Abstract
Externalizing symptoms robustly predict adolescent substance use (SU); however, findings regarding internalizing symptoms have been mixed, suggesting that there may be important moderators of the relationship between internalizing problems and SU. The present study used a longitudinal community sample (N=387, 55% female, 83% White) to test whether externalizing symptoms moderated the relationship between internalizing symptoms and trajectories of alcohol and marijuana use from early (age 11–12 years old) to late (age 18–19 years old) adolescence. Two-part latent growth models were used to distinguish trajectories of probability of use from trajectories of amount of use among users. Results suggested that externalizing symptoms moderated the association between internalizing symptoms and probability of alcohol, but not marijuana use. The highest probability of alcohol use was observed at high levels of externalizing symptoms and low levels of internalizing symptoms. A negative protective effect of internalizing symptoms on probability of alcohol use was strongest in early adolescence for youth high on externalizing symptoms. Although moderation was not supported for amount of use among users, both domains of symptomology were associated with amount of alcohol and marijuana use as first-order effects. High levels of externalizing symptoms and low levels of internalizing symptoms were associated with high levels of amount of use among users. These findings suggest that developmental models of substance use that incorporate internalizing symptomology should consider the context of externalizing problems and distinguish probability and amount of use.
Keywords: Internalizing problems, externalizing problems, substance use, trajectories
Many developmental models of adolescent substance use (SU) include mental health symptoms, which are commonly organized into two broad domains of externalizing symptoms (e.g., delinquency and aggression) and internalizing symptoms (e.g., anxiety and depression; Achenbach & Rescorla, 2001; Lahey et al., 2004). Externalizing symptoms (e.g., delinquency, aggression) robustly predict adolescent SU and evidence accumulated from decades of research support externalizing symptoms as part of a developmental cascade that sets in motion a sequence of negative socialization processes that culminate in early onset and escalation of SU (e.g., Dodge et al., 2009).
Although internalizing symptoms are frequently discussed as being involved in the etiology of adolescent SU often through a self-medication mechanism (Khantzian, 1997), the association between this domain of symptoms and adolescent SU has been equivocal (Colder, Chassin, Lee, & Villalta, 2010; Hussong, Jones, Stein, Baucom, & Boeding, 2011). One possible explanation for mixed findings is that the association between internalizing symptoms and adolescent SU may depend on other moderating variables. Given the high rates of co-occurrence of internalizing and externalizing symptoms in adolescence (Angold, Costello, & Erkanli, 1999) and the robust pathway from externalizing symptoms to adolescent SU, externalizing symptoms are an important context within which to consider the effects of internalizing symptoms on SU. Although studies have found that the effects of internalizing symptoms on adolescent SU are diminished when statistically controlling for externalizing symptoms (e.g., King, Iacono, & McGue, 2004), few studies have considered externalizing symptoms as a potential moderator. Another possibility is that the risk or protective status of internalizing symptoms may depend on whether growth in the probability of use or amount of use is examined as the outcome. In this paper, we test whether externalizing symptoms moderated the association between internalizing symptoms and trajectories of alcohol and marijuana use, and whether this interaction effect operated differently for probability and amount of use using a two-part growth model.
In one of the few developmental accounts of the role of internalizing problems in the development of adolescent SU, Hussong et al. (2011) suggested that the high co-occurrence internalizing and externalizing symptoms and the strong influence externalizing symptoms on SU during this period may obscure the unique effects of internalizing symptoms on adolescent SU. One possibility they considered is that externalizing symptoms may operate as a moderator of the relationship between internalizing symptoms and adolescent SU. A few studies have tested the interaction between externalizing and internalizing symptoms predicting adolescent SU with mixed results. Maslowsky and Schulenberg (2013) found support for a synergistic interaction such that high levels of depressive symptoms were associated with high levels of SU, but only when conduct problems were high. Depression symptoms were unrelated to SU at low levels of conduct problems. This pattern was consistent across alcohol, cigarette, and marijuana use. One key limitation of this study was that the data were cross-sectional, making it difficult to determine direction of effects. This is of concern with respect to the association between depression symptoms and SU as there is evidence that SU can increase depression symptoms (Marmorstein, Iacono, & Malone, 2010; McCarty et al., 2012).
In prior work we used a longitudinal design to test whether the interaction between internalizing and externalizing symptoms in early adolescence (11–12 years old) predicted adolescent alcohol and drug use (a composite of cigarette, marijuana, and other illicit SU) 2 years later (Scalco et al., 2014). Results supported moderation, but contrary to Maslowsky and Schulenberg (2013), the nature of this interaction suggested a protective effect of internalizing symptoms. High levels of internalizing symptoms were prospectively associated with low levels of SU, and this protective effect was only evident at high levels of externalizing problems. This suggests that internalizing symptoms dampen risk associated with externalizing symptoms. Mason, Hitchings, and Spoth (2008) found a similar moderating pattern in a longitudinal study that included early adolescent conduct disorder and depression symptoms (age 11 years) predicting late adolescent SU (age 18 years). In the current study, we extend this prior work by examining whether the interaction between internalizing and externalizing symptoms in early adolescence predict escalation of alcohol and marijuana use during adolescence into young adulthood.
In examining potential interactive effects on trajectories of SU, we distinguished trajectories of probability of use from trajectories of amount of use. In their developmental account, Hussong et al. (2011) posited that youth who experience high levels of internalizing symptoms may be delayed in the onset of SU, but that once initiated, SU would escalate rapidly. Delayed onset for these youth may be due to fear of potential negative consequences of use or because of social withdrawal that protects them from peer contexts that support SU. However, as youth age, SU becomes more normative and acceptable, and perceptions of risk of SU decline (Johnston, O’Malley, Bachman, & Schulenberg, 2010), and these changes may spur drug naïve youth to try alcohol and drugs. Once they initiate, youth experiencing internalizing symptoms may be motivated to use drugs and alcohol to relieve emotional distress through a self-medication mechanism (Johnson, Mullin, Marshall, Bonn-Miller, & Zvolensky, 2010; Khantzian, 1997; Stewart, Zvolensky, & Eifert, 2001), resulting in escalation in levels of use.
This developmental framework suggests that internalizing symptoms may be associated with slow increases in the probability of SU. This protective effect on probability of use might occur regardless of levels of externalizing (unconditional effect) or might be most evident at high levels of externalizing symptoms (moderation) consistent with our prior work (Scalco et al., 2014). In contrast, internalizing symptoms may increase risk for escalation of amount of SU, particularly in the context of high externalizing symptoms (moderation). Youth who experience high levels of internalizing symptoms may be motivated to self-medicate emotional distress, and high levels of externalizing symptoms may place youth in risky peer contexts that provide access to alcohol and drugs and support use. This would be consistent with a synergistic interaction similar to the one supported by Maslowsky and Schulenberg (2013). Although a few studies have examined predictors of trajectories of probability of use and amount of SU, none have examined the proposed interaction between internalizing and externalizing symptoms (e.g., Brown, Catalano, Fleming, Haggerty, & Abbott, 2005; Capaldi, Stoolmiller, Kim, & Yoerger, 2009).
