Abstract
Objective
The study compared the 7-point Subjective Global Assessment (SGA) and the Protein Energy Wasting (PEW) Score with Nutrition Evaluations (NutrE) conducted by registered dietitian nutritionists (RDNs) in identifying PEW risk in stage five chronic kidney disease (CKD) patients on maintenance hemodialysis (MHD).
Design and Methods
This study is a secondary analysis of a cross-sectional study entitled “Development and Validation of a Predictive energy Equation in Hemodialysis”. PEW risk identified by the 7-point SGA and the PEW Score were compared against the NutrE conducted by RDNs through data examination from the original study (reference standard).
Subjects
A total of 133 patients were included for the analysis.
Main Outcome Measures
The sensitivity, specificity, positive and negative predictive value (PPV and NPV), positive and negative likelihood ratio (PLR and NLR) of both scoring tools were calculated when compared against the reference standard.
Results
The patients were predominately African American (n=112, 84.2%), non-Hispanic (n=101, 75.9%), and male (n=80, 60.2%). Both the 7-point SGA (sensitivity =78.6%, specificity = 59.1%, PPV = 33.9%, NPV = 91.2%, PLR = 1.9 and NLR = 0.4) and the PEW Score (sensitivity = 100%, specificity= 28.6%, PPV = 27.2%, NPV = 100%, PLR = 1.4 and NLR = 0) were more sensitive than specific in identifying PEW risk. The 7-point SGA may miss 21.4% patients having PEW and falsely identify 40.9% of patients who do not have PEW. The PEW Score can identify PEW risk in all patients but 71.4% of patients identified may not have PEW risk.
Conclusions
Both the 7-point SGA and the PEW Score could identify PEW risk. The 7-point SGA was more specific and the PEW Score was more sensitive. Both scoring tools were found to be clinically confident in identifying patients who were actually not at PEW risk.
Keywords: Protein Energy Wasting, Subject Global Assessment, Maintenance Hemodialysis, Nutrition evaluations, diagnostic tests, Validity
Introduction
In the United States, approximately fourteen percent of the population has chronic kidney disease (CKD).1 One in two of the CKD patients on maintenance dialysis (MHD) will die within three years after the initiation of MHD.1 Such a high death rate is a serious public health issue causing high cost in human loss and substantive burden in medical expenses.1
Protein energy wasting (PEW) is one of the independent risk factors associated with the high mortality rate among CKD patients on MHD.2–7 PEW is a critical condition characterized by inadequate nutrient intake, accumulation of uremic toxins, inflammation and catabolism.6, 8 The International Society of Renal Nutrition and Metabolism (ISRNM) defines PEW as “a state of decreased body stores of protein and energy fuels” and proposed that the diagnostic criteria of PEW be comprised of four categories: abnormal biochemical indicators; low body weight, low body fat or significant weight loss; reduced muscle mass; and low energy or protein consumption.5, 9
There is no gold standard for identifying PEW risk. Nutrition evaluations (NutrE) conducted by registered dietitian nutritionists (RDNs) on stage five CKD patients on MHD using the ISRNM diagnostic criteria is a common clinical practice for PEW risk identification. However, different nutrition screening and assessment scoring tools have been modified or developed in an attempt to aid in identifying PEW risk.6, 10–12 An example of a nutrition screening tool in identifying PEW risk is the Protein Energy Wasting Score (PEW Score).6 Examples of nutrition assessment scoring tools in identifying PEW risk include subjective global assessment (SGA), dialysis malnutrition score (DMS), malnutrition inflammation score (MIS), geriatric nutritional risk index (GNRI) and composite score of protein-energy nutritional status (cPENS).7, 10, 11, 13
Nevertheless, there is still no consensus regarding which tool should be used for identifying PEW risk. Most studies have investigated the use of these scoring tools in predicting mortality instead of identifying PEW risk or diagnosing PEW.6, 7, 11 Early nutrition intervention is critical for patients identified with PEW risk to maintain and improve health outcomes.5, 8, 9
The purpose of the study was to compare the 7-point SGA and the PEW Score as diagnostic tools against NutrE conducted by RDNs using ISRNM diagnostic criteria for PEW to identify PEW risk in stage five CKD patients on MHD. The 7-point SGA, recommended by the Kidney Disease/Dialysis Outcomes and Quality Initiative (K/DOQI), is a validated nutrition assessment tool for stage five CKD patients on MHD.14 It was not designed to identify PEW risk or diagnose PEW but is already applied in this manner in studies.14, 15 While the 7-point SGA is validated to conduct nutrition assessment, it is uncertain if it can be used to properly identify PEW risk because PEW is a result of multiple nutrition and non-nutrition mechanisms due to the progression of CKD patients on MHD, but not just under-nutrition.5
The PEW Score is a simplified screening tool developed by Moreau-Gaudry et al. to identify PEW risk.6 The PEW Score is based on readily available clinical and biological values that comprise the ISRNM diagnostic criteria for PEW.6 The PEW Score was found to be useful in predicting survival in CKD patients on MHD, but has not been validated for use in clinical practice.6 While the PEW Score is a screening tool and not like a nutrition assessment tool as the 7-point SGA, it is uncertain if they would identify PEW risk similarly.
