Abstract
Background
Apalutamide is a potent androgen receptor (AR) antagonist that targets the AR ligand-binding domain and prevents AR nuclear translocation, DNA binding, and transcription of AR gene targets. Objective: To evaluate the activity and safety of apalutamide in patients with high-risk nonmetastatic castration-resistant prostate cancer (nmCRPC).
Design, setting, and participants
We conducted a multicenter phase 2 study of nmCRPC patients with a high risk for progression (prostate-specific antigen [PSA] ≥8 ng/ml or PSA doubling time [PSA DT] ≤10 mo).
Intervention
Patients received 240 mg/d apalutamide while continuing on androgen-deprivation therapy.
Outcome measurements and statistical analysis
Primary end point was 12-wk PSA response (Prostate Cancer Working Group 2 criteria). Secondary end points included safety, time to PSA progression (TTPP), and metastasis-free survival (MFS).
Results and limitations
A total of 51 patients were enrolled; four patients with metastatic disease were excluded from the efficacy analysis. Patient characteristics included median age, 71 yr; Eastern Cooperative Oncology Group performance status 0 (76%); Gleason score ≤ 7 (57%); median PSA 10.7 ng/ml; and PSA DT ≤10 mo (45%). At median follow-up of 28.0 mo, 18 patients (35%) remained in the study. Overall, 89% of patients had ≥50% PSA decline at 12 wk. Median TTPP was 24.0 mo (95% confidence interval [CI], 16.3 mo–not reached [NR]); median MFS was NR (95% CI, 33.4 mo–NR). Most of the patients discontinued study treatment (n = 33) due to disease progression (n = 11 [22%]) or adverse events (AEs) (n = 9 [18%]). The most common AE was fatigue (any grade, n = 31 [61%]) although grade ≥3 fatigue was uncommon (n = 2 [4%]). These represent the first apalutamide nmCRPC patient clinical data.
Conclusions
In high-risk nmCRPC patients, apalutamide was safe with robust activity based on durable PSA responses and disease control.
Patient summary
Antitumor activity and the safety of apalutamide in patients with nonmetastatic castration-resistant prostate cancer support continued development in this setting.
Trial registration
ClinicalTrials.gov identifier NCT01171898
Keywords: Antitumor activity, Apalutamide, Castration-resistant prostate cancer, Safety
1. Introduction
Androgen-deprivation therapy (ADT) is the standard first-line treatment for patients with metastatic prostate cancer (PCa) and a routine part of management for many men with nonmetastatic PCa. Initial ADT achieves responses in nearly all patients, although most patients progress to castration-resistant disease within a few years [1]. In men with nonmetastatic castration-resistant prostate cancer (nmCRPC), higher prostate-specific antigen (PSA) and shorter PSA doubling time (PSA DT) are associated with high risk for metastases and death [2–4]. Examining patients at regular intervals is important because patients with a short PSA DT are often found with occult metastases. National Comprehensive Cancer Network PCa clinical practice guidelines recommend more frequent bone imaging for patients with a PSA DT ≤ 8 mo [5]. To date, there are no approved treatments for nmCRPC.
Apalutamide is a potent antagonist of the androgen receptor (AR) in development for the treatment of men with CRPC as well as earlier disease including localized PCa and metastatic hormone-sensitive PCa [6]. Apalutamide selectively binds to the ligand-binding domain of AR and blocks AR nuclear translocation or binding to androgen response elements. Unlike bicalutamide, apalutamide antagonized AR-mediated signaling in AR overexpressing human CRPC cell lines [7]. In mice bearing human CRPC xenografts, apalutamide produced dose-dependent tumor regressions superior to those achieved with bicalutamide or enzalutamide [6].
On the basis of these promising preclinical results, a first-in-human phase 1/2 study was conducted (ARN-509-001) in patients with CRPC. The 18F-fluoro-α-dihydrotestosterone positron emission tomography/computed tomography imaging analysis in 16 patients with metastatic CRPC (mCRPC) indicated an optimal biologic dose of 240 mg/d of apalutamide; the phase 1 portion of the study in 30 mCRPC patients determined that a phase 2 dose of 240 mg/d was safe and well tolerated [8]. The phase 2 portion of the study evaluates apalutamide activity in three distinct patient cohorts: nmCRPC, abiraterone acetate–naive mCRPC, and post–abiraterone acetate mCRPC. We report the phase 2 results for patients in the nmCRPC cohort.