The Current Study
Although prior work has examined whether the interaction between internalizing and externalizing symptoms predict adolescent SU, several important gaps remain in the literature. No studies have considered whether the interaction between internalizing and externalizing symptoms predict trajectories of SU. Furthermore, no studies have distinguished the potential different role of internalizing symptoms on trajectories of probability and amount of SU. The current study addressed these gaps and provides a developmental extension of prior work to clarify the role of internalizing symptoms in etiology of adolescent SU. Since Scalco et al. (2014), we have collected four additional waves of data that now span early (age 11–12) to late adolescence (age 18–19). We model trajectories of use/no use (probability of use) and amount of SU as a two-part growth model (Olsen & Schafer, 2001), and test whether the interaction between internalizing and externalizing symptoms in early adolescence predicts these trajectories.
Method
Participants
The current sample was drawn from a longitudinal study of adolescent SU. A community sample of 387 adolescents and a caregiver was recruited using random-digit dialing (RDD) procedures and both listed and unlisted telephone numbers. RDD was particularly well suited for the current study considering 98.5% of households in sampling frame (Erie County, NY) have a landline. Adolescents were eligible for the study if they were between the ages of 11 or 12 at recruitment, and did not have any disabilities that would preclude them from either understanding or completing the assessment. Recruitment started in April 2007 and was completed in February 2009. For more information about recruitment procedures, eligibility criteria, and sample description see Trucco, Colder, Wieczorek, Lengua, and Hawk (2014).
The current study utilized data from Waves 1 through 7 of the longitudinal project. The average age of participants was 11.6, 12.6, 13.6, 14.6, 15.5, 16.6, and 17.9 at Waves 1–7, respectively. The sample was approximately evenly split on gender (55% female) and was predominantly non-Hispanic Caucasian (83.1%) or African American (9.1%). Median family income at Wave 1 was $70,000 and 6% of the families received public assistance income. The sample demographics compared well to demographics of families within our sampling frame, which was Erie County, NY (see Trucco et al., 2014).
Overall retention across waves was strong; after Wave 1, sample size varied between 354 (91%) to 373 (96%). Chi-square and ANOVA analyses were conducted using data from the first assessment to determine whether there was differential attrition over time. No significant differences between participants who completed all interviews and those not present for at least one assessment were found for minority status (minority vs. majority), Χ2[1, N=386]= 0.72, p=.40, φ=.04), gender, Χ2[1, N=387]= 1.26, p=.26, φ=.06, age, F[1, 386]=0.04, p= .84, d=0.03, parental education (some high school or high school graduate, technical school or some college, college degree or beyond), Χ2[2, N=387]=1.19, p=.55, φ=.05, marital status (caregiver married vs. not married), Χ2[1, N=387]=2.48, p=.12, φ=.08, family income, F[1, 361]=1.29, p=.26, d=0.18, lifetime alcohol, Χ2[1, N=387]=1.82, p=.18, φ=.07 or cigarette use Χ2[1, N=387]=.35, p=.55, φ=.03, internalizing problems, F[1, 386]=2.67, p=.10, d= 0.24, or externalizing problems, F[1, 386]=3.74, p=.05, d=0.27. This lack of differences and associated small effect sizes, the low rate of attrition, and our data analytic approach (full information maximum likelihood estimation), which permitted inclusion of cases with missing data, suggest that missing data likely had a limited impact on our findings.
Procedures
Interviews at Waves 1–3 were conducted annually in university research offices. Transportation was provided for families (1 caregiver and 1 adolescent) upon request. Before beginning the interviews research assistants obtained consent from caregivers and assent from adolescents. Research assistants interviewed the caregiver and adolescent in separate rooms to enhance privacy. Data collection involved the administration of behavioral tasks evaluating different cognitive abilities as well as computer administered questionnaires assessing a wide range of family, peer, and individual level risk and protective factors for the initiation and escalation of adolescent SU. In this report, we focus on behavior problem and SU measures. Families were compensated $75, $85, and $125 dollars at Waves 1–3, respectively.
Waves 4–6 consisted of an annual brief telephone administered audio-Computer Assisted Self Interview (CASI) of SU that took 10–15 minutes to complete. Parents provided consent over the phone and were given a phone number and PIN for their adolescent to use. Assent from the adolescent was obtained at the initiation of the audio-CASI survey.
Wave 7 assessments occurred approximately 13 months after the Wave 6 assessment. Procedures were similar to those used in Waves 1–3. Given the age of our sample at W7, some adolescents had moved away from home and were no longer living locally (most of those who relocated did so to attend college). We did not want to exclude these adolescents from participating and so we offered the option of completing the questionnaires remotely (N=18 or 5% of the W7 sample completed the questionnaires remotely and not in our research offices). Adolescents were compensated $125 for completing the full assessment or $50 for completing only the online questionnaire. Caregivers were compensated $40.
Measures
Substance Use
SU items were taken from National Youth Survey (Elliott & Huizinga, 1983). Marijuana use (including hashish, hash, THC, pot, grass, weed, and reefer) was assessed at W1–W6 with a fill-in-the-blank item that asked adolescent to report how many times in the past year they used marijuana. At W7 the response format changed to 9-point response scale (1 = not at all to 8 = everyday), and this scale was converted to represent the number of days of marijuana use in the past year (e.g., 1 day/week was converted to 52).
Adolescents reported alcohol use without parental permission at W1–W6 using two fill-in-the-blank items (past year frequency and typical number of drinks consumed on drinking days). A drink was defined as 12 ounces of beer, 1 wine cooler (12 oz.), 1 glass of wine (4 oz.), 1 shot of liquor (1 ¼ oz.), or 1 mixed drink. At W7 the response format for past year frequency of alcohol use changed to an 8-point response scale (1=not at all to 8=everyday), and this scale was converted to represent the number of drinking days in the past year as described above. Typical quantity of alcohol use at W7 was assessed using a past 90-day daily drinking calendar (Collins, Parks, & Marlatt, 1985). Typical quantity of consumption at Wave 7 was computed by taking the average number of drinks consumed across drinking days. A quantity by frequency index was created to represent the total number of drinks in the past year for Waves 1–7. For each wave, extreme outliers were assigned values at three standard deviations above the mean (Tabachnick & Fidell, 2007). Descriptive statistics of SU variables are presented in Table 1.
Table 1.
