Abstract
Background
Identification of risk factors for lower extremity (LE) injury in sport and military/first-responder occupations is required to inform injury prevention strategies.
Objective
To determine if poor movement quality is associated with LE injury in sport and military/first-responder occupations.
Material and methods
Five electronic databases were systematically searched. Studies selected included: original data; analytic design; movement quality outcome (qualitative rating of functional compensation, asymmetry, impairment or efficiency of movement control); LE injury sustained with sport or military/first-responder occupation. The PRISMA guidelines were followed. Two independent authors assessed the quality [Downs and Black (DB) criteria] and level of evidence (Oxford Centre of Evidence-Based Medicine model).
Results
Of 4361 potential studies, 17 were included. The majority were low quality cohort studies (level 4 evidence). Median DB score was 11/33 (range 3–15). Heterogeneity in methodology and injury definition precluded meta-analyses. The Functional Movement Screen was the most common outcome investigated (15/17 studies). Four studies considered interrelationships between risk factors, seven reported diagnostic accuracy and none tested an intervention program targeting individuals identified as high-risk. There is inconsistent evidence that poor movement quality is associated with increased risk of LE injury in sport and military/first-responder occupations.
Conclusions
Future research should focus on high quality cohort studies to identify the most relevant movement quality outcomes for predicting injury risk followed by developing and evaluating pre-participation screening and LE injury prevention programs through high quality randomized controlled trials targeting individuals at greater risk of injury based upon screening tests with validated test properties.
Keywords: Athletic Injuries, Lower Extremity, Movement Screening, Occupational Injuries, Risk Factors
BACKGROUND
Due to the increasing prevalence and cost of treating chronic musculoskeletal (MSK) conditions such as hip, knee and ankle osteoarthritis (OA) there has been a call for scientific inquiry focused on shifting the approach taken to manage these conditions away from treatment and toward prevention.1 From an epidemiological perspective prevention of chronic MSK conditions may include strategies aimed at reducing MSK injuries in susceptible populations (primary prevention) and/or strategies aimed at slowing down or halting the onset of the chronic MSK disorder after a MSK injury has occurred (secondary prevention). Susceptible populations for MSK injury include those that participate in sport and recreation, or have a service related occupation (e.g., military and first responders such as police officers, fire fighters and paramedics).2,3 For example epidemiological surveys have shown that the risk of injury is 1.5 to 2.0 times greater amongst individuals that participate in a variety of sporting and physical activities,2 and that MSK injury is the leading cause of disability in the military.4 In both of these at risk populations the most common MSK injuries are those that involve the lower extremities (LE).3
Van Mechelen5 proposed a 4-step model for injury prevention. This model involves establishing the extent of the specific injury burden of interest, followed by identifying injury risk factors and causal mechanisms through prospective analysis. The first two steps inform the development and introduction of preventative strategies (step four), which should then be evaluated to determine their impact on injury burden (step five). Finch et al6 expanded upon this model emphasizing the importance of evaluating the effectiveness of preventative strategies in real-world implementation contexts and Meeuwisse et al7 emphasized the importance of acknowledging that injury is a consequence of complex interactions of multiple risk factors and inciting events. Consequently, studies aimed at identifying risk factors for LE injuries and accompanying preventative strategies should engage end-users, utilize a prospective design and ensure an adequate sample size to facilitate biostatistical methods that consider the interrelationships between various risk factors.8 Further, to establish the value of injury risk screening on injury burden it is crucial that there is an accumulation of high quality evidence indicating that an intervention program targeting those at high risk of injury based on a screening program is more beneficial than a non-targeted intervention.9
Concomitant to injury prevention models is the development of approaches to identify ‘high-risk’ individuals. Identification of these individuals enables prevention programs to be individually targeted, improving their effectiveness and public health impact (e.g., health care cost reduction). One method that is widely used to identify individuals at high-risk of injury are movement screening tests. The value of these tests is that they can be administered on-field or in clinical settings and are less costly than tests that require specialized equipment or highly trained personnel (e.g., laboratory tools such as 3D motion analysis). Additional advantages of movement screening tests are that they can be administered to a large number of individuals, are easily adapted to various sporting or occupation environments and provide almost immediate results. Further, as movement is modifiable, these tests provide information that can directly inform a prevention strategy and possibly assist in return to activity decisions.
Movement screening can involve the assessment of a single movement task or a composite battery of movement tasks. Further, participants can be assessed on their physical performance and/or the quality with which they move. Assessment of physical performance would consider a quantifiable outcome(s) of sport or occupational strength, power, balance, agility etc., often through multi-joint movements (e.g., Triple Single Leg Hop, Y Balance Test).10,11 Conversely, assessment of movement quality involves qualitative identification and rating of functional compensations, asymmetries, impairments or efficiency of movement control through transitional (e.g. squats, sit to stand, lunge) or dynamic movement (e.g. hopping, walking, running, landing, cutting) tasks. Both physical performance and movement quality assessments would ideally align with the sport or occupation specific context. Although there is consensus and several recent high-quality summaries of the clinimetric properties (e.g., validity, reliability and diagnostic accuracy) and evidence related to predicting injury risk and successful return to sport for physical performance outcomes,10,11 the same cannot be said for movement quality outcomes.
