oxide/Nitric Oxide Synthase
Nitric oxide (NO) is involved in a variety of processes including as host defense, regulation of vascular tone, and modulation of the immune response. NO enters cells readily, and reacts with various molecular targets. Through the enzyme nitric oxide synthase (NOS), NO is generated from L-arginine. To date, three nitric oxide synthases (NOS) isoforms have been studied in stroke: endothelial NOS (eNOS or NOS-3), neuronal NOS (nNOS or NOS-1), and inducible NOS (iNOS or NOS-2). iNOS is found almost exclusively in inflammatory cells, including circulating leukocytes, microglia, but also in astrocytes. iNOS mRNA and protein both increase in experimental stroke [221–223]. In addition to its participation in various signaling pathways, NO is thought to cause direct DNA damage through the formation of peroxynitrite, when NO reacts with superoxide [224–226]. Pharmacological inhibition or genetic deletion of iNOS leads to reduced infarct volume and improved neurological outcomes [222, 227]. Further, in therapeutic hypothermia, where cooling conditions leads to neuroprotection, microglia have been shown to generate less NO and iNOS [228], and estrogen and progesterone appears protect the brain from experimental stroke by modulating iNOS expression [229, 230].
4.5. Reactive Oxygen Species
Immune cells generate reactive oxygen species (ROS) through several enzyme systems. These include COX, nicotinamide adenine dinucleotide phosphate (NADPH) oxidase, xanthine dehydrogenase and xanthine oxidase. The myeloperoxidase (MPO) and monoamine oxidase (MAO) systems lead to the production of hypocholorous acid and hydrogen peroxide, respectively. The most studied ROS in the ischemic brain is superoxide anion. Superoxide anion has been shown to cause direct brain injury, or indirect injury when it reacts with NO to generate peroxynitrite [231].
NOX is a multi-component enzyme originally identified in immune cells. It contains both cytoplasmic subunits (p45phox, p67phox, and p40phox and Rac2) and plasma membrane subunits (p91phox, p22phox). After NOX activation and phosphorylation, the cytosolic subunits translocate to the membrane and form a complete complex on the cell surface, enabling activated NOX to generate superoxide from oxygen by transferring electrons from NADPH [232]. Experimental stroke leads to increases in brain NOX [233], and NOX generated superoxide may be the major effector molecule which cause microglia to exacerbate ischemic injury [234]. In fact, mice lacking the gp91 subunit of NOX have reduced ischemic lesion size compared to wildtype controls [235]. By transplanting NOX deficient bone marrow in to wildtype host mice, or vice versa, NOX in circulating immune cells was found to contribute more to stroke pathology compared to NOX found in microglia [236]. NOX has also been implicated as an important factor by which hyperglycemia exacerbates stroke outcome [237].
Found largely in neutrophils and monocytes, myeloperoxidase (MPO) is a bactericical enzyme whose actions are through H2O2 and hypochlorous acid. Increases in serum MPO may predict stroke risk, and MPO has been observed in experimental stroke models of both temporary and permanent MCAO [37]. Interestingly, infarct size in MPO deficient mice actually increased after stroke, suggesting a beneficial role [238]. Products of nitrosylation were also increased in MPO deficient mice, suggesting that any protective effect of MPO may be through scavenging nitrotyrosine, which is produced via peroxynitrite reactions [238]. Thus, MPO may paradoxically attenuate ROS-mediated damage.
4.6. Matrix Metalloproteinases (MMPs)
Matrix metalloproteinases (MMPs) comprise a group of proteases involved in the breakdown of proteins of the extracellular matrix. These proteases are normally involved in a variety of physiological processes including development, wound healing, cone growth, ovulation and angiogenesis. However, under injury conditions such as brain ischemia, MMPs are upregulated and activated especially within peri-infarct areas, and are part of the neuroinflammatory response. MMPs exist in a pro-form, that is, they are present in an inactivated state. However, MMPs are activated when cleaved by proteases such as plasmin or other MMPs [239]. Tissue plasminogen activator (tPA) disrupts the extracellular matrix as well as components of the BBB through activation of plasmin. This may result in extrusion of serum protein and even hemorrhage [240, 241]. Microglia are a major source of MMPs, and ischemia can also cause MMP activation in astrocytes [242].
In models of focal ischemia, MMP-9 activity increases at 15–48 h) and returns to baseline around 15 days. MMP-2 peaks at 5 days and returns to baseline around 15 days [243, 244]. MMPs contribute to apoptotic neuronal cell death by processing death receptor ligands, TNF-α and FasL. Not surprisingly, pharmacologic MMP inhibition reduces infarct size, brain edema and hemorrhage [245]. However, not all MMPs appear to contribute to stroke pathology. In fact, mice lacking MMP-9, but not MMP-2 had smaller infarcts compared to wildtype controls [246, 247]. MMP-2 deficient mice fared no differently than control mice following focal cerebral ischemia. Observations at the clinical level seem to parallel findings in rodent stroke models. In stroke patients, serum MMP-9 levels appeared to correlate to stroke severity, whereas MMP-2 did not [248]. Considering that MMP-9 is produced by immune cells, but MMP-2 is not, emphasizes the significance of the immune system in stroke pathogenesis. Like NOX, MMP-9 derived from circulating leukocytes, rather than MMP-9 from brain, appears to contribute more to ischemic brain injury. Chimeric mice transplanted with bone marrow from MMP-9 deficient mice suffered less injury than chimeric MMP-9 deficient mice transplanted with marrow containing intact MMP-9 [249].
Not all MMP functions are detrimental. MMPs may also be involved in plasticity and recovery. Mice subjected to focal cerebral ischemia and treated with the broad spectrum MMP inhibitor (GM6001) had decreased migration of neuronal precursor cells from the subventricular zone (SVZ) into the striatum [250], indicating that MMPs are important in neurogenic migration. MMPs also associate with angiogenic factors including vascular endothelial growth factor (VEGF). MMP inhibition suppressed neurovascular remodeling post stroke, and reduced VEGF signaling [251].
5. TRANSCRIPTIONAL REGULATION OF INFLAMMATION
Several transcription factors are active following cerebral ischemia leading to changes in gene expression. Those transcription factors known to be involved in the ischemic inflammatory response will be discussed here.
5.1. Nuclear Factor κB (NF-κB)
Nuclear factor-kappaB (NF-κB) is largely associated with the initiation of inflammatory responses [252]. It has been widely studied in stroke models. It contains dimers of the Rel family subunits: Rel (cRel), RelA (p65), RelB, NF-κB1 (p50 and the p105 precursor) and NF-κB. NF-κB most commonly exists as a heterodimer composed of Rel A (p65) and p50. It is located in the cytoplasm in an inactivated state where it is bound to IκB, its endogenous inhibitor protein. Several pro-inflammatory stimuli activate IκB’s upstream kinase (IKK). Once activated, IKK phosphorylates IκB at serines 32 and 36 leading to its phosphorylation, ubiquitination and degradation by the cell’s proteasome. NF-κB, now free from IκB, is able to translocate into the nucleus, where it binds to concensus κB sites, sites contained within the promoters of many inflammatory genes previously discussed. While therapeutic hypothermia correlated to reduced IKK and NF-κB activation, suggesting a damaging role for NF-κB [253], its role in stroke is still conflicting [254]. Mice lacking NF-κB’s p50 subunit subjected to stroke are protected [255], observations consistent with a damaging role of NF-κB. Pharmacologically inhibiting NF-κB with S-nitrosoglutathione (GSNO) similarly led to improved outcome [115]. IKK inhibition also reduced infarct size in stroke experiments [256], and constitutive activation of IKK led to larger infarct size [256]. Similar observations were made in a global ischemia where treatment with NF-κB decoy oligodeoxynucleotides reduced neuronal damage [257]. However, diethyldithiocarbamate (DDTC), a NF-κB inhibitor, given to rats subjected to experimental stroke led to increased infarct sizes compared to controls, consistent with a beneficial role of NF-κB [258]. It is unclear why these conflicting observations exist, but some have speculated over whether this may depend on the cell type in which NFkB is activated, the experimental model used, or an off target effect of the pharmacological inhibitors used.
5.2. Mitogen-Activated Protein Kinase (MAPK)
Mitogen-activated protein kinases (MAPK) are a cascade of kinase phosphorylation and transcription factor activation enzymes which ultimately regulate inflammatory gene production [2, 259]. Three interlinked MAPK signaling pathways have been studied in cerebral ischemia. They include the stress-activated protein kinases/c-Jun N-terminal kinases (SAPK/JNK), p38 MAPKs and extracellular signal-regulated kinases (ERKs) [259–261]. p38 MAPK is involved in the upregulation of many proinflammatory genes [262]. In global cerebral ischemia, MLK3-MKK4-JNK activation has been documented as early as 30 min post injury onset, with a second period of activation 3 days later [263]. Knockdown of POSH (plenty of SH3s) using antisense oligodeoxynucleotides protected neurons of the hippocampal CA1 region, and reduced POSH interactions with MLK3, MKK4 and phospho-JNKs. JNK signaling was also attenuated. In a model of in vitro ischemia in astrocytes, the addition of bone marrow stromal cells led to MAPK activation and subsequently exerted protection to astrocytes [264]. Using a neuronal membrane lipid precursor, CDP-choline, others have demonstrated improved recovery after ischemic stroke, and this was associated with decreased phosphorylation of MAP-kinase family members, ERK1/2, MEK1/2, and Elk-1 transcription factor. In global cerebral ischemia, activated p38 MAPK has been detected in hippocampal neurons [261] and microglia [265], and suggests a role in inflammation. Consistent with a damaging role of inflammation in brain ischemia, treatment with p38 MAPK inhibitor lead to less brain injury and decreased neurological deficits [2].
6. INITIATION OF INNATE IMMUNE RESPONSES
The initiation of the immune response following stroke is still not fully clear, but recent studies have focused on various pro-inflammatory factors elaborated by the ischemic brain that might act on receptors involved in innate immune responses. The two main groups of innate immune receptors studied in brain ischemia are found on microglia and circulating immune cells, and include the Toll-like receptors (TLRs) and purinergic receptors. The ischemic brain is thought to generate extracellular nucleic acid following cell lysis. These and other ligands are often referred to as danger associated molecular pattern molecules (DAMPs). When bound to their respective ligands, an inflammasome is formed consisting of nucleic acids such ATP, UTP, adenosine and other pro-inflammatory molecules such as caspase 1, leading to the maturation and elaboration of pro-inflammatory cytokines and a full blown inflammatory response [13, 266] Toll-like receptors (TRLs) and purinergic receptors are widely expressed on microglia [13, 267].
6.1. Toll-Like Receptors
Toll-like receptors (TLRs) exist on the cell surface in order to recognize extracellular pathogens through pathogen-associated molecular patterns (PAMPs). They are also known to recognize similar patterns on injured or altered cell surfaces, and these are patterns are collectively known as death associated molecular patterns (DAMPs). They have been the focus of recent investigation, and are considered to play pivotal roles in the initiation of the inflammatory response in stroke and related injuries [268, 269]. In addition to traditional immune cells, TLRs have also been described on other cells of the nervous system, including microglia, astrocytes, neurons, and cells of the cerebral vasculature [270, 271]. Reports in the brain ischemia literature point to DAMPs, including high mobility group box 1 protein (HMGB1) [272], heat shock proteins, extracellular peroxire-doxin [273] and nucleic acids [13] as likely ligands for TLRs.
Microglial activation following cerebral ischemia is associated with signaling through TLRs, particularly TLR2 and TLR4. TLR activation leads to increased cytokine expression, and other immune responses ultimately leading to brain cell damage. Increased brain TLR2 expression has been documented in both in vitro and in vivo stroke models [274–276]. Genes upregulated as a result of TLR2 activation include NF-κB, Cyclooxygenase-2 (COX2), IL-1β, IL-17, IL-23, and TNF-α, all of which have been shown to increase after ischemia [274, 276–278]. Yao et al. [278] showed that upregulation of TLR2 and IL-1β expression in an in vitro ischemia model led to neuronal cell death. The ischemic insult induced IL-1β, but cell death was prevented in TLR2 knockout mice. However, Hua et al. [279] reported that mice lacking TLR 2 had larger infarcts and increased mortality compared to wildtype mice. Brain ischemia also leads to increased TLR4 expression. In some reports, TLR4 deficient mice had smaller infarcts and better neurological function compared to wild-type mice. This was not the case for TLR3 or TLR9, however. TLR4 co-localized to microglia and TLR4 deficient mice had few numbers of activated microglia compared to mice with intact receptor [280, 281].
6.2. Purinergic Receptors
Purinergic receptors have been detected in both brain and periphery. They are a family of receptors that execute various cellular functions. P2 purinoreceptors are both ionotropic and metabotropic. The P2X family are ionotropic and regulate ion flow, whereas the P2Y subfamily are metabotropic and are G-protein coupled. In microglia and other immune cells, purinergic receptors are involved in migration and phagocytosis [282]. Purinergic receptors on microglia are of relevance to understanding how inflammation may be initiated in brain injury because they are capable of binding nucleotides released by injured cells. Microglial purinergic receptors has mostly focused on P2X7, where it has been shown to activate microglia in experimental brain ischemia. Pharmacologic blockade of P2X7 led to decreased ischemic damage [283–286]. Less work has been carried out on the P2Y receptor; however, of clinical relevance is the P2Y12 receptor [282, 287]. P2Y12 found on platelets as well as immune cells, and is inhibited by clopidogrel, a widely prescribed antiplatelet agent. P2Y12 is present on the surface of microglia and is activated by ATP or ADP. Once activated, P2Y12 promotes microglial chemotaxis and is also involved in the phosphorylation of Akt [288]. We have recently shown that P2Y12 mediates microglial migration in brain ischemia, and its deficiency or inhibition is neuroprotective [289].
7. INFLAMMATORY RESPONSES TO THE OTHER ORGANS FOLLOWING ISCHEMIC STROKE
Recent studies indicate that inflammatory responses following stroke affect the entire body, and not simply the brain. For example, splenectomy has been shown to confer neuroprotection against experimental stroke. The spleen is an important lymphatic organ, and sequesters red and white blood cells. It is involved in antibody synthesis, and also removes antibody coated cells from the circulation. Ajmo et al. [290] showed that splenectomy reduced lesion size in a stroke model and resulted in decreased numbers of activated microglia, macrophages, and neutrophils in the brain. These data suggest that spleen-mediated peripheral immune responses contribute to the inflammation in stroke, and that splenectomy could improve stroke outcome.
Evidence suggests that stroke renders the body in a state of immunodepression which could be detrimental. Soon after stroke, circulating immune cells are quickly reduced, thus increasing the risk of developing infections. This systemic immunodepression has been documented as early as 12 hours post stroke, and continues out to several weeks [11, 291, 292]. Immune cells of the spleen, thymus, liver and lymph node are reduced following stroke, and this may explain the observed immunosuppression [11, 153, 291–293]. The immunosuppression has been attributed to increased activity of the sympathetic nervous system (SNS) and the hypothalamic-pituitary-adrenal axis (HPA) [11, 294]. As a result, immune cells undergo increased apoptosis in these organs after stroke, and cause these secondary organs to atrophy [11, 153, 291]. However, whether lower numbers of immune cells in the circulation are due to their entry into ischemic brain has yet to be definitively shown.
A consequence of this immunodepression is thought to lead to infectious complications which often arise after stroke [11, 153, 291] and lead to worsened outcome [295–297]. While hyperactivity of the SNS and the HPA is thought to underlie this phenomenon, the precise signals and mechanisms that trigger this immunodepression remain unclear. Blocking the SNS and HPA in experimental stroke models prevented splenocyte apoptosis and decreased circulating lymphocytes, along with decreased infection and reduced mortality [11, 294]. In line with experimental studies, evidence of SNS-mediated immunosuppression in stroke patients has been reported [3]. T and B lymphocytes undergo apoptosis in stroke, and this can increase susceptibility to infection [298]. The vagal cholinergic anti-inflammatory pathway appears to be another means of cross talk between the CNS and immune system. The vagus nerve can be activated by pro-inflammatory cytokines to release acetylcholine. This in turn inhibits the release of pro-inflammatory mediators by macrophages [299, 300]. Vagal nerve stimulation has been shown to inhibit the release of pro-inflammatory cytokines and improves outcomes in different stroke models [300]. Thus, this vagal cholinergic anti-inflammatory pathway may also be involved in post stroke immunodepression.
