Abstract
Objectives
To estimate age-related patterns in nonmedical prescription opioid (NMPO) use in the US population and disorder among past-year users at ages 12–34 between 2002–2014, controlling for period and birth-cohort effects.
Methods
Data are from 13 consecutive cross-sectional National Surveys on Drug Use and Health (N = 542,556). Synthetic longitudinal cohorts spanning ages 12–34 were created and an age-period-cohort analysis was implemented based on the Intrinsic Estimator algorithm.
Results
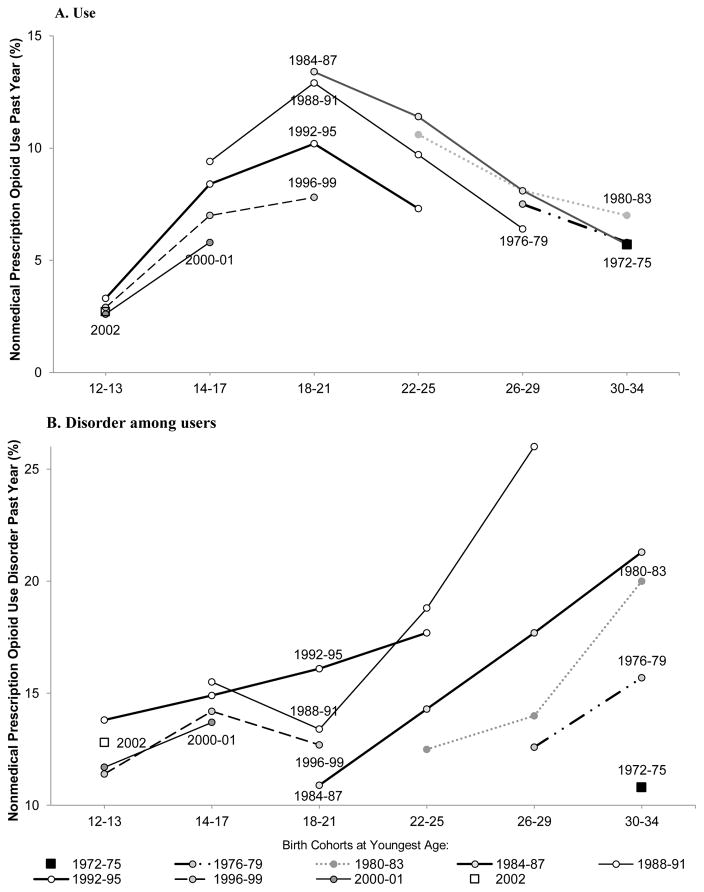
In every birth cohort, past-year NMPO use increases during adolescence, peaks at ages 18–21, decreases through ages 30–34; disorder among past-year users increases from ages 18–21 through 30–34. Use at ages 12–34 decreased from the 1984–87 birth cohorts to more recently-born cohorts. Peak prevalence of use at ages 18–21 has also decreased, and the rates of increase from ages 14–17 to ages 18–21 are slowing down. Disorder at ages 18–34 increased from the 1976–79 to 1992–95 cohorts, but decreased at ages 12–17 from the 1992–95 to the most recently-born 2000–02 cohorts. The years 2010–2014 were characterized by lower NMPO use but higher disorder than 2002–2009.
Conclusions
Increasing NMPO disorder among users aged 18–34 warrants concern. However, declining NMPO use among 12–34 year-olds, a declining rate of increase from adolescence to early adulthood, and a suggestive decline in disorder among the most recent adolescent cohorts may forecast a potential reduction in the public health crisis associated with NMPO drugs.
Keywords: Non-medical prescription opioid use, Non-medical prescription use disorder, Age-period-cohort analysis, Years 2002–2014, National Survey on Drug Use and Health
1. Introduction
The use and associated morbidity of nonmedical prescription opioid (NMPO) constitute major public health problems that have become the focus of intense governmental, media and scientific attention (Compton et al., 2015; Volkow et al., 2014). In 2015, the government announced an initiative, updated in 2016 (The White House, 2016), to address prescription drug abuse and heroin use. The initiative emphasized prescriber training, increasing naloxone use, and improving access to treatment. Many states implemented legislation to control medical prescription of opioids (Franklin et al., 2015; Johnson, 2014). Several reports have described patterns of use (Kerridge et al., 2015; Martins et al., 2014), risk factors for use (Katz et al., 2013), or trends in NMPO use and disorder prevalence among adolescents and adults (Han et al., 2015; Jones, 2017; Martins et al., 2017; McCabe et al., 2014). From 2003 to 2014, overall prevalence of NMPO use decreased, while prevalence of frequent use and disorder increased (Han et al., 2015; Jones, 2017). Trends differed by age and use pattern. In the population, use decreased among adolescents aged 12–17 and young adults aged 18–25; disorders decreased among adolescents, but increased among those older than 25 (Jones, 2017). Among users, disorders increased among those aged 18–34 (Martins et al., 2017). While several studies have investigated NMPO use in specific age groups, especially adolescents, college students (Boyd et al., 2009; McCabe et al., 2013; McCabe et al., 2014; Nargiso et al., 2015) or older adults (Schepis and McCabe, 2016), rarely have use patterns been examined by age over time in the same sample (Han et al., 2015; Jones, 2017; Martins et al., 2017; Miech et al., 2013).
The use of drugs, whether legal or illegal, is an age-graded behavior, with prevalence generally the highest in early adulthood (CBHSQ, 2015a; Kandel et al., 2017). Use increases sharply from adolescence to ages 18–25 for cigarettes, alcohol, marijuana, cocaine, and heroin, and starts to decline as of age 26 for marijuana and cocaine, and age 35 for other drugs. As discussed later, age patterns for NMPOs are similar to those for marijuana and cocaine. Changes in drug use over the life cycle reflect different biological, psychological and social influences in the context of normative transitions in social roles (Schulenberg and Maggs, 2001). Onset and escalation of use in adolescence is thought to develop in response to peer pressure, risk-taking and sensation-seeking in a period of major changes in brain development. The decline beginning in the mid-twenties reflects the assumption of traditional adult work and family roles (Griffin, 2010; Sussman, 2013), and their incompatibility with substance use (Yamaguchi, 1990; Yamaguchi and Kandel, 1985). Similar processes likely apply to NMPO use.
