Abstract
Children with autism spectrum disorder (ASD) require substantial support to address the core symptoms of ASD and co-occurring behavioral/developmental conditions. This study explores the early diagnostic experiences of school-aged children with ASD using survey data from a large probability-based national sample. Multivariate linear regressions were used to examine age when parent reported developmental concern to doctor, received ASD diagnosis, and first obtained services. Children whose parents had concerns about their child's verbal communication reported earlier ages for all outcomes when compared to children of parents who did not have verbal communication concerns. Children whose parents had concerns about their child's nonverbal communication or unusual gestures/movements received an earlier diagnosis than children whose parents did not have these specific concerns.
Keywords: Autism spectrum disorder, national surveys, diagnosis, epidemiology
Autism spectrum disorder (ASD) encompasses a set of complex neurodevelopmental disorders characterized by deficits in social communication and social interaction, as well as restricted or repetitive behaviors or interests (APA, 2013). The number of children diagnosed with ASD has greatly increased in the past decade (Blumberg et al., 2013; CDC, 2014), in part due to increased awareness and a broader conceptualization of ASD (King and Bearman, 2009; Matson and Shoemaker, 2009; Ozonoff et al., 2009; Rice et al., 2012) --- factors likely to influence the use and age of ASD diagnosis. Coincident with the rise in identified ASD is an increasing demand for early detection, evaluation, and treatment of ASD and other developmental disorders (Crane and Winsler, 2008). A current focus on identifying ASD during the first years of life (Johnson and Myers, 2007) is driven in part by emerging evidence that early intensive intervention has led to increased IQ levels, improved communication skills and behavior, and a reduction of the severity of ASD symptoms (Howlin, et al., 2009; Warren et al., 2011). The development of empirically supported clinical tools and strategies have made early ASD identification possible for some young children (Lord and Luyster, 2006). While these advances have ushered in progress toward more children being diagnosed at earlier ages (Pringle et al., 2012), most children with ASD are still not diagnosed until four or older, despite a reported ability for clinicians to diagnose a child as early as the second year of life (CDC, 2014; Esler, 2015).
There is notable variability in the average age at which children are diagnosed with ASD, which is unsurprising given the heterogeneity of symptoms seen among children with an ASD diagnosis (Daniels & Mandell, 2013). Developmental course and symptomatic presentation of ASD may differ by the specific type of ASD diagnosis (e.g. Autistic Disorder, Asperger's Disorder) and by whether the child has a co-occurring condition. An earlier age of ASD diagnosis has been found to be more common in children with Autistic disorder and those with an intellectual disability (CDC, 2014; Landa et al., 2007; Mandell et al., 2005; Shattuck et al., 2009). In addition, certain symptom types (e.g., severe cognitive or language deficits, poor nonverbal communication, repetitive motor mannerisms) may hasten the provision of diagnosis (Maenner et al., 2013; Shattuck et al., 2009).
Several demographic characteristics have been associated with later age of diagnosis; being female or a racial/ethnic minority, living in rural areas, having lower household income, and having multiple primary care physicians (Durkin et al. 2010; Giarelli et al., 2010). Additionally, the referral source for diagnostic evaluation influences the timing of diagnosis, with children referred by an early intervention program being more likely to receive an early diagnosis than those referred by a primary care physician (Twyman et al., 2009). Finally, it should not be overlooked that clinicians often balance the emotional and clinical weight of giving a diagnosis on a family and the potential for symptoms to change, which may contribute to delays in diagnosis (Filipek et al., 1999).
Despite several studies focused on factors that influence the timing of the ASD diagnosis, little research has examined the relation between specific parental concerns and age of diagnosis within a large clinically diverse national dataset. Previous research has found parental concerns about language and communication delays to be some of the earliest reported concerns among parents of children eventually diagnosed with ASD (e.g. Hess & Landa, 2012; Kozlowski et al., 2011). Concerns about behavioral problems typically lag behind verbal communication concerns, perhaps because the range of typical behavior is broad in early childhood and parents may not take particular notice of behavioral clues that their child is veering from typical development until the child has passed the age where certain behaviors are viewed as developmentally appropriate (Werner et al., 2005).
A better understanding of the pathways from early concerns to diagnosis is important for determining how to help families obtain an accurate assessment of their child's development and access services at an earlier age. As parents are in the best position to observe their child's early development, doctors rely on them to monitor developmental milestones and report any concerns they may have. These actions can represent critical first steps towards improving the outcome trajectory and prognosis for children with ASD, by establishing an early parent-professional partnership (Baird et al., 2001).
This study used data from a 2011 probability-based, randomized, national sample of children diagnosed with ASD and explores the diagnostic experiences of families raising a child with ASD, with a focus on the relationship between specific parental concerns and the age parents report concerns to their child's doctor, the age the child receives an ASD diagnosis, and the age the child starts receiving services. It is hypothesized that children with parent-reported verbal communication problems had earlier outcomes, while children with parent-reported behavioral difficulties had later outcomes.
Methods
Data Source
Data used for this study came from the 2011 Survey of Pathways to Diagnosis and Services (“Pathways”), which was a follow-up to the 2009-2010 National Survey of Children with Special Health Care Needs (NS-CSHCN), and was conducted by the National Center for Health Statistics (NCHS) as a module of the State and Local Area Integrated Telephone Survey (SLAITS) and was funded by the National Institute of Mental Health (CDC, 2011). Households eligible to be re-contacted for Pathways had children who were ever diagnosed with ASD, intellectual disability (ID) or developmental delay (DD) at the time of the NS-CSHCN. Pathways was a cross-sectional telephone and mailed survey designed to collect information on the early experiences associated with the emergence and ultimate diagnosis and treatment of ASD, ID, and DD in the United States non-institutionalized child population.