Methods
This study is a secondary analysis of a cross-sectional study, and the research reported in this publication was supported by the National Institute of Diabetes and Digestive and Kidney Disease (NIDDK) of the National Institutes of Health under Award Numbers 1R15DK090593-01A1, 6R15DK090593-02 and 3R15DK090593-02S1. The title of the original study was “Development and Validation of a Predictive energy Equation in Hemodialysis” and the methodology of the study was previously published by Olejnik et al.16
Study Population
From September 2012 to August 2015, patients were recruited from three research institutions in the Northeastern region of the United States (Rutgers University, Case Western Reserve University, and Pennsylvania State University-Hershey Medical Center). The inclusion criteria were adults aged 18 years or older, diagnosed with stage five CKD initiated on MHD three times per week for at least three months and the ability to answer study-related questions. Patients were excluded if they were hospitalized or had active infection, non-healing wound, any cardiac-related events, surgical procedures less than thirty days prior to study enrollment, self-reported routine use of dietary supplements or recreational drugs that may impact metabolic rate, and were pregnant, lactating, or three months post-partum. A total of 133 cases were available for the analysis.
The 7-point SGA
The 7-point SGA was conducted by trained study personnel in the original study and the data was extracted for the secondary analysis of the current study. The 7-point SGA utilizes a seven point Likert scale for the subjective ratings of six components to reflect nutritional status.14, 15 The six components include weight change, dietary intake, gastrointestinal symptoms, functional capacity, disease state/comorbidities, and physical exam.14 The overall SGA score is rated subjectively based on the ratings of the six individual components. There are three overall SGA ratings: well nourished (score six or seven), moderate or suspected malnourished (score three, four or five) and severe malnourished (score one or two).17 For the purpose of this study, the criteria for administering the SGA described by Steiber et al14 were followed. The results of the 7-point SGA were dichotomized in order to compare against the results of the NutrE conducted by RDNs. The overall SGA ratings of six or seven were categorized as “Not at PEW risk” while the overall SGA ratings of one to five were all categorized as “At PEW risk” since patients having ratings of one to five were considered as moderate malnourished or severe malnourished according to the protocol of the 7-point SGA.14
The PEW Score
The PEW Score was calculated retrospectively in the current study according to the protocol described by Moreau-Gaurdy et al. using the data from the original study.6 The four components for the PEW Score are serum albumin level, body mass index (BMI), pre-dialysis serum creatinine normalized by body surface area (Scr/BSA) and normalized protein nitrogen appearance (nPNA). The threshold values for each component, according to the protocol, are 3.8g/dL for serum albumin; 23 kg/m2 for BMI; 380 μmol/L/m2 for Scr/BSA and 0.8 g/kg/day for nPNA. For each component, if a patient had a value greater than the threshold value, s/he received one point for that component. If a patient had a value less than the threshold value, s/he received zero points for that component. Therefore, the total PEW Score ranges from zero to four.6 There are four overall PEW Score ratings and they are normal nutritional status (score four), slight wasting (score three), moderate wasting (score two) and severe wasting (score zero to one).6 For the purpose of this study, the results of the PEW Score were dichotomized in order to compare against the results of the NutrE conducted by RDNs. The overall PEW Score of four was categorized as “Not at PEW risk” while the overall PEW Score of zero to three were all categorized as “At PEW risk” since patients having ratings of zero to three were considered as slight wasting, moderate wasting or severe wasting.
Nutrition Evaluation by RDN using ISRNM diagnostic criteria for PEW
Nutrition evaluations (NutrE) conducted by RDNs is a common clinical practice to determine the PEW risk of a patient, and the use of ISRNM diagnostic criteria in the NutrE enables RDNs to further confirm the PEW risk in stage 5 CKD patients on MHD.
The Renal Dietitians Practice Group of the Academy of Nutrition and Dietetics and the Council of Renal Nutrition of the National Kidney Foundation have established the Standards of Practice and Standards of Professional Performance for RDNs in Nephrology Care.18 These standards have listed the knowledge, skills and competencies that an RDN must have in order to provide safe and effective nutrition care in different nephrology settings. As a result, these standards provide RDNs a basis to provide nutrition assessment and care in patients with renal problems.18
The ISRNM diagnostic criteria for PEW were developed as a framework to provide a basis to guide clinicians in assessing PEW in CKD.9 With different clinical, nutritional and biochemical parameters that may contribute to the development of PEW, four main categories (abnormal biochemical indicators; low body weight, low body fat or significant weight loss; reduced muscle mass; and low energy or protein consumption) were recommended by the expert panel as the diagnostic criteria for PEW.19 However, it was noted that additional nutrition and inflammation parameter may also be potential clues to PEW development.19 Therefore, it may not be ideal to solely use the ISRNM diagnostic criteria for PEW as the only indication to categorize patients having PEW risk.19
As a result, it is hypothesized that the use of NutrE conducted by RDNs plus ISRNM diagnostic criteria for PEW is a more comprehensive evaluation and can best identify patients at PEW risk.9, 18–20 In this secondary analysis, the results of the NutrE were used as the reference standard to compare with the 7-point SGA and the PEW Score.
NutrE were conducted by evaluating the data obtained from the research appointments in the original NIDDK funded study. Two RDNs were recruited to conduct the NutrE for this study. Since the current study is a secondary analysis of a cross-sectional study, the RDNs were not able to meet the patients in-person for the NutrE. Both RDNs practice renal nutrition independently and they were blinded from the overall 7-point SGA scores, the PEW Scores and each other’s evaluations.
