Abstract
Over 20% of patients with cirrhosis are nonadherent with hepatocellular carcinoma (HCC) surveillance recommendations; however, few studies have evaluated the impact of patient-level factors on surveillance receipt. We characterized the association between HCC surveillance receipt and patient knowledge, attitudes, and perceived barriers in a racially diverse and socioeconomically disadvantaged cohort of patients with cirrhosis. Patients with cirrhosis followed at a large urban hospital were invited to complete a survey about HCC surveillance between August 2014 and December 2015. Multivariable logistic regression was performed to identify factors associated with HCC surveillance receipt during the 12-month period preceding and 6-month period after survey administration. We achieved a response rate of 71.8% (n = 541 of 753). Patients demonstrated high levels of HCC-related knowledge (summary score, 77.7%); however, 48.6% believed that eating a healthy diet precluded the need for HCC surveillance, and 34.0% believed that HCC surveillance was not necessary if they had a normal physical exam and/or lacked clinical symptoms. Patients expressed worry about developing and dying from HCC, but nearly half (49.9%) of patients reported barriers to receiving HCC surveillance, including difficulty with the scheduling process (30.5%), costs of surveillance testing (25.3%), and transportation difficulties (17.3%). HCC surveillance receipt was significantly higher in patients who knew cirrhosis is a risk factor for developing HCC (odds ratio [OR], 3.09; 95% confidence interval [CI], 1.25–7.62) and significantly lower in those reporting barriers to surveillance (OR, 0.42; 95% CI, 0.25–0.70).
Conclusion
Patients with cirrhosis are knowledgeable and interested in HCC surveillance; however, patient-reported barriers are associated with lower surveillance rates in clinical practice and represent potential intervention targets to improve HCC surveillance effectiveness.
Hepatocellular carcinoma (HCC) is the third-leading cause of cancer-related death worldwide and one of the leading causes of death in patients with cirrhosis.(1) Prognosis for patients with HCC depends on tumor stage at diagnosis, with curative options only available for patients diagnosed at an early stage.(2) Despite improvement in overall survival over time, most patients continue to be diagnosed at advanced stages and 5-year survival rates remain below 20%.(3) Racial/ethnic minorities have higher rates of late-stage tumor detection as well as significantly lower stage-adjusted survival rates than non-Hispanic Caucasians.(4,5)
Poor HCC clinical outcomes are, in part, attributed to underuse of surveillance among at-risk patients with cirrhosis. Several cohort studies have demonstrated that HCC surveillance is associated with higher rates of early tumor detection, curative treatment receipt, and overall survival(6); however, fewer than 20% of patients with cirrhosis in the United States undergo HCC surveillance.(7) HCC surveillance rates are even lower among racial-ethnic minorities and patients of low socioeconomic status (SES), likely related to a combination of medical, socioeconomic, and cultural issues.(8)
Although provider recommendation is reported to be a strong predictor for HCC surveillance,(9) patient-level factors may also play an important role in surveillance underuse. In prospective cohort studies, nearly 1 in 5 patients were nonadherent with provider recommendations for HCC surveillance.(10,11) The cancer-screening literature has applied theoretical models of behavior change and demonstrated that patients’ poor knowledge, negative attitudes, or perceived barriers to cancer screening may be associated with lower screening rates.(12,13) However, most studies evaluating HCC surveillance correlates have primarily focused on patient sociodemographic and clinical characteristics.(7,14) The effect of theory-based, patient-reported psychosocial factors on HCC surveillance completion has not been quantified. A better understanding of patient knowledge, attitudes, and barriers, particularly among low-income minorities, is crucial to develop and implement effective interventions to improve HCC surveillance rates.(15) Therefore, the aim of our study was to characterize patient-level knowledge, attitudes, and barriers regarding HCC surveillance and their association with receipt of HCC surveillance in a racially diverse and socioeconomically disadvantaged cohort of patients with cirrhosis.
Patients and Methods
STUDY POPULATION
Electronic medical records of patients being observed at Parkland Health and Hospital System (Parkland), the safety net health system of Dallas County, were screened to identify adult patients with cirrhosis. Parkland is an integrated health care system including 12 primary care provider clinics, outpatient hepatology and multidisciplinary liver tumor clinics, and a tertiary hospital—all sharing a single electronic medical record (EMR) system.
Patients were initially identified using a validated set of International Classification of Diseases, Ninth Revision codes for cirrhosis (571.2, 571.5) or cirrhosis complications (456.0, 456.1, 456.2, 456.21, 567.23, 572.2, 572.3, and 572.4).(16) Presence of cirrhosis was then confirmed by chart review before survey administration by one of the authors (A.S., M.K., or J.P.), with diagnosis based on consistent histology, noninvasive markers of fibrosis, including FibroSure, or imaging showing a cirrhotic-appearing liver with associated signs of portal hypertension, including splenomegaly, varices, or thrombocytopenia. We excluded patients with (1) grade 3–4 encephalopathy, (2) patient self-reported low literacy precluding survey completion, (3) language other than English or Spanish, (4) personal history of HCC, or (5) history of liver transplantation (LT). The study was approved by the Institutional Review Board of UT Southwestern Medical Center (Dallas, TX).
SURVEY DEVELOPMENT AND ADMINISTRATION
Eligible patients were recruited to complete the survey at the time of a clinic appointment or by telephone between August 2014 and December 2015. A convenience sample of patients were approached in the waiting room by one of the study investigators (S.F. or J.P.) before their clinic appointment, consented, and asked to complete a self-administered paper survey. Study investigators (S.F or M.K) also consented and administered the survey by telephone to a random sample of patients with cirrhosis who did not have an upcoming clinic appointment.