Descriptive information for substance use at all waves (non-users excluded from continuous variables)
|
Alcohol Use
| ||||||||
|---|---|---|---|---|---|---|---|---|
| Original metric
|
Log transformed
|
|||||||
| n | % | M | SD | M | SD | Skew | Kurtosis | |
| W1 | 10 | 2.58 | 0.89 | 0.74 | −0.54 | 1.04 | −.31 | −1.24 |
| W2 | 39 | 10.46 | 4.46 | 9.10 | −0.02 | 1.72 | .38 | .63 |
| W3 | 80 | 21.68 | 5.90 | 14.63 | 0.34 | 1.52 | .85 | .26 |
| W4 | 106 | 28.89 | 13.63 | 19.03 | 1.68 | 1.46 | .06 | −1.00 |
| W5 | 140 | 39.44 | 29.01 | 53.75 | 1.97 | 1.74 | .22 | −.78 |
| W6 | 173 | 49.86 | 42.48 | 73.12 | 2.47 | 1.77 | −.12 | −.77 |
| W7 | 209 | 59.54 | 236.88 | 361.89 | 4.22 | 1.84 | −.29 | −.80 |
|
| ||||||||
| Marijuana Use | ||||||||
|
| ||||||||
| Original metric
|
Log transformed
|
|||||||
| n | % | M | SD | M | SD | Skew | Kurtosis | |
|
| ||||||||
| W1* | 0 | 0 | – | – | – | – | – | – |
| W2* | 7 | 1.88 | 4.86 | 3.18 | 1.36 | .78 | −.64 | .26 |
| W3 | 31 | 8.40 | 8.74 | 10.52 | 1.58 | 1.13 | .12 | −.88 |
| W4 | 45 | 12.26 | 26.13 | 51.14 | 1.91 | 1.65 | .53 | −.82 |
| W5 | 53 | 14.93 | 49.79 | 98.08 | 2.30 | 1.79 | .59 | −.55 |
| W6 | 89 | 25.65 | 38.67 | 81.88 | 2.15 | 1.68 | .61 | −.40 |
| W7 | 164 | 46.72 | 94.61 | 126.79 | 2.90 | 2.20 | .00 | −1.65 |
Note. W = Wave;
Not included in analysis because of low endorsement; n = number of subjects who used alcohol at each wave; Original metric (alcohol) = average number of drinks per drinking episode × number of drinking episodes per year; Original metric (marijuana) = number times smoked marijuana in past year.
Behavior Problems
Hussong et al. (2011) suggested elevated levels of internalizing symptoms in a circumscribed period of time (e.g., a given month or year) may be less germane to trajectories of SU than chronic or stably high internalizing symptoms. Accordingly, we combined symptom reports across 3 years in early adolescence to represent chronic levels of symptoms. Problem behavior was assessed using the Youth Self Report (YSR) form of the Achenbach System of Empirical Behavioral Assessment (ASEBA, Achenbach & Rescorla, 2001). We removed the SU items to eliminate item overlap with our outcomes of interest (alcohol and marijuana use). The rule-breaking (12 items) and aggressive scales (17 items) were combined by taking the average of the items to form an externalizing problems scale score at each wave. Cronbach’s alpha was .95 at each wave. The withdrawn depressed (8 items) and anxious depressed (13 items) scales were combined into an internalizing problems scale at each wave. Cronbach’s alpha ranged from .81 to .87.
Analysis Plan
Hypotheses were tested using structural equation modeling with a latent variable interaction estimated in Mplus version 7.3 (Muthén & Muthén, 1998–2012). Missing data were handled using full information maximum likelihood. Our final model of interest included latent variable interactions between externalizing and internalizing behavior problems predicting growth in SU specified as two-part growth models. Our two-part growth models followed Olsen and Schafer (2001). These models involved simultaneous estimation of dichotomous use (no/yes) and log transformed continuous use when use occurred. When no use occurred in a given year, the corresponding continuous use variable was set to missing. We first modeled growth in the dichotomous and continuous variables separately before estimating the full two-part model. Alcohol and marijuana use were examined in separate models. Marijuana use at Waves 1–2 was rare (see Table 1) as would be expected given the age of our sample. Given the low rates use at these assessments, marijuana use was modeled using Waves 3–7. Alcohol use trajectories were estimated using all waves (Waves 1–7). Time was coded such that the intercept was specified as use at Wave 3 to provide temporal precedence between behavior problems and intercepts of the growth models. We compared a variety of parameterizations of time, including polynomial (linear and quadratic trends), piecewise, and nonlinear proportional change (Bollen & Curran, 2006). We do not report the results of all of these model comparisons, but rather focus on our final most parsimonious and best fitting model. Nested test results are available from the first author upon request.
After the unconditional two-part growth models were estimated we introduced the behavioral problems factors that included the latent variable interactions of interest. Behavior problem factors were estimated using the latent moderated structural equations approach (Klein & Moosbrugger, 2000) with maximum likelihood robust (MLR) estimation. Externalizing and internalizing problems were each specified by three indicators (W1–W3 scale scores). SU growth factors were regressed on the behavior problem factors and their latent interaction. We estimated three conditional growth models by sequentially adding behavior problem latent factors. Model I included internalizing symptoms. Model II included both internalizing and externalizing symptoms, and Model III added the latent interaction. This allowed us to examine how the effect of internalizing symptoms changed when externalizing symptoms was added as a predictor. All models included age and gender as statistical control variables. In the case of statistically significant interaction effects, we plotted model implied trajectories at low (10th and 25th percentile) and high (75th and 90th) levels of behavior problems.
Results
Descriptive Analysis
As expected given the age of our sample, rates, and amount of marijuana (frequency) and alcohol (quantity × frequency) use were low at our earlier waves and increased over time (see Table 1). This suggests that our study was well suited to examine escalation of SU that is common during adolescence. Descriptive statistics and correlations for behavior problem variables at each wave are presented in Table 2. Age and gender at Wave 1 were also included. None of the behavior problem variables correlated significantly with age. All other correlation coefficients were statistically significant and above .20 (no correlation exceeded .75). Across wave stability coefficients were moderate to strong and positive for both clusters of symptoms. Correlations also indicated moderate to strong associations between externalizing and internalizing problems.
Table 2.
Correlation Matrix of Behavior Problem Variables with Means, Standard Deviations, Skewness, and Kurtosis
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | |
|---|---|---|---|---|---|---|---|---|
| 1. Age | .59 | |||||||
| 2. Gender (Female = 0) | −.04a | .50 | ||||||
| 3. W1 Externalizing | .07 | .23a | .19 | |||||
| 4. W2 Externalizing | .02 | .20a | .72 | .21 | ||||
| 5. W3 Externalizing | .10 | .08a | .59 | .75 | .23 | |||
| 6. W1 Internalizing | .07 | .05a | .59 | .37 | .32 | .21 | ||
| 7. W2 Internalizing | −.01 | .01a | .43 | .59 | .51 | .59 | .23 | |
| 8. W3 Internalizing | −.01 | −.12a | .36 | .47 | .59 | .52 | .76 | .23 |
|
| ||||||||
| Means | 12.09 | .45 | .24 | .25 | .27 | .27 | .24 | .23 |
| Skew | −.16 | .20 | 1.52 | 1.46 | 1.25 | .94 | 1.71 | 1.74 |
| Kurtosis | −1.12 | −1.97 | 4.09 | 4.24 | 1.95 | .49 | 3.92 | 4.23 |
Note. W = Wave; Standard deviations on the diagonal; Bolded coefficients are stability estimates
point-biserial correlations are presented.