As identification of risk factors and casual mechanisms are precursors to the development of effective prevention strategies, the lack of consensus related to movement quality risk factors for LE injury in sport and service occupations has likely hindered the process of developing and evaluating injury prevention strategies. The primary objective of this systematic review is to determine whether screening movement quality (a qualitative rating of functional compensation, asymmetry, impairment or efficiency of movement control either with individual movements tasks or a composite battery of movement tasks) can predict LE injury in sport and/or occupational (e.g., military, first responders) populations of all ages. A secondary objective is to summarize the clinimetric properties of the movement quality screening tests in the identified literature to inform clinicians and future research aimed at the development and use of movement quality screening.
METHODS
This review was registered in the PROSPERO database (CRD42015026958) and conducted according to the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guidelines.12
Data Sources and Search
Relevant studies were identified by searching five online databases, selected based on their relevance to the research topics, from inception to January 2016. These databases included: Medline, EMBASE (Excerpta medical databases), CINAHL (Cumulative Index to Nursing and Allied Health Literature), Sport Discus, and SCOPUS. The combination of medical subject headings (MeSH) and text words that were used to execute each search was developed in consultation with a health sciences librarian scientist (LD). Appendix 1 outlines the search terms used for population, injury type, screening type, screening quality, measurement as well as limits and exclusions, along with combinations of search terms that formed the final search strategy. The search strategy (specifically filters 3 and 4) from Kroman et al13 was heavily used as a source of search terms for screening quality and measurement concepts. Limits included: English language; human and MSK condition studies published in peer-reviewed journal. Articles were organized using the reference management software package, EndNote version 7.1 (Thomson Reuters, 2013). The number of references obtained from each search strategy for each database was recorded and a running total constructed. After accounting for duplication, the titles and corresponding abstracts of all returned records were independently reviewed by two of the authors blinded to record author(s) and journal title using a Microsoft Excel workbook designed specifically for screening.14 Data were compiled and consensus (first between the two reviewers and if required by the lead author) regarding potentially relevant studies was reached on items in which there was disagreement. Prior to title and abstract review all authors independently screened a random sample of 120 titles and abstracts in which they were blinded to authors and journal title and reached strong agreement with the lead author (agreement ranging from 81–97%, Kappa ranging from 0.13–0.49) using an Excel workbook designed specifically for this purpose.14,15 Finally, two authors independently reviewed the full text of all potentially relevant studies to determine final study selection.
Study Selection
Studies were included if they investigated the prospective association between a movement quality outcome (defined as a qualitative rating of functional compensation, asymmetry, impairment or efficiency of movement control during either an individual movement task or battery of movement tasks) and MSK LE injury (defined as an injury involving the hip joint or distal). Additional inclusion criteria included: primary research with original data, analytic or intervention design, an outcome measure of LE injury sustained during sport or military/first-responder occupation participation and an objective exposure measure of one or more potential movement quality risk factor for LE injury. Studies were excluded if they were not written in English or involved animal models or cadavers. Further, conference proceedings or abstracts, editorials, commentaries, opinion-based papers review articles (systematic and narrative), case series, case studies, or studies in which screening did not take place prior to injury onset (e.g., cross-sectional) were excluded.
Data extraction and study rating process
Data extracted from each study included: study year; design; study location and population (e.g., sport, military/first-responder occupation, age, sample size); injury outcome (e.g., definition) and how it was ascertained; injury estimates (e.g., incidence proportion, incidence rate, prevalence); risk factors, and results (e.g., significant and non-significant) including measures of reliability, measures of risk [e.g., difference in means, correlations, odds ratio (OR), incidence rate ratios; IRR and risk ratio (RR)] and diagnostic accuracy (e.g., sensitivity, specificity, negative predictive value, positive predictive value, positive or negative likelihood ratios). Two authors independently assessed the quality and level of evidence of each study. Quality of evidence was evaluated based on criteria for internal validity (study design, quality of reporting, presence of selection and misclassification bias, potential confounding) and external validity (generalizability) using the Downs and Black (DB) quality assessment tool which assigns an individual score calculated out of 32 total points for each study (11 points for reporting, 3 points for external validity, 7 points for bias, 6 points for confounding and 5 for power: Appendix 2)16. The level of evidence represented by each study was categorized based upon the Oxford Centre of Evidence Based Medicine (OCEBM) 2009 model (Appendix 3).17 As per study exclusion criteria, levels 1a, 2a, 3a (systematic reviews), 4 (case series) and 5 (opinion-based papers) were not included. Discrepancies in DB scoring or OCEBM categorization were resolved first by consensus between the two reviewers who rated the study and if required, by the lead author (JW).
Data synthesis
Extracted data, quality and level of evidence were summarized for each study. The quantity, quality and level of evidence for the most commonly investigated movement quality risk factors for LE injury in sport military/first-responder occupation were collated.