2. Patients and methods
ARN-509-001 (NCT01171898) is a phase 1/2 multicenter open-label study. Phase 1 was completed in May 2012 and the results were published [8]. Patients were enrolled into the phase 2 expansion cohorts from November 2011 to June 2012, and the study is ongoing. The review boards at all participating institutions approved the study that was conducted according to the Declaration of Helsinki, the International Conference on Harmonisation, and the Guidelines for Good Clinical Practice. All patients gave written informed consent.
2.1. Patients
All patients had histologically or cytologically confirmed PCa and had received ongoing ADT with a gonadotropin-releasing hormone analog or inhibitor, or orchiectomy (ie, surgical or medical castration). Patients in the nmCRPC cohort had no radiographic evidence of distant metastases (central nervous system [CNS], vertebral, or meningeal) as determined by central review (pelvic lymph nodes <3 cm below the iliac bifurcation were allowed). They met the following inclusion criteria: castrate levels of serum testosterone ≤50 ng/dl within 4 wk of study enrollment, an Eastern Cooperative Oncology Group performance status of 0–1, a life expectancy ≥3 mo, a corrected QT interval ≤450 ms, and adequate cardiac, renal, hepatic, and bone marrow function. The patients had a high risk for developing metastases, defined as either a PSA value ≥8 ng/ ml obtained within 3 mo prior to enrollment or PSA DT ≤10 mo. Patients were excluded if they had been treated previously with enzalutamide, abiraterone acetate, or ketoconazole, or had a history of seizures or conditions that predispose to seizures or concurrent treatment with medications known to have seizure potential.
2.2. Study design
Patients were enrolled in three cohorts: nmCRPC, chemotherapy/ abiraterone acetate–naive mCRPC, and mCRPC post–abiraterone acetate, as shown in Figure 1 [8]. This study focuses on the high-risk nmCRPC expansion cohort. Patients received apalutamide 240 mg/d based on the biologically efficacious dose established in the phase 1 study [8]. Patients with nmCRPC received continuous daily dosing until disease progression defined as evidence of PSA progression and radiographic progression as described below, or clinical progression alone (skeletal-related event or pain progression requiring intervention). Dose modifications (eg, short treatment breaks or dose reduction) were allowed in case of treatment-related adverse events (AEs).
Fig. 1.
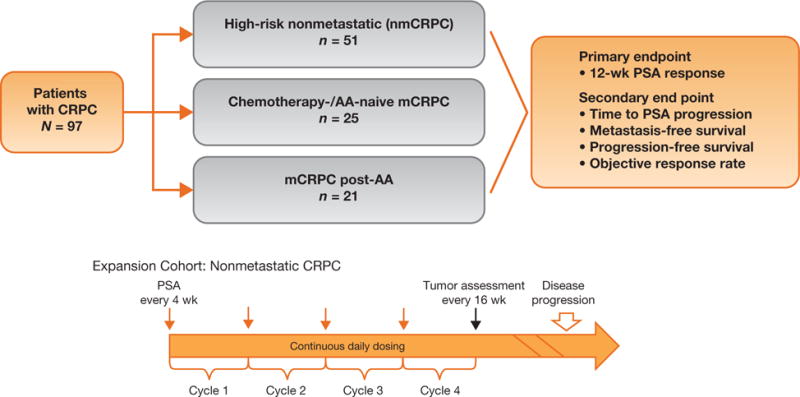
Study design. Progression-free survival not analyzed for the nonmetastatic castration-resistant prostate cancer (nmCRPC) cohort and for four patients with metastatic disease not included in the nmCRPC efficacy analysis.
AA = abiraterone acetate; CRPC = castration-resistant prostate cancer; mCRPC = metastatic castration-resistant prostate cancer; PSA = prostate-specific antigen.
2.3. End points
PSA response was assessed using the Prostate Cancer Working Group 2 (PCWG2) criteria [9]. Imaging evaluations were performed every 16 wk. The primary end point was the posttreatment percentage change in PSA relative to baseline at 12 wk (or earlier for those who discontinued therapy) and maximal change at any time on the study. The secondary efficacy end points included time to PSA progression (TTPP), measured from the start of treatment until the criteria for PSA progression were met, according to the modified PCWG2 (≥25% and >2 ng/ml above PSA nadir confirmed ≥3 wk later or >2 ng/ml above baseline PSA after 12 wk), and metastasis-free survival (MFS), measured from the start of treatment until new metastatic lesions were seen on computed tomography/magnetic resonance imaging scans by modified Response Evaluation Criteria in Solid Tumors [10] and/or 99m-technetium-methylene diphosphate bone scans (after repeat imaging ≥6 wk later), independently verified by central imaging.
2.4. Safety
Safety was assessed on an ongoing basis from the first dose until 30 d after the last dose or until the resolution of any drug-related AE.
