Abstract
Purpose of Review
Esophageal high-resolution manometry (HRM) is the current state-of-the-art diagnostic tool to evaluate esophageal motility patterns and, as such, is widely adopted in clinical practice. This paper will review the interpretation of esophageal HRM in clinical practice.
Recent Findings
HRM uses a high-resolution catheter to transmit intraluminal pressure data that is subsequently converted into dynamic esophageal pressure topography plots. Metric data from esophageal pressure topography plots is synthesized to yield an esophageal motility diagnosis according to the Chicago Classification, a formal analytic scheme for esophageal motility disorders, which is currently in version 3.0.
The standard HRM protocol consists of a baseline phase and a series of ten wet swallows in the supine position. Additionally, data from swallows in the seated position and provocative HRM maneuvers provide useful information about motility properties. Combined high-resolution impedance technology is also clinically available and enables concurrent assessment of bolus transit and post-prandial responses. Finally, there is ongoing interest to optimize the training and competency assessment for interpretation of HRM in clinical practice.
Summary
Esophageal HRM is a valuable and sophisticated clinical tool to evaluate esophageal motility patterns. Emerging clinical applications of esophageal HRM include combined impedance technology, provocative maneuvers, and post-prandial evaluation.
Keywords: Esophageal motility, Chicago Classification, Impedance Manometry
Introduction
Advances in high resolution manometry (HRM) with esophageal pressure topography (EPT) have revolutionized the clinical evaluation of esophageal motility disorders. 1
Esophageal manometry assesses esophageal motility patterns by measuring the amplitude of contractile events in the esophagus and its sphincters in relation to time. Pressure sensors along the length of a manometry catheter transmit intraluminal esophageal pressure signals to a receiving device in which data is recorded and displayed. Indications for esophageal manometry include evaluation of non-obstructive dysphagia, peristaltic reserve prior to anti-reflux surgery, symptoms of regurgitation and non-cardiac chest pain, and transit symptoms following foregut intervention. 1
HRM represents an evolution from conventional line tracings. HRM incorporates up to 36 pressure sensors spaced 1cm apart along a catheter, as opposed to the conventional manometry catheter with few (typically 3 to 5) widely-spaced sensors. In contrast to the unidirectional conventional line plots, HRM data is converted into seamless and dynamic spatiotemporal EPT plots by advanced software algorithms (Figures 1 & 2). 2, 3 In response to advances in HRM, the International HRM Working Group proposed a new classification scheme of esophageal motility disorders based on HRM metrics in 2009, known as the Chicago Classification. 4, 5 The Chicago Classification is currently in version 3.0 ,and represents the standard interpretation scheme used in clinical practice. 6 Studies comparing conventional line tracing and HRM report improved diagnostic accuracy, ease of interpretation and better inter-rater agreement with HRM. 7–9 In addition, software programs are able to auto-generate analyses according to HRM metrics. Consequently, esophageal HRM has emerged not only as a research tool, but as a widely adopted and indispensable clinical tool. Despite the aforementioned advances in HRM, auto-generated analyses can result in misdiagnosis, and a high quality interpretation of esophageal manometry requires a nuanced understanding of esophageal physiology and competency in interpretation skills. 10
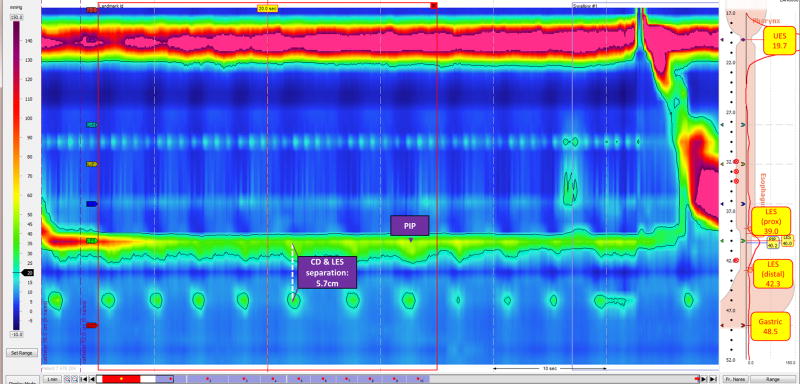
Figure 1. Baseline Period.
In high-resolution manometry with esophageal pressure topography, pressure is assessed in relation to time and distance. Pressure is displayed as a heat map with dark blue representing lower pressures and higher pressures colored red to purple. The horizontal axis represents time. In this window, time is displayed in 10 second intervals; zooming in or out will change the time interval. The vertical axis represents distance and each black circle corresponds to a pressure sensor. In this window distance is portrayed as cm from the nares; clicking on ‘Fr. Nares’ can change the display to represent cm from the lower esophageal sphincter (LES) or sensor number.