However, age comparisons at one time point or across successive cross-sectional surveys may not reflect true maturational changes, since cross-sectional age differences confound developmental changes with cohort differences and period effects. Variations over time in behaviors by age results from three types of changes: “Age effects, or variation associated with different age groups; period effects, or variation over time periods that affect all age groups simultaneously; and cohort effects or changes across groups of individuals who experience an initial event, such as birth in the same year (pp. 1697–98)” (Yang et al., 2008). Period and cohort effects reflect social and environmental influences. Miech et al. (2013) implemented an age-cohort-period analysis of NMPO use in the population between 1985 and 2009, the youngest cohorts born in 1990–94, the oldest in 1930–34. The prevalence of nonmedical analgesics (opioids), increased across all cohorts and ages in recent years (2006–2009), especially among youths aged 15–24.
We here examine age-related patterns of NMPO use and disorder from adolescence to adulthood from 2002 to 2014, the most recent year for which national data from the National Survey on Drug Use and Health (NSDUH) (SAMHSA, 2015a) can be used for trend analysis. Changes in question wording preclude comparisons of 2015 data with data from earlier surveys (CBHSQ, 2015b). To identify age differences in use and disorder over time, which reflect true developmental changes independent of period and cohort effects, we implemented an age-period-cohort analysis (Yang et al., 2008) for ages 12–34. This age range includes the periods of onset into NMPO use and of highest prevalence of use in the population. Synthetic longitudinal cohorts were created by following members of different birth cohorts as they age in successive cross-sectional national surveys. NMPO use disorder was examined among users, rather than in the population, to control for historical changes in prevalence of use. The synthetic cohorts approximate a longitudinal design and permit an assessment of developmental changes in NMPO use and disorder, while controlling for potentially confounding period and cohort effects. By disaggregating patterns of NMPO use and disorder by birth cohorts, we provide historical insights into these patterns that enhance our understanding of current NMPO behavior and may help anticipate future trends.
2. Methods
2.1. Sample
Data are from 13 consecutive cross-sectional surveys (2002–2014) from the NSDUH, annual cross-sectional surveys of drug use in multistage representative probability samples of the US population aged 12 and older (SAMHSA, 2015b). The target civilian non-institutionalized population represents over 98% of the population. Persons in non-institutional group quarters (homeless shelters, rooming houses, college dormitories), civilians on military bases are included; individuals on active military duty, in jail, drug treatment programs, hospitals, the homeless not in shelters are excluded. Age groups at highest risk for drug use (12–17, 18–25) are oversampled (CBHSQ, 2015c). Approximately 67,500 persons are interviewed annually. Completion rates range from 63% to 70%. Public use data sets were used for ages 12–34. The birth cohorts included in the analysis ranged from 1972 to 2002.
The study was granted expedited approval by the New York State Psychiatric Institute – Columbia University Department of Psychiatry Institutional Review Board.
2.2. Data collection and measures
Data were collected with computer-assisted personal interviews (CAPI) by an interviewer, and audio-computer assisted self-interviewing (ACASI) for substance use.
Self-reported use of nonmedical prescription opioids
Asked about use of prescription pain relievers (opioids) without a prescription or for the experience or feeling they caused; 21 specific pain relievers were listed. Respondents were asked about lifetime use and how long ago they last used the drugs. Past-year use (12 months) = 1; no = 0.
NMPO use disorder
Met DSM-IV criteria for abuse (1 of 4 criteria) or dependence (3 of 7 criteria). Ascertained among past 12-month NMPO users.
Age
In the data set, coded in single years for ages 12 to 21; grouped for ages 22–23, 24–25, 26–29, and 30–34.
2.3. Statistical analysis
2.3.1. Creation of synthetic cohorts for ages 12–34
Synthetic longitudinal cohorts were created with cross-sectional data from the 13 surveys from 2002 to 2014 for ages 12–34 (N = 542,556). Each survey includes representative members of birth cohorts, who can be followed in successive surveys as they age. Because of aggregated age coding, single year birth cohorts could not be tracked over time after age 21. Cohorts were grouped so that number of ages and years in each period were equal. Due to constraints imposed by the age grouping, four years was the optimal equal-time duration. Four periods were defined: 2002–2005; 2006–2009; 2010–2013; 2014, a single year. Birth cohorts were aggregated over successive four-year intervals, except for 2014. Nine birth cohorts groups (born from 1972 to 2002) were constructed spanning ages 12–13, 14–17, 18–21, 22–25, 26–29, 30–34 (Supplementary Table 11). Because ages 10–11 are not surveyed in the NSDUH, ages 12–13 are limited to two-years; because of age coding by NSDUH, 30–34 includes 5 years. Two cohorts were assessed only once: cohort 1972–75 at ages 30–34; cohort 2002 at ages 12–13. Two cohorts were assessed twice: cohort 1976–79 at ages 26–29 and 30–34; cohort 2000–01 at ages 12–13 and 14–17. Two cohorts were assessed three times: cohort 1980–83 at ages 22–25, 26–29, 30–34; cohort 1996–99 at ages 12–13, 14–17, and 18–21. Three cohorts were assessed four times: cohort 1984–87 from ages 18–21 to 30–34; cohort 1988–91, from ages 14–17 to 26–29; and cohort 1992–95, from ages 12–13 to 22–25. Hence, birth cohorts were tracked over different lengths of time, ranging from 1 to 12 years, and covered ages 12–13 to 22–25, ages 14–17 to 26–29, and ages 18–21 to 30–34.
