Abstract
A mounting body of literature recommends that treatment for fibromyalgia (FM) encompass medications, exercise and improvement of coping skills. However, there is a significant gap in determining an effective counterpart to pharmacotherapy that incorporates both exercise and coping. The aim of this randomized controlled trial was to evaluate the effects of a comprehensive yoga intervention on FM symptoms and coping. A sample of 53 female FM patients were randomized to the 8-week Yoga of Awareness program (gentle poses, meditation, breathing exercises, yoga-based coping instructions, group discussions) or to wait-listed standard care. Data were analyzed by intention to treat. At post-treatment, women assigned to the yoga program showed significantly greater improvements on standardized measures of FM symptoms and functioning, including pain, fatigue, and mood, and in pain catastrophizing, acceptance, and other coping strategies. This pilot study provides promising support for the potential benefits of a yoga program for women with FM.
Keywords: Fibromyalgia, Pain, Randomized controlled trial, Yoga, Meditation, Mindfulness
1. Introduction
Fibromyalgia (FM) is a debilitating condition affecting 11–15 million persons in the US [61]. Most FM patients use health services extensively; FM carries an annual direct cost for care of >$20 billion [61]. FDA-indicated drug therapies are generally only 30% effective in relieving symptoms and 20% effective in improving function [48]. Multiple position statements recommend that medications be accompanied by exercise and coping skills approaches [19,28].
Yoga is a mind/body discipline which may fulfill the need for both exercise and coping skills components of FM treatment [30,36]. In recent years yoga has been widely adopted by FM patients of all cultural backgrounds [33]. Yoga comprises a wide variety of methods, such as meditation and breathing exercises, beyond the physical poses that have become popularly identified with yoga. Yoga styles vary greatly in the methods they emphasize.
Thus far only one small randomized controlled trial (RCT) has tested the effects of yoga on FM. This trial reported 30% improvement in overall symptoms (n = 33) [22].
The present study was a RCT of a more comprehensive intervention, “Yoga of Awareness”. In this program gentle yoga poses are complemented by meditation and breathing exercises, yoga-based coping presentations, and group discussions. Previous Yoga of Awareness studies in breast cancer have demonstrated improvements in pain, fatigue, sleep and mood [14,15] – symptoms which are prominent in FM. We hypothesized that the intervention would be superior to a wait-listed standard care condition on measures of FM symptoms and functional deficits, and pain coping strategies.
2. Methods
2.1. Subjects
The 53 participants in this study were all women ≥21 years of age. Given the much higher prevalence of FM in females (80–90%), and the positive effects for women with breast cancer in our earlier trials, we chose to include only women in this phase of our research plans [61]. To be eligible, patients had to meet the following criteria: be diagnosed with FM by American College of Rheumatology (ACR) criteria [64] for at least 1 year, and be on a stable regimen of pharmacologic and/or non-pharmacologic treatment for FM ≥3 months. Patients with any of the following conditions were excluded from the study: (a) residing >70 miles from the research site or unavailable to attend the intervention at one of the scheduled times, (b) currently engaged in intensive yoga practice (practice >3 days/week), (c) actively contemplating suicide (none were excluded on this basis), (d) currently undergoing disability application, determination or litigation, (e) scheduled for elective surgery during the study period, (f) physically disabled in a manner that precluded meaningful participation in the intervention (e.g., quadriplegic paralysis), (g) unwilling to forgo changing their voluntary pharmacologic and/or non-pharmacologic treatments for the length of their participation in the study, or (h) do not speak English.
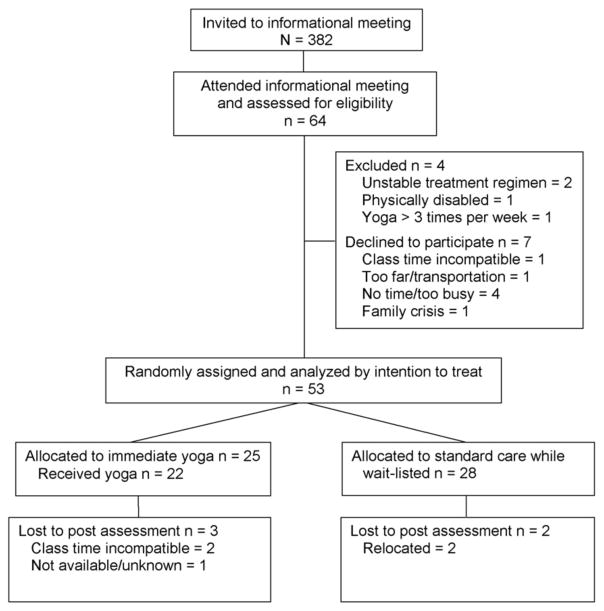
2.2. Study flow
Fig. 1 developed from the CONSORT statement shows the progression of subjects through the treatment study. Potential participants were identified between October 2009 – January 2010 from a database of FM patients referred to our university tertiary care center who had indicated their interest in participating in research studies. An invitation to attend an informational meeting about the study was sent out by email (or standard mail if email addresses were unknown) to 382 women whose street addresses were within the catchment area. The meeting was attended by 64 women who were briefly assessed for eligibility. Of 56 women who enrolled in the study and initially appeared eligible, three patients were excluded based on a priori criteria: two because they were not on stable FM treatment regimens for ≥3 months (1 = newly diagnosed trigeminal neuropathy; 1 = started pain coping class, changed doctors and medications) and one because of an excessively disabling vestibular diagnosis (physician had prohibited walking up stairs and other postural elevation changes). Thus 53 were randomized (yoga = 25, standard care while wait-listed = 28).
Fig. 1.
Study participant flow.
The completion rate at the post-treatment assessment was 91%. There were three noncompleters in the yoga condition (2 = class time incompatible; 1 = not available/unknown) and two in the wait-listed condition (both relocated). The only baseline predictor of noncompletion was age, such that noncompleters were significantly younger than completers (M = 41 vs. 55 years, p = .006).
2.3. Study design and procedure
The protocol for this study was approved by the Oregon Health and Science University Institutional Review Board. After signing informed consent forms, patients completed the baseline assessment. Patients meeting inclusion and exclusion criteria were then randomly assigned to either start the yoga program immediately (yoga condition) or 3 months later (wait-list control condition). While recognizing its limitations (please see Section 5) we chose a wait-listed standard care model because of the pilot nature of the study, and because participants assigned to a wait list are often more motivated to remain in a study in order to eventually receive a desired intervention [12,35]. Randomization assignments were generated by an individual not involved in the study using a random number table. Assignments were concealed in envelopes that were not opened until patients had completed their baseline assessment. Patients completed the post-treatment assessment immediately after the yoga condition had finished the 8-week intervention. The research assistants collecting assessment data were kept blind with regard to patient condition assignments. Patients received $25 for completing the post-treatment assessment. Throughout their participation in the study, all patients continued to receive the standard care provided by their health care providers.
2.4. Treatment conditions
2.4.1. Yoga of Awareness intervention condition
This intervention aimed to fulfill the need for both exercise and coping skills training as complements to standard medical treatments for FM. The intervention consisted of eight once-per-week 120 min group classes (7–12 patients per group) held in an exercise studio at the Oregon Health & Science University School of Nursing. All the groups were led by a certified yoga teacher (K.M.C.) who has received comprehensive training in traditional schools of yoga, holds a master’s degree in health education, and has extensive experience in teaching yoga and meditation techniques to medical patients and the general public. To standardize delivery of the intervention, a manual was developed which provided detailed class guidelines which were followed by the yoga teacher.
Yoga of Awareness is an innovative, comprehensive yoga program, which for this study was tailored to address pain, fatigue, sleep disturbance, and emotional distress in FM. The program is based on the ancient Indian discipline of yoga (meaning “yoking” or “union”). During recent years, as the physical exercises of yoga (asana) have become popularized in Western countries, the term “yoga” in common usage has largely become synonymous with this single aspect of the fuller discipline. In actuality, yoga comprises a wide variety of methods and approaches, with meditation (dhyana), breathing exercises (pranayama), study of the application of yogic principles to optimal coping (swadhyaya, literally “self-study”), and practitioner meetings and interchange (satsang) among the most common practices [21]. Each Yoga of Awareness class included approximately 40 min of gentle stretching poses (see details below), 25 min of mindfulness meditation (e.g., awareness of breath, awareness of awareness itself), 10 min of breathing techniques (e.g., full yogic breath, breathing into sensation), 20 min of didactic presentations on the application of yogic principles to optimal coping, and 25 min of group discussions (e.g., experiences while practicing yoga at home).