In this window, the interpreter is clicked into the baseline period, as represented by the red frame. There are two high-pressure zones corresponding to the upper esophageal sphincter (UES) and lower esophageal sphincter (LES). As depicted by the yellow boxes, the corresponding markers are positioned to reflect UES and LES (proximal and distal border). In addition, the gastric marker is positioned at least 2cm below the distal border of the LES and in this particular case is positioned distal to the hiatus hernia. The pressure inversion point (PIP) is identified (purple box labeled PIP). The separation between the crural diaphragm (CD) and the LES is assessed; in this case, it is estimated at 5.7 cm consistent with a type III esophagogastric junction morphology. (Esophageal pressure topography plot reproduced with permission from the Esophageal Center at Northwestern Medicine Digestive Health Center.)
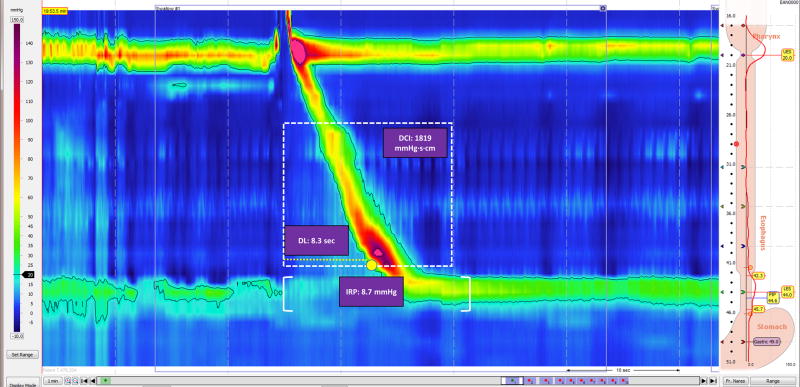
Figure 2. Swallow Phase.
In this high-resolution manometry esophageal pressure topography plot, the interpreter is viewing swallow #1. The swallow begins with the relaxation of the upper esophageal sphincter (UES) and deglutitive relaxation of the lower esophageal sphincter (LES) with aboral contraction along the length of the esophagus and restoration of the baseline LES pressure. The yellow circle corresponds to the contractile deceleration point (CDP). The distal contractile integral (DCI) measures the contractile vigor along time and the distance spanning the transition zone and proximal border of the LES. The distal latency (DL) measures the time interval from UES relaxation to CDP, represented by the yellow dashed line. The integrated relaxation pressure (IRP) corresponds to the lowest mean 4 seconds of axial pressure from onset of UES relaxation. In this example the DCI is normal (between 450 to 8,000 mmHg·s·cm), the DL is normal (greater than 4.5s), and the IRP is normal (less than 15mmHg using the Sierra system).
HRM Protocol
A technically adequate HRM procedure is essential to HRM interpretation. 10 During the HRM procedure, the HRM catheter is placed transnasally and positioned to ideally span the length of the esophagus, with the distal sensor positioned two to three centimeters below the diaphragm. A standard HRM protocol consists of a baseline quiescent period lasting at least 30 seconds, followed by a series of ten 5-mL, room temperature water swallows in the supine or reclined position. 10, 11 While the Chicago Classification v3.0 is based on normative data in the supine position,6 HRM may be performed in the reclined or seated position, which in certain scenarios is a preferred, safer, and more informative protocol. Despite high concordance for motility diagnosis between positions, peristaltic and esophagogastric junction (EGJ) pressures are lower in the seated position; as such, the procedure report should document patient position. 11–14 Although Chicago Classification v3.0 is based on 10 water swallows, studies demonstrate that interpretation based on fewer swallows does not compromise the diagnosis; thus, an expert panel agreed that a high quality exam require a minimum of seven wet swallows. 15
Interpretation of Esophageal HRM
Interpretation of an esophageal HRM study requires interaction with software-generated EPT plots in order to examine manometric properties during the baseline period and each swallow, and synthesize these data to produce an esophageal motility diagnosis.
Baseline Assessment
Within the baseline window, the interpreter will position baseline landmarks, examine upper esophageal sphincter (UES) characteristics and basal EGJ pressures, identify the pressure inversion point (PIP), and assess EGJ morphology (Figure 1) in order to gather important information regarding anatomic profiles and resting pressures. 1, 11
The PIP indicates the point of transition from the intraabdominal cavity to the intrathoracic cavity, and is manometrically displayed by an inverse directionality of the intraabdominal and intrathoracic pressure signals which magnifies with deep inspiration. The PIP is absent in cases where the manometry catheter does not traverse the lower esophageal sphincter (LES). Additionally, cases of a looped catheter in the esophageal body may manifest as a “butterfly” or mirror image. Assessment and documentation of the PIP is essential to HRM interpretation as the absence of the PIP indicates a technically inadequate study. 1
An added value of HRM is the ability to assess the spatial relationship between the crural diaphragm and LES, referred to as the EGJ morphology. According to the Chicago Classification v3.0, there are three EGJ morphology type: type I indicates absence of hiatal hernia, type II indicates a small hernia and type III indicates a hiatal hernia greater than 2cm and is further classified as type IIIa and IIIb based on PIP location. 6
Swallow Assessment
Motility patterns during swallows provide valuable information about esophageal contractility and sphincter relaxation in response to bolus. Diagnosis of an esophageal motility disorder requires assessment of the integrated relaxation pressure (IRP), contractile function, and pressurization (Figure 2).