The completion rate for the Pathways survey was 62%, which when multiplied by the 26% response rate of the NS-CSHCN, translates to a 16% overall response rate. While estimates based on telephone surveys with low response rates may be unreliable due to selection biases resulting from sampling, nonresponse, lack of coverage of households without telephones, and respondent classification and reporting errors, the use of sampling weights helps account for the potential nonresponse bias introduced from both surveys. Verbal consent for Pathways and NS-CSHCN was obtained from the parent or guardian respondent (hereafter referred to as the parent) at the time of each interview. Only one child was sampled from a given household; if more than one child was eligible, one was randomly selected. More information about Pathways and NS-CSHCN, including the non-response bias analysis, sampling design and development of sample weights is available at: http://www.cdc.gov/nchs/slaits/spds.htm.
Participants
The Pathways sample included 4,032 children with special health care needs (CSHCN) who were 6-17 years old and whose parent completed the NS-CSHCN and reported at that time that they had once been told by a doctor or other health care provider that their child had ASD, ID, or DD. Inclusion criteria for analysis required a current parent-reported ASD diagnosis at the time of the Pathways survey (n=1,420) (these CSHCN with current ASD will hereafter be referred to simply as “children with ASD” given that few children with ASD lack the need for above routine health and related services that define CSHCN) (CAMHI, 2013). Parents were required to have reported concerns to their child's doctor about their child's development to be included in the statistical analysis (n=1,287).
Measures
Diagnostic criteria
At the time of the 2011 Pathways survey, parents were asked to confirm that they had been told by a “doctor or other health care provider” that their child ever had “autism, Asperger's Disorder, pervasive developmental disorder, or other autism spectrum disorder,” as they indicated during the 2009-2010 NS-CSHCN interview. Parents were then asked a follow-up question after confirming a previous diagnosis: “To the best of your knowledge, does [your child] currently have autism or ASD?” Parents were also asked whether they had been told by a doctor or other health care provider that their child currently has “intellectual disability or mental retardation,” which was first identified in the NS-CSHCN and confirmed in Pathways.
Age outcomes
Age of first reported parental concern, ASD diagnosis, and first services
Parents reported how old their child was when they “first talked to a doctor or other health care provider about their concerns” about their child's development (herein referred to as age of “reported parental concern”), as well as when a doctor or other health care provider first told them their child had ASD. The doctor or other health care provider was a school professional (e.g. school nurse or school psychologist) for approximately 5% of the sample. Parents were also asked at what age(s) their child began receiving specific services to meet his/her developmental needs. It should be noted that these services could occur before the child received a formal ASD diagnosis, and may have been for symptoms unrelated to the child's ASD. The services initiated when the child was the youngest were considered “first services.” Services included the use of physical therapy, social skills training, occupational therapy, speech or language therapy, behavioral intervention or modification services, sensory integration therapy, and cognitive based therapy.
Type of first concern
Parents were asked whether they were concerned about 17 different behaviors, problems, or delayed milestones regarding their child's development when they “first wondered if there might be something not quite right with their child's development.” To reduce the scope of the analyses, like concerns were grouped by the authors into seven categories including verbal communication (talked later than usual, was not talking at all, did not talk as well as other children, some speech skills were lost), medical problems (seizures, lack of physical growth, stomach problems, other medical problems), nonverbal communication (didn't make eye contact when playing or talking with others, didn't respond to sound or when called, didn't understand tone of voice, facial expressions or body language cues), motor problems (problems with coordination, gross motor skills, fine motor skills), behavioral difficulties (sleeping or eating problems, high activity level, wandering, tantrums, aggressive or destructive behavior, difficulty playing or interacting with others, insisted on sameness or had difficulties with change), learning difficulties (difficulty learning new things or skills, and didn't understand what adults asked of him/her), and the presence of unusual gestures/movements (hand-flapping, toe-walking, self-spinning). Based on the age when the parent was first worried about their child's development, parents were only asked about developmental behaviors, problems or milestones that could have occurred before that age. Parents could endorse multiple concerns; it was assumed all concerns occurred at about the same time.
Demographics
Child demographics included child's current age, sex, race/ethnicity, and the presence of younger or older biological siblings. Household characteristics included income (recoded as federal poverty level percentage (U.S. Department of HHS, 2011), highest educational attainment of household members, and family structure (two biological/adoptive/step-parents vs. all other family structures).
Data Analysis
All estimates were calculated using Stata 12.0 (StataCorp, 2011) which accounted for the complex survey design and population weights. Missing data for household income were multiply imputed and provided by NCHS. Demographic and age outcome characteristics are presented in Table 1. Differences between younger (ages 6-11 at the time of the survey) and older children (ages 12-17 at the time of the study) were calculated utilizing t-tests or corrected χ2 tests (presented as F-values to account for the survey design). The presence of specific parental concerns is presented in Table 2, with differences between age cohorts compared through adjusted logistic regressions. The sample was subdivided into a younger and older cohort in order to examine if recent efforts (e.g. Learn the Signs. Act Early – Daniel et al., 2009) to lower the age at which children with ASD are screened, diagnosed and received early intervention services may have changed the reported concerns for the cohorts within the sample. Early identification has been linked to improved outcomes, particularly when children are able to receive early intervention services (Reichow, 2012; Wallace & Rogers, 2010).
Table 1. Demographics and age of outcomes for the population by age cohort.
