Abstract
Objectives: To evaluate the rate of perioperative complications after plasmakinetic bipolar and monopolar transurethral resection of bladder tumor (BTURB and MTURB). In addition, the study identifies patient and procedure characteristics associated with early complications.
Patients and Methods: Retrospective review was conducted on patients undergoing transurethral resection of bladder tumor procedures at a single institution from 2003 to 2013 to assess the 30-day complication rates associated with BTURB and MTURB.
Results: Four hundred twenty-seven patients met inclusion criteria and underwent 586 procedures (379 BTURB and 207 MTURB). Baseline patient demographics, tumor stage, and tumor grade were similar in BTURB and MTURB cohorts. The overall complication rate was 34.3% for MTURB and 26.7% for BTURB. The most frequent complications were acute urinary retention (AUR) 11%, hematuria 8%, and urinary tract infection (UTI) 7%. There was no statistical difference in rates of AUR, hematuria, UTI, or readmission for continuous bladder irrigation or hemostasis procedures between BTURB and MTURB cohorts. There was a trend toward lower perforation rate during BTURB (2.6% vs 5.8%). In multivariate logistic regression analysis, MTURB, male gender, and large resections were predictive of overall complications. Male gender was associated with hematuria and AUR. Large bladder tumor resection size was also associated with increased risk of overall complications and AUR.
Conclusion: BTURB was associated with a lower risk of overall complications, but there was no difference in the rate of hematuria in the two cohorts. Male gender and large tumor size are associated with higher risk of early complications.
Keywords: : bladder cancer, transurethral resection of bladder tumors, plasmakinetic bipolar resection
Introduction
In 2014, there were an estimated 74,690 new cases of bladder cancer (BC) diagnosed in the United States, making it the fourth most common cancer in men and 11th most common in women.1 Transurethral resection of bladder tumors (TURB) is the initial procedure performed for all new bladder cancer diagnoses for pathological staging and grading. It also serves as definitive treatment for nonmuscle-invasive tumors, the latter representing greater than 75% of new cases of BC.2
The technology utilized for TURB has evolved over time. Monopolar cautery, which requires external patient grounding and nonconductive irrigation solution (water, glycine, sorbitol, or mannitol), was the modality historically utilized for TURB (MTURB). After its introduction in the early 2000s, many urologists have adopted plasmakinetic bipolar resection technology. The principle advantage of bipolar resection technology is the ability to perform transurethral procedures with isotonic saline irrigation, thus avoiding the risk of transurethral resection (TUR) syndrome. Studies in the transurethral resection of the prostate (TURP) literature have demonstrated comparable complication rates between monopolar and bipolar resection, with increasing evidence supporting fewer bleeding events and absence of TUR syndrome with bipolar resection.3–5
To date, there are limited data as to whether plasmakinetic bipolar cautery (BTURB) confers any advantage in patients undergoing TURB. To better understand the adverse events following TURB, we performed the largest single-center retrospective review to date comparing outcomes from monopolar and plasmakinetic bipolar TURB. In addition, the study identified patient and procedure characteristics associated with an increased risk of early postoperative complications after TURB.
Patients and Methods
After institutional review board approval, all TURB procedures performed at our academic institution from January 1, 2003 to April 30, 2013 were reviewed. The data collected included patient demographics, procedure characteristics, pathology results, adverse events, and subsequent interventions within 30 days of TURB.
All procedures were performed by academic staff urologists with the assistance of resident physicians. Perioperative antibiotics were administered in all cases based on preoperative urine cultures. TURB was performed as an outpatient surgery unless there was concern for perioperative adverse events secondary to patient comorbidities or intraoperative findings. Cases were excluded from analysis if an additional concurrent surgical procedure was performed, if a true resection was not performed (i.e., if a cold-cup biopsy was performed followed by simple fulguration), there was known concomitant upper tract tumor, or medical records were incomplete.