RESULTS
Identification of studies
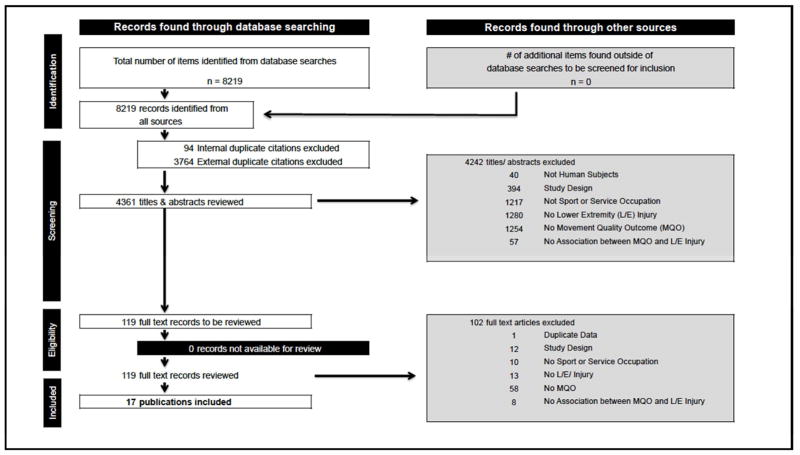
An overview of the study identification process is provided in Figure 1. The initial search yielded 8219 articles, 3858 duplicates were removed leaving 4361 potentially relevant articles. Following the removal of studies not meeting inclusion criteria based on abstract review (e.g., not human studies, ineligible study design, not sport or military/first-responder occupation, no LE injury, no movement quality risk factor, no association between a movement quality risk factor and LE injury) this was reduced to 119. Subsequent to full article evaluation by the two independent reviewers, 102 were excluded leaving 17 studies deemed appropriate for inclusion to the systematic review. Due to inconsistent methodology and injury definition, and heterogeneity of the risk factors examined, meta-analyses was precluded (see Table 1).
Figure 1.
Study identification PRISMA flowsheet
Table 1.
Summary of Data Extracted from Included Studies
| Study Features (author, year, design, country) |
Participants (sport, level, sex, age, sample size) |
Outcome (definition and ascertainment) |
Injury estimate | Exposure (Risk factor(s) |
Reported as significant risk factor(s) |
Reported statistics |
Reported non- significant risk factor(s) |
DB score (/23)^ |
Level of Evidence |
|---|---|---|---|---|---|---|---|---|---|
| Azzam et al., 201518 Historical Cohort United States |
Professional Basketball Players Male = 34 Age = not reported n = 34 (17 injuries) |
Injury = traumatic or overuse MSK event resulting from basketball that led to time loss of ≥7 days from practice and/or games. Ascertained by ATC |
50% of players experienced an injury over the 2008–2011 seasons |
Movement Quality
|
|
|
|
9 | 4 |
| Bardenett et al., 201519 Cohort United States |
High School Athletes (multiple sports) Male = 77 Female = 97 Mean age (range): 15.2 (11–18) n=176 (39 injuries) |
Injury = a MSK injury resulting from organized high school sport practice or competition that required medical attention (sought care from ATC, PT, physician or other health care provider) and was restricted from full participation ≥1 practice or game. Ascertained by ATC |
69.5% of players experienced an injury over the 2012 fall season |
Movement Quality
|
|
|
12 | 4 | |
| Bushman et al., 201520 Cohort United States |
Military Soldiers Male = 2,476 Age range: 18–57 n = 2,476 (916 injuries) |
Injury = all inpatient and outpatient medical encounters for any overuse and traumatic injury found in a soldiers’ electronic medical records with ECD-9_CM diagnostic code determined to be an injury. Overuse injuries ICD-9-CM codes 710–739 Traumatic injuries ICD-9-CM codes 800–999 Ascertained by Defense Medial Surveillance System |
Any injury: 37% Overuse: 28% Traumatic 16% In the 6 months following screening |
Movement Quality
|
Any injury
|
|
12 | 4 | |
| Butler et al., 201321 Cohort United States |
Firefighter trainees Sex = not reported Age: not reported n=108 (number of injuries not reported) |
Injury = any episode that resulted in 3 consecutive missed days of training due to MSK pain Ascertained: Strength and conditioning staff |
No injury estimate was reported for the 16 week training academy |
|
|
SEN: 0.83 SPE: 0.62 PLR: 2.2 NLR: 0.26 |
|
8 | 4 |
| Chorba et al., 201022 Cohort United States |
NCAA Division II collegiate athletes Female = 38 Mean age (SD): 19.2±1.2 n=38 (18 injuries) |
Injury = a MSK injury resulting from organized intercollegiate sport practice or competition that required medical attention or advice from an ATC, AT student or physician. Ascertained: ATC |
47% of players experienced an injury over the 2007–2008 season |
|
|
SPE = 0.74 |
n/a | 9 | 4 |
| Dossa et al., 201431 Cohort Canada |
Junior hockey players Male = 20 Mean age (range): 18.2 (16–20) n=20 (17 injuries) |
Injury = a physical condition which occurred during a game or practice which resulted in the player missing ≥1 game. Contact = involved collision with another body, ice, boards, puck or stick. Non-contact = not a contact injury Ascertained: ATC |
85% of players experienced an injury over the 2013–2014 season (76 games) |
|
n/a | n/a |
SPE: 0.7 (0.3,0.9) PLR: 1.7 (0.6,5.2) NLR: 0.7 (0.2,0.9) |
12 | 4 |
| Garrison et al., 201523 Cohort United States |
NCAA Division I collegiate athletes Sex = not reported Age range: 17–22 n=160 (52 injuries) |
Injury = any MSK pain complaint associated with athletic participation, that required consultation with an ATC, PT or MD and resulted in modified training for ≥24 hours or required protective splinting or taping for continued participation Ascertained: ATC |