2.3.2. Estimation of age, period and cohort effects for past-year NMPO use in the population and disorder among users at ages 12–34
Two age-period-cohort analyses (APC) were performed using the intrinsic estimator (IE) (Yang et al., 2008) to examine (1) the mutually adjusted effects of age, period and cohort on NMPO use in the population, and (2) disorder among users, from 2002–2014. Disorders were examined among NMPO users to control for historical changes in prevalence of NMPO use in the population. The aggregation of time (for ages, cohorts, and periods) was 4 years. Although assessed only once, two groups (2002 and 1972–75 cohorts) were included in the APC analysis. Last-year NMPO use and disorder were expressed as a logistic function:
where P=probability of NMPO use (disorder); u=intercept; αi=coefficient of the ith age effect for i=six age groups (12–13, 14–17, 18–21, 22–25, 26–29, 30–34); βj=coefficient of the jth period effect for j=four periods (2002–2005–2006–2009–2010–2013–2014);ϒk=coefficient of the kth cohort effect for k=nine cohorts (1972–75, 1976–79, 1980–83, 1984–87, 1988–91, 1992–95, 1996–99, 2000–01, 2002). Because age, period, and cohort are linear functions of one another (cohort = period - age), identifiability constraints must be placed on the design matrix so that a unique solution can be obtained from the regression, when age, period, and cohort dummy variables are included simultaneously. Conventional approaches to identifiability constraints make assumptions about equality of certain parameters, constraining the first two periods, or ages, or cohorts to have the same effect. The intrinsic estimator (IE) avoids making equality assumptions and instead places identifiability constraints on the age, period and cohort parameters using a principal component method thereby removing “the influence of the design matrix on coefficients estimates” (Yang et al., 2008: p. 1707). The IE method allows cohort and period effects to be controlled in order to estimate the independent effects of age on NMPO. Age and period are controlled to estimate cohort effects, and age and cohort are controlled to estimate period effects on NMPO. The reference groups for age, period and cohort effects were the respective means of the effects for each component, making it possible to compare directly the effects of each category within each component. The IE was used in similar studies (Keyes and Miech, 2013; Miech et al., 2013). The APC was implemented with the add-on file for the “Intrinsic Estimator for Generalized Linear Models” algorithm in StataMP v14 (StataCorp, 2015).
The APC analysis estimates the independent main effects of age, period and birth cohort but cannot estimate variations in age effects by birth cohort or period effects by age. Thus, additional post-hoc descriptive analyses of rates derived from the synthetic cohorts examined if age patterns differed among birth cohorts and if period effects differed among age groups. These analyses were implemented in SUDAAN 11.0.1 (Research Triangle Institute, 2012), with design effects adjusted by a Taylor series linearization, and sample weights reflecting selection probabilities at various stages of the sampling design. Weights were adjusted at levels of screener and questionnaire dwelling units to account for nonresponse, extreme values, and poststratification (CBHSQ, 2015c).
3. Results
3.1. Prevalence of past-year NMPO use in the population and disorder among users aged 12–34 by age in 2014
The cross-sectional 2014 data indicate wide differences in rates of NMPO use and disorder by age. Past-year prevalence of NMPO in the population increases from adolescence to early adulthood, and decreases gradually thereafter. Prevalence is 4.8% (95% CI = 4.4%–5.3%) among adolescents aged 12–17, almost doubles to 7.6% (95% CI = 7.0%–8.3%) among young adults aged 18–25, and decreases to 6.0% (95% CI = 5.3%–6.8%) among 26–34 year olds.
In contrast to use, prevalence of disorder among past-year users is similar at ages 12–17 (13.5%, 95% CI = 10.3%–17.5%) and 18–25 (15.1%, 95% CI = 12.5%–18.1%), and increases at ages 26–34 (23.5%, 95% CI = 20.2%–27.2%).
3.2. Age, birth cohort, and period effects in NMPO use in the population
As noted above, age comparisons at one point in time may not reflect true maturational changes, since cross-sectional age differences confound developmental changes with cohort differences and period effects. Synthetic birth cohorts for persons born in 1976–79 to 2000–01 were tracked in successive cross-sectional national surveys and provide segmented longitudinal data ranging from ages 12–13 to ages 30–34 (Table 1).
Table 1.
Past-year nonmedical prescription opioid (NMPO) use in the population and NMPO use disorder among past-year nonmedical prescription opioid users by age and period of assessment from ages 12 to 34 in 13 consecutive annual surveys (NSDUH 2002–2014).