We used a theoretical model of patient behavior for HCC surveillance (Fig. 1), based on the Health Behavior Framework, to guide selection of relevant variables for survey development.(17,18) The survey took approximately 20 minutes to complete and was divided into four sections: (1) knowledge about HCC, (2) potential barriers to HCC surveillance completion, (3) patient attitudes, and (4) demographic information. The first section assessed level of knowledge and consisted of 12 true-false questions with three domains: five questions regarding HCC risk and need for surveillance, four questions about surveillance logistics and effectiveness, and three questions about HCC treatment and prognosis. The second section assessed the presence of potential patient-, provider-, and system-level barriers to HCC surveillance completion, including patient refusal, financial or transportation concerns, lack of provider recommendation, and scheduling difficulties using yes/no response options. The section assessing patient attitudes included two domains: worry about HCC and information-seeking behavior. The patient apprehension domain estimated patient level of concern about developing HCC and/or dying from HCC as well as any impact of surveillance on level of concern using a 5-point Likert scale. Information-seeking questions assessed confidence in current level of HCC-related knowledge and desire for more information. Demographic information included age, sex, race and ethnicity, marital status, living situation, level of education, employment status, and household income. Questions were adapted from earlier validated surveys when available.(19,20) After initial development of the survey, we pretested it using cognitive interviewing methods with 10 English-speaking and 10 Spanish-speaking patients.(21,22)
FIG. 1.
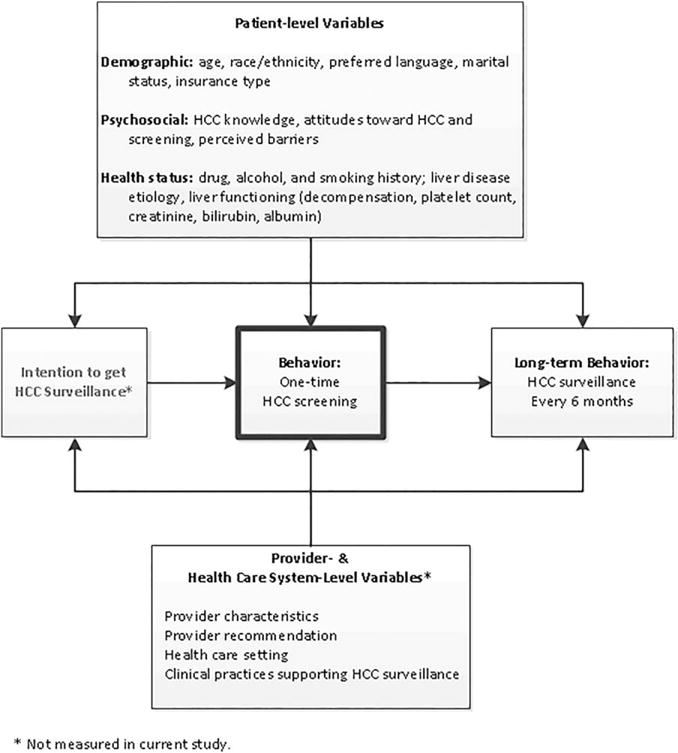
Model of patient behavior for HCC surveillance.
EMR DATA COLLECTION
Additional correlates, including patient demographics, clinical history, and laboratory data, were obtained through standardized abstraction of the EMR. We did not collect provider- or clinic-level characteristics, although we previously demonstrated that there are no differences in clinic practices supporting HCC surveillance.(19) Patient age, sex, race, ethnicity, preferred language, and insurance type as reported on the survey were verified using EMR data. We detailed drug, alcohol, and smoking history, with active alcohol abuse defined as drinking more than 40 g/day. Patients were classified according to etiology of liver disease using laboratory data and clinical notes as follows: hepatitis C virus (HCV; positive HCV antibody or viral load); hepatitis B virus (positive hepatitis B surface antigen or viral load), alcohol-related liver disease (as determined by clinic provider), nonalcoholic steatohepatitis (NASH; presence of metabolic syndrome in absence of other causes of chronic liver disease or as determined by clinic provider), and other. Data regarding presence of decompensation (ascites or hepatic encephalopathy [HE]) were abstracted from clinical notes and classified as none, mild or controlled, and severe or uncontrolled. Laboratory data of interest at time of survey administration included platelet count, creatinine, bilirubin, albumin, and international normalized ratio.
STUDY OUTCOMES
Our primary outcome of interest was receipt of abdominal imaging for surveillance purposes within the 12-month period preceding and 6-month period after survey administration. We evaluated surveillance completion instead of patients’ intent to complete surveillance because it could be collected in a standardized and objective manner using EMR data. We only included imaging for surveillance purposes because patient knowledge and attitudes about HCC surveillance would not affect the likelihood of having exams for diagnostic purposes. We used a study period surrounding the time of survey administration to minimize potential for changes in patient knowledge or attitudes. We recorded all imaging (ultrasound, contrast-enhanced computed tomography, or contrast-enhanced magnetic resonance imaging) and alpha fetoprotein (AFP) results during the study period. Imaging performed at outside institutions were included if results were recorded in the EMR. Intent of imaging (surveillance vs. nonsurveillance purposes) was determined through review of imaging orders and associated clinical notes. Indications, including “surveillance,” “screening,” “rule out HCC,” and “cirrhosis” were classified as surveillance indications, whereas exams performed for any symptoms or signs, for example, abdominal pain or elevated liver enzymes, were classified as diagnostic exams.