Firstly, the RDNs evaluated each patient’s records independently by looking at the five nutrition assessment domains: 1) food/nutrition-related history, 2) biochemical data, medical tests and procedures, 3) anthropometric measurements, 4) nutrition-focused physical findings, and 5) client history.21 The parameters examined in the NutrE are described in Table 1. After that, the RDNs used the ISRNM diagnostic criteria for PEW (Table 2) to evaluate each patient’s record. The evaluations of each nutrition assessment domain and diagnostic criteria guided their clinical decisions to assign the patient as either “Not at PEW risk” or “At PEW risk”.
Table 1.
Parameters evaluated by registered dietitian nutritionists (RDNs) for each nutrition assessment domain in nutrition evaluation (NutrE).
| Nutrition Assessment Domains | Parameters in NutrE |
|---|---|
| 1) Food/Nutrition Related History | Dietary intake data (on both dialysis and non-dialysis days) |
| 2) Anthropometric Measurements and Vital Signs | Height, Weight, Dry Weight, Average interdialytic weight gain, blood pressure |
| 3) Biochemical Data, Medical Tests, and Procedures | Serum albumin, blood urea nitrogen, normalized protein catabolic rate, C-reactive protein, white blood cells, hemoglobin, intact parathyroid hormone, hemoglobin A1C, serum creatinine |
| 4) Nutrition-Focused Physical Findings | Nutrition-specific quality of life (NSQOL) questionnaire results, subjective global assessment sub-components (functional capacity, physical exam) |
| 5) Client History | Demographic characteristics (age, gender, race, ethnicity and Chronic kidney disease etiology) |
Table 2.
The ISRNM diagnostic criteria for PEW in CKD
| Threshold | Threshold |
|---|---|
| Biochemical Indicators | Serum albumin less than 3.8g/dLa Serum prealbumin (transthyretin) less than 30 mg/dLa Serum cholesterol less than 100 mg/dLa |
| Body Mass | BMI less than 23kg/m2b Unintentional weight loss: 5% over three months or 10% over six months b Total body fat percentage less than10% b |
| Muscle Mass | Muscle wasting: reduced muscle mass-5% over three months or 10% over six months Reduced mid-arm muscle circumference areac (reduction over 10% in relation to the fiftieth percentile of reference population) Appearance of creatinined |
| Dietary Intake | Unintentional low DPI: less than 0.8 g/kg/day for at least two months for patients on hemodialysise or less than 0.6 g/kg/day for patients with CKD stage 2–5. Unintentional low DEI: less than 25 kcal/kg/day for at least two monthse. |
At least three categories listed above (and at least one test in each of the selected category) must be met in order to satisfy the PEW diagnosis.
Data is not valid if low concentrations are caused by abnormal urinary or gastrointestinal protein loss, livers diseases or cholesterol lowering medications.
Certain Asian population might be desirable to have lower BMI; post-dialysis weight or edema-free mass must be used.
Only trained anthropometrist can conduct the measurements.
Both muscle mass and meat intake can influence the appearance of creatinine.
Dietary diaries and interviews can be used. Protein intake can be assessed by calculation of normalized protein equivalent of total nitrogen appearance.
Abbreviations: BMI, Body mass index; CKD, chronic kidney disease; DPI, Dietary protein intake; DEI, Dietary energy intake, PEW, protein energy wasting
Each RDN provided their report independently to the principal investigator to indicate which patient was “At PEW risk” and which patient was “Not at PEW risk”. Cohen’s kappa coefficient was determined to measure the agreement between the two RDNs in conducting the NutrE and using the ISRNM diagnostic criteria to identify PEW risk. For discrepancies between the two RDNs in assigning PEW risk status on individual patients, consensus was achieved through discussions between the two RDNs on the patients in regularly scheduled meetings (conference calls) organized and moderated by the principal investigator. During each meeting, the parameters in each nutrition assessment domain of the patient were discussed until consensus was achieved in assigning PEW status for the patients. It was agreed that if consensus was not achieved during the meetings, the patient would be removed from the dataset.
According to the ISRNM diagnostic criteria, there are four categories of readily utilizable criteria and they are biochemical indicators, body mass, muscle mass and dietary intake (Table 2). Three out of the four categories must be satisfied before a patient can be diagnosed as having PEW. However, the ISRNM consensus review stated that there can be other causes and manifestations of PEW in CKD patients on MHD in addition to the four selected diagnostic criteria.9, 19 For the purpose of this study, the ISRNM diagnostic criteria for PEW were used as a reference only for the RDNs in conducting the NutrE. The RDNs made the final decision in assigning PEW risk status for each patient regardless of whether the patient’s health condition fulfilled the ISRNM diagnostic criteria.
Statistical Analysis
Statistical analysis of the demographic data was performed using Statistical Package for the Social Sciences (SPSS, Inc., Chicago, IL, USA) version 24.0. Continuous data were presented as the mean ± standard deviation (SD).
