Abstract
STUDY DESIGN
Quasi-experimental clinical trial.
OBJECTIVES
This study compared outcomes from graded exercise and graded exposure activity prescriptions for patients participating in a multidisciplinary rehabilitation program for chronic low back pain. Our primary purpose was to investigate whether pain and disability outcomes differed based on treatment received (graded exercise or graded exposure). Our secondary purpose was to investigate if changes in selected psychological factors were associated with pain and disability outcomes.
BACKGROUND
Behavioral interventions have been advocated for decreasing pain and disability from low back pain, yet relatively few comparative studies have been reported in the literature.
METHODS
Consecutive sample with chronic low back pain recruited over a 16-month period from an outpatient chronic pain clinic. Patients received physical therapy supplemented with either graded exercise (n = 15) or graded exposure (n = 18) principles. Graded exercise included general therapeutic activities and was progressed with a quota-based system. Graded exposure included specific activities that were feared due to back pain and was progressed with a hierarchical exposure paradigm. Psychological measures were pain-related fear (Fear-Avoidance Beliefs Questionnaire, Tampa Scale for Kinesiophobia, Fear of Pain Questionnaire), pain catastrophizing (Coping Strategies Questionnaire), and depressive symptoms (Beck Depression Inventory). Primary outcome measures were pain intensity (visual analog scale) and self-report of disability (modified Oswestry Disability Questionnaire).
RESULTS
Statistically significant improvements (P<.01) were observed for pain intensity and disability at discharge. The rate of improvement did not differ based on behavioral intervention received (P>.05 for these comparisons). Overall, 50% of patients met criterion for minimally important change for pain intensity, while 30% met this criterion for disability. Change in depressive symptoms was associated with change in pain intensity, while change in pain catastrophizing was associated with change in disability.
CONCLUSIONS
Physical therapy supplemented with graded exercise or graded exposure resulted in equivalent clinical outcomes for pain intensity and disability. The overall treatment effects were modest in this setting. Instead of being associated with a specific behavioral intervention, reductions in pain and disability were associated with reductions in depressive symptoms and pain catastrophizing, respectively.
LEVEL OF EVIDENCE
Therapy, level 2b–.
Keywords: behavioral intervention, fear-avoidance model, pain catastrophizing
The Fear-Avoidance Model of Musculoskeletal Pain (FAM) is a psychological model for the development and maintenance of chronic low back pain.27 The original FAM29 and later modified version50,51 propose that the primary affective and cognitive components influencing pain perception are pain-related fear (including fear of movement and reinjury) and pain catastrophizing. These factors interact to determine the individual’s initial behavioral response to pain, which occurs on a continuum from avoidance to confrontation. Long-term avoidance behavior has been hypothesized to have adverse psychological, physical, and societal consequences,5,26,29,51 although evidence for this hypothesis is not absolute.43
Treatment strategies based on the FAM have been described in the literature.6,15,30,48,52 While these treatments vary in their application, they all have the common goal of encouraging a confrontation response. Graded exercise and graded exposure are interventions that have been used to dose exercise and activity for patients with chronic low back pain. Graded exercise involves continually improving exercise and activity tolerance utilizing a quota system instead of pain abatement.12 Graded exposure involves exposing patients to specific situations of which they are fearful during rehabilitation.18,48 Exposure proceeds in a hierarchical fashion, starting with exercise or activity that elicits minimal amounts of fear and then gradually increasing to situations that elicit larger amounts of fear.48,49
Graded exposure is believed to be the more effective intervention option because the activity prescription is specific to feared activities and inclusion of such activities in rehabilitation programs will be more likely to result in favorable clinical outcomes.27 Evidence supporting the effectiveness of graded exposure comes from within-subject studies demonstrating reduction of pain-related fear and disability in comparison to graded exercise.8,48,49 There are fewer available studies offering outcome comparisons for groups of patients receiving graded exposure, and such data could potentially aid clinical decision making.
This study compared pain intensity and disability outcomes for consecutive patients with chronic low back pain who received physical therapy supplemented with graded exposure or graded exercise. Our primary purpose was to determine whether pain intensity and disability outcomes were associated with treatment received (graded exercise or graded exposure). We hypothesized that graded exposure would be associated with superior outcomes, based on the previously reported studies involving within-subject designs.8,48,49 Our secondary purpose was to investigate if changes in selected psychological factors from the FAM were associated with changes in pain intensity and disability. We hypothesized that reduction in pain-related fear and/or pain catastrophizing would be predictive of successful clinical outcomes. These particular FAM variables were investigated because their reduction has been highlighted as important for successful clinical outcomes.16,42,56
METHODS
General Procedures
The University of Florida’s Institutional Review Board approved the protocol for this study. Patients were screened for eligibility by 1 of the authors (V.T.W.), with assistance from his clinical staff. Eligible patients read and signed a consent form approved by The University of Florida Institutional Review Board, before participating in any study-related procedures. After providing informed consent, patients completed self-report questionnaires and, after 4 to 5 weeks, completed a follow-up assessment consisting of the same self-report questionnaires.
Subjects
Consecutive patients were recruited from an interdisciplinary pain rehabilitation program in Jacksonville, FL. Inclusion criteria for this study were the following: (1) between 18 and 70 years of age; (2) ability to read the questionnaires that are part of the protocol (approximately 8th grade reading level); and (3) meet criteria for at least 1 of the following Quebec Task Force on Spinal Disorders1 diagnostic classifications (1c, chronic low back pain without radiation below the gluteal fold; 2c, chronic low back pain with proximal radiation to the knee; 3c, chronic low back pain with distal radiation below the knee; 9.2, postsurgical status more than 6 months after surgical intervention, symptomatic; or 10, chronic pain syndrome).
Exclusion criteria for this study were (1) concurrent musculoskeletal pain in jaw, neck, or shoulder, (2) concurrent diagnosis of fibromyalgia, and (3) meeting any 1 of the following Quebec Task Force on Spinal Disorders diagnostic classifications (1a or 1b, acute or subacute low back pain without radiation below the gluteal fold; 2a or 2b, acute or subacute low back pain with proximal radiation to the knee; 3a or 3b, acute or subacute low back pain with distal radiation below the knee; 4a or 4b or 4c, acute or subacute or chronic low back pain with distal radiation below the knee and neurological signs; 5, presumptive lumbar nerve root compression; 6, confirmed lumbar nerve root compression; 7, confirmed lumbar spinal stenosis; 8, postsurgical status less than 6 months after surgical intervention; 9.1, postsurgical status more than 6 months after surgical intervention, asymptomatic; or 11, other spinal disorders including metastatic disease, visceral disease, or fracture). There were no restrictions of study participation on the basis of sex or race.
Self-report Questionnaires
Patients completed validated self-report questionnaires, consistent with recommended domains for trials of clinical pain.9 These questionnaires were completed in the clinical setting, with research assistants available to answer basic questions related to the questionnaires. The research assistants were specifically instructed not to assist patients in completing the questionnaires.
Pain Intensity
Patients rated pain intensity with a 10-cm visual analog scale, with written descriptors at 0 (“no pain intensity”) and 10 (“maximum pain intensity”). Visual analog scale pain intensity ratings have demonstrated reliability for patients with chronic low back pain,37 and they have been validated as a ratio scale measure for patients with chronic pain.36 Patients were asked to rate their average pain intensity during the past week using the visual analog scale. A similar technique was previously found to be a valid representation of the actual average pain intensity experienced by patients with chronic pain.24
Disability
Disability was assessed with the modified Oswestry Disability Questionnaire (ODQ), which is a disease-specific self-report questionnaire.10,11 The modified ODQ is a 10-item questionnaire and each ODQ item is scored from 0 to 5. Items on the ODQ focus on how much low back pain is limiting activities of daily living, like sitting, standing, walking, and lifting. The ODQ used in this study was modified from the original by substituting a section regarding employment/ home-making ability for the section related to sex life.11,40 This modified version of the ODQ has been found to have high levels of reliability (ICC = 0.90) and responsiveness (effect size, 1.8) in patients with low back pain.11,40 The final score for the ODQ was expressed as a percentage, with higher numbers indicating greater disability (range, 0–100).