Unconditional Two-Part Growth Models
Marijuana Growth Models
Non-linear slope factors provided a good fit to the data for both the dichotomous and frequency marijuana use variables. For dichotomous marijuana use, the first four loadings of the slope factor were fixed and the last was freely estimated (0, 1, 2, 3, 5.21 for W3–W7, respectively). We followed the default parameterization for growth models with binary observed variables and estimated the thresholds with intercepts of observed variables constrained to zero. The slope factor mean, M = 0.88, p<.01, and factor loadings indicated an increase in the probability of use that was particularly pronounced between W6 and W7. Significant variance in the intercept, σ2 = 9.01, p<.01, and slope, σ2 = 0.38, p<.05, suggested individual variability in growth trajectories. The intercept and slope factors were unrelated, covariance = −0.58, p>.35. The model chi-square is the only model fit statistic available when modeling growth in binary observed variables, and this index suggested that our model provided a good fit to the data, χ2(25) = 29.10, p>.05.
For frequency of marijuana use among marijuana users, the first two slope factor loadings were fixed and the remainder were freely estimated (0, 1, 1.92, 2.32, 4.30 for W3–W7, respectively). The slope factor mean, M = 0.41, p<.05, suggested an increased in frequency of marijuana use over time for marijuana users, with a sharp increase between W6 and W7 as indicated by the factor loadings. There was significant variance in the intercept, σ2 = 1.0, p<.01, but not in the slope, σ2 = 0.12, p>.30. The intercept-slope covariance was not statistically significant, covariance =−.05, p>.60. This model fit the data well, χ2(7) = 6.52, p>.05, CFI = 1.0, TLI = 1.01, RMSEA = .00.
The final model combined growth factors for both dichotomous and continuous variables into a two-part model. Loadings for the slope factors were constrained to the estimates from the unconditional models and covariances between the growth factors for the dichotomous and continuous variables were estimated. There was no variability in the slope factor for frequency of marijuana use, and therefore, only covariances between intercepts and the slope factor for the dichotomous variables were estimated. The only statistically significant covariance across growth models was between the intercepts, covariance=3.54, p<.01, suggesting that high probability of marijuana use was associated with high frequency of use at Wave 3. The likelihood ratio chi-square test for the growth model for the dichotomous variables suggested good fit to the data, χ2(26) = 28.06, p>.05. No other model fit statistics are available for this model.
Alcohol Growth Models
Non-linear slope factors for the dichotomous and continuous alcohol use variables provided a good fit the data. For the slope factor of the dichotomous variables, the first three factor loadings were fixed and the last four were freely estimated (−2, −1, 0, 0.26, 0.64, 0.93, 1.26 for W1–W7, respectively). The slope mean was positive and statistically significant, M = 2.88, p<.01, suggesting an increasing trend in probability of alcohol use. There was significant variation in the intercept, σ2 = 8.10, p<.01, and slope, σ2 = 1.63, p<.01. The covariance between the intercept and slope was negative, covariance = −1.66, p<.01, suggesting that a high probability of alcohol use at Wave 3 was associated with a slower than average increase in probability of drinking. The final model for the dichotomous variables fit the data well, χ2(119) = 108.07, p>.05.
The non-linear growth model for quantity × frequency of alcohol use for drinkers included fixed factor loadings for the first three waves and then freely estimated loadings thereafter (−2, −1, 0, 2.22, 2.61, 3.77, and 6.86 for W1–W7, respectively). The slope factor mean, M = 0.61, p=.01, and factor loadings suggested that quantity × frequency of use for drinkers increased over time with a particularly steep increase between W6 and W7. There was significant variance in the intercept, σ2 = 0.94, p<.01, and slope, σ2 = 0.02, p<.05, suggesting individual differences in the trajectories. The covariance between the intercept and slope factors was not statistically significant, covariance = 0.02, p=.47. Model fit was significantly improved with the addition of a covariance between use at W5 and W6, covariance = 0.94, p<.01, and this covariance was retained in our final model. The final model provided adequate fit to the data, χ2(19) = 25.89 p>.05, CFI = .95, TLI = .95, RMSEA = .04.
The final model combined growth models for the dichotomous and continuous alcohol variables into a two-part model. Loadings for the slope factors were constrained to the estimates from the unconditional models and covariances across the growth models were freely estimated. Two covariances across the growth models were statistically significant (between the intercepts, covariance=3.87, p<.01, and between the intercept of the continuous variables and the slope of the dichotomous variables, covariance=−0.69, p<.05). The final unconditional two-part alcohol growth model provided a good fit to the data, χ2(119) = 108.08, p>.05.
Conditional Two-Part Growth Models1,2
The behavior problem measurement model (externalizing & internalizing symptoms) was tested before adding these latent factors as predictors to our two-part growth models. Modification indices suggested the addition of covariances across time for internalizing at W1 and W2, and within time covariances for observed symptom variables at W1 and W3. Factor loadings for each indicator were constrained to be equal across waves. The final model fit the data well, χ2(7)= 8.03, p>.05, CFI = .999, TLI = .998, RMSEA = .02. Factor loadings were all statistically significant (p<.05) and standardized loadings ranged between 0.68 and 0.93. There was significant variance in both latent factors (ps < .05), and R2 for the indicators ranged from .46 and .86. Next, these factors were introduced into our two-part growth models.
Conditional Marijuana Growth Models
Resulting path coefficients from the three conditional marijuana models are presented in Table 3. Model I shows that high levels of internalizing symptoms were associated with high probability of marijuana use at W3 (a statistically significant path to the intercept of the dichotomous variables). However, internalizing symptoms emerged as a protective factor when examined in the context of externalizing symptoms (Model II). In Model II, high levels of internalizing symptoms were associated with a low probability of marijuana use at W3 (a marginally statistically significant path to the intercept of the dichotomous variables) and slower than average increase in probability of use (a statistically significant path to the slope of the dichotomous variables). High levels of externalizing symptoms were associated with a high probability of use at W3 and with high frequency of use for users at W3 (statistically significant paths to both intercepts). There was no evidence for the internalizing × externalizing symptom interaction factor predicting the growth factors (Model III).
Table 3.
Conditional Two-Part Growth Model Unstandardized Regression Paths for Marijuana Use
| Dichotomous Portion: Use vs. No Use
|
Continuous Portion: Frequency of Use
|
|||||||
|---|---|---|---|---|---|---|---|---|
| Intercept | Slope | Intercept | Slope | |||||
| Marijuana Model 1 | Est. | SE | Est. | SE | Est. | SE | Est. | SE |
|
|
|
|
||||||
| Age | 1.46** | .46 | −.10 | .12 | .61* | .30 | −.19* | .09 |
| Gender (Female = U) | .13 | .25 | .11 | .07 | −.18 | .17 | .17** | .05 |
| Internalizing | 3.74** | 1.24 | −.72# | .37 | .90 | 1.02 | −.06 | .26 |
| Marijuana Model 2 | ||||||||
|
|
|
|
||||||
| Age | 1.50** | .46 | −.13 | .12 | .67* | .27 | −.21* | .09 |
| Gender (Female = U) | −.07 | .25 | .10 | .07 | −.31# | .16 | .17** | .05 |
| Internalizing | −5.01# | 2.90 | −1.47# | .81 | −4.79* | 1.98 | −.25 | .69 |
| Externalizing | 11.40*** | 2.85 | 1.06 | .83 | 7.25*** | 1.82 | .13 | .60 |
| Marijuana Model 3 | ||||||||
|
|
|
|
||||||
| Age | 1.43** | .47 | −.10 | .12 | .71* | .28 | −.22* | .09 |
| Gender (Female = U) | −.07 | .24 | .10 | .07 | −.32 | .16 | .17** | .05 |
| Internalizing | −3.38 | 2.90 | −1.76* | .84 | −5.31** | 2.04 | −.10 | .71 |
| Externalizing | 11.80*** | 2.89 | .83 | .85 | 6.93*** | 1.94 | .23 | .63 |
| Externalizing × Internalizing | −4.42 | 4.67 | 3.28 | 3.16 | 1.84 | 2.17 | −.52 | .70 |
Note.