Surveillance receipt was first characterized as an ordinal outcome: consistent surveillance (≥1 imaging study during each 6-month period); inconsistent surveillance (≥1 imaging study during each study period, but not meeting criteria for semiannual surveillance); and no surveillance. Given the small number of patients with consistent surveillance, patients with consistent and inconsistent surveillance were combined for correlates analyses.
A secondary outcome of interest was overall patient knowledge. Each of the 12 true-false questions in the survey was awarded 1 point if correct and 0 if incorrect, “don’t know,” or left blank. A summary scale of the items was created, with higher scores indicating more accurate knowledge.
STATISTICAL ANALYSIS
Distributions of patient characteristics and perceptions of surveillance were reported with descriptive statistics. Univariate and multivariable logistic regression was performed to identify factors (patient knowledge, attitudes, barriers, and EMR-derived clinical variables) associated with our dichotomous measure of HCC surveillance receipt (any surveillance vs. no surveillance). The multivariable model included variables of a priori clinical importance (e.g., race/ethnicity, Child Pugh score) and factors significant on univariate analyses. Predictor variables with P < 0.10 in univariate analyses were included in multivariable models to minimize type 2 error. Statistical significance was defined as P < 0.05 for multivariable analyses. We required 480 patients to have 90% power to detect a difference of 15% in HCC surveillance rates,(18) assuming a baseline surveillance rate of 50% and prespecified alpha of 0.05. To identify factors associated with overall patient knowledge, we performed a secondary analysis using multivariable ordinal logistic regression. The multivariable model included variables of a priori clinical importance (e.g., race/ethnicity, educational attainment) and factors significant on univariate analyses. All data analysis was performed using Stata software (version 11; StataCorp LP, College Station, TX).
Results
PATIENT CHARACTERISTICS
Of 753 patients approached, 541 (71.8%) agreed to complete the survey, including 384 patients who completed the survey in clinic and 157 by telephone. Reasons for nonresponse include nonworking phone number or did not answer telephone (n = 109), patient refusal (n = 52 by telephone and 32 in clinic), and being admitted to the hospital, rehab facility, or jail (n = 19). Patient characteristics are detailed in Table 1. Median age was 56 years (interquartile range [IQR], 51–61) and 56.4% were male. The cohort was racially/ethnically diverse, with 43.4% Hispanics, 27.4% non-Hispanic Caucasians, and 25.7% blacks. Most (73.0%) patients had Medicaid or were covered by a county medical assistance plan, 23.3% had Medicare, and 3.7% had private insurance. The most common etiologies of cirrhosis were HCV infection (50.7%), alcohol-induced (26.0%), and NASH/cryptogenic (10.2%). Most patients had compensated cirrhosis, with 48.7% having Child Pugh A cirrhosis, 36.5% Child Pugh B cirrhosis, and 14.8% Child Pugh C cirrhosis. Ascites was present in 48.2% of patients, and 30.5% had grade I-II HE.
TABLE 1.
Patient Characteristics
| Characteristic | Receipt of Any Surveillance (n = 356) | No Surveillance (n = 185) |
|---|---|---|
| Age, years | 55.4 ± 8.6 | 55.1 ± 10.1 |
| Sex, % male | 206 (57.9) | 99 (53.5) |
| Race/ethnicity (%) | ||
| Non-Hispanic Caucasian | 100 (28.1) | 48 (25.9) |
| Black | 84 (23.6) | 55 (29.7) |
| Hispanic | 157 (44.1) | 78 (42.2) |
| Other/unknown | 15 (4.2) | 4 (2.2) |
| Primary language, % English | 273 (76.7) | 144 (77.8) |
| Insurance status (%) | ||
| Uninsured | 160 (44.9) | 94 (50.8) |
| Medicaid | 102 (28.7) | 39 (21.1) |
| Medicare | 80 (22.5) | 46 (24.9) |
| Private insurance | 14 (3.9) | 6 (3.2) |
| Educational attainment (%) | ||
| Did not graduate high school | 92 (25.8) | 38 (20.5) |
| High school degree | 168 (47.2) | 86 (46.5) |
| Attended but did not graduate college | 74 (20.8) | 51 (27.6) |
| College degree | 20 (5.6) | 10 (5.4) |
| Annual household income (%) | ||
| Less than $10,000 | 233 (65.4) | 126 (68.1) |
| $10,000–$20,000 | 70 (19.7) | 31 (16.8) |
| Greater than $20,000 | 38 (10.7) | 21 (11.4) |
| Not reported | 15 (4.2) | 7 (3.8) |
| Marital status, % married | 112 (31.5) | 53 (28.7) |
| Living situation, % alone | 80 (22.5) | 46 (24.9) |
| Etiology of liver disease (%) | ||
| Hepatitis C | 190 (53.4) | 83 (44.9) |
| Hepatitis B | 8 (2.2) | 6 (3.2) |
| Alcohol-related | 91 (25.6) | 49 (26.5) |
| NASH | 34 (9.5) | 21 (11.4) |
| Other | 33 (9.3) | 26 (14.0) |
| Child Pugh class (%) | ||
| A | 166 (48.4) | 74 (49.3) |
| B | 122 (35.6) | 58 (38.7) |
| C | 55 (16.0) | 18 (12.0) |
| Presence of HE (%) | 120 (33.7) | 45 (24.3) |
| Presence of ascites (%) | 175 (49.2) | 86 (46.5) |
| Receipt of hepatology care (%) | 327 (91.9) | 135 (73.0) |
PATIENT KNOWLEDGE OF HCC SURVEILLANCE
The percent of correct responses for each of the 12 knowledge questions ranged from 51.4% to 92.6% (Table 2). Patients demonstrated lower levels of knowledge about HCC risk factors than HCC surveillance and treatment logistics and effectiveness (P < 0.001). Although over 90% of patients knew that patients with cirrhosis are higher risk for HCC than those without cirrhosis, there were several notable knowledge deficiencies. Nearly half believed eating a healthy diet could sufficiently lower risk of HCC to no longer require HCC surveillance. Similarly, 20% of patients erroneously believed HCC surveillance is not necessary in the absence of abdominal pain, 28.5% believed HCC surveillance can be stopped after a couple normal ultrasound exams, and 34% believed HCC surveillance is not necessary if their physical exam is normal.