Fear of Pain
The Fear of Pain Questionnaire (FPQ-III) was used to measure fear of pain. The FPQ-III is a 30-item, 5-point rating scale (1 [“not at all”] to 5 [“extreme”]) that measures fear about specific situations that would normally produce minor, medical, or severe pain.32 The FPQ-III is a commonly used and well-validated instrument that is appropriate for use in nonclinical and clinical populations.2,32,33 We reported the total score of the FPQ-III, as it best matched the purpose of this study.
Fear-Avoidance Beliefs
The Fear-Avoidance Beliefs Questionnaire (FABQ) was used to quantify fear-avoidance beliefs.53 The FABQ is an 11-item, 7-point rating scale (0 [“strongly disagree”] to 6 [“agree”]), with physical activity and work subscales. The test-retest stability of the FABQ (kappa for individual items, 0.74) has been reported in the literature for patients with chronic low back pain.53 Reliability coefficients ranging from 0.77 to 0.95 have also been reported for the questionnaire.21,23,35,53 The FABQ has been validated in studies demonstrating that it explains unique amounts of variance in work loss and disability, after controlling for other relevant factors.53
Kinesiophobia
The TSK is a 17-item questionnaire, with individual items scored from 1 (strongly disagree) to 4 (strongly agree) and reversed scoring for items 4, 8, 12, and 16. Test- retest reliability has been reported as Pearson r of 0.78 for patients with acute low back pain retaking the TSK within 24 hours.46 Test-retest reliability has also been reported for patients with chronic low back pain over a 76-hour period (ICC = 0.82), with standardized error of the measurement of 3.16.55 Several studies have consistently found poor loading of the reverse-scored items, and it has been recommended that these items be dropped from the questionnaire.20,22,39 Therefore, only the 13 non–reversed-scored items were reported in the current study (TSK-13).
Pain Catastrophizing
The Coping Strategies Questionnaire (CSQ) is a 27-item, 7-point rating scale (from 0 [“never”] to 6 [“always”]) that measures the frequency of use for common pain-coping strategies.41 The CSQ contains a 6-item catastrophizing subscale that measures helpless and pessimistic cognitions related to pain perception. Only the catastrophizing subscale was included in the current study. This subscale is a commonly used and well-validated instrument,25,38,41,44 and we used a revised scoring system (CSQ-R) to report the catastrophizing subscale.38
Depressive Symptoms
The Beck Depression Inventory (BDI) is a 21-item, self-report measure of cognitive, affective, and neurovegetative symptoms of depression.3 Each symptom is rated on a 4-point scale, with higher ratings associated with more depression. The total score of the BDI was reported in this study, as we were interested in the general influence of depressive symptoms.
Treatment
All patients were enrolled in a chronic pain rehabilitation program in Jacksonville, FL. This was an interdisciplinary program that included interaction with clinical psychologists, physical therapists, physicians, case managers, biofeedback therapists, nurses, and occupational therapists. Patients participated in a structured 7-hour day of rehabilitation consisting of set blocks of time with each of the afore-mentioned professionals (TABLE 1). The duration of the program varied for each subject, with typical completion time occurring at 3 to 5 weeks. Individual physical therapy, psychotherapy, biofeedback, and medical follow-up were also provided on a weekly basis. The overall philosophy of the program is one that encourages limited use of opiate medication, education in pain-coping strategies, relaxation training, and intensive musculoskeletal-oriented physical therapy. Psychological treatment and education provided in the program focus on reducing pain-related fear and catastrophizing, altering dysfunctional pain response patterns, and utilizing adaptive coping styles, relaxation techniques, and anger management to assist with pain relief. Psychological treatment also provided cognitive and behavioral strategies to reduce emotional distress.
TABLE 1.
Structure Of Chronic Pain Rehabilitation Program
| Time | monday | Tuesday | Wednesday | Thursday | Friday |
|---|---|---|---|---|---|
| 9:00 AM | Pain education class | Pain education class | Pain education class | Pain education class | Pain education class |
| 10:00 AM | Flexibility training* | Flexibility training* | Flexibility training* | Flexibility training* | Flexibility training* |
| 10:30 AM | Cardiovascular training | Cardiovascular training | Cardiovascular training | Cardiovascular training | Cardiovascular training |
| 11:00 AM | Strength training* | Strength training* | Strength training* | Strength training* | Strength training* |
| 11:15 AM | Relaxation therapy | Relaxation therapy | Relaxation therapy | Relaxation therapy | Relaxation therapy |
| 11:45 AM | Lunch | Lunch | Lunch | Lunch | Lunch |
| 1:00 PM | Flexibility training* | Flexibility training* | Flexibility training* | Flexibility training* | Flexibility training* |
| 1:30 PM | Stabilization* | Stabilization* | Stabilization* | Stabilization* | Stabilization* |
| 2:00 PM | Material handling* | Material handling* | Material handling* | Material handling* | Therapeutic activity* |
| 2:30 PM | Therapeutic exercise* | Therapeutic exercise* | Therapeutic exercise* | Therapeutic exercise* | Therapeutic activity* |
| 3:00 PM | Recreation | Medical follow-up | Treatment review | Break | Pain education class (preparation for weekend) |
| 3:30 PM | Relaxation therapy | Medical follow-up | Relaxation therapy | Patient staffng | Pain education class (preparation for weekend) |
| 4:00 PM | Medical follow-up | Patient staffng | Pain education class (preparation for weekend) |
Indicates time when graded exercise or graded exposure principles were implemented.
In physical therapy an emphasis was placed on evaluation of the musculoskeletal system, with goals of improving physical impairment and function. In this rehabilitation program, patients performed a daily average of 3 hours of exercise and physical activity under the supervision of a physical therapist (TABLE 1). The exercise sessions consisted of flexibility training of the lower extremity and spine, stabilization training for lumbar musculature, strength training for lower and upper extremities, and cardiovascular training. The physical activity sessions consisted of activities that mimicked job duties in material handling, including lifting, carrying, and fine motor skills (ie, assembling and sorting). The physical activity sessions also consisted of activities that mimicked activities of daily living tasks, including cleaning and cooking. For the purposes of this study, either graded exercise or graded exposure principles were used by the physical therapists to dose exercise and physical activity that occurred during flexibility training, strength training, stabilization, material handling, or therapeutic activity (TABLE 1).
Graded Exercise
The physical therapist administered the exercise and physical activity using a quota system similar to that described in the rehabilitation literature.14,15 First, tolerance to the particular exercise and activity prescribed by the therapist was determined. That level was then set as the initial quota. Patient exercise and physical activity was then progressed based on whether the patient met the initial quota or not. Patients meeting the quota received positive reinforcement and an increase in the quota. Those not meeting the quota were encouraged to meet the quota during the next session, and the importance of maintaining activity levels was stressed.
Graded Exposure
The physical therapist administered exercise and physical activity using an exposure paradigm similar to that described in the rehabilitation literature.18 First, exercise and activity that were fearful to the patient were determined using the Fear of Daily Activities Questionnaire (FDAQ).17 The FDAQ is a validated questionnaire that listed 10 activities that patients with chronic low back pain were commonly fearful of, for example, lifting, carrying, twisting, and bending.17 The questionnaire also had 2 options for open-ended responses where the subject could provide additional examples of activities that were feared. Patients rated each of the items using a numerical rating scale that ranged from 0 (no fear) to 100 (maximal fear). The physical therapist selected 2 items that were ranked as most fearful for implementation in the daily exercise and activity program.18 A summary of the fear ratings from the FDAQ and the frequency for each activity considered part of the graded exposure protocol are included in TABLE 2. Initially, the exercise and activity were introduced to the patient at an intensity that did not increase fear. Patients’ exercise and physical activity levels were progressed based on whether they reported decreased fear of the exercise and activity. Those reporting decreased fear received positive reinforcement and the level of the exercise and activity were increased. Patients reporting no change in fear were encouraged to continue exposure at the current intensity.