p<.10;
p < .05;
p < .01;
p <.001;
Conditional Alcohol Growth Models
The initial conditional models for alcohol use did not converge. However, when the non-significant covariance between the slope and intercept growth factors of the continuous variables was constrained to zero, the models converged without any problems. Hence, subsequent two-part models for alcohol constrained this covariance to be zero. Estimates from the three conditional alcohol models are presented in Table 4. In Model I, internalizing symptoms associations were similar for the growth factors of the dichotomous and continuous variables. High levels of internalizing symptoms were associated with high probability use at W3 and with high quantity × frequency of alcohol use for drinkers at W3 (statistically significant paths to both intercepts). Like the marijuana use models, the effects of internalizing symptoms became more clearly protective when examined in the context of externalizing symptoms (Model II). In Model II, high levels of internalizing symptoms were associated with low probability of alcohol use at W3 and with low quantity × frequency of use for drinkers at W3. High levels of externalizing symptoms were associated with a high probability of alcohol use at W3 and with high levels of quantity × frequency of use for drinkers at W3 (both intercepts), and with slower than average increases in probability of use (slope of the dichotomous variables). The latter effect is likely attributable to low probability of use at earlier waves (e.g., W3) and an increase in probability of use that occurs later for low externalizers relative to high externalizers.
Table 4.
Conditional Two-Part Growth Model Unstandardized Regression Paths for Alcohol Use
| Dichotomous Portion: Use vs. No Use
|
Continuous Portion: Frequency of Use
|
|||||||
|---|---|---|---|---|---|---|---|---|
| Intercept | Slope | Intercept | Slope | |||||
| Alcohol Model 1 | Est. | SE | Est. | SE | Est. | SE | Est. | SE |
|
|
|
|
||||||
| Age | 1.46*** | .31 | −.24 | .24 | .88*** | .19 | −.03 | .04 |
| Gender (Female = 0) | −.30 | .35 | .09 | .26 | −.33 | .24 | .13** | .05 |
| Internalizing | 4.31** | 1.20 | −3.90*** | .86 | 2.62** | .93 | −.47** | .16 |
| Alcohol Model 2 | ||||||||
|
|
|
|
||||||
| Age | 1.43*** | .28 | −.30 | .23 | .90*** | .18 | −.04 | .04 |
| Gender (Female = 0) | −.87** | .33 | .35 | .27 | −.63** | .24 | .14** | .05 |
| Internalizing | −6.95*** | 1.94 | .37 | 1.40 | −3.60* | 1.46 | −.27 | .28 |
| Externalizing | 13.82*** | 2.23 | −5.03** | 1.52 | 7.47*** | 1.55 | −.14 | .28 |
| Alcohol Model 3 | ||||||||
|
|
|
|
||||||
| Age | 1.26*** | .27 | −.18 | .23 | .88*** | .18 | −.04 | .04 |
| Gender (Female = 0) | −.86** | .33 | .32 | .26 | −.64* | .24 | .15** | .05 |
| Internalizing | −5.39** | 1.78 | −.90 | 1.39 | −3.44** | 1.49 | −.30 | .28 |
| Externalizing | 14.90*** | 2.04 | −5.73*** | 1.49 | 7.72*** | 1.58 | −.19 | .29 |
| Externalizing × Internalizing | −10.56** | 3.20 | 6.11** | 2.10 | −1.74 | 2.19 | .33 | .37 |
Note.
p<.10;
p < .05;
p < .01;
p <.001;
Model III shows that the internalizing × externalizing interaction predicted the growth factors for the dichotomous variables, but not for the continuous variables. Our approach to estimating latent variable interactions estimates the latent means to be zero, and hence, the first-order effects in Model III represent the effects of internalizing symptoms at average levels of externalizing, or conversely, the effects of externalizing symptoms at average levels of internalizing symptoms. The conditional trajectories for the growth model of the dichotomous variables are presented in Figure 1 (conditioned on the 25th and 75th percentiles of externalizing symptoms in Panel A and on the 10th and 90th percentiles in Panel B). At the early assessments (W1 and W2), high externalizing symptoms were associated with increased the probability of drinking, and there is little evidence of an effect of internalizing symptoms unless observations were at the extremes of externalizing symptoms. At the extremes of externalizing symptoms, as shown in Panel B, high levels of internalizing symptoms were associated with decreased probability of use, but only among youth at the 90th percentile of externalizing behavior problems. By W7, this protective effect of high internalizing problems was evident for youth both high and low on externalizing symptoms (Panels A and B of Figure 1).
Figure 1.
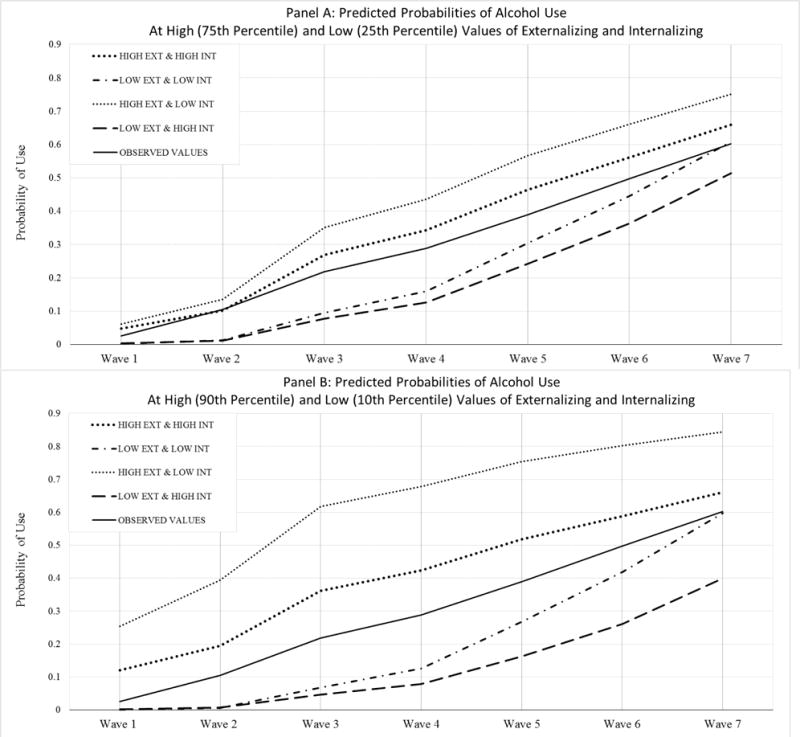
Model Implied Trajectories for Likelihood of Alcohol Use across Levels of Externalizing (EXT) and Internalizing (INT)
To test when the protective effect of internalizing symptoms became similar for youth high and low on externalizing symptoms, we re-estimated six additional growth models changing the specification of the intercept to W1, W2, and W4–W7. The internalizing × externalizing interaction factor was a statistically significant predictor of the intercept for dichotomous variables when it was specified at W1, W2, W4, and W5, βs=−11.80 to −3.23, ps < .05, and the nature of this interaction was similar to that described in our main analysis with W3 specified as the intercept. However, the path coefficient from the internalizing × externalizing interaction factor to the intercept of dichotomous variables was not statistically significant when the intercept was specified at W6 and W7, βs=−2.12 to −3.12, ps>.30. The first-order effect of internalizing symptoms on the W6–W7 intercepts was statistically significant and negative, βs=−2.91 to −3.12, ps<.05. This pattern suggests that internalizing symptoms were protective for youth, regardless of levels of externalizing symptoms at W6 and W7. However, at the earlier waves, internalizing symptoms were only protective for youth high in externalizing symptoms.