8. BENCH TO BEDSIDES: TRIALS, TRIBULATIONS AND PROMISING THERAPIES
8.1. Clinical Trials
Following several promising preclinical studies, a few clinical trials were carried out to determine whether anti-inflammatory strategies were beneficial. However, some of these trials did not meet with success either due to unanticipated effects of the agents tested or inappropriate study design [301–303]. Yet, with increased knowledge of the complexities of inflammation in stroke, a few treatments may be on the horizon.
8.1.1. Anti-Integrin
In order to limit leukocyte adhesion and migration into the infarcted brain, a few clinical studies treated stroke patients with anti-integrin therapies. LeukArrest studied a humanized CD11/CD18 antibody in stroke patients who presented within a 12 hour window [302]. The Acute Stroke Therapy by Inhibition of Neutrophils (ASTIN) trial studied treatment with a nonantibody peptide, recombinant neutrophil inhibiting factor (rNIF). rNIF was given within 6 hours of symptom onset [304]. Unfortunately, in both cases, studies were stopped early due to a lack of effect in primary endpoints. Both drugs seemed to have a beneficial effect in animal stroke models [38, 136], but the lack of benefit in humans may be explained by later treatment windows in humans, or inherent differences in neutrophil integrins between humans and other species. Consistent with this line of thinking, CD11b decreases after stroke in humans [305], but has been shown to increase in rodent stroke models [306].
8.1.2. Anti-ICAM1
Antibodies against the adhesion molecule ICAM-1 was studied at the phase III clinical trial level in stroke patients. The results of the study showed that ICAM-1 antibody failed to improve outcome in ischemic stroke, but it also showed that such antibody treatment actually made outcome worse [301, 303]. Unfortunately, the antibody given to study participants was a murine antibody, and had not been adapted for use in humans. This may have lead to complement activation by the presence of a non-humanized antibody, and the development of clinically significant fever and other adverse immune events, thus negating any potential neuroprotective benefit of ICAM-1 blocking [98]. Further, the rationale for treatment with anti-adhesion strategies was based on the observation of the ‘no-reflow’ phenomenon in animals models, but this phenomenon had not been clearly documented in humans. Thus, the “no-reflow” phenomenon, thought to be due to leukocyte plugging of the brain’s microvasculature, might be relevant in rodent stroke models, but of limited or unknown relevance in humans [307].
8.1.3. Minocycline
Minocycline is tetracycline family antibiotic. It has also been shown to inhibit both inflammatory and apoptotic pathways in stroke models. Of its anti-inflammatory properties, minocycline has been shown to suppress microglial activation, and inhibit MMP and NO production. Its anti-inflammatory effect appears to be due to a mechanism inhibiting MAPK activation in microglia [308]. As such, minocycline has been shown to protect the brain against cerebral ischemia and lessen functional impairment [77, 309–311]. Lampl et al. [312] conducted a clinical trial giving oral minocycline to ischemic patients and found that functional endpoints were improved amongst minocycline-treated patients. However, this study was an open-label, evaluator-blinded study and the total number of the patients was relatively small. A second study established safety, dose ranging and feasibility in combination with rt-PA [313], and that intravenous minocycline administration could decrease plasma matrix metalloproteinase-9 in stroke patients [314]. Clinical studies to determine minocycline’s efficacy in stroke and long term recovery (Neuroprotection with minocycline therapy for acute stroke recovery trial, NeuMAST) are also ongoing.
8.2 Future Therapies
8.2.1. FTY 720
FTY720 (Fingolimod) is a sphingosine-1-phosphate (S1P) receptor agonist, and was developed as an anti-inflammatory agent [315, 316]. It is already FDA-approved for the treatment of multiple sclerosis. FTY720 crosses the blood-brain barrier where it can be phosphorylated by sphin-gosine kinase (SphK) [317, 318], into the active compound phospho-FTY720, which then acts on S1P receptor subtypes S1P1, S1P3, S1P4, S1P5. It has been shown to be neuroprotective effect against many central nervous system diseases including cerebral ischemia [318–322]. FTY720 regulates myelination of axons and activation of microglia following injury, as well as proliferation and migration of neural precursor cells and neuronal differentiation. It has also been shown to have antiapoptotic and anti-inflammatory properties [321–327]. FTY720 exerts its immunomodulatory actions by affecting lymphocyte production, trafficking, and apoptosis through S1P receptors leading to the depletion of circulating lymphocytes, and prevents release of lymphocytes from the lymph nodes. Most of the past reports have shown beneficial effects of S1P in brain ischemia, but Liesz et al. [57] showed opposite results. These authors found that while FTY720 treatment did show a reduction of lymphocyte brain infiltration, they did not observe significant reduction in infarct volumes and improvement in neurological deficits [57]. Liu et al. [328] recently published a meta-analysis of the FTY720’s efficacy in animal models of cerebral ischemia. In this analysis, they concluded that FTY720 reduced infarct volume and improved functional outcome. However, the authors also indicated that more experimental studies should be performed to evaluate the safety of FTY720 in the future. Thus, the S1P pathways are a promising area of investigation for stroke treatment.
9. BRIEF SUMMARY
Inflammation following ischemic stroke is increasingly recognized as a key element in its progression. In this review we have focused on many key players which are involved in the inflammatory responses following stroke, such as cellular components including microglia and leukocytes, adhesion molecules, inflammatory mediators and chemokines. While acute inflammatory responses appear to exacerbate ischemic injury, later responses may be essential in recovery and repair. This may explain some of the conflicting reports in the scientific literature. Regardless, future work towards a better understanding of this field are needed, with the hopes of translating discoveries into treatments for stroke patients.
Acknowledgments
This work was supported by grants from the National Institutes of Health (NS40516, to MY), the Veteran’s Merit Award (I01 BX000589 to MY), the Uehara Foundation (2013 Research Fellowship, to MK). Grants to MY were administered by the Northern California Institute for Research and Education, and supported by resources of the Veterans Affairs Medical Center, San Francisco, California.
Footnotes
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
Send Orders for Reprints to reprints@benthamscience.ae
References
- 1.Durukan A, Tatlisumak T. Acute ischemic stroke: overview of major experimental rodent models, pathophysiology, and therapy of focal cerebral ischemia. Pharmacol Biochem Behav. 2007;87(1):179–197. doi: 10.1016/j.pbb.2007.04.015. [DOI] [PubMed] [Google Scholar]
- 2.Barone FC, Feuerstein GZ. Inflammatory mediators and stroke: new opportunities for novel therapeutics. J Cereb Blood Flow Metab. 1999;19(8):819–834. doi: 10.1097/00004647-199908000-00001. [DOI] [PubMed] [Google Scholar]
- 3.Chamorro A, Hallenbeck J. The harms and benefits of inflammatory and immune responses in vascular disease. Stroke. 2006;37(2):291–293. doi: 10.1161/01.STR.0000200561.69611.f8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Davies CA, Loddick SA, Stroemer RP, Hunt J, Rothwell NJ. An integrated analysis of the progression of cell responses induced by permanent focal middle cerebral artery occlusion in the rat. Exp Neurol. 1998;154(1):199–212. doi: 10.1006/exnr.1998.6891. [DOI] [PubMed] [Google Scholar]
- 5.Becker KJ. Inflammation and acute stroke. Curr Opin Neurol. 1998;11(1):45–49. doi: 10.1097/00019052-199802000-00008. [DOI] [PubMed] [Google Scholar]
- 6.Stanimirovic D, Shapiro A, Wong J, Hutchison J, Durkin J. The induction of ICAM-1 in human cerebromicrovascular endothelial cells (HCEC) by ischemia-like conditions promotes enhanced neutrophil/HCEC adhesion. J Neuroimmunol. 1997;76(1–2):193–205. doi: 10.1016/s0165-5728(97)00057-x. [DOI] [PubMed] [Google Scholar]
- 7.Morioka T, Kalehua AN, Streit WJ. Characterization of microglial reaction after middle cerebral artery occlusion in rat brain. J Comp Neurol. 1993;327(1):123–132. doi: 10.1002/cne.903270110. [DOI] [PubMed] [Google Scholar]
- 8.Suzuki H, Abe K, Tojo S, Morooka S, Kimura K, Mizugaki M, Itoyama Y. Postischemic expression of P-selectin immunore-activity in rat brain. Neurosci Lett. 1997;228(3):151–154. doi: 10.1016/s0304-3940(97)00385-6. [DOI] [PubMed] [Google Scholar]
- 9.Hallenbeck JM. Significance of the inflammatory response in brain ischemia. Acta Neurochir Suppl. 1996;66:27–31. doi: 10.1007/978-3-7091-9465-2_5. [DOI] [PubMed] [Google Scholar]
- 10.Danton GH, Dietrich WD. Inflammatory mechanisms after ischemia and stroke. J Neuropathol Exp Neurol. 2003;62(2):127–136. doi: 10.1093/jnen/62.2.127. [DOI] [PubMed] [Google Scholar]
- 11.Prass K, Meisel C, Hoflich C, Braun J, Halle E, Wolf T, Ruscher K, Victorov IV, Priller J, Dirnagl U, Volk HD, Meisel A. Stroke-induced immunodeficiency promotes spontaneous bacterial infections and is mediated by sympathetic activation reversal by poststroke T helper cell type 1-like immunostimulation. J Exp Med. 2003;198(5):725–736. doi: 10.1084/jem.20021098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Han HS, Yenari MA. Cellular targets of brain inflammation in stroke. Curr Opin Investig Drugs. 2003;4(5):522–529. [PubMed] [Google Scholar]
- 13.Iadecola C, Anrather J. The immunology of stroke: from mechanisms to translation. Nat Med. 2011;17(7):796–808. doi: 10.1038/nm.2399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Spite M, Serhan CN. Novel lipid mediators promote resolution of acute inflammation: impact of aspirin and statins. Circ Res. 2010;107(10):1170–1184. doi: 10.1161/CIRCRESAHA.110.223883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schilling M, Besselmann M, Muller M, Strecker JK, Ringel-stein EB, Kiefer R. Predominant phagocytic activity of resident microglia over hematogenous macrophages following transient focal cerebral ischemia: an investigation using green fluorescent protein transgenic bone marrow chimeric mice. Exp Neurol. 2005;196(2):290–297. doi: 10.1016/j.expneurol.2005.08.004. [DOI] [PubMed] [Google Scholar]
- 16.Denes A, Vidyasagar R, Feng J, Narvainen J, McColl BW, Kauppinen RA, Allan SM. Proliferating resident microglia after focal cerebral ischaemia in mice. J Cereb Blood Flow Metab. 2007;27(12):1941–1953. doi: 10.1038/sj.jcbfm.9600495. [DOI] [PubMed] [Google Scholar]
- 17.Ishikawa M, Zhang JH, Nanda A, Granger DN. Inflammatory responses to ischemia and reperfusion in the cerebral microcirculation. Front Biosci. 2004;9:1339–1347. doi: 10.2741/1330. [DOI] [PubMed] [Google Scholar]
- 18.del Zoppo G, Ginis I, Hallenbeck JM, Iadecola C, Wang X, Feuerstein GZ. Inflammation and stroke: putative role for cytokines, adhesion molecules and iNOS in Brain Res.ponse to ischemia. Brain Pathol. 2000;10(1):95–112. doi: 10.1111/j.1750-3639.2000.tb00247.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dietrich PY, Walker PR, Saas P. Death receptors on reactive astrocytes: a key role in the fine tuning of brain inflammation? Neurology. 2003;60(4):548–554. doi: 10.1212/01.wnl.0000042049.74547.7f. [DOI] [PubMed] [Google Scholar]
- 20.Pantoni L, Sarti C, Inzitari D. Cytokines and cell adhesion molecules in cerebral ischemia: experimental bases and therapeutic perspectives. Arterioscler Thromb Vasc Biol. 1998;18(4):503–513. doi: 10.1161/01.atv.18.4.503. [DOI] [PubMed] [Google Scholar]
- 21.Yilmaz G, Granger DN. Cell adhesion molecules and ischemic stroke. Neurol Res. 2008;30(8):783–793. doi: 10.1179/174313208X341085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stanimirovic D, Satoh K. Inflammatory mediators of cerebral endothelium: a role in ischemic brain inflammation. Brain Pathol. 2000;10(1):113–126. doi: 10.1111/j.1750-3639.2000.tb00248.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wang X, Siren AL, Liu Y, Yue TL, Barone FC, Feuerstein GZ. Upregulation of intercellular adhesion molecule 1 (ICAM-1) on brain microvascular endothelial cells in rat ischemic cortex. Brain Res Mol Brain Res. 1994;26(1–2):61–68. doi: 10.1016/0169-328x(94)90074-4. [DOI] [PubMed] [Google Scholar]
- 24.Stanimirovic DB, Wong J, Shapiro A, Durkin JP. Increase in surface expression of ICAM-1, VCAM-1 and E-selectin in human cerebromicrovascular endothelial cells subjected to ischemia-like insults. Acta Neurochir Suppl. 1997;70:12–16. doi: 10.1007/978-3-7091-6837-0_4. [DOI] [PubMed] [Google Scholar]
- 25.Hess DC, Zhao W, Carroll J, McEachin M, Buchanan K. Increased expression of ICAM-1 during reoxygenation in brain endothelial cells. Stroke. 1994;25(7):1463–1467. doi: 10.1161/01.str.25.7.1463. discussion 1468. [DOI] [PubMed] [Google Scholar]
- 26.Howard EF, Chen Q, Cheng C, Carroll JE, Hess D. NF-kappa B is activated and ICAM-1 gene expression is upregulated during reoxygenation of human brain endothelial cells. Neurosci Lett. 1998;248(3):199–203. doi: 10.1016/s0304-3940(98)00239-0. [DOI] [PubMed] [Google Scholar]