TABLE 2.
Fear Of Daily Activities Questionnaire(FDAQ) Ratings For Patients Participating In Study*
| Activity | Potential for G† | Mean ± SD | Mode | 25th Percentile | 50th Percentile | 75th Percentile |
|---|---|---|---|---|---|---|
| Sitting for longer than 1h | 9 (8.1%) | 64.3 ± 26.5 | 50 | 50 | 70 | 80 |
| Standing for longer than 30 min | 10 (9.0%) | 63.5 ± 32.8 | 90 | 40 | 75 | 90 |
| Walking for longer than 30 min‡ | 14 (12.6%) | 67.4 ± 32.4 | 100 | 50 | 80 | 90 |
| Lifting less than 20 lb (9.1 kg)‡ | 1 (0.9%) | 40.0 ± 25.6 | 40 | 20 | 40 | 70 |
| Lifting more than 20 lb (9.1 kg)‡ | 17 (15.3%) | 71.8 ± 27.2 | 100 | 50 | 75 | 100 |
| Carrying less than 20 lb (9.1 kg)‡ | 1 (0.9%) | 40.3 ± 28.0 | 30 | 20 | 40 | 70 |
| Carrying more than 20 lb (9.1 kg)‡ | 19 (17.1%) | 71.6 ± 27.6 | 100 | 50 | 70 | 100 |
| Twisting | 18 (16.2%) | 69.5 ± 29.7 | 100 | 60 | 80 | 95 |
| Reaching to floor | 14 (12.6%) | 66.0 ± 32.3 | 100 | 50 | 75 | 100 |
| Performing back exercises‡ | 8 (7.0%) | 49.8 ± 34.2 | 50 | 20 | 50 | 80 |
Patients rated each of these activities on a scale from 0 (no fear) to 100 (maximal fear).
Highly rated FDAQ activities (>40 rating) were considered for graded exposure (GX) treatment, and the 2 highest rated were included in the rehabilitation program. The amounts reported in this column were the numbers the corresponding category was rated as 2 highest (ties included).
Indicates that these activities were routinely included as part of the graded exercise program, but with different exercise prescription parameters.
Treatment Assignment
We were not able to randomly assign treatment for this study. Patients were enrolled on an individual basis into the chronic pain rehabilitation program. These patients were then entered into the group exercise sessions with patients previously enrolled in the program, although exercise parameters differed based on enrollment status. This clinical structure meant that individual randomization would have resulted in treatment contamination. Therefore, we utilized quasi-experimental methodology and compared outcomes for groups of consecutive patients enrolled for this study. It was predetermined that patients enrolled in the first 8 months of the study would receive graded exercise and those enrolled in the next 8 months would receive graded exposure.
Data Analysis
Descriptive statistics were generated for the entire sample for the available demographic, clinical, and self-report variables. Then comparisons were made across the graded exercise and graded exposure interventions using independent t tests and chi-square for continuous and categorical data, respectively. Subsequent data analyses were organized around the 2 purposes of this study. The primary purpose was to determine the effects of graded exercise in comparison to graded exposure on the outcome measures. For this purpose, a separate mixed-model ANOVA was employed for each outcome measure (pain intensity and disability), with time (pretreatment and posttreatment) as the within-subject factor and group (graded exercise and graded exposure) as the between-subject factor.
A planned secondary analysis assessed the association of changes in psychologic variables to changes in outcome measures. These secondary analyses were comprised of a 2-stage process. First, the FABQ, TSK, FPQ, CSQ-R catastrophizing subscale, and BDI variables were assessed with a repeated-measures ANOVA to determine any significant treatment-related changes. Those variables that had a reliable treatment change were used in subsequent analyses to test whether they predicted change in pain intensity or disability. The prediction hypotheses were assessed via correlation of the residualized change scores for the psychologic variable on the residualized change scores of the primary outcome variables (pain intensity and disability). Use of residualized change scores is recommended to avoid statistical errors associated with the use of raw change scores.13 Specifically, residualized change scores were computed for each variable by regressing pretreatment scores on posttreatment scores.7 These residuals (ie, residualized change scores) were then used as the variables in subsequent correlation analyses. This is one way of controlling for regression effects from the influence of the starting level of a variable on the same variable posttreatment.7 Thus, the residual represents the posttreatment effect, with the pretreatment influence removed statistically.
RESULTS
A total of 82 patients entered the pain program during the study period. Patients were excluded for having medical diagnoses or symptom distribution inconsistent with the inclusion criteria (n = 29) or for being unable to independently read the questionnaires (n = 3). Of the 50 patients who were eligible for the study, 33 provided informed consent and participated in the study. TABLE 3 provides a summary of the demographic and clinical measures for the entire sample and for each treatment group. The treatment groups were similar at baseline on each of these measures, including age, sex, type of low back pain, and medication use. Of the 33 that initially enrolled in the study, 24 (72.7%) provided follow-up data related to pain intensity, while 17 (51.5%) provided follow-up data for disability. There were no statistical differences for those completing versus those not completing the study for baseline pain intensity, disability, fear of pain, fear-avoidance beliefs, kinesiophobia, catastrophizing, or depressive symptoms (all P>.05).
TABLE 3.
Demographic and clinical Summary of patients Participating in Graded Exercise and Graded Exposure Outcome Comparison
| Variable | Total Sample (n = 33) |
Graded Exercise (n = 15) |
Graded Exposure (n = 18) |
P Value |
|---|---|---|---|---|
| Sex | .37 | |||
| Males | 16 | 6 | 10 | |
| Females | 17 | 9 | 8 | |
| Age(y) | 45.8 (10.3) | 47.1 (11.9) | 44.8 (9.1) | .54 |
| Education (y) | 12.9 (2.2) | 13.4(2.3) | 12.5(2.2) | .27 |
| Smoking status (n smokers) | 16 | 6 | 10 | .38 |
| Type of LBP (n work-related) | 24 | 9 | 15 | .11 |
| Using opioid medication (n) | 20 | 8 | 12 | .31 |
| Using antidepressant medication (n) | 17 | 10 | 7 | .15 |
Abbreviation: LBP, low back pain
Primary Outcomes by Behavioral Treatment
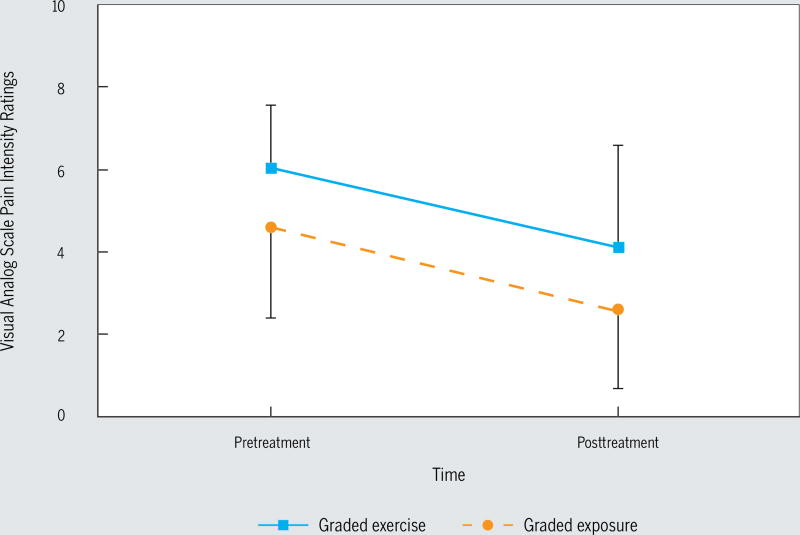
Data describing the changes in pain intensity and pain-related disability are summarized in TABLE 4. There were pretreatment differences in pain intensity, with those patients receiving graded exercise having higher pain scores (P = .04). The group-by-time interaction was not significant, suggesting that both groups responded equivalently to their respective treatments (F1,22 = 0.06, P = .81, η2<0.01). For pain intensity, results indicated a significant main effect for time (F1,22 = 23.8, P<.01, η2 = 0.52), with both groups showing lower pain scores posttreatment. When minimal important change (MIC) was considered, 50% of patients experienced a change that met or exceeded the MIC of 2.0 for pain intensity.34 There was also a main effect of group (F1,22 = 5.5, P = .03, η2 = 0.20), indicating that the graded exercise group had higher pain scores overall. The pain intensity data are depicted in FIGURE 1.