Yoga of Awareness draws strongly on the Kripalu school of yoga, which along with the safe performance of physical poses emphasizes the inner dimensions of yogic practice, including mindfulness training [21]. Mindfulness entails strategies for developing greater moment-to-moment presence of mind, and acceptance of and willingness to learn from pain and other stressful experiences, so as to begin to recognize clearly what choices contribute to more well being versus suffering [39,43]. Accordingly the coping strategies employed in this intervention were drawn from the yoga tradition, rather than from the repertoire of standard cognitive-behavioral therapy (CBT) coping strategies (such as progressive relaxation and cognitive reframing) [16]. These yoga-based coping strategies included reconnecting with “simple being” (the familiar, immediate sense of just being present at any given moment), discovering and observing the wave-like pattern (arising, cresting, subsiding) of all types of experiences as a way to maintain poise amidst the tumult of stressful circumstances, distinguishing between actual events and our minds’ tendencies for creating “stories” about these events, practicing kindness and patience with oneself and others, practicing “yogic sleep” (yoga nidra, an exercise that cultivates simultaneous deep relaxation and full alertness), and other strategies drawn from the yoga tradition. Applications of yoga to daily life were also assigned each week (e.g., in-the-moment acceptance of pain).
Patients were supplied with yoga mats, blankets, eye pillows, and bolsters for doing yoga poses. Participants were encouraged to practice at home 20–40 min per day, 5–7 days per week, guided by a professionally produced DVD featuring FM patients (supplemented by audio recordings and an illustrated handbook as needed). The yoga poses consisted of a single sequence that offered versions that could be done either in a chair or out of a chair. The sequence included self-massage, warm-ups, table, mountain, mountain with sun arms, breath of joy, warrior 1 flow, chair, downward-facing dog on chair, sphinx, modified locust, child’s pose, supine core strengthening, supine pigeon, supine thoracic twist flow, bridge, knees to chest, and corpse. Students were also introduced to a restorative version of legs in a chair with pelvis support and a twist over a bolster.
The yoga teacher highlighted the need for gentle practice when one’s body is challenged by illness, and participants were encouraged to work according to their limits, rather than rigidly adhere to concepts about how postures must be performed. The protocol employed a series of low intensity, low impact yoga poses which were modified for common pathophysiologic changes in FM [37]. For example, eccentric and repetitive muscle activities were minimized to reduce muscle microtrauma; slow transition from lying to standing was incorporated due to FM-related changes in the autonomic nervous system; and peripheral pain generators such as knee osteoarthritis were minimized by adapting standing poses to sitting or lying poses. Foam blocks were used to minimize wrist pain or carpal tunnel symptoms in certain poses. This tailoring of poses reflected research showing low intensity, low impact, customizable exercise programs yield low attrition rates in FM, whereas high rates of attrition or worsening FM symptoms have been reported in studies that employed high intensity, repetitive exercises that were not sensitive to the underlying pathophysiology of FM [22,36,37].
Participants kept a daily record of time spent in yoga practice which was collected during weekly sessions. To boost retention and adherence, the teacher contacted patients who missed sessions to negotiate attendance barriers and or to address home practice barriers (if average practice <20 min).
2.4.2. Standard care while wait-listed control condition
This condition controlled for any effects of symptom measurement reactivity in patients receiving routine FM medical care. These participants were contacted by phone at the 5-week point of the intervention period to answer any questions and to set up the post-treatment assessment. After the post-treatment assessment, these patients were invited to participate in the yoga program.
2.5. Assessment procedures
Outcome assessments were administered at baseline (2 weeks before the yoga condition intervention began), and at post-treatment (the same week the yoga condition intervention had ended). Three types of measurement instruments – standardized questionnaires, physical tests, and daily diaries – were employed to capture information about FM symptoms and functional deficits, and pain coping strategies.
2.6. Questionnaires assessing fibromyalgia symptoms and functional deficits
2.6.1. Fibromyalgia symptoms and functional deficits
The primary treatment outcome measure was the Total Score of the Fibromyalgia Impact Questionnaire Revised (FIQR), a 21-item self-assessment of the following fibromyalgia symptoms and functional deficits: pain, fatigue, stiffness, poor sleep, depression, poor memory, anxiety, tenderness, poor balance, and environment sensitivity [3,7]. Scores range from 0–100 with higher scores indicating more symptom burden and functional limitations in FM. The FIQR is a recently updated version of the widely used Fibromyalgia Impact Questionnaire (FIQ) which has been extensively validated in clinical trials. The FIQR has good psychometric properties and comparable scoring characteristics to the original FIQ, making it possible to compare FIQ and FIQR results. In addition to the Total Score, the FIQR includes scales for Symptoms, Function, and Overall Impact. In this study, the reliability coefficients of the FIQR scales were: Total Score, .93; Symptoms, .87; Function, .93; and Overall Impact, .79.
2.6.2. Overall improvement in fibromyalgia symptoms
The Patient Global Impression of Change (PGIC), a well-established outcome measure required by the FDA in FM trials, was used to assess overall improvement in fibromyalgia symptoms. This measure is designed to be administered only once, at post-treatment [24]. The PGIC asked patients to rate overall improvement in FM symptoms during the study using a single 7-point scale anchored by “very much improved” and “very much worsened”.
2.7. Physical tests of fibromyalgia symptoms and functional deficits
2.7.1. Myalgic tender points
The number of tender points and extent of tenderness was measured to derive the Total Myalgic Score (TMS) as determined by patients’ responses to digital application of 4 kg of pressure over 4 s at 18 sites as described in the ACR criteria for FM [64]. A single examiner (K.D.J.) performed all tests. Scores range from 11–53 with higher scores indicating greater pain.
2.7.2. Strength deficits
Functional strength deficits were measured by the Timed Chair Rise [46]. In this test, seated subjects are asked to rise to full height with arms crossed over their chest as many times as possible within 30 s.
2.7.3. Balance deficits
Functional balance deficits were measured by the Sensory Integration for Balance Test (SCBT) [34]. In this test subjects stand on a NASA-grade 60 × 60 cm block of 4-inch, medium-density Tempur foam with eyes open, then closed. The scores for Balance-Eyes Open and Balance-Eyes Closed are the number of seconds the position is held, up to 30 s maximum.
2.8. Questionnaires assessing pain coping strategies
2.8.1. Pain acceptance
Pain acceptance was measured by the Chronic Pain Acceptance Questionnaire (CPAQ) [42]. The 20-item CPAQ is a valid and reliable instrument for self-assessment of participation in daily activities regardless of pain (Activity Engagement Despite Pain) and willingness to tolerate pain (Pain Willingness). The Acceptance Total Score combines the Activity Engagement Despite Pain and Pain Willingness subscales, with scores ranging from 0–120 with higher scores indicating greater pain acceptance. In this study, the reliability coefficients of these scales were: Acceptance Total Score, .89; Activity Engagement Despite Pain, .88; and Pain Willingness, .73;
2.8.2. Pain catastrophizing
The 6-item catastrophizing subscale of the widely used Coping Strategies Questionnaire (CSQ) was used to capture the frequency of patients’ responses to pain that characterize it as being awful, horrible and unbearable [47]. Scores range from 0–36 with higher scores indicating greater pain catastrophizing. This measure’s reliability coefficient in this study was .90.
2.8.3. Adaptive and maladaptive pain coping strategies
A wide range of pain coping strategies was assessed with scales from the Vanderbilt Multidimensional Pain Coping Inventory (VMPCI) [53] The VMPCI is an extensively validated self-report questionnaire from which we selected 10 scales of strategies that previous research had shown to be either usually adaptive (Problem Solving, Positive Reappraisal, Distraction, Use of Religion, and Use of Social Support) or maladaptive (Distancing, Self-blame, Self-isolation, Confrontation, and Disengagement) [52,53] In this study, the reliability coefficients of these scales were: Problem Solving, .77; Reappraisal, .68; Distraction, .66; Use of Religion, .96; Seeking Social Support, .73; Distancing, .79; Self-blame, .66; Self-isolation, .91; Confrontation, .77; and Disengagement, .85.