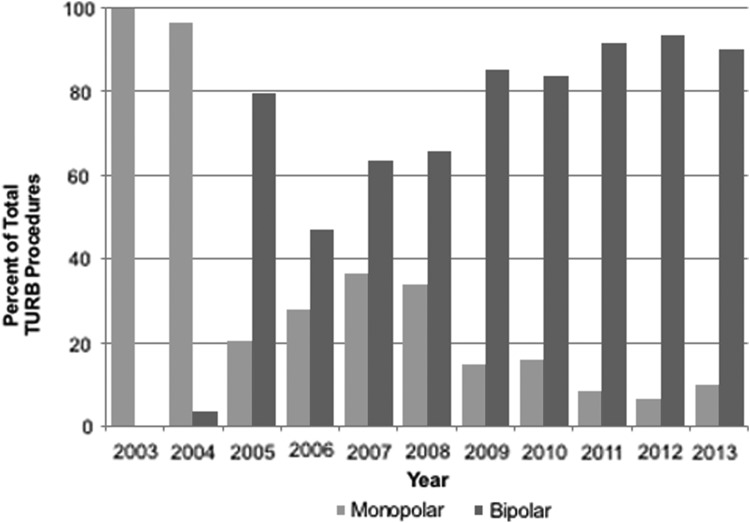
All MTURB procedures were performed with a 26F or 28F continuous flow Iglesias resectoscope sheath, bladder resection loop, and the Valley Lab Force FX™ electrosurgical generator (Covidien, Minneapolis, MN) on the factory-recommended settings for TURB (100–170 W for cut and 70–120 W for coagulation). All BTURB procedures were performed with the Gyrus ACMI Bipolar Plasmakinetic Tissue Management System (Olympus, Southborough, MA) continuous flow resectoscope and bladder resection loop. At the beginning of the study period, all procedures were MTURB until our first BTURB case was performed in 2004. The distribution of resection type over time is illustrated in Figure 1. Throughout the study period, one surgeon continued to use MTURB for all cases. Among the other surgeons, there was no selection bias for resection modality based on tumor size or patient comorbidity as BTURB was used routinely by the conclusion of the study period.
FIG. 1.
Distribution of cautery type over time during study period.
The primary outcome measure was overall complication rate for MTURB and BTURB within 30 days of surgery. Hematuria was classified as a clinically relevant complication if severe enough to warrant urethral catheter placement for manual irrigation, continuous bladder irrigation, or a secondary hemostasis procedure. Acute urinary retention (AUR) was defined as a complication if the patient developed acute retention necessitating urethral catheter placement. Planned urethral catheter placement at the conclusion of TURB was not considered a complication. Urinary tract infection (UTI) was defined by patients complaining of new lower urinary tract symptoms and urine culture growing >105 colony-forming units of bacteria. Dysuria was considered a complication when, in the absence of UTI, symptoms were severe enough to warrant initiation of an anticholinergic medication. Cases of bladder perforation were recognized intraoperatively. The overall complication rate was defined as the sum of these surgical complications as well as cardiopulmonary, renal, and other medical complications consequent to TURB within 30 days of surgery.
Patient-procedure baseline characteristics and outcomes were compared between BTURB and MTURB groups using Wilcoxon rank-sum tests for continuous variables and Fisher's exact tests for categorical variables. Multivariable logistic regression was used to model each binary outcome (all complications, hematuria, AUR, and UTI) separately. Each model was fit using generalized estimating equations to account for within-subject correlation for patients with multiple procedures. The procedure type (BTURB vs MTURB) was the primary predictor variable. These models also controlled for age, sex, American Society of Anesthesiologists (ASA) score, tumor stage, tumor size, anticoagulant or antiplatelet medication use, and surgery completion status. All statistical analyses were performed using R version 3.1.0 (R Foundation for Statistical Computing, www.R-project.org). All p-values were two sided and p < 0.05 was considered statistically significant.
Results
During the study period, 427 patients underwent 586 TURB procedures (207 MTURB, 379 BTURB). The majority of patients underwent one TURB procedure (n = 320, 75%). Patient characteristics and tumor size, stage, and grade are reported in Table 1. Mean patient age was 69 years and 31% were women. ASA score was significantly higher in the BTURB group, but the remainder of patient characteristics was similar in MTURB and BTURB cohorts. Complete resection was performed in 92% of cases and the distribution of tumor size, stage, and grade was equivalent in the two cohorts.