- 27.Arvin B, Neville LF, Barone FC, Feuerstein GZ. The role of inflammation and cytokines in brain injury. Neurosci Biobehav Rev. 1996;20(3):445–452. doi: 10.1016/0149-7634(95)00026-7. [DOI] [PubMed] [Google Scholar]
- 28.Hartl R, Schurer L, Schmid-Schonbein GW, del Zoppo GJ. Experimental antileukocyte interventions in cerebral ischemia. J Cereb Blood Flow Metab. 1996;16(6):1108–1119. doi: 10.1097/00004647-199611000-00004. [DOI] [PubMed] [Google Scholar]
- 29.Chopp M, Li Y, Jiang N, Zhang RL, Prostak J. Antibodies against adhesion molecules reduce apoptosis after transient middle cerebral artery occlusion in rat brain. J Cereb Blood Flow Metab. 1996;16(4):578–584. doi: 10.1097/00004647-199607000-00007. [DOI] [PubMed] [Google Scholar]
- 30.Wang Q, Tang XN, Yenari MA. The inflammatory response in stroke. J Neuroimmunol. 2007;184(1–2):53–68. doi: 10.1016/j.jneuroim.2006.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nilupul Perera M, Ma HK, Arakawa S, Howells DW, Markus R, Rowe CC, Donnan GA. Inflammation following stroke. J Clin Neurosci. 2006;13(1):1–8. doi: 10.1016/j.jocn.2005.07.005. [DOI] [PubMed] [Google Scholar]
- 32.Kim JS. Cytokines and adhesion molecules in stroke and related diseases. J Neurol Sci. 1996;137(2):69–78. doi: 10.1016/0022-510x(95)00338-3. [DOI] [PubMed] [Google Scholar]
- 33.Huang J, Upadhyay UM, Tamargo RJ. Inflammation in stroke and focal cerebral ischemia. Surg Neurol. 2006;66(3):232–245. doi: 10.1016/j.surneu.2005.12.028. [DOI] [PubMed] [Google Scholar]
- 34.Bowes MP, Rothlein R, Fagan SC, Zivin JA. Monoclonal antibodies preventing leukocyte activation reduce experimental neurologic injury and enhance efficacy of thrombolytic therapy. Neurology. 1995;45(4):815–819. doi: 10.1212/wnl.45.4.815. [DOI] [PubMed] [Google Scholar]
- 35.Clark WM, Lauten JD, Lessov N, Woodward W, Coull BM. The influence of antiadhesion therapies on leukocyte subset accumulation in central nervous system ischemia in rats. J Mol Neurosci. 1995;6(1):43–50. doi: 10.1007/BF02736758. [DOI] [PubMed] [Google Scholar]
- 36.Connolly ES, Jr, Winfree CJ, Springer TA, Naka Y, Liao H, Yan SD, Stern DM, Solomon RA, Gutierrez-Ramos JC, Pinsky DJ. Cerebral protection in homozygous null ICAM-1 mice after middle cerebral artery occlusion. Role of neutrophil adhesion in the pathogenesis of stroke. J Clin Invest. 1996;97(1):209–216. doi: 10.1172/JCI118392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Garau A, Bertini R, Colotta F, Casilli F, Bigini P, Cagnotto A, Mennini T, Ghezzi P, Villa P. Neuroprotection with the CXCL8 inhibitor repertaxin in transient brain ischemia. Cytokine. 2005;30(3):125–131. doi: 10.1016/j.cyto.2004.12.014. [DOI] [PubMed] [Google Scholar]
- 38.Yenari MA, Kunis D, Sun GH, Onley D, Watson L, Turner S, Whitaker S, Steinberg GK. Hu23F2G, an antibody recognizing the leukocyte CD11/CD18 integrin, reduces injury in a rabbit model of transient focal cerebral ischemia. Exp Neurol. 1998;153(2):223–233. doi: 10.1006/exnr.1998.6876. [DOI] [PubMed] [Google Scholar]
- 39.Zheng Z, Yenari MA. Post-ischemic inflammation: molecular mechanisms and therapeutic implications. Neurol Res. 2004;26(8):884–892. doi: 10.1179/016164104X2357. [DOI] [PubMed] [Google Scholar]
- 40.Li GZ, Zhong D, Yang LM, Sun B, Zhong ZH, Yin YH, Cheng J, Yan BB, Li HL. Expression of interleukin-17 in ischemic brain tissue. Scand J Immunol. 2005;62(5):481–486. doi: 10.1111/j.1365-3083.2005.01683.x. [DOI] [PubMed] [Google Scholar]
- 41.Stevens SL, Bao J, Hollis J, Lessov NS, Clark WM, Stenzel-Poore MP. The use of flow cytometry to evaluate temporal changes in inflammatory cells following focal cerebral ischemia in mice. Brain Res. 2002;932(1–2):110–119. doi: 10.1016/s0006-8993(02)02292-8. [DOI] [PubMed] [Google Scholar]
- 42.Becker K, Kindrick D, Relton J, Harlan J, Winn R. Antibody to the alpha4 integrin decreases infarct size in transient focal cerebral ischemia in rats. Stroke. 2001;32(1):206–211. doi: 10.1161/01.str.32.1.206. [DOI] [PubMed] [Google Scholar]
- 43.Brait VH, Rivera J, Broughton BR, Lee S, Drummond GR, Sobey CG. Chemokine-related gene expression in the brain following ischemic stroke: no role for CXCR2 in outcome. Brain Res. 2011;1372:169–179. doi: 10.1016/j.brainres.2010.11.087. [DOI] [PubMed] [Google Scholar]
- 44.Kleinschnitz C, Schwab N, Kraft P, Hagedorn I, Dreykluft A, Schwarz T, Austinat M, Nieswandt B, Wiendl H, Stoll G. Early detrimental T-cell effects in experimental cerebral ischemia are neither related to adaptive immunity nor thrombus formation. Blood. 2010;115(18):3835–3842. doi: 10.1182/blood-2009-10-249078. [DOI] [PubMed] [Google Scholar]
- 45.Hurn PD, Subramanian S, Parker SM, Afentoulis ME, Kaler LJ, Vandenbark AA, Offner H. T- and B-cell-deficient mice with experimental stroke have reduced lesion size and inflammation. J Cereb Blood Flow Metab. 2007;27(11):1798–1805. doi: 10.1038/sj.jcbfm.9600482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Shichita T, Sugiyama Y, Ooboshi H, Sugimori H, Nakagawa R, Takada I, Iwaki T, Okada Y, Iida M, Cua DJ, Iwakura Y, Yoshimura A. Pivotal role of cerebral interleukin-17-producing gammadeltaT cells in the delayed phase of ischemic brain injury. Nat Med. 2009;15(8):946–950. doi: 10.1038/nm.1999. [DOI] [PubMed] [Google Scholar]
- 47.Yilmaz G, Arumugam TV, Stokes KY, Granger DN. Role of T lymphocytes and interferon-gamma in ischemic stroke. Circulation. 2006;113(17):2105–2112. doi: 10.1161/CIRCULATIONAHA.105.593046. [DOI] [PubMed] [Google Scholar]
- 48.Saino O, Taguchi A, Nakagomi T, Nakano-Doi A, Kashiwamura S, Doe N, Nakagomi N, Soma T, Yoshikawa H, Stern DM, Okamura H, Matsuyama T. Immunodeficiency reduces neural stem/progenitor cell apoptosis and enhances neurogenesis in the cerebral cortex after stroke. J Neurosci Res. 2010;88(11):2385–2397. doi: 10.1002/jnr.22410. [DOI] [PubMed] [Google Scholar]
- 49.Liesz A, Suri-Payer E, Veltkamp C, Doerr H, Sommer C, Rivest S, Giese T, Veltkamp R. Regulatory T cells are key cere-broprotective immunomodulators in acute experimental stroke. Nat Med. 2009;15(2):192–199. doi: 10.1038/nm.1927. [DOI] [PubMed] [Google Scholar]
- 50.Ren X, Akiyoshi K, Vandenbark AA, Hurn PD, Offner H. CD4+FoxP3+ regulatory T-cells in cerebral ischemic stroke. Metab Brain Dis. 2011;26(1):87–90. doi: 10.1007/s11011-010-9226-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wong CH, Jenne CN, Lee WY, Leger C, Kubes P. Functional innervation of hepatic iNKT cells is immunosuppressive following stroke. Science. 2011;334(6052):101–105. doi: 10.1126/science.1210301. [DOI] [PubMed] [Google Scholar]
- 52.Nadareishvili ZG, Li H, Wright V, Maric D, Warach S, Hallenbeck JM, Dambrosia J, Barker JL, Baird AE. Elevated pro-inflammatory CD4+CD28- lymphocytes and stroke recurrence and death. Neurology. 2004;63(8):1446–1451. doi: 10.1212/01.wnl.0000142260.61443.7c. [DOI] [PubMed] [Google Scholar]
- 53.Dinkel K, Dhabhar FS, Sapolsky RM. Neurotoxic effects of polymorphonuclear granulocytes on hippocampal primary cultures. Proc Natl Acad Sci USA. 2004;101(1):331–336. doi: 10.1073/pnas.0303510101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Harrison DG, Guzik TJ, Goronzy J, Weyand C. Is hypertension an immunologic disease? Curr Cardiol Rep. 2008;10(6):464–469. doi: 10.1007/s11886-008-0073-6. [DOI] [PubMed] [Google Scholar]
- 55.Barry M, Bleackley RC. Cytotoxic T lymphocytes: all roads lead to death. Nat Rev Immunol. 2002;2(6):401–409. doi: 10.1038/nri819. [DOI] [PubMed] [Google Scholar]
- 56.Konoeda F, Shichita T, Yoshida H, Sugiyama Y, Muto G, Hasegawa E, Morita R, Suzuki N, Yoshimura A. Therapeutic effect of IL-12/23 and their signaling pathway blockade on brain ischemia model. Biochem Biophys Res Commun. 2010;402(3):500–506. doi: 10.1016/j.bbrc.2010.10.058. [DOI] [PubMed] [Google Scholar]
- 57.Liesz A, Zhou W, Mracsko E, Karcher S, Bauer H, Schwarting S, Sun L, Bruder D, Stegemann S, Cerwenka A, Sommer C, Dalpke AH, Veltkamp R. Inhibition of lymphocyte trafficking shields the brain against deleterious neuroinflammation after stroke. Brain. 2011;134(Pt 3):704–720. doi: 10.1093/brain/awr008. [DOI] [PubMed] [Google Scholar]
- 58.Brait VH, Jackman KA, Walduck AK, Selemidis S, Diep H, Mast AE, Guida E, Broughton BR, Drummond GR, Sobey CG. Mechanisms contributing to cerebral infarct size after stroke: gender, reperfusion, T lymphocytes, and Nox2-derived superoxide. J Cereb Blood Flow Metab. 2010;30(7):1306–1317. doi: 10.1038/jcbfm.2010.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kreutzberg GW. Microglia: a sensor for pathological events in the CNS. Trends Neurosci. 1996;19(8):312–318. doi: 10.1016/0166-2236(96)10049-7. [DOI] [PubMed] [Google Scholar]
- 60.El Khoury J, Hickman SE, Thomas CA, Loike JD, Silverstein SC. Microglia, scavenger receptors, and the pathogenesis of Alzheimer’s disease. Neurobiol Aging. 1998;19(1 Suppl):S81–84. doi: 10.1016/s0197-4580(98)00036-0. [DOI] [PubMed] [Google Scholar]
- 61.Thomas WE. Brain macrophages: evaluation of microglia and their functions. Brain Res Brain Res Rev. 1992;17(1):61–74. doi: 10.1016/0165-0173(92)90007-9. [DOI] [PubMed] [Google Scholar]
- 62.Lai AY, Todd KG. Microglia in cerebral ischemia: molecular actions and interactions. Can J Physiol Pharmacol. 2006;84(1):49–59. doi: 10.1139/Y05-143. [DOI] [PubMed] [Google Scholar]
- 63.Zhang Z, Chopp M, Powers C. Temporal profile of microglial response following transient (2 h) middle cerebral artery occlusion. Brain Res. 1997;744(2):189–198. doi: 10.1016/S0006-8993(96)01085-2. [DOI] [PubMed] [Google Scholar]
- 64.Schubert P, Morino T, Miyazaki H, Ogata T, Nakamura Y, Marchini C, Ferroni S. Cascading glia reactions: a common pathomechanism and its differentiated control by cyclic nucleotide signaling. Ann N Y Acad Sci. 2000;903:24–33. doi: 10.1111/j.1749-6632.2000.tb06346.x. [DOI] [PubMed] [Google Scholar]
- 65.Saito S, Matsuura M, Tominaga K, Kirikae T, Nakano M. Important role of membrane-associated CD14 in the induction of IFN-beta and subsequent nitric oxide production by murine macrophages in response to bacterial lipopolysaccharide. Eur J Biochem. 2000;267(1):37–45. doi: 10.1046/j.1432-1327.2000.00956.x. [DOI] [PubMed] [Google Scholar]
- 66.Beschorner R, Schluesener HJ, Gozalan F, Meyermann R, Schwab JM. Infiltrating CD14+ monocytes and expression of CD14 by activated parenchymal microglia/macrophages contribute to the pool of CD14+ cells in ischemic brain lesions. J Neuroimmunol. 2002;126(1–2):107–115. doi: 10.1016/s0165-5728(02)00046-2. [DOI] [PubMed] [Google Scholar]
- 67.Lehnardt S, Massillon L, Follett P, Jensen FE, Ratan R, Rosenberg PA, Volpe JJ, Vartanian T. Activation of innate immunity in the CNS triggers neurodegeneration through a Toll-like receptor 4-dependent pathway. Proc Natl Acad Sci USA. 2003;100(14):8514–8519. doi: 10.1073/pnas.1432609100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Zhang RL, Chopp M, Zaloga C, Zhang ZG, Jiang N, Gautam SC, Tang WX, Tsang W, Anderson DC, Manning AM. The temporal profiles of ICAM-1 protein and mRNA expression after transient MCA occlusion in the rat. Brain Res. 1995;682(1–2):182–188. doi: 10.1016/0006-8993(95)00346-r. [DOI] [PubMed] [Google Scholar]
- 69.Stoll G, Jander S, Schroeter M. Inflammation and glial responses in ischemic brain lesions. Prog Neurobiol. 1998;56(2):149–171. doi: 10.1016/s0301-0082(98)00034-3. [DOI] [PubMed] [Google Scholar]
- 70.Dirnagl U, Iadecola C, Moskowitz MA. Pathobiology of ischaemic stroke: an integrated view. Trends Neurosci. 1999;22(9):391–397. doi: 10.1016/s0166-2236(99)01401-0. [DOI] [PubMed] [Google Scholar]
- 71.Clausen BH, Lambertsen KL, Babcock AA, Holm TH, Dagnaes-Hansen F, Finsen B. Interleukin-1beta and tumor necrosis factor-alpha are expressed by different subsets of microglia and macrophages after ischemic stroke in mice. J Neuroinflammation. 2008;5:46. doi: 10.1186/1742-2094-5-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Wood PL. Microglia as a unique cellular target in the treatment of stroke: potential neurotoxic mediators produced by activated microglia. Neurol Res. 1995;17(4):242–248. doi: 10.1080/01616412.1995.11740321. [DOI] [PubMed] [Google Scholar]
- 73.Zhang N, Komine-Kobayashi M, Tanaka R, Liu M, Mizuno Y, Urabe T. Edaravone reduces early accumulation of oxidative products and sequential inflammatory responses after transient focal ischemia in mice brain. Stroke. 2005;36(10):2220–2225. doi: 10.1161/01.STR.0000182241.07096.06. [DOI] [PubMed] [Google Scholar]
- 74.Gunther A, Kuppers-Tiedt L, Schneider PM, Kunert I, Berrouschot J, Schneider D, Rossner S. Reduced infarct volume and differential effects on glial cell activation after hyperbaric oxygen treatment in rat permanent focal cerebral ischaemia. Eur J Neurosci. 2005;21(11):3189–3194. doi: 10.1111/j.1460-9568.2005.04151.x. [DOI] [PubMed] [Google Scholar]
- 75.Yu YM, Kim JB, Lee KW, Kim SY, Han PL, Lee JK. Inhibition of the cerebral ischemic injury by ethyl pyruvate with a wide therapeutic window. Stroke. 2005;36(10):2238–2243. doi: 10.1161/01.STR.0000181779.83472.35. [DOI] [PubMed] [Google Scholar]
- 76.Yrjanheikki J, Keinanen R, Pellikka M, Hokfelt T, Koistinaho J. Tetracyclines inhibit microglial activation and are neuroprotective in global brain ischemia. Proc Natl Acad Sci USA. 1998;95(26):15769–15774. doi: 10.1073/pnas.95.26.15769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Yrjanheikki J, Tikka T, Keinanen R, Goldsteins G, Chan PH, Koistinaho J. A tetracycline derivative, minocycline, reduces inflammation and protects against focal cerebral ischemia with a wide therapeutic window. Proc Natl Acad Sci USA. 1999;96(23):13496–13500. doi: 10.1073/pnas.96.23.13496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Giulian D, Corpuz M, Chapman S, Mansouri M, Robertson C. Reactive mononuclear phagocytes release neurotoxins after ischemic and traumatic injury to the central nervous system. J Neurosci Res. 1993;36(6):681–693. doi: 10.1002/jnr.490360609. [DOI] [PubMed] [Google Scholar]