| AGE | ||||||
|---|---|---|---|---|---|---|
| Period | 12–13 % (95%CI) | 14–17 % (95%CI) | 18–21 % (95%CI) | 22–25 % (95%CI) | 26–29 % (95%CI) | 30–34 % (95%CI) |
| A. Prevalence of past-year NMPO use at specific ages among aggregated birth cohorts (N = 542,556) | ||||||
| 2002–2005 | 3.3a (3.0–3.7) | 9.4a (9.1–9.8) | 13.4a (12.9–13.8) | 10.6a (10.1–11.0) | 7.5a,b (6.8–8.2) | 5.7a (5.1–6.3) |
| 2006–2009 | 2.9b (2.7–3.2) | 8.4b (8.1–8.8) | 12.9a (12.5–13.3) | 11.4b (10.9–11.9) | 8.1a (7.3–8.9) | 5.8a (5.3–6.4) |
| 2010–2013 | 2.6b (2.4–2.9) | 7.0c (6.6–7.3) | 10.2b (9.7–10.7) | 9.7c (9.3–10.2) | 8.1a (7.5–8.9) | 7.0b (6.4–7.6) |
| 2014 | 2.7a,b (2.2–3.3) | 5.8d (5.2–6.5) | 7.8c (7.0–8.8) | 7.3d (6.6–8.2) | 6.4b (5.5–7.5) | 5.7a (4.9–6.7) |
| B. Prevalence of NMPO use disorder among past-year users at specific ages among aggregated birth cohorts (N = 46,264) | ||||||
| 2002–2005 | 13.8a (11.1–17.1) | 15.5a (14.0–17.2) | 10.9a (9.8–12.1) | 12.5a (11.3–13.8) | 12.6a (10.0–15.8) | 10.8a (8.4–13.7) |
| 2006–2009 | 11.4a (8.9–14.6) | 14.9a (13.5–16.5) | 13.4b (12.1–14.7) | 14.3a,b (12.8–16.1) | 14.0a,b (11.3–17.2) | 15.7b (12.7–19.2) |
| 2010–2013 | 11.7a (8.5–15.8) | 14.2a (12.7–15.9) | 16.1c (14.5–17.8) | 18.8b (16.7–21.0) | 17.7b (14.7–21.2) | 20.0b (16.3–24.3) |
| 2014 | 12.8a (7.5–21.1) | 13.7a (10.0–18.3) | 12.7a,b,c (9.7–16.5) | 17.7b,c (13.8–22.4) | 26.0c (21.2–31.5) | 21.3b (15.6–28.2) |
| C. Birth cohorts by age and period | ||||||
| 2002–2005 | 1992–95 | 1988–91 | 1984–87 | 1980–83 | 1976–79 | 1972–75 |
| 2006–2009 | 1996–99 | 1992–95 | 1988–91 | 1984–87 | 1980–83 | 1976–79 |
| 2010–2013 | 2000–01 | 1996–99 | 1992–95 | 1988–91 | 1984–87 | 1980–83 |
| 2014 | 2002 | 2000–01 | 1996–99 | 1992–95 | 1988–91 | 1984–87 |
Different superscripts indicate statistically significant (p < 0.05) birth cohort or period effects within each age group (column).
The cross-sectional age patterns are consistently observed longitudinally. In every birth cohort, NMPO use is lowest at ages 12–13, increases sharply during adolescence, peaks at ages 18–21, and declines with increasing age to age 34 (Table 1, Panel A; Figure 1, Panel A). Controlling for period and birth cohort effects, the APC analysis indicates that the odds of past-year use increased by a factor of 3.40 from ages 12–13 (odds ratio [OR] = 0.48, 95% CI = 0.46–0.50) to ages 18–21 (OR = 1.63, 95% CI = 1.60–1.67), but decreased by a factor of 0.48 from ages 18–21 to ages 30–34 (OR = 0.79, 95% CI = 0.76–0.82) (Table 2).
Figure 1.
Past-year nonmedical prescription (A) opioid use, (B) opioid use disorder among past-year nonmedical prescription opioid users by aggregated birth cohorts from ages 12 to 34 in 13 consecutive annual surveys (NSDUH 2002–2014).
Table 2.
Age-period-cohort analysis of past-year nonmedical prescription opioid (NMPO) use in the population and NMPO use disorder among past-year nonmedical prescription opioid users in aggregated birth cohorts from ages 12 to 34 in 13 consecutive annual surveys (NSDUH 2002–2014).
| NMPO Use (N = 542,556) | NMPO Use Disorder (N = 46,264) | |||
|---|---|---|---|---|
| Age | Odds Ratioc | 95% CI | Odds Ratioc | 95% CI |
| 12–13 | 0.48*** | (0.46–0.50) | 0.99 | (0.90–1.10) |
| 14–17 | 1.26*** | (1.23–1.29) | 0.93* | (0.87–0.99) |
| 18–21 | 1.63*** | (1.60–1.67) | 0.78** | (0.74–0.83) |
| 22–25 | 1.30*** | (1.26–1.33) | 0.98 | (0.92–1.04) |
| 26–29 | 0.99 | (0.95–1.03) | 1.08 | (0.98–1.20) |
| 30–34 | 0.79*** | (0.76–0.82) | 1.30*** | (1.18–1.45) |
| Period | ||||
| 2002–05 | 1.06*** | (1.04–1.08) | 0.83*** | (0.79–0.88) |
| 2006–09 | 1.10*** | (1.08–1.12) | 0.92** | (0.88–0.97) |
| 2010–13 | 1.00 | (0.98–1.02) | 1.10*** | (1.04–1.16) |
| 2014a | 0.86*** | (0.83–0.89) | 1.18*** | (1.08–1.30) |
| Birth Cohortb | ||||
| 1972–75 | 0.97 | (0.91–1.03) | 0.90 | (0.76–1.07) |
| 1976–79 | 1.02 | (0.97–1.07) | 1.00 | (0.86–1.16) |
| 1980–83 | 1.18*** | (1.13–1.23) | 1.02 | (0.91–1.14) |
| 1984–87 | 1.23*** | (1.19–1.28) | 1.16** | (1.04–1.28) |
| 1988–91 | 1.14*** | (1.10–1.18) | 1.34*** | (1.22–1.48) |
| 1992–95 | 0.97 | (0.94–1.01) | 1.27*** | (1.15–1.41) |
| 1996–99 | 0.87*** | (0.83–0.90) | 1.02 | (0.90–1.14) |
| 2000–01 | 0.79*** | (0.75–0.83) | 0.84* | (0.72–0.98) |
| 2002 | 0.93 | (0.79–1.10) | 0.65 | (0.39–1.08) |
Only one birth cohort was interviewed in 2014.
Birth cohorts are specified for the youngest age group in each four-year period.
The reference groups for age effects, period effects, and birth cohort effects are the respective means of the effects of age, period, and birth cohort.
p < 0.05;
p < 0.01;
p < 0.001
There are also birth cohort effects. Controlling for period and age effects, the APC analysis establishes that the more recent birth cohorts (born as of 1996) have the lowest odds of past-year NMPO use (Table 2). Prevalence of use increased from the 1972–79 to the 1984–87 birth cohorts, and then declined consistently among the more recent cohorts. For example, 18–21 year olds born in 1984–87 have higher rates of past-year NMPO use (13.4%, 95% CI = 12.9%–13.8%) than 18–21 year olds born in 1996–99 (7.8%, 95% CI = 7.0%–8.8%) (Table 1, Panel A).