32.5% of players experienced an injury over the season |
Movement Quality
|
|
n/a | 8 | 4 | |
| Hotta et al., 201533 Cohort Japan |
Collegiate track and field athletes Male: 84 Mean age (range): 20.0 (18–24) n= 84 (15 injuries) |
Running injury = a MSK injury that occurred during participation in track and field practice or competition that prevented participation for 4 weeks. Ascertained: not reported |
17.9% of runners experienced an injury over a 6 month season |
Movement Quality
|
|
|
14 | 4 | |
| Kiesel et al., 200724 Cohort United States |
Professional American football players Sex = not reported Age = not reported n=46 (13 injuries) |
Injury = on the injury reserve list and a time loss of ≥3 weeks. Ascertained: not reported |
28.3% of players experienced an injury over the season |
|
|
SEN: 0,54 (0.3,0.7) SPE: 0.91 (0.8,0.96) PLR: 5.92 (2.0,18.4) NLR: 0.51 (0.3,0.8) |
n/a | 7 | 4 |
| Kiesel et al., 201425 Cohort United States |
Professional American football players Sex = not reported Age = not reported n=238 (60 injuries) |
Injury = MSK injury resulting in time loss from preseason practice or games. Ascertained: Sports medicine staff |
25% of players experienced an injury over the preseason |
|
|
SEN: 0.58 (0.5,0.7) SPE: 0.62 (0.6,0.7)
SPE: 0.87 (0.8,0.9) |
|
8 | 4 |
| Knapik et al., 201526 Historical Cohort United States |
Coast Guard cadets Male = 770 Female = 275 Mean age (SD) Male: 18.1 (0.7) Female: 17.9 (0.7) n=1,045 (number of injuries not reported) |
Injury = any physical bodily damage resulting in a clinic visit which was suspected to be caused by cadet training. Ascertained: PT and other health care providers |
Male = CII 18.6% Female = CII 24.7% For candidates attending classes between 2004–2007 |
|
Males
|
Males
SEN: 0.22 SPE: 0.87Females
SPE: 0.61
|
Males
|
9 | 4 |
| Lisman et al., 201327 Cohort United States |
Marine Corps Officer Trainees Male = 874 Mean age (SD): 22.4±2.7 n=874 (number of injuries not reported) |
Any Injury = sought medical care ≥1 times during training due to physical bodily damage resulting from training Overuse = sought medical care for presumed long-term repetitive energy exchanges that led to cumulative micro-trauma Traumatic = sought medical care for acute or sudden energy exchanges leading to abrupt overload and tissue damage Ascertained: Health care providers |
Not reported (6 or 10 week training) |
Movement Quality
|
Any Injury
|
Any Injury
|
|
15 | 2b |
| Padua et al., 201528 Cohort United States |
Elite youth soccer players Male = 348 Female = 481 Mean age (SD, Range): 13.9 (1.8, 11–18) n=829 (7 injuries) |
Injury = ACL tear verified at surgical reconstruction Non-contact = no direct contact to the LE by an external force Indirect-Contact = contact with a body part other than the knee Ascertained: self-report verified by surgeon |
0.8 % of players experienced an ACL tear over 2006–2009 seasons IRR = 0.006 (0002,0.012) |
|
|
SPE: 0.65 (0.62,0.67) PPV: 0.01 (0.006,0.03) NPV: 0.998 (0.991,0.999) |
n/a | 11 | 2b |
| Shojaedin et al., 201432 Cohort Iran |
Competitive or recreational university athletes Male = 50 Female = 50 Mean age (SD; range): 22.6 (3.0; 18–25) n=100 (35 injuries) |
Any injury = not reported Knee injury = not reported Ankle injury = not reported |
35% sustained injury during the season |
|
Any injury
|
Any Injury
SPE: 0.78 PLR: 2.46 NLR: 0.62 |
|
3 | 4 |
| Smith et al., 201234 Case-control (embedded in a cohort) United States |
High school and college athletes Male = 29 Female = 73 Mean age (SD): 18.3 (2) n= 92 (28 injured) |
Noncontact ACL tear = ACL tear resulting from a non-knee contact event with another athlete, ground, or extraneous structure Ascertained: orthopedic surgeon, MRI and surgery |
30.4% of athletes sustained an injury over 1 season |
|
|
|
|
14 | 3b |
| Warren et al., 201529 Cohort United States |
NCAA Division 1 collegiate athletes Male = 89 Female = 78 Age range: 18–24 n= 167 (74 injuries) |
Injury = First non-contact MSK problem that resulted in medical intervention. Non-contact injury: non-contact mechanism Contact injury = contact mechanism Ascertained: ATC |
44% of athletes experienced an injury over the competitive season |
Movement Quality
|
|
|
11 | 4 | |
| Wiese et al., 201430 Cohort United States |
NCAA Division 1 collegiate American football players Sex: not reported Mean age (SD): 18.9 ± 1.3 n = 144 (93 injuries) |
Injury = initial MSK problem arising from organized training or game requiring medical attention and restricted participation for ≤ 1 days LE injury = groin – toes Overuse injury = tendinopathy, muscle spasm, tightness or soreness Non-contact injury = non-contact mechanism Injury >10 days Ascertained: ATC |