Integrated Relaxation Pressure
The IRP is the most discriminatory HRM metric according to the Chicago Classification. The IRP is a measure of deglutitive relaxation based on four seconds of the lowest mean axial pressure, continuous or discontinuous, across the LES during the 10-second period after a swallow. An abnormal IRP indicates abnormal transit across the EGJ. 16 According to the Chicago Classification v3.0, the overall IRP is expressed as the median IRP of ten wet swallows. 4, 5 The reported range for normal IRPs differs across manometric systems. With the Sierra system (Sierra Scientific Instruments [of Given Imaging], Los Angeles California) IRP values above 15mmHg indicate an EGJ outflow obstruction. However, in the setting of absent peristalsis, an IRP cutoff of 10mmHg may indicate type I achalasia. In addition, absent peristalsis with at least 20% of swallows with panesophageal pressurization should raise suspicion for type II achalasia regardless of IRP. 17 Thus, the IRP is an important metric to assess adequacy of EGJ relaxation, however IRP values vary with different patterns of contractility and among manufacturers.
Contractile Function
HRM assessment of esophageal contractile function is based on the distal contractile integral (DCI), distal latency (DL) and peristaltic integrity. The DCI measures the vigor of peristalsis in the smooth muscle esophagus. The DCI is determined by summing pressures exceeding 20mmHg within the time/length field spanning the smooth muscle transition zone to the proximal aspect of the EGJ. DCI values are calculated as units of mmHg·s·cm. According to Chicago Classification v3.0, a DCI greater than 8,000 mmHg·s·cm indicates hypercontractility, whereas DCI values below 450 mmHg·s·cm signify weak peristalsis, with values below 100 mmHg·s·cm representing a failed swallow. DCI values between 450 to 8000 mmHg·s·cm are within normal range, though values at the upper limit of normal (5,000 to 8,000 mmHg·s·cm) may indicate a degree of increased contractile vigor. 6, 18 Latency and peristaltic integrity should only be assessed in the context of DCI values above 450 mmHg·s·cm.
The DL is a time measurement from the start of swallow-induced UES opening to arrival of esophageal contraction at the contractile deceleration point, the inflection point in the wavefront velocity proximal to the EGJ. A swallow is considered premature or spastic if the DL is less than 4.5 seconds. 6,19 Borderline normal DL values (e.g., 4.5 to 5.5 seconds) may indicate a spastic disorder in evolution.
Peristaltic integrity is evaluated by the presence of spatial breaks or gaps in the peristaltic contraction across the UES to the EGJ under a 20mmHg isobaric contour. According to Chicago Classification v3.0, breaks longer than 5cm indicate a fragmented swallow. 6
Esophageal Pressurization
An added advantage of HRM is the ability to assess intrabolus pressurization patterns. Esophageal pressurization occurs when swallowed liquid is trapped between two contracting segments of the esophagus, and is abnormal when pressurization exceeds 30mmHg. Pressurization spanning the UES to the EGJ is considered panesophageal pressurization, and is the defining feature of type II achalasia. Compartmentalized pressurization extending from the contractile deceleration point to the EGJ may indicate a distal outflow obstruction. EGJ pressurization spanning the zone between the LES and crural diaphragm may be encountered with a hiatal hernia. 6
Diagnosing an Esophageal Motility Pattern
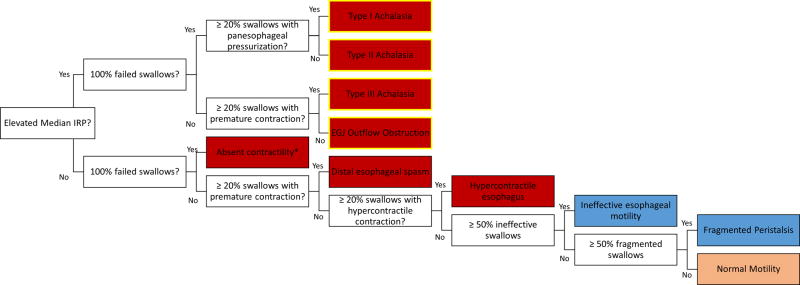
The Chicago Classification v3.0 is a hierarchical analytic scheme used to determine an esophageal motility diagnosis (Table 1, Figure 3). The initial decision point begins with identification of an EGJ outflow obstruction on the basis of an elevated median IRP (>15mmHg using the Sierra system). 6 EGJ outflow obstructive disorders are further classified based on contractile and pressurization patterns. Type I achalasia manifests absent contractility without panesophageal pressurization. In contrast, when EGJ outflow obstruction is present but there is panesophageal pressurization in at least 20% of swallows, type II achalasia is diagnosed; type II achalasia is associated with the greatest likelihood of response to treatment. Finally, in type III or spastic achalasia, contractility is present with at least 20% of swallows being premature. Historically, spastic achalasia was felt to be the least likely to respond to treatment; however, a recent metanalysis reports a 92% response to extended peroral endoscopic myotomy (POEM). 20 Cases of an increased median IRP that do not meet criteria for the three achalasia subtypes are termed EGJ outflow obstruction (EGJOO). 6
Table 1. Defintion of HRM Metrics.