Comparison of 7-point SGA and PEW Score against NutrE
To compare the 7-point SGA and PEW Score against the results of the NutrE conducted by RDNs as diagnostic tools for PEW in CKD patients on MHD, the sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), positive likelihood ratio (PLR), negative likelihood ratio (NLR) of 7-point SGA and PEW Score were calculated.10
Sensitivity is the accuracy of the diagnostic test in correctly identifying patients who have the disease.22 Specificity is the ability of the diagnostic test to correctly identify patients who do not have the disease.22 Positive Predictive Value (PPV) is the probability of disease for patients with a positive screening test result.22 Negative Predictive Value (NPV) is the probability that patients do not have the disease with a negative screening test result.22 Positive likelihood ratio (PLR) refers to the increase in disease probability when the screening test result is positive. Negative likelihood ratio (NLR) refers to the decrease in disease probability when the screening test result is negative.23
The equations in calculating sensitivity, specificity, PPV, NPV, PLR and NLR are listed as follows:
Sensitivity = True positives/(true positives + false negatives)
Specificity = True negatives/(true negatives + false positives)
PPV = True test positives/all test positives
NPV = True test negatives/all test negatives
PLR = Sensitivity/(1-specificity)
NLR = (1-sensitivity)/specificity
Statistical analysis (sensitivity, specificity, PPV, NPV, PLR & NLR) of each scoring tool in identifying PEW risks when compared with NutrE conducted by RDNs using ISRNM diagnostic criteria for PEW was performed using Open Source Epidemiologic Statistics for Public Health, version 3.01 (OpenEpi).24 After determining the number of true positives (“At PEW risk” in both scoring tool and the reference standard), false positives (“At PEW risk” in scoring tool but “Not at PEW risk” in reference standard), false negatives (“Not at PEW risk” in scoring tool but at “At PEW risk” in reference standard) and true negatives (“Not at PEW risk” in both scoring tool and reference standard) by SPSS, the results were entered into the statistical program and formulas for the statistical analysis of the current study (sensitivity, specificity, PPV, NPV, PLR & NLR) were applied. The 95% confidence interval was estimated using the Wilson score interval within OpenEpi.
Power Analysis
In studies investigating the accuracy of diagnostic tests, power calculations were rarely reported and there are no standard guidelines available on how to determine the number of patients needed for this type of study by power analysis.25, 26 Hess et al. proposed a three-step method in determining the sample size needed for studies investigating the accuracy of diagnostic tests.25 This method takes into account the margin of error and the estimated sensitivity or specificity.25 By applying the three-step method described by Hess et al, the sample size needed for 80% power to estimate the sensitivity and specificity of 95% for both the 7-point SGA and the PEW Score with a relative margin of error ≤0.05 was at 102 patients. This study achieved 80% power by analyzing a total of 133 patients.
Results
Patient characteristics
A total of 133 patients were included in the analysis (Table 3), including 80 (60.2%) males and 53 (39.8%) females, and their mean age was 54.8 ± 12.0 years. The majority of the patients were African American (n=112, 84.2%) and non-Hispanic (n=101, 75.9%). The major etiologies of CKD were diabetes (n=46, 34.6%) and hypertension (n=50, 37.6%). Body mass index (BMI) was 30.2 ± 6.8 kg/m2.
Table 3.
Summary of the characteristics of patients enrolled in the study entitled “Development and Validation of a Predictive Energy Equation in Hemodialysis” (n=133)
| Characteristics | n (%) |
|---|---|
| Age in years (mean ± SD) | 54.8 ± 12.0 |
| Gender | |
| Male | 80 (60.2) |
| Female | 53 (39.8) |
| Race | |
| Caucasian | 21 (15.8) |
| African American | 112 (84.2) |
| Ethnicity | |
| Hispanic | 10 (7.5) |
| Non-Hispanic | 101 (75.9) |
| Unknown | 22 (16.5) |
| CKD Etiology* | |
| Diabetes (Type 1 or 2) | 46 (34.6) |
| Hypertension | 50 (37.6) |
| Glomerulonephritis | 7 (5.3) |
| Polycystic Kidney | 4 (3.0) |
| Others | 64 (48.1) |
As patients could have more than one CKD etiology, the sum of the percentage is more than 100.
PEW diagnosis
According to the results obtained from the NutrE conducted by the two renal RDNs of the 133 patients, 106 (79.7%) patients were assigned the same PEW risk status by both RDNs and 27 (20.3%) required further discussion to achieve consensus regarding their PEW risk status. The Cohen’s kappa coefficient was determined to be 0.412, which indicates a moderate agreement range between the two RDNs in identifying PEW risk in this group of patients.27
Three one-hour meetings of the RDNs were organized and moderated by the principal investigator during the study period to discuss the 27 patients in question. The most challenging area for the RDNs to achieve consensus was assessing patient-rated appetite, since follow-up questions to clarify these responses were not possible, given the use of pre-collected data. However, the opportunity to review variables which either supported or refuted PEW risk enabled the RDNs to achieve consensus. Therefore, no patient was removed from the dataset for the final analysis. Based on the final result of the NutrE, 28 (21.1%) patients were rated “at PEW risk” and 105 (78.9%) patients were rated “Not at PEW risk” (Table 4).
Table 4.
Prevalence of PEW risk in the stage 5 CKD patients on MHD based on 7-point SGA, PEW Score, and NutrE conducted by RDs using ISRNM diagnostic criteria for PEW (n=133)
| Nutritional Status | 7-point SGA | PEW Score | NutrE by RDNs using ISRNM diagnostic criteria |
|---|---|---|---|
| At PEW Risk n (%) | 65 (48.9) | 103 (77.4) | 28 (21.1) |
| Not at PEW Risk n (%) | 68 (51.1) | 30 (22.6) | 105 (78.9) |
From the original 7-point SGA ratings, 68 (51.1%) patients were rated well-nourished (score six or seven), 65 (48.9%) patients were rated moderate or suspected malnourished (score three, four or five) and no patients were rated severe malnourished (score one or two). According to the PEW Score, 30 (22.6%) patients had normal nutritional status (score four), 57 (42.9%) patients had slight wasting (score three), 36 (27.1%) patients had moderate wasting (score two) and 10 (7.5%) patients had severe wasting (score one and zero).