| Total (n=1,287) | Current Age 6-11 (n=668) | Current Age 12-17 (n=619) | χ2 or t-test value | p-value | |
|---|---|---|---|---|---|
| Child Characteristics | |||||
|
| |||||
| Gender (%) | 0.13 | .72 | |||
| Male | 82.1 | 81.6 | 82.8 | ||
| Female | 17.9 | 18.5 | 17.2 | ||
| Race/ethnicity (%) | 2.85 | .04 | |||
| Non-Hispanic White | 67.9 | 63.5 | 73.2* | ||
| Non-Hispanic Black | 10.5 | 10.1 | 11.0 | ||
| Non-Hispanic Other | 10.4 | 11.7 | 8.8 | ||
| Hispanic | 11.2 | 14.7 | 7.0* | ||
| Presence of Older Sibling (%) | 57.9 | 57.4 | 58.4 | 0.05 | .83 |
| Presence of Younger Sibling (%) | 55.5 | 58.6 | 51.8 | 2.10 | .15 |
| Current Intellectual Disability | 23.9 | 21.4 | 26.9 | 1.67 | .20 |
|
| |||||
| Household Characteristics | |||||
|
| |||||
| Highest Parental Education | |||||
| Level (%) | 0.32 | .72 | |||
| Less than High School | 7.7 | 8.9a | 6.3a | ||
| High School Graduate | 15.3 | 15.6 | 15.1 | ||
| More than High School | 76.9 | 75.5 | 78.6 | ||
| Federal Poverty Level (%) | 3.05 | .03 | |||
| < 100% | 18.4 | 21.3 | 15.3 | ||
| 100 - <200% | 19.3 | 23.0 | 15.7 | ||
| 200 - <400% | 33.9 | 29.2 | 37.4 | ||
| > 400% | 28.4 | 26.5 | 31.6 | ||
| Household Structure (%) | 0.56 | .45 | |||
| Two Parent Household | 70.6 | 72.2 | 68.7 | ||
| Other | 29.4 | 27.8 | 31.3 | ||
|
| |||||
| Age of Outcomesb, years (SE) | |||||
|
| |||||
| Reported Concern to Doctor | 2.50 (0.09) | 2.28 (0.09) | 2.76 (0.15) | -2.75 | <.01 |
| Reported Concern to Schoolc | 3.91 (0.09) | 3.73 (0.10) | 4.12 (0.15) | -2.23 | .03 |
| First Services | 3.90 (0.11) | 3.48 (0.13) | 4.43 (0.19) | -4.10 | <.001 |
| ASD Diagnosis | 5.23 (0.14) | 4.43 (0.15) | 6.21 (0.24) | -6.27 | <.001 |
Notes. ASD = autism spectrum disorder
Estimates have a relative standard error above 30% and may be unreliable.
Differences between age of outcomes were calculated utilizing a weighted t-test.
Parents were asked, “Did you ever talk to a teacher, school nurse, school counselor, or other school professional about your concerns with [your child's] development?” Approximately 91% of parents reported a concern to their child's school as well as their child's doctor. Parents who affirmed they had talked to a school professional were subsequently asked “How old was [your child] when you first talked to a teacher, school nurse, school counselor, or other school professional about your concerns?”
Difference between subgroup is significant at p < .05
Table 2. The likelihood of children belonging to the younger cohort based on specific parental concerns.
| Total (n=1,287) | Current Age 6-11 (n=668) | Current Age 12-17 (n=619) | Adjusted Odds Ratio1 | |
|---|---|---|---|---|
| Specific Concerns (%) | ||||
|
| ||||
| Verbal Communication | 68.9 | 73.0 | 63.9 | 1.69* (1.01-2.81) |
| Behavioral Difficulties | 87.9 | 86.7 | 89.3 | 0.57 (0.27-1.20) |
| Motor Problems | 66.4 | 66.4 | 66.3 | 1.10 (0.72-1.66) |
| Nonverbal Communication | 88.8 | 89.5 | 87.8 | 1.15 (0.67-1.95) |
| Learning Difficulties | 69.7 | 70.5 | 68.7 | 0.94 (0.54-1.64) |
| Unusual Gestures/Movements | 45.0 | 46.9 | 42.8 | 1.13 (0.73-1.76) |
| Medical Problems | 23.1 | 24.4 | 21.5 | 1.24 (0.73-2.12) |
Odds ratios for each specific concern was adjusted by all other concerns
p<.05
Three multivariate linear regressions were used to examine the association between child and household characteristics and the early outcomes of interest (reported parental concern, ASD diagnosis, first services) (see Table 3). Three additional models examined the association between specific parental concerns and the three outcomes of interest, adjusting for child (age cohort, gender, race/ethnicity, presence of younger or older biological siblings, current intellectual disability diagnosis), household demographics (federal poverty level percentage, highest educational attainment of household members, family structure), and whether the parent spoke to the child's school about concerns with their child's development (see Table 4). Age of reported concern was added to the models for ASD diagnosis and age of first services. A series of interaction terms between specific early concerns and age cohort, as well as demographic characteristics and age cohort, were tested for to determine if the relationship between demographic characteristics, specific concerns and age outcomes differed by the age of the children; only significant interactions were kept in the final model. Finally, a series of analyses examined the relationships between age of ASD diagnosis and age of reported concern, and between age of first services and age of reported concern, using linear regressions adjusted for child and household characteristics and whether the parent had spoken to the child's school.
Table 3. Multivariate linear regression models for reported concern, ASD diagnosis, and first services.
| Age Outcome | Reported Concern | ASD Diagnosis | First Services |
|---|---|---|---|
|
| |||
| β̂ (95% CI) | β̂ (95% CI) | β̂ (95% CI) | |
| Characteristics | |||
|
| |||
| Aged 6-11 | -0.56** (-0.93, -0.18) | -1.51*** (-2.04, -0.99) | -0.76*** (-1.11, -0.41) |
| Male | 0.03 (-0.46, 0.51) | -0.09 (-0.74, 0.56) | 0.48* (0.09, 0.87) |
| Race/Ethnicity | |||
| Non-Hispanic White | Reference | Reference | Reference |
| Non-Hispanic Black | 0.43 (-0.33, 1.18) | -0.03 (-0.89, 0.83) | 0.10 (-0.54, 0.73) |
| Non-Hispanic Other | 0.05 (-0.46, 0.56) | -0.39 (-1.46, 0.68) | 0.12 (-0.41, 0.63) |
| Hispanic | 0.28 (-0.51, 1.07) | 0.21 (-0.54, 0.95) | 0.63* (0.02, 1.23) |
| Younger sibling | 0.18 (-0.16, 0.53) | 0.13 (-0.36, 0.62) | 0.21 (-0.15, 0.57) |
| Older sibling | -0.39* (-0.77, -0.02) | 0.39 (-0.10, 0.88) | 0.46** (0.12, 0.81) |
| Current ID | -0.57** (-0.97, -0.17) | -0.43 (-1.03, 0.17) | -0.49* (-0.92, -0.06) |
| Highest Education | |||
| < High School | Reference | Reference | Reference |
| High School | 0.24 (-0.65, 1.13) | 0.22 (-1.08, 1.52) | 0.20 (-0.65, 1.05) |
| > High School | -0.10 (-1.03, 0.82) | 0.29 (-0.94, 1.53) | -0.55 (-1.32, 0.21) |
| Federal Poverty Level | |||
| <100% | Reference | Reference | Reference |
| 100-200% | 0.24 (-0.39, 0.87) | -0.16 (-0.96, 0.64) | 0.25 (-0.47, 0.97) |
| 200-400% | 0.16 (-0.52, 0.83) | -0.64 (-1.49, 0.22) | 0.05 (-0.55, 0.65) |
| >400% | 0.24 (-0.48, 0.96) | -0.36 (-1.21, 0.50) | 0.12 (-0.54, 0.78) |
| Two Parent Household | -0.13 (-0.61, 0.35) | -0.07 (-0.68, 0.55) | -0.26 (-0.68, 0.15) |
| Talked to School | 0.26 (-0.28, 0.79) | 0.31 (-0.42, 1.05) | 0.02 (-0.45, 0.50) |
Notes.