2.5. Statistical analysis
The sample size was based primarily on clinical judgment. A combined 12-wk PSA response rate of at least 20% in the nmCRPC cohort was considered of clinical interest to warrant further development of apalutamide in nmCRPC. If 22 of 70 patients (including a chemotherapy/abiraterone acetate cohort not described here) achieved a 12-wk PSA response of at least 50%, the lower exact 95% confidence interval (CI) was 20.9% with the upper limit of 43.6%. All patients who received at least one dose of apalutamide were included in the efficacy (excluding four patients who had baseline metastases) and safety analyses. Summary statistics were reported for demographics, baseline characteristics, AEs, vital signs, and clinical laboratory evaluations. The change in PSA at 12 wk relative to baseline and the maximal change in PSA at any time on the study relative to baseline are presented in waterfall plots and descriptively summarized. The Kaplan-Meier method was used to estimate the median time to events and 95% CIs.
3. Results
3.1. Patients
The high-risk nmCRPC cohort enrolled 51 patients from November 2011 to June 2012. The data cut-off for database lock and primary analysis was December 31, 2014. Median patient age was 71 yr (range: 51–88); most patients were white (47 of 51 [92%]). Median baseline PSA was 10.7 ng/ml (Table 1). Patients were enrolled with a PSA ≥8 ng/ml (21 of 51 [41%]) or PSA DT ≤10 mo (23 of 51 [45%]), with seven patients having both criteria met (14%). Most patients (80%) had received prior treatment with a first-generation anti-androgen (ie, bicalutamide, flutamide, or nilutamide) (Table 1). Four patients had metastatic disease and were excluded from the efficacy analysis because they later were determined to have metastases on their screening scans (Fig. 2). At a median follow-up of 28.0 mo, 18 of 51 patients (35%) remained in the study. Most who went off the study did so either for disease progression (11 of 51 [22%]) or AEs (9 of 51 [18%]). The median treatment duration was 26.9 mo (range: <1–37.8).
Table 1.
Patient characteristics
| High-risk nmCRPC | |
|---|---|
| n | 51 |
| Age, yr, median (range) | 71 (51–88) |
| ECOG PS, n (%) | |
| 0 | 39 (76) |
| 1 | 12 (24) |
| Gleason score at initial diagnosis, n (%) | |
| ≤7 | 29 (57) |
| 8–10 | 18 (35) |
| Not available | 4 (8) |
| Time since initial diagnosis, mo, median (range) | 119.5 (20–238) |
| Baseline PSA, ng/ml, median (range) | 10.7 (0.5–201.7) |
| High-risk definition, n (%) | |
| PSA ≥8 ng/ml, median (range) | 21 (41) |
| PSA DT ≤10 mo | 23 (45) |
| Both criteria | 7 (14) |
| Prior hormonal therapy, n (%) | |
| LHRH | 46 (90)* |
| Antiandrogen† | 41 (80) |
| Bicalutamide | 41 (80) |
| Flutamide | 6 (12) |
| Nilutamide | 8 (16) |
ECOG PS = Eastern Cooperative Oncology Group performance status; LHRH = luteinizing hormone-releasing hormone; nmCRPC = nonmetastatic castration-resistant prostate cancer; PSA = prostate-specific antigen; PSA DT = prostate-specific antigen doubling time.
Three patients had an orchiectomy; two patients did not receive ongoing hormonal therapy because serum testosterone was at castrate levels at screening and remained at castrate levels without LHRH.
Patients may have been treated with more than one antiandrogen.
Fig. 2.
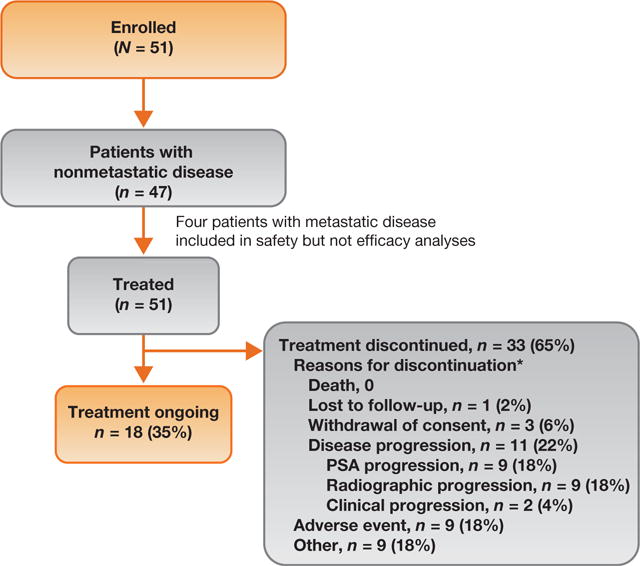
Patient disposition.
