Abstract
The shortage of health workers impedes universal coverage of quality HIV services, especially in those countries hardest hit by the epidemic. The dramatic increase in international aid to scale-up HIV services, including antiretroviral therapy (ART), has highlighted workforce deficiencies and provided an opportunity to strengthen health systems capacity. In Mozambique, a country with a high HIV burden and a staggering workforce deficit, the Ministry of Health looked to past experience in workforce expansion to rapidly build ART delivery capacity, including reliance on existing non-physician clinicians (NPC) to prescribe ART and dramatically increasing the output of NPC training. As a result of responsible task shifting, the number of facilities providing ART tripled during a 6-month period, and patients from disadvantaged areas have access to quality ART services. Because the NPC-driven ART approach is integrated into primary health care, the addition of new clinical staff also promises to improve general health services.
Keywords: AIDS/HIV, ART, health systems strengthening, human resources for health, task shifting, mozambique
The global shortage of health workers has become a matter of widespread concern, representing the principal impediment for achieving the health Millennium Development Goals and universal access to HIV services.1,2 The workforce shortage has been years in the making, caused by multiple factors, including low production of clinicians, inefficient and inappropriate placement, inadequate provider time devoted to public sector work, and brain drain, both internal and external. The clinical needs required for rapid expansion of HIV care and treatment with antiretroviral therapy (ART) have exacerbated the workforce shortage, further increasing the demand for trained clinicians, often in countries with an inadequate health workforce. We describe how efforts by the Mozambique Ministry of Health (MOH) to expand universal access to ART have reinvigorated the training of nonphysician clinicians (NPCs). We also describe how the process of task-shifting clinical responsibilities to NPCs has increased access to and quality of ART by integrating HIV care into primary health care (PHC) services.
BACKGROUND
The health workforce coverage in Mozambique has long been among the lowest in the world, with fewer than 3 physicians and 21 nurses per 100,000 inhabitants.3 Nearly half of Mozambican physicians work in the capital city, Maputo, worsening the poor coverage elsewhere.4 Mozambique’s health workforce crisis intensified shortly after independence in 1974, when the majority of physicians (mostly Portuguese nationals) left the country, with fewer than 80 physicians remaining to care for a population of 10.6 million.5,6 Since then, Mozambique has relied on expatriate physicians and a new category of health provider—specifically, técnicos de medicina—to take over many of the clinical and managerial tasks of the physicians who left Mozambique. Training and placement of técnicos was expanded to support the government’s efforts to rapidly expand PHC, emphasizing equitable access to preventive and basic curative services, which included an increase in the number of health facilities from 326 in 1975 to 1195 in 1985 and the training of an additional 10,000 health workers by 1990.7 The focus on expanding the cadre of técnicos was critical during this period, when Mozambique had fewer than 100 physicians and its sole medical school was producing only 10 to 25 new physicians per year. The expansion of the técnicos cadre was supported by the shorter training duration (initially 3 years, shortened to 2.5, compared with 6 years required to train physicians), the existence of multiple training institutes capable of producing new técnicos, lower training costs (estimated to be a one-tenth of that of physicians),8 and salaries that were a quarter of that of an average physician.9 Since its creation, the técnicos de medicina cadre has proven a stable force in the health system, staffing primarily rural underserved areas, with técnicos less prone than physicians to leave the public sector to work in nongovernmental agencies, the private sector, or health systems in wealthier nations.10
Despite the advantages of técnicos de medicina, the training of new health workers, including técnicos de medicina, was curtailed in Mozambique after 1986, largely due to structural adjustment policies that reduced public sector rolls and an intensifying war that affected health system training and management capacity.11 Interest in técnicos was renewed with the national commitment to provide universal ART in 2003. At that time, health system policymakers, managers, and donors grappled with building national capacity to meet the enormous HIV care needs in the country, which had an overall adult HIV prevalence of more than 15% and less than 1% of the estimated 1.2 million Mozambicans with HIV accessing ART.12 The creation of a national ART scale-up plan with new funding from the Clinton HIV/AIDS Initiative, the United States President’s Emergency Plan for AIDS Relief, and the Global Fund to Fight AIDS, Tuberculosis and Malaria provided an opportunity to build sustainable health workforce capacity that could strengthen the health system beyond HIV care itself. The scale-up plan focused on training physicians to initiate ART at 24 large referral hospitals in the first year, followed by rapid expansion and integration of ART into many smaller health facilities. Because the numbers of existing physicians were inadequate to cover the large number of facilities in the rapid scale-up, the national plan included a renewed effort to train new técnicos as an essential element of workforce expansion for HIV care. Moreover, the plan envisioned integrating ART into PHC, where physicians and técnicos would attend to all patients. Notably, the training of new physicians also increased at approximately the same time, with the creation of a new private medical school in 2001, creation of a new public medical school in 2006, and a doubling of school class size at Eduardo Mondlane University, the country’s primary medical school.
METHODS AND DATA SOURCES
Data regarding técnico and physician graduates, health facilities providing ART, and patients on ART were abstracted from routine Mozambique MOH reports and Eduardo Mondlane University records. Separate evaluations of quality of care were conducted by the authors.