2.9. Daily diaries assessing pain, fatigue, distress, vigor, acceptance and relaxation
Using an online service, SurveyMonkey.com, real-time daily measures were collected for a set of FM symptoms and pain coping strategies during 1 week at baseline and 1 week immediately post-treatment [1,12,14,15,16,18,25]. Using 0–10 single item scales in which higher scores reflected greater amounts, the diaries assessed daily pain, fatigue, emotional distress, and vigor, along with success at coping via acceptance and relaxation strategies. Minutes spent in home yoga practice (postures, meditation, and breathing exercises) were also assessed among those in the yoga condition. Five subjects who had limited home internet access completed pen-and-paper equivalent diaries which were returned each day using pre-stamped envelopes.
Subjects were called as need be during the first week of each diary recording period to inquire about any difficulties completing the online diaries. The baseline diary completion rate was good, 87%. Among patients who completed the post-treatment assessment, the diary completion rate was similar, 86%.
2.10. Demographic and clinical variables
We collected information about standard demographic and clinical variables (age, years since diagnosis, years symptomatic, race/ethnicity, marital status, education, employment). Also, at the post-treatment assessment information was collected about any changes in medications or in medical or alternative treatments for FM.
3. Statistical analyses
The primary treatment outcome measure was the Total Score of the Fibromyalgia Impact Questionnaire Revised (FIQR) [3,7]. Power calculations had indicated that an initial sample of 56, and an adjustment to compensate for attrition of up to 25%, would leave at least 42 subjects (≥21 per condition) and provide statistical power >.95 to detect a moderate size (i.e., .50) between-conditions effect on the primary outcome.
To verify that randomization produced equivalent groups, regression and chi square analyses were conducted on demographic and clinical characteristics, and baseline dependent measures. Intention to treat (ITT) methods were followed for all primary outcome analyses, using the last-observation-carried-forward method. Because this was a preliminary study and we were concerned about the need to balance committing type 1 error against the possibility of dismissing potentially important findings, a minimum alpha level of .05 was used for all analyses. Two-sided statistical tests were used throughout.
Post-treatment effects were evaluated using three types of analyses in accordance with the different types of data. With one exception, in all these analyses the post-treatment outcome score was the dependent variable, with the corresponding baseline outcome score as the covariate. The exception was for the PGIC, which was only assessed at post-treatment, hence the regression model for this outcome did not include a baseline covariate.
The three types of analyses used were as follows: Firstly, for data that met goodness-of-fit normality criteria we employed standard analyses of covariance (ANCOVAs); outcomes in this category included the total scores and subscales of the FIQR and the CPAQ. Secondly, for non-normal data, which included all the remaining questionnaire data and the physical tests data, we utilized bootstrap regression models. Bootstrapping is a nonparametric approach to hypothesis testing that is increasingly recommended for many types of analyses, especially for non-normal data in small clinical samples [13,17,32,60]. Bootstrapping generates an empirical approximation of the sampling distribution of a statistic by repeated random re-sampling from the available data, and uses this distribution to calculate bias corrected and accelerated effect-size estimates and p-values (5000 re-samples were taken for each of these analyses). Thirdly, data from the daily diary measures were analyzed by multilevel random effects modeling, a statistically advanced technique which is advantageous for data sets with many repeated measures [9,14,16,49]. In multilevel models, regression values are independently computed for each patient in the sample, and then aggregated to derive adjusted means (i.e., intercepts) for the average patient.
Three sets of supplementary analyses were also conducted. These included (1) a repeat of primary outcome analyses restricted to subjects who had completed the post-treatment assessment, (2) calculations of the clinical significance of outcomes, and (3) correlational analyses of treatment adherence variables (attendance, and adherence to home yoga practice) relative to outcome measures.
4. Results
4.1. Sample characteristics and equivalence of treatment conditions
There were no significant differences between the yoga and control groups in demographic and clinical characteristics, or baseline dependent measures. The characteristics of the sample are summarized in Table 1. The mean age of the 53 patients in the study was 53.7 years (SD = 11.5), and average time since diagnosis was 11.6 years (SD = 7.2). Participants were primarily Caucasian (92.5%), relatively well educated (58.5%≥college degree) and currently married or in a partnered relationship (69.8%).
Table 1.
Characteristics of the sample, combined and by treatment condition.
| Characteristic | Total Sample (n = 53) | Yoga Condition (n = 25) | Control Condition (n = 28) |
|---|---|---|---|
| n(%)/M(SD) | n(%)/M(SD) | n(%)/M(SD) | |
| Age, years | 53.7 (11.5) | 51.4 (13.7) | 55.8 (8.9) |
| Years since diagnosis | 11.6 (7.2) | 10.6 (7.5) | 12.5 (7.0) |
| Years symptomatic | |||
| 1–5 years | 3 (5.7%) | 2 (8.0%) | 1 (3.6%) |
| 6–10 years | 14 (26.4%) | 6 (24.0%) | 8 (28.6%) |
| >10 years | 36 (67.9%) | 17 (68.0%) | 19 (67.9%) |
| Race/ethnicity | |||
| Caucasian | 49 (92.5%) | 23 (92.0%) | 26 (92.9%) |
| Native American | 3 (5.7%) | 2 (8.0%) | 1 (3.6%) |
| Other | 2 (3.8%) | 1 (4.0%) | 1 (3.6%) |
| Education | |||
| Less than college | 4 (7.5%) | 1 (4.0%) | 3 (10.7%) |
| Some college | 18 (34.0%) | 9 (36.0%) | 9 (32.1%) |
| College degree | 18 (34.0%) | 9 (36.0%) | 9 (32.1%) |
| Graduate studies | 13 (24.5%) | 6 (24.0%) | 7 (25.0%) |
| Marital status | |||
| Married/partnered | 37 (69.8%) | 21 (84.0%) | 16 (57.1%) |
| Divorced/separated | 11 (20.8%) | 3 (12.0%) | 8 (28.6%) |
| Never married | 4 (7.5%) | 1 (4.0%) | 3 (10.7%) |
| Widowed | 1 (1.9%) | 0 (0.0%) | 1 (3.6%) |
| Employment status | |||
| Employed | 22 (41.5%) | 12 (48.0%) | 10 (35.7%) |
4.2. Treatment outcome results
4.2.1. Results for fibromyalgia symptoms and functional deficits
Fibromyalgia symptoms and functional deficits by group are shown in Table 2, along with treatment effect values from both standard and bootstrap regression analyses. Results from analyses evaluating post-treatment group differences on the primary outcome measure, the FIQR Total Score, were significant favoring the yoga condition. Significant FIQR results were also demonstrated for the FIQR Symptoms and Overall Impact subscales, and the individual FIQR items for pain, fatigue, stiffness, depression, poor memory, anxiety, tenderness, poor balance, and environment sensitivity. Additional significant findings favoring the yoga condition were seen in the PGIC estimate of overall improvement in fibromyalgia symptoms, and strength (Timed Chair Rise). Several trends toward greater improvement in the yoga condition were also found, including for the FIQR Function subscale, the Balance-Eyes Open score, and the individual FIQR for poor sleep. The tender point score and tenderness, assessed by the Total Myalgic Score, did not improve.
Table 2.