TABLE 4.
Treatment Summery For Primary Outcome And Psychological Measures*
| P value | ||||
|---|---|---|---|---|
| Graded Exercise Group |
Graded Exposure Group |
Interaction† | Time‡ | |
| Primary outcome measures | ||||
| Pain intensity (0–10) | .81 | <01 | ||
| Pretreatment§ | 6.3 ± 1.2 | 4.6 ± 2.1 | ||
| Posttreatment§ | 4.1 ± 2.5 | 2.6 ± 1.9 | ||
| Pain related disability (0–100) | .44 | <01 | ||
| Pretreatment | 56.0 ± 13.9 | 43.3 ± 12.5 | ||
| Posttreatment | 470 ± 171 | 38.0 ± 14.1 | ||
| Psychologic measures | ||||
| Fear of pain (30–150) | .25 | .33 | ||
| Pretreatment | 63.3 ± 18.1 | 80.6 ± 22.0 | ||
| Posttreatment | 64.4 ± 22.0 | 677 ± 28.9 | ||
| Fear-avoidance beliefs, physical activity (0–24) | .39 | .08 | ||
| Pretreatment | 15.8 ± 6.2 | 171 ± 5.6 | ||
| Posttreatment | 14.4 ± 75 | 13.3 ± 6.9 | ||
| Fear-avoidance beliefs, work (0–42) | .88 | .78 | ||
| Pretreatment | 33.7 ± 6.8 | 30.6 ± 12.3 | ||
| Posttreatment | 32.6 ± 6.9 | 30.2 ± 10.3 | ||
| Kinesiophobia (13–52) | .60 | .10 | ||
| Pretreatment | 30.0 ± 5.8 | 32.1 ± 7.0 | ||
| Post-treatment | 26.0 ± 8.7 | 30.0 ± 9.1 | ||
| Pain catastrophizing (0–36) Pretreatment | 18.7 ± 10.9 | 14.8 ± 10.0 | .70 | <.01 |
| Posttreatment | 76 ± 8.9 | 5.9 ± 6.1 | ||
| Depressive symptoms (0–63) | .92 | <.01 | ||
| Pretreatment | 23.3 ± 10.2 | 28.1 ± 15.7 | ||
| Posttreatment | 6.5 ± 6.0 | 11.9 ± 10.9 | ||
All values reported as mean ± SD unless otherwise indicated.
Interaction refers to the P value for the group-by-time effect.
Time refers to the P value for the pretreatment-posttreatment main effect.
Indicates significant group differences (P<.05).
FIGURE 1.
Change in pain intensity for graded exercise and graded exposure groups.
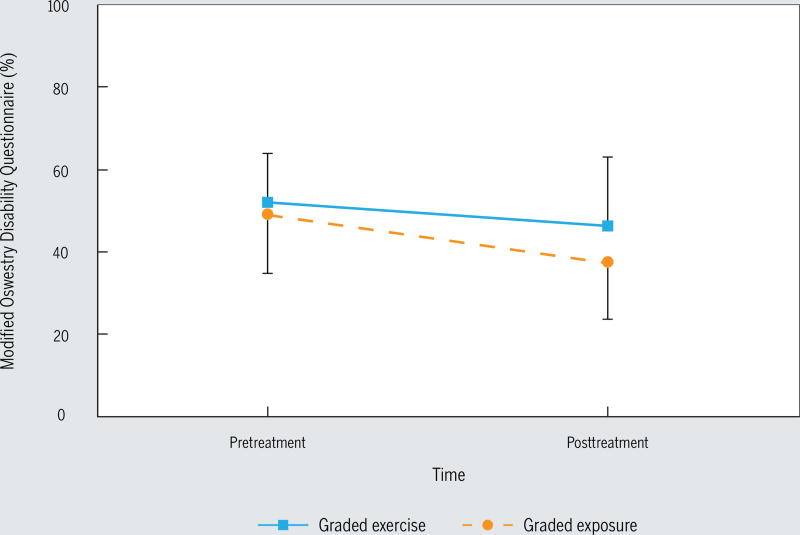
For disability, a similar pattern was observed. Groups responded equivalently to treatment (F1,15 = 0.6, P = .44, η2 = 0.04) with no main effect for group (F1,1 = 2.7, P = .12, η2 = 0.15), indicating similar overall pain-related disability. Both groups showed a significant reduction in ODQ scores following treatment (F1,15 = 9.7, P<.01, η2 = 0.39). When MIC was considered, 30% of patients experienced a change that met or exceeded the MIC of 10.0 for the ODQ.34 The disability data are depicted in FIGURE 2.
FIGURE 2.
Change in disability for graded exercise and graded exposure groups.