- 79.Huang WC, Qiao Y, Xu L, Kacimi R, Sun X, Giffard RG, Yenari MA. Direct protection of cultured neurons from ischemia-like injury by minocycline. Anat Cell Biol. 2010;43(4):325–331. doi: 10.5115/acb.2010.43.4.325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Watanabe H, Abe H, Takeuchi S, Tanaka R. Protective effect of microglial conditioning medium on neuronal damage induced by glutamate. Neurosci Lett. 2000;289(1):53–56. doi: 10.1016/s0304-3940(00)01252-0. [DOI] [PubMed] [Google Scholar]
- 81.Lalancette-Hebert M, Gowing G, Simard A, Weng YC, Kriz J. Selective ablation of proliferating microglial cells exacerbates ischemic injury in the brain. J Neurosci. 2007;27(10):2596–2605. doi: 10.1523/JNEUROSCI.5360-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Weston RM, Jones NM, Jarrott B, Callaway JK. Inflammatory cell infiltration after endothelin-1-induced cerebral ischemia: histochemical and myeloperoxidase correlation with temporal changes in brain injury. J Cereb Blood Flow Metab. 2007;27(1):100–114. doi: 10.1038/sj.jcbfm.9600324. [DOI] [PubMed] [Google Scholar]
- 83.Frank-Cannon TC, Alto LT, McAlpine FE, Tansey MG. Does neuroinflammation fan the flame in neurodegenerative diseases? Mol Neurodegener. 2009;4:47. doi: 10.1186/1750-1326-4-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Benveniste EN. Cytokine actions in the central nervous system. Cytokine Growth Factor Rev. 1998;9(3–4):259–275. doi: 10.1016/s1359-6101(98)00015-x. [DOI] [PubMed] [Google Scholar]
- 85.Che X, Ye W, Panga L, Wu DC, Yang GY. Monocyte chemoattractant protein-1 expressed in neurons and astrocytes during focal ischemia in mice. Brain Res. 2001;902(2):171–177. doi: 10.1016/s0006-8993(01)02328-9. [DOI] [PubMed] [Google Scholar]
- 86.Pekny M, Nilsson M. Astrocyte activation and reactive gliosis. Glia. 2005;50(4):427–434. doi: 10.1002/glia.20207. [DOI] [PubMed] [Google Scholar]
- 87.Kadhim HJ, Duchateau J, Sebire G. Cytokines and brain injury: invited review. J Intensive Care Med. 2008;23(4):236–249. doi: 10.1177/0885066608318458. [DOI] [PubMed] [Google Scholar]
- 88.Nowicka D, Rogozinska K, Aleksy M, Witte OW, Skangiel-Kramska J. Spatiotemporal dynamics of astroglial and microglial responses after photothrombotic stroke in the rat brain. Acta Neurobiol Exp (Wars) 2008;68(2):155–168. doi: 10.55782/ane-2008-1685. [DOI] [PubMed] [Google Scholar]
- 89.Zhu Y, Roth-Eichhorn S, Braun N, Culmsee C, Rami A, Krieglstein J. The expression of transforming growth factor-beta1 (TGF-beta1) in hippocampal neurons: a temporary upregulated protein level after transient forebrain ischemia in the rat. Brain Res. 2000;866(1–2):286–298. doi: 10.1016/s0006-8993(00)02240-x. [DOI] [PubMed] [Google Scholar]
- 90.Dong Y, Benveniste EN. Immune function of astrocytes. Glia. 2001;36(2):180–190. doi: 10.1002/glia.1107. [DOI] [PubMed] [Google Scholar]
- 91.Endoh M, Maiese K, Wagner J. Expression of the inducible form of nitric oxide synthase by reactive astrocytes after transient global ischemia. Brain Res. 1994;651(1–2):92–100. doi: 10.1016/0006-8993(94)90683-1. [DOI] [PubMed] [Google Scholar]
- 92.Hewett SJ, Muir JK, Lobner D, Symons A, Choi DW. Potentiation of oxygen-glucose deprivation-induced neuronal death after induction of iNOS. Stroke. 1996;27(9):1586–1591. doi: 10.1161/01.str.27.9.1586. [DOI] [PubMed] [Google Scholar]
- 93.Donohue PJ, Richards CM, Brown SA, Hanscom HN, Buschman J, Thangada S, Hla T, Williams MS, Winkles JA. TWEAK is an endothelial cell growth and chemotactic factor that also potentiates FGF-2 and VEGF-A mitogenic activity. Arterioscler Thromb Vasc Biol. 2003;23(4):594–600. doi: 10.1161/01.ATV.0000062883.93715.37. [DOI] [PubMed] [Google Scholar]
- 94.Yepes M, Brown SA, Moore EG, Smith EP, Lawrence DA, Winkles JA. A soluble Fn14-Fc decoy receptor reduces infarct volume in a murine model of cerebral ischemia. Am J Pathol. 2005;166(2):511–520. doi: 10.1016/S0002-9440(10)62273-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Saas P, Boucraut J, Walker PR, Quiquerez AL, Billot M, Desplat-Jego S, Chicheportiche Y, Dietrich PY. TWEAK stimulation of astrocytes and the proinflammatory consequences. Glia. 2000;32(1):102–107. [PubMed] [Google Scholar]
- 96.Sughrue ME, Mehra A, Connolly ES, Jr, D’Ambrosio AL. Anti-adhesion molecule strategies as potential neuroprotective agents in cerebral ischemia: a critical review of the literature. Inflamm Res. 2004;53(10):497–508. doi: 10.1007/s00011-004-1282-0. [DOI] [PubMed] [Google Scholar]
- 97.Guha M, Mackman N. LPS induction of gene expression in human monocytes. Cell Signal. 2001;13(2):85–94. doi: 10.1016/s0898-6568(00)00149-2. [DOI] [PubMed] [Google Scholar]
- 98.DeGraba TJ. The role of inflammation after acute stroke: utility of pursuing anti-adhesion molecule therapy. Neurology. 1998;51(3 Suppl 3):S62–68. doi: 10.1212/wnl.51.3_suppl_3.s62. [DOI] [PubMed] [Google Scholar]
- 99.Emsley HC, Tyrrell PJ. Inflammation and infection in clinical stroke. J Cereb Blood Flow Metab. 2002;22(12):1399–1419. doi: 10.1097/01.WCB.0000037880.62590.28. [DOI] [PubMed] [Google Scholar]
- 100.Clark WM, Lessov N, Lauten JD, Hazel K. Doxycycline treatment reduces ischemic brain damage in transient middle cerebral artery occlusion in the rat. J Mol Neurosci. 1997;9(2):103–108. doi: 10.1007/BF02736854. [DOI] [PubMed] [Google Scholar]
- 101.Connolly ES, Jr, Winfree CJ, Prestigiacomo CJ, Kim SC, Choudhri TF, Hoh BL, Naka Y, Solomon RA, Pinsky DJ. Exacerbation of cerebral injury in mice that express the P-selectin gene: identification of P-selectin blockade as a new target for the treatment of stroke. Circ Res. 1997;81(3):304–310. doi: 10.1161/01.res.81.3.304. [DOI] [PubMed] [Google Scholar]
- 102.Kitagawa K, Matsumoto M, Mabuchi T, Yagita Y, Ohtsuki T, Hori M, Yanagihara T. Deficiency of intercellular adhesion molecule 1 attenuates microcirculatory disturbance and infarction size in focal cerebral ischemia. J Cereb Blood Flow Metab. 1998;18(12):1336–1345. doi: 10.1097/00004647-199812000-00008. [DOI] [PubMed] [Google Scholar]
- 103.Soriano SG, Coxon A, Wang YF, Frosch MP, Lipton SA, Hickey PR, Mayadas TN. Mice deficient in Mac-1 (CD11b/CD18) are less susceptible to cerebral ischemia/reperfusion injury. Stroke. 1999;30(1):134–139. doi: 10.1161/01.str.30.1.134. [DOI] [PubMed] [Google Scholar]
- 104.Haring HP, Berg EL, Tsurushita N, Tagaya M, del Zoppo GJ. E-selectin appears in nonischemic tissue during experimental focal cerebral ischemia. Stroke. 1996;27(8):1386–1391. doi: 10.1161/01.str.27.8.1386. discussion 1391–1382. [DOI] [PubMed] [Google Scholar]
- 105.Suzuki H, Abe K, Tojo S, Kimura K, Mizugaki M, Itoyama Y. A change of P-selectin immunoreactivity in rat brain after transient and permanent middle cerebral artery occlusion. Neurol Res. 1998;20(5):463–469. doi: 10.1080/01616412.1998.11740549. [DOI] [PubMed] [Google Scholar]
- 106.Zhang RL, Chopp M, Zhang ZG, Phillips ML, Rosenbloom CL, Cruz R, Manning A. E-selectin in focal cerebral ischemia and reperfusion in the rat. J Cereb Blood Flow Metab. 1996;16(6):1126–1136. doi: 10.1097/00004647-199611000-00006. [DOI] [PubMed] [Google Scholar]
- 107.Prestigiacomo CJ, Kim SC, Connolly ES, Jr, Liao H, Yan SF, Pinsky DJ. CD18-mediated neutrophil recruitment contributes to the pathogenesis of reperfused but not nonreperfused stroke. Stroke. 1999;30(5):1110–1117. doi: 10.1161/01.str.30.5.1110. [DOI] [PubMed] [Google Scholar]
- 108.Zhang RL, Chopp M, Jiang N, Tang WX, Prostak J, Manning AM, Anderson DC. Anti-intercellular adhesion molecule-1 antibody reduces ischemic cell damage after transient but not permanent middle cerebral artery occlusion in the Wistar rat. Stroke. 1995;26(8):1438–1442. doi: 10.1161/01.str.26.8.1438. discussion 1443. [DOI] [PubMed] [Google Scholar]
- 109.Carlos TM, Harlan JM. Leukocyte-endothelial adhesion molecules. Blood. 1994;84(7):2068–2101. [PubMed] [Google Scholar]
- 110.Barkalow FJ, Goodman MJ, Gerritsen ME, Mayadas TN. Brain endothelium lack one of two pathways of P-selectin-mediated neutrophil adhesion. Blood. 1996;88(12):4585–4593. [PubMed] [Google Scholar]
- 111.Zhang R, Chopp M, Zhang Z, Jiang N, Powers C. The expression of P- and E-selectins in three models of middle cerebral artery occlusion. Brain Res. 1998;785(2):207–214. doi: 10.1016/s0006-8993(97)01343-7. [DOI] [PubMed] [Google Scholar]
- 112.Bargatze RF, Kurk S, Butcher EC, Jutila MA. Neutrophils roll on adherent neutrophils bound to cytokine-induced endothelial cells via L-selectin on the rolling cells. J Exp Med. 1994;180(5):1785–1792. doi: 10.1084/jem.180.5.1785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Huang J, Choudhri TF, Winfree CJ, McTaggart RA, Kiss S, Mocco J, Kim LJ, Protopsaltis TS, Zhang Y, Pinsky DJ, Connolly ES., Jr Postischemic cerebrovascular E-selectin expression mediates tissue injury in murine stroke. Stroke. 2000;31(12):3047–3053. [PubMed] [Google Scholar]
- 114.Huang J, Kim LJ, Mealey R, Marsh HC, Jr, Zhang Y, Tenner AJ, Connolly ES, Jr, Pinsky DJ. Neuronal protection in stroke by an sLex-glycosylated complement inhibitory protein. Science. 1999;285(5427):595–599. doi: 10.1126/science.285.5427.595. [DOI] [PubMed] [Google Scholar]
- 115.Khan M, Jatana M, Elango C, Paintlia AS, Singh AK, Singh I. Cerebrovascular protection by various nitric oxide donors in rats after experimental stroke. Nitric Oxide. 2006;15(2):114–124. doi: 10.1016/j.niox.2006.01.008. [DOI] [PubMed] [Google Scholar]
- 116.Goussev AV, Zhang Z, Anderson DC, Chopp M. P-selectin antibody reduces hemorrhage and infarct volume resulting from MCA occlusion in the rat. J Neurol Sci. 1998;161(1):16–22. doi: 10.1016/s0022-510x(98)00262-7. [DOI] [PubMed] [Google Scholar]
- 117.Mocco J, Choudhri T, Huang J, Harfeldt E, Efros L, Klingbeil C, Vexler V, Hall W, Zhang Y, Mack W, Popilskis S, Pinsky DJ, Connolly ES., Jr HuEP5C7 as a humanized monoclonal anti-E/P-selectin neurovascular protective strategy in a blinded placebo-controlled trial of nonhuman primate stroke. Circ Res. 2002;91(10):907–914. doi: 10.1161/01.res.0000042063.15901.20. [DOI] [PubMed] [Google Scholar]
- 118.Lehmberg J, Beck J, Baethmann A, Uhl E. Effect of P-selectin inhibition on leukocyte-endothelium interaction and survival after global cerebral ischemia. J Neurol. 2006;253(3):357–363. doi: 10.1007/s00415-005-0996-4. [DOI] [PubMed] [Google Scholar]
- 119.Yenari MA, Sun GH, Kunis DM, Onley D, Vexler V. L-selectin inhibition does not reduce injury in a rabbit model of transient focal cerebral ischemia. Neurol Res. 2001;23(1):72–78. doi: 10.1179/016164101101198154. [DOI] [PubMed] [Google Scholar]
- 120.Chen Y, Ruetzler C, Pandipati S, Spatz M, McCarron RM, Becker K, Hallenbeck JM. Mucosal tolerance to E-selectin provides cell-mediated protection against ischemic brain injury. Proc Natl Acad Sci USA. 2003;100(25):15107–15112. doi: 10.1073/pnas.2436538100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Takeda H, Spatz M, Ruetzler C, McCarron R, Becker K, Hallenbeck J. Induction of mucosal tolerance to E-selectin prevents ischemic and hemorrhagic stroke in spontaneously hypertensive genetically stroke-prone rats. Stroke. 2002;33(9):2156–2163. doi: 10.1161/01.str.0000029821.82531.8b. [DOI] [PubMed] [Google Scholar]
- 122.Kalinowska A, Losy J. PECAM-1, a key player in neuroinflammation. Eur J Neurol. 2006;13(12):1284–1290. doi: 10.1111/j.1468-1331.2006.01640.x. [DOI] [PubMed] [Google Scholar]
- 123.Yoshimoto T, Houkin K, Tada M, Abe H. Induction of cytokines, chemokines and adhesion molecule mRNA in a rat forebrain reperfusion model. Acta Neuropathol. 1997;93(2):154–158. doi: 10.1007/s004010050596. [DOI] [PubMed] [Google Scholar]
- 124.Bowes MP, Zivin JA, Rothlein R. Monoclonal antibody to the ICAM-1 adhesion site reduces neurological damage in a rabbit cerebral embolism stroke model. Exp Neurol. 1993;119(2):215–219. doi: 10.1006/exnr.1993.1023. [DOI] [PubMed] [Google Scholar]
- 125.Kanemoto Y, Nakase H, Akita N, Sakaki T. Effects of anti-intercellular adhesion molecule-1 antibody on reperfusion injury induced by late reperfusion in the rat middle cerebral artery occlusion model. Neurosurgery. 2002;51(4):1034–1041. doi: 10.1097/00006123-200210000-00033. discussion 1041–1032. [DOI] [PubMed] [Google Scholar]
- 126.Vemuganti R, Dempsey RJ, Bowen KK. Inhibition of intercellular adhesion molecule-1 protein expression by antisense oligonucleotides is neuroprotective after transient middle cerebral artery occlusion in rat. Stroke. 2004;35(1):179–184. doi: 10.1161/01.STR.0000106479.53235.3E. [DOI] [PubMed] [Google Scholar]
- 127.Ding C, He Q, Li PA. Diabetes increases expression of ICAM after a brief period of cerebral ischemia. J Neuroimmunol. 2005;161(1–2):61–67. doi: 10.1016/j.jneuroim.2004.12.011. [DOI] [PubMed] [Google Scholar]
- 128.Blann A, Kumar P, Krupinski J, McCollum C, Beevers DG, Lip GY. Soluble intercelluar adhesion molecule-1, E-selectin, vascular cell adhesion molecule-1 and von Willebrand factor in stroke. Blood Coagul Fibrinolysis. 1999;10(5):277–284. doi: 10.1097/00001721-199907000-00009. [DOI] [PubMed] [Google Scholar]
- 129.Justicia C, Martin A, Rojas S, Gironella M, Cervera A, Panes J, Chamorro A, Planas AM. Anti-VCAM-1 antibodies did not protect against ischemic damage either in rats or in mice. J Cereb Blood Flow Metab. 2006;26(3):421–432. doi: 10.1038/sj.jcbfm.9600198. [DOI] [PubMed] [Google Scholar]