Fibromyalgia symptoms and functional deficits means and standard deviations at baseline and post-treatment (Post), and treatment effect values from standard (F) or bootstrap (β) regression analyses.
| Variable | Yoga | Control | Effect | F/β | P | ||
|---|---|---|---|---|---|---|---|
|
|
|
||||||
| Baseline Mean (SD) | Post Mean (SD) | Baseline Mean (SD) | Post Mean (SD) | ||||
| FIQR total score | 48.32 (17.47) | 35.49 (17.61) | 49.26 (17.71) | 48.69 (18.88) | 15.28 | F | .0003*** |
| Symptoms (FIQR) | 27.16 (7.59) | 20.08 (8.25) | 26.84 (9.23) | 27.50 (8.43) | 20.52 | F | <.0001*** |
| Function (FIQR) | 12.36 (7.16) | 9.73 (7.52) | 12.85 (6.22) | 12.40 (6.59) | 3.36 | F | .0727^ |
| Overall impact (FIQR) | 8.80 (4.84) | 5.68 (3.65) | 9.57 (5.43) | 8.79 (5.57) | 7.79 | β | .0074** |
| Pain (FIQR) | 5.24 (12.18) | 4.12 (2.05) | 5.11 (2.31) | 5.14 (2.27) | −1.11 | β | .0186** |
| Fatigue (FIQR) | 6.36 (2.18) | 4.76 (2.52) | 6.39 (2.17) | 6.71 (1.61) | −1.94 | β | .0006*** |
| Stiffness (FIQR) | 6.36 (2.00) | 4.72 (1.90) | 5.68 (2.36) | 5.82 (1.79) | −1.40 | β | .0025** |
| Poor sleep (FIQR) | 7.16 (2.43) | 5.72 (3.09) | 5.83 (2.83) | 6.11 (2.90) | −1.31 | β | .0592^ |
| Depression (FIQR) | 2.76 (2.60) | 1.68 (2.01) | 4.21 (2.67) | 3.75 (2.70) | −1.52 | β | .0199* |
| Poor memory (FIQR) | 5.40 (2.57) | 4.20 (2.75) | 5.21 (2.59) | 5.43 (2.52) | −1.35 | β | .0213* |
| Anxiety (FIQR) | 4.20 (3.03) | 2.68 (2.59) | 4.54 (3.13) | 4.14 (2.19) | 1.28 | β | .0407* |
| Tenderness (FIQR) | 6.00 (2.74) | 5.00 (2.97) | 5.32 (2.29) | 5.96 (2.36) | −1.47 | β | .0077** |
| Poor balance (FIQR) | 4.64 (2.16) | 3.12 (2.44) | 4.64 (2.18) | 4.89 (2.54) | −1.77 | β | .0018** |
| Environment sensitivity (FIQR) | 6.20 (2.97) | 4.16 (2.78) | 6.75 (2.46) | 7.04 (2.25) | −2.62 | β | .0001*** |
| Overall improvement (PGIC) | 5.05 (0.72) | 3.69 (80.8) | 32.92 | β | <.0001*** | ||
| Total myalgic score | 38.03 (7.97) | 29.26 (12.19) | 36.44 (7.63) | 29.04 (10.54) | −1.22 | β | .6236 |
| Number of tender points | 17.32 (1.41) | 15.61 (2.45) | 17.07 (1.33) | 15.18 (3.71) | 0.28 | β | .7474 |
| Strength (timed chair rise) | 9.75 (3.01) | 11.88 (4.13) | 10.00 (3.17) | 10.64 (3.63) | 1.52 | β | .0344* |
| Balance-eyes open (SCBT) | 27.76 (4.82) | 30.00 (0.00) | 29.64 (1.89) | 29.29 (3.78) | 1.27 | β | .0881^ |
| Balance-eyes closed (SCBT) | 26.25 (7.72) | 29.60 (2.00) | 24.68 (8.91) | 27.32 (8.99) | 1.52 | β | .2427 |
Bootstrap values are bias corrected and accelerated, based on 5000 bootstrap replications.
p < 0.05.
p < 0.01.
p < 0.001.
p < 0.10 (trend).
4.2.2. Results for pain coping strategies
Table 3 shows pain coping strategies outcomes by group, along with treatment effect values from both standard and bootstrap regression analyses. Significant results indicating greater improvement in the yoga condition were found in pain catastrophizing (CSQ), activities engagement despite pain (CPAQ), and the VMPCI scales for problem solving, positive reappraisal, use of religion, self-isolation, and disengagement. Trends toward greater improvement in the yoga condition were seen in distancing, and confrontation coping strategies (VMPCI).
Table 3.
Pain coping strategies means and standard deviations at baseline and post-treatment (Post), and treatment effect values from standard (F) or bootstrap (β) regression analyses.
| Variable | Yoga | Control | Effect | F/β | P | ||
|---|---|---|---|---|---|---|---|
|
|
|
||||||
| Baseline Mean (SD) | Post Mean (SD) | Baseline Mean (SD) | Post Mean (SD) | ||||
| Acceptance total score (CPAQ) | 70.32 (15.92) | 75.40 (13.10) | 62.61 (19.18) | 65.61 (17.57) | 2.73 | F | .1046 |
| Activity engagement (CPAQ) | 43.32 (11.21) | 46.48 (9.33) | 36.82 (11.48) | 38.43 (10.42) | 3.49 | F | .0465* |
| Pain willingness (CPAQ) | 27.00 (6.56) | 28.92 (7.31) | 25.79 (8.87) | 27.18 (8.35) | 0.32 | F | .5731 |
| Pain catastrophizing (CSQ) | 1.33 (1.07) | 0.94 (0.87) | 1.68 (1.24) | 1.62 (1.03) | −0.47 | β | .0154* |
| Problem solving (VMPCI) | 2.67 (0.87) | 2.78 (0.55) | 2.45 (0.77) | 2.43 (0.51) | 0.26 | β | .0310* |
| Positive reappraisal (VMPCI) | 2.78 (0.76) | 2.833 (0.54) | 2.36 (0.52) | 2.36 (0.49) | 0.27 | β | .0285* |
| Distraction (VMPCI) | 2.81 (0.81) | 2.45 (0.73) | 2.43 (0.71) | 2.41 (0.81) | −0.24 | β | .1331 |
| Use of religion (VMPCI) | 2.14 (1.41) | 2.32 (1.41) | 1.56 (1.38) | 1.54 (1.17) | 0.28 | β | .0281* |
| Use of social support (VMPCI) | 1.77 (0.81) | 1.73 (0.80) | 1.90 (0.84) | 1.89 (0.79) | −0.06 | β | .6496 |
| Distancing (VMPCI) | 2.62 (0.80) | 2.44 (0.69) | 1.87 (0.89) | 2.18 (0.75) | −0.24 | β | .0715^ |
| Self-blame (VMPCI) | 2.86 (0.65) | 2.70 (0.64) | 2.52 (0.67) | 2.58 (0.60) | −0.07 | β | .6197 |
| Self-isolation (VMPCI) | 2.08 (1.16) | 1.51 (0.86) | 2.30 (1.17) | 2.17 (1.00) | −0.53 | β | .0029** |
| Confrontation (VMPCI) | 1.20 (0.98) | 0.92 (0.77) | 1.43 (0.94) | 1.34 (0.81) | −0.28 | β | .0707^ |
| Disengagement (VMPCI) | 1.06 (0.76) | 0.74 (0.59) | 1.14 (0.74) | 1.14 (0.66) | −0.35 | β | .0096** |
Variable Yoga Control Baseline Post Baseline Post Mean (SD) Mean (SD) Mean (SD) Bootstrap values are bias corrected and accelerated, based on 5000 bootstrap replications.
p < 0.05.
p < 0.01.
p < 0.10 (trend).
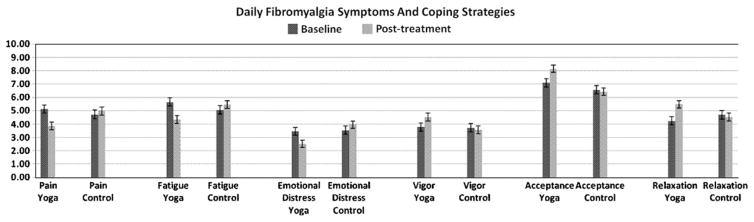
4.2.3. Results for daily diary measures of fibromyalgia symptoms and coping strategies
Fig. 2 displays a graph of the adjusted mean scores produced by multilevel random effects analyses for the six diary outcomes. Results demonstrated significant improvements in the yoga condition in comparison with the control condition in all diary items: symptom scores for pain (β = −1.47, t = −5.90, p < .0001), fatigue (β = −1.68, t = −6.23, p <.0001), emotional distress (β = −1.34, t = −4.92, p < .0001), and vigor (β = 0.92, t = 3.62, p = .0005); and success at acceptance (β = 1.20, t = 5.10, p < .0001) and relaxation (β = 1.38, t = 4.36, p < .0001) coping strategies.