Changes in Psychologic Factors
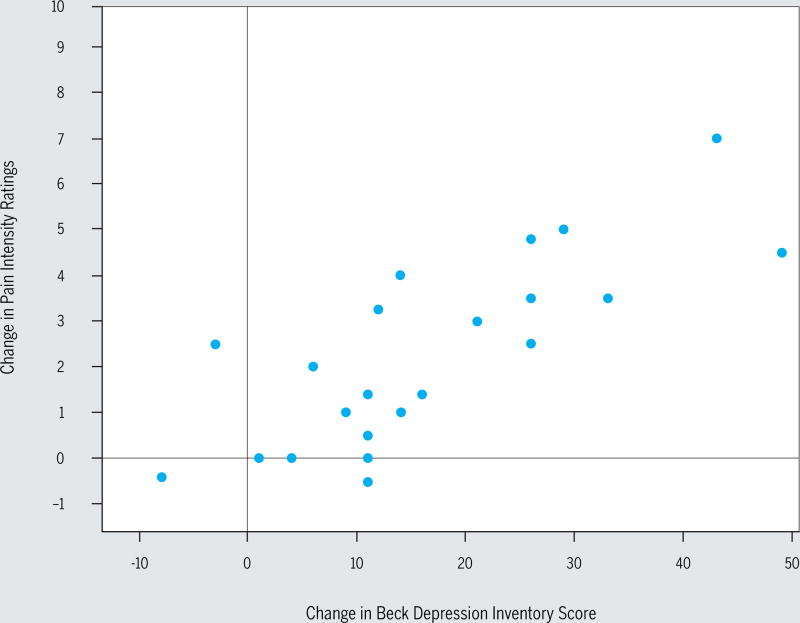
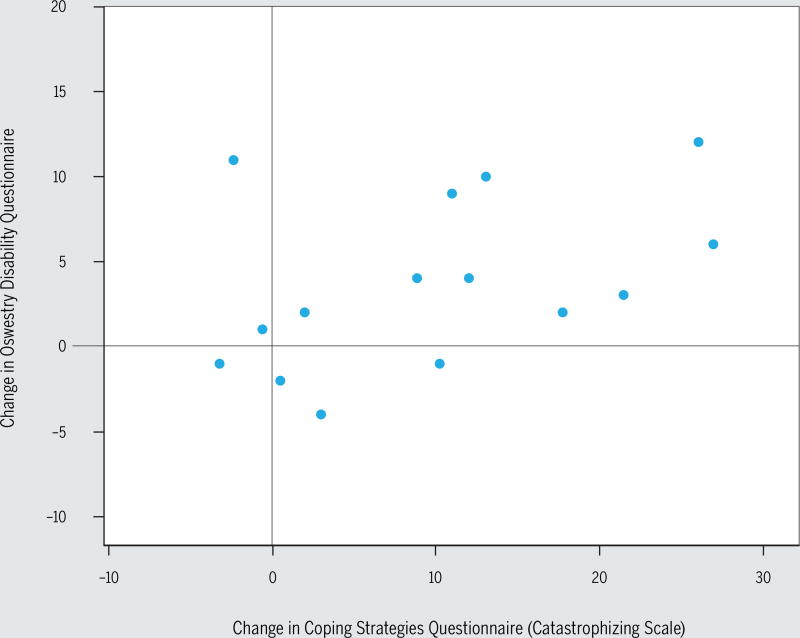
Data describing the changes in psychologic variables are summarized in TABLE 4. The TSK (F1,15 = 3.0, P = .10), FPQ (F1,15 = 1.0, P = .33), and FABQ work and physical activity scales (F1,14 = 0.08 and 3.6, P = .78 and .08, respectively) did not demonstrate statistically reliable changes following treatment. In contrast, the catastrophizing subscale of the CSQ-R and BDI for depressive symptoms did show significant reductions following treatment (F1,13 = 13.5, P<.01, η2 = 0.51 and F1,20 = 28.4, P<.01, η2 = 0.59, respectively), with both treatment groups showing equivalent reductions posttreatment. The associations among changes in the key outcome variables (pain, disability) and in the psychological variables were then further examined. Pearson correlation coefficients among residualized change scores are presented in TABLE 5 for the 3 psychologic variables that most likely changed over time: the FABQ-PA, CSQ-R, and BDI. Statistically reliable associations were found between pain intensity and depressive symptoms (r = 0.56, P<.01) and disability and catastrophizing (r = 0.64, P<.01). These associations indicated that decrease in depressive symptoms was strongly associated with decrease in pain intensity (FIGURE 3) and decrease in pain catastrophizing was strongly associated with decreased disability (FIGURE 4).
TABLE 5.
Person Correlations Among Pain Intensity, Disability, and Psychologic Measures*
| Change in: | Change in Pain Intensity | Change in Disability |
|---|---|---|
| Fear-avoidance beliefs (physical activity) | −0.28 | 0.18 |
| Pain catastrophizing | −0.22 | 0.64† |
| Depressive symptoms | 0.56* | 0.27 |
Correlations represent associations among residualized change score for the appropriate variables.
Indicates P<.01.
FIGURE 3.
Change in depressive symptoms has positive association with change in pain intensity ratings.
FIGURE 4.
Change in pain catastrophizing has positive association with change in disability score.
DISCUSSION
This study compared clinical outcomes for patients with chronic low back pain who received graded exercise to patients who received graded exposure while participating in a rehabilitation program that featured intensive physical therapy supplemented with either graded exercise or graded exposure. We hypothesized that graded exposure would be associated with better patient outcomes. Contrary to our hypothesis and the theoretical expectations of the FAM, both graded exercise and graded exposure treatment approaches reduced pain intensity and disability at the same rate. The overall improvement from these approaches was modest, with 50% and 30% of patients exceeding minimal improvement thresholds for pain intensity and disability, respectively.34 Instead of being associated with a particular treatment approach, improvements in pain intensity and disability were robustly predicted by improvements in depressive symptoms and pain catastrophizing, respectively.
In determining exercise and activity parameters, there are obvious theoretical differences in graded exposure and graded exercise. We attempted to account for those differences when creating the dosing paradigms utilized in this study. However, the implementation of graded exercise and graded exposure may result in treatment overlap, and this is a potential explanation for the lack of differences observed in this study. Simply stated, dosing exercise and activity based on quota principles (ie, graded exercise) is not absent of exposure to exercise and activities of which the patient might also be fearful. Activities that were commonly rated as fearful for patients participating in this study included lifting, carrying, and walking (TABLE 2), which are activities that would also typically be included in chronic low back pain rehabilitation programs, especially for programs that have a goal of returning patients to work. Our current data suggest that it may not be necessary to implement a formal exposure paradigm if the graded exercise component includes a variety of activities, including those that individuals with chronic low back pain are likely to fear (eg, lifting, carrying, and walking). Instead, exposure paradigms may need to include activities that are not typically incorporated in rehabilitation programs, but are rated as highly fearful, like twisting and reaching to the floor (TABLE 2).
Our results complement evidence from recently reported clinical trials investigating the efficacy of graded exposure. Linton et al31 compared the effects of graded exposure plus usual care to a wait list control group for 46 patients with at least 3 months of activity restriction due to low back pain and elevated levels of pain-related fear. Patients receiving graded exposure had larger improvements in function, but not for pain intensity or pain-related fear. The wait list control group then received graded exposure, and statistical improvements were observed for function and pain-related fear but not for pain intensity. Leeuw et al28 compared the effects of graded exercise and graded exposure for 85 patients with at least 3 months of low back pain. At the 6-month follow-up, the authors reported no statistically significant differences between graded exercise and graded exposure for functional disability, main complaints, daily activity levels, or pain intensity. The authors noted some favorable trends for graded exposure, including statistically significant reductions in pain catastrophizing and perceived harmfulness of activities.28 George et al19 investigated the effects of physical therapy augmented with graded exercise or graded exposure for 108 patients with 24 weeks or less duration of low back pain. At the 6-month follow-up, the authors reported no statistically significant differences for pain and disability outcomes. However, graded exposure was associated with larger 6-month improvements in pain-related fear in comparison to physical therapy augmented with graded exercise. The evidence to date indicates that graded exposure is only superior to wait list control conditions,31 and that graded exposure and graded exercise are likely to be associated with similar outcomes for pain intensity and disability. Future clinical studies will determine whether use of graded exposure is warranted to effectively treat chronic low back pain.
As a secondary purpose, this study investigated if changes in psychological factors were associated with improvement in pain intensity and disability. Our results suggested that reductions in depressive symptoms and pain catastrophizing were strongly associated with reductions in pain intensity and disability, respectively. The link between depressive symptoms and pain intensity is well established, and these findings support that a reduction in depressive symptoms often occurs with a reduction in pain intensity, even when the depressive symptoms are not explicitly addressed. The findings related to pain catastrophizing were consistent with our hypothesis and the FAM, which stresses the importance of decreasing catastrophizing in chronic low back pain rehabilitation.27 However, it was interesting to note that kinesiophobia and fear-avoidance beliefs did not improve in this sample. This finding was counter to our hypothesis, as we expected improvement in pain-related fear to be associated with reductions in pain and disability, as observed in our previous trials.16,19 A previous study reported that reduction of catastrophizing mediated the outcomes for both pain intensity and disability, regardless of whether the treatment was cognitive or physical in nature.42 The results of our study converge with this finding, and with other studies reporting the importance of reducing pain catastrophizing.45,54 This information may be used to tailor interventions to specifically target reduction of depressive symptoms and pain catastrophizing to improve outcomes for patients with chronic low back pain.