- 130.Zhang LH, Wei EQ. Neuroprotective effect of ONO-1078, a leukotriene receptor antagonist, on transient global cerebral ischemia in rats. Acta Pharmacol Sin. 2003;24(12):1241–1247. [PubMed] [Google Scholar]
- 131.Cervera A, Justicia C, Reverter JC, Planas AM, Chamorro A. Steady plasma concentration of unfractionated heparin reduces infarct volume and prevents inflammatory damage after transient focal cerebral ischemia in the rat. J Neurosci Res. 2004;77(4):565–572. doi: 10.1002/jnr.20186. [DOI] [PubMed] [Google Scholar]
- 132.Smith CW. Leukocyte-endothelial cell interactions. Semin Hema-ol. 1993;30(4 Suppl 4):45–53. discussion 54–45. [PubMed] [Google Scholar]
- 133.Sharar SR, Winn RK, Harlan JM. The adhesion cascade and anti-adhesion therapy: an overview. Springer Semin Immunopathol. 1995;16(4):359–378. doi: 10.1007/BF00196093. [DOI] [PubMed] [Google Scholar]
- 134.Harmon D, Lan W, Shorten G. The effect of aprotinin on hypoxia-reoxygenation-induced changes in neutrophil and endothelial function. Eur J Anaesthesiol. 2004;21(12):973–979. doi: 10.1017/s0265021504000365. [DOI] [PubMed] [Google Scholar]
- 135.Koh SH, Park Y, Song CW, Kim JG, Kim K, Kim J, Kim MH, Lee SR, Kim DW, Yu HJ, Chang DI, Hwang SJ, Kim SH. The effect of PARP inhibitor on ischaemic cell death, its related inflammation and survival signals. Eur J Neurosci. 2004;20(6):1461–1472. doi: 10.1111/j.1460-9568.2004.03632.x. [DOI] [PubMed] [Google Scholar]
- 136.Jiang N, Moyle M, Soule HR, Rote WE, Chopp M. Neutrophil inhibitory factor is neuroprotective after focal ischemia in rats. Ann Neurol. 1995;38(6):935–942. doi: 10.1002/ana.410380615. [DOI] [PubMed] [Google Scholar]
- 137.Relton JK, Sloan KE, Frew EM, Whalley ET, Adams SP, Lobb RR. Inhibition of alpha4 integrin protects against transient focal cerebral ischemia in normotensive and hypertensive rats. Stroke. 2001;32(1):199–205. doi: 10.1161/01.str.32.1.199. [DOI] [PubMed] [Google Scholar]
- 138.Liu T, Clark RK, McDonnell PC, Young PR, White RF, Barone FC, Feuerstein GZ. Tumor necrosis factor-alpha expression in ischemic neurons. Stroke. 1994;25(7):1481–1488. doi: 10.1161/01.str.25.7.1481. [DOI] [PubMed] [Google Scholar]
- 139.Sairanen T, Carpen O, Karjalainen-Lindsberg ML, Paetau A, Turpeinen U, Kaste M, Lindsberg PJ. Evolution of cerebral tumor necrosis factor-alpha production during human ischemic stroke. Stroke. 2001;32(8):1750–1758. doi: 10.1161/01.str.32.8.1750. [DOI] [PubMed] [Google Scholar]
- 140.Allan SM, Rothwell NJ. Cytokines and acute neurodegeneration. Nat Rev Neurosci. 2001;2(10):734–744. doi: 10.1038/35094583. [DOI] [PubMed] [Google Scholar]
- 141.Pinteaux E, Rothwell NJ, Boutin H. Neuroprotective actions of endogenous interleukin-1 receptor antagonist (IL-1ra) are mediated by glia. Glia. 2006;53(5):551–556. doi: 10.1002/glia.20308. [DOI] [PubMed] [Google Scholar]
- 142.Boutin H, LeFeuvre RA, Horai R, Asano M, Iwakura Y, Rothwell NJ. Role of IL-1alpha and IL-1beta in ischemic brain damage. J Neurosci. 2001;21(15):5528–5534. doi: 10.1523/JNEUROSCI.21-15-05528.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Buttini M, Sauter A, Boddeke HW. Induction of interleukin-1 beta mRNA after focal cerebral ischaemia in the rat. Brain Res Mol Brain Res. 1994;23(1–2):126–134. doi: 10.1016/0169-328x(94)90218-6. [DOI] [PubMed] [Google Scholar]
- 144.Davies CA, Loddick SA, Toulmond S, Stroemer RP, Hunt J, Rothwell NJ. The progression and topographic distribution of interleukin-1beta expression after permanent middle cerebral artery occlusion in the rat. J Cereb Blood Flow Metab. 1999;19(1):87–98. doi: 10.1097/00004647-199901000-00010. [DOI] [PubMed] [Google Scholar]
- 145.Haqqani AS, Nesic M, Preston E, Baumann E, Kelly J, Stanimirovic D. Characterization of vascular protein expression patterns in cerebral ischemia/reperfusion using laser capture micro-dissection and ICAT-nanoLC-MS/MS. FASEB J. 2005;19(13):1809–1821. doi: 10.1096/fj.05-3793com. [DOI] [PubMed] [Google Scholar]
- 146.Yamasaki Y, Matsuura N, Shozuhara H, Onodera H, Itoyama Y, Kogure K. Interleukin-1 as a pathogenetic mediator of ischemic brain damage in rats. Stroke. 1995;26(4):676–680. doi: 10.1161/01.str.26.4.676. discussion 681. [DOI] [PubMed] [Google Scholar]
- 147.Hara H, Friedlander RM, Gagliardini V, Ayata C, Fink K, Huang Z, Shimizu-Sasamata M, Yuan J, Moskowitz MA. Inhibition of interleukin 1beta converting enzyme family proteases reduces ischemic and excitotoxic neuronal damage. Proc Natl Acad Sci USA. 1997;94(5):2007–2012. doi: 10.1073/pnas.94.5.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Rothwell NJ, Luheshi GN. Interleukin 1 in the brain: biology, pathology and therapeutic target. Trends Neurosci. 2000;23(12):618–625. doi: 10.1016/s0166-2236(00)01661-1. [DOI] [PubMed] [Google Scholar]
- 149.Basu A, Lazovic J, Krady JK, Mauger DT, Rothstein RP, Smith MB, Levison SW. Interleukin-1 and the interleukin-1 type 1 receptor are essential for the progressive neurodegeneration that ensues subsequent to a mild hypoxic/ischemic injury. J Cereb Blood Flow Metab. 2005;25(1):17–29. doi: 10.1038/sj.jcbfm.9600002. [DOI] [PubMed] [Google Scholar]
- 150.Mulcahy NJ, Ross J, Rothwell NJ, Loddick SA. Delayed administration of interleukin-1 receptor antagonist protects against transient cerebral ischaemia in the rat. Br J Pharmacol. 2003;140(3):471–476. doi: 10.1038/sj.bjp.0705462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Yang GY, Zhao YJ, Davidson BL, Betz AL. Overexpression of interleukin-1 receptor antagonist in the mouse brain reduces ischemic brain injury. Brain Res. 1997;751(2):181–188. doi: 10.1016/s0006-8993(96)01277-2. [DOI] [PubMed] [Google Scholar]
- 152.Murakami Y, Saito K, Hara A, Zhu Y, Sudo K, Niwa M, Fujii H, Wada H, Ishiguro H, Mori H, Seishima M. Increases in tumor necrosis factor-alpha following transient global cerebral ischemia do not contribute to neuron death in mouse hippocampus. J Neurochem. 2005;93(6):1616–1622. doi: 10.1111/j.1471-4159.2005.03163.x. [DOI] [PubMed] [Google Scholar]
- 153.Offner H, Subramanian S, Parker SM, Afentoulis ME, Vandenbark AA, Hurn PD. Experimental stroke induces massive, rapid activation of the peripheral immune system. J Cereb Blood Flow Metab. 2006;26(5):654–665. doi: 10.1038/sj.jcbfm.9600217. [DOI] [PubMed] [Google Scholar]
- 154.Uno H, Matsuyama T, Akita H, Nishimura H, Sugita M. Induction of tumor necrosis factor-alpha in the mouse hippocampus following transient forebrain ischemia. J Cereb Blood Flow Metab. 1997;17(5):491–499. doi: 10.1097/00004647-199705000-00002. [DOI] [PubMed] [Google Scholar]
- 155.Hallenbeck JM. The many faces of tumor necrosis factor in stroke. Nat Med. 2002;8(12):1363–1368. doi: 10.1038/nm1202-1363. [DOI] [PubMed] [Google Scholar]
- 156.Pan W, Kastin AJ. Tumor necrosis factor and stroke: role of the blood-brain barrier. Prog Neurobiol. 2007;83(6):363–374. doi: 10.1016/j.pneurobio.2007.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Yang GY, Gong C, Qin Z, Ye W, Mao Y, Bertz AL. Inhibition of TNFalpha attenuates infarct volume and ICAM-1 expression in ischemic mouse brain. Neuroreport. 1998;9(9):2131–2134. doi: 10.1097/00001756-199806220-00041. [DOI] [PubMed] [Google Scholar]
- 158.Barone FC, Arvin B, White RF, Miller A, Webb CL, Willette RN, Lysko PG, Feuerstein GZ. Tumor necrosis factor-alpha. A mediator of focal ischemic brain injury. Stroke. 1997;28(6):1233–1244. doi: 10.1161/01.str.28.6.1233. [DOI] [PubMed] [Google Scholar]
- 159.Ginis I, Jaiswal R, Klimanis D, Liu J, Greenspon J, Hallenbeck JM. TNF-alpha-induced tolerance to ischemic injury involves differential control of NF-kappaB transactivation: the role of NF-kappaB association with p300 adaptor. J Cereb Blood Flow Metab. 2002;22(2):142–152. doi: 10.1097/00004647-200202000-00002. [DOI] [PubMed] [Google Scholar]
- 160.Bruce AJ, Boling W, Kindy MS, Peschon J, Kraemer PJ, Carpenter MK, Holtsberg FW, Mattson MP. Altered neuronal and microglial responses to excitotoxic and ischemic brain injury in mice lacking TNF receptors. Nat Med. 1996;2(7):788–794. doi: 10.1038/nm0796-788. [DOI] [PubMed] [Google Scholar]
- 161.Sriram K, O’Callaghan JP. Divergent roles for tumor necrosis factor-alpha in the brain. J Neuroimmune Pharmacol. 2007;2(2):140–153. doi: 10.1007/s11481-007-9070-6. [DOI] [PubMed] [Google Scholar]
- 162.Amantea D, Nappi G, Bernardi G, Bagetta G, Corasaniti MT. Post-ischemic brain damage: pathophysiology and role of inflammatory mediators. FEBS J. 2009;276(1):13–26. doi: 10.1111/j.1742-4658.2008.06766.x. [DOI] [PubMed] [Google Scholar]
- 163.McCoy MK, Tansey MG. TNF signaling inhibition in the CNS: implications for normal brain function and neurodegenerative disease. J Neuroinflammation. 2008;5:45. doi: 10.1186/1742-2094-5-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Pradillo JM, Romera C, Hurtado O, Cardenas A, Moro MA, Leza JC, Davalos A, Castillo J, Lorenzo P, Lizasoain I. TNFR1 upregulation mediates tolerance after brain ischemic preconditioning. J Cereb Blood Flow Metab. 2005;25(2):193–203. doi: 10.1038/sj.jcbfm.9600019. [DOI] [PubMed] [Google Scholar]
- 165.Clark WM, Rinker LG, Lessov NS, Hazel K, Hill JK, Stenzel-Poore M, Eckenstein F. Lack of interleukin-6 expression is not protective against focal central nervous system ischemia. Stroke. 2000;31(7):1715–1720. doi: 10.1161/01.str.31.7.1715. [DOI] [PubMed] [Google Scholar]
- 166.Yamashita T, Sawamoto K, Suzuki S, Suzuki N, Adachi K, Kawase T, Mihara M, Ohsugi Y, Abe K, Okano H. Blockade of interleukin-6 signaling aggravates ischemic cerebral damage in mice: possible involvement of Stat3 activation in the protection of neurons. J Neurochem. 2005;94(2):459–468. doi: 10.1111/j.1471-4159.2005.03227.x. [DOI] [PubMed] [Google Scholar]
- 167.Herrmann O, Tarabin V, Suzuki S, Attigah N, Coserea I, Schneider A, Vogel J, Prinz S, Schwab S, Monyer H, Brombacher F, Schwaninger M. Regulation of body temperature and neuroprotection by endogenous interleukin-6 in cerebral ischemia. J Cereb Blood Flow Metab. 2003;23(4):406–415. doi: 10.1097/01.WCB.0000055177.50448.FA. [DOI] [PubMed] [Google Scholar]
- 168.Smith CJ, Emsley HC, Gavin CM, Georgiou RF, Vail A, Barberan EM, del Zoppo GJ, Hallenbeck JM, Rothwell NJ, Hopkins SJ, Tyrrell PJ. Peak plasma interleukin-6 and other peripheral markers of inflammation in the first week of ischaemic stroke correlate with brain infarct volume, stroke severity and long-term outcome. BMC Neurol. 2004;4:2. doi: 10.1186/1471-2377-4-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Rallidis LS, Vikelis M, Panagiotakos DB, Rizos I, Zolindaki MG, Kaliva K, Kremastinos DT. Inflammatory markers and inhospital mortality in acute ischaemic stroke. Atherosclerosis. 2006;189(1):193–197. doi: 10.1016/j.atherosclerosis.2005.11.032. [DOI] [PubMed] [Google Scholar]
- 170.Jung JE, Kim GS, Chan PH. Neuroprotection by interleukin-6 is mediated by signal transducer and activator of transcription 3 and antioxidative signaling in ischemic stroke. Stroke. 2011;42(12):3574–3579. doi: 10.1161/STROKEAHA.111.626648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Gertz K, Kronenberg G, Kalin RE, Baldinger T, Werner C, Balkaya M, Eom GD, Hellmann-Regen J, Krober J, Miller KR, Lindauer U, Laufs U, Dirnagl U, Heppner FL, Endres M. Essential role of interleukin-6 in post-stroke angiogenesis. Brain. 2012;135(Pt 6):1964–1980. doi: 10.1093/brain/aws075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Strle K, Zhou JH, Shen WH, Broussard SR, Johnson RW, Freund GG, Dantzer R, Kelley KW. Interleukin-10 in the brain. Crit Rev Immunol. 2001;21(5):427–449. [PubMed] [Google Scholar]
- 173.Spera PA, Ellison JA, Feuerstein GZ, Barone FC. IL-10 reduces rat brain injury following focal stroke. Neurosci Lett. 1998;251(3):189–192. doi: 10.1016/s0304-3940(98)00537-0. [DOI] [PubMed] [Google Scholar]
- 174.Ooboshi H, Ibayashi S, Shichita T, Kumai Y, Takada J, Ago T, Arakawa S, Sugimori H, Kamouchi M, Kitazono T, Iida M. Postischemic gene transfer of interleukin-10 protects against both focal and global brain ischemia. Circulation. 2005;111(7):913–919. doi: 10.1161/01.CIR.0000155622.68580.DC. [DOI] [PubMed] [Google Scholar]
- 175.Pelidou SH, Kostulas N, Matusevicius D, Kivisakk P, Kostulas V, Link H. High levels of IL-10 secreting cells are present in blood in cerebrovascular diseases. Eur J Neurol. 1999;6(4):437–442. doi: 10.1046/j.1468-1331.1999.640437.x. [DOI] [PubMed] [Google Scholar]
- 176.Tarkowski E, Rosengren L, Blomstrand C, Wikkelso C, Jensen C, Ekholm S, Tarkowski A. Intrathecal release of pro- and anti-inflammatory cytokines during stroke. Clin Exp Immunol. 1997;110(3):492–499. doi: 10.1046/j.1365-2249.1997.4621483.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.van Exel E, Gussekloo J, de Craen AJ, Bootsma-van der Wiel A, Frolich M, Westendorp RG. Inflammation and stroke: the Leiden 85-Plus Study. Stroke. 2002;33(4):1135–1138. doi: 10.1161/01.str.0000014206.05597.9e. [DOI] [PubMed] [Google Scholar]
- 178.Flanders KC, Ren RF, Lippa CF. Transforming growth factor-betas in neurodegenerative disease. Prog Neurobiol. 1998;54(1):71–85. doi: 10.1016/s0301-0082(97)00066-x. [DOI] [PubMed] [Google Scholar]
- 179.Pang L, Ye W, Che XM, Roessler BJ, Betz AL, Yang GY. Reduction of inflammatory response in the mouse brain with adenoviral-mediated transforming growth factor-ss1 expression. Stroke. 2001;32(2):544–552. doi: 10.1161/01.str.32.2.544. [DOI] [PubMed] [Google Scholar]
- 180.Lu YZ, Lin CH, Cheng FC, Hsueh CM. Molecular mechanisms responsible for microglia-derived protection of Sprague-Dawley rat brain cells during in vitro ischemia. Neurosci Lett. 2005;373(2):159–164. doi: 10.1016/j.neulet.2004.10.004. [DOI] [PubMed] [Google Scholar]