65% of players experienced an injury over 1 season 52% LE 39% overuse 42% noncontact 20% >10 days |
|
|
|
|
10 | 4 |
Statistically significant p<0.05,
Multivariable analyses,
Estimated from reported injury incidence,
analyses did not account for matched design,
Maximum Downs and Black Score for prospective cohort study = 23, while the maximum score for a randomized control trail is 33, AC = abdominal crunch, ASLR = active straight leg raise, ATC = certified athletic trainers, BMI = body mass index (kg/m2), CI = confidence interval, DB = Downs and Black Score, DF = dorsiflexion, DS = deep squat, FMS = Functional Movement Screen, GES = general sport and exercise, HR = Hazard ratio, hrs=hours, HS = hurdle step, ICD-9-CM = International Classification of Disease, Ninth Revision, Clinical Modification, ILL = in-line lunge, IR = incidence rate, IRR = incidence rate ratio, LE = lower extremity, LESS = Landing Error Scoring System, LOE = level of evidence, n/a = not applicable, MD = medical doctor, MSK = musculoskeletal, n/a = not applicable, NLR = negative likelihood ratio, OR = odds ratio, PLR = positive likelihood ratio, PT = physical therapists, PU = pull ups, ROM=range of motion, RR = risk ratio, RS = rotary stability, RT = 3-mile run time, SD = standard deviation, SLHB = single leg hamstring bridge, SLR = straight leg raise, SM = shoulder mobility, TOP = tenderness on palpation, TSPU = trunk stability push-up, TXHD = triple cross-over hop for distance, UE = upper extremity, VDJ = vertical drop jump, wks = weeks, YBT = Y-balance test, yrs = years.
Study characteristics
Characteristics of the 17 included studies are summarized in Table 1. Sixteen of the 17 studies were cohort studies, representing four countries (13 from the United States,18–30 1 each from Canada31, Iran32 and Japan33) published between 2007 and 2015. Thirteen18,19,22–25,28–34 of the studies investigated the value of movement quality screening for athletes (including three18,24,25 involving professional athletes and four22,23,29,30 involving National Collegiate Athletic Association athletes22,23,29,30; 2128 total participants; 1159 males and 817 females), two20,27 in the military (total male participants 3350) and two21,26 in first responder trainees (total participants 1153; unable to distinguish by sex). Fourteen18–20,24–34 of the studies are believed to have included male participants, while seven19,22,26,28,29,32,34 of the studies included female participants. Five21,23–25,30 of the studies did not specify participant sex however based on the sport or military group investigated in three24,25,30 of these it is likely the participants were male. The age range of the athletes was 11–25 years, military members 18–57 years and first responder trainees 11–22 years. One of the studies involving first responder trainees21 and three18,24,25 with athletes did not report age range. Amongst the 17 studies, three20,26,27 had a sample size greater than 500, five20,23,25,29,30 had at least 50 injury cases (range 7–916 with three not reporting the number of injured participants) and four20,27,29,33 utilized a multivariable statistical approach to identify if movement quality outcomes could identify injury risk. Five22,24,25,28,31 of the 17 studies included a metric of diagnostic accuracy and no studies were identified that assessed the value of screening for movement quality on reducing the burden of LE injury.
Clinimetric Properties
Fifteen18–27,29–33 of the 17 studies (88%) employed the Functional Movement Screen (FMS) to assess movement quality, while two28,34 used the Lower Extremity Scoring System (LESS). Of those using the FMS only three22,23,33 investigated the reliability of their measurement system while one34 of the investigations employing the LESS embedded an assessment of reliability into the study design. The most common reliability statistic estimated was an intraclass correlation coefficient with two29,33 of the 17 studies including 95% confidence intervals (CI). One33 study reported estimates of measurement precision.
Injury estimates
Descriptions of injury estimates (incidence proportion, incidence rate, prevalence), effect estimates (IRR, RR, OR) and significant and non-significant movement quality outcomes are presented in Table 1.
Quality and level of evidence
The highest level of evidence demonstrated by all reviewed studies was level 2b (cohort study) with the majority (13/17) of studies classified as level 4 which corresponds to low quality cohort study (n< 500, injury sample < 50, lack of multivariable analyses).