RESULTS
The number of newly trained técnicos and medical students increased dramatically since the initiation of the national ART program (Fig. 1), and by mid-2006, the first wave of newly graduated técnicos had been deployed at health facilities. After authorization to prescribe ART in February 2006, a nationwide training initiative was launched that reached the majority of clinically active técnicos with 2 weeks of materials related to HIV care. Supported by the integrated care approach, the number of facilities with ART tripled over a 6-month period, including predominately small, rural, and periurban health centers, 45% of which were managed by a técnico de medicina. By March 2007, 167 health facilities covering 147 Mozambican districts and municipalities were capable of providing ART, accompanied by a growing number of patients on ART (Fig. 2).
FIGURE 1.
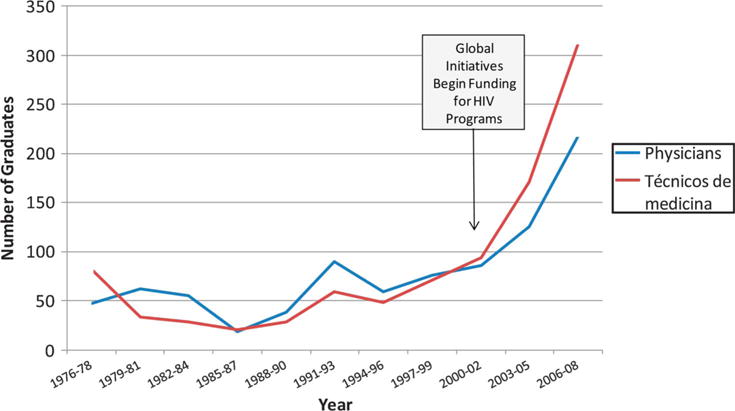
Number of physician and técnico de medicina graduates per 3-year period in Mozambique.
FIGURE 2.
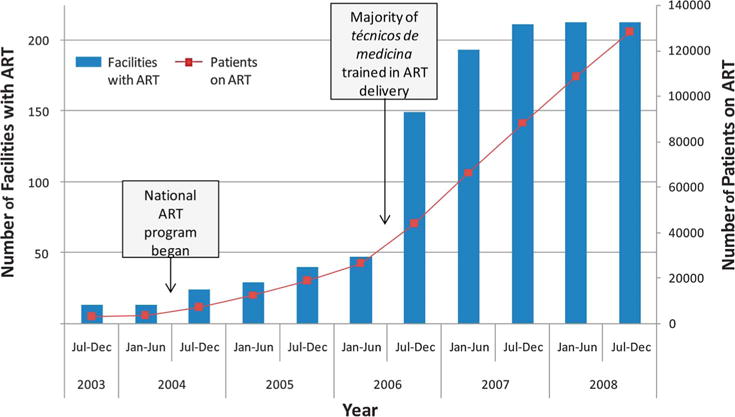
Scale-up of health facilities and patients on ART in Mozambique.
Separate evaluations have demonstrated that técnicos de medicina provide quality ART services. Results from a retrospective cohort study carried out among nearly 6000 patients initiating ART in 2 large urban HIV clinics staffed by both physicians and técnicos demonstrated statistically equivalent or better quality of care measures (including whether a CD4 was measured at 6 and 12 months post ART initiation, adherence to ARV medicines, and patient death or loss to follow-up) for patients whose initial providers were técnicos compared with those whose primary providers were physicians.13 Furthermore, técnicos were more present in these clinics, spending 160% more time seeing patients than physicians, though there were twice as many physicians staffing the clinics as técnicos. In a separate analysis of 24 facilities providing ART in central Mozambique, loss to follow-up among patients on ART was found to be 7.6% at clinics with lower patient volume that were almost exclusively staffed by técnicos, compared with 20.9% at high-volume clinics managed by physicians (P = 0.001).14
During 2007, as ART was integrated into the wider PHC system, the MOH phased out separate HIV care clinics, converting them into integrated ambulatory clinics that provide chronic care, including ART. This change has created opportunities to strengthen the capacity of técnicos, physicians, and nurses to diagnose and provide care for common chronic diseases, including hypertension, diabetes, and other conditions.
DISCUSSION
The experience in Mozambique has demonstrated how ART expansion has increased both the reliance on NPCs for HIV care and the overall number of clinical providers. These workforce strategies facilitated the integration of ART into PHC, resulting in an increase in numbers of both facilities providing ART and patients receiving quality ART. The recognition by the MOH and donors of Mozambique’s human resource deficits, accompanied by the infusion of new funding associated with ART, facilitated the development of pragmatic strategies to meet the increased clinical staffing requirements associated with ART expansion and general PHC needs.
The ART imperative justified an accelerated training plan that was widely supported throughout the Mozambique government and donor agencies, creating new policy space to rapidly expand the government health workforce. External funding for HIV care has not only been a critical element of workforce expansion but has also facilitated the rehabilitation of health facilities and improved laboratory capacity in ways that enhance the quality of all care services.