Also evident from Figure 1 is that the combination of high externalizing symptoms with low internalizing symptoms is associated with the highest probability of use. This was true at all waves and was most apparent at the extremes of behavior problems. The combination of low externalizing and low internalizing symptoms, descriptive of youth who are free of mental health symptoms, was associated with a low probability of drinking at W1–W3 followed by a more rapid increase than the sample average trajectory (depicted by the solid black line) after W4.
Discussion
The literature examining the association between internalizing symptoms and adolescent SU is mixed with studies showing that internalizing symptoms are unrelated to adolescent SU and operate as both a risk and protective factor (Colder et al., 2010). We examined two issues that may account for these inconsistencies. First, we tested a moderational model whereby externalizing problems were expected to moderate the impact of internalizing symptoms on growth in adolescent SU. Second, we distinguished between trajectories of probability of use and amount of use for users because the risk and protective status of internalizing symptoms may be different for these outcomes. Our findings suggested that externalizing symptoms moderated the association between internalizing symptoms and trajectories of probability of alcohol use, and that this interaction was negative consistent with a protective effect. Although the proposed interaction was not supported for probability of marijuana use, or for frequency of marijuana use or quantity × frequency of alcohol use, there was evidence for protective first-order effects of internalizing symptoms on these outcomes. These findings are considered in turn below.
Our moderational model was only supported for probability of alcohol use, and the nature of this interaction was consistent with internalizing symptoms operating as a protective factor by reducing the likelihood of drinking. This is consistent with internalizing symptoms delaying initiation of alcohol use as suggested by findings of Sung, Erklani, Angold, and Costello (2004). This protective effect showed an interesting developmental pattern. In early and middle adolescence (W1–W5), internalizing symptoms only served a protective function for youth high in externalizing symptoms. However, in late adolescence (W6–W7), there was evidence for a general protective effect internalizing symptoms regardless of levels of externalizing symptoms. High rates of use and early initiation of alcohol use have been linked to externalizing symptoms (e.g., Dodge et al., 2009; King et al., 2004), and this early starter pattern likely provides enough variability in early adolescence for internalizing problems to serve a protective function for youth elevated on externalizing symptoms. Probability of use started out lower and increased later for youth low in externalizing symptoms, and hence, the emergence of the protective effect of internalizing symptoms was delayed for these youth. Prior studies examining mediational pathways suggest that a likely mechanism for this protective effect is that internalizing symptoms decrease affiliations with deviant peers who support and model SU, and who provide access to drugs and alcohol (Fite, Colder, & O’Connor, 2006; Mason et al., 2008; Scalco et al., 2014).
These moderational findings build on similar findings reported in the literature, but offer a richer account of developmental processes. In contrast to prior studies that used only one or two repeated assessments (Mason et al., 2008; Scalco et al., 2014), we used seven time points to chart the unfolding of SU from early adolescence into young adulthood. Moreover, prior work has not distinguished probability of use from amount of use, which is an important distinction when characterizing escalation of use during adolescence. Our findings suggest an important caveat for previously observed interaction effects of externalizing and internalizing symptoms. That is, internalizing symptoms decrease the probability of alcohol use, and the timing of this protective effect depends on the co-occurrence of externalizing symptoms, but this is not true for predicting amounts of use for users (frequency of marijuana or quantity × frequency of alcohol use). This might help explain some inconsistencies in the literature as the association between internalizing symptoms and SU depends on age of the sample, levels of co-occurring externalizing symptoms, and the outcome examined.
Our moderational findings are in contrast with some prior work suggesting heightened risk for adolescent SU as the result of co-occurring high internalizing and high externalizing symptoms (e.g., Marmorstein & Iacono, 2001; Riggs, Baker, Mikulich, Young, & Crowley, 1995). These studies did not formally test moderation, and they used grouping strategies, rather than operationalizing symptoms dimensionally, and included clinical or high risk samples. These differences likely account for discrepancies in findings. The nature of risk associated with co-occurrence of internalizing and externalizing symptoms may very well operate differently in normative community samples, such as the case in our study, versus high risk clinical samples.
In contrast to probability of alcohol use, we found limited support for an interaction predicting growth in probability of marijuana use. Age of onset of marijuana use compared to alcohol use is typically later (Substance Abuse and Mental Health Services Administration, 2010), and this is consistent with prevalence rates of use in our sample as well as others (Johnston, O’Malley, Miech, Bachman, & Schulenberg, 2014). There was no lifetime marijuana use at the first assessment in our study, and rates of marijuana use were consistently lower than rates of alcohol use. As marijuana use continues to increase in later waves, we may begin to see a more robust interaction emerge.
Although the proposed internalizing × externalizing interaction was also not supported as a predictor of growth in amount of use for users (frequency of marijuana use and quantity × frequency of alcohol use), there was evidence for internalizing symptoms as a protective first-order effect on the intercepts of these outcomes. That is, high levels of internalizing symptoms were associated with low frequency of marijuana use and with low quantity × frequency of alcohol use. This protective effect did not emerge until externalizing symptoms was included in the model. Furthermore, in the case of alcohol use, the effect of internalizing problems on the intercept of probability and quantity × frequency of use was positive and flipped to be negative only when externalizing symptoms were included in the model. This pattern was also evident when predicting the intercept for probability of marijuana use and it might further help to explain inconsistencies in the literature. That is, the strength and direction of the association between internalizing symptoms and SU seems to depend on whether unique effects of internalizing symptoms are examined above and beyond externalizing symptoms.