High resolution manometry metrics form the basis of the Chicago Classification.
| Assessment | Metric | Classification | Definition |
|---|---|---|---|
| Contractile Vigor | Distal Contractile Integral |
|
|
| Latency Interval | Distal latency* |
|
|
| Peristaltic Integrity | Peristaltic break in 20mmHg isobaric contour* |
|
|
| Pressurization pattern | Pressurization in 30mmHg isobaric contour |
|
|
Note that a swallow is ineffective if either failed or weak.
A distal contractile integral > 450 mmHg·s·cm is required for assessment of distal latency and peristaltic integrity.
Esophagogastric junction (EGJ); Upper esophageal sphincter (UES); Crural diaphragm (CD); Lower esophageal sphincter (LES).
Figure 3. Hierarchical interpretation scheme according to the Chicago Classification version 3.0.
The colored boxes correspond to 10 esophageal motility patterns per the Chicago Classification v3.0. The red boxes denote the major motility disorders, with those outlined in yellow representing disorders with an esophagogastric junction outflow obstruction. The blue boxes correspond to the minor motility disorders. Integrated relaxation pressure (IRP); Esophagogastric junction (EGJ).
Alternatively, abnormal esophageal motility patterns may be observed without EGJ outflow obstruction (i.e. with normal median IRP). These disorders include absent contractility, distal esophageal spasm, hypercontractile esophagus, and minor motility disorders of ineffective esophageal motility and fragmented peristalsis. A diagnosis of absent contractility is made when 100% of the observed swallows are failed. In distal esophageal spasm, at least 20% of swallows are premature contractions; 6 of note, opiate use may generate spastic motility patterns. 6, 21 In hypercontractile, or Jackhammer esophagus, at least 20% of swallows are hypercontractile. 6 Though hypercontractile swallows manifest as single- or multi-peaked contractions, the clinical relevance of these contraction types is unclear. 22
In contrast to major motility disorders, minor motility disorders may be observed in healthy volunteers and carry a better prognosis. 23 Ineffective esophageal motility is diagnosed when more than 50% of swallows are ineffective (DCI <450 mmHg·s·cm), not meeting criteria for absent contractility. Ineffective esophageal motility indicates poor bolus transit in the distal esophagus, and is found in nearly 50% of patients with GERD. 24 Fragmented peristalsis indicates the presence of clinically important breaks, which are more common in patients with dysphagia than in controls. In fragmented peristalsis, at least 50% of contractions are fragmented (i.e. breaks in the 20 mmHg isobaric contour are >5 cm) and do not meet criteria for ineffective esophageal motility (i.e. DCI is >450 mmHg·s·cm). 6 Although all disorders with an elevated median IRP (e.g., achalasia subtypes I, II and III, and EGJOO) are considered major motility disorders, the clinical relevance of EGJOO is variable, and further studies are needed to clarify whether EGJOO represents a major or minor motility disorder.
Documented Interpretation of Esophageal HRM
According to quality measures for esophageal manometry, six key components are essential in an HRM procedure report: indication for study, motility diagnosis accompanied by classification scheme used for interpretation, summary of results, tabulated results, technical limitations if applicable, and ensuring communication of results to referring provider. 10 (Table 2).
Table 2. Recommended toolkit for step-by-step interpretation of esophageal high-resolution manometry.
| Toolkit for the Clinical Interpretation of Esophageal High Resolution Manometry | |
|---|---|
| First Steps |
|
| Baseline Phase |
|
| Individual Swallow |
|
| Synthesize the Information |
|
| Documentation | Include the following information in an esophageal manometry procedure report
|
| Optional Applications |
|
Integrated relaxation pressure (IRP); Esophagogastric junction (EGJ); Upper esophageal sphincter (UES); Crural diaphragm (CD); Lower esophageal sphincter (LES); Contractile deceleration point (CDP); Distal contractile integral (DCI); Distal latency (DL).
HRM Interpretation Beyond the Standard Esophageal HRM Protocol
Esophageal HRM has replaced conventional manometry systems as the standard diagnostic tool in the evaluation of non-obstructive esophageal motility disorders. In addition, HRM is emerging as a useful clinical tool to understand distinct properties of esophageal motility, and to characterize GERD and pharyngeal mechanisms.