Table 1.
Baseline Patient and Procedure Characteristics
| All | MTURB | BTURB | p | |
|---|---|---|---|---|
| n | 586 | 207 | 379 | |
| Mean age in years (range) | 69 (22–101) | 69 (22–101) | 69 (29–100) | 0.940 |
| Women, n (%) | 180 (31) | 60 (29) | 120 (32) | 0.500 |
| Mean ASA score | 2.7 | 2.63 | 2.74 | 0.011 |
| TURB per patient during study period, n (%) | ||||
| 1 | 320 (74.9) | |||
| 2 | 75 (17.6) | |||
| ≥3 | 32 (7.5) | |||
| Preoperative anticoagulant or antiplatelet medication, n (%) | 232 (40) | 73 (35) | 159 (42) | 0.133 |
| Size of bladder tumor resection, n (%) | 0.629 | |||
| Small: 0.5–2.0 cm | 265 (45) | 97 (47) | 168 (44) | |
| Medium: 2.0–5.0 cm | 215 (37) | 70 (34) | 145 (38) | |
| Large: >5.0 cm | 104 (18) | 38 (19) | 66 (17) | |
| Complete resection, n (%) | 540 (92) | 193 (93) | 347 (92) | 0.523 |
| Muscle invasion, n (%) | 0.183 | |||
| Noninvasive | 498 (85) | 170 (82) | 328 (87) | |
| Muscle Invasive | 88 (15) | 37 (18) | 51 (13) | |
| Pathology | 0.341 | |||
| Benign, n (%) | 79 (13.9) | 31 (15.6) | 48 (13.0) | |
| PUNLMP | 26 (4.6) | 12 (6.0) | 14 (3.8) | |
| Low-grade urothelial carcinoma | 179 (31.5) | 62 (31.1) | 117 (31.6) | |
| High-grade urothelial carcinoma | 222 (39.0) | 72 (36.2) | 150 (40.5) | |
| Planned postoperative urethral catheter, n (%) | 288 (49.1) | 122 (58.9) | 166 (43.8) | 0.0005 |
ASA = American Society of Anesthesiology; BTURB = bipolar transurethral resection of bladder tumor; MTURB = monopolar transurethral resection of bladder tumor; PUNLMP = papillary urothelial neoplasm of low malignant potential.
The univariate analysis of complications is reported in Table 2. The overall complication rate was 34.3% for MTURB and 26.7% for BTURB with the difference not obtaining statistical significance (p = 0.058). The rate of hematuria was similar in the two groups (8.7% MTURB and 7.4% BTURB), but the two cases necessitating transfusion occurred after MTURB. AUR, UTI, and dysuria occurred at similar rates in the two cohorts. The rate of bladder perforation was higher with MTURB (5.8% vs 2.6%), but a higher percentage of perforation events was attributed to stimulation of the obturator reflex during BTURB (40% vs 8%, see Table 3). The 21 cases of extraperitoneal perforation were managed with urethral catheter bladder decompression, and the single case of intraperitoneal perforation (after BTURB) was managed with laparotomy and cystorrhaphy. Cardiopulmonary and renal complications were more frequent in the MTURB cohort and one case of TUR syndrome occurred after MTURB. One mortality occurred 3 weeks after MTURB due to respiratory and renal failure in a patient with advanced age and multiple comorbidities.
Table 2.