Neither internalizing nor externalizing predicted growth in the amount of use among users (either as a main effect or an interaction). Once an adolescent chooses to use marijuana or alcohol, it is possible that other more proximal cognitive, social, or biological factors influence escalation of amount of use. In the cognitive domain, outcome expectancies are likely to shift after initial experimentation with drugs and alcohol (e.g., Colder et al., 2014; Colder et al., in press) and may be more influential in the escalation in amount of use. Social context may also be important. There is ample evidence that social norms are important influences of adolescent and young adult SU (e.g., Borsari & Carey, 2003) and that youth interested in SU are likely to select into peer groups that support SU (e.g., Scalco, Trucco, Coffman, & Colder, 2015). Hence, after initiation and selection into a substance using peer group, social normative influences may drive escalation in amount of use. In the biological domain, current models of adolescent risk behavior emphasize the role of brain development during this period (Steinberg, 2008). These models emphasize the combination of a rapid increase in motivation for reward and sensations seeking, and slow development of self-regulation to explain increases in adolescent risk behavior, including substance use. These neural changes may play a more proximal role in escalation in amount use relative to internalizing and externalizing symptoms.
Limitations and Conclusions
Results from this study should be understood within the context of certain limitations. First, our study included a community sample that was assessed from early to late adolescence, and may not generalize to high risk or clinical samples, or to older ages as youth transition out of the teen years. There is evidence that the co-occurrence of internalizing and externalizing problems may operate in a synergistic fashion in clinical samples (Riggs et al., 1995) and that internalizing problems more consistently predict SU later in adolescence (Sung et al., 2004) and in early adulthood (Hussong et al., 2011). This suggests that findings regarding interactive effects may depend on sample characteristics. Second, we did not examine use-related problems. Internalizing symptoms may be more strongly linked to use-related problems than to use (Hussong et al., 2011). Examining use-related problems was beyond the scope of the current study, in part because our sample is just now aging into a high risk period for the development of SU problems. However, examining the proposed moderational model with respect to use-related problems remains an important direction for research. Third, internalizing and externalizing symptoms are higher-order symptom domains composed of multiple symptom clusters. Although we did not have strong a priori reasons to expect that the subdomains of externalizing symptoms (e.g., delinquency, aggression) would differentially moderate the association of internalizing symptoms with SU, we did consider potential unique effects of anxiety and depression symptoms (see Footnote 1), and there was little difference in our findings across these symptom clusters. There are other symptom clusters that might be of interest to the moderational model we propose (e.g., post-traumatic stress, social anxiety symptoms). A useful direction for future research may be to extend our work to consider other internalizing symptom clusters.
Despite these limitations our findings inform current developmental models of adolescent SU (Dodge et al., 2009; Zucker, 2006). There is currently no developmental model that accounts for the role of internalizing symptoms in the etiology of adolescent SU. Our findings suggest that such a developmental model would need to consider the effect of internalizing symptoms in the context of co-occurring externalizing symptoms and to distinguish trajectories use/no use and amount of use that span early to late adolescence. Considering co-occurrence with externalizing problems from a longitudinal perspective will help clarify the association between internalizing symptoms and adolescent SU. The protective effect of internalizing symptoms that we observed calls into question whether self-medication models of SU are relevant to adolescent SU in the general population. Furthermore, our findings suggest that preventive interventions for adolescent SU that target internalizing symptoms may have limited utility for unselected community adolescents.
Acknowledgments
This research was funded by a grant from the National Institute on Drug Abuse (R01 DA019631) awarded to Dr. Craig R. Colder.
Footnotes
Conflict of Interest: The authors declare that they have no conflict of interest.
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent: Informed consent was obtained from all individual participants included in the study.
We also considered the possibility that our proposed moderational model might be different for anxiety and depression symptoms. There is some evidence that subdomains of internalizing symptoms may operate differently in the etiology of adolescent SU (Colder et al., 2010). Accordingly, we used the ASEBA Diagnostic Statistical Manual (DSM) – oriented scales for anxiety and affective symptoms (depression symptoms), and tested interactions between these clusters of symptoms and externalizing symptoms. Interaction effects for anxiety by externalizing and depression by externalizing replicated across both alcohol and marijuana models. That is, only the slope for probability of alcohol use was predicted by the interaction terms. Moreover, the strength of the anxiety by externalizing and depression by externalizing interactions on the slope were similar, β = 5.51, p<.01 and β = 5.80, p<.01, respectively. This suggests that depression and anxiety do not operate differently in our moderational model predicting trajectories of alcohol and marijuana use.
Multiple group models were used to test for potential gender differences in relations between the symptom variables and growth factors. To do this, we computed observed symptom variables and their cross-products. Nested model tests revealed no significant gender differences in the association of externalizing and internalizing symptoms and the interaction term with marijuana use, Δχ2(12) = 16.02, p>.05, or alcohol use, Δχ2(12) = 12.79, p>.05, growth factors.
References
- Achenbach TM, Rescorla LA. Youth Self-Report for Ages 11–18. Burlington, VT: ASEBA; 2001. [Google Scholar]
- Angold A, Costello EJ, Erkanli A. Comorbidity. Journal of Child Psychology and Psychiatry. 1999;40:57–87. doi: 10.1111/1469-7610.00424. [DOI] [PubMed] [Google Scholar]
- Bollen KA, Curran PJ. Latent curve models: A structural equation perspective. Vol. 467. Hoboken, NJ: John Wiley & Sons; 2006. [Google Scholar]
- Borsari B, Carey KB. Injunctive and descriptive norms in college drinking: A review of the research. Journal of Substance Abuse. 2003;13:391–424. doi: 10.1016/s0899-3289(01)00098-0. [DOI] [PubMed] [Google Scholar]
- Brown EC, Catalano RF, Fleming CB, Haggerty KP, Abbott RD. Adolescent substance use outcomes in the Raising Healthy Children project: A two-part latent growth curve analysis. Journal of Consulting and Clinical Psychology. 2005;73:699–710. doi: 10.1037/0022-006X.73.4.699. [DOI] [PubMed] [Google Scholar]
- Capaldi DM, Stoolmiller M, Kim HK, Yoerger K. Growth in alcohol use in at-risk adolescent boys: Two-part random effects prediction models. Drug and Alcohol Dependence. 2009;105:109–117. doi: 10.1016/j.drugalcdep.2009.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colder CR, Chassin L, Lee MR, Villalta IK. Developmental perspectives: Affect and adolescent substance use. In: Kassel J, editor. Substance abuse and emotion. 2010. pp. 109–135. [DOI] [Google Scholar]