Provocative Measures
Provocative measures might provide useful clinical information beyond that provided by standard HRM protocols. In addition to the traditional wet swallows, viscous and solid boluses are used with increased diagnostic yield for obstructive processes. Multiple rapid swallows (five 2-mL water swallows less than 3 seconds apart) and rapid water bolus (200 mL water within 30 seconds) both rely on intact deglutitive inhibition during swallows with a robust contractile response following the last swallow as a marker of peristaltic reserve. 25, 26 Peristaltic reserve is reportedly impaired in non-erosive reflux disease, systemic sclerosis, and postoperative dysphagia following antireflux surgery, and additionally distinguishes between achalasia subtypes. 26–28 Rapid water boluses may additionally induce esophageal pressurization in the setting of subtle outflow obstruction. 29
Esophageal High-Resolution Impedance Manometry
High-resolution impedance manometry (HRIM) catheters embed impedance sensors between high-resolution circumferential pressure sensors, enabling concurrent assessment of bolus transit in relation to manometric changes. 30 HRIM metrics examining bolus transit include the esophageal impedance integral as a surrogate for bolus retention 31, intrabolus pressure as a marker of esophageal wall state during bolus transit 32, and bolus flow time as a measurement of trans-EGJ pressure gradients during flow. 33, 34 Post-prandial HRIM also provides valuable information about manometric responses to digestive stimuli such as transient LES relaxation episodes, rumination syndrome, and belching disorders. 35–37
GERD and Pharyngeal Mechanisms
There are ongoing efforts to develop HRM metrics related to structural and motor functions relevant to mechanisms of GERD. For instance, the EGJ Contractile Index is an HRM metric assessing integrity of the EGJ barrier function and predicts response to anti-reflux surgery. 38, 39 In addition, HRM is increasingly used as a part of the speech language pathologist’s armamentarium to evaluate oropharyngeal dysphagia. 40
Quality of HRM Interpretation
HRM is a complex tool, and the interpretation of HRM guides important clinical decisions such as the indication for and potential response to surgery. As such, it is requisite that gastroenterologists interpreting HRM in unsupervised practice are sufficiently trained and demonstrate adequate levels of competency. Unfortunately, only a minority of US training programs provide formal esophageal motility training, and gastroenterology practices are not equipped to measure interpreter quality. 10, 41–43 In order to assure high quality esophageal HRM interpretation, the development of methods to provide standardized training and competency assessment is a current priority. 10, 44
Conclusion
HRM is a sophisticated diagnostic tool to assess esophageal motility patterns, and has been widely adopted into clinical practice. Interpretation of esophageal HRM requires careful assessment of the baseline phase and each swallow, and synthesis of findings towards a motility diagnosis. Ongoing research and future clinical applications of HRM include impedance metrics to further evaluate bolus transit and post-prandial mechanisms, provocative measures to delineate subtle esophageal abnormalities, and the role of HRM in characterizing GERD and oropharyngeal dysphagia. A current priority is to develop training and competency assessment methods for the interpretation of HRM.
Key Points.
High-resolution manometry with esophageal pressure topography is a sophisticated diagnostic tool to assess esophageal motility. Application of the Chicago Classification to high-resolution manometry metrics generates diagnoses of esophageal motility disorders.
Interpretation of esophageal high-resolution manometry involves interaction with the software system to assess the baseline period for anatomic landmarks, pressure inversion point and esophagogastric junction morphology and to examine individual swallow properties of deglutitive lower esophageal sphincter relaxation, contractile function and pattern, and pressurization.
Newer applications of esophageal high-resolution manometry include provocative measures during study protocol, the addition of combined impedance monitoring, and exploration of other esophageal pathophysiology such as gastroesophageal reflux disease and oropharyngeal dysphagia.
Ensuring adequate training and competency of physicians who interpret esophageal high-resolution manometric studies is a priority issue.
Acknowledgments
None
Financial support and sponsorship: RY: Supported by NIH T32DK101363
Abbreviations
- CDP
Contractile deceleration point
- DCI
Distal contractile integral
- DL
Distal latency
- EGJ
Esophagogastric junction
- EPT
Esophageal pressure topography
- HRIM
High resolution impedance manometry
- HRM
High resolution manometry
- IRP
Integrated relaxation pressure
- LES
Lower esophageal sphincter
- PIP
Pressure inversion point
- UES
Upper esophageal sphincter
- v3.0
Version 3.0
Footnotes
Author Contributions:
RY: Literature review, drafting of manuscript, critical revision of manuscript, finalization of manuscript.