p<.05
p<.01
p<.001
ASD = autism spectrum disorder; ID = intellectual disability
All models are adjusted for child and household characteristics. Child characteristics include child's age, gender, race/ethnicity, the presence of younger or older biological siblings and current intellectual disability diagnosis. Household characteristics include federal poverty level percentage, highest educational attainment of household members, and family structure (two biological/adoptive/step-parents vs. all other family structures). Age of ASD diagnosis and first services were additionally adjusted by age of reported parental concern.
Table 4. Multivariate linear regression models for reported concern, ASD diagnosis, and first services, including parental concerns.
| Age Outcome | Reported Concern | ASD Diagnosis | First Services | |
|---|---|---|---|---|
|
| ||||
| β̂ (95% CI) | β̂ (95% CI) | β̂ (95% CI) | ||
| Parental Concerns | ||||
|
| ||||
| Verbal Communication | -0.79*** (-1.21, -0.38) | -1.71** (-2.69, -0.73) | -0.58* (-1.11, -0.04) | |
| Behavioral Difficulties | 1.04** (0.45, 1.64) | 0.66 (-0.23, 1.55) | -0.05 (-0.77, 0.68) | |
| Motor Problems | -0.14 (-0.48, 0.19) | 0.31 (-0.22, 0.83) | -0.09 (-0.48, 0.29) | |
| Nonverbal Communication | -0.06 (-0.51, 0.39) | -0.91* (-1.66, -0.17) | -0.17 (-0.60, 0.27) | |
| Learning Difficulties | 0.90*** (0.43, 1.38) | 0.07 (-0.60, 0.73) | -0.11 (-0.64, 0.43) | |
| Unusual Gestures/Movements | 0.24 (-0.12, 0.59) | -1.26*** (-1.78, -0.74) | -0.34 (-0.73, 0.05) | |
| Medical Problems | -0.24 (-0.75, 0.26) | 0.48 (-0.09, 1.05) | 0.11 (-0.31, 0.53) | |
Notes.
p<.05
p<.01
p<.001
ASD = autism spectrum disorder; ID = intellectual disability
All models are adjusted for child and household characteristics and whether the parent talked to the child's school regarding concerns about the child's development. Child characteristics include child's age, gender, race/ethnicity, the presence of younger or older biological siblings and current intellectual disability diagnosis. Household characteristics include federal poverty level percentage, highest educational attainment of household members, and family structure (two biological/adoptive/step-parents vs. all other family structures). Age of ASD diagnosis and first services were additionally adjusted by age of reported parental concern.
Results
Table 1 presents demographic estimates of the population subdivided into age cohorts. Children with ASD were predominantly male (82.1%) and came from two parent households (70.6%) and households where the highest educated household member had at least graduated from high school (76.9%). There were few significant demographic differences found between age cohorts. Children in the younger cohort had an earlier age of reported parental concerns (p<.01), service initiation (p<.001) and ASD diagnosis (p<.001) than children in the older cohort. Approximately half (49.2%) of all children received services before their diagnosis (children could receive services for ASD symptoms or developmental delays before a formal diagnosis).
Before children reached 3 years of age, 63.8% had parents who had reported a concern to their child's doctor, 18.5% had received an ASD diagnosis, and 32.3% were receiving services. Additional differences between age cohorts are presented in Figure 1. Children in the younger cohort were more likely than children in the older cohort to have had a parent report a concern to their child's doctor (65.3% vs. 62.0%), received an ASD diagnosis (23.5% vs. 12.5%), and started receiving services (37.3% vs. 26.1%) before turning three years old.
Figure 1. Percentage of children with reported parental concern, first service, and ASD diagnosis before three years of age, by age cohort.
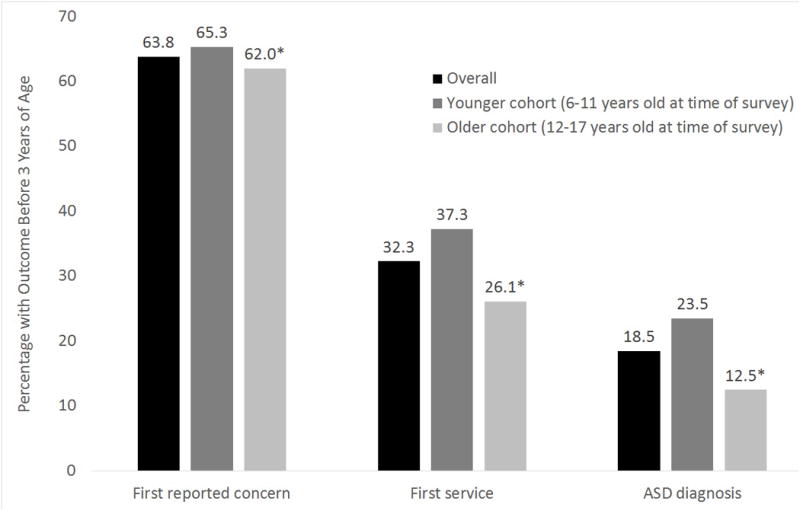
Notes: * p<.05. Differences between the percentage of children who had an outcome before three years of age by cohort were compared with unajdusted logistic regressions.