PSA = prostate-specific antigen.
*Patients may have discontinued due to more than one type of progression.
3.2. Prostate-specific antigen outcome
The median change in PSA from baseline to week 12, per PCWG2 criteria, was −85% (range: −99.9 to 52.2). The median maximal change in PSA from baseline to any point during the study was −93% (range: −99.9 to 47.5). This corresponded to a PSA response (≥50% decline in PSA after baseline) at 12 wk of 89% (Table 2 and Fig. 3A). The maximal PSA response (maximal percentage reduction [≥50%] after baseline at any time) was reported in 94% of patients (Table 2 and Fig. 3B).
Table 2.
Efficacy outcomes
| High-risk nmCRPC (n = 47)* | |
|---|---|
| PSA response, wk, n (%)† | |
| 12 | 42/47 (89) |
| 24 | 40/47 (85) |
| 36 | 22/47 (47) |
| Maximal PSA response, n (%)‡ | 44/47 (94) |
| Median MFS, mo (95% CI) | NR (33.4–NR) |
| Median time to PSA progression, mo (95% CI) | 24.0 (16.3–NR) |
CI = confidence interval; MFS = metastasis-free survival; nmCRPC = nonmetastatic castration-resistant prostate cancer; NR = not reached; PSA = prostate-specific antigen.
Four patients with metastatic disease at baseline were not included.
A ≥50% decline in PSA from baseline from Prostate Cancer Working Group 2.
Maximal PSA response is the maximal percentage reduction after baseline at any time point.
Fig. 3.
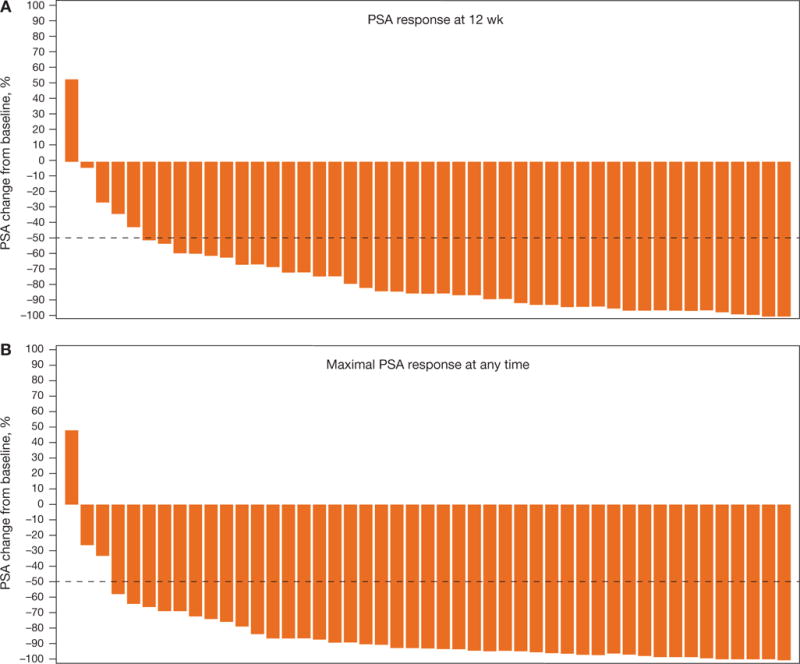
Waterfall plot for (A) 12-wk prostate-specific antigen (PSA) response and (B) maximal PSA response at any time.
3.3. Secondary end points
A total of 53% of patients (25 of 47) with nmCRPC had PSA progression while on the study. At a median follow-up of 28.0 mo, the median TTPP and MFS were 24 mo (95% CI, 16.3 mo-not reached [NR]) and NR (95% CI, 33.4 mo-NR), respectively (Table 2 and Fig. 4).
Fig. 4.