Conflicts of interest: None
References
- 1.Gyawali CP, Patel A. Esophageal motor function: technical aspects of manometry. Gastrointest Endosc Clin N Am. 2014;24:527–43. doi: 10.1016/j.giec.2014.06.003. [DOI] [PubMed] [Google Scholar]
- 2.Gyawali CP, Bredenoord AJ, Conklin JL, et al. Evaluation of esophageal motor function in clinical practice. Neurogastroenterol Motil. 2013;25:99–133. doi: 10.1111/nmo.12071. [DOI] [PubMed] [Google Scholar]
- 3.Clouse RE, Prakash C. Topographic esophageal manometry: an emerging clinical and investigative approach. Dig Dis. 2000;18:64–74. doi: 10.1159/000016967. [DOI] [PubMed] [Google Scholar]
- 4.Kahrilas PJ, Ghosh SK, Pandolfino JE. Esophageal motility disorders in terms of pressure topography: the Chicago Classification. J Clin Gastroenterol. 2008;42:627–35. doi: 10.1097/MCG.0b013e31815ea291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Roman S, Gyawali CP, Xiao Y, Pandolfino JE, Kahrilas PJ. The Chicago classification of motility disorders: an update. Gastrointest Endosc Clin N Am. 2014;24:545–61. doi: 10.1016/j.giec.2014.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6**.Kahrilas PJ, Bredenoord AJ, Fox M, et al. The Chicago Classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil. 2015;27:160–74. doi: 10.1111/nmo.12477. Chicago Classification version 3.0 is the most recently updated version of the Chicago Classification, the analytic scheme for esophageal motility disorders based on high-resolution manometry. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Soudagar AS, Sayuk GS, Gyawali CP. Learners favour high resolution oesophageal manometry with better diagnostic accuracy over conventional line tracings. Gut. 2012;61:798–803. doi: 10.1136/gutjnl-2011-301145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8**.Carlson DA, Ravi K, Kahrilas PJ, et al. Diagnosis of Esophageal Motility Disorders: Esophageal Pressure Topography vs. Conventional Line Tracing. Am J Gastroenterol. 2015;110:967–77. doi: 10.1038/ajg.2015.159. quiz 78. Interpreter agreement and diagnostic accuracy is higher with high-resolution manometry compared to conventional manometry. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9**.Roman S, Huot L, Zerbib F, et al. High-Resolution Manometry Improves the Diagnosis of Esophageal Motility Disorders in Patients With Dysphagia: A Randomized Multicenter Study. Am J Gastroenterol. 2016;111:372–80. doi: 10.1038/ajg.2016.1. Diagnostic yield is improved with high-resolution manometry compared to conventional manometry. [DOI] [PubMed] [Google Scholar]
- 10**.Yadlapati R, Gawron AJ, Keswani RN, et al. Identification of Quality Measures for Performance of and Interpretation of Data From Esophageal Manometry. Clin Gastroenterol Hepatol. 2016;14:526–34. e1. doi: 10.1016/j.cgh.2015.10.006. Quality measures developed for esophageal manometry based on a national expert based RAND UCLA Appropriateness Method. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11*.Patel A, Ding A, Mirza F, Gyawali CP. Optimizing the high-resolution manometry (HRM) study protocol. Neurogastroenterol Motil. 2015;27:300–4. doi: 10.1111/nmo.12494. The baseline landmark phase can be obtained at the end of the study, and may optimize study duration wtihout compromising quality of the study. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sweis R, Anggiansah A, Wong T, Kaufman E, Obrecht S, Fox M. Normative values and inter-observer agreement for liquid and solid bolus swallows in upright and supine positions as assessed by esophageal high-resolution manometry. Neurogastroenterol Motil. 2011;23 doi: 10.1111/j.1365-2982.2011.01682.x. 509-e198. [DOI] [PubMed] [Google Scholar]
- 13.Roman S, Damon H, Pellissier PE, Mion F. Does body position modify the results of oesophageal high resolution manometry? Neurogastroenterol Motil. 2010;22:271–5. doi: 10.1111/j.1365-2982.2009.01416.x. [DOI] [PubMed] [Google Scholar]
- 14.Xiao Y, Read A, Nicodeme F, Roman S, Kahrilas PJ, Pandolfino JE. The effect of a sitting vs supine posture on normative esophageal pressure topography metrics and Chicago Classification diagnosis of esophageal motility disorders. Neurogastroenterol Motil. 2012;24:e509–16. doi: 10.1111/j.1365-2982.2012.02001.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Roman S, Kahrilas PJ, Boris L, Bidari K, Luger D, Pandolfino JE. High-resolution manometry studies are frequently imperfect but usually still interpretable. Clin Gastroenterol Hepatol. 2011;9:1050–5. doi: 10.1016/j.cgh.2011.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ghosh SK, Pandolfino JE, Rice J, Clarke JO, Kwiatek M, Kahrilas PJ. Impaired deglutitive EGJ relaxation in clinical esophageal manometry: a quantitative analysis of 400 patients and 75 controls. Am J Physiol Gastrointest Liver Physiol. 2007;293:G878–85. doi: 10.1152/ajpgi.00252.2007. [DOI] [PubMed] [Google Scholar]