Table 2 describes the behavioral and developmental characteristics of the population. Behavioral (87.9%) and nonverbal communication concerns (88.8%) were the most commonly endorsed concerns among parents who reported concerns to their child's doctor. Differences were examined between age cohort at the time of the survey, with parents of younger children being more likely to have reported a concern about their child's verbal communication (p<.05) than parents of older children.
Demographic Characteristics
Table 3 contains a separate multivariate linear regression for each of the three age outcomes with a focus on child and household demographics. Younger children had an earlier reported parental concern (β̂ =-0.56, 95% CI: -0.93, -0.18), ASD diagnosis (β̂=-1.51, 95% CI: -2.04, -0.99), and first service (β̂=-0.76, 95% CI: -1.11, -0.41) than older children. Males received services later than females (β̂=0.48, 95% CI: 0.09, 0.87). Children with an older sibling had earlier reported parental concerns (β̂=-0.39, 95% CI: -0.77, -0.02) and later first services (β̂=0.46, 95% CI: 0.12, 0.81) than children without an older sibling. Children currently diagnosed with in intellectual disability had earlier reported parental concerns (β̂=-0.57, 95% CI: -0.97, -0.17) and earlier first services (β̂=-0.49, 95% CI: -0.92, -0.06) than children without an intellectual disability. Finally, Hispanic children received later services than Non-Hispanic White children (β̂=0.63, 95% CI: 0.02, 1.23).
Early Concerns
Table 4 also presents a separate multivariate linear regression for each of the three outcomes, with a focus on early parental concerns, after adjusting for child and household demographics and whether the parent spoke to the child's school. Children with ASD whose parents reported that their first concerns included verbal communication problems had an earlier age of reported parental concern (β̂=-0.79, 95% CI: -1.21, -0.38), ASD diagnosis (β̂=-1.71, 95% CI: -2.69, -0.73), and first services (β̂=-0.58, 95% CI: -1.11, -0.04), than children whose parent did not report a concern about verbal communication. Children whose parents reported a behavioral concern had a later age of reported concern to their child's doctor (β̂=1.04, 95% CI: 0.45, 1.64) as did children whose parents reported learning difficulties (β̂=0.90, 95% CI: 0.43, 1.38) when compared to children whose parents did not have these specific concerns. Children whose parents had concerns about their child's nonverbal communication (β̂=-0.91, 95% CI: -1.66, -0.17) and the presence of unusual gestures and movements (β̂=-1.26, 95% CI: -1.78, -0.74) received an ASD diagnosis earlier than children whose parents did not have these concerns. There was a significant interaction between the child's age cohort and the presence of a parental concern about verbal communication (β̂=1.53, 95% CI: 0.45, 2.61) --- in the older cohort, the difference in age of diagnosis between children with and without parents who had concerns about verbal communication was significantly greater than the difference in the younger cohort. A similar interaction was found between age cohort and a child being Hispanic for age of first service (β̂=1.12, 95% CI: 0.16, 2.08), with delays in first service greater between Hispanic and non-Hispanic children in the older cohort than the younger cohort.
A final series of analyses explored relationships between the three age outcomes and revealed that children whose parents reported concerns to their child's doctor or other health care provider when the child was older received a later ASD diagnosis (β̂=0.57, 95% CI: 0.47, 0.67), and received their first services (β̂=0.71, 95% CI: 0.62, 0.80) later than children whose parents reported concerns when the child was younger (Full model results available upon request).
Discussion
This study found several child characteristics and parental developmental concerns associated with the reported age when parents first spoke to their child's doctor or other health care provider about a developmental concern, the age the child received an ASD diagnosis, and the age the child started receiving services.
Children diagnosed with ASD whose parents reported initial concerns about verbal communication were younger when their parents reported these concerns, when they received an ASD diagnosis and when they began to receive services. Children whose parents noted specific concerns about their child's nonverbal communication and the presence of unusual gestures and movements were diagnosed with ASD at a younger age, findings that are consistent with those in another national sample of children with ASD (Maenner et al., 2013). It has been reported elsewhere that children diagnosed with speech delays and language deficits or with unusual gestures and movements also receive earlier diagnoses (Bickel et al., 2015; De Giacomo and Fombonne, 1998; Mandell et al., 2005), which may additionally be related to the greater availability of services (e.g. speech, occupational, or physical therapy) at a younger age.
The study also revealed a later age of reported parental concern among children whose parents first had noticed behavior difficulties. It has been suggested that a parent may not report a behavioral concern to their child's doctor until after the behaviors are no longer seen as developmentally appropriate. It may be particularly challenging for a parent to recognize behaviors specific to ASD when they occur during early, otherwise, typical development (Herlihy et al., 2015; Werner et al., 2005). This may be compounded by the fact that many children with ASD present with other developmental delays that have a high level of symptom overlap (e.g. ADHD) (Rao & Landa, 2014). For these reasons, Herlihy and colleagues (2015) emphasized the importance of encouraging parents to report any concerns to their child's doctor as early as possible, while similarly encouraging clinicians to probe parents for any concerns, particularly about their older children. Intriguingly, later ages when parents reported behavioral concerns to the doctor did not translate into later ages of first treatment, suggesting despite potential reporting delays, children are receiving important interventions.
Interestingly, there was no relationship found between concerns about motor problems and any of the age outcomes. Motor function has received considerable attention given the notable delays in gross and fine motor skills among children diagnosed with ASD (Fournier et al., 2010). It is possible that much like behavioral problems, parents do not express concern about their child's motor functions until the problem persists past a developmentally appropriate age, but perhaps not to the extent of the previously mentioned behavioral problems.