For the purpose of this study, patients were categorized as either “At PEW risk” or “Not at PEW risk”. Based on the results from the 7-point SGA and PEW Score, the number of patients at PEW risk was, respectively, 65 (48.9%) and 103 (77.4%).
Comparison of 7-point SGA and PEW Score against NutrE
In comparing the results of the two scoring tools (7-point SGA and PEW Score) against the reference standard (retrospective NutrE conducted by RDNs with the use of ISRNM diagnostic criteria for PEW), a comparison table (Table 5) was developed. Based on the results of true positives and true negatives, the 7-point SGA and the PEW Score identified the same level of PEW risk as the NutrE conducted by RDNs in 84 (63%) and 58 (43.6%) patients, respectively.
Table 5.
Results of the scoring tools (7-point SGA and PEW score) compared against the NutrE conducted by Registered Dietitian Nutritionists (RDNs) (reference standard) in identifying PEW risk (n=133)
| 7-point SGA | PEW Score | ||||
|---|---|---|---|---|---|
| Reference Standard (NutrE conducted by RDN with the use of ISRNM diagnostic criteria for PEW) | Positive (At PEW risk) | Negative (Well Nourished) | Positive (At PEW risk) | Negative (Well Nourished) | |
| Positive (At PEW risk) | 22a | 6c | 28a | 0c | |
| Negative (Well Nourished) | 43b | 62d | 75b | 30d | |
True positives (“At PEW risk” in both scoring tool and the reference standard)
False positives (“At PEW risk” in scoring tool but “Not at PEW risk” in reference standard)
False negatives (“Not at PEW risk” in scoring tool but at “At PEW risk” in reference standard)
True negatives (“Not at PEW risk” in both scoring tool and reference standard)
Figure 1 compared the sensitivity and specificity between the 7-point SGA and the PEW Score. The sensitivity of both scoring tools in identifying PEW risk was higher than their specificity. The sensitivity of the PEW Score (100%) was higher than that of the 7-point SGA (78.6%) but the specificity of the PEW Score (28.6%) was much lower than that of the 7-point SGA (59.1%). Other components in evaluating the validity of the 7-point SGA and the PEW Score were listed in Table 6.
Figure 1. Comparison of sensitivity and specificity between the 7-point SGA and the PEW Score in identifying PEW risk in Stage five CKD patients on MHD.
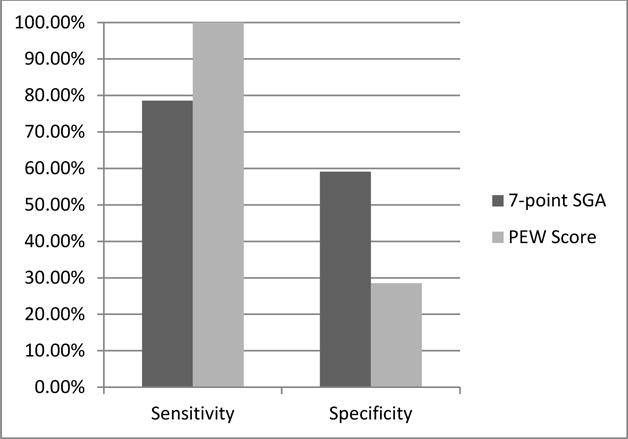
Sensitivity: the accuracy of the 7-point SGA and PEW score in correctly identifying patients who PEW risk.
Specificity: the ability of the 7-point SGA and PEW score to correctly identify patients who do not have PEW risk.
Table 6.
The sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), positive likelihood ratio (PLR) and negative likelihood ratio (NLR) of the 7-point subjective global assessment (SGA) and protein energy wasting (PEW) score in comparison with nutrition evaluation (NutrE) conducted by registered dietitian nutritionists (RDN)s with the use of International Society of Renal Metabolism (ISRNM) diagnostic criteria for PEW. (n=133)
| Parameters | 7-point SGA (95% confidence intervals) | PEW Score (95% confidence intervals) |
|---|---|---|
| Sensitivity (%) | 78.6 (60.46, 89.79) | 100 (87.94, 100) |
| Specificity (%) | 59.1 (49.48, 67.97) | 28.6 (20.81, 37.85) |
| PPV (%) | 33.9 (23.53, 45.96) | 27.2 (19.53, 36.48) |
| NPV (%) | 91.2 (82.06, 95.89) | 100 (88.65, 100) |
| PLR | 1.9 (1.79, 2.06) | 1.4 (1.36, 1.44) |
| NLR | 0.4 (0.26, 0.51) | 0 (0, undefined) |
Discussion
PEW is prevalent in patients diagnosed with CKD on MHD and which leads to poor quality of life and a high mortality risk. Early detection of PEW risk with nutrition intervention can help maintaining and improving health outcomes in this group of patients.5, 8, 9 In order to efficiently identify PEW risk, a screening tool or an assessment tool with high validity when compared with NutrE conducted by RDNs using ISRNM diagnostic criteria for PEW is desired.