- 17.Lin Z, Kahrilas PJ, Roman S, Boris L, Carlson D, Pandolfino JE. Refining the criterion for an abnormal Integrated Relaxation Pressure in esophageal pressure topography based on the pattern of esophageal contractility using a classification and regression tree model. Neurogastroenterol Motil. 2012;24:e356–63. doi: 10.1111/j.1365-2982.2012.01952.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ghosh SK, Pandolfino JE, Zhang Q, Jarosz A, Shah N, Kahrilas PJ. Quantifying esophageal peristalsis with high-resolution manometry: a study of 75 asymptomatic volunteers. Am J Physiol Gastrointest Liver Physiol. 2006;290:G988–97. doi: 10.1152/ajpgi.00510.2005. [DOI] [PubMed] [Google Scholar]
- 19.Roman S, Lin Z, Pandolfino JE, Kahrilas PJ. Distal contraction latency: a measure of propagation velocity optimized for esophageal pressure topography studies. Am J Gastroenterol. 2011;106:443–51. doi: 10.1038/ajg.2010.414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20*.Khan MA, Kumbhari V, Ngamruengphong S, et al. Is POEM the Answer for Management of Spastic Esophageal Disorders? A Systematic Review and Meta-Analysis. Dig Dis Sci. 2017;62:35–44. doi: 10.1007/s10620-016-4373-1. Extended peroral endoscopic myotomy may yield better prognosis for spastic achalasia than previously considered. [DOI] [PubMed] [Google Scholar]
- 21*.Roman S, Kahrilas PJ. Distal esophageal spasm. Curr Opin Gastroenterol. 2015;31:328–33. doi: 10.1097/MOG.0000000000000187. Review on the current state of distal esophageal spasm. [DOI] [PubMed] [Google Scholar]
- 22*.Herregods TV, Smout AJ, Ooi JL, Sifrim D, Bredenoord AJ. Jackhammer esophagus: Observations on a European cohort. Neurogastroenterol Motil. 2016 doi: 10.1111/nmo.12975. Explores the significance of single-peaked versus multi-peaked hypercontractile contractions. [DOI] [PubMed] [Google Scholar]
- 23**.Ravi K, Friesen L, Issaka R, Kahrilas PJ, Pandolfino JE. Long-term Outcomes of Patients With Normal or Minor Motor Function Abnormalities Detected by High-resolution Esophageal Manometry. Clin Gastroenterol Hepatol. 2015;13:1416–23. doi: 10.1016/j.cgh.2015.02.046. A minor motility disorder may portend better prognosis compared to a major motility disorder. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24*.Abdel Jalil AA, Castell DO. Ineffective Esophageal Motility (IEM): the Old-New Frontier in Esophagology. Curr Gastroenterol Rep. 2016;18:1. doi: 10.1007/s11894-015-0472-y. An update on ineffective esophageal motility. [DOI] [PubMed] [Google Scholar]
- 25.Shaker A, Stoikes N, Drapekin J, Kushnir V, Brunt LM, Gyawali CP. Multiple rapid swallow responses during esophageal high-resolution manometry reflect esophageal body peristaltic reserve. Am J Gastroenterol. 2013;108:1706–12. doi: 10.1038/ajg.2013.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stoikes N, Drapekin J, Kushnir V, Shaker A, Brunt LM, Gyawali CP. The value of multiple rapid swallows during preoperative esophageal manometry before laparoscopic antireflux surgery. Surg Endosc. 2012;26:3401–7. doi: 10.1007/s00464-012-2350-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27*.Carlson DA, Crowell MD, Kimmel JN, et al. Loss of Peristaltic Reserve, Determined by Multiple Rapid Swallows, Is the Most Frequent Esophageal Motility Abnormality in Patients With Systemic Sclerosis. Clin Gastroenterol Hepatol. 2016;14:1502–6. doi: 10.1016/j.cgh.2016.03.039. Multiple rapid swallows demonstrated poor peristaltic reserve in patients with systemic sclerosis. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28*.Martinucci I, Savarino EV, Pandolfino JE, et al. Vigor of peristalsis during multiple rapid swallows is inversely correlated with acid exposure time in patients with NERD. Neurogastroenterol Motil. 2016;28:243–50. doi: 10.1111/nmo.12719. Peristaltic reserve measured by multiple rapid swallow is inversely correlated with acid exposure time on ph-impedance in a study comparing positive and negative pH-impedance studies. [DOI] [PubMed] [Google Scholar]
- 29**.Marin I, Serra J. Patterns of esophageal pressure responses to a rapid drink challenge test in patients with esophageal motility disorders. Neurogastroenterol Motil. 2016;28:543–53. doi: 10.1111/nmo.12749. Rapid water bolus or drink challenge identified patterns that distinguish healty subjects and hypocontractile peristalsis, non-obstructive hypercontractile motility, or achalasia. [DOI] [PubMed] [Google Scholar]