Fig. 2.
Daily fibromyalgia symptoms and coping strategies scores (0–10 scales) at baseline and post-treatment in the yoga and control conditions (all p < .001). Values are multilevel random effects for adjusted means, with error bars showing standard errors.
4.3. Supplementary analyses results
4.3.1. Completers outcomes analyses
A repeat of primary outcome analyses restricted to subjects who had completed the post-treatment assessment produced results that were similar to those obtained from ITT analyses, with parameters indicating slightly greater effects favoring the yoga condition. Two outcomes that had demonstrated trends toward significance in the ITT data reached significant levels in the completers analyses: poor sleep (β = −0.57, p = .04) and confrontational coping (β = −0.35, p = .04).
4.3.2. Clinical significance of changes
We examined data from completers in the yoga condition to determine whether observed improvements met criteria for clinically significant changes. For the primary outcome, the FIQR Total Score, the observed 31.4% reduction in this measure was more than double the 14% minimal clinically significant difference criterion recommended by Bennett et al. [6], with 55.6% of yoga subjects reaching ≥30% reduction in this measure [24]. The FIQR item for pain was reduced 24.1%, with 50.0% of yoga subjects recording ≥30% reduction in pain [24].
All the remaining FIQR subscales and individual symptom items were also considerably reduced in the yoga subjects: Function subscale, 24.8%; Impact subscale, 40.0%; Symptoms subscale, 29.8%; fatigue, 29.9%; tenderness, 29.1%; poor sleep, 23.9%; depression, 41.5%; poor memory, 25.2%; anxiety, 42.2%; tenderness, 18.9%; poor balance, 37.6%; and environmental sensitivity, 36.4%. Means of daily diary symptom scores were similarly reduced: pain, 25.9%; fatigue, 23.6%; emotional distress, 30.1%. All the above improvements range between minimally to moderately important clinical changes according to the new consensus guidelines published by the Initiative on Methods, Measurement, and Pain Assessment in Clinical Trials (IMMPACT), an international group of pain researchers [23,24].
Although no clear consensus yet exists on what constitutes clinically important changes in measures of coping, if we transpose the IMMPACT group’s gauge of one-half of the standard deviation of a mood scale as clinically significant, then several of the coping improvements in the yoga subjects may also be considered clinically significant [24]. Qualifying by this criterion would be changes in pain catastrophizing, disengagement, acceptance (from diaries), and relaxation (from diaries). Lastly, considering the PGIC measure of overall improvement in fibromyalgia symptoms [24], 4.5% in the yoga condition vs. 0.0% in the control reported being “very much better”, 9.1% in the yoga condition vs. 0.0% in the control were “much better”, 77.3 in the yoga condition vs. 19.2% in the control were “a little better”, 4.5% in the yoga condition vs. 38.5% in the control reported “no change”, 4.5% in the yoga condition vs. 34.6% in the control were “a little worse”, and 0.0% in the yoga condition vs. 7.7% in the control were “much worse”.
4.3.3. Relationship of attendance and yoga home practice rates to outcomes
To examine associations between treatment adherence variables (attendance, and adherence to home yoga practice) and outcome measures, first residual scores were calculated for each outcome (the post-treatment score regressed on the baseline score), which were then entered into correlational analyses. These tests produced several significant findings.
Attendance rates
The average attendance among yoga condition participants was seven out of eight classes (range 4–8). Attendance rates were significantly correlated with the FIQR fatigue residual score, such that higher attendance was associated with less fatigue (r[25] = −0.40, p < .05). There were trends for associations with three other outcomes in a similar manner, such that higher attendance was related to improvements in the FIQR Total Score (r[25] = −0.34, p = .09), the FIQR Symptoms subscale (r[25] = −0.35, p = .08), and strength (r[24] = 0.36, p = .08).
Home yoga practice rates
We had two gauges of home practice: First, during the intervention yoga participants kept daily records of minutes spent doing posture, meditation and breathing exercise, and these records were collected each week during class; and second, when completing their post-treatment online daily diary measures, yoga subjects also reported on their practice rates for 7 days. These two assessments of practice rates were highly correlated (0.87). Because the intervention practice records covered a much more extensive period (7 vs. 1 week), herein we are reporting only on correlations between outcome residual scores and the intervention practice rates.
Average daily home practice rates were as follows: total practice = 40 min (range 11–97), postures = 19 min (range 4–57), meditation = 13 min (range 2–29), and breathing exercises = 8 min (range 2–16). Average total practice rates were significantly correlated with the residual scores of several outcomes, such that more practice was associated with greater overall improvement in symptoms (PGIC; r[22] = 0.50, p = .02), and more improvement in the FIQR fatigue score (r[25] = −0.55, p = .01) and relaxation (from diaries; r[25] = 0.44, p = .03). There was also a trend for greater improvement in the FIQR Poor Memory score to be correlated with higher total practice rates (r[25] = −0.35, p = .09).
The practice rates for both postures and meditation were separately correlated with these same outcomes in a very similar manner, with only slight variations in the parameter values. The practice rate for breathing exercises was significantly correlated only with PGIC scores.
5. Discussion
This study examined the impact of a yoga intervention on a sample of women with FM. Our findings provide preliminary evidence, based on various types of measures (standardized questionnaires, physical tests, daily diaries) that the intervention may be helpful for improving a wide range of FM symptoms and functional deficits, including pain, fatigue, stiffness, poor sleep, depression, poor memory, anxiety, tenderness, poor balance, environment sensitivity, vigor, and limited strength. Moreover, a majority of the improvements seen in this study qualified as clinically significant changes. Interestingly, whereas the subjects reported a marked improvement in tenderness, this was not associated with a significant improvement in the Total Myalgic Score. This paradoxical result has been noted in many other FM treatment studies and warrants further exploration.
In addition, the results suggested the yoga intervention led to a beneficial shift in how patients cope with pain, including greater use of adaptive pain coping strategies (i.e., problem solving, positive reappraisal, use of religion, activity engagement despite pain, acceptance, relaxation) and less use of maladaptive strategies (i.e., catastrophizing, self-isolation, disengagement, confrontation). These changes may seem surprising, given that the coping strategies employed in the intervention were drawn from the yoga tradition and differed markedly from standard CBT coping skills. One implication of these findings is that the promotion of adaptive coping does not rely on a circumscribed set of skills that “teach to the test”, but rather may be produced by a wide variety of approaches.
Although yoga has been practiced for millennia, only recently have researchers begun to demonstrate yoga’s effects on persons suffering from persistent pain, including those with chronic low back pain, osteoarthritis, carpal tunnel syndrome, kidney failure, and cancer-related pain [14,15,26,27,50,63,65]. The present study was preceded by an earlier trial of an 8 week “Relaxing Yoga” intervention for FM [22]. That study reported improvements in overall symptoms and pain, the magnitude of which were very similar to our findings on these outcomes. However, conclusions from the earlier study were restricted by failure to follow intention-to-treat methods, the narrow range of outcomes assessed, the very small sample (N = 33), and difficulties with retention (18% attrition). Another limitation of this earlier study was the yoga program’s exclusive targeting of relaxation. Reviews of coping skills treatments for FM indicate that relaxation training is more effective when included in a broader approach incorporating elements such as cognitive coping techniques and educational components [4,51,56,57].
The intention of the yoga program we employed was to fulfill the need for both exercise and coping skills training as effective counterparts to pharmacotherapy for FM [5,19,28]. Recent reviews of exercise trials concur that aerobic exercise and also strength training usually improves some FM symptoms and physical functioning, but rarely shows effects on pain or mood [10,11,36]. In contrast, reviews of FM coping skills trials have concluded that such treatments usually show mild to moderate post-treatment effects on pain, mood, and disability [4,51,56,57]. However, several reviews have emphasized that the best results have been produced by multimodal interventions that combine both exercise and coping skills training [4,51,56,57].