TABLE 2.
Proportion of Patient Knowledge Items Answered Correctly
| Knowledge Item | Proportion Correct (n = 541) |
|---|---|
| Patients with cirrhosis are at high risk for developing HCC (%) | 491 (90.8) |
| Eating a healthy diet does not sufficiently lower HCC risk to preclude a need for surveillance (%) | 278 (51.4) |
| Lack of abdominal pain does not preclude need for HCC surveillance (%) | 433 (80.0) |
| Patients with two consecutive normal surveillance ultrasound exams require continued HCC surveillance (%) | 387 (71.5) |
| Normal physical exam and labs does not preclude need for HCC surveillance (%) | 357 (66.0) |
| Ultrasound is the primary recommended modality for HCC surveillance (%) | 462 (85.4) |
| Patients with cirrhosis should have HCC surveillance performed at least once per year (%) | 478 (88.4) |
| Surveillance does not prevent development of HCC (%) | 418 (77.3) |
| Surveillance does not preclude diagnosis with advanced HCC (%) | 392 (72.5) |
| HCC can be cured if diagnosed at an early stage (%) | 429 (79.3) |
| Patients with HCC will die without cancer treatment (%) | 419 (77.5) |
| HCC does not spontaneously resolve without cancer treatment (%) | 501 (92.6) |
| Summary score for all questions, % (n = 12) | 77.7 |
| Summary score for risk factors questions, % (n = 5) | 71.9 |
| Summary score for surveillance logistics and efficacy questions, % (n = 4) | 80.9 |
| Summary score for treatment questions, % (n = 3) | 83.1 |
Factors associated with higher levels of overall knowledge on univariate analysis (Table 3) included Caucasian race, English as primary language, HCV- related cirrhosis, Child Pugh A cirrhosis, receipt of hepatology subspecialty care, higher educational attainment, and high perceived likelihood of dying from HCC. Being married, living alone, and lack of insurance were associated with lower levels of knowledge. Because of collinearity between language and race/ethnicity, language was not included in the multivariable model. Age, sex, and self-reported household income were examined, but were not significant on univariate analysis. On multivariable analysis, increased level of knowledge was significantly associated with Caucasian race, Medicare insurance status, receipt of hepatology subspecialty care, and higher educational attainment (Table 3).
TABLE 3.
Predictors of Higher Patient Knowledge
| Variable | Univariate Models OR (95% CI) | Multivariable Model AOR (95% CI)* |
|---|---|---|
| Race/ethnicity | ||
| Non-Hispanic | Reference | Reference |
| Caucasian | ||
| Black | 0.46 (0.30–0.70) | 0.53 (0.33–0.85) |
| Hispanic | 0.20 (0.14–0.30) | 0.38 (0.24–0.61) |
| Other/unknown | 0.37 (0.15–0.91) | 0.53 (0.21–1.31) |
| English language as preferred language | 3.83 (2.67–5.48) | Collinear |
| Insurance status | ||
| Uninsured | Reference | Reference |
| Medicaid | 1.49 (1.04–2.15) | 1.25 (0.84–1.87) |
| Medicare | 1.73 (1.18–2.53) | 1.75 (1.15–2.65) |
| Private insurance | 0.96 (0.45–2.04) | 1.0 (0.42–2.38) |
| Educational attainment | ||
| Did not graduate high school | Reference | Reference |
| High school degree | 3.03 (2.07–4.43) | 2.14 (1.41–3.26) |
| Attended but did not graduate college | 3.84 (2.46–6.00) | 2.68 (1.61–4.44) |
| College degree | 5.79 (2.77–12.11) | 3.20 (1.42–7.20) |
| Marital status (being married) | 0.55 (0.40–0.76) | NS |
| Living alone | 1.43 (1.01–2.03) | NS |
| HCV etiology of cirrhosis | 1.79 (1.33–2.42) | NS |
| Child Pugh A cirrhosis | 1.42 (1.03–1.94) | NS |
| Perceived likelihood of dying from HCC | 1.57 (1.16–2.12) | NS |
| Receipt of hepatology care | 1.49 (1.10–2.00) | 1.45 (1.05–2.01) |
Significant associations in bold.
Abbreviations: AOR, adjusted odds ratio; NS, not significant.