The 7-point SGA is a validated tool to assess nutritional status in stage 5 CKD patients on MHD but it was not validated to identify PEW risk.14 In using the 7-point SGA to identify PEW risk in this study, the sensitivity, specificity, PPV, NPV, PLR, NLR of the 7-point SGA were calculated when compared to the retrospective NutrE conducted by RDNs using the ISRNM diagnostic criteria for PEW. In reviewing the components of the 7-point SGA and comparing with the NutrE in this study, all components in the 7-point SGA (weight change, dietary intake, gastrointestinal symptoms, functional capacity, disease state/comorbidities, and physical exam) were also assessed by the retrospective NutrE conducted by RDNs using the ISRNM diagnostic criteria. However, since the 7-point SGA does not have the components on biochemical indicators, this may affect the results in using it in determining PEW risk in stage 5 CKD patients on MHD.28
The PEW Score is a screening tool and it was previously verified in predicting survival in CKD patients on MHD.6 For identifying PEW risk using the PEW Score in this study, the sensitivity, specificity, PPV, NPV, PLR, NLR of the PEW Score were calculated when compared with the retrospective NutrE conducted by RDNs using the ISRNM diagnostic criteria for PEW. As the PEW Score solely uses readily available clinical and biological values at bedside, which here was simulated by examining previously collected data, without considering other components like appetite, dietary intake and physical examination, this scoring tool was found to be highly sensitive (100%) but poorly specific (28.6%) in diagnosing PEW in stage 5 CKD patients on MHD. As a result, many patients identified as at PEW risk by the PEW Score may not actually be at risk, but no patients at PEW risk were missed by using the PEW Score.
Both 7-point SGA and the PEW Score were found in this study to be more sensitive than specific in identifying PEW risk. Therefore, both scoring tools may identify PEW risk in patients that may not actually have the risk (false positives). In reviewing the other components in evaluating the validity of the scoring tools in identifying PEW risk, both scoring tools (7-point SGA and the PEW Score) had higher NPV than PPV. Therefore, when either scoring tool identifies a patient as “Not at PEW risk”, the probability of that patient not being at PEW risk is high (91.2% and 100% probability for the 7-point SGA and PEW Score, respectively). However, when either scoring tool identifies a patient as “at PEW risk”, the probability of that patient at PEW risk is low (33.9% and 27.2% probability for the 7-point SGA and PEW Score, respectively). A diagnostic tool with a PLR higher than 10 and a NLR lower than 0.1 is considered being a clinical confident tool to rule in and rule out diagnoses respectively.29 However, based on the findings of our study, the PEW Score is the only diagnostic tool that can provide diagnostic benefit in ruling out patients not at PEW risk.
Clinicians are reminded that some patients with PEW risk may be missed if the 7-point SGA is used as the only diagnostic tool for PEW risk identification due to its lower sensitivity than the PEW Score. Missing patients at PEW risk may lead to serious consequences in patient’s health conditions and which is not desirable. Besides, training is needed for healthcare professionals to use the 7-point SGA accurately. On the contrary, the PEW Score is a simple and easy-to-use screening tool and it is able to capture all patients who are at PEW risk. However, due to its lower specificity than the 7-point SGA, it may falsely capture those not at risk for being at risk for PEW. Providing nutrition intervention to patients not at PEW risk may do no harm to the patients but medical resources may be misused or wasted. Further studies on the combined use of the PEW Score for screening and the 7-point SGA for assessment in identifying PEW risk on patients are recommended as it may possibly improve the overall diagnostic benefits of the scoring tools for PEW risk identification.
There were three limitations of this study. Firstly, this study was limited to a cross-sectional, secondary analysis of adult male and non-pregnant females patients between the ages of 18 to 80 years who had stage 5 CKD on MHD and participated in the research entitled “Development and validation of a predictive energy equation in hemodialysis study” within the Northeastern region of the United States from September 1, 2012 to August 31, 2015. Data were limited to the information obtained from the patient’s medical records and during their research appointment. The RDNs conducting the NutrE did not have the opportunity to assess and interview the patients in-person.
Secondly, the results of the 7-point SGA and the PEW Score were dichotomized as either “At PEW risk” or “Not at PEW risk” for the analysis. As patients may be at different stages of PEW based on the ratings of the scoring tools, such cut-offs may affect the results of the study. For example, patients scored six by the 7-point SGA have at least one abnormal result in one of the components and they may also be at PEW risk. Therefore, further studies determining the appropriate cut-off points for the scoring tools may further strengthen the use of the 7-point SGA and the PEW Score in identifying PEW risk for stage five CKD patients in MHD. Finally, the results of this study showed that none of the patients were originally rated as severely malnourished (score one or two) in the 7-point SGA and only 10 (7.5%) patients were originally rated as severe wasting (score one or zero) in the PEW Score. Such low number of patients in those ratings may affect the overall representations of stage five CKD patients on MHD. A study focusing on patients with lower ratings in the 7-point SGA and the PEW Score may improve the strength of the current study.
Practical Application
This study showed that there are differences in using the 7-point SGA and the PEW Score in identifying PEW risk in stage five CKD patients on MHD. Both of the scoring tools could be used to identify PEW risk based on the results of this study. The 7-point SGA, in addition to being a validated nutrition assessment tool recommended by K/DOQI, can be used to identify PEW risk with a sensitivity of 78.6% and a specificity of 59.1% when compared with NutrE conducted by RDNs using ISRNM diagnostic criteria for PEW. Therefore, by using only the 7-point SGA, clinicians can obtain information on both the nutritional status and the PEW risk status of stage five CKD patients on MHD. The PEW Score is a quick and easy screening scoring tool to identify PEW risk and it has a very high sensitivity (100%) but a very low specificity (28.6%) when compared with NutrE conducted by RDNs using ISRNM diagnostic criteria for PEW in this study. Both scoring tools were found to be clinically confident to rule out patients who are not at PEW risk.