Although multimodal in nature, the Yoga of Awareness program stands in contrast to previous multimodal interventions with FM patients, in that it integrates a wide spectrum of yoga-based techniques – postures, mindfulness meditation, breathing exercises, application of yogic principles to optimal coping, and group discussions. Nonetheless, the results of the present study compare favorably to previous multimodal trials both in terms of the range (FM symptoms, physical functioning, pain, mood, coping skills) and magnitude of improvements observed. For example, Mannerkorpi et al. studied 58 patients randomly assigned to a 6-month program combining pool exercise with CBT-based stress management and relaxation skills, or to standard care control [40]. Post-treatment analyses revealed mostly modest but statistically significant changes favoring the intervention group in the FIQ Total Score (13.6% reduction in the treatment group vs. 31.4% in the current study), the Function subscale (15.8% vs. 24.8% in the current study) and the FIQ item score for anxiety (23.5% vs. 42.2% in the current study). Other scales showed reductions in pain (9.5% vs. 25.9% from diaries in the current study), emotional distress (9.7% vs. 30.1% from diaries in the current study), depression (8.6% vs. 41.5% for the FIQR depression item in this study) and in quality of life. Improvements in a timed walking test and in grip strength were also reported.
The question of what processes can account for changes observed in a clinical trial is critical to understanding the ultimate utility of an intervention and for advancing science. We had several reasons to expect that this intervention may reduce symptoms in women with FM. First, yoga cultivates a healthy acceptance of and willingness to learn from pain and other stressful experiences. The important role of acceptance in decreasing the emotional distress and sympathetic activation associated with pain and other unpleasant symptomatology has received increased research focus and clinical attention [29,41,59]. Second, previous data indicate that yoga produces invigorating effects on mental and physical energies in a manner similar to aerobic exercise, and thereby may improve the fatigue that plagues FM patients [8,14,15,20]. Third, research has shown that yoga produces the relaxation response (an integrated set of changes that includes increased breath volume, decreased heart rate, etc.) [55,58]. Since autonomic dysregulation has been implicated in the generation of FM symptoms, researchers have posited that psychophysiologically soothing techniques are likely to promote the alleviation of FM symptoms such as pain and emotional distress [30,62]. Lastly, studies have demonstrated that yoga promotes both balance [31,38] and strength [45] – two functional deficits targeted by FM exercise interventions [36].
We found some empirical support in this investigation for all of these therapeutic processes. However, much more work is needed to determine which of these mechanisms may have mediated patients’ improvements, what biological changes may underlie yoga-related changes in FM symptoms, and most importantly, to rule out mere attention or placebo response as the intervention’s primary therapeutic processes [2,44].
Accrual and retention (91%) in this study were good [36]. Attendance at classes was also good (average of seven out of eight sessions), as was adherence to home yoga practice (average total of 40 min per day). Notably, those who practiced yoga more had better outcomes on several measures. Patients’ anecdotal reports also suggested that they found the yoga training very helpful for managing their symptoms. For example, one patient remarked that “I did the practice twice in one day and that evening, I actually fell asleep without pain. I slept all the way through the night. I couldn’t remember the last time I had slept through the night”. Another commented that “I am learning how to be my own best friend. When I rest in simply being, I can let the anxiety wave wash through and learn how to ride it”.
Major limitations of our study should be noted. The generalizability of these preliminary findings is restricted by the small sample, the absence of follow-up, and over-reliance on self-report data. Moreover, as stated above, any conclusions are especially limited by the lack of an attention placebo or active control condition [2,44]. This same limitation applies however to most of the multimodal exercise-and-coping skills FM trials that have been published, which likewise used either wait-list or standard care controls [57]. Inclusion of an appropriate control condition, preferably an active treatment condition, is crucial for a larger, more thorough study of yoga for FM. Further methodological improvements for such a study could include follow-up assessments (e.g., 6 months post-treatment), analyses of potential mechanisms of therapeutic effects – including both physiological (e.g., changes in cerebral pain processing as indicated by quantitative sensory tests [54]) and psychological mechanisms (e.g., mindfulness, acceptance, relaxation), analyses of moderators of treatment outcome (e.g., is yoga more helpful for patients with lower vs. greater body mass index), and of the types (e.g., postures vs. meditation) and doses of yoga practice needed to achieve adequate symptom reductions.
In conclusion, the findings of this pilot study provide promising preliminary support for the beneficial effects of yoga in patients with FM. The improvements documented herein are important enough to warrant further study.
Acknowledgments
This work was supported by a grant from the Oregon Health & Science University Medical Research Foundation and resources supplied by the Fibromyalgia Information Foundation. The authors wish to thank Janice Hoffman, Rogelyn Kwock, and Rebecca Ross for their valuable assistance in conducting this study.
Footnotes
Conflict of interest
The present manuscript is submitted exclusively to Pain and is not under consideration in any other journal. There are no financial relationships that might lead to a conflict of interest.
References
- 1.Affleck G, Urrows S, Tennen H, Higgins P, Abeles M. Sequential daily relations of sleep, pain intensity, and attention to pain among women with fibromyalgia. Pain. 1996;68:363–8. doi: 10.1016/s0304-3959(96)03226-5. [DOI] [PubMed] [Google Scholar]
- 2.Arias AJ, Steinberg K, Banga A, Trestman RL. Systematic review of the efficacy of meditation techniques as treatments for medical illness. J Altern Complement Med. 2006;12:817–32. doi: 10.1089/acm.2006.12.817. [DOI] [PubMed] [Google Scholar]
- 3.Bennett R. The Fibromyalgia Impact Questionnaire (FIQ): a review of its development, current version, operating characteristics and uses. Clin Exp Rheumatol. 2005;23:S154–62. [PubMed] [Google Scholar]
- 4.Bennett R, Nelson D. Cognitive behavioral therapy for fibromyalgia. Nature Clin Pract Rheumatol. 2006;2:416–24. doi: 10.1038/ncprheum0245. [DOI] [PubMed] [Google Scholar]
- 5.Bennett RM. Rational management of fibromyalgia. Rheum Dis Clin North Am. 2002;28:xiii–xv. [PubMed] [Google Scholar]
- 6.Bennett RM, Bushmakin AG, Cappelleri JC, Zlateva G, Sadosky AB. Minimal clinically important difference in the fibromyalgia impact questionnaire. J Rheumatol. 2009;36:1304–11. doi: 10.3899/jrheum.081090. [DOI] [PubMed] [Google Scholar]