- 30**.Patel A, Gyawali CP. How to Optimally Apply Impedance in the Evaluation of Esophageal Dysmotility. Curr Gastroenterol Rep. 2016;18:60. doi: 10.1007/s11894-016-0534-9. A review on the role of impedance in esophageal motility testing. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lin Z, Nicodeme F, Lin CY, et al. Parameters for quantifying bolus retention with high-resolution impedance manometry. Neurogastroenterol Motil. 2014;26:929–36. doi: 10.1111/nmo.12346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lin Z, Yim B, Gawron A, Imam H, Kahrilas PJ, Pandolfino JE. The four phases of esophageal bolus transit defined by high-resolution impedance manometry and fluoroscopy. Am J Physiol Gastrointest Liver Physiol. 2014;307:G437–44. doi: 10.1152/ajpgi.00148.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lin Z, Imam H, Nicodeme F, et al. Flow time through esophagogastric junction derived during high-resolution impedance-manometry studies: a novel parameter for assessing esophageal bolus transit. Am J Physiol Gastrointest Liver Physiol. 2014;307:G158–63. doi: 10.1152/ajpgi.00119.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34*.Carlson DA, Lin Z, Kahrilas PJ, et al. High-Resolution Impedance Manometry Metrics of the Esophagogastric Junction for the Assessment of Treatment Response in Achalasia. Am J Gastroenterol. 2016;111:1702–10. doi: 10.1038/ajg.2016.442. The bolus flow time provides important information in the follow-up of achalasia treatment. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35**.Roman S, Holloway R, Keller J, et al. Validation of criteria for the definition of transient lower esophageal sphincter relaxations using high-resolution manometry. Neurogastroenterol Motil. 2016 doi: 10.1111/nmo.12920. Definition of transient lower esophageal sphincter relaxations based on high-resolution impedance manometry. [DOI] [PubMed] [Google Scholar]
- 36.Kessing BF, Bredenoord AJ, Smout AJ. Objective manometric criteria for the rumination syndrome. Am J Gastroenterol. 2014;109:52–9. doi: 10.1038/ajg.2013.428. [DOI] [PubMed] [Google Scholar]
- 37.Kessing BF, Bredenoord AJ, Smout AJ. The pathophysiology, diagnosis and treatment of excessive belching symptoms. Am J Gastroenterol. 2014;109:1196–203. doi: 10.1038/ajg.2014.165. (Quiz) 204. [DOI] [PubMed] [Google Scholar]
- 38**.Wang D, Patel A, Mello M, Shriver A, Gyawali CP. Esophagogastric junction contractile integral (EGJ-CI) quantifies changes in EGJ barrier function with surgical intervention. Neurogastroenterol Motil. 2016;28:639–46. doi: 10.1111/nmo.12757. The esophagogastric junction contractile integral provides a quantified assessment of the esophagogastric junction barrier function before and after surgical intervention. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nicodeme F, Pipa-Muniz M, Khanna K, Kahrilas PJ, Pandolfino JE. Quantifying esophagogastric junction contractility with a novel HRM topographic metric, the EGJ-Contractile Integral: normative values and preliminary evaluation in PPI non-responders. Neurogastroenterol Motil. 2014;26:353–60. doi: 10.1111/nmo.12267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Knigge MA, Thibeault S, McCulloch TM. Implementation of high-resolution manometry in the clinical practice of speech language pathology. Dysphagia. 2014;29:2–16. doi: 10.1007/s00455-013-9494-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41**.Rao SS, Parkman HP. Advanced training in neurogastroenterology and gastrointestinal motility. Gastroenterology. 2015;148:881–5. doi: 10.1053/j.gastro.2015.03.026. Few training programs incorporate formal motility curriculum. [DOI] [PubMed] [Google Scholar]
- 42*.Yadlapati R, Keswani RN, Pandolfino JE. Competency based medical education in gastrointestinal motility. Neurogastroenterol Motil. 2016;28:1460–4. doi: 10.1111/nmo.12835. A review on the current state of competency based training and assessment in gastrointestinal motility. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43**.Yadlapati R, Keswani RN, Ciolino JD, et al. A System to Assess the Competency for Interpretation of Esophageal Manometry Identifies Variation in Learning Curves. Clin Gastroenterol Hepatol. 2016 doi: 10.1016/j.cgh.2016.07.024. Learning curves for the interpretation of high resolution manometry vary by learner and a minority demonstrate competency after interpreting 50 cases. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44*.Yadlapati R, Keswani RN, Dunbar KB, et al. Benchmarks for the interpretation of esophageal high-resolution manometry. Neurogastroenterol Motil. 2016 doi: 10.1111/nmo.12971. A national consensus process determined minimal competency benchmarks for the interpretation of high-resolution manometry by interpreter type. [DOI] [PMC free article] [PubMed] [Google Scholar]