PATIENT ATTITUDES ABOUT HCC SURVEILLANCE
Patients demonstrated high levels of worry regarding HCC (42.3% worried and 24.0% extremely worried), with 282 (52.1%) expressing concern that they are likely to develop HCC in their lifetime and 250 (46.3%) expressing concern they are likely to die from HCC. Only 40 (7.4%) patients believed they are extremely unlikely to die from HCC. Patients expressed reassurance from undergoing HCC surveillance, with 375 (69.4%) reporting HCC surveillance is likely to find HCC at an early stage allowing curative therapy and 221 (41.0%) reported HCC surveillance decreases their risk of dying from HCC. Accordingly, 89.5% of patients rated having knowledge about HCC surveillance as important, and 88.8% believed it is important to undergo HCC surveillance.
PATIENT-REPORTED BARRIERS TO HCC SURVEILLANCE
The prevalence of patient-reported barriers to HCC surveillance is illustrated in Fig. 2. The most common perceived barriers to HCC surveillance were difficulty with the scheduling process for ultrasound exams (30.5%), costs of surveillance tests (25.3%), uncertainty of where to get surveillance ultrasound performed (19.6%), and difficulty with transportation (17.3%). Half (49.9%) of patients reported at least one of these barriers, with 22.8% reporting a multitude of these barriers. Perceived poor surveillance test efficacy (13.9%), fear of finding cancer (11.3%), time commitment (10.2%), and fear of pain from surveillance tests (9.5%) were uncommon barriers to HCC surveillance.
FIG. 2.
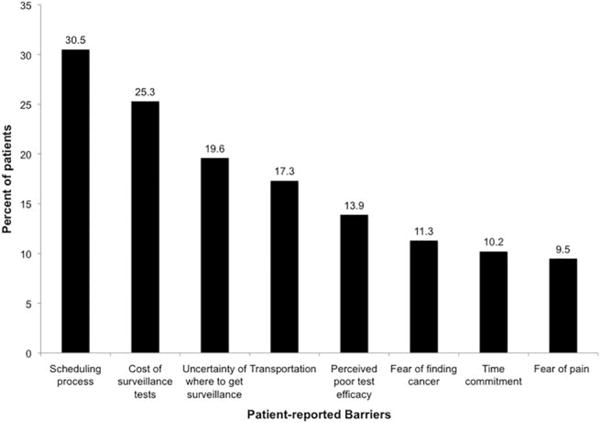
Patient-reported barriers to HCC surveillance.
HCC SURVEILLANCE RECEIPT
Surveillance imaging was performed at least once during the study period in 356 (65.8%) patients, with only 15 (2.8%) having consistent surveillance every 6 months. An additional 91 patients received ultrasound imaging for nonsurveillance purposes and were classified as having no surveillance. AFP was performed at least once during the study period in 92.4% of 356 patients with imaging-based surveillance and 70.2% of the 185 patients without imaging-based surveillance.
In univariate analysis, receipt of any surveillance was directly associated with hepatology subspecialty care (70.8% vs. 36.7%; P < 0.001), HCV etiology of cirrhosis (69.6% vs. 62.4%; P = 0.08), reporting lower levels of HCC-related worry because of surveillance (69.3% vs. 60.9%; P = 0.04), belief that HCC surveillance reduces chance of dying from HCC (71.5% vs. 63.7%; P = 0.10), and knowledge that cirrhosis is a primary risk factor for HCC development (67.0% vs. 54.2%; P = 0.08). Receipt of HCC surveillance was inversely associated with the presence of patient-reported barriers to surveillance (53.6% vs. 71.1%; P = 0.001). Receipt of HCC surveillance was not associated with patient age (P = 0.74), sex (P = 0.33), Caucasian race (P = 0.60), or English as primary language (P = 0.76). Similarly, we did not find an association between receipt of surveillance and overall level of knowledge (P = 0.89), perceived importance of undergoing surveillance (P = 0.62), or perceived likelihood of developing HCC (P = 0.36).
In multivariable analysis, receipt of any surveillance was positively associated with receipt of hepatology subspecialty care (odds ratio [OR], 2.65; 95% confidence interval [CI], 1.30–5.41), HCV etiology of cirrhosis (OR, 2.08; 95% CI, 1.19–3.63), and patient knowledge that cirrhosis is a high-risk state for developing HCC (OR, 3.09; 95% CI, 1.25–7.62); presence of any of the commonly reported barriers was inversely associated with receipt of HCC surveillance (OR, 0.42; 95% CI, 0.25–0.70; Table 4).
TABLE 4.
Predictors of HCC Surveillance Receipt
| Variable | Univariate Models OR (95% CI) | Multivariable Model* AOR (95% CI) |
|---|---|---|
| Age (continuous) | 1.00 (0.98–1.02) | † |
| Female sex | 0.84 (0.59–1.20) | † |
| Caucasian race | 1.11 (0.74–1.67) | † |
| English as primary language | 0.94 (0.61–1.43) | † |
| HCV etiology of cirrhosis (vs. other etiologies) | 1.37 (0.96–1.97) | 2.09 (1.20–3.65) |
| Receipt of hepatology care | 4.18 (2.53–6.88) | 2.64 (1.30–5.40) |
| Knowledge: Cirrhosis is risk factor for HCC | 1.72 (0.94–3.13) | 3.02 (1.23–7.39) |
| Attitude: Surveillance reduces HCC mortality | 1.43 (0.94–2.19) | NS |
| Attitude: Surveillance reduces worry about HCC | 1.45 (1.01–2.07) | NS |
| Patient-reported barriers to HCC surveillance | 0.47 (0.30–0.73) | 0.42 (0.25–0.70) |
Adjusted for race/ethnicity and Child Pugh class A cirrhosis given a priori importance. Significant associations in bold.