Results of Univariate Analysis
| All (%) | MTURB (%) | BTURB (%) | p | |
|---|---|---|---|---|
| Any complication | 172 (29.4) | 71 (34.3) | 101 (26.7) | 0.058 |
| Hematuria | 46 (7.9) | 18 (8.7) | 28 (7.4) | 0.630 |
| Readmission for continuous bladder irrigation or cystoscopy with clot evacuation | 24 (4.1) | 10 (4.8) | 14 (3.7) | 0.518 |
| Transfusion | 2 (0.34) | 2 (0.96) | 0 (0) | 0.126 |
| Acute urinary retention | 64 (10.9) | 23 (11.1) | 41 (10.8) | 0.891 |
| UTI | 42 (7.2) | 16 (7.7) | 26 (6.9) | 0.738 |
| Perforation | 22 (3.8) | 12 (5.8) | 10 (2.6) | 0.068 |
| Perforation due to obturator nerve reflex | 5 (0.85) | 1 (0.48) | 4 (1.1) | |
| Perforation necessitating laparotomy | 1 (0.17) | 0 (0) | 1 (0.26) | |
| Transurethral resection syndrome | 1 (0.17) | 1 (0.48) | 0 (0) | |
| Deep venous thrombosis | 1 (0.17) | 1 (0.48) | 0 (0) | |
| Acute kidney injury | 4 (0.68) | 3 (1.45) | 1 (0.26) | |
| Hypercarbic respiratory failure | 1 (0.17) | 1 (0.48) | 0 (0) | |
| Transient ischemic attack | 1 (0.17) | 1 (0.48) | 0 (0) | |
| 30-Day mortality rate | 1 (0.17) | 1 (0.48) | 0 (0) |
UTI = urinary tract infection.
Table 3.
Case Details for Bladder Perforation Due to Obturator Nerve Reflex
| Case number | 179 | 207 | 519 | 547 | 576 |
|---|---|---|---|---|---|
| Age (years) | 85 | 42 | 79 | 74 | 59 |
| Sex | Male | Male | Male | Male | Male |
| Resection type | MTURB | BTURB | BTURB | BTURB | BTURB |
| Resection location resulting in obturator reflex | Multifocal | Unknown | Left anterior | Posterior, bladder base | Left inferolateral |
| Tumor burden (cm) | 2.5–5.0 | 2.5–5.0 | >5.0 | 2.5–5.0 | 2.5–5.0 |
| Perforation type | Extraperitoneal | Extraperitoneal | Extraperitoneal | Extraperitoneal | Extraperitoneal |
| Pathology | Carcinoma in situ | Ta low grade | Ta high grade | Follicular cystitis | Ta low grade |
Results from the multivariable regression analysis are listed in Table 4. BTURB was associated with a lower incidence of overall complications (0.64, 95% confidence interval [CI] 0.44, 0.94, p = 0.022). Male gender and larger tumor resection size were associated with higher overall complication rates. Male gender was also associated with a higher risk of hematuria (odds ratio [OR] 2.8, 95% CI 1.2, 6.4), but there was no association between resection energy type and hematuria. Increased risk of AUR was associated with male gender (OR 2.9, 95% CI 1.4, 6.0) and larger tumor resection size (OR 2.9, 95% CI 1.3, 6.3). No patient or perioperative variables were associated with UTI.
Table 4.
Results of Multivariate Analysis
| Any complication | OR | 95% CI | p |
|---|---|---|---|
| Men vs women | 1.63 | 1.08, 2.44 | 0.019 |
| ASA score | 1.05 | 0.69, 1.58 | 0.834 |
| BTURB vs MTURB | 0.64 | 0.44, 0.94 | 0.022 |
| Large vs small resection | 2.46 | 1.41, 4.31 | 0.002 |
| Anticoagulant or antiplatelet medication use | 1.46 | 0.98, 2.16 | 0.061 |
| Hematuria | |||
| Men vs women | 2.77 | 1.19, 6.44 | 0.018 |
| BTURB vs MTURB | 0.72 | 0.38, 1.35 | 0.307 |
| Large vs small resection | 1.58 | 0.62, 4.06 | 0.341 |
| Anticoagulant or antiplatelet medication use | 1.55 | 0.82, 2.93 | 0.179 |
| Muscle invasive vs noninvasive | 0.81 | 0.32, 2.00 | 0.642 |
| Urinary retention | |||
| Male vs female | 2.90 | 1.41, 5.95 | 0.004 |
| BTURB vs MTURB | 0.94 | 0.53, 1.65 | 0.818 |
| Large vs small resection | 2.86 | 1.29, 6.33 | 0.010 |
| Muscle invasive vs noninvasive | 1.03 | 0.47, 2.23 | 0.945 |
| UTI | |||
| Male vs female | 0.95 | 0.48, 1.87 | 0.879 |
| BTURB vs MTURB | 0.89 | 0.46, 1.74 | 0.735 |
| Large vs small resection | 0.86 | 0.28, 2.60 | 0.788 |
CI = confidence interval; OR = odds ratio.