Acknowledgments
The authors thank the collaborating nephrologists, clinical managers and registered dietitian nutritionists at Fresenius Medical Care facilities in Newark, NJ area, Centers for Dialysis Care and University Hospitals in Cleveland, OH area, and Penn State-Hershey Medical Center, in Hershey, PA. We would also like to thank the research staff at Frenova Renal Research LLC and our student research assistants at each study site for their contributions.
Funding Sources:
This work was supported by the National Institutes of Health [grant numbers 1R15DK090593-01A1, 6R15DK090593-02 and 3R15DK090593-02S1]
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Simon Siu-Man Sum, Rutgers University, Newark, New Jersey, USA Herbalife International of America, Inc., Torrance, California, USA.
Andrea F. Marcus, School of Health Professions, Rutgers University, Newark, New Jersey, USA.
Debra Blair, Fresenius Kidney Care, Hampshire County Dialysis, Northampton, MA, USA.
Laura A. Olejnik, US Renal Care, Inc., Downers Grove, IL, USA.
Joyce Cao, Herbalife International of America, Inc. Torrance, California, USA.
J. Scott Parrott, School of Health Professions, Rutgers University, Newark, New Jersey, USA.
Emily N. Peters, School of Health Professions, Rutgers University, Newark, New Jersey, USA.
Rosa K. Hand, School of Medicine, Case Western Reserve University, Cleveland, Ohio, USA.
Laura D. Byham-Gray, School of Health Professions, Rutgers University, Newark, New Jersey, USA.
References
- 1.United States Renal Data System. 2015 USRDS annual data report: Epidemiology of kidney disease in the United States. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2015. [Google Scholar]
- 2.Bonanni A, Mannucci I, Verzola D, et al. Protein-energy wasting and mortality in chronic kidney disease. International journal of environmental research and public health. 2011 May;8(5):1631–1654. doi: 10.3390/ijerph8051631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Foucan L, Merault H, Velayoudom-Cephise FL, Larifla L, Alecu C, Ducros J. Impact of protein energy wasting status on survival among Afro-Caribbean hemodialysis patients: a 3-year prospective study. SpringerPlus. 2015;4:452. doi: 10.1186/s40064-015-1257-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gracia-Iguacel C, Gonzalez-Parra E, Perez-Gomez MV, et al. Prevalence of protein-energy wasting syndrome and its association with mortality in haemodialysis patients in a centre in Spain. Nefrologia: publicacion oficial de la Sociedad Espanola Nefrologia. 2013;33(4):495–505. doi: 10.3265/Nefrologia.pre2013.Apr.11979. [DOI] [PubMed] [Google Scholar]
- 5.Jadeja YP, Kher V. Protein energy wasting in chronic kidney disease: An update with focus on nutritional interventions to improve outcomes. Indian journal of endocrinology and metabolism. 2012 Mar;16(2):246–251. doi: 10.4103/2230-8210.93743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Moreau-Gaudry X, Jean G, Genet L, et al. A simple protein-energy wasting score predicts survival in maintenance hemodialysis patients. Journal of renal nutrition: the official journal of the Council on Renal Nutrition of the National Kidney Foundation. 2014 Nov;24(6):395–400. doi: 10.1053/j.jrn.2014.06.008. [DOI] [PubMed] [Google Scholar]
- 7.Rambod M, Bross R, Zitterkoph J, et al. Association of Malnutrition-Inflammation Score with quality of life and mortality in hemodialysis patients: a 5-year prospective cohort study. American journal of kidney diseases: the official journal of the National Kidney Foundation. 2009 Feb;53(2):298–309. doi: 10.1053/j.ajkd.2008.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Obi Y, Qader H, Kovesdy CP, Kalantar-Zadeh K. Latest consensus and update on protein-energy wasting in chronic kidney disease. Current opinion in clinical nutrition and metabolic care. 2015 May;18(3):254–262. doi: 10.1097/MCO.0000000000000171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Carrero JJ, Stenvinkel P, Cuppari L, et al. Etiology of the protein-energy wasting syndrome in chronic kidney disease: a consensus statement from the International Society of Renal Nutrition and Metabolism (ISRNM) Journal of renal nutrition: the official journal of the Council on Renal Nutrition of the National Kidney Foundation. 2013 Mar;23(2):77–90. doi: 10.1053/j.jrn.2013.01.001. [DOI] [PubMed] [Google Scholar]
- 10.As’habi A, Tabibi H, Nozary-Heshmati B, Mahdavi-Mazdeh M, Hedayati M. Comparison of various scoring methods for the diagnosis of protein-energy wasting in hemodialysis patients. International urology and nephrology. 2014 May;46(5):999–1004. doi: 10.1007/s11255-013-0638-1. [DOI] [PubMed] [Google Scholar]