There were few demographic characteristics associated with the age outcomes of interest. Consistently, younger children had earlier ages for all outcomes, which is consistent with a decline in age of diagnosis in recent cohorts (Fountain et al., 2011), a recent increased recognition of ASD symptoms, and a growing awareness of the need for early identification over the past decade (Matson and Kozlowski, 2011). Study findings may reflect the earliest efforts to lower the age at which children are screened for potential developmental disabilities in the younger cohort (Daniel et al., 2009). A recent examination of children aged four years of age in 2010 and children aged four years of age in 2006 using data from the Autism and Developmental Disabilities Monitoring Network also revealed significant decreases in the age of first diagnosis and age of first comprehensive evaluation in a younger cohort (Christensen et al., 2015).
Children who have an older sibling may have had an earlier age of reported parental concern because they have parents who are more attuned to their child's development, or are more aware of deviations from typical development. Other researchers have found that children with older siblings who were also diagnosed with ASD have parents who report earlier concerns to their child's doctor (Herlihy et al., 2015), and that birth order is a predictor of age of ASD diagnosis (Bickel et al., 2015).
The lack of racial or ethnic differences in the age of diagnosis adds to the currently mixed literature on the subject (Daniels and Mandell, 2013). A later age of service use among Hispanic children relative to Non-Hispanic White children could be the result of the overall difficulties minority populations encounter in attempting to access services (Liptak et al., 2008; Thomas et al., 2007). Hispanic children with ASDs receive fewer specialty services and procedures while having higher unmet services needs when compared to their non-Hispanic peers (Broder-Fingert et al., 2013; Magaña et al., 2013).
Children with ASD who were also diagnosed with an intellectual disability had an earlier age of parental reported concern and service initiation. An intellectual disability may prompt earlier parental concerns about development generally which can result in earlier recognition and intervention by clinicians. In addition, intellectual disability may present as part of a syndrome where genetic or other physical markers are present during the pre- or perinatal period. This combination can also lead to earlier treatment and diagnosis of ASD (De Giacomo and Fombonne, 1998).
A number of study limitations should be considered. First, the study data come from a probability-based national sample of children with special health care needs who were previously diagnosed with ASD who were initially identified in NS-CSHCN and then successfully re-contacted for Pathways. Consequently, the response rate is the product of two survey response rates. Estimates based on telephone surveys with low response rates may be unreliable due to selection biases resulting from sampling, nonresponse, lack of coverage of households without telephones, and respondent classification and reporting errors. The impact of these potential biases on the results presented in this study is unknowable. Therefore, the representativeness of the estimates cannot be confirmed because biases may remain that are not related to known demographics. However, sample weights were calculated in accordance with best practices for sample surveys which included adjustments for known demographic correlates of nonresponse that have been shown to minimize the potential for non-response bias (CDC, 2011). The composition of the analytic sample of children in the current study was compared to the population of children currently diagnosed with ASD from the 2011-2012 National Survey of Children's Health (NSCH), a nationally representative sample of children in the United States. Although children did not differ on the average age of ASD diagnosis, nor on several key demographics (sex, race, household income, family type), children in the current study come from higher educated households than children in the NSCH. This may limit the generalizability of findings, as age outcomes and parental concerns could look differently in children from households with less educated parents.
In addition, Pathways is a cross-sectional survey. Data about first concerns and diagnostic history were collected at only one point in time for children whose ages ranged from 6 to 17 years of age. All parents were asked to reflect over a time period that extended back almost the entirety of their child's life as it related to their child's developmental history and diagnostic experiences. For this reason, parents of the oldest children needed to reflect over the longest reference periods, which could introduce the possibility for differential recall biases as it relates to the accuracy of the parent's report. Additionally, older children had a longer time period than younger children to have experienced all three age-outcomes which translated to later outcomes in the older cohort of children. However, we used interactions terms to explore the difference between cohorts and specific concerns and demographic characteristics and found few differences. We also adjusted appropriate models by the child's age and the age of the first parental concern in the hopes of minimizing this potential bias. Finally, the survey uses parent reports as the sole basis of developmental history and diagnostic data, lacking clinical validation. Children were required to have an ASD diagnosis to be included in the study, but there are likely children in the population who qualify for an ASD diagnosis but simply have not yet been diagnosed. These children would be missed by parental report.
Future studies would benefit from a longitudinal cohort design which would minimize the risk of recall bias, allow for children to be followed for an extended and equal period of time, and accommodate survival analyses which could provide additional insight into the relationship between parental concern, age of ASD diagnosis and age of first service.
Conclusions
As the number of children diagnosed with an ASD has increased in the past decade and efforts to identify and intervene with children early are heightened, it is important to examine the experiences of families raising children with developmental disabilities in the general population. Guidelines offered by the Council on Children with Disabilities of the American Academy of Pediatrics (AAP) (Johnson and Myers, 2007) underscore the importance of early identification, through the use of standardized developmental screening instruments (rather than narrowing attention to just parents' pressing concerns (e.g. behavioral problems)), as well as the importance of referrals to developmental and educational programs for positive outcomes. The lowered ages found for parental reported concern, ASD diagnosis, and service usage for the younger cohort of the present study are consistent with recommendations. However, despite these improvements, overall fewer than 1 in 5 children with ASD had received their ASD diagnosis before age 3, and children whose parents reported concerns to their child's doctor or other health care provider at a later age received a delayed ASD diagnosis, and perhaps more importantly were delayed in entering support services.
Acknowledgments
The authors have no conflicts of interest to disclose, financial or otherwise.
Footnotes
Disclaimer: The findings and conclusions in this paper are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention, the National Institutes of Health, the Health Resources and Services Administration, or Emory University.
Contributor Information
Benjamin Zablotsky, National Center for Health Statistics, 3311 Toledo Road, Hyattsville, MD, 20782, United States.
Lisa J. Colpe, National Institute of Mental Health, Bethesda, MD 20892, United States.
Beverly A. Pringle, National Institute of Mental Health, Bethesda, MD 20892, United States.
Michael D. Kogan, Maternal and Child Health Bureau, Rockville, MD 20857, United States.
Catherine Rice, Emory University, Atlanta, GA 30322, United States.
Stephen J. Blumberg, National Center for Health Statistics, Hyattsville, MD, 20782, United States.