Not only does the peak prevalence of use at ages 18–21 declines from older to more recent birth cohorts, but the rates of increase from adolescence (ages 14–17) to peak prevalence are slowing down (Figure 1, Panel A). The increase (slope) among the youngest 1996–99 birth cohorts is no longer significant (OR = 1.14, 95% CI = 0.99–1.31), and is significantly lower (t = 2.97, p <0.01) than the increase among the oldest 1988–91 birth cohorts (OR = 1.42, 95% CI = 1.35–1.50).
Period effects were also observed. Controlling for age and cohort, the APC analysis marked years 2002–2005 and 2006–2009 as periods of higher NMPO use than 2010–2013, with a further decrease in 2014 (Table 2). For example, among 14–17 year olds, the rate of NMPO use was 9.4% (95% CI = 9.1%–9.8%) in 2002–2005, dropped to 7.0% (95% CI = 6.6%–7.3%) in 2010–2013 and 5.8% (95% CI = 5.2%–5.8%) in 2014 (Table 1, Panel A). Among 22–25 year olds, similar declines were observed, from 10.6% (95% CI = 10.1%–11.0%) in 2002–2005, to 9.7% (95% CI = 9.3%–10.2%) in 2010–13, and 7.3% (95% CI = 6.6%–8.2%) in 2014. The decline in NMPO use by period was not observed among those aged 26–34.
3.3. Age, birth cohort and period effects in NMPO disorder among past-year users
APC analysis of NMPO disorder among past-year users revealed age patterns different from those observed for use (Table 2). Controlling for period and birth cohort effects, the odds of disorder decreased by a factor of 0.84 from ages 14–17 (OR = 0.93, 95% CI = 0.87–0.99) to ages 18–21 (OR = 0.78, 95% CI = 0.74–0.83), but increased by a factor of 1.66 from ages 18–21 to ages 30–34 (OR = 1.30, 95% CI = 1.18–1.45). Prevalence of disorder was lower at ages 14–17 than all age groups combined, further decreased at ages 18–21, then increased as of ages 26–29, reaching peak prevalence at ages 30–34.
Birth cohort effects were also significant. NMPO use disorders among past-year NMPO users increased from ages 18–21 to 30–34 in each successive more recent birth cohort, from the 1976–79 through the 1992–95 cohorts. For example, 26–29 year old NMPO users born in 1988–91 had higher rates of disorder (26.0%, 95% CI = 21.2%–31.5%) than those born in 1976–79 (12.6%, 95% CI = 10.0%–15.8%) (Table 1, Panel B; Figure 1, Panel B). This increasing trend in prevalence of disorder by birth cohorts leveled off in the 1996–99 birth cohorts, and decreased in the youngest cohorts born in 2000–01 and 2002. Disorder decreased at ages 12–17 from the 1992–95 to most recently born cohorts. For example, 12–13 year old NMPO users born in 2000–01 had lower disorder (11.7%, 95% CI = 8.5%–15.8%) than those born in 1992–95 (13.8%, 95% CI = 11.1%–17.1%), although the difference was not statistically significant. At ages 18–21, the rate of disorder among those born in 1996–99 was not higher than in earlier cohorts (1984–95).
There were period effects, with years 2002–2009 reflecting lower rates of disorder, and years 2010 to 2014 reflecting higher rates (Table 1, Panel B). In 2002–2005, 12.5% (95% CI = 11.3%–13.8%) of 22–25 year old past-year NMPO users met criteria for disorder compared to 17.7% (95% CI = 13.8%–22.4%) in 2014, an increase of 41.6%. For those aged 30–34, the rates were 10.8% (95% CI = 8.4%–13.7%) versus 21.3% (95% CI = 15.6%–28.2%), an increase of almost 100%. Although not statistically different, rates of disorder decreased between 2002–2005 and 2014 among adolescents aged 12–13 and 14–17.
4. Discussion
Age-specific rates of NMPO use reflect historical changes that have occurred in the use of these drugs over the last twelve years. These changes are obscured when the population is considered as a whole. Using a synthetic cohort approach based on tracking members of the same birth cohorts in successive cross-sectional national surveys, we documented that there are consistent but different maturational patterns in NMPO use in the population and in disorder among NMPO users. An age-period-cohort analysis allowed us to specify age effects independently of social and environmental influences captured by period and cohort effects. In every cohort, NMPO use increases dramatically through adolescence, peaks at ages 18–21, and declines in early and middle adulthood. There also period effects with NMPO use decreasing from 2002–2009 to 2014, especially among adolescents and young adults aged 18–25. Simultaneously, rates of use from mid-adolescence to early adulthood have been increasing at a slower rate among the most recent birth cohorts and the prevalence at ages of peak use has been decreasing successively from the 1984–87 to more recently born cohorts (1996–99). Miech et al. (2013), who analyzed NSDUH data for years 1985–2009, reported higher rates of NMPO use among young people born between 1980 and 1994 compared to those born prior to 1980. By contrast, by considering five more recent years (2010–2014) and starting with more recent cohorts as of survey years 2002, rather than 1985, we observed a decline in NMPO use among youths. The causes for the decreasing rates of use observed among more recent cohorts are not well understood. These declines may reflect policies designed to increase prescription drug monitoring programs (Bao et al., 2016), those designed to reduce medical prescription of opioids for chronic pain (Franklin et al., 2015) and the nonmedical use of opioid analgesics (Compton et al., 2015; Jones, 2017), as well as media focus on the problems of addiction (Nelson et al., 2015).