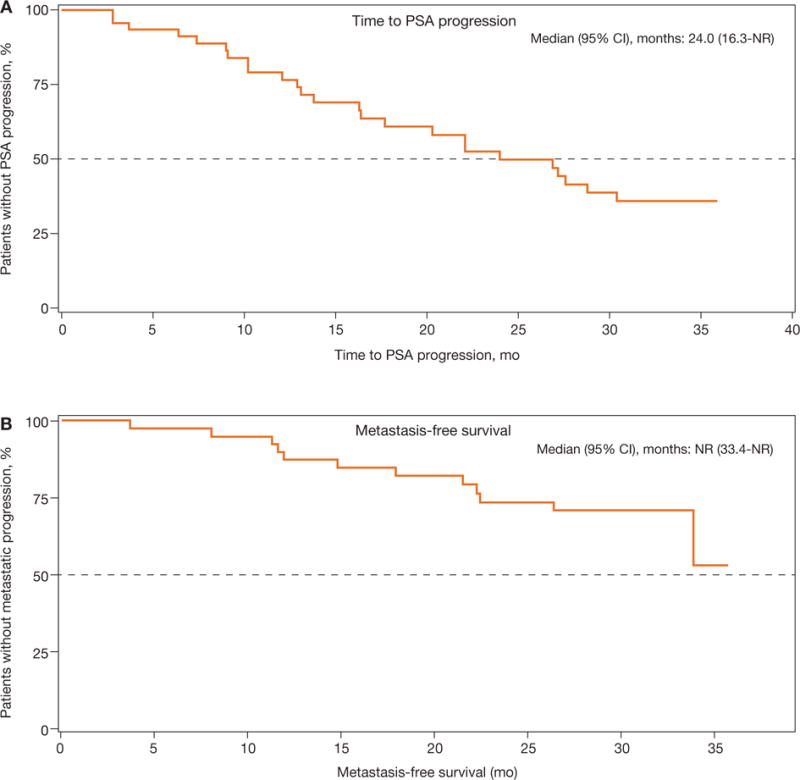
Secondary end points: (A) Time to prostate-specific antigen progression (PSA); (B) metastasis-free survival.
CI = confidence interval; NR = not reached.
3.4. Safety
The most common treatment-emergent adverse events (TEAEs) regardless of relationship to the study drug were fatigue (61%), diarrhea (43%), and nausea (39%) (Table 3). Most TEAEs were grade 1 or 2. Grade ≥3 TEAEs reported in more than one patient each were fatigue (n = 2 [4%]), hypertension (n = 2 [4%]), and malignant melanoma (n = 2 [4%]). The most common TEAEs related to study treatment were fatigue (45%), diarrhea (29%), and nausea (25%); no serious TEAEs were considered related to study treatment. No seizures, amnesia, or visual disturbance were reported. Headache and dizziness were reported in seven patients (14%) and six patients (12%), respectively. TEAEs of a fall (all grade 1 or 2) were reported in five patients (10%) with a resultant grade 1 contusion in one patient. Another patient had several TEAEs (all grade 1 or 2) including a contusion secondary to a fall not reported as an AE. TEAEs that led to permanent treatment discontinuation were fatigue (n = 2 [4%]); abdominal adhesions, bone marrow tumor cell infiltration, brain cancer, colorectal cancer, decreased appetite, drug hypersensitivity, dysphagia, esophageal cancer, nerve root compression, and macular rash (n = 1 [2% each]); it was possible for patients to experience more than one TEAE leading to treatment discontinuation. TEAEs that led to dose modification were fatigue (n = 2 [4%]); choking, contusion, erythematous rash, and vomiting (n = 1 [2% each]). TEAEs that led to dose interruption were observed in 15 patients (29%); the only TEAE leading to dose interruption that was observed in more than one patient was diarrhea in two patients (4%).
Table 3.
Treatment-emergent adverse events occurring in ≥15% of patients
| High-risk nmCRPC (n = 51) | ||
|---|---|---|
| All grades | Grade ≥3* | |
| No. of patients with ≥1 TEAE | 51 (100) | 21 (41) |
| No. of patients with a serious TEAE | 16 (31) | 12 (24) |
| TEAEs, n (%) | All grades | Grade ≥3* |
| Fatigue | 31 (61) | 2 (4) |
| Diarrhea | 22 (43) | 1 (2) |
| Nausea | 20 (39) | 0 |
| Arthralgia | 11 (22) | 1 (2) |
| Back pain | 11 (22) | 0 |
| Dysgeusia | 11 (22) | 0 |
| Hypothyroidism | 11 (22) | 0 |
| Hot flush | 10 (20) | 0 |
| Pain in extremity | 10 (20) | 1 (2) |
| Cough | 10 (20) | 0 |
| Abdominal pain | 9 (18) | 0 |
| Decreased weight | 9 (18) | 0 |
| Pollakiuria | 9 (18) | 0 |
| Constipation | 8 (16) | 0 |
| Nasopharyngitis | 8 (16) | 0 |
| Hematuria | 8 (16) | 0 |
| Upper respiratory infection | 8 (16) | 0 |
nmCRPC = nonmetastatic castration-resistant prostate cancer; TEAE = treatment-emergent adverse event.
Listed grade ≥3 adverse events are those with an overall incidence ≥15%.