- 11.de Roij van Zuijdewijn CL, Ter Wee PM, Chapdelaine I, et al. A Comparison of 8 Nutrition-Related Tests to Predict Mortality in Hemodialysis Patients. Journal of renal nutrition: the official journal of the Council on Renal Nutrition of the National Kidney Foundation. 2015 Mar 25; doi: 10.1053/j.jrn.2015.02.005. [DOI] [PubMed] [Google Scholar]
- 12.Vegine PM, Fernandes AC, Torres MR, Silva MI, Avesani CM. Assessment of methods to identify protein-energy wasting in patients on hemodialysis. Jornal brasileiro de nefrologia: ‘orgao oficial de Sociedades Brasileira e Latino-Americana de Nefrologia. 2011 Mar;33(1):55–61. [PubMed] [Google Scholar]
- 13.Beberashvili I, Azar A, Sinuani I, et al. Comparison analysis of nutritional scores for serial monitoring of nutritional status in hemodialysis patients. Clinical journal of the American Society of Nephrology: CJASN. 2013 Mar;8(3):443–451. doi: 10.2215/CJN.04980512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Steiber A, Leon JB, Secker D, et al. Multicenter study of the validity and reliability of subjective global assessment in the hemodialysis population. Journal of renal nutrition: the official journal of the Council on Renal Nutrition of the National Kidney Foundation. 2007 Sep;17(5):336–342. doi: 10.1053/j.jrn.2007.05.004. [DOI] [PubMed] [Google Scholar]
- 15.Steiber AL, Kalantar-Zadeh K, Secker D, McCarthy M, Sehgal A, McCann L. Subjective Global Assessment in chronic kidney disease: a review. Journal of renal nutrition: the official journal of the Council on Renal Nutrition of the National Kidney Foundation. 2004 Oct;14(4):191–200. [PubMed] [Google Scholar]
- 16.Olejnik LA, Peters EN, Parrott JS, et al. Abbreviated Steady State Intervals for Measuring Resting Energy Expenditure in Patients on Maintenance Hemodialysis. JPEN Journal of parenteral and enteral nutrition. 2016 Jul 27; doi: 10.1177/0148607116660981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Detsky AS, McLaughlin JR, Baker JP, et al. What is subjective global assessment of nutritional status? JPEN Journal of parenteral and enteral nutrition. 1987 Jan-Feb;11(1):8–13. doi: 10.1177/014860718701100108. [DOI] [PubMed] [Google Scholar]
- 18.Kent PS, McCarthy MP, Burrowes JD, et al. Academy of Nutrition and Dietetics and National Kidney Foundation: revised 2014 standards of practice and standards of professional performance for registered dietitian nutritionists (competent, proficient, and expert) in nephrology nutrition. Journal of the Academy of Nutrition and Dietetics. 2014 Sep;114(9):1448–1457 e1445. doi: 10.1016/j.jand.2014.05.006. [DOI] [PubMed] [Google Scholar]
- 19.Fouque D, Kalantar-Zadeh K, Kopple J, et al. A proposed nomenclature and diagnostic criteria for protein-energy wasting in acute and chronic kidney disease. Kidney international. 2008 Feb;73(4):391–398. doi: 10.1038/sj.ki.5002585. [DOI] [PubMed] [Google Scholar]
- 20.Sabatino A, Regolisti G, Karupaiah T, et al. Protein-energy wasting and nutritional supplementation in patients with end-stage renal disease on hemodialysis. Clinical nutrition. 2016 Jun 18; doi: 10.1016/j.clnu.2016.06.007. [DOI] [PubMed] [Google Scholar]
- 21.Academy of Nutrition and Dietetics. International Dietetics and Nutrition Terminology (IDNT) Reference Manual: Standard Language for the Nutrition Care Process. 4th. Chicago, IL: 2012. [Google Scholar]
- 22.Boston University. School of Public Health. Screening for disease. 2016 http://sphweb.bumc.bu.edu/otlt/MPH-Modules/EP/EP713_Screening/. Accessed August 25, 2016.
- 23.Ebell M, Barry H. Evidence-Based Medicine Course. 2008 http://omerad.msu.edu/ebm/index.html. Accessed August 30, 2016.
- 24.Dean AG, Sullivan KM, Soe MM. Open Source Epidemiologic Statistics for Public Health, 3.01. www.OpenEpi.com. Accessed August 30, 2016.
- 25.Hess AS, Shardell M, Johnson JK, et al. Methods and recommendations for evaluating and reporting a new diagnostic test. European journal of clinical microbiology & infectious diseases: official publication of the European Society of Clinical Microbiology. 2012 Sep;31(9):2111–2116. doi: 10.1007/s10096-012-1602-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jones SR, Carley S, Harrison M. An introduction to power and sample size estimation. Emergency medicine journal: EMJ. 2003 Sep;20(5):453–458. doi: 10.1136/emj.20.5.453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Viera AJ, Garrett JM. Understanding interobserver agreement: the kappa statistic. Family medicine. 2005 May;37(5):360–363. [PubMed] [Google Scholar]
- 28.Gowda S, Desai PB, Kulkarni SS, Hull VV, Math AA, Vernekar SN. Markers of renal function tests. North American journal of medical sciences. 2010 Apr;2(4):170–173. [PMC free article] [PubMed] [Google Scholar]
- 29.Deeks JJ, Altman DG. Diagnostic tests 4: likelihood ratios. Bmj. 2004 Jul 17;329(7458):168–169. doi: 10.1136/bmj.329.7458.168. [DOI] [PMC free article] [PubMed] [Google Scholar]