Integration of HIV care into PHC has facilitated efficiency in overall workforce allocation, reducing the number of clinical staff that would otherwise be removed from general care to staff vertical HIV centers of excellence. Deployment of newly trained técnicos provides opportunities to staff rural and smaller urban clinics with clinical cadres that are more likely to continue to work in PHC provided via the public sector. Furthermore, training, salaries, and benefits cost less for técnicos than for physicians.
Given the positive experience with técnicos in HIV care, Mozambique will likely continue to train and employ técnicos as a viable long-term strategy for meeting Mozambique’s health workforce needs. Even with the recent expansion of physician providers, Mozambique remains far from meeting the estimated 7-fold increase in health workers necessary to reach the Millennium Development Goals.15 Using a mix of physicians and responsible task shifting to nonphysician providers, the Mozambique health system can maintain its momentum in ART scale-up while strengthening the wider PHC system.
Acknowledgments
Supported by a grant from the Doris Duke Charitable Foundation’s Operations Research for AIDS Care and Treatment in Africa (ORACTA) Initiative.
Footnotes
Data presented: not applicable.
References
- 1.Scheffler RM, Liu JX, Kinfu Y, et al. Forecasting the global shortage of physicians: an economic- and needs-based approach. Bull World Health Organ. 2008;86:516B–523B. doi: 10.2471/BLT.07.046474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chen L, Evans T, Anand S, et al. Human resources for health: overcoming the crisis. Lancet. 2004;364:1984–1990. doi: 10.1016/S0140-6736(04)17482-5. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization (WHO) The World Health Report 2006: Working Together for Health. Geneva, Switzerland: WHO; 2006. [Google Scholar]
- 4.Decima E, Dreesch N, Kiarie W. Human Capacity Development (HCD) Assessment and Strategy Development for the Health Sector in Mozambique. Washington, DC: US Agency for International Development; 2004. [Google Scholar]
- 5.Pereira C, Cumbi A, Malalane R, et al. Meeting the need for emergency obstetric care in Mozambique: work performance and histories of medical doctors and assistant medical officers trained for surgery. BJOG. 2007;114:1530–1533. doi: 10.1111/j.1471-0528.2007.01489.x. [DOI] [PubMed] [Google Scholar]
- 6.World Population Prospects: The 2008 Revision. [Web page] New York, NY: United Nations Web site; Population Division of the Department of Economic and Social Affairs of the United Nations Secretariat. Available at: http://esa.un.org/unpp. Accessed June 1, 2009. [Google Scholar]
- 7.Lindelow M, Ward P, Zorzi N. Primary Health Care in Mozambique: Service Delivery in a Complex Hierarchy. Washington, DC: The World Bank; p. 2004. (Africa Region Human Development Working Paper Series). [Google Scholar]
- 8.Ipas and IHCAR (Division of International Health of the Department of Public Health Sciences, Karolinska Institutet, Stockholm) Deciding Women’s Lives Are Worth Saving: Expanding the Role of Midlevel Providers in Safe Abortion Care. Chapel Hill, NC: Ipas and IHCAR; 2004. Issues in Abortion Care 7. [Google Scholar]
- 9.Ministério da Saúde. Plano estratégico de desenvolvimento dos recursos humanos, periódo 2005–2010. Maputo, Mozambique: Ministério da Saúde;; 2005. [Google Scholar]
- 10.Dovlo D. Using mid-level cadres as substitutes for internationally mobile health professionals in Africa: a desk review. Hum Resour Health. 2004;2:7. doi: 10.1186/1478-4491-2-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cliff J. Donor dependence or donor control? The case of Mozambique. Community Dev J. 1993;28:237–244. [Google Scholar]
- 12.Instituto Nacional de Estatistica (INE) Impacto demográfico do HIV/SIDA em Moçxambique. Maputo, Mozambique: INE; 2002. [Google Scholar]
- 13.Gimbel-Sherr K, Augusto O, Micek M, et al. Task shifting to mid-level clinical health providers: an evaluation of quality of ART provided by técnicos de medicina and physicians in Mozambique [abstract WEAX0105]. Presented at: XVII International AIDS Conference; August 3–8, 2008; Mexico City, Mexico. [Google Scholar]
- 14.Lambdin B, Micek M, Pfeiffer J, et al. Impact of human resource levels and patient volume on loss to follow-up and mortality in antiretroviral therapy programs in Mozambique [abstract TUPED115]. Presented at: 5th IAS Conference on HIV Pathogenesis, Treatment and Prevention; July 19–22, 2009; Cape Town, South Africa. [Google Scholar]
- 15.Ooms G, Van Damme W, Temmerman M. Medicines without doctors: why the Global Fund must fund salaries of health workers to expand AIDS treatment. PLoS Med. 2007;4:e128. doi: 10.1371/journal.pmed.0040128. Available at: http://doctorswithoutborders.org/events/symposiums/2008-aids-iac/assets/files/Medicins-without-Doctors-PLoS.pdf. Accessed May 28, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]