The median methodological quality for all 21 studies, based on the DB criteria, was 11/33 (range 3–15) with only 9/17 scoring greater than 10. The aim of the DB criteria is to assess scientific study methodological quality (inclusive of randomized and non-randomized intervention as well as observational studies). As all of the included studies were observational in nature, 7 items (4, 8, 14, 19, 23, 24, and 27; totaling 10 points) on the DB checklist were not applicable. Areas in which the included studies were consistently limited included: incomplete description of how the sample was representative of the population of interest (e.g., insufficient description of participant characteristics such as sex, history of previous injury, training exposure); limited description of the characteristics of those lost to follow-up; insufficient reporting of how participants were lost to follow-up and differing length of follow-up were accounted for in statistical analyses; inadequate sample size; and lack of adjustment for potential modification and confounding by factors, such as exposure and previous injury. Of further note is the fact that two of the studies reported significant findings even though the 95%CI of the statistical estimate included a null value and that 11/17 studies were published in non-indexed journals or in journals with an impact factor less than 2.
Synthesis of results
The quantity, quality and level of evidence for the most commonly investigated movement quality outcomes are summarized in Table 3. The most common risk factors investigated included age, FMS total score, FMS total score ≤14, FMS total score ≤12, FMS hurdle step, FMS in-line lunge, FMS deep squat, LESS total score and LESS total score ≥5. Based on this synthesis there is inconsistent evidence that poor movement quality is associated with increased risk of LE injury in sport and military/first-responder occupation.
DISCUSSION
To our knowledge, this is the first systematic review examining movement quality risk factors for LE injury in sport and military/first responder occupations that incorporates both a formal evaluation of study quality and level of evidence. Overall there is inconsistent level 4 evidence that poor movement quality is a risk factor for LE injury in sport and military/first-responder occupation populations. Accordingly, as the identification of risk factors is the first step in the injury prevention, it remains unknown if movement quality screening has a role in reducing the burden of LE injury in these populations.
It is important to highlight that the findings of this review are based upon a synthesis and evaluation of existing literature, and as such they are limited by the inadequacies of studies included. Overall there was a lack of consistent high quality evidence to support nominating any particular movement quality outcome as a risk factor due to inadequate reporting of concepts essential to establishing internal and external validity. The biggest threats to internal validity were related to the possibility of selection bias, and the reporting of, and adjustment for, potential confounding by factors such as sex, injury history and training exposure. Specifically, due to the lack of participant characteristic reporting it was often difficult to determine if the individuals selected for a study differed systematically from those in the source population. Equally important was the consistent omission of the characteristics of those lost to follow-up, which made it impossible to determine if participants lost to follow-up were systematically different from those retained in a study. The inability to determine selection bias not only questions the internal validity of several included studies, it impacts the degree to which the findings of these studies can be generalized to the larger population from which the samples were drawn (external validity).
As indicated earlier, it is highly unlikely that a LE injury is a result of a single risk factor or aberrant movement pattern, but rather the consequence of complex interactions between multiple risk factors and inciting events.7 Multivariable biostatistical techniques can explore these complex interactions given an adequate sample size. Bahr and Holme8 estimated that 50 injury cases are needed to detect a moderate to strong association between a risk factor and injury. Of the 17 studies included in this review only four20,27,29,33 employed multivariable biostatistical techniques, of which only two20,29 had 50 or more injury cases (with one27 not reporting the number of injury cases) and were able to assess the influence of additional covariates (e.g., body mass index, smoking status, muscular and cardiovascular fitness, battalion, previous injury history, sex, age and sport). As sex, previous injury, and exposure to training are known to influence the incidence of MSK LE injury the lack of reporting and assessment of the impact of these factors on the association between a pre-season movement quality deficit and injury incidence with adequate sample size and biostatistical techniques brings into question the value of only assessing movement quality to establish injury risk.
It is important to consider that the true value of being able to identify risk factors for future injury is dependent upon it actually leading to strategies that result in injury reduction in real world contexts. This empirical validation requires an accumulation of high quality evidence indicating that an intervention program targeting those at high risk of injury based on a screening test is more beneficial than a non-targeted intervention.9 However before such a hypothesis can be tested there needs to be an accumulation of high quality evidence demonstrating a strong relationship between the risk factor, which was assessed with a valid and reliable screening test employing a specific cut-off value, and injury. Further, the predictive ability of the specific screening test cut-off value must be validated in multiple populations.9
To date, movement quality tests lack the foundation of rigorous development and validation (e.g. psychometrics) common in other fields35 and there is a lack of high quality evidence demonstrating a strong relationship between any single movement quality outcome and injury. As movement quality tests were not specifically developed as diagnostic tools, but rather to identify deficits that inform clinical interventions from a mechanistic perspective, this is perhaps not surprising.9,36 Although several cut-off points for high LE injury risk have been proposed (e.g., FMS total score ≤ 14,24 FMS total score ≤12,30 and LESS total score ≥528), none appear to have sufficient diagnostic accuracy to be useful in real world contexts. For example the sensitivity and specificity of a FMS total score ≤14 has been shown be between 0.54–0.83 and 0.61–0.91 respectively.22,24,25,37 This suggests that almost half of individuals that go on to suffer a injury may not have a FMS total score ≤14 and over half of those that do not go on to suffer an injury may not have a FMS total score ≤14.