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th. Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- Baird G, Charman T, Cox A, Baron-Cohen S, Swettenham J, Wheelwright S, Drew A. Screening and surveillance for autism and pervasive developmental disorders. Archives of Disease in Childhood. 2001;84(6):468–475. doi: 10.1136/adc.84.6.468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bickel J, Bridgemohan C, Sideridis G, Huntington N. Child and family characteristics associated with age of diagnosis of an autism spectrum disorder in a tertiary care setting. Journal of Developmental and Behavioral Pediatrics. 2015;36:1–7. doi: 10.1097/DBP.0000000000000117. [DOI] [PubMed] [Google Scholar]
- Blumberg SJ, Bramlett MD, Kogan MD, Schieve LA, Jones JR, Lu MC. Changes in prevalence of parent-reported autism spectrum disorder in school-aged U.S. children: 2007 to 2011-2012. National Health Statistics Reports. 2013;65:1–12. [PubMed] [Google Scholar]
- Broder-Fingert S, Shui A, Pulcini CD, Kurowski D, Perrin JM. Racial and ethnic differences in subspecialty service use by children with autism. Pediatrics. 2013;132(1):94–100. doi: 10.1542/peds.2012-3886. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Prevalence of autism spectrum disorders — Autism and Developmental Disabilities Monitoring Network, 11 Sites, United States, 2010. MMWR. 2014;63(2):1–21. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention; National Center for Health Statistics; State and Local Area Integrated Telephone Survey. 2009-2010 National Survey of Children with Special Health Care Needs Frequently Asked Questions. [Accessed May 31, 2014];2011 Available at http://www.cdc.gov/nchs/slaits/cshcn.htm.
- Child and Adolescent Health Measurement Initiative (CAHMI) National Profile of Children with Special Health Care Needs and Autism Spectrum Disorders: Key Findings from the 2009/10 NS-CSHCN and 2011/12 NSCH. [Accessed October 12, 2014];Maternal and Child Health Bureau (MCHB) 2013 Available at http://www.childhealthdata.org.
- Christensen DL, Bilder DA, Zahorodny W, Pettygrove S, Durkin MS, Fitzgerald RT, Yeargin-Allsopp M. Prevalence and Characteristics of Autism Spectrum Disorder Among 4-Year-Old Children in the Autism and Developmental Disabilities Monitoring Network. Journal of Developmental & Behavioral Pediatrics. 2015 doi: 10.1097/DBP.0000000000000235. [DOI] [PubMed] [Google Scholar]
- Crane JL, Winsler A. Early autism detection: Implications for pediatric practice and public policy. Journal of Disability Policy Studies. 2008;18(4):245–253. [Google Scholar]
- Daniel KL, Prue C, Taylor MK, Thomas J, Scales M. ‘Learn the signs. Act early’: A campaign to help every child reach his or her full potential. Public Health. 2009;123:e11–e16. doi: 10.1016/j.puhe.2009.06.002. [DOI] [PubMed] [Google Scholar]
- Daniels AM, Mandell DS. Explaining differences in age at autism diagnosis: a critical review. Autism. 2013;178(5):583–597. doi: 10.1177/1362361313480277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Giacomo A, Fombonne E. Parental recognition of developmental abnormalities in autism. European Child and Adolescent Psychiatry. 1998;3:131–136. doi: 10.1007/s007870050058. [DOI] [PubMed] [Google Scholar]
- Durkin MS, Maenner MJ, Meaney FJ, Levy SE, DiGuiseppi C, Nicholas JS, Schieve LA, et al. Socioeconomic inequality in the prevalence of autism spectrum disorder: Evidence from a U.S. cross-sectional study. PLoS ONE. 2010;5(7):1–8. doi: 10.1371/journal.pone.0011551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esler AN, Hus Bal V, Guthrie W, Wetherby A, Ellis Weismer S, Lord C. The autism diagnostic observation schedule, toddler module: standardized severity scores. Journal of Autism and Developmental Disorders. 2015 doi: 10.1007/s10803-015-2432-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Filipek PA, Accardo PJ, Baranek GT, Cook EH, Jr, Dawson G, Gravel JS, Volkmar FR. The screening and diagnosis of autistic spectrum disorders. Journal of Autism and Developmental Disorders. 1999;29(6):439–484. doi: 10.1023/a:1021943802493. [DOI] [PubMed] [Google Scholar]
- Fountain C, King MD, Bearman PS. Age of diagnosis for autism: individual and community factors across 10 birth cohorts. Journal of Epidemiology and Community Health. 2011;65:503–510. doi: 10.1136/jech.2009.104588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fournier KA, Hass CJ, Naik SK, Lodha N, Cauraugh JH. Motor coordination in autism spectrum disorders: A synthesis and meta-analysis. Journal of Autism and Developmental Disorders. 2010;40(10):1227–1240. doi: 10.1007/s10803-010-0981-3. [DOI] [PubMed] [Google Scholar]
- Giarelli E, Wiggins LD, Rice CE, Levy SE, Kirby RS, Pinto-Martin J, Mandell D. Sex differences in the evaluation and diagnosis of autism spectrum disorders among children. Disability and Health Journal. 2010;3(2):107–116. doi: 10.1016/j.dhjo.2009.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herlihy L, Knoch H, Vibert B, Fein D. Parents' first concerns about toddlers with autism spectrum disorder: Effect of sibling status. Autism. 2015;19(1):20–28. doi: 10.1177/1362361313509731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hess CR, Landa RJ. Predictive and concurrent validity of parent concern about young children at risk for autism. Journal of Autism and Developmental Disorders. 2012;42:575–584. doi: 10.1007/s10803-011-1282-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howlin P, Magiati I, Charman T. Systematic review of early intensive behavioral interventions for children with autism. Journal of Intellectual and Developmental Disabilities. 2009;114(1):23–41. doi: 10.1352/2009.114:23;nd41. [DOI] [PubMed] [Google Scholar]