By disaggregating patterns of NMPO use and of disorder among users by birth cohorts, we provide historical insights into these patterns that enhance our understanding of current NMPO behavior and may help anticipate future trends. Prevalence of NMPO disorder among past-year users decreased from ages 14–17 to 18–21, but increased among users 22–34 years old, with peak prevalence at ages 30–34. Among 18–34 year olds, disorder increased from the 1976–79 through the 1992–95 birth cohorts, and across years 2002–2014. However, prevalence of disorder among 18–21 year olds born in the more recent 1996–99 cohorts was similar to those born in earlier cohorts (1984–95), and prevalence of disorder among the most recent birth cohorts of 12–17 year olds (born in 2000–2002) was lower than in earlier cohorts. This suggests that the expected rate of disorder among these cohorts as they age may continue to be lower than in previous cohorts. However, this interpretation must be tempered by the fact that these cohorts provide few measures and cover a short series of years.
It is beyond the scope of this paper to investigate the mechanisms that could account for the cohort differences that we observed. These mechanisms may differ at different stages of the life cycle and for different birth cohorts. In adolescence, factors might include changes in levels of risk-taking or social norms regarding drug use. In adulthood, one set of mechanisms consonant with the role incompatibility framework, in which NMPO use is lower among those married and employed than those not married or not employed, would include secular trends in marriage and employment rates.
Limitations of the analysis result partially from the available data. In the publicly available NSDUH data, from age 22 to 34, respondents’ ages are grouped into two, four or five year categories. Ages after 34 are grouped into fifteen-year categories and cannot be included in the analysis. This reduces the precision with which individual birth cohorts can be tracked over successive surveys in the APC analysis, the ages that can be tracked, the duration of the tracking period, and the precision of the estimates. In addition, disorders were measured by the DSM-IV. We grouped respondents who met DSM-IV criteria for abuse or dependence to increase comparability with the DSM-5, which combines abuse and dependence criteria to define substance use disorders. In the National Epidemiologic Survey on Alcohol and Related Conditions-III, the prevalence of past-year DSM-5 opioid disorders other than heroin (based on 2+ criteria) was higher by 14% than for DSM-IV [0.89% (SE=0.05%) versus 0.78% (SE=0.05%)] and concordance between the two measures was excellent (Goldstein et al., 2015). The impact of this change in definition on the present results should be minor, since the difference in rates based on the two nosological systems is small.
The data illustrate the importance of examining different age groups when considering the public health consequences of NMPO drug use in the population. Several trends are notable: rates of NMPO use consistently decline from the peak in early adulthood to adulthood, rates among youths have declined over the last decade, and the progression in use from adolescence to early adulthood is slowing down. These trends may presage continuing decreases in the number of adult NMPO users with disorder. It is well known that, irrespective of the drug class, those who start using drugs in adolescence are more likely to continue using these drugs in adulthood and to become heavy users; the earlier the age of onset, the greater the likelihood that users will become addicted (Coffey and Patton, 2016; Dawson et al., 2008; USDHHS, 2012; Volkow, 2006). The same processes appear to characterize the developmental pattern of NMPO use. A follow-up of a national sample of high school seniors from Monitoring the Future (MF) from age 18 found that, controlling for other drug use (cigarettes, binge-drinking, marijuana, barbiturates/sedatives misuse, prescribed opioids) and demographics, lifetime prescription opioid misuse was the strongest predictor of misuse five years later (Miech et al., 2015). In another MF sample, NMPO at age 18 was the strongest predictor of substance use disorders at age 35 (McCabe et al., 2016). Currently, while prevalence of use is decreasing among adolescents, rates of disorder among users are increasing among young adults. Whether the overall number of individuals with disorder increases or decreases will be a function of the size of the decline in number of users and the number of addicted individuals among users. However, as the number of users declines, those with disorder and other psychiatric comorbidities increases (Han et al., 2015), counterbalancing the reduction in burden from the decrease in overall use.
Given sex and racial/ethnic differences in patterns of NMPO use and disorder (Back et al., 2010; Kerridge et al., 2015; Salas et al., 2016; SAMHSA, 2015b), future work should implement APC analyses by sex and race/ethnicity.
Age differentiation of patterns of NMPO use and disorder at one point in time and over time allows the identification of individuals in the population who are most at risk for negative outcomes because of nonmedical prescription opioid use and who should be the target of prevention and intervention efforts. These efforts need to focus on adolescents and young adults. Patterns of NMPO use and disorder among different age groups in the population need to be better understood.
Supplementary Material
Highlights.
An age-period-cohort analysis spanning ages 12–34 was implemented.
Across birth cohorts, nonmedical prescription opioid use peaked at ages 18–21.
Use at ages 12–34 decreased from the older to more recently born cohorts.
Disorder increased in adults across cohorts, decreased for youth in recent cohorts.
These trends may forecast a reduction in nonmedical prescription opioid use burden.
Acknowledgments
Role of Funding Source
This research was supported by grant R01 DA036748 from the National Institute on Drug Abuse (D. Kandel, PI). Support was also provided by the New York State Psychiatric Institute (Griesler). The funding organizations had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
We want to thank the anonymous reviewers for their helpful comments.
Footnotes
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:...
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:...
Contributors
M. Hu conducted the data analysis. M. Wall provided statistical consultation. All the authors contributed to the design of the analysis, reviewed the analysis, and participated in the writing of the manuscript. All authors have approved the final article.