Discussion
TURB is the gold standard procedure for the diagnosis, staging, grading, and initial treatment of BC. Although it is one of the most common endoscopic procedures performed by urologists, data regarding morbidity from TURB are limited. Reported overall complication rates vary widely from 5% to 43%, depending on the definition of postoperative complications.6–9 Despite the widespread utilization of BTURB, outcome data comparing it to MTURB are limited.
Complication rates following different surgical approaches are of more than academic interest. A study based on the 2011 National Surgical Quality Improvement Program (NSQIP) database identified TURB as the outpatient urologic surgery with the highest readmission rate of 5%.10 In the United States, the Patient Protection and Affordable Care Act includes the Hospital Readmission Reduction Program, which penalizes hospitals for above average readmission rates for several medical diagnoses as well as select orthopedic surgeries. In the future, similar penalties may be extended to readmissions after urologic surgery; so there will be additional incentive to prevent early postoperative complications. Against this backdrop, it becomes increasingly important to understand both technical and patient-dependent variables contributing to an increased risk for complications. To our knowledge, this study is the largest single-institution comparison of early postoperative complications between MTURB and BTURB.
A recent meta-analysis was performed on the limited literature comparing outcomes from MTURB and BTURB.11 In this review, BTURB was found to have shorter operative time, lower decrease in hemoglobin level, shorter catheterization time as well as lower rates of obturator nerve reflex and bladder perforation. In a population-based study, Sugihara and colleagues compared perioperative outcomes between monopolar and bipolar TURB with a focus on incidence of severe bladder injury.12 The authors found no difference in the rates of subsequent hemostasis procedures or transfusion, but reported a lower incidence of perforation necessitating open repair or drain placement after BTURB (0.3%) compared to MTURB (0.6%). The incidence of other complications, including cardiopulmonary events and infectious complications, was lower in their BTURB cohort as well (4.6% vs 5.8%).
In our study, there was a statistically higher ASA score for the BTURB cohort. Patient comorbidity did not impact the decision to perform MTURB versus BTURB. A potential explanation is the distribution of BTURB cases being performed more frequently later in the study period (see Fig. 1), and the higher ASA score is a reflection of increasing anesthetic complexity and comorbidity of patients as our academic practice has grown and referral patterns have shifted. In multivariate analysis, ASA score was not found to be associated with any complication nor was it associated with hematuria, UTI, or AUR. Therefore, the difference in ASA score between MTURB and BTURB cohorts does not impact the findings of our study.
Muscle-invasive BC was identified in 15% of cases, which is somewhat lower than the 25% incidence reported in the literature.13,14 High-grade BC was diagnosed in 39% of our series, which is higher than the 25% reported in a contemporary bladder series utilizing the 2004 World Health Organization (WHO) classification system.15 By virtue of our hospital being a tertiary referral center, patients often pursue follow-up with a local urologist for surveillance of nonmuscle-invasive BC, which can explain why only 25% patients underwent more than one TURB procedure in this study. Furthermore, the practice of performing restaging TURB for high-grade disease has evolved over our study period.2
Hematuria is the most frequent complication after TURB, with 2% to 13% rate of clinically relevant bleeding reported in MTURB studies.6–9 Bipolar resection energy has been shown to have a greater depth of coagulation and is thought to have improved hemostatic properties.16 In the TURP literature, a meta-analysis demonstrated reduced risk of TUR syndrome and clot retention after plasmakinetic bipolar procedures with equivalent operative times, transfusion rates, and urethral complications.17 Our overall rate of hematuria was 7.9%, and 4.1% of patients required readmission for continuous bladder irrigation or a hemostasis procedure. There was no difference in the hematuria rate between MTURB and BTURB cases. The two patients in our series who required transfusion (0.34%) underwent MTURB, but due to transfusion being a rare event, the difference did not reach statistical significance. The reported transfusion rate after TURB is 0.9% to 13% and in the recent meta-analysis, there was no difference in transfusion rate between MTURB and BTURB.6,7,9,11,12 Interestingly, perioperative use of anticoagulants or antiplatelet medications (aspirin or clopidogrel) was not associated with increased risk of hematuria or overall complications in our study.