The ability to establish a link between poor movement quality and injury risk hold great potential for identifying modifiable causal mechanisms for injury, which can be addressed with a targeted intervention. For example the LESS aims to identify movement quality errors during jump-landing28 such as decreased hip flexion and knee valgus that have been associated with anterior cruciate ligament injury. In doing so provides a starting point for targeted interventions aimed at improving jump-landing mechanics and reducing an individual’s future ACL injury risk. However, the link between other movement quality outcomes that have an association with LE injury, such as reduced shoulder mobility19 or other FMS components, is not as intuitive. Without a theoretical basis linking the ‘non-optimal movement’ to the injury, it would be difficult to know how to use the finding of an “abnormal” movement to guide an intervention aimed at reducing injury risk. This is a limitation of some movement quality outcomes that will have to be addressed prior to widespread application.
A final consideration is that this review was unable to identify any investigation that had assessed the value of screening for movement quality for reducing the burden of LE injury through targeted interventions in sport or military/first-responder occupation populations. With that said there are several examples of attempts to do this in the field of sport injury prevention using physical performance outcomes that can provide valuable guidance38,39 Specifically, these studies highlight the importance of developing an implementation strategy in conjunction with the intervention and then tracking and accounting for adherence to the prevention programs in the analysis.
Limitations
Meta-analyses were not possible due to the fact that the assumptions for meta-analyses were not satisfied by the included studies. In particular, there was considerable inconsistency in methodology (e.g., reporting and controlling for confounding) and heterogeneity of injury definition. For example, the injury definition covered the span of ‘a MSK injury resulting from organized intercollegiate sport practice or competition that required medical attention or advice from a certified athletic trainer, athletic training student or physician’22 to ‘a MSK injury that occurred during participation in track and field practice or competition that prevented participation for 4 weeks’33. This inconsistency in injury definition led to injury estimates ranging from 0.8 % to 85% of participants across the included studies. Further, despite a comprehensive search strategy and rigorous approach to study selection, it is important to acknowledge the possibility of omitting a relevant study and inclusion of only English language articles as additional potential limitations. Finally, as the findings of this review are based upon a synthesis and evaluation of existing literature it is important to point out that the current evidence base of studies that have assessed the prospective relationship between poor movement quality and LE injury may not have considered all possible movement quality screening tests (e.g., Nine Battery Test,40 Performance Matrix,41 Single Leg Squat,42–44 Tuck Jump Assessment and Star Excursion Balance Test45).
Recommendations
Both cohort and intervention study designs can play an important role in identifying potential risk factors and reducing the burden of LE injury in sport and military/first-responder occupations.8,9 While cohort studies are critical for establishing temporality between a risk factor and subsequent injury, randomized controlled trials (RCTs) provide the strongest evidence for the causal nature of a risk factor and the effectiveness of modifying that factor on injury burden. Based upon the studies reviewed it is recommended that future research focus on high quality cohort studies aimed at identifying the most relevant movement quality outcomes for predicting injury followed by establishing the diagnostic accuracy of the movement quality screening tests used to assess these risk factors in relevant populations. Given the challenges and high cost of undertaking high quality cohort studies, an alternative approach may be to simultaneously develop and evaluate pre-participation screening and LE injury prevention programs through high quality RCT’s targeting athletes or workers at greater risk of injury based upon previous injury. Further recommendations include; ensuring consistency in injury definition amongst studies attempting to determine the relationship between a movement quality outcome and subsequent injury that aligns with international consensus46 and the development of movement quality screening tools according to psychometric principles.35 Implementation of these recommendations will assist in the advancement of injury prediction and prevention.
CONCLUSIONS
Based on the findings of this systematic review it is recommended future research focus on high quality cohort studies to identify the most relevant movement quality outcomes for predicting injury. This should be followed by development and evaluation of pre-participation screening and LE injury prevention programs through high quality randomized controlled trials targeting athletes or workers at greater risk of injury based upon psychometrically sound movement screening tests.
Table 2.
Summary of significant and non-significant movement quality outcomes by quantity, quality and level of evidence.
| Level of Evidence^ | 1 | 2 | 3 | 4 | 5 | Total Studies | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| a | b: RCT | c | a | b: True/Quasi Experimental | b: Cohort | b: Historical Cohort | c | a | b: Case Control | Pilot cohort Cross-sectional | |||||||
| Risk Factor | SIG | NOT | SIG | NOT | SIG | NOT | SIG | NOT | |||||||||
| FMS total score | 4 3–12) | 1 (10) | 5 | ||||||||||||||
| FMS ≤14 | 1 (15) | 5 (7–12) | 4 (9–14) | 10 | |||||||||||||
| FMS ≤ 12 | 1* (9) | 3 (10–12) | 4 | ||||||||||||||
| FMS HS | 2 (9–12) | 4 (8–12) | 6 | ||||||||||||||
| FMS ILL | 2 (12) | 4 (8–14) | 6 | ||||||||||||||
| FMS DS | 3 (8–14) | 3 (9–11) | 6 | ||||||||||||||
| LESS total score | 1 (11) | 1 (14) | 2 | ||||||||||||||
| LESS ≥ 5 | 1 (11) | 1 (14) | 2 | ||||||||||||||
Cell values represent number of studies (range of Downs and Black quality assessment tool scores). As per exclusion criteria, systematic reviews (1a, 2a, 3a), case series (4) and opinion-based papers (5) were not included (shown in dark grey).