Not entered into multivariable model because of lack of significance in univariate analyses.
Abbreviations: AOR, adjusted odds ratio; NS, not significant.
Author names in bold designate shared co-first authorship.
In a post-hoc analysis, receipt of imaging for any reason over the 18-month period was directly associated with receipt of hepatology care (OR, 4.77; 95% CI, 2.63–8.64) and inversely associated with the presence of any of the commonly reported barriers to surveillance (OR, 0.47; 95% CI, 0.30–0.74). We did not find an association between receipt of any imaging and patient age (P = 0.64), sex (P = 0.36), Caucasian race (P = 0.94), HCV etiology (P = 0.75), overall level of knowledge (P = 0.58), or knowledge that cirrhosis is a high-risk state for developing HCC (P = 0.77).
Discussion
To the best of our knowledge, our study is the first survey assessing patient knowledge, attitudes, and barriers for HCC surveillance in a racially diverse and socioeconomically disadvantaged cohort of patients. We found that patients demonstrated high levels of HCC-related knowledge and expressed concern for developing and dying from HCC; however, they reported several barriers to receiving HCC surveillance, including difficulty with the scheduling process, costs of surveillance testing, and transportation difficulties. Surveillance rates were significantly higher in patients who knew cirrhosis was a risk factor for HCC development and significantly lower in those who reported barriers to HCC surveillance, suggesting that patient knowledge deficits and surveillance barriers may be important intervention targets to increase HCC surveillance rates in the United States.
Although a past survey study from the University of Michigan among 160 patients with cirrhosis reported high levels of knowledge about HCC risk, surveillance logistics, and treatment, this patient population represented a highly selected patient population (>80% Caucasian, >63% college educated, and highly insured) and may not be applicable to other populations.(20) Our current survey was administered in a racially diverse and socioeconomically disadvantaged cohort of patients followed in a large safety net health system. Patient knowledge, attitudes, and barriers of this population are particularly important to understand given increased HCC risk, lower surveillance rates, and worse prognosis among racial/ethnic minorities and patients of low SES.(4,23,24)
Despite differences in patient populations, patients demonstrated high levels of basic knowledge regarding HCC risk, surveillance logistics, and prognosis. Most important, 90% of patients understood that cirrhosis is a high-risk state for HCC and that ultrasound-based surveillance should be performed every 6–12 months. However, HCC surveillance rates were significantly lower among the subset of patients who did not know that patients with cirrhosis were at high risk for developing HCC, highlighting the importance of discussing this issue with all patients with cirrhosis. We also found several other knowledge deficiencies that warrant targeted patient education efforts. Nearly half of patients believed that eating a healthy diet could preclude the need for HCC surveillance, and over one third believed that HCC surveillance was not necessary if they had a normal physical exam and/or were asymptomatic. Furthermore, over one fourth of patients believed that HCC surveillance could be stopped after two normal ultrasound exams, potentially partly explaining “surveillance fatigue” and decreasing adherence rates as patients are followed over time.
Overall, patients expressed high levels of concern for developing and/or dying from HCC. Although they expressed reassurance in terms of HCC surveillance improving early tumor detection, less than half of patients believed that HCC surveillance reduces mortality. This uncertainty regarding HCC surveillance’s survival benefit could contribute to patients placing a lower priority on HCC surveillance and lead to nonadherence with surveillance recommendations. The reason for the disparity in reassurance for early tumor detection and mortality reduction is unclear, but may relate to how providers communicate benefits of HCC surveillance. A similar pattern was noted in a survey study among primary care providers caring for patients with cirrhosis.(19) Provider communication style and their level of enthusiasm for cancer screening benefits has been a strong predictor of adherence in colon and breast cancer screening.(25) If provider communication also impacted HCC surveillance adherence, this would highlight the need for higher-quality data characterizing the survival benefit of HCC surveillance in patients with cirrhosis. These data would also support studies evaluating the impact of interventions, such as provider communication training or audit feedback, on patient attitudes and surveillance adherence.(26)
Nearly half of all patients reported issues with ultrasound scheduling, costs, transportation, or uncertainty where to get surveillance ultrasound performed. Although these barriers are likely more common among socioeconomically disadvantaged patients, they highlight important intervention targets that can increase HCC surveillance rates. Effective intervention strategies can be adapted from breast and colon cancer screening programs, where similar barriers have been reported.(27–30) Simple reassurance about insurance coverage may be sufficient to allay fears of surveillance costs, and having clinic staff schedule ultrasounds the same day as clinic visits can likely mitigate patient issues with ultrasound scheduling, transportation, and uncertainty regarding potential surveillance sites. Comparative effectiveness trials evaluating intervention strategies to address patient-reported barriers are needed.
It is important to note that our study had limitations. Our study was performed in a single large, safety net hospital and may not be generalized to other practice settings. For example, our results might not be generalizable to patients associated with transplant centers given that most patients in safety net health systems are not eligible for LT given social and/or financial barriers.(31) However, we feel this study population is particularly important to evaluate given higher incidence and mortality rates among racial/ethnic minorities and socioeconomically disadvantaged patients. A national survey is needed to see whether our data are representative of patients receiving care in other settings. Survey studies are inherently limited by response and recall biases. Although we had a high response rate (>70%), there is also the possibility of nonresponse bias, in which patients knowledgeable and/or interested in HCC surveillance were more likely to respond. However, we feel these limitations are outweighed by its notable strengths, including its large, racially diverse sample size and the fact that it is one of the first studies to evaluate the combination of sociodemographic, clinical, and patient-reported psychosocial factors affecting HCC surveillance utilization, providing insight into potential patient-level intervention targets to increase HCC surveillance rates.