Our finding of a trend toward lower bladder perforation rate with BTURB is supported by other studies and statistical significance was reached in Zhao's meta-analysis.11,12,18 A study of 1284 TURB cases by HerKommer and colleagues reported a bladder perforation rate of 3.8% and identified female gender, body mass index <25 kg/m2, higher tumor stage, and larger resection size to be risk factors for perforation.19
Adductor contraction due to electrical stimulation of the obturator nerve, known as obturator nerve reflex (ONR), is a well-described event that can occur during TURB with an incidence of 1.5% to 4.9%.6,18,20 Since BTURB does not require electrical current to pass through the patient into an external grounding pad, it was initially theorized that ONR would be less of a concern than during MTURB. Zhao reported a lower rate of ONR during BTURB.11 In our experience, ONR resulted in bladder perforation in five cases (Table 3). Four of these cases occurred during BTURB, suggesting that ONR is more frequent during BTURB than expected. Ozer and colleagues reported a higher rate of ONR during BTURB compared to MTURB (35% vs 8%) and consequently a higher rate of bladder perforation during BTURB.21 These findings suggest that ONR remains a potential complication when BTURB is performed in proximity to the obturator nerve. Our practice is to request systemic neuromuscular paralytic administration by the anesthesiologist before resection of tumors involving the inferolateral bladder.
In multivariate regression analysis, bipolar resection energy was associated with a lower risk of overall complications. Trends toward lower incidence of perforation, transfusion, TUR syndrome, and medical complications after BTURB likely account for this result from multivariate analysis. Our results and other recent studies suggest that BTURB has a lower rate of adverse events compared to MTURB.11,12,18 Furthermore, there is evidence that BTURB results in less cautery artifact, which can obscure interpretation of pathology and accurate staging.22 For these reasons, our institution has moved toward preferentially using BTURB for all cases.
Male gender was the demographic variable most associated with adverse events, including overall complications, hematuria, and AUR. The association with male gender and hematuria as well as AUR is likely related to prostatic bleeding resulting from instrumentation and the higher incidence of high pressure voiding due to bladder outlet obstruction in men. An NSQIP review was performed in 2005 to identify risk factors for adverse outcomes after TURB. Presence of disseminated disease, weight loss, low serum albumin, elevated creatinine, dependent functional status, and emergent case basis were factors associated with adverse outcomes.23 Because NSQIP is a Veterans Affairs Medical Centers initiative, 99% of the patients in the study were men and thus female gender did not reach statistical significance for having a lower risk of complications.
Since many institutions routinely place indwelling catheters after TURB, the rate of postoperative urinary retention is not well established. The rate of AUR was 11% and was associated with male gender and larger resection size in multivariate analysis. In our series, a case was considered to have a planned urethral catheter placement at the conclusion of TURB if there was no plan for an immediate voiding trial after the procedure. Leaving a urethral catheter in place for the purposes of instilling an immediate postoperative dose of intravesical chemotherapy was not considered a planned urethral catheter if the catheter was removed after drainage of the medication. Planned urethral catheter placement followed 49.1% of TURB procedures with a significantly higher rate of 58.9% after MTURB compared to 43.8% of BTURB cases (p = 0.0005). The higher rate of planned urethral catheter placement after MTURB could have impacted the subsequent rates of AUR, hematuria, and UTI. The decreased utilization of planned urethral catheter in BTURB cases is more a reflection of changing practices over time rather than any specific concerns related to the cautery modality.
Irrespective of the difference in utilization of planned catheters in the two cohorts, our data support consideration of urethral catheter placement and bladder rest for several days after TURB of large tumors or in men with advanced age.