- 7.Bennett RM, Friend R, Jones KD, Ward R, Han BK, Ross RL. The revised Fibromyalgia Impact Questionnaire (FIQR): validation and psychometric properties. Arthritis Res Therapy. 2009;11:R120. doi: 10.1186/ar2783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Berger BG, Owen DR. Mood alteration with yoga and swimming: aerobic exercise may not be necessary. Percept Mot Skills. 1992;75:1331–43. doi: 10.2466/pms.1992.75.3f.1331. [DOI] [PubMed] [Google Scholar]
- 9.Bolger N, Davis A, Rafaeli E. Diary methods: capturing life as it is lived. Annu Rev Psychol. 2003;54:579–616. doi: 10.1146/annurev.psych.54.101601.145030. [DOI] [PubMed] [Google Scholar]
- 10.Brosseau L, Wells GA, Tugwell P, Egan M, Wilson KG, Dubouloz C-J, Casimiro L, Robinson VA, McGowan J, Busch A, Poitras S, Moldofsky H, Harth M, Finestone HM, Nielson W, Haines-Wangda A, Russell-Doreleyers M, Lambert K, Marshall AD, Veilleux L, Ottawa Panel M. Ottawa Panel evidence-based clinical practice guidelines for aerobic fitness exercises in the management of fibromyalgia: part 1. Phys Ther. 2008;88:857–71. doi: 10.2522/ptj.20070200. [DOI] [PubMed] [Google Scholar]
- 11.Busch AJ, Barber KAR, Overend TJ, Peloso PMJ, Schachter CL. Exercise for treating fibromyalgia syndrome. Cochrane database of systematic reviews. 2007:CD003786. doi: 10.1002/14651858.CD003786.pub2. [DOI] [PMC free article] [PubMed]
- 12.Carson JW, Carson KM, Gil KM, Baucom DH. Mindfulness-based relationship enhancement. Behav Therapy. 2004;35:471–94. [Google Scholar]
- 13.Carson JW, Carson KM, Gil KM, Baucom DH. Self-expansion as a mediator of relationship improvements in a mindfulness intervention. J Marriage Family Therapy. 2007;33:517–28. doi: 10.1111/j.1752-0606.2007.00035.x. [DOI] [PubMed] [Google Scholar]
- 14.Carson JW, Carson KM, Porter LS, Keefe FJ, Seewaldt VL. Yoga of Awareness program for menopausal symptoms in breast cancer survivors: Results from a randomized trial. Supportive care in cancer. 2009 doi: 10.1007/s00520-009-0587-5. [DOI] [PubMed] [Google Scholar]
- 15.Carson JW, Carson KM, Porter LS, Keefe FJ, Shaw H, Miller JM. Yoga for women with metastatic breast cancer: results from a pilot study. J Pain Symptom Manage. 2007;33:331–41. doi: 10.1016/j.jpainsymman.2006.08.009. [DOI] [PubMed] [Google Scholar]
- 16.Carson JW, Keefe FJ, Affleck G, Rumble ME, Caldwell DS, Beaupre PM, Kashikar-Zuck S, Sandstrom M, Weisberg JN. A comparison of conventional pain coping skills training and pain coping skills training with a maintenance training component: a daily diary analysis of short- and long-term treatment effects. J Pain. 2006;7:615–25. doi: 10.1016/j.jpain.2006.02.008. [DOI] [PubMed] [Google Scholar]
- 17.Carson JW, Keefe FJ, Lowry KP, Porter LS, Goli V, Fras AM. Conflict about expressing emotions and chronic low back pain: associations with pain and anger. J Pain. 2007;8:405–11. doi: 10.1016/j.jpain.2006.11.004. [DOI] [PubMed] [Google Scholar]
- 18.Carson JW, Keefe FJ, Lynch TR, Carson KM, Goli V, Fras AM, Thorp SR. Loving-kindness meditation for chronic low back pain: results from a pilot trial. J Holistic Nurs. 2005;23:1–18. doi: 10.1177/0898010105277651. [DOI] [PubMed] [Google Scholar]
- 19.Carville SF, Arendt-Nielsen S, Bliddal H, Blotman F, Branco JC, Buskila D, Da Silva JAP, Danneskiold-Samsoe B, Dincer F, Henriksson C, Henriksson KG, Kosek E, Longley K, McCarthy GM, Perrot S, Puszczewicz M, Sarzi-Puttini P, Silman A, Spath M, Choy EH, Eular EULAR evidence-based recommendations for the management of fibromyalgia syndrome. Ann Rheum Dis. 2008;67:536–41. doi: 10.1136/ard.2007.071522. [DOI] [PubMed] [Google Scholar]
- 20.Cohen L, Warneke C, Fouladi RT, Rodriguez MA, Chaoul-Reich A. Psychological adjustment and sleep quality in a randomized controlled trial of the effects of a Tibetan yoga intervention in patients with lymphoma. Cancer. 2004;100:2253–60. doi: 10.1002/cncr.20236. [DOI] [PubMed] [Google Scholar]
- 21.Cope S. The wisdom of yoga. New York: Bantam Books; 2006. [Google Scholar]
- 22.da Silva GD, Lorenzi-Filho G, Lage LV. Effects of yoga and the addition of Tui Na in patients with fibromyalgia. J Altern Complement Med. 2007;13:1107–13. doi: 10.1089/acm.2007.0615. [DOI] [PubMed] [Google Scholar]
- 23.Dworkin RH, Turk DC, McDermott MP, Peirce-Sandner S, Burke LB, Cowan P, Farrar JT, Hertz S, Raja SN, Rappaport BA, Rauschkolb C, Sampaio C. Interpreting the clinical importance of group differences in chronic pain clinical trials: IMMPACT recommendations. Pain. 2009;146:238–44. doi: 10.1016/j.pain.2009.08.019. [DOI] [PubMed] [Google Scholar]
- 24.Dworkin RH, Turk DC, Wyrwich KW, Beaton D, Cleeland CS, Farrar JT, Haythornthwaite JA, Jensen MP, Kerns RD, Ader DN, Brandenburg N, Burke LB, Cella D, Chandler J, Cowan P, Dimitrova R, Dionne R, Hertz S, Jadad AR, Katz NP, Kehlet H, Kramer LD, Manning DC, McCormick C, McDermott MP, McQuay HJ, Patel S, Porter L, Quessy S, Rappaport BA, Rauschkolb C, Revicki DA, Rothman M, Schmader KE, Stacey BR, Stauffer JW, von Stein T, White RE, Witter J, Zavisic S. Interpreting the clinical importance of treatment outcomes in chronic pain clinical trials: IMMPACT recommendations. J Pain. 2008;9:105–21. doi: 10.1016/j.jpain.2007.09.005. [DOI] [PubMed] [Google Scholar]
- 25.Fors EA, Sexton H, Gotestam KG. The effect of guided imagery and amitriptyline on daily fibromyalgia pain: a prospective, randomized, controlled trial. J Psychiatr Res. 2002;36:179–87. doi: 10.1016/s0022-3956(02)00003-1. [DOI] [PubMed] [Google Scholar]
- 26.Garfinkel MS, Schumacher HR, Jr, Husain A, Levy M, Reshetar RA, Full N, Schumacher HRJ, Husain A, Levy M, Reshetar RA. Evaluation of a yoga based regimen for treatment of osteoarthritis of the hands. J Rheumatol. 1994;21:2341–3. [PubMed] [Google Scholar]
- 27.Garfinkel MS, Singhal A, Katz WA, Allan DA, Reshetar R, Schumacher HR, Jr, Full N, Singhal A, Katz WA, Allan DA, Reshetar R, Schumacher HRJ. Yoga-based intervention for carpal tunnel syndrome: a randomized trial. JAMA. 1998;280:1601–3. doi: 10.1001/jama.280.18.1601. [DOI] [PubMed] [Google Scholar]
- 28.Goldenberg DL, Burckhardt C, Crofford L. Management of fibromyalgia syndrome. JAMA. 2004;292:2388–95. doi: 10.1001/jama.292.19.2388. [DOI] [PubMed] [Google Scholar]
- 29.Gross JJ. Emotion regulation: affective, cognitive, and social consequences. Psychophysiology. 2002;39:281–91. doi: 10.1017/s0048577201393198. [DOI] [PubMed] [Google Scholar]
- 30.Hadhazy VA, Ezzo J, Creamer P, Berman BM. Mind-body therapies for the treatment of fibromyalgia. A systematic review. J Rheumatol. 2000;27:2911–8. [PubMed] [Google Scholar]
- 31.Hart CEF, Tracy BL. Yoga as steadiness training: effects on motor variability in young adults. J Strength Condit Res. 2008;22:1659–69. doi: 10.1519/JSC.0b013e31818200dd. [DOI] [PubMed] [Google Scholar]
- 32.Henderson AR. The bootstrap: a technique for data-driven statistics. Using computer-intensive analyses to explore experimental data. Clin Chim Acta. 2005;359:1–26. doi: 10.1016/j.cccn.2005.04.002. [DOI] [PubMed] [Google Scholar]
- 33.Holdcraft LC, Assefi N, Buchwald D. Complementary and alternative medicine in fibromyalgia and related syndromes. Best Practice Res in Clin Rheumatol. 2003;17:667–83. doi: 10.1016/s1521-6942(03)00037-8. [DOI] [PubMed] [Google Scholar]