4. Discussion
In this phase 2 study of apalutamide, we confirm the safety and tolerability profile of the previously established biologically efficacious dose of 240 mg/d [8] in the nmCRPC cohort. This study used several measures to determine the antitumor activity of apalutamide including declines in PSA level per PCWG2 criteria [9], TTPP, and MFS. With apalutamide treatment, 89% of patients (42 of 47) with high-risk nmCRPC experienced a ≥50% decline in PSA level after 12 wk on the study, with a maximal PSA response (≥50% after baseline at any time) reported in 94% of patients (44 of 47). At 28.0 mo of follow-up, the median TTPP and MFS were 24 mo and NR, respectively. Grade 3 and 4 TEAEs were infrequent. The most common treatment-related TEAEs were fatigue (45%), diarrhea (29%), and nausea (25%); these were mostly grade 1 and 2. Collectively, these data support the continued clinical development of apalutamide in future efficacy and safety studies of men with nmCRPC.
The most common grade 3 and 4 TEAEs were fatigue (n = 2 [4%]), hypertension (n = 2 [4%]), and malignant melanoma (n = 2 [4%]). Grade 3 secondary malignant melanomas were observed after 2.5 yr in one patient and 1 yr in a second. They were considered unrelated to the study drug and were not associated with dose reductions or interruptions. The most common treatment-related TEAEs were fatigue (45%), diarrhea (29%), and nausea (25%); these were mostly grade 1 and 2. Overall, apalutamide was safe and well tolerated.
Risk of seizures has been identified with AR antagonists as a class and is thought to be mediated via CNS-based γ -aminobutyric acid A receptors [11]; this represents an exclusion criterion in studies of enzalutamide [12–14] as in the current study with apalutamide. No seizures were reported in the current study, consistent with the safety data from the phase 1 clinical trial of apalutamide [8]. Falls have been reported to be more frequently observed with enzalutamide compared with placebo [12] and may also represent an AR antagonist class risk related to CNS effects. In the current study, five patients experienced grade 1 and 2 falls, but these falls were not reported as serious and did not result in discontinuation of the study drug.
Safe and effective treatment to delay or prevent the development of metastatic disease in nmCRPC is an important unmet medical need. The results of phase 3 metastasis prevention studies of zoledronic acid, denosumab, clodronic acid, and atrasentan did not support the regulatory approval of these agents for treatment of patients with nmCRPC [15–18]. The results of these phase 3 studies, however, have helped define the natural history of nmCRPC and facilitate the description of high risk based on PSA kinetics.
Strengths of this phase 2 study include the multicenter design and relatively long follow-up interval. The pre-specified definition of the high-risk nmCRPC cohort is also a substantial strength. Limitations include the nonrandomized nature of the study and the modest sample size.
The results of this phase 2 study informed the design of the global SPARTAN study (NCT01946204). SPARTAN is a multicenter double-blind placebo-controlled phase 3 trial to evaluate the efficacy and safety of apalutamide in patients with nmCRPC at high risk for progression, defined as a PSA DT ≤10 mo. The primary end point is MFS. Key secondary end points are overall survival, time to symptomatic progression, time to initiation of cytotoxic chemotherapy, radiographic progression-free survival, and time to metastasis. SPARTAN is ongoing [19]. Additional phase 3 trials in the high-risk nmCRPC patient population are also under way for the AR inhibitors enzalutamide (NCT02003924 [20]) and ODM-201 (NCT02200614 [21]).
In the absence of comparative studies of apalutamide, enzalutamide, and ODM-201, it is not possible to draw conclusions about the relative efficacy and safety of the different AR antagonists in the treatment of patients with nmCRPC. Nevertheless, AR antagonists appear promising in exerting clinical benefit in the nmCRPC population based on the results of this study as well as those of the STRIVE study [13].
Overall, apalutamide was well tolerated in this cohort of patients with high-risk nmCRPC, with a safety profile consistent with the previous phase 1 study. No serious TEAEs or seizures were reported.
5. Conclusions
Apalutamide was safe and well tolerated in patients with high-risk nmCRPC in the phase 2 portion of the study. Apalutamide exhibited robust activity in patients with high-risk nmCRPC based on durable PSA responses and disease control. These results support further clinical development of apalutamide in nmCRPC.
Acknowledgments
Writing assistance was provided by Ira Mills of PAREXEL and Patricia Pelton of Janssen Research & Development.
Funding/Support and role of the sponsor: This study was funded by Aragon Pharmaceuticals, Inc. and supported by Janssen Research & Development. The sponsors were involved in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, and approval of the manuscript. Janssen Research & Development, LLC, is performing work on behalf of Aragon. Writing assistance was funded by Janssen Global Services, LLC.
Footnotes
Author contributions: Matthew R. Smith had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Smith, Antonarakis, Shore, Higano, Chow Maneval, Rathkopf.