There are limitations in this study inherent to its retrospective design. The temporal differences in the use of MTURB and BTURB introduce confounders of changes in patient management practices and improvement in surgeon skill over time. Despite these confounders, a strength of our study is that our data represent the experience of eight faculty who performed both types of procedures, with the distribution of procedure type over time demonstrated in Figure 1. The low incidence of hematuria, transfusion, and perforation makes it difficult to reach statistical significance when comparing MTURB and BTURB with the number of patients included in our analysis. To confirm our findings, BTURB and MTURB should ideally be studied in a multicenter randomized, prospective trial similar to those performed in the TURP literature.
Conclusions
Our study confirms that despite being a common procedure performed by urologists, TURB frequently results in early postoperative complications. In multivariate regression analysis, BTURB was found to have a favorable overall complication profile, but there was no difference in the rate of clinically significant hematuria between BTURB and MTURB. Despite not necessitating external patient grounding, obturator nerve reflex and adductor contraction can occur during BTURB. Men are at a greater risk of all complications, hematuria, and urinary retention. Larger bladder tumor size was also associated with overall complications and urinary retention.
Abbreviations Used
- ASA
American Society of Anesthesiologists
- AUR
acute urinary retention
- BC
bladder cancer
- BTURB
bipolar transurethral resection of bladder tumor
- CTSI
clinical and translational science award
- MTURB
monopolar transurethral resection of bladder tumor
- NSQIP
national surgical quality improvement program
- ONR
obturator nerve reflex
- TUR
transurethral resection
- TURB
transurethral resection of bladder tumor
- TURP
transurethral resection of the prostate
- UTI
urinary tract infection
Acknowledgments
Statistical analysis supported, in part, by grant 1UL1RR031973 from the Clinical and Translational Science Award (CTSI) program of the National Center for Research Resources, National Institutes of Health.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Cancer Facts and Figures. American Cancer Society. 2014
- 2.Babjuk M, Burger M, Zigeuner R, Shariat SF, van Rhijn BW, Compérat E, et al. EAU guidelines on non-muscle-invasive urothelial carcinoma of the bladder: Update 2013. Eur Urol 2013;64:639–653 [DOI] [PubMed] [Google Scholar]
- 3.Stucki P, Marini L, Mattei A, Xafis K, Boldini M, Danuser H. Bipolar versus monopolar transurethral resection of the prostate: A prospective randomized trial focusing on bleeding complications. J Urol 2015;193:1371–1375 [DOI] [PubMed] [Google Scholar]
- 4.Mamoulakis C, Trompetter M, de la Rosette J. Bipolar transurethral resection of the prostate: The “golden standard” reclaims its leading position. Curr Opin Urol 2009;19:26–32 [DOI] [PubMed] [Google Scholar]
- 5.Mamoulakis C, Skolarikos A, Schulze M, Scoffone CM, Rassweiler JJ, Alivizatos G, et al. Results from an international multicentre double-blind randomized controlled trial on the perioperative efficacy and safety of bipolar vs monopolar transurethral resection of the prostate. BJU Int 2012;109:240–248 [DOI] [PubMed] [Google Scholar]
- 6.Collado A, Chéchile GE, Salvador J, Vicente J. Early complications of endoscopic treatment for superficial bladder tumors. J Urol 2000;164:1529–1532 [PubMed] [Google Scholar]
- 7.Nieder AM, Meinbach DS, Kim SS, Soloway MS. Transurethral bladder tumor resection: Intraoperative and postoperative complications in a residency setting. J Urol 2005;174:2307–2309 [DOI] [PubMed] [Google Scholar]
- 8.Kondás J, Szentgyörgyi E. Transurethral resection of 1250 bladder tumours. Int Urol Nephrol 1992;24:35–42 [DOI] [PubMed] [Google Scholar]