These unexpected results may be evidence of a difference between the constructs of catastrophizing and those related to pain-related fear. These results may also suggest that pain catastrophizing is more of a general appraisal of consequences of pain, while the pain-related fear measures are related to the probability of pain occurring from a given activity. Another potential explanation for our discordant findings is that although the chronic low back pain rehabilitation program had goals of reducing both pain catastrophizing and pain-related fear, the techniques implemented in this setting were only effective at reducing pain catastrophizing. It is also possible that pain-related fear for patients with chronic low back pain is less amenable to change, in comparison to pain catastrophizing. This explanation seems plausible because the pain-related fear levels in the current study were comparable to or slightly higher than those from previous studies that reported improvements in fear-avoidance beliefs and included patients with acute or subacute low back pain.6,15 Although our discordant findings for pain catastrophizing and pain-related fear are interesting, it is important to remember that there is ambiguity in the literature on this topic. For example, changes in pain-related fear, but not changes in pain catastrophizing, were predictive of changes in disability for patients with chronic low back pain.56 In contrast, both pain-related fear and pain catastrophizing contributed to disability for patients with acute low back pain.47 Timing of the reduction may also be a consideration, as early reductions in pain catastrophizing and later reductions in pain-related fear were predictive of return to work.54 Therefore, the recommendation from these data to focus on depressive symptoms and pain catastrophizing should be taken with some caution. At this point, there is not enough agreement in the literature to make definitive recommendations on which specific psychological constructs should be the focus of chronic low back pain rehabilitation.
The limitations of the current study should be taken into consideration when interpreting its results. The primary limitation of this study is that we used a quasi-experimental design to preserve integrity of the treatment conditions. The clinical setting prevented us from implementing an experimental design with random assignment. Patients participated in group exercise and individual randomization raised the potential of treatment contamination (ie, patients or therapists assigned to graded exposure performing graded exercise). Despite lack of randomization, there were minimal pretreatment differences observed, and the results of this study were negative, which means that we did not overestimate the treatment effects of graded exposure (a concern with nonrandomized designs).4 Furthermore, the negative results for graded exposure are consistent with recent randomized trials,19,28 suggesting convergence despite different methodologies.
Another limitation of this study is that it took place in an interdisciplinary setting, so our results are best interpreted for physical therapists practicing in similar clinical settings. Also, we did not incorporate a control group, so we cannot speak to the absolute effects of these approaches. The benefits to the patients seemed modest when minimal change thresholds were considered, but without an alternate comparison group (ie, waitlist control group) we do not know the “true” size of these effects. It is possible that the described graded exercise and exposure approaches were not effective, and it is also possible that the chronic nature of this patient population limits the size of expected treatment effects. Future studies should consider experimental designs and control groups, if clinical environments are amenable to such methodology. In addition, because the exposure intervention represents a more classic phobia intervention, future studies should consider selection criteria aimed at identifying and including participants who meet criteria for a phobia diagnosis. We would anticipate a greater effect of exposure intervention for such a subset of patients.
Another limitation is that our design did not allow us to determine whether the observed decrease in catastrophizing and its association with a reduction in disability was a result of quota attainment or exposure in physical therapy, or from other cognitive interventions implemented during the rehabilitation program. Future studies should account for these limitations by including more focused interventions that isolate the potential “active” components of the interventions (eg, quota attainment or hierarchical exposure). Another limitation of this study is the relatively small sample size and potential for low statistical power. We do not believe type II error was a concern for our primary purpose of comparing graded exposure to graded exercise. The observed effects were very small (η2<0.05) for the group-by-time interactions related to pain intensity and disability. Therefore, the most appropriate conclusion is that there was likely no clinically or statistically meaningful difference between the 2 treatment groups over time. Indeed, the time effects were robust and indicated improvements for both groups. However, it is worth noting that the study might have lacked adequate power for our secondary purpose of investigating psychological factors, specifically for the FABQ-PA.
CONCLUSION
These data suggest that the exposure inherent in graded exercise may be sufficient to induce similar outcomes in pain intensity and disability. When psychological processes were considered, reductions in pain intensity were strongly associated with reduction of depressive symptoms and reductions in disability were strongly associated with reductions in pain catastrophizing.
KEY POINTS.
FINDINGS
Graded exercise and graded exposure resulted in similar treatment outcomes for patients with chronic low back pain who received intensive, impairment-focused physical therapy within a multidisciplinary setting. Instead, improvements in pain intensity and disability were associated with changes in depressive symptoms and pain catastrophizing, respectively.
IMPLICATION
Physical therapists considering behavioral interventions for patients with chronic low back painin interdisciplinary settings should be aware that there were no differences in these treatment approaches. Instead, the goal to reduce depressive symptoms and pain catastrophizing may be more important than the selection of specific intervention approach.
CAUTION
This study lacked random assignment of treatments and a control group that received no treatment at all. Therefore, we cannot consider the absolute effects of these treatments. Also, this study took place in an interdisciplinary setting, so the results are best generalized to similar treatment environments.
Acknowledgments
Jennifer Martin and Jean Crago assisted with the informed consent procedure and administration of questionnaires. Amanda lames and Regina McCarthy coordinated recruitment from the Brooks Health System to the Brooks Center for Rehabilitation Studies.