Acquisition of data: Smith, Antonarakis, Ryan, Berry, Shore, Liu, Alumkal, Higano, Chow Maneval, Rathkopf.
Analysis and interpretation of data: Smith, Antonarakis, Ryan, Shore, Liu, Alumkal, Higano, Chow Maneval, Bandekar, de Boer, Yu, Rathkopf. Drafting of the manuscript: Smith, Shore, Alumkal, Higano, de Boer, Yu. Critical revision of the manuscript for important intellectual content: Smith, Antonarakis, Ryan, Shore, Liu, Alumkal, Higano, Chow Maneval, Bandekar, de Boer, Yu, Rathkopf.
Statistical analysis: Bandekar.
Obtaining funding: Yu.
Administrative, technical, or material support: Yu.
Supervision: Yu.
Other (specify): None.
Financial disclosures: Matthew R. Smith certifies that all conflicts of interest, including specific financial interests and relationships and affiliations relevant to the subject matter or materials discussed in the manuscript (eg, employment/affiliation, grants or funding, consultancies, honoraria, stock ownership or options, expert testimony, royalties, or patents filed, received, or pending), are the following: Matthew R. Smith has served as a consultant to Janssen Research & Development. Emmanuel S. Antonarakis has served as a consultant/adviser to Janssen Biotech, Astellas, Medivation, ESSA, Sanofi, and Dendreon; he has received research funding from Aragon Pharmaceuticals, Johnson & Johnson, Janssen Biotech, Astellas, Tokai, Sanofi, Dendreon, Exelixis, Novartis, and Genentech. Charles J. Ryan has received honoraria from Janssen Research & Development. William R. Berry has received research grants from AHRQ. Neal D. Shore is a consultant/adviser to Algeta, Amgen, Bayer, BNI, Dendreon, Ferring, Janssen, Millennium, and Sanofi. Glenn Liu has nothing to report. Joshi J. Alumkal has received research funding from Aragon Pharmaceuticals. Celestia S. Higano received consulting fees or honoraria from AbbVie, Algeta, Astellas, Bayer, Dendreon, Genentech, Johnson & Johnson, Medivation, Novartis, Pfizer, and Veridex; grants or research support from Amgen, Aragon Pharmaceuticals, AstraZeneca, Bayer, Dendreon, Exelixis, Genentech, Johnson & Johnson, Medivation, Millennium, Novartis, OncoGenex, Sanofi-Aventis US, Taxynergy, and Teva; and other financial benefits from Cell Therapeutics. Edna Chow Maneval was an employee at Aragon Pharmaceuticals. Rajesh Bandekar is an employee of Janssen Research & Development and holds stock and stock options in Johnson & Johnson. Carla J. de Boer is an employee of Janssen Biologics and holds stock and stock options in Johnson & Johnson. Margaret K. Yu is an employee of Janssen Research & Development and holds stock and stock options in Johnson & Johnson. Dana E. Rathkopf has served as a consultant/adviser to and has received research funding from Janssen Research & Development, AstraZeneca, Celgene, Ferring, Medivation, Millennium/ Takeda, and Novartis.
References
- 1.Chi KN, Bjartell A, Dearnaley D, et al. Castration-resistant prostate cancer: from new pathophysiology to new treatment targets. Eur Urol. 2009;56:594–605. doi: 10.1016/j.eururo.2009.06.027. [DOI] [PubMed] [Google Scholar]
- 2.Smith MR, Kabbinavar F, Saad F, et al. Natural history of rising serum prostate-specific antigen in men with castrate nonmetastatic prostate cancer. J Clin Oncol. 2005;23:2918–25. doi: 10.1200/JCO.2005.01.529. [DOI] [PubMed] [Google Scholar]
- 3.Smith MR, Cook R, Lee KA, Nelson JB. Disease and host characteristics as predictors of time to first bone metastasis and death in men with progressive castration-resistant nonmetastatic prostate cancer. Cancer. 2011;117:2077–85. doi: 10.1002/cncr.25762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Smith MR, Saad F, Oudard S, et al. Denosumab and bone metastasis-free survival in men with nonmetastatic castration-resistant prostate cancer: exploratory analyses by baseline prostate-specific antigen doubling time. J Clin Oncol. 2013;31:3800–6. doi: 10.1200/JCO.2012.44.6716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Prostate cancer, v.1.2016. National Comprehensive Cancer Network; NCCN clinical practice guidelines in oncology (NCCN Guidelines) Web site. http://www.nccn.org/professionals/physician_gls/pdf/prostate.pdf. [DOI] [PubMed] [Google Scholar]