Conflict of Interest
The authors report no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Back SE, Payne RL, Simpson AN, Brady KT. Gender and prescription opioids: findings from the National Survey on Drug Use and Health. Addict Behav. 2010;35:1001–7. doi: 10.1016/j.addbeh.2010.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bao Y, Pan Y, Taylor A, Radakirshnan S, Luo F, Pincus HA, Schackman BR. Prescription drug monitoring programs are associated with sustained reductions in opioid prescribing by physicians. Health Affairs. 2016;35:1045–51. doi: 10.1377/hlthaff.2015.1673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyd CJ, Teter CJ, West BT, Morales M, McCabe SE. Non-medical use of prescription analgesics: A three-year national longitudinal study. J Addict Dis. 2009;28:232–42. doi: 10.1080/10550880903028452. http://www.dx.doi.org/10.1080/10550880903028452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Behavioral Health Statistics and Quality (CBHSQ) Results from the 2014 National Survey on Drug Use and Health: Detailed Tables. Substance Abuse and Mental Health Services Administration (SAMHSA); Rockville, MD: 2015a. [Google Scholar]
- Center for Behavioral Health Statistics and Quality (CBHSQ) National Survey on Drug Use and Health: 2014 and 2015 Redesign Changes. Substance Abuse and Mental Health Services Administration (SAMHSA); Rockville, MD: 2015b. [PubMed] [Google Scholar]
- Center for Behavioral Health Statistics and Quality (CBHSQ) 2014 National Survey on Drug Use and Health: Methodological Summary and Definitions. Substance Abuse and Mental Health Services Administration (SAMHSA); Rockville, MD: 2015c. [Google Scholar]
- Coffey C, Patton GC. Cannabis use in adolescence and young adulthood: A review of findings from the Victorian Adolescent Health Cohort Study. Canad J Psychiatry. 2016;61:318–27. doi: 10.1177/0706743716645289. http://www.dx.doi.org/10.1177/0706743716645289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compton WM, Boyle M, Wargo E. Prescription opioid abuse: Problems and responses. Prev Med. 2015;80:5–9. doi: 10.1016/j.ypmed.2015.04.003. http://www.dx.doi.org/10.1016/j.ypmed.2015.04.003. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Goldstein RB, Chou SP, Ruan WJ, Grant BF. Age at first drink and the first incidence of adult-onset DSM-IV alcohol use disorders. Alcohol Clin Exp Res. 2008;32:2149–60. doi: 10.1111/j.1530-0277.2008.00806.x. http://www.dx.doi.org/10.1111/j.1530-0277.2008.00806.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franklin G, Sabel J, Jones CM, Mai J, Baumgartner C, Banta-Green CJ, Neven D, Tauben DJ. A comprehensive approach to address the prescription opioid epidemic in Washington State: Milestones and lessons learned. Am J Public Health. 2015;105:463–9. doi: 10.2105/AJPH.2014.302367. http://www.dx.doi.org/10.2105/AJPH.2014.302367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein RB, Chou SP, Smith SM, Jung J, Zhang H, Saha TD, Pickering RP, Ruan WJ, Huang B, Grant BF. Nosologic comparisons of DSM-IV and DSM-5 alcohol and drug use disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions-III. J Stud Alcohol Drugs. 2015;76:378–88. doi: 10.15288/jsad.2015.76.378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffin KW. The Epidemiology of Substance Use among Adolescents, and Young Adults: A Developmental Perspective. In: Scheir LM, editor. Handbook of Drug Use Etiology: Theory, Methods, and Empirical Findings. American Psychological Association; Washington, D.C: 2010. pp. 73–92. [Google Scholar]
- Han B, Compton WM, Jones CM, Cai R. Nonmedical prescription opioid use and use disorders among adults aged 18 through 64 years in the United States, 2003–2013. JAMA. 2015;314:1468–78. doi: 10.1001/jama.2015.11859. http://www.dx.doi.org/10.1001/jama.2015.11859. [DOI] [PubMed] [Google Scholar]
- Johnson H. Decline in drug overdose deaths after state policy changes – Florida, 2010–2012. MMWR Morb Mortal Wkly Rep. 2014;63:569–74. [PMC free article] [PubMed] [Google Scholar]
- Jones CM. The paradox of decreasing nonmedical opioid analgesic use and increasing abuse or dependence – an assessment of demographic and substance use trends, United States, 2003–2014. Addict Behav. 2017 Feb;:229–35. doi: 10.1016/j.addbeh.2016.08.027. http://dx.doi.org/10.1016/j.addbeh.2016.08.027. [DOI] [PubMed]
- Kandel DB, Griesler PC, Hu M-C, Kerridge BT, Grant BF. Epidemiololgy of Substance Use Disorders. In: Charney DS, et al., editors. Neurobiology of Mental Illness. Oxford University Press; New York, NY: 2017. in press. [Google Scholar]
- Katz C, El-Gabalawy R, Keyes KM, Martins SS, Sareen J. Risk factors for incident nonmedical prescription opioid use and abuse and dependence: Results from a longitudinal nationally representative sample. Drug Alc Depend. 2013;132:107–13. doi: 10.1016/j.drugalcdep.2013.01.010. http://www.dx.doi.org/10.1016/j.drugalcdep.2013.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerridge BT, Saha TD, Chou SP, Zhang H, Jung J, Ruan WJ, Smith SM, Huang B, Hasin DS. Gender and nonmedical prescription opioid use and DSM-5 nonmedical prescription opioid use disorder: Results from the National Epidemiologic Survey on Alcohol and Related Conditions - III. Drug Alc Depend. 2015;156:47–56. doi: 10.1016/j.drugalcdep.2015.08.026. http://www.dx.doi.org/10.1016/j.drugalcdep.2015.08.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes KM, Miech R. Age, period, and cohort effects in heavy episodic drinking in the US from 1985 to 2009. Drug Alc Depend. 2013;132:140–8. doi: 10.1016/j.drugalcdep.2013.01.019. http://www.dx.doi.org/10.1016/j.drugalcdep.2013.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martins SS, Kim JH, Chen LY, Levin D, Keyes KM, Cerdá M, Storr CL. Nonmedical prescription drug use among US young adults by educational attainment. Soc Psychiatry Psychiatr Epidmiol. 2014;50:713–24. doi: 10.1007/s00127-014-0980-3. http://www.doi.org/10.1007/s00127-014-0980-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martins SS, Segura LE, Santaella-Tenorio J, Perimutter A, Fenton MC, Cerdá M, Keyes KM, Ghandour LA, Storr CL, Hasin DS. Prescription opioid use disorder and heroin use among 12–34 year-olds in the United States from 2002 to 2014. Addict Behav. 2017:236–41. doi: 10.1016/j.addbeh.2016.08.033. http://dx.doi.org/10.1016/j.addbeh.2016.08.033. [DOI] [PMC free article] [PubMed]