- 181.Kim JS, Gautam SC, Chopp M, Zaloga C, Jones ML, Ward PA, Welch KM. Expression of monocyte chemoattractant protein-1 and macrophage inflammatory protein-1 after focal cerebral ischemia in the rat. J Neuroimmunol. 1995;56(2):127–134. doi: 10.1016/0165-5728(94)00138-e. [DOI] [PubMed] [Google Scholar]
- 182.Wang X, Yue TL, Barone FC, Feuerstein GZ. Monocyte chemoattractant protein-1 messenger RNA expression in rat ischemic cortex. Stroke. 1995;26(4):661–665. doi: 10.1161/01.str.26.4.661. discussion 665–666. [DOI] [PubMed] [Google Scholar]
- 183.Gerard C, Rollins BJ. Chemokines and disease. Nat Immunol. 2001;2(2):108–115. doi: 10.1038/84209. [DOI] [PubMed] [Google Scholar]
- 184.Bajetto A, Bonavia R, Barbero S, Florio T, Schettini G. Chemokines and their receptors in the central nervous system. Front Neuroendocrinol. 2001;22(3):147–184. doi: 10.1006/frne.2001.0214. [DOI] [PubMed] [Google Scholar]
- 185.Rossi D, Zlotnik A. The biology of chemokines and their receptors. Annu Rev Immunol. 2000;18:217–242. doi: 10.1146/annurev.immunol.18.1.217. [DOI] [PubMed] [Google Scholar]
- 186.Bizzarri C, Beccari AR, Bertini R, Cavicchia MR, Giorgini S, Allegretti M. ELR+ CXC chemokines and their receptors (CXC chemokine receptor 1 and CXC chemokine receptor 2) as new therapeutic targets. Pharmacol Ther. 2006;112(1):139–149. doi: 10.1016/j.pharmthera.2006.04.002. [DOI] [PubMed] [Google Scholar]
- 187.Rollins BJ. Chemokines. Blood. 1997;90(3):909–928. [PubMed] [Google Scholar]
- 188.Semple BD, Kossmann T, Morganti-Kossmann MC. Role of chemokines in CNS health and pathology: a focus on the CCL2/CCR2 and CXCL8/CXCR2 networks. J Cereb Blood Flow Metab. 2010;30(3):459–473. doi: 10.1038/jcbfm.2009.240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Chen Y, Hallenbeck JM, Ruetzler C, Bol D, Thomas K, Berman NE, Vogel SN. Overexpression of monocyte chemoat-tractant protein 1 in the brain exacerbates ischemic brain injury and is associated with recruitment of inflammatory cells. J Cereb Blood Flow Metab. 2003;23(6):748–755. doi: 10.1097/01.WCB.0000071885.63724.20. [DOI] [PubMed] [Google Scholar]
- 190.Terao S, Yilmaz G, Stokes KY, Russell J, Ishikawa M, Kawase T, Granger DN. Blood cell-derived RANTES mediates cerebral microvascular dysfunction, inflammation, and tissue injury after focal ischemia-reperfusion. Stroke. 2008;39(9):2560–2570. doi: 10.1161/STROKEAHA.107.513150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Terao Y, Ohta H, Oda A, Nakagaito Y, Kiyota Y, Shintani Y. Macrophage inflammatory protein-3alpha plays a key role in the inflammatory cascade in rat focal cerebral ischemia. Neurosci Res. 2009;64(1):75–82. doi: 10.1016/j.neures.2009.01.017. [DOI] [PubMed] [Google Scholar]
- 192.Tarozzo G, Campanella M, Ghiani M, Bulfone A, Beltramo M. Expression of fractalkine and its receptor, CX3CR1, in response to ischaemia-reperfusion brain injury in the rat. Eur J Neurosci. 2002;15(10):1663–1668. doi: 10.1046/j.1460-9568.2002.02007.x. [DOI] [PubMed] [Google Scholar]
- 193.Soriano SG, Amaravadi LS, Wang YF, Zhou H, Yu GX, Tonra JR, Fairchild-Huntress V, Fang Q, Dunmore JH, Huszar D, Pan Y. Mice deficient in fractalkine are less susceptible to cerebral ischemia-reperfusion injury. J Neuroimmunol. 2002;125(1–2):59–65. doi: 10.1016/s0165-5728(02)00033-4. [DOI] [PubMed] [Google Scholar]
- 194.Stamatovic SM, Shakui P, Keep RF, Moore BB, Kunkel SL, Van Rooijen N, Andjelkovic AV. Monocyte chemoattrac-tant protein-1 regulation of blood-brain barrier permeability. J Cereb Blood Flow Metab. 2005;25(5):593–606. doi: 10.1038/sj.jcbfm.9600055. [DOI] [PubMed] [Google Scholar]
- 195.Newman MB, Willing AE, Manresa JJ, Davis-Sanberg C, Sanberg PR. Stroke-induced migration of human umbilical cord blood cells: time course and cytokines. Stem Cells Dev. 2005;14(5):576–586. doi: 10.1089/scd.2005.14.576. [DOI] [PubMed] [Google Scholar]
- 196.Kelly S, Bliss TM, Shah AK, Sun GH, Ma M, Foo WC, Masel J, Yenari MA, Weissman IL, Uchida N, Palmer T, Steinberg GK. Transplanted human fetal neural stem cells survive, migrate, and differentiate in ischemic rat cerebral cortex. Proc Natl Acad Sci USA. 2004;101(32):11839–11844. doi: 10.1073/pnas.0404474101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Wang L, Li Y, Chen J, Gautam SC, Zhang Z, Lu M, Chopp M. Ischemic cerebral tissue and MCP-1 enhance rat bone marrow stromal cell migration in interface culture. Exp Hematol. 2002;30(7):831–836. doi: 10.1016/s0301-472x(02)00829-9. [DOI] [PubMed] [Google Scholar]
- 198.Wang L, Li Y, Chen X, Chen J, Gautam SC, Xu Y, Chopp M. MCP-1, MIP-1, IL-8 and ischemic cerebral tissue enhance human bone marrow stromal cell migration in interface culture. Hematology. 2002;7(2):113–117. doi: 10.1080/10245330290028588. [DOI] [PubMed] [Google Scholar]
- 199.Shichinohe H, Kuroda S, Yano S, Hida K, Iwasaki Y. Role of SDF-1/CXCR4 system in survival and migration of bone marrow stromal cells after transplantation into mice cerebral infarct. Brain Res. 2007;1183:138–147. doi: 10.1016/j.brainres.2007.08.091. [DOI] [PubMed] [Google Scholar]
- 200.Adibhatla RM, Hatcher JF, Larsen EC, Chen X, Sun D, Tsao FH. CDP-choline significantly restores phosphatidylcholine levels by differentially affecting phospholipase A2 and CTP: phosphocholine cytidylyltransferase after stroke. J Biol Chem. 2006;281(10):6718–6725. doi: 10.1074/jbc.M512112200. [DOI] [PubMed] [Google Scholar]
- 201.Sanchez-Moreno C, Dashe JF, Scott T, Thaler D, Folstein MF, Martin A. Decreased levels of plasma vitamin C and increased concentrations of inflammatory and oxidative stress markers after stroke. Stroke. 2004;35(1):163–168. doi: 10.1161/01.STR.0000105391.62306.2E. [DOI] [PubMed] [Google Scholar]
- 202.Bonventre JV, Huang Z, Taheri MR, O’Leary E, Li E, Moskowitz MA, Sapirstein A. Reduced fertility and postischaemic brain injury in mice deficient in cytosolic phospholipase A2. Nature. 1997;390(6660):622–625. doi: 10.1038/37635. [DOI] [PubMed] [Google Scholar]
- 203.Schwab JM, Beschorner R, Meyermann R, Gozalan F, Schluesener HJ. Persistent accumulation of cyclooxygenase-1-expressing microglial cells and macrophages and transient upregulation by endothelium in human brain injury. J Neurosurg. 2002;96(5):892–899. doi: 10.3171/jns.2002.96.5.0892. [DOI] [PubMed] [Google Scholar]
- 204.Iadecola C, Sugimoto K, Niwa K, Kazama K, Ross ME. Increased susceptibility to ischemic brain injury in cyclooxygenase-1-deficient mice. J Cereb Blood Flow Metab. 2001;21(12):1436–1441. doi: 10.1097/00004647-200112000-00008. [DOI] [PubMed] [Google Scholar]
- 205.Candelario-Jalil E, Gonzalez-Falcon A, Garcia-Cabrera M, Alvarez D, Al-Dalain S, Martinez G, Leon OS, Springer JE. Assessment of the relative contribution of COX-1 and COX-2 iso-forms to ischemia-induced oxidative damage and neurodegeneration following transient global cerebral ischemia. J Neurochem. 2003;86(3):545–555. doi: 10.1046/j.1471-4159.2003.01812.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Nogawa S, Zhang F, Ross ME, Iadecola C. Cyclo-oxygenase-2 gene expression in neurons contributes to ischemic brain damage. J Neurosci. 1997;17(8):2746–2755. doi: 10.1523/JNEUROSCI.17-08-02746.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Iadecola C, Forster C, Nogawa S, Clark HB, Ross ME. Cyclooxygenase-2 immunoreactivity in the human brain following cerebral ischemia. Acta Neuropathol. 1999;98(1):9–14. doi: 10.1007/s004010051045. [DOI] [PubMed] [Google Scholar]
- 208.Sairanen T, Ristimaki A, Karjalainen-Lindsberg ML, Paetau A, Kaste M, Lindsberg PJ. Cyclooxygenase-2 is induced globally in infarcted human brain. Ann Neurol. 1998;43(6):738–747. doi: 10.1002/ana.410430608. [DOI] [PubMed] [Google Scholar]
- 209.Kawano T, Anrather J, Zhou P, Park L, Wang G, Frys KA, Kunz A, Cho S, Orio M, Iadecola C. Prostaglandin E2 EP1 receptors: downstream effectors of COX-2 neurotoxicity. Nat Med. 2006;12(2):225–229. doi: 10.1038/nm1362. [DOI] [PubMed] [Google Scholar]
- 210.Sugimoto K, Iadecola C. Delayed effect of administration of COX-2 inhibitor in mice with acute cerebral ischemia. Brain Res. 2003;960(1–2):273–276. doi: 10.1016/s0006-8993(02)03805-2. [DOI] [PubMed] [Google Scholar]
- 211.Iadecola C, Niwa K, Nogawa S, Zhao X, Nagayama M, Araki E, Morham S, Ross ME. Reduced susceptibility to ischemic brain injury and N-methyl-D-aspartate-mediated neurotoxicity in cyclooxygenase-2-deficient mice. Proc Natl Acad Sci USA. 2001;98(3):1294–1299. doi: 10.1073/pnas.98.3.1294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Dore S, Otsuka T, Mito T, Sugo N, Hand T, Wu L, Hurn PD, Traystman RJ, Andreasson K. Neuronal overexpression of cyclooxygenase-2 increases cerebral infarction. Ann Neurol. 2003;54(2):155–162. doi: 10.1002/ana.10612. [DOI] [PubMed] [Google Scholar]
- 213.Manabe Y, Anrather J, Kawano T, Niwa K, Zhou P, Ross ME, Iadecola C. Prostanoids, not reactive oxygen species, mediate COX-2-dependent neurotoxicity. Ann Neurol. 2004;55(5):668–675. doi: 10.1002/ana.20078. [DOI] [PubMed] [Google Scholar]
- 214.Rao AM, Hatcher JF, Kindy MS, Dempsey RJ. Arachidonic acid and leukotriene C4: role in transient cerebral ischemia of gerbils. Neurochem Res. 1999;24(10):1225–1232. doi: 10.1023/a:1020916905312. [DOI] [PubMed] [Google Scholar]
- 215.Tomimoto H, Shibata M, Ihara M, Akiguchi I, Ohtani R, Budka H. A comparative study on the expression of cyclooxygenase and 5-lipoxygenase during cerebral ischemia in humans. Acta Neuropathol. 2002;104(6):601–607. doi: 10.1007/s00401-002-0590-0. [DOI] [PubMed] [Google Scholar]
- 216.Baskaya MK, Hu Y, Donaldson D, Maley M, Rao AM, Prasad MR, Dempsey RJ. Protective effect of the 5-lipoxygenase inhibitor AA-861 on cerebral edema after transient ischemia. J Neurosurg. 1996;85(1):112–116. doi: 10.3171/jns.1996.85.1.0112. [DOI] [PubMed] [Google Scholar]
- 217.Song Y, Wei EQ, Zhang WP, Zhang L, Liu JR, Chen Z. Minocycline protects PC12 cells from ischemic-like injury and inhibits 5-lipoxygenase activation. Neuroreport. 2004;15(14):2181–2184. doi: 10.1097/00001756-200410050-00007. [DOI] [PubMed] [Google Scholar]
- 218.Kitagawa K, Matsumoto M, Hori M. Cerebral ischemia in 5-lipoxygenase knockout mice. Brain Res. 2004;1004(1–2):198–202. doi: 10.1016/j.brainres.2004.01.018. [DOI] [PubMed] [Google Scholar]
- 219.Lapchak PA, Maher P, Schubert D, Zivin JA. Baicalein, an antioxidant 12/15-lipoxygenase inhibitor improves clinical rating scores following multiple infarct embolic strokes. Neuroscience. 2007;150(3):585–591. doi: 10.1016/j.neuroscience.2007.09.033. [DOI] [PubMed] [Google Scholar]
- 220.Rai G, Joshi N, Jung JE, Liu Y, Schultz L, Yasgar A, Perry S, Diaz G, Zhang Q, Kenyon V, Jadhav A, Simeonov A, Lo EH, van Leyen K, Maloney DJ, Holman TR. Potent and selective inhibitors of human reticulocyte 12/15-lipoxygenase as anti-stroke therapies. J Med Chem. 2014;57(10):4035–4048. doi: 10.1021/jm401915r. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Iadecola C, Zhang F, Xu S, Casey R, Ross ME. Inducible nitric oxide synthase gene expression in brain following cerebral ischemia. J Cereb Blood Flow Metab. 1995;15(3):378–384. doi: 10.1038/jcbfm.1995.47. [DOI] [PubMed] [Google Scholar]
- 222.Iadecola C, Zhang F, Xu X. Inhibition of inducible nitric oxide synthase ameliorates cerebral ischemic damage. Am J Physiol. 1995;268(1 Pt 2):R286–292. doi: 10.1152/ajpregu.1995.268.1.R286. [DOI] [PubMed] [Google Scholar]
- 223.Lakhan SE, Kirchgessner A, Hofer M. Inflammatory mechanisms in ischemic stroke: therapeutic approaches. J Transl Med. 2009;7:97. doi: 10.1186/1479-5876-7-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Cui J, Holmes EH, Liu PK. Oxidative damage to the c-fos gene and reduction of its transcription after focal cerebral ischemia. J Neurochem. 1999;73(3):1164–1174. doi: 10.1046/j.1471-4159.1999.0731164.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Cui J, Holmes EH, Greene TG, Liu PK. Oxidative DNA damage precedes DNA fragmentation after experimental stroke in rat brain. FASEB J. 2000;14(7):955–967. doi: 10.1096/fasebj.14.7.955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Huang D, Shenoy A, Cui J, Huang W, Liu PK. In situ detection of AP sites and DNA strand breaks bearing 3’-phosphate termini in ischemic mouse brain. FASEB J. 2000;14(2):407–417. doi: 10.1096/fasebj.14.2.407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Zhao X, Haensel C, Araki E, Ross ME, Iadecola C. Gene-dosing effect and persistence of reduction in ischemic brain injury in mice lacking inducible nitric oxide synthase. Brain Res. 2000;872(1–2):215–218. doi: 10.1016/s0006-8993(00)02459-8. [DOI] [PubMed] [Google Scholar]
- 228.Han HS, Qiao Y, Karabiyikoglu M, Giffard RG, Yenari MA. Influence of mild hypothermia on inducible nitric oxide synthase expression and reactive nitrogen production in experimental stroke and inflammation. J Neurosci. 2002;22(10):3921–3928. doi: 10.1523/JNEUROSCI.22-10-03921.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Coughlan T, Gibson C, Murphy S. Modulatory effects of pro-gesterone on inducible nitric oxide synthase expression in vivo and in vitro. J Neurochem. 2005;93(4):932–942. doi: 10.1111/j.1471-4159.2005.03068.x. [DOI] [PubMed] [Google Scholar]
- 230.Park EM, Cho S, Frys KA, Glickstein SB, Zhou P, Anrather J, Ross ME, Iadecola C. Inducible nitric oxide synthase contributes to gender differences in ischemic brain injury. J Cereb Blood Flow Metab. 2006;26(3):392–401. doi: 10.1038/sj.jcbfm.9600194. [DOI] [PubMed] [Google Scholar]