- 6.Clegg NJ, Wongvipat J, Joseph JD, et al. ARN-509: a novel antiandrogen for prostate cancer treatment. Cancer Res. 2012;72:1494–503. doi: 10.1158/0008-5472.CAN-11-3948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jung ME, Ouk S, Yoo D, et al. Structure-activity relationship for thiohydantoin androgen receptor antagonists for castration-resistant prostate cancer (CRPC) J Med Chem. 2010;53:2779–96. doi: 10.1021/jm901488g. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rathkopf DE, Morris MJ, Fox JJ, et al. Phase I study of ARN-509, a novel antiandrogen, in the treatment of castration-resistant prostate cancer. J Clin Oncol. 2013;31:3525–30. doi: 10.1200/JCO.2013.50.1684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Scher HI, Halabi S, Tannock I, et al. Design and end points of clinical trials for patients with progressive prostate cancer and castrate levels of testosterone: recommendations of the Prostate Cancer Clinical Trials Working Group. J Clin Oncol. 2008;26:1148–59. doi: 10.1200/JCO.2007.12.4487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Therasse P, Arbuck SG, Eisenhauer EA, et al. New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst. 2000;92:205–16. doi: 10.1093/jnci/92.3.205. [DOI] [PubMed] [Google Scholar]
- 11.Foster WR, Car BD, Shi H, et al. Drug safety is a barrier to the discovery and development of new androgen receptor antagonists. Prostate. 2011;71:480–8. doi: 10.1002/pros.21263. [DOI] [PubMed] [Google Scholar]
- 12.Beer TM, Armstrong AJ, Rathkopf DE, et al. Enzalutamide in metastatic prostate cancer before chemotherapy. N Engl J Med. 2014;371:424–33. doi: 10.1056/NEJMoa1405095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Penson DF, Armstrong AJ, Concepcion R, et al. Enzalutamide versus bicalutamide in castration-resistant prostate cancer: the STRIVE trial. J Clin Oncol. 2016 Jan 25; doi: 10.1200/JCO.2015.64.9285. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 14.Scher HI, Fizazi K, Saad F, et al. Increased survival with enzalutamide in prostate cancer after chemotherapy. N Engl J Med. 2012;367:1187–97. doi: 10.1056/NEJMoa1207506. [DOI] [PubMed] [Google Scholar]
- 15.Mason MD, Sydes MR, Glaholm J, et al. Oral sodium clodronate for nonmetastatic prostate cancer–results of a randomized double-blind placebo-controlled trial: Medical Research Council PR04 (ISRCTN61384873) J Natl Cancer Inst. 2007;99:765–76. doi: 10.1093/jnci/djk178. [DOI] [PubMed] [Google Scholar]
- 16.Nelson JB, Love W, Chin JL, et al. Phase 3, randomized, controlled trial of atrasentan in patients with nonmetastatic, hormone-refractory prostate cancer. Cancer. 2008;113:2478–87. doi: 10.1002/cncr.23864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Smith MR, Saad F, Coleman R, et al. Denosumab and bone-metastasis-free survival in men with castration-resistant prostate cancer: results of a phase 3, randomised, placebo-controlled trial. Lancet. 2012;379:39–46. doi: 10.1016/S0140-6736(11)61226-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wirth M, Tammela T, Cicalese V, et al. Prevention of bone metastases in patients with high-risk nonmetastatic prostate cancer treated with zoledronic acid: efficacy and safety results of the Zometa European Study (ZEUS) Eur Urol. 2015;67:482–91. doi: 10.1016/j.eururo.2014.02.014. [DOI] [PubMed] [Google Scholar]
- 19.Tombal B, Jassem J, Shreeve SM, et al. SPARTAN - a randomized double-blind, comparative study of ARN-509 plus androgen deprivation therapy (ADT) vs ADT alone in nonmetastatic castration-resistant prostate cancer (M0-CRPC) [abstract 806TiP]. Paper presented at: European Society for Medical Oncology (ESMO) Annual Congress; September 26–30, 2014; Madrid, Spain. [Google Scholar]
- 20.Sternberg CN, Fizazi K, Saad F, et al. PROSPER: A phase 3 study of enzalutamide in non-metastatic (M0) castration-resistant prostate cancer (CRPC) patients [abstract 802TiP]. Paper presented at: European Society for Medical Oncology (ESMO) Annual Congress; September 26–30, 2014; Madrid, Spain. [Google Scholar]
- 21.Efficacy and safety study of ODM-201 in men with high-risk non-metastatic castration-resistant prostate cancer (ARAMIS) ClinicalTrials.gov. Web site. https://clinicaltrials.gov/ct2/show/NCT02200614. Accessed April 15, 2015.