The protocol for this study was approved by The University of Florida Institutional Review Board. Steven Z. George and Michael E. obinson were supported by NIH-NIAMS grant AR051128 while preparing this manuscript. The Brooks Center for Rehabilitation Studies provided funding for the research assistants and laboratory space. Other than the aforementioned grant support, the authors have no financial disclosure of conflict of interest to report for this manuscript.
References
- 1.Scientific approach to the assessment and management of activity-related spinal disorders. A monograph for clinicians. Report of the Quebec Task Force on Spinal Disorders. Spine (Phila Pa 1976) 1987;12:S1–59. [PubMed] [Google Scholar]
- 2.Albaret MC, Munoz Sastre MT, Cottencin A, Mullet E. The Fear of Pain questionnaire: factor structure in samples of young, middle-aged and elderly European people. Eur J Pain. 2004;8:273–281. doi: 10.1016/j.ejpain.2003.09.005. http://dx.doi.org/10.1016/j.ejpain.2003.09.005. [DOI] [PubMed] [Google Scholar]
- 3.Beck AT, Steer RA. Beck Depression Inventory: Manual. San Antonio, TX: Psychological Corporation; 1987. [Google Scholar]
- 4.Benson K, Hartz AJ. A comparison of observational studies and randomized, controlled trials. N Engl J Med. 2000;342:1878–1886. doi: 10.1056/NEJM200006223422506. [DOI] [PubMed] [Google Scholar]
- 5.Bortz WM., 2nd The disuse syndrome. West J Med. 1984;141:691–694. [PMC free article] [PubMed] [Google Scholar]
- 6.Burton AK, Waddell G, Tillotson KM, Summerton N. Information advice to patients with back pain can have a positive effect. A randomized controlled trial of a novel educational booklet in primary care. Spine (Phila Pa 1976) 1999;24:2484–2491. doi: 10.1097/00007632-199912010-00010. [DOI] [PubMed] [Google Scholar]
- 7.Cronbach LJ, Furby L. How we should measure “change” - or should we? Psych Bulletin. 1970;74:68–80. [Google Scholar]
- 8.de Jong JR, Vlaeyen JW, Onghena P, Goossens ME, Geilen M, Mulder H. Fear of movement/(re) injury in chronic low back pain: education or exposure in vivo as mediator to fear reduction? Clin J Pain. 2005;21:9–17. doi: 10.1097/00002508-200501000-00002. discussion 69–72. [DOI] [PubMed] [Google Scholar]
- 9.Dworkin RH, Turk DC, Wyrwich KW, et al. Interpreting the clinical importance of treatment outcomes in chronic pain clinical trials: IMMPACT recommendations. J Pain. 2008;9:105–121. doi: 10.1016/j.jpain.2007.09.005. http://dx.doi.org/10.1016/j.jpain.2007.09.005. [DOI] [PubMed] [Google Scholar]
- 10.Fairbank JC, Couper J, Davies JB. O’Brien JP The Oswestry low back pain disability questionnaire. Physiotherapy. 1980;66:271–273. [PubMed] [Google Scholar]
- 11.Fairbank JC, Pynsent PB. The Oswestry Disability Index. Spine (Phila Pa 1976) 2000;25:2940–2952. doi: 10.1097/00007632-200011150-00017. discussion 2952. [DOI] [PubMed] [Google Scholar]
- 12.Fordyce WE, Fowler RS, Jr, Lehmann JF, Delateur BJ, Sand PL, Trieschmann RB. Operant conditioning in the treatment of chronic pain. Arch Phys Med Rehabil. 1973;54:399–408. [PubMed] [Google Scholar]
- 13.Gardner RC. Neufeld RWJ. Use of the simple change score in correlational analyses. Educ Psychol Meas. 1987;47:849–864. http://dx.doi.org/10.1177/0013164487474001. [Google Scholar]
- 14.George SZ, Bialosky JE, Fritz JM. Physical therapist management of a patient with acute low back pain and elevated fear-avoidance beliefs. Phys Ther. 2004;84:538–549. [PubMed] [Google Scholar]
- 15.George SZ, Fritz JM, Bialosky JE, Donald DA. The effect of a fear-avoidance-based physical therapy intervention for patients with acute low back pain: results of a randomized clinical trial. Spine (Phila Pa 1976) 2003;28:2551–2560. doi: 10.1097/01.BRS.0000096677.84605.A2. http://dx.doi.org/10.1097/01.BRS.0000096677.84605.A2. [DOI] [PubMed] [Google Scholar]
- 16.George SZ, Fritz JM, McNeil DW. Fear-avoidance beliefs as measured by the fear-avoidance beliefs questionnaire: change in fear-avoidance beliefs questionnaire is predictive of change in self-report of disability and pain intensity for patients with acute low back pain. Clin J Pain. 2006;22:197–203. doi: 10.1097/01.ajp.0000148627.92498.54. [DOI] [PubMed] [Google Scholar]
- 17.George SZ, Valencia C, Zeppieri G, Jr, Robinson ME. Development of a self-report measure of fearful activities for patients with low back pain: the fear of daily activities questionnaire. Phys Ther. 2009;89:969–979. doi: 10.2522/ptj.20090032. http://dx.doi. org/10.2522/ptj.20090032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.George SZ, Zeppieri G. Physical therapy utilization of graded exposure for patients with low back pain. J Orthop Sports Phys Ther. 2009;39:496–505. doi: 10.2519/jospt.2009.2983. http://dx.doi.org/10.2519/jospt.2009.2983. [DOI] [PubMed] [Google Scholar]
- 19.George SZ, Zeppieri G, Jr, Cere AL, et al. A randomized trial of behavioral physical therapy interventions for acute and sub-acute low back pain ( NCT00373867) Pain. 2008;140:145–157. doi: 10.1016/j.pain.2008.07.029. http://dx.doi.org/10.1016/j.pain.2008.07.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Goubert L, Crombez G, Van Damme S, Vlaeyen JW, Bijttebier P, Roelofs J. Confirmatory factor analysis of the Tampa Scale for Kinesiophobia: invariant two-factor model across low back pain patients and fibromyalgia patients. Clin J Pain. 2004;20:103–110. doi: 10.1097/00002508-200403000-00007. [DOI] [PubMed] [Google Scholar]
- 21.Holm I, Friis A, Storheim K, Brox JI. Measuring self-reported functional status and pain in patients with chronic low back pain by postal questionnaires: a reliability study. Spine (Phila Pa 1976) 2003;28:828–833. [PubMed] [Google Scholar]
- 22.Houben RM, Leeuw M, Vlaeyen JW, Goubert L, Picavet HS. Fear of movement/injury in the general population: factor structure and psychometric properties of an adapted version of the Tampa Scale for Kinesiophobia. J Behav Med. 2005;28:415–424. doi: 10.1007/s10865-005-9011-x. http://dx.doi.org/10.1007/sl0865-005-9011-x. [DOI] [PubMed] [Google Scholar]
- 23.Jacob T, Baras M, Zeev A, Epstein L. Low back pain: reliability of a set of pain measurement tools. Arch Phys Med Rehabil. 2001;82:735–742. doi: 10.1053/apmr.2001.22623. http://dx.doi.org/10.1053/apmr.2001.22623. [DOI] [PubMed] [Google Scholar]
- 24.Jensen MP, Turner LR, Turner JA, Romano JM. The use of multiple-item scales for pain intensity measurement in chronic pain patients. Pain. 1996;67:35–40. doi: 10.1016/0304-3959(96)03078-3. [DOI] [PubMed] [Google Scholar]
- 25.Keefe FJ, Brown GK, Wallston KA, Caldwell DS. Coping with rheumatoid arthritis pain: catastrophizing as a maladaptive strategy. Pain. 1989;37:51–56. doi: 10.1016/0304-3959(89)90152-8. [DOI] [PubMed] [Google Scholar]
- 26.Kottke FJ. The effects of limitation of acitivity upon the human body. JAMA. 1966;196:825–830. [PubMed] [Google Scholar]
- 27.Leeuw M, Goossens ME, Linton SJ, Crombez G, Boersma K, Vlaeyen JW. The fear-avoidance model of musculoskeletal pain: current state of scientific evidence. J Behav Med. 2007;30:77–94. doi: 10.1007/s10865-006-9085-0. http://dx.doi.org/10.1007/s10865-006-9085-0. [DOI] [PubMed] [Google Scholar]
- 28.Leeuw M, Goossens ME, van Breukelen GJ, et al. Exposure in vivo versus operant graded activity in chronic low back pain patients: results of a randomized controlled trial. Pain. 2008;138:192–207. doi: 10.1016/j.pain.2007.12.009. http://dx.doi.org/10.1016/j.pain.2007.12.009. [DOI] [PubMed] [Google Scholar]
- 29.Lethem J, Slade PD, Troup JD, Bentley G. Outline of a fear-avoidance model of exaggerated pain perception--I. Behav Res Ther. 1983;21:401–408. doi: 10.1016/0005-7967(83)90009-8. [DOI] [PubMed] [Google Scholar]