- 231.Chan PH. Reactive oxygen radicals in signaling and damage in the ischemic brain. J Cereb Blood Flow Metab. 2001;21(1):2–14. doi: 10.1097/00004647-200101000-00002. [DOI] [PubMed] [Google Scholar]
- 232.Groemping Y, Rittinger K. Activation and assembly of the NADPH oxidase: a structural perspective. Biochem J. 2005;386(Pt 3):401–416. doi: 10.1042/BJ20041835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Vallet P, Charnay Y, Steger K, Ogier-Denis E, Kovari E, Herrmann F, Michel JP, Szanto I. Neuronal expression of the NADPH oxidase NOX4, and its regulation in mouse experimental brain ischemia. Neuroscience. 2005;132(2):233–238. doi: 10.1016/j.neuroscience.2004.12.038. [DOI] [PubMed] [Google Scholar]
- 234.Yenari MA, Xu L, Tang XN, Qiao Y, Giffard RG. Microglia potentiate damage to blood-brain barrier constituents: improvement by minocycline in vivo and in vitro. Stroke. 2006;37(4):1087–1093. doi: 10.1161/01.STR.0000206281.77178.ac. [DOI] [PubMed] [Google Scholar]
- 235.Walder CE, Green SP, Darbonne WC, Mathias J, Rae J, Dinauer MC, Curnutte JT, Thomas GR. Ischemic stroke injury is reduced in mice lacking a functional NADPH oxidase. Stroke. 1997;28(11):2252–2258. doi: 10.1161/01.str.28.11.2252. [DOI] [PubMed] [Google Scholar]
- 236.Tang XN, Zheng Z, Giffard RG, Yenari MA. Significance of marrow-derived nicotinamide adenine dinucleotide phosphate oxidase in experimental ischemic stroke. Ann Neurol. 2011;70(4):606–615. doi: 10.1002/ana.22476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Won SJ, Tang XN, Suh SW, Yenari MA, Swanson RA. Hyperglycemia promotes tissue plasminogen activator-induced hemorrhage by Increasing superoxide production. Ann Neurol. 2011;70(4):583–590. doi: 10.1002/ana.22538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Takizawa S, Aratani Y, Fukuyama N, Maeda N, Hirabayashi H, Koyama H, Shinohara Y, Nakazawa H. Deficiency of myeloperoxidase increases infarct volume and nitrotyrosine formation in mouse brain. J Cereb Blood Flow Metab. 2002;22(1):50–54. doi: 10.1097/00004647-200201000-00006. [DOI] [PubMed] [Google Scholar]
- 239.Rosenberg GA. Matrix metalloproteinases in neuroinflammation. Glia. 2002;39(3):279–291. doi: 10.1002/glia.10108. [DOI] [PubMed] [Google Scholar]
- 240.Kelly MA, Shuaib A, Todd KG. Matrix metalloproteinase activation and blood-brain barrier breakdown following thrombolysis. Exp Neurol. 2006;200(1):38–49. doi: 10.1016/j.expneurol.2006.01.032. [DOI] [PubMed] [Google Scholar]
- 241.Yamashita T, Kamiya T, Deguchi K, Inaba T, Zhang H, Shang J, Miyazaki K, Ohtsuka A, Katayama Y, Abe K. Dissociation and protection of the neurovascular unit after thrombolysis and reperfusion in ischemic rat brain. J Cereb Blood Flow Metab. 2009;29(4):715–725. doi: 10.1038/jcbfm.2008.164. [DOI] [PubMed] [Google Scholar]
- 242.Rosenberg GA, Cunningham LA, Wallace J, Alexander S, Estrada EY, Grossetete M, Razhagi A, Miller K, Gearing A. Immunohistochemistry of matrix metalloproteinases in reperfusion injury to rat brain: activation of MMP-9 linked to stromelysin-1 and microglia in cell cultures. Brain Res. 2001;893(1–2):104–112. doi: 10.1016/s0006-8993(00)03294-7. [DOI] [PubMed] [Google Scholar]
- 243.Rosenberg GA, Estrada EY, Dencoff JE. Matrix metalloproteinases and TIMPs are associated with blood-brain barrier opening after reperfusion in rat brain. Stroke. 1998;29(10):2189–2195. doi: 10.1161/01.str.29.10.2189. [DOI] [PubMed] [Google Scholar]
- 244.Romanic AM, White RF, Arleth AJ, Ohlstein EH, Barone FC. Matrix metalloproteinase expression increases after cerebral focal ischemia in rats: inhibition of matrix metalloproteinase-9 reduces infarct size. Stroke. 1998;29(5):1020–1030. doi: 10.1161/01.str.29.5.1020. [DOI] [PubMed] [Google Scholar]
- 245.Pfefferkorn T, Rosenberg GA. Closure of the blood-brain barrier by matrix metalloproteinase inhibition reduces rtPA-mediated mortality in cerebral ischemia with delayed reperfusion. Stroke. 2003;34(8):2025–2030. doi: 10.1161/01.STR.0000083051.93319.28. [DOI] [PubMed] [Google Scholar]
- 246.Asahi M, Asahi K, Jung JC, del Zoppo GJ, Fini ME, Lo EH. Role for matrix metalloproteinase 9 after focal cerebral ischemia: effects of gene knockout and enzyme inhibition with BB-94. J Cereb Blood Flow Metab. 2000;20(12):1681–1689. doi: 10.1097/00004647-200012000-00007. [DOI] [PubMed] [Google Scholar]
- 247.Asahi M, Sumii T, Fini ME, Itohara S, Lo EH. Matrix metalloproteinase 2 gene knockout has no effect on acute brain injury after focal ischemia. Neuroreport. 2001;12(13):3003–3007. doi: 10.1097/00001756-200109170-00050. [DOI] [PubMed] [Google Scholar]
- 248.Montaner J, Alvarez-Sabin J, Molina C, Angles A, Abilleira S, Arenillas J, Gonzalez MA, Monasterio J. Matrix metalloproteinase expression after human cardioembolic stroke: temporal profile and relation to neurological impairment. Stroke. 2001;32(8):1759–1766. doi: 10.1161/01.str.32.8.1759. [DOI] [PubMed] [Google Scholar]
- 249.Gidday JM, Gasche YG, Copin JC, Shah AR, Perez RS, Shapiro SD, Chan PH, Park TS. Leukocyte-derived matrix metalloproteinase-9 mediates blood-brain barrier breakdown and is proinflammatory after transient focal cerebral ischemia. Am J Physiol Heart Circ Physiol. 2005;289(2):H558–568. doi: 10.1152/ajpheart.01275.2004. [DOI] [PubMed] [Google Scholar]
- 250.Lee SR, Kim HY, Rogowska J, Zhao BQ, Bhide P, Parent JM, Lo EH. Involvement of matrix metalloproteinase in neuroblast cell migration from the subventricular zone after stroke. J Neurosci. 2006;26(13):3491–3495. doi: 10.1523/JNEUROSCI.4085-05.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Zhao BQ, Wang S, Kim HY, Storrie H, Rosen BR, Mooney DJ, Wang X, Lo EH. Role of matrix metalloproteinases in delayed cortical responses after stroke. Nat Med. 2006;12(4):441–445. doi: 10.1038/nm1387. [DOI] [PubMed] [Google Scholar]
- 252.Baeuerle PA, Henkel T. Function and activation of NF-kappa B in the immune system. Annu Rev Immunol. 1994;12:141–179. doi: 10.1146/annurev.iy.12.040194.001041. [DOI] [PubMed] [Google Scholar]
- 253.Han HS, Karabiyikoglu M, Kelly S, Sobel RA, Yenari MA. Mild hypothermia inhibits nuclear factor-kappaB translocation in experimental stroke. J Cereb Blood Flow Metab. 2003;23(5):589–598. doi: 10.1097/01.WCB.0000059566.39780.8D. [DOI] [PubMed] [Google Scholar]
- 254.Cechetto DF. Role of nuclear factor kappa B in neuropathological mechanisms. Prog Brain Res. 2001;132:391–404. doi: 10.1016/S0079-6123(01)32090-3. [DOI] [PubMed] [Google Scholar]
- 255.Schneider A, Martin-Villalba A, Weih F, Vogel J, Wirth T, Schwaninger M. NF-kappaB is activated and promotes cell death in focal cerebral ischemia. Nat Med. 1999;5(5):554–559. doi: 10.1038/8432. [DOI] [PubMed] [Google Scholar]
- 256.Herrmann O, Baumann B, de Lorenzi R, Muhammad S, Zhang W, Kleesiek J, Malfertheiner M, Kohrmann M, Potrovita I, Maegele I, Beyer C, Burke JR, Hasan MT, Bujard H, Wirth T, Pasparakis M, Schwaninger M. IKK mediates ischemia-induced neuronal death. Nat Med. 2005;11(12):1322–1329. doi: 10.1038/nm1323. [DOI] [PubMed] [Google Scholar]
- 257.Ueno T, Sawa Y, Kitagawa-Sakakida S, Nishimura M, Morishita R, Kaneda Y, Kohmura E, Yoshimine T, Matsuda H. Nuclear factor-kappa B decoy attenuates neuronal damage after global brain ischemia: a future strategy for brain protection during circulatory arrest. J Thorac Cardiovasc Surg. 2001;122(4):720–727. doi: 10.1067/mtc.2001.115917. [DOI] [PubMed] [Google Scholar]
- 258.Hill WD, Hess DC, Carroll JE, Wakade CG, Howard EF, Chen Q, Cheng C, Martin-Studdard A, Waller JL, Beswick RA. The NF-kappaB inhibitor diethyldithiocarbamate (DDTC) increases brain cell death in a transient middle cerebral artery occlusion model of ischemia. Brain Res Bull. 2001;55(3):375–386. doi: 10.1016/s0361-9230(01)00503-2. [DOI] [PubMed] [Google Scholar]
- 259.Irving EA, Bamford M. Role of mitogen- and stress-activated kinases in ischemic injury. J Cereb Blood Flow Metab. 2002;22(6):631–647. doi: 10.1097/00004647-200206000-00001. [DOI] [PubMed] [Google Scholar]
- 260.Irving EA, Barone FC, Reith AD, Hadingham SJ, Parsons AA. Differential activation of MAPK/ERK and p38/SAPK in neurones and glia following focal cerebral ischaemia in the rat. Brain Res Mol Brain Res. 2000;77(1):65–75. doi: 10.1016/s0169-328x(00)00043-7. [DOI] [PubMed] [Google Scholar]
- 261.Sugino T, Nozaki K, Takagi Y, Hattori I, Hashimoto N, Moriguchi T, Nishida E. Activation of mitogen-activated protein kinases after transient forebrain ischemia in gerbil hippocampus. J Neurosci. 2000;20(12):4506–4514. doi: 10.1523/JNEUROSCI.20-12-04506.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Kyriakis JM, Avruch J. Mammalian mitogen-activated protein kinase signal transduction pathways activated by stress and inflammation. Physiol Rev. 2001;81(2):807–869. doi: 10.1152/physrev.2001.81.2.807. [DOI] [PubMed] [Google Scholar]
- 263.Zhang QG, Wang RM, Yin XH, Pan J, Xu TL, Zhang GY. Knock-down of POSH expression is neuroprotective through down-regulating activation of the MLK3-MKK4-JNK pathway following cerebral ischaemia in the rat hippocampal CA1 subfield. J Neurochem. 2005;95(3):784–795. doi: 10.1111/j.1471-4159.2005.03435.x. [DOI] [PubMed] [Google Scholar]
- 264.Gao Q, Li Y, Chopp M. Bone marrow stromal cells increase astrocyte survival via upregulation of phosphoinositide 3-kinase/threonine protein kinase and mitogen-activated protein kinase kinase/extracellular signal-regulated kinase pathways and stimulate astrocyte trophic factor gene expression after anaerobic insult. Neuroscience. 2005;136(1):123–134. doi: 10.1016/j.neuroscience.2005.06.091. [DOI] [PubMed] [Google Scholar]
- 265.Walton KM, DiRocco R, Bartlett BA, Koury E, Marcy VR, Jarvis B, Schaefer EM, Bhat RV. Activation of p38MAPK in microglia after ischemia. J Neurochem. 1998;70(4):1764–1767. doi: 10.1046/j.1471-4159.1998.70041764.x. [DOI] [PubMed] [Google Scholar]
- 266.Martinon F, Burns K, Tschopp J. The inflammasome: a molecular platform triggering activation of inflammatory caspases and processing of proIL-beta. Mol Cell. 2002;10(2):417–426. doi: 10.1016/s1097-2765(02)00599-3. [DOI] [PubMed] [Google Scholar]
- 267.Thauerer B, Zur Nedden S, Baier-Bitterlich G. Purine nucleosides: endogenous neuroprotectants in hypoxic brain. J Neurochem. 2012;121(3):329–342. doi: 10.1111/j.1471-4159.2012.07692.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Liew FY, Xu D, Brint EK, O’Neill LA. Negative regulation of toll-like receptor-mediated immune responses. Nat Rev Immunol. 2005;5(6):446–458. doi: 10.1038/nri1630. [DOI] [PubMed] [Google Scholar]
- 269.Piccinini AM, Midwood KS. DAMPening inflammation by modulating TLR signalling. Mediators Inflamm. 2010;2010 doi: 10.1155/2010/672395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Carty M, Bowie AG. Evaluating the role of Toll-like receptors in diseases of the central nervous system. Biochem Pharmacol. 2011;81(7):825–837. doi: 10.1016/j.bcp.2011.01.003. [DOI] [PubMed] [Google Scholar]
- 271.Kong Y, Le Y. Toll-like receptors in inflammation of the central nervous system. Int Immunopharmacol. 2011;11(10):1407–1414. doi: 10.1016/j.intimp.2011.04.025. [DOI] [PubMed] [Google Scholar]
- 272.Yang QW, Lu FL, Zhou Y, Wang L, Zhong Q, Lin S, Xiang J, Li JC, Fang CQ, Wang JZ. HMBG1 mediates ischemia-reperfusion injury by TRIF-adaptor independent Toll-like receptor 4 signaling. J Cereb Blood Flow Metab. 2011;31(2):593–605. doi: 10.1038/jcbfm.2010.129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Shichita T, Hasegawa E, Kimura A, Morita R, Sakaguchi R, Takada I, Sekiya T, Ooboshi H, Kitazono T, Yanagawa T, Ishii T, Takahashi H, Mori S, Nishibori M, Kuroda K, Akira S, Miyake K, Yoshimura A. Peroxiredoxin family proteins are key initiators of post-ischemic inflammation in the brain. Nat Med. 2012;18(6):911–917. doi: 10.1038/nm.2749. [DOI] [PubMed] [Google Scholar]
- 274.Ziegler G, Harhausen D, Schepers C, Hoffmann O, Rohr C, Prinz V, Konig J, Lehrach H, Nietfeld W, Trendelenburg G. TLR2 has a detrimental role in mouse transient focal cerebral ischemia. Biochem Biophys Res Commun. 2007;359(3):574–579. doi: 10.1016/j.bbrc.2007.05.157. [DOI] [PubMed] [Google Scholar]
- 275.Lalancette-Hebert M, Phaneuf D, Soucy G, Weng YC, Kriz J. Live imaging of Toll-like receptor 2 response in cerebral ischaemia reveals a role of olfactory bulb microglia as modulators of inflammation. Brain. 2009;132(Pt 4):940–954. doi: 10.1093/brain/awn345. [DOI] [PubMed] [Google Scholar]
- 276.Tu XK, Yang WZ, Shi SS, Wang CH, Zhang GL, Ni TR, Chen CM, Wang R, Jia JW, Song QM. Spatio-temporal distribution of inflammatory reaction and expression of TLR2/4 signaling pathway in rat brain following permanent focal cerebral ischemia. Neurochem Res. 2010;35(8):1147–1155. doi: 10.1007/s11064-010-0167-6. [DOI] [PubMed] [Google Scholar]
- 277.Lv M, Liu Y, Zhang J, Sun L, Liu Z, Zhang S, Wang B, Su D, Su Z. Roles of inflammation response in microglia cell through Toll-like receptors 2/interleukin-23/interleukin-17 pathway in cerebral ischemia/reperfusion injury. Neuroscience. 2011;176:162–172. doi: 10.1016/j.neuroscience.2010.11.066. [DOI] [PubMed] [Google Scholar]
- 278.Yao H, Felfly H, Wang J, Zhou D, Haddad GG. DIDS protects against neuronal injury by blocking Toll-like receptor 2 activated-mechanisms. J Neurochem. 2009;108(3):835–846. doi: 10.1111/j.1471-4159.2008.05838.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.Hua F, Ma J, Ha T, Kelley JL, Kao RL, Schweitzer JB, Kalbfleisch JH, Williams DL, Li C. Differential roles of TLR2 and TLR4 in acute focal cerebral ischemia/reperfusion injury in mice. Brain Res. 2009;1262:100–108. doi: 10.1016/j.brainres.2009.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Caso JR, Pradillo JM, Hurtado O, Lorenzo P, Moro MA, Lizasoain I. Toll-like receptor 4 is involved in brain damage and inflammation after experimental stroke. Circulation. 2007;115(12):1599–1608. doi: 10.1161/CIRCULATIONAHA.106.603431. [DOI] [PubMed] [Google Scholar]