- McCabe SE, Schulenberg JE, O’Malley PM, Patrick ME, Kloska DD. Non-medical use of prescription opioids during the transition to adulthood: A multi-cohort national longitudinal study. Addiction. 2013;109:102–10. doi: 10.1111/add.12347. http://www.dx.doi.org/10.1111/add.12347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, Veliz P, Schulenberg JE. Adolescent context of exposure to prescription opioids and substance use disorder symptoms at age 35: A national longitudinal study. Pain. 2016;157:2173–8. doi: 10.1097/j.pain.0000000000000624. http://www.dx.doi.org/10.1097/j.pain.0000000000000624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, West BT, Teter CJ, Boyd CJ. Trends in medical use, diversion, and nonmedical use of prescription medications among college students from 2003 to 2013: Connecting the dots. Addict Behav. 2014;39:1176–82. doi: 10.1016/j.addbeh.2014.03.008. http://www.dx.doi.org/10.1016/j.addbeh.2014.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miech R, Bohnert A, Heard K, Boardman J. Increasing use of nonmedical analgesics among younger cohorts in the United States: A birth cohort effect. J Adolesc Health. 2013;52:35–41. doi: 10.1016/j.jadohealth.2012.07.016. http://www.dx.doi.org/10.1016/j.jadohealth.2012.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miech R, Johnston L, O’Malley PM, Keyes KM, Heard K. Prescription opioids in adolescence and future opioid misuse. Pediatrics. 2015;136:e1169–77. doi: 10.1542/peds.2015-1364. http://www.dx.doi.org/10.1542/peds.2015-1364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nargiso JE, Ballard EL, Skeer MR. A systematic review of risk and protective factors associated with nonmedical use of prescription drugs among youth in the United States: A social ecological perspective. J Stud Alcohol Drugs. 2015;76:5–20. http://dx.doi.org/10.15288/jsad.2015.76.5. [PubMed] [Google Scholar]
- Nelson LS, Juurlink DN, Perrone J. Addressing the opioid epidemic. JAMA. 2015;314:1453–1517. doi: 10.1001/jama.2015.12397. [DOI] [PubMed] [Google Scholar]
- The White House. Fact Sheet: Obama Administration Announces Additional Actions to Address the Prescription Opioid Abuse and Heroin Epidemic; March 29, 2016; Washington, DC. 2016. [Accessed March 31 2016]. https://www.whitehouse.gov/thepress-office/2016/03/29/fact-sheet-obama-administration-announces-additionalactions-address. [Google Scholar]
- Research Triangle Institute. SUDAAN Language Manual, 2012. 1 and 2. Research Triangle Institute; Research Triangle Park, N.C: www.rti.org/sudaan. [Google Scholar]
- Salas J, Sherrer JF, Schneider FD. Racial differences in the association between nonmedical prescription opioid abuse/dependence, and major depression. Subst Abuse. 2016;37:25–30. doi: 10.1080/08897077.2015.1129523. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA) 2014 National Survey on Drug Use and Health Public Use Data File and Public Use File Codebook. PUF-2014_10/915. Center for Behavioral Health Statistics and Quality (CBHSQ); Rockville, MD: 2015a. [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA) Nonmedical use of prescription pain relievers varies by race and ethnicity. 2015b Jun 26; [Google Scholar]
- Schepis TS, McCabe SE. Trends in older adult nonmedical prescription drug use prevalence: Results from the 2002–2003 and 2012–2013 National Survey on Drug Use and Health. Addict Behav. 2016;60:219–22. doi: 10.1016/j.addbeh.2016.04.020. http://www.dx.doi.org/10.1016/j.addbeh.2016.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulenberg J, Maggs JL. Monitoring the Future Occaisional Paper 51. Institute for Social Research; Ann Arbor, MI: A developmental perspective on alcohol and other drug use during adolescence and the transition to young adulthood, 2001. [Google Scholar]
- StataCorp. Stata Statistical Software: Release 14, 2015. StataCorp LP; College Station, TX: [Google Scholar]
- Sussman S. A lifespan developmental-stage approach to tobacco and other drug abuse prevention. ISRN Addict. 2013;2013:19. doi: 10.1155/2013/745783. http://dx.doi.org/10.1155/2013/745783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Department of Health and Human Services (HHS) A report of the Surgeon General. Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion; Atlanta, GA: 2012. Preventing tobacco use among youth and young adults. [PubMed] [Google Scholar]
- Volkow ND. Altered pathways: Drug abuse and age of onset. Add Prof. 2006;4:26–9. [Google Scholar]
- Volkow ND, Frieden TR, Hyde PS, Cha SS. Medication-assisted therapies – tackling the opioid-overdose epidemic. N Engl J Med. 2014;370:2063–6. doi: 10.1056/NEJMp1402780. http://www.dx.doi.org/10.1056/NEJMp1402780. [DOI] [PubMed] [Google Scholar]
- Yamaguchi K. Drug use and its social covariates from the period of adolescence to young adulthood. In: Galanter M, editor. Recent developments in alcoholism. Springer; Boston, MA: 1990. pp. 125–43. [PubMed] [Google Scholar]
- Yamaguchi K, Kandel DB. On the resolution of role incompatibility: Life event history analysis of family roles and marijuana use. Am J Sociol. 1985;90:1284–1325. [Google Scholar]
- Yang Y, Schulhofer-Wohl S, Wenjiang JF, Land KC. The intrinsic estimator for age-period cohort analysis: What it is and how to use it. Am J Sociol. 2008;113:1697–1736. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.