- 9.Dick A, Barnes R, Hadley H, Bergman RT, Ninan CA. Complications of transurethral resection of bladder tumors: Prevention, recognition and treatment. J Urol 1980;124:810–811 [DOI] [PubMed] [Google Scholar]
- 10.Rambachan A, Matulewicz RS, Pilecki M, Kim JY, Kundu SD. Predictors of readmission following outpatient urological surgery. J Urol 2014;192:183–188 [DOI] [PubMed] [Google Scholar]
- 11.Zhao C, Tang K, Yang H, Xia D, Chen Z. Bipolar versus monopolar transurethral resection of nonmuscle-invasive bladder cancer: A meta-analysis. J Endourol 2016;30:5–12 [DOI] [PubMed] [Google Scholar]
- 12.Sugihara T, Yasunaga H, Horiguchi H, Matsui H, Nishimatsu H, Nakagawa T, et al. Comparison of perioperative outcomes including severe bladder injury between monopolar and bipolar transurethral resection of bladder tumors: A population based comparison. J Urol 2014;192:1355–1359 [DOI] [PubMed] [Google Scholar]
- 13.Burger M, Catto JW, Dalbagni G, Grossman HB, Herr H, Karakiewicz P, et al. Epidemiology and risk factors of urothelial bladder cancer. Eur Urol 2013;63:234–241 [DOI] [PubMed] [Google Scholar]
- 14.Chang SS, Bochner BH, Chou R, Dreicer R, Kamat AM, Lerner SP, et al. Treatment of Non-Metastatic Muscle-Invasive Bladder Cancer: AUA/ASCO/ASTRO/SUO Guideline. J Urol 2017;pii: : 57836–57842 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.May M, Brookman-Amissah S, Roigas J, Hartmann A, Störkel S, Kristiansen G, et al. Prognostic accuracy of individual uropathologists in noninvasive urinary bladder carcinoma: A multicentre study comparing the 1973 and 2004 World Health Organisation classifications. Eur Urol 2010;57:850–858 [DOI] [PubMed] [Google Scholar]
- 16.Huang X, Wang XH, Wang HP, Qu LJ. Comparison of the microvessel diameter of hyperplastic prostate and the coagulation depth achieved with mono- and bipolar transurethral resection of the prostate. A pilot study on hemostatic capability. Scand J Urol Nephrol 2008;42:265–268 [DOI] [PubMed] [Google Scholar]
- 17.Mamoulakis C, Ubbink DT, de la Rosette JJ. Bipolar versus monopolar transurethral resection of the prostate: A systematic review and meta-analysis of randomized controlled trials. Eur Urol 2009;56:798–809 [DOI] [PubMed] [Google Scholar]
- 18.Del Rosso A, Pace G, Masciovecchio S, Saldutto P, Galatioto GP, Vicentini C. Plasmakinetic bipolar versus monopolar transurethral resection of non-muscle invasive bladder cancer: A single center randomized controlled trial. Int J Urol 2013;20:399–403 [DOI] [PubMed] [Google Scholar]
- 19.Herkommer K, Hofer C, Gschwend JE, Kron M, Treiber U. Gender and body mass index as risk factors for bladder perforation during primary transurethral resection of bladder tumors. J Urol 2012;187:1566–1570 [DOI] [PubMed] [Google Scholar]
- 20.Pu XY, Wang HP, Wu YL, Wang XH. Use of bipolar energy for transurethral resection of superficial bladder tumors: Long-term results. J Endourol 2008;22:545–549 [DOI] [PubMed] [Google Scholar]
- 21.Ozer K, Horsanali MO, Gorgel SN, Ozbek E. Bladder injury secondary to obturator reflex is more common with plasmakinetic transurethral resection than monopolar transurethral resection of bladder cancer. Cent European J Urol 2015;68:284–288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mashni J, Godoy G, Haarer C, Dalbagni G, Reuter VE, Al-Ahmadie H, et al. Prospective evaluation of plasma kinetic bipolar resection of bladder cancer: Comparison to monopolar resection and pathologic findings. Int Urol Nephrol 2014;46:1699–1705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hollenbeck BK, Miller DC, Taub D, Dunn RL, Khuri SF, Henderson WG, et al. Risk factors for adverse outcomes after transurethral resection of bladder tumors. Cancer 2006;106:1527–1535 [DOI] [PubMed] [Google Scholar]