- Johnson CP, Myers SM. American Academy of Pediatrics Council on Children with Disabilities. Identification and evaluation of children with autism spectrum disorders. Pediatrics. 2007;120(5):1183–1215. doi: 10.1542/peds.2007-2361. [DOI] [PubMed] [Google Scholar]
- King M, Bearman P. Diagnostic change and the increased prevalence of autism. International Journal of Epidemiology. 2009;38(5):1224–1234. doi: 10.1093/ije/dyp261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kozlowski AM, Matson JL, Horovitz M. Parents' first concerns of their child's development in toddlers with autism spectrum disorders. Developmental Neurorehabilitation. 2011;14(2):72–78. doi: 10.3109/17518423.2010.539193. [DOI] [PubMed] [Google Scholar]
- Landa RJ, Holman KC, Garrett-Mayer E. Social and communication development in toddlers with early and later diagnosis of autism spectrum disorders. Archives of General Psychiatry. 2007;64(7):853–864. doi: 10.1001/archpsyc.64.7.853. [DOI] [PubMed] [Google Scholar]
- Liptak GS, Benzoni LB, Mruzek DW, Nolan KW, Thingvoll MA, Wade CM, Fryer GE. Disparities in diagnosis and access to health services for children with autism: data from the National Survey of Children's Health. Journal of Developmental and Behavioral Pediatrics. 2008;29(3):152–160. doi: 10.1097/DBP.0b013e318165c7a0. [DOI] [PubMed] [Google Scholar]
- Lord C, Luyster R. Early diagnosis of children with autism spectrum disorders. Clinical Neuroscience Research. 2006;6(3-4):189–194. [Google Scholar]
- Maenner MJ, Schieve LA, Rice CE, Cunniff C, Giarelli E, Kirby RS, Durkin MS. Frequency and pattern of documented diagnostic features and the age of autism identification. Journal of the American Academy of Child and Adolescent Psychiatry. 2013;52(4):401–413. doi: 10.1016/j.jaac.2013.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mandell DS, Novak MM, Zubritsky CD. Factors associated with age of diagnosis among children with autism spectrum disorders. Pediatrics. 2005;116(6):1480–1486. doi: 10.1542/peds.2005-0185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magaña S, Lopez K, Aguinaga A, Morton H. Access to diagnosis and treatment services among latino children with autism spectrum disorders. Intellectual and Developmental Disabilities. 2013;51(3):141–153. doi: 10.1352/1934-9556-51.3.141. [DOI] [PubMed] [Google Scholar]
- Matson JL, Kozlowski AM. The increasing prevalence of autism spectrum disorders. Research in Autism Spectrum Disorders. 2011;5:418–425. [Google Scholar]
- Matson JL, Shoemaker M. Intellectual disability and its relationship to autism spectrum disorders. Research in Developmental Disabilities. 2009;30(6):1107–1114. doi: 10.1016/j.ridd.2009.06.003. [DOI] [PubMed] [Google Scholar]
- Ozonoff S, Young GS, Steinfeld MB, Hill MM, Cook I, Hutman T, Sigman M. How early do parent concerns predict later autism diagnosis? Journal of Developmental and Behavioral Pediatrics. 2009;30(5):367–375. doi: 10.1097/dbp.0b013e3181ba0fcf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pringle B, Colpe LJ, Blumberg SJ, Avila RM, Kogan MD. Diagnostic history and treatment of school-aged children with autism spectrum disorder and special health care needs. NCHS Data Brief. 2012;97:1–8. [PubMed] [Google Scholar]
- Rao PA, Landa PJ. Association between severity of behavioral phenotype and comorbid attention deficit hyperactivity disorder symptoms in children with autism spectrum disorder. Autism. 2014;18(3):272–280. doi: 10.1177/1362361312470494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reichow B. Overview of meta-analyses on early intensive behavioral intervention (EIBI) for young children with autism spectrum disorders. Journal of Autism and Developmental Disorders. 2012;42:512–520. doi: 10.1007/s10803-011-1218-9. [DOI] [PubMed] [Google Scholar]
- Rice CE, Rosanoff M, Dawson G, Durkin MS, Croen LA, Singer A, Yeargin-Allsopp M. Evaluating changes in the prevalence of the autism spectrum disorders (ASDs) Public Health Reviews. 2012;34(2):1–22. doi: 10.1007/BF03391685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shattuck PT, Durkin M, Maenner M, Newschaffer C, Mandell DS, Wiggins L, Cuniff C. Timing of identification among children with an autism spectrum disorder: Findings from a population-based surveillance study. Journal of the American Academy of Child and Adolescent Psychiatry. 2009;48(5):474–483. doi: 10.1097/CHI.0b013e31819b3848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- StataCorp. Stata Statistical Software: Release 12. College Station TX: StataCorp LP; 2011. [Google Scholar]
- Thomas KC, Ellis AR, McLaurin C, Daniels J, Morrissey JP. Access to care for autism-related services. Journal of Autism and Developmental Disorders. 2007;37:1902–1912. doi: 10.1007/s10803-006-0323-7. [DOI] [PubMed] [Google Scholar]
- Twyman KA, Maxim RA, Leet TL, Ultmann MH. Parents' developmental concerns and age variance at diagnosis of children with autism spectrum disorder. Research in Autism Spectrum Disorders. 2009;3(2):489–495. [Google Scholar]
- U.S. Department of Health and Human Services. 2011 HHS Guidelines. Federal Register. 2011 Jan 20;76(13):3637–3638. [Google Scholar]
- Wallace KS, Rogers SJ. Intervening in infancy: implications for autism spectrum disorders. Journal of Child Psychology and Psychiatry. 2010;51(12):1300–1320. doi: 10.1111/j.1469-7610.2010.02308.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warren Z, McPheeters ML, Sathe N, Foss-Feig JH, Glasser A, Veenstra-VanderWeele J. A systematic review of early intensive intervention for autism spectrum disorders. Pediatrics. 2011;127(5):e1303–e1311. doi: 10.1542/peds.2011-0426. [DOI] [PubMed] [Google Scholar]
- Werner E, Dawson G, Munson J, Osterling J. Variation in early developmental course in autism and its relation with behavioral outcome at 3-4 years of age. Journal of Autism and Developmental Disorders. 2005;35(3):337–350. doi: 10.1007/s10803-005-3301-6. [DOI] [PubMed] [Google Scholar]