- 281.Hyakkoku K, Hamanaka J, Tsuruma K, Shimazawa M, Tanaka H, Uematsu S, Akira S, Inagaki N, Nagai H, Hara H. Toll-like receptor 4 (TLR4): but not TLR3 or TLR9, knock-out mice have neuroprotective effects against focal cerebral ischemia. Neuroscience. 2010;171(1):258–267. doi: 10.1016/j.neuroscience.2010.08.054. [DOI] [PubMed] [Google Scholar]
- 282.Skaper SD. Ion channels on microglia: therapeutic targets for neuroprotection. CNS Neurol Disord Drug Targets. 2011;10(1):44–56. doi: 10.2174/187152711794488638. [DOI] [PubMed] [Google Scholar]
- 283.Melani A, Amadio S, Gianfriddo M, Vannucchi MG, Volonte C, Bernardi G, Pedata F, Sancesario G. P2X7 receptor modulation on microglial cells and reduction of brain infarct caused by middle cerebral artery occlusion in rat. J Cereb Blood Flow Metab. 2006;26(7):974–982. doi: 10.1038/sj.jcbfm.9600250. [DOI] [PubMed] [Google Scholar]
- 284.Yanagisawa D, Kitamura Y, Takata K, Hide I, Nakata Y, Taniguchi T. Possible involvement of P2X7 receptor activation in microglial neuroprotection against focal cerebral ischemia in rats. Biol Pharm Bull. 2008;31(6):1121–1130. doi: 10.1248/bpb.31.1121. [DOI] [PubMed] [Google Scholar]
- 285.Arbeloa J, Perez-Samartin A, Gottlieb M, Matute C. P2X7 receptor blockade prevents ATP excitotoxicity in neurons and reduces brain damage after ischemia. Neurobiol Dis. 2012;45(3):954–961. doi: 10.1016/j.nbd.2011.12.014. [DOI] [PubMed] [Google Scholar]
- 286.Chu K, Yin B, Wang J, Peng G, Liang H, Xu Z, Du Y, Fang M, Xia Q, Luo B. Inhibition of P2X7 receptor ameliorates transient global cerebral ischemia/reperfusion injury via modulating inflammatory responses in the rat hippocampus. J Neuroinflammation. 2012;9:69. doi: 10.1186/1742-2094-9-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Inoue K. Purinergic systems in microglia. Cell Mol Life Sci. 2008;65(19):3074–3080. doi: 10.1007/s00018-008-8210-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288.Irino Y, Nakamura Y, Inoue K, Kohsaka S, Ohsawa K. Akt activation is involved in P2Y12 receptor-mediated chemotaxis of microglia. J Neurosci Res. 2008;86(7):1511–1519. doi: 10.1002/jnr.21610. [DOI] [PubMed] [Google Scholar]
- 289.Webster CM, Hokari M, Tang XN, Yenari MA. P2Y12 receptors in ischemic inflammation: A new role for clopidogrel? Stroke. 2011;42(3):e296. [Google Scholar]
- 290.Ajmo CT, Jr, Vernon DO, Collier L, Hall AA, Garbuzova-Davis S, Willing A, Pennypacker KR. The spleen contributes to stroke-induced neurodegeneration. J Neurosci Res. 2008;86(10):2227–2234. doi: 10.1002/jnr.21661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 291.Liesz A, Hagmann S, Zschoche C, Adamek J, Zhou W, Sun L, Hug A, Zorn M, Dalpke A, Nawroth P, Veltkamp R. The spectrum of systemic immune alterations after murine focal ischemia: immunodepression versus immunomodulation. Stroke. 2009;40(8):2849–2858. doi: 10.1161/STROKEAHA.109.549618. [DOI] [PubMed] [Google Scholar]
- 292.Gendron A, Teitelbaum J, Cossette C, Nuara S, Dumont M, Geadah D, du Souich P, Kouassi E. Temporal effects of left versus right middle cerebral artery occlusion on spleen lymphocyte subsets and mitogenic response in Wistar rats. Brain Res. 2002;955(1–2):85–97. doi: 10.1016/s0006-8993(02)03368-1. [DOI] [PubMed] [Google Scholar]
- 293.Martin A, Aguirre J, Sarasa-Renedo A, Tsoukatou D, Garofalakis A, Meyer H, Mamalaki C, Ripoll J, Planas AM. Imaging changes in lymphoid organs in vivo after brain ischemia with three-dimensional fluorescence molecular tomography in transgenic mice expressing green fluorescent protein in T lymphocytes. Mol Imaging. 2008;7(4):157–167. [PubMed] [Google Scholar]
- 294.Prass K, Braun JS, Dirnagl U, Meisel C, Meisel A. Stroke propagates bacterial aspiration to pneumonia in a model of cerebral ischemia. Stroke. 2006;37(10):2607–2612. doi: 10.1161/01.STR.0000240409.68739.2b. [DOI] [PubMed] [Google Scholar]
- 295.Aslanyan S, Weir CJ, Diener HC, Kaste M, Lees KR. Pneumonia and urinary tract infection after acute ischaemic stroke: a tertiary analysis of the GAIN International trial. Eur J Neurol. 2004;11(1):49–53. doi: 10.1046/j.1468-1331.2003.00749.x. [DOI] [PubMed] [Google Scholar]
- 296.Hilker R, Poetter C, Findeisen N, Sobesky J, Jacobs A, Neveling M, Heiss WD. Nosocomial pneumonia after acute stroke: implications for neurological intensive care medicine. Stroke. 2003;34(4):975–981. doi: 10.1161/01.STR.0000063373.70993.CD. [DOI] [PubMed] [Google Scholar]
- 297.Langhorne P, Stott DJ, Robertson L, MacDonald J, Jones L, McAlpine C, Dick F, Taylor GS, Murray G. Medical complications after stroke: a multicenter study. Stroke. 2000;31(6):1223–1229. doi: 10.1161/01.str.31.6.1223. [DOI] [PubMed] [Google Scholar]
- 298.Urra X, Cervera A, Villamor N, Planas AM, Chamorro A. Harms and benefits of lymphocyte subpopulations in patients with acute stroke. Neuroscience. 2009;158(3):1174–1183. doi: 10.1016/j.neuroscience.2008.06.014. [DOI] [PubMed] [Google Scholar]
- 299.Pavlov VA, Wang H, Czura CJ, Friedman SG, Tracey KJ. The cholinergic anti-inflammatory pathway: a missing link in neuroimmunomodulation. Mol Med. 2003;9(5–8):125–134. [PMC free article] [PubMed] [Google Scholar]
- 300.Tracey KJ. Physiology and immunology of the cholinergic antiinflammatory pathway. J Clin Invest. 2007;117(2):289–296. doi: 10.1172/JCI30555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 301.Use of anti-ICAM-1 therapy in ischemic stroke: results of the Enlimomab Acute Stroke Trial. Neurology. 2001;57(8):1428–1434. doi: 10.1212/wnl.57.8.1428. [DOI] [PubMed] [Google Scholar]
- 302.Becker KJ. Anti-leukocyte antibodies: LeukArrest (Hu23F2G) and Enlimomab (R6.5) in acute stroke. Curr Med Res Opin. 2002;18(Suppl 2):s18–22. doi: 10.1185/030079902125000688. [DOI] [PubMed] [Google Scholar]
- 303.Schneider D, Berrouschot J, Brandt T, Hacke W, Ferbert A, Norris SH, Polmar SH, Schafer E. Safety, pharmacokinetics and biological activity of enlimomab (anti-ICAM-1 antibody): an open-label, dose escalation study in patients hospitalized for acute stroke. Eur Neurol. 1998;40(2):78–83. doi: 10.1159/000007962. [DOI] [PubMed] [Google Scholar]
- 304.Krams M, Lees KR, Hacke W, Grieve AP, Orgogozo JM, Ford GA. Acute Stroke Therapy by Inhibition of Neutrophils (ASTIN): an adaptive dose-response study of UK-279,276 in acute ischemic stroke. Stroke. 2003;34(11):2543–2548. doi: 10.1161/01.STR.0000092527.33910.89. [DOI] [PubMed] [Google Scholar]
- 305.Caimi G, Canino B, Ferrara F, Montana M, Musso M, Porretto F, Carollo C, Catania A, Lo Presti R. Granulocyte integrins before and after activation in acute ischaemic stroke. J Neurol Sci. 2001;186(1–2):23–26. doi: 10.1016/s0022-510x(01)00495-6. [DOI] [PubMed] [Google Scholar]
- 306.Campanella M, Sciorati C, Tarozzo G, Beltramo M. Flow cytometric analysis of inflammatory cells in ischemic rat brain. Stroke. 2002;33(2):586–592. doi: 10.1161/hs0202.103399. [DOI] [PubMed] [Google Scholar]
- 307.Del Zoppo GJ. Why do all drugs work in animals but none in stroke patients? 1. Drugs promoting cerebral blood flow. J Intern Med. 1995;237(1):79–88. doi: 10.1111/j.1365-2796.1995.tb01144.x. [DOI] [PubMed] [Google Scholar]
- 308.Tikka T, Fiebich BL, Goldsteins G, Keinanen R, Koistinaho J. Minocycline, a tetracycline derivative, is neuroprotective against excitotoxicity by inhibiting activation and proliferation of microglia. J Neurosci. 2001;21(8):2580–2588. doi: 10.1523/JNEUROSCI.21-08-02580.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 309.Koistinaho M, Malm TM, Kettunen MI, Goldsteins G, Starckx S, Kauppinen RA, Opdenakker G, Koistinaho J. Minocycline protects against permanent cerebral ischemia in wild type but not in matrix metalloprotease-9-deficient mice. J Cereb Blood Flow Metab. 2005;25(4):460–467. doi: 10.1038/sj.jcbfm.9600040. [DOI] [PubMed] [Google Scholar]
- 310.Liu Z, Fan Y, Won SJ, Neumann M, Hu D, Zhou L, Weinstein PR, Liu J. Chronic treatment with minocycline preserves adult new neurons and reduces functional impairment after focal cerebral ischemia. Stroke. 2007;38(1):146–152. doi: 10.1161/01.STR.0000251791.64910.cd. [DOI] [PubMed] [Google Scholar]
- 311.Tang XN, Wang Q, Koike MA, Cheng D, Goris ML, Blankenberg FG, Yenari MA. Monitoring the protective effects of minocycline treatment with radiolabeled annexin V in an experimental model of focal cerebral ischemia. J Nucl Med. 2007;48(11):1822–1828. doi: 10.2967/jnumed.107.041335. [DOI] [PubMed] [Google Scholar]
- 312.Lampl Y, Boaz M, Gilad R, Lorberboym M, Dabby R, Rapoport A, Anca-Hershkowitz M, Sadeh M. Minocycline treatment in acute stroke: an open-label, evaluator-blinded study. Neurology. 2007;69(14):1404–1410. doi: 10.1212/01.wnl.0000277487.04281.db. [DOI] [PubMed] [Google Scholar]
- 313.Fagan SC, Waller JL, Nichols FT, Edwards DJ, Pettigrew LC, Clark WM, Hall CE, Switzer JA, Ergul A, Hess DC. Minocycline to improve neurologic outcome in stroke (MINOS): a dose-finding study. Stroke. 2010;41(10):2283–2287. doi: 10.1161/STROKEAHA.110.582601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 314.Switzer JA, Hess DC, Ergul A, Waller JL, Machado LS, Portik-Dobos V, Pettigrew LC, Clark WM, Fagan SC. Matrix metalloproteinase-9 in an exploratory trial of intravenous minocycline for acute ischemic stroke. Stroke. 2011;42(9):2633–2635. doi: 10.1161/STROKEAHA.111.618215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 315.Pelletier D, Hafler DA. Fingolimod for multiple sclerosis. N Engl J Med. 2012;366(4):339–347. doi: 10.1056/NEJMct1101691. [DOI] [PubMed] [Google Scholar]
- 316.Baumruker T, Billich A, Brinkmann V. FTY720, an immunomodulatory sphingolipid mimetic: translation of a novel mechanism into clinical benefit in multiple sclerosis. Expert Opin Investig Drugs. 2007;16(3):283–289. doi: 10.1517/13543784.16.3.283. [DOI] [PubMed] [Google Scholar]
- 317.Billich A, Bornancin F, Devay P, Mechtcheriakova D, Urtz N, Baumruker T. Phosphorylation of the immunomodulatory drug FTY720 by sphingosine kinases. J Biol Chem. 2003;278(48):47408–47415. doi: 10.1074/jbc.M307687200. [DOI] [PubMed] [Google Scholar]
- 318.Pfeilschifter W, Czech-Zechmeister B, Sujak M, Mirceska A, Koch A, Rami A, Steinmetz H, Foerch C, Huwiler A, Pfeilschifter J. Activation of sphingosine kinase 2 is an endogenous protective mechanism in cerebral ischemia. Biochem Biophys Res Commun. 2011;413(2):212–217. doi: 10.1016/j.bbrc.2011.08.070. [DOI] [PubMed] [Google Scholar]
- 319.Brinkmann V, Davis MD, Heise CE, Albert R, Cottens S, Hof R, Bruns C, Prieschl E, Baumruker T, Hiestand P, Foster CA, Zollinger M, Lynch KR. The immune modulator FTY720 targets sphingosine 1-phosphate receptors. J Biol Chem. 2002;277(24):21453–21457. doi: 10.1074/jbc.C200176200. [DOI] [PubMed] [Google Scholar]
- 320.Czech B, Pfeilschifter W, Mazaheri-Omrani N, Strobel MA, Kahles T, Neumann-Haefelin T, Rami A, Huwiler A, Pfeilschifter J. The immunomodulatory sphingosine 1-phosphate analog FTY720 reduces lesion size and improves neurological outcome in a mouse model of cerebral ischemia. Biochem Biophys Res Commun. 2009;389(2):251–256. doi: 10.1016/j.bbrc.2009.08.142. [DOI] [PubMed] [Google Scholar]
- 321.Hasegawa Y, Suzuki H, Sozen T, Rolland W, Zhang JH. Activation of sphingosine 1-phosphate receptor-1 by FTY720 is neuroprotective after ischemic stroke in rats. Stroke. 2010;41(2):368–374. doi: 10.1161/STROKEAHA.109.568899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 322.Wei Y, Yemisci M, Kim HH, Yung LM, Shin HK, Hwang SK, Guo S, Qin T, Alsharif N, Brinkmann V, Liao JK, Lo EH, Waeber C. Fingolimod provides long-term protection in rodent models of cerebral ischemia. Ann Neurol. 2011;69(1):119–129. doi: 10.1002/ana.22186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 323.Kimura A, Ohmori T, Kashiwakura Y, Ohkawa R, Madoiwa S, Mimuro J, Shimazaki K, Hoshino Y, Yatomi Y, Sakata Y. Antagonism of sphingosine 1-phosphate receptor-2 enhances migration of neural progenitor cells toward an area of brain. Stroke. 2008;39(12):3411–3417. doi: 10.1161/STROKEAHA.108.514612. [DOI] [PubMed] [Google Scholar]
- 324.Yagi H, Kamba R, Chiba K, Soga H, Yaguchi K, Nakamura M, Itoh T. Immunosuppressant FTY720 inhibits thymocyte emigration. Eur J Immunol. 2000;30(5):1435–1444. doi: 10.1002/(SICI)1521-4141(200005)30:5<1435::AID-IMMU1435>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- 325.Brinkmann V, Pinschewer DD, Feng L, Chen S. FTY720: altered lymphocyte traffic results in allograft protection. Transplantation. 2001;72(5):764–769. doi: 10.1097/00007890-200109150-00002. [DOI] [PubMed] [Google Scholar]
- 326.Jung CG, Kim HJ, Miron VE, Cook S, Kennedy TE, Foster CA, Antel JP, Soliven B. Functional consequences of S1P receptor modulation in rat oligodendroglial lineage cells. Glia. 2007;55(16):1656–1667. doi: 10.1002/glia.20576. [DOI] [PubMed] [Google Scholar]
- 327.Stessin AM, Gursel DB, Schwartz A, Parashar B, Kulidzhanov FG, Sabbas AM, Boockvar J, Nori D, Wernicke AG. FTY720, sphingosine 1-phosphate receptor modulator, selectively radioprotects hippocampal neural stem cells. Neurosci Lett. 2012;516(2):253–258. doi: 10.1016/j.neulet.2012.04.004. [DOI] [PubMed] [Google Scholar]
- 328.Liu J, Zhang C, Tao W, Liu M. Systematic Review and meta-analysis of the Efficacy of sphingosine-1-phosphate (S1P) receptor agonist FTY720 (fingolimod) in Animal Models of Stroke. Int J Neurosci. 2013;123(3):163–169. doi: 10.3109/00207454.2012.749255. [DOI] [PubMed] [Google Scholar]