Overall, our study provides important insights into patient knowledge, attitudes, and barriers regarding HCC surveillance among patients with cirrhosis. Despite having overall high levels of HCC-related knowledge, they have misconceptions about HCC surveillance and report several barriers to implementation. These misconceptions and perceived barriers might partly explain the gap between the efficacy of HCC surveillance and its effectiveness in clinical practice. Overall, these findings highlight the need for patient education and systems-level interventions to decrease barriers for increasing HCC surveillance rates and optimizing HCC surveillance effectiveness.
Acknowledgments
This work was conducted with support from the Agency for Healthcare Research and Quality (R24 HS022418), the University of Texas Southwestern Center for Patient-Centered Outcomes Research, and an ACG Junior Faculty Development Award awarded to Dr. Singal. The content is solely the responsibility of the authors and does not necessarily represent the official views of the University of Texas Southwestern Medical Center and its affiliated academic and health care centers or the Agency for Healthcare Research and Quality.
Abbreviations
- AFP
alpha fetoprotein
- CI
confidence interval
- EMR
electronic medical record
- HCV
hepatitis C virus
- HCC
hepatocellular carcinoma
- HE
hepatic encephalopathy
- IQR
interquartile range
- LT
liver transplantation
- NASH
nonalcoholic steatohepatitis
- OR
odds ratio
- SES
socioeconomic status
Footnotes
Potential conflict of interest: Dr. Singal consults for and is on the speakers’ bureau for Bayer. Dr. Yopp is on the speakers’ bureau for Bayer and received grants from Novartis and Peregrine.
Author names in bold designate shared co-first
References
- 1.El-Serag HB, Rudolph KL. Hepatocellular carcinoma: epidemiology and molecular carcinogenesis. Gastroenterology. 2007;132:2557–2576. doi: 10.1053/j.gastro.2007.04.061. [DOI] [PubMed] [Google Scholar]
- 2.Singal AG, Marrero JA. Recent advances in the treatment of hepatocellular carcinoma. Curr Opin Gastroenterol. 2010;26:189–195. doi: 10.1097/MOG.0b013e3283383ca5. [DOI] [PubMed] [Google Scholar]
- 3.Altekruse SF, McGlynn KA, Reichman ME. Hepatocellular carcinoma incidence, mortality, and survival trends in the United States from 1975 to 2005. J Clin Oncol. 2009;27:1485–1491. doi: 10.1200/JCO.2008.20.7753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ha J, Yan M, Aguilar M, Bhuket T, Tana M, Liu B, et al. Race/ethnicity-specific disparities in cancer incidence, burden of disease, and overall survival among patients with hepatocellular carcinoma in the U. S Cancer. 2016;122:2512–2523. doi: 10.1002/cncr.30103. [DOI] [PubMed] [Google Scholar]
- 5.Sloane D, Chen H, Howell C. Racial disparity in primary hepatocellular carcinoma: tumor stage at presentation, surgical treatment and survival. J Natl Med Assoc. 2006;98:1934–1939. [PMC free article] [PubMed] [Google Scholar]
- 6.Singal AG, Pillai A, Tiro J. Early detection, curative treatment, and survival rates for hepatocellular carcinoma surveillance in patients with cirrhosis: a meta-analysis. PLoS Med. 2014;11:e1001624. doi: 10.1371/journal.pmed.1001624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Singal AG, Yopp A, Skinner CS, Packer M, Lee WM, Tiro JA. Utilization of hepatocellular carcinoma surveillance among American patients: a systematic review. J Gen Intern Med. 2012;27:861–867. doi: 10.1007/s11606-011-1952-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Singal AG, Li X, Tiro J, Kandunoori P, Adams-Huet B, Nehra M, Yopp A. Racial, social, and clinical determinants of hepatocellular carcinoma surveillance. Am J Med. 2015;128:90 e1–7. doi: 10.1016/j.amjmed.2014.07.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Singal AG, Yopp AC, Gupta S, Skinner CS, Halm EA, Okolo E, et al. Failure rates in the hepatocellular carcinoma surveillance process. Cancer Prev Res (Phila) 2012;5:1124–1130. doi: 10.1158/1940-6207.CAPR-12-0046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Collier J, Sherman M. Screening for hepatocellular carcinoma. HEPATOLOGY. 1998;27:273–278. doi: 10.1002/hep.510270140. [DOI] [PubMed] [Google Scholar]
- 11.Henrion J, Libon E, De Maeght S, Deltenre P, Schapira M, Ghilain JM, et al. [Screening for hepatocarcinoma in a cohort with cirrhosis mainly of alcoholic origin][Article in French] Gastroenterol Clin Biol. 2003;27:534–539. [PubMed] [Google Scholar]
- 12.Klein WM, Bloch M, Hesse BW, McDonald PG, Nebeling L, O’Connell ME, et al. Tesauro G. Behavioral research in cancer prevention and control: a look to the future. Am J Prev Med. 2014;46:303–311. doi: 10.1016/j.amepre.2013.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rakowski W, Breslau ES. Perspectives on behavioral and social science research on cancer screening. Cancer. 2004;101(5 Suppl):1118–1130. doi: 10.1002/cncr.20503. [DOI] [PubMed] [Google Scholar]