- 30.Lindstrom I, Ohlund C, Eek C, et al. The effect of graded activity on patients with subacute low back pain: a randomized prospective clinical study with an operant-conditioning behavioral approach. Phys Ther. 1992;72:279–290. doi: 10.1093/ptj/72.4.279. discussion 291-273. [DOI] [PubMed] [Google Scholar]
- 31.Linton SJ, Boersma K, Jansson M, Overmeer T, Lindblom K, Vlaeyen JW. A randomized controlled trial of exposure in vivo for patients with spinal pain reporting fear of work-related activities. Eur J Pain. 2008;12:722–730. doi: 10.1016/j.ejpain.2007.11.001. http://dx.doi.org/10.1016/j.ejpain.2007.11.001. [DOI] [PubMed] [Google Scholar]
- 32.McNeil DW, Rainwater AJ., 3rd Development of the Fear of Pain Questionnaire-Ill. J Behav Med. 1998;21:389–410. doi: 10.1023/a:1018782831217. [DOI] [PubMed] [Google Scholar]
- 33.Osman A, Breitenstein JL, Barrios FX, Gutierrez PM, Kopper BA. The Fear of Pain Questionnaire-Ill: further reliability and validity with nonclinical samples. J Behav Med. 2002;25:155–173. doi: 10.1023/a:1014884704974. [DOI] [PubMed] [Google Scholar]
- 34.Ostelo RW, Deyo RA, Stratford P, et al. Interpreting change scores for pain and functional status in low back pain: towards international consensus regarding minimal important change. Spine (Phila Pa 1976) 2008;33:90–94. doi: 10.1097/BRS.0b013e31815e3a10. http://dx.doi.org/10.1097/BRS.0b013e31815e3a10. [DOI] [PubMed] [Google Scholar]
- 35.Pfingsten M, Kroner-Herwig B, Leibing E, Kronshage U, Hildebrandt J. Validation of the German version of the Fear-Avoidance Beliefs Questionnaire (FABQ) Eur J Pain. 2000;4:259–266. doi: 10.1053/eujp.2000.0178. http://dx.doi.org/10.1053/eujp.2000.0178. [DOI] [PubMed] [Google Scholar]
- 36.Price DD, McGrath PA, Rafii A, Buckingham B. The validation of visual analogue scales as ratio scale measures for chronic and experimental pain. Pain. 1983;17:45–56. doi: 10.1016/0304-3959(83)90126-4. [DOI] [PubMed] [Google Scholar]
- 37.Roach KE, Brown MD, Dunigan KM, Kusek CL, Walas M. Test-retest reliability of patient reports of low back pain. J Orthop Sports Phys Ther. 1997;26:253–259. doi: 10.2519/jospt.1997.26.5.253. [DOI] [PubMed] [Google Scholar]
- 38.Robinson ME, Riley JL, 3rd, Myers CD, et al. The Coping Strategies Questionnaire: a large sample, item level factor analysis. Clin J Pain. 1997;13:43–49. doi: 10.1097/00002508-199703000-00007. [DOI] [PubMed] [Google Scholar]
- 39.Roelofs J, Goubert L, Peters ML, Vlaeyen JW, Crombez G. The Tampa Scale for Kinesiophobia: further examination of psychometric properties in patients with chronic low back pain and fibromyalgia. Eur J Pain. 2004;8:495–502. doi: 10.1016/j.ejpain.2003.11.016. http://dx.doi.org/10.1016/j.ejpain.2003.11.016. [DOI] [PubMed] [Google Scholar]
- 40.Roland M, Fairbank J. The Roland-Morris Disability Questionnaire and the Oswestry Disability Questionnaire. Spine (Phila Pa 1976) 2000;25:3115–3124. doi: 10.1097/00007632-200012150-00006. [DOI] [PubMed] [Google Scholar]
- 41.Rosenstiel AK, Keefe FJ. The use of coping strategies in chronic low back pain patients: relationship to patient characteristics and current adjustment. Pain. 1983;17:33–44. doi: 10.1016/0304-3959(83)90125-2. [DOI] [PubMed] [Google Scholar]
- 42.Smeets RJ, Vlaeyen JW, Kester AD, Knottnerus JA. Reduction of pain catastrophizing mediates the outcome of both physical and cognitive-behavioral treatment in chronic low back pain. J Pain. 2006;7:261–271. doi: 10.1016/j.jpain.2005.10.011. http://dx.doi.org/10.1016/j.jpain.2005.10.011. [DOI] [PubMed] [Google Scholar]
- 43.Smeets RJ, Wittink H. The deconditioning paradigm for chronic low back pain unmasked? Pain. 2007;130:201–202. doi: 10.1016/j.pain.2007.04.024. http://dx.doi.org/10.lOl6/j.pain.200704.024. [DOI] [PubMed] [Google Scholar]
- 44.Stewart MW, Harvey ST, Evans IM. Coping and catastrophizing in chronic pain: a psychometric analysis and comparison of two measures. J Clin Psychol. 2001;57:131–138. doi: 10.1002/1097-4679(200101)57:1<131::aid-jclp13>3.0.co;2-l. http://dx.doi.org/10.1002/1097-4679(200101)57:1<131::AID-JCLP13>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 45.Sullivan MJ, Stanish WD. Psychologically based occupational rehabilitation: the Pain-Disability Prevention Program. Clin J Pain. 2003;19:97–104. doi: 10.1097/00002508-200303000-00004. [DOI] [PubMed] [Google Scholar]
- 46.Swinkels-Meewisse EJ, Swinkels RA, Verbeek AL, Vlaeyen JW, Oostendorp RA. Psychometric properties of the Tampa Scale for Kinesiophobia and the Fear-Avoidance Beliefs Questionnaire in acute low back pain. Man Ther. 2003;8:29–36. doi: 10.1054/math.2002.0484. [DOI] [PubMed] [Google Scholar]
- 47.Swinkels-Meewisse IE, Roelofs J, Oostendorp RA, Verbeek AL, Vlaeyen JW. Acute low back pain: pain-related fear and pain catastrophizing influence physical performance and perceived disability. Pain. 2006;120:36–43. doi: 10.1016/j.pain.2005.10.005. http://dx.doi.org/10.1016/j.pain.2005.10.005. [DOI] [PubMed] [Google Scholar]
- 48.Vlaeyen JW, de Jong J, Geilen M, Heuts PH, van Breukelen G. Graded exposure in vivo in the treatment of pain-related fear: a replicated single-case experimental design in four patients with chronic low back pain. Behav Res Ther. 2001;39:151–166. doi: 10.1016/s0005-7967(99)00174-6. [DOI] [PubMed] [Google Scholar]
- 49.Vlaeyen JW, de Jong J, Geilen M, Heuts PH, van Breukelen G. The treatment of fear of movement/(re)injury in chronic low back pain: further evidence on the effectiveness of exposure in vivo. Clin J Pain. 2002;18:251–261. doi: 10.1097/00002508-200207000-00006. [DOI] [PubMed] [Google Scholar]
- 50.Vlaeyen JW, Kole-Snijders AM, Boeren RG, van Eek H. Fear of movement/(re)injury in chronic low back pain and its relation to behavioral performance. Pain. 1995;62:363–372. doi: 10.1016/0304-3959(94)00279-N. [DOI] [PubMed] [Google Scholar]
- 51.Vlaeyen JW, Linton SJ. Fear-avoidance and its consequences in chronic musculoskeletal pain: a state of the art. Pain. 2000;85:317–332. doi: 10.1016/S0304-3959(99)00242-0. [DOI] [PubMed] [Google Scholar]
- 52.Von Korff M, Balderson BH, Saunders K, et al. A trial of an activating intervention for chronic back pain in primary care and physical therapy settings. Pain. 2005;113:323–330. doi: 10.1016/j.pain.2004.11.007. http://dx.doi.org/10.1016/j.pain.2004.11.007. [DOI] [PubMed] [Google Scholar]
- 53.Waddell G, Newton M, Henderson I, Somerville D, Main CJ. A Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain. 1993;52:157–168. doi: 10.1016/0304-3959(93)90127-B. [DOI] [PubMed] [Google Scholar]
- 54.Wideman TH, Adams H, Sullivan MJ. A prospective sequential analysis of the fear-avoidance model of pain. Pain. 2009;145:45–51. doi: 10.1016/j.pain.2009.04.022. http://dx.doi.org/10.1016/j.pain.2009.04.022. [DOI] [PubMed] [Google Scholar]
- 55.Woby SR, Roach NK, Urmston M, Watson PJ. Psychometric properties of the TSK-11: a shortened version of the Tampa Scale for Kinesiophobia. Pain. 2005;117:137–144. doi: 10.1016/j.pain.2005.05.029. http://dx.doi.org/10.1016/j.pain.2005.05.029. [DOI] [PubMed] [Google Scholar]
- 56.Woby SR, Watson PJ, Roach NK, Urmston M. Are changes in fear-avoidance beliefs, catastrophizing, and appraisals of control, predictive of changes in chronic low back pain and disability? Eur J Pain. 2004;8:201–210. doi: 10.1016/j.ejpain.2003.08.002. http://dx.doi.org/10.1016/j.ejpain.2003.08.002. [DOI] [PubMed] [Google Scholar]