- 34.Horak F, Frank J, Wrisley D. The Balance Evaluation Systems Test (BESTest): development of a clinical tool to differentiate types of balance deficits. Physical therapy. 2009 doi: 10.2522/ptj.20080071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hsu MC, Schubiner H, Lumley MA, Stracks JS, Clauw DJ, Williams DA. Sustained pain reduction through affective self-awareness in fibromyalgia: a randomized controlled trial. J Gen Internal Med. 2010 doi: 10.1007/s11606-010-1418-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jones KD, Adams D, Winters-Stone K, Burckhardt CS. A comprehensive review of 46 exercise treatment studies in fibromyalgia (1988–2005) Health Qual Life Outcomes. 2006;4:67. doi: 10.1186/1477-7525-4-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jones KD, Clark SR. Individualizing the exercise prescription for persons with fibromyalgia. Rheum Dis Clin North Am. 2002;28:419–36. doi: 10.1016/s0889-857x(01)00010-2. [DOI] [PubMed] [Google Scholar]
- 38.Krishnamurthy M, Telles S. Effects of Yoga and an Ayurveda preparation on gait, balance and mobility in older persons. Med Sci Monitor. 2007;13:LE19–20. [PubMed] [Google Scholar]
- 39.Krishnamurti J. Choiceless awareness. Ojai, CA: Krishnamurti Foundation; 1992. [Google Scholar]
- 40.Mannerkorpi K, Nyberg B, Ahlmen M, Ekdahl C. Pool exercise combined with an education program for patients with fibromyalgia syndrome. A prospective, randomized study. J Rheumatol. 2000;27:2473–81. [PubMed] [Google Scholar]
- 41.McCracken LM, Carson JW, Eccleston C, Keefe FJ. Acceptance and change in the context of chronic pain. Pain. 2004;109:4–7. doi: 10.1016/j.pain.2004.02.006. [DOI] [PubMed] [Google Scholar]
- 42.McCracken LM, Vowles KE, Eccleston C. Acceptance of chronic pain: component analysis and a revised assessment method. Pain. 2004;107:159–66. doi: 10.1016/j.pain.2003.10.012. [DOI] [PubMed] [Google Scholar]
- 43.Nisargadatta M. I am that. Durham NC: Acorn Press; 1985. [Google Scholar]
- 44.Ospina MB, Bond K, Karkhaneh M, Buscemi N, Dryden DM, Barnes V, Carlson LE, Dusek JA, Shannahoff-Khalsa D. Clinical trials of meditation practices in health care: characteristics and quality. J Altern Complement Med. 2008;14:1199–213. doi: 10.1089/acm.2008.0307. [DOI] [PubMed] [Google Scholar]
- 45.Raub JA, Full N. Psychophysiologic effects of Hatha Yoga on musculoskeletal and cardiopulmonary function: a literature review. J Altern Complement Med. 2002;8:797–812. doi: 10.1089/10755530260511810. [DOI] [PubMed] [Google Scholar]
- 46.Rikli RE, Jones CJ. Senior fitness test manual. Champaign, IL: Human Kinetics; 2001. [Google Scholar]
- 47.Rosenstiel AK, Keefe FJ. The use of coping strategies in chronic low back pain patients: relationship to patient characteristics and current adjustment. Pain. 1983;17:33–44. doi: 10.1016/0304-3959(83)90125-2. [DOI] [PubMed] [Google Scholar]
- 48.Russell IJ, Mease PJ, Smith TR, Kajdasz DK, Wohlreich MM, Detke MJ, Walker DJ, Chappell AS, Arnold LM. Efficacy and safety of duloxetine for treatment of fibromyalgia in patients with or without major depressive disorder: results from a 6-month, randomized, double-blind, placebo-controlled, fixed-dose trial. Pain. 2008;136:432–44. doi: 10.1016/j.pain.2008.02.024. [DOI] [PubMed] [Google Scholar]
- 49.Schwartz JE, Stone AA. Strategies for analyzing ecological momentary assessment data. Health Psychol. 1998;17:6–16. doi: 10.1037//0278-6133.17.1.6. [DOI] [PubMed] [Google Scholar]
- 50.Sherman KJ, Cherkin DC, Erro J, Miglioretti DL, Deyo RA. Comparing yoga, exercise, and a self-care book for chronic low back pain: a randomized, controlled trial. Ann Intern Med. 2005;143:849–56. doi: 10.7326/0003-4819-143-12-200512200-00003. [DOI] [PubMed] [Google Scholar]
- 51.Sim J, Adams N. Systematic review of randomized controlled trials of non-pharmacological interventions for fibromyalgia. Clin J Pain. 2002;18:324–36. doi: 10.1097/00002508-200209000-00008. [DOI] [PubMed] [Google Scholar]
- 52.Sinclair VG, Wallston KA, Dwyer KA, Blackburn DS, Fuchs H. Effects of a cognitive-behavioral intervention for women with rheumatoid arthritis. Res Nurs Health. 1998;21:315–26. doi: 10.1002/(sici)1098-240x(199808)21:4<315::aid-nur4>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 53.Smith CA, Wallston KA, Dwyer KA, Dowdy SW. Beyond good and bad coping: a multidimensional examination of coping with pain in persons with rheumatoid arthritis. Ann Behav Med. 1997;19:11–21. doi: 10.1007/BF02883422. [DOI] [PubMed] [Google Scholar]
- 54.Staud R, Robinson ME, Price DD. Isometric exercise has opposite effects on central pain mechanisms in fibromyalgia patients compared to normal controls. Pain. 2005;118:176–84. doi: 10.1016/j.pain.2005.08.007. [DOI] [PubMed] [Google Scholar]
- 55.Telles S, Naveen KV. Yoga for rehabilitation: an overview. Ind J Med Sci. 1997;51:123–7. [PubMed] [Google Scholar]
- 56.Thieme K, Gracely RH. Are psychological treatments effective for fibromyalgia pain? Curr Rheumatol Rep. 2009;11:443–50. doi: 10.1007/s11926-009-0065-6. [DOI] [PubMed] [Google Scholar]
- 57.van Koulil S, Effting M, Kraaimaat FW, van Lankveld W, van Helmond T, Cats H, van Riel PLCM, de Jong AJL, Haverman JF, Evers AWM. Cognitive-behavioural therapies and exercise programmes for patients with fibromyalgia: state of the art and future directions. Ann Rheum Dis. 2007;66:571–81. doi: 10.1136/ard.2006.054692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Vempati RP, Telles S. Yoga-based guided relaxation reduces sympathetic activity judged from baseline levels. Psychol Rep. 2002;90:487–94. doi: 10.2466/pr0.2002.90.2.487. [DOI] [PubMed] [Google Scholar]
- 59.Vowles KE, McCracken LM, Eccleston C. Patient functioning and catastrophizing in chronic pain: the mediating effects of acceptance. Health Psychol. 2008;27:S136–43. doi: 10.1037/0278-6133.27.2(Suppl.).S136. [DOI] [PubMed] [Google Scholar]
- 60.Walters SJ, Campbell MJ. The use of bootstrap methods for analysing health-related quality of life outcomes (particularly the SF-36) Health Qual Life Outcomes. 2004;2:70. doi: 10.1186/1477-7525-2-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.White KP, Harth M. Classification, epidemiology, and natural history of fibromyalgia. Curr Pain Headache Rep. 2001;5:320–9. doi: 10.1007/s11916-001-0021-2. [DOI] [PubMed] [Google Scholar]
- 62.Williams DA. Psychological and behavioural therapies in fibromyalgia and related syndromes. Best Pract Res Clin Rheumatol. 2003;17:649–65. doi: 10.1016/s1521-6942(03)00034-2. [DOI] [PubMed] [Google Scholar]
- 63.Williams KA, Petronis J, Smith D, Goodrich D, Wu J, Ravi N, Doyle EJ, Jr, Gregory JR, Munoz KM, Gross R, Steinberg L. Effect of Iyengar yoga therapy for chronic low back pain. Pain. 2005;115:107–17. doi: 10.1016/j.pain.2005.02.016. [DOI] [PubMed] [Google Scholar]
- 64.Wolfe F, Smythe HA, Yunus MB, Bennett RM, Bombardier C, Goldenberg DL, Tugwell P, Campbell SM, Abeles M, Clark P. The American college of rheumatology 1990 criteria for the classification of fibromyalgia. Report of the Multicenter Criteria Committee. Arthritis Rheum. 1990;33:160–72. doi: 10.1002/art.1780330203. [DOI] [PubMed] [Google Scholar]
- 65.Yurtkuran M, Alp A, Yurtkuran M, Dilek K. A modified yoga-based exercise program in hemodialysis patients: a randomized controlled study. Complement Ther Med. 2007;15:164–71. doi: 10.1016/j.ctim.2006.06.008. [DOI] [PubMed] [Google Scholar]