- 14.Davila JA, Morgan RO, Richardson PA, Du XL, McGlynn KA, El-Serag HB. Use of surveillance for hepatocellular carcinoma among patients with cirrhosis in the United States. HEPATOLOGY. 2010;52:132–141. doi: 10.1002/hep.23615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Glanz K, Bishop DB. The role of behavioral science theory in development and implementation of public health interventions. Annu Rev Public Health. 2010;31:399–418. doi: 10.1146/annurev.publhealth.012809.103604. [DOI] [PubMed] [Google Scholar]
- 16.Nehra MS, Ma Y, Clark C, Amarasingham R, Rockey DC, Singal AG. Use of administrative claims data for identifying patients with cirrhosis. J Clin Gastroenterol. 2013;47:e50–e54. doi: 10.1097/MCG.0b013e3182688d2f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bastani R, Glenn BA, Taylor VM, Chen MS, Jr, Nguyen TT, Stewart SL, Maxwell AE. Integrating theory into community interventions to reduce liver cancer disparities: The Health Behavior Framework. Prev Med. 2010;50:63–67. doi: 10.1016/j.ypmed.2009.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Maxwell AE, Bastani R, Chen MS, Jr, Nguyen TT, Stewart SL, Taylor VM. Constructing a theoretically based set of measures for liver cancer control research studies. Prev Med. 2010;50:68–73. doi: 10.1016/j.ypmed.2009.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dalton-Fitzgerald E, Tiro J, Kandunoori P, Halm EA, Yopp A, Singal AG. Practice patterns and attitudes of primary care providers and barriers to surveillance of hepatocellular carcinoma in patients with cirrhosis. Clin Gastroenterol Hepatol. 2015;13:791–798e1. doi: 10.1016/j.cgh.2014.06.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Singal A, Volk M, Rakoski M, Fu S, Su G, McCurdy H, Marrero J. Patient involvement is correlated with higher HCC surveillance in patients with cirrhosis. J Clin Gastroenterol. 2011;45:727–732. doi: 10.1097/MCG.0b013e31820989d3. [DOI] [PubMed] [Google Scholar]
- 21.Beatty P, Willis G. Research synthesis: the practice of cognitive interviewing. Public Opin Q. 2007;71:287–311. [Google Scholar]
- 22.Willis G. Cognitive interviewing: a tool for improving questionnaire design. Thousand Oaks, CA: Sage; 2004. [Google Scholar]
- 23.Artinyan A, Mailey B, Sanchez-Luege N, Khalili J, Sun CL, Bhatia S, et al. Race, ethnicity, and socioeconomic status influence the survival of patients with hepatocellular carcinoma in the United States. Cancer. 2010;116:1367–1377. doi: 10.1002/cncr.24817. [DOI] [PubMed] [Google Scholar]
- 24.Shebl FM, Capo-Ramos DE, Graubard BI, McGlynn KA, Altekruse SF. Socioeconomic status and hepatocellular carcinoma in the United States. Cancer Epidemiol Biomarkers Prev. 2012;21:1330–1335. doi: 10.1158/1055-9965.EPI-12-0124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fox SA, Heritage J, Stockdale SE, Asch SM, Duan N, Reise SP. Cancer screening adherence: does physician-patient communication matter? Patient Educ Couns. 2009;75:178–184. doi: 10.1016/j.pec.2008.09.010. [DOI] [PubMed] [Google Scholar]
- 26.Price-Haywood EG, Harden-Barrios J, Cooper LA. Comparative effectiveness of audit-feedback versus additional physician communication training to improve cancer screening for patients with limited health literacy. J Gen Intern Med. 2014;29:1113–1121. doi: 10.1007/s11606-014-2782-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Green AR, Peters-Lewis A, Percac-Lima S, Betancourt JR, Richter JM, Janairo MP, et al. Barriers to screening colonoscopy for low-income Latino and white patients in an urban community health center. J Gen Intern Med. 2008;23:834–840. doi: 10.1007/s11606-008-0572-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sabatino SA, Lawrence B, Elder R, Mercer SL, Wilson KM, DeVinney B, et al. Effectiveness of interventions to increase screening for breast, cervical, and colorectal cancers: nine updated systematic reviews for the guide to community preventive services. Am J Prev Med. 2012;43:97–118. doi: 10.1016/j.amepre.2012.04.009. [DOI] [PubMed] [Google Scholar]
- 29.Singal AG, Tiro JA, Gupta S. Improving hepatocellular carcinoma screening: applying lessons from colorectal cancer screening. Clin Gastroenterol Hepatol. 2013;11:472–477. doi: 10.1016/j.cgh.2012.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Singal AG, Gupta S, Tiro JA, Skinner CS, McCallister K, Sanders JM, et al. Outreach invitations for FIT and colonoscopy improve colorectal cancer screening rates: a randomized controlled trial in a safety net health system. Cancer. 2016;122:456–463. doi: 10.1002/cncr.29770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Singal AG, Chan V, Getachew Y, Guerrero R, Reisch JS, Cuthbert JA. Predictors of liver transplant eligibility for patients with hepatocellular carcinoma in a safety net hospital. Dig Dis Sci. 2012;57:580–586. doi: 10.1007/s10620-011-1904-7. [DOI] [PubMed] [Google Scholar]