- Colder CR, O’Connor RM, Read JP, Eiden RD, Lengua LJ, Hawk LW, Jr, Wieczorek WF. Growth trajectories of alcohol information processing and associations with escalation of drinking in early adolescence. Psychology of Addictive Behaviors. 2014;28:659–670. doi: 10.1037/a0035271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colder CR, Trucco EM, Lopez-Vergara HI, O’Connor RM, Hawk LW, Wieczorek WF, Eiden RD. Cognitive appraisals of alcohol use in early adolescence: Psychosocial predictors and reciprocal associations with alcohol use. Journal of Early Adolescence. doi: 10.1177/0272431615611256. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins RL, Parks GA, Marlatt GA. Social determinants of alcohol consumption: the effects of social interaction and model status on the self-administration of alcohol. Journal of Consulting and Clinical Psychology. 1985;53:189–200. doi: 10.1037//0022-006x.53.2.189. [DOI] [PubMed] [Google Scholar]
- Dodge KA, Malone PS, Lansford JE, Miller S, Pettit GS, Bates JE. A dynamic cascade model of the development of substance-use onset. Monographs of the Society for Research in Child Development. 2009;74:1–120. doi: 10.1111/j.1540-5834.2009.00528.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elliott DS, Huizinga D. Social class and delinquent behavior in a national youth panel: 1976–1980. Criminology. 1983;21:149–177. [Google Scholar]
- Fite PJ, Colder CR, O’Connor RM. Childhood behavior problems and peer selection and socialization: Risk for adolescent alcohol use. Addictive Behaviors. 2006;31:1454–1459. doi: 10.1016/j.addbeh.2005.09.015. [DOI] [PubMed] [Google Scholar]
- Hussong AM, Jones DJ, Stein GL, Baucom DH, Boeding S. An internalizing pathway to alcohol use and disorder. Psychology of Addictive Behaviors. 2011;25:390–404. doi: 10.1037/a0024519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson K, Mullin JL, Marshall EC, Bonn‐Miller MO, Zvolensky M. Exploring the mediational role of coping motives for marijuana use in terms of the relation between anxiety sensitivity and marijuana dependence. The American Journal on Addictions. 2010;19:277–282. doi: 10.1111/j.1521-0391.2010.00041.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE. Monitoring the Future: National Survey Results on Drug Use, 1975–2009. Volume I: Secondary School Students. Bethesda, MD: National Institute on Drug Abuse (NIDA); 2010. (NIH Publication No. 10-7584). [Google Scholar]
- Johnston LD, O’Malley PM, Miech RA, Bachman JG, Schulenberg JE. Monitoring the Future National Survey Results on Drug Use, 1975–2013: Overview, Key Findings on Adolescent Drug Use. Ann Arbor, MI: Institute for Social Research, The University of Michigan; 2014. [Google Scholar]
- Khantzian EJ. The self-medication hypothesis of substance use disorders: A reconsideration and recent applications. Harvard Review of Psychiatry. 1997;4:231–244. doi: 10.3109/10673229709030550. [DOI] [PubMed] [Google Scholar]
- King SM, Iacono WG, McGue M. Childhood externalizing and internalizing psychopathology in the prediction of early substance use. Addiction. 2004;99:1548–1559. doi: 10.1111/j.1360-0443.2004.00893.x. [DOI] [PubMed] [Google Scholar]
- Klein AG, Moosbrugger H. Maximum likelihood estimation of latent interaction effects with the LMS method. Psychometrika. 2000;65:457–474. doi: 10.1007/BF02296338. [DOI] [Google Scholar]
- Lahey BB, Applegate B, Waldman ID, Loft JD, Hankin BL, Rick J. The structure of child and adolescent psychopathology: generating new hypotheses. Journal of Abnormal Psychology. 2004;113:358–385. doi: 10.1037/0021-843X.113.3.358. [DOI] [PubMed] [Google Scholar]
- Marmorstein NR, Iacono WG. An investigation of female adolescent twins with both major depression and conduct disorder. Journal of the American Academy of Child & Adolescent Psychiatry. 2001;40:299–306. doi: 10.1097/00004583-200103000-00009. [DOI] [PubMed] [Google Scholar]
- Marmorstein NR, Iacono WG, Malone SM. Longitudinal associations between depression and substance dependence from adolescence through early adulthood. Drug and Alcohol Dependence. 2010;107:154–160. doi: 10.1016/j.drugalcdep.2009.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maslowsky J, Schulenberg JE. Interaction matters: Quantifying conduct problem by depressive symptoms interaction and its association with adolescent alcohol, cigarette, and marijuana use in a national sample. Development and Psychopathology. 2013;25:1029–1043. doi: 10.1017/S0954579413000357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mason WA, Hitchings JE, Spoth RL. The interaction of conduct problems and depressed mood in relation to adolescent substance involvement and peer substance use. Drug and Alcohol Dependence. 2008;96:233–248. doi: 10.1016/j.drugalcdep.2008.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarty CA, Wymbs BT, King KM, Mason WA, Stoep AV, McCauley E, Baer J. Developmental consistency in associations between depressive symptoms and alcohol use in early adolescence. Journal of Studies on Alcohol and Drugs. 2012;73:444–453. doi: 10.15288/jsad.2012.73.444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO, editors. Mplus user’s guide. Seventh. Los Angelos, CA: Muthén and Muthén; 1998–2012. [Google Scholar]
- Olsen MK, Schafer JL. A two-part random-effects model for semicontinuous longitudinal data. Journal of the American Statistical Association. 2001;96:730–745. [Google Scholar]
- Riggs PD, Baker S, Mikulich SK, Young SE, Crowley TJ. Depression in substance-dependent delinquents. Journal of the American Academy of Child Adolescent Psychiatry. 1995;34:764–771. doi: 10.1097/00004583-199506000-00017. [DOI] [PubMed] [Google Scholar]
- Scalco MD, Colder CR, Hawk LW, Read JP, Wieczorek WF, Lengua LJ. Internalizing and externalizing problem behavior and early adolescent substance use: A test of a latent variable interaction and conditional indirect effects. Psychology of Addictive Behaviors. 2014;28:828–840. doi: 10.1037/a0035805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scalco M, Trucco EM, Coffman D, Colder CR. Selection and socialization effects in early adolescent alcohol use: A propensity score analysis. Journal of Abnormal Child Psychology. 2015;43:1131–1143. doi: 10.1007/s10802-014-9969-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinberg L. A social neuroscience perspective on adolescent risk-raking. Developmental Review. 2008;28:78–106. doi: 10.1016/j.dr.2007.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart SH, Zvolensky MJ, Eifert GH. Negative-reinforcement drinking motives mediate the relation between anxiety sensitivity and increased drinking behavior. Personality and Individual Differences. 2001;31:157–171. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2009 national survey on drug use and health: Volume I Summary of national findings. Rockville, MD: Office of Applied Studies; 2010. (NSDUH Series H-34A, DHHS Publication No. SMA 10-4586 Findings). [Google Scholar]
- Sung M, Erkanli A, Angold A, Costello EJ. Effects of age at first substance use and psychiatric comorbidity on the development of substance use disorders. Drug and Alcohol Dependence. 2004;75:287–299. doi: 10.1016/j.drugalcdep.2004.03.013. [DOI] [PubMed] [Google Scholar]
- Tabachnick BG, Fidell LS. Using multivariate statistics. 5th. Boston: Pearson/Allyn & Bacon; 2007. [Google Scholar]
- Trucco EM, Colder CR, Wieczorek WF, Lengua LJ, Hawk LW., Jr Early adolescent alcohol use in context: How neighborhoods, parents, and peers impact youth. Development and Psychopathology. 2014;26:425–436. doi: 10.1017/S0954579414000042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zucker RA. Alcoholism: A life span perspective on etiology and course. In: Sameroff AJ, editor. Developmental Psychopathology. 2nd. New York, NY: Kluwer Academic/Plenum Press Publishers; 2006. pp. 569–585. [Google Scholar]