Level of evidence is based on the modified Oxford Centre for Evidence-Based Medicine Model.
= female participants only, DS = deep squat, FMS = Functional Movement Screen, HS = hurdle step, ILL = in-line lunge, LESS = Landing Error Scoring System.
WHAT ARE THE NEW FINDINGS.
There is conflicting level 4 evidence that movement quality outcomes are risk factors for lower extremity injury in sport and military/first-responder occupation populations.
There is a need for consistency in injury definition amongst studies attempting to determine the relationship between a movement quality outcome and subsequent injury.
Based on the work done in the field it is recommended that investigators focus on high quality cohort studies to identify the most relevant movement quality outcomes for predicting injury risk that account for the multifactorial nature of injury by ensuring adequate sample size and employing relevant biostatistical techniques.
Acknowledgments
FUNDING
N Booysen is funded by the National Institute for Health Research (Grant number: CDRF-2014-05-021), D Wilson and M Warner are funded by Arthritis Research UK (Grant number: 20194), C Lewis is supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health (Award number K23 AR063235). C Emery is funded through a Chair in Pediatric Rehabilitation (Alberta Children’s Hospital Foundation). These sponsors had no involvement with respect to design, collection or data analyses, interpretation, writing or submission
All of the authors are members of the International Movement Screening group of the Arthritis Research UK Centre for Sport, Exercise and Osteoarthritis http://www.sportsarthritisresearchuk.org/seoa/international-movement-screening-and-interventions-group-imsig/imsig.aspx. The authors would like to acknowledge the assistance of Matt Attwood (PhD student), Department for Health, University of Bath, Bath UK, Connor Power (PhD student), Faculty of Health Sciences, University of Southampton, Southampton, UK and Tim Gribbin (Research Coordinator), Uniformed Services University of the Health Sciences, Bethesda, Maryland, USA for their help in screening titles and abstracts, as well as Joanne Bartram, Arthritis Research UK Centre for Sport, Exercise and Osteoarthritis Administrator for her administrative support.
APPENDIX 1: SEARCH TERMS, STRATEGIES AND RESULTS
SEARCH TERMS AND STRATEGIES
1. Search Concepts
athletic and first responders and military
injuries
lower extremity
movement
measuring quality
lower extremity movement quality tests (meet criteria of above 3 concepts)
clinimetric properties
limits and exclusions
2. Search terms and Strategies
a. Ovid MEDLINE(R) In-Process & Other Non-Indexed Citations, Ovid MEDLINE(R) Daily and Ovid MEDLINE(R) 1946 to Present
Athletic Injuries/
exp Sports/
Athletes/
Military Personnel/
exp Emergency Responders/
(sport or sports or athlet* or runners or (run* adj2 (marathon* or competitive* or casual* or recreation*)) or joggers or police* or officer* or firefighter* or firem* or fire personnel or military or army or navy or air force or airforce or soldier* or armed forces or armed service* or active duty* or veteran* or paramedic or first responder* or (emergency adj2 responder*) or ambulance or emergency medical technician*).mp.
(active adj3 (individual* or population* or participant* or male* or female* or men or women or persons or students or adult* or patients or adolescent*)).mp.
or/1–7
exp hip injuries/or exp leg injuries/or hip dislocation/or knee dislocation/or patellar dislocation/
femoracetabular impingement/or patellofemoral pain syndrome/
((injur* or pain* or tear or tears or sprain* or strain* or dislocation* or impingement* or instability) adj6 (risk or risks or predict* or associat* or correlat* or screen* or prevent* or sport* or athletic or running)).mp.
((injur* or pain* or tear or tears or sprain* or strain* or dislocation* or impingement* or instability) adj8 (lower extremit* or lower limb* or hip or hips or thigh or thighs or leg or legs or knee or knees or ankle* or foot or foots or toe or toes or ACL or PCL or ((anterior or posterior) adj cruciate adj2 ligament*) or femoracetabular or femur or (menisc* adj3 (tibia* or lateral)) or patellofemoral)).mp.
“Sprains and Strains”/
Joint Instability/
Pain/
Athletic Injuries/
Dislocations/
“Wounds and Injuries”/
or/9–18
exp hip injuries/or exp leg injuries/or hip dislocation/or knee dislocation/or patellar dislocation/
(lower extremit* or lower limb* or hip or hips or thigh or thighs or leg or legs or knee or knees or ankle* or foot or foots or toe or toes or ACL or PCL or ((anterior or posterior) adj cruciate adj2 ligament*) or femoracetabular or femur or (menisc* adj3 (tibia* or lateral)) or patellofemoral).mp.
(run or running or jog* or squat* or minisquat* or balance or lunge or lunges or hop or jump or jumping or walk or walking or step-up or hurdle or gait).mp.
20 or 21 or 22
motor activity/
(exercis* or (physical adj (activit* or perform* or function*))).mp.
(function* adj (activ* or perform*)).mp.
(motor or movement or motion or dynamic or moving).mp.
(run or running or jog* or squat* or minisquat* or balance or lunge or lunges or hop or jump or jumping or walk or walking or step-up or hurdle or gait).mp.
or/24–27
“Task Performance and Analysis”/
(functional test* or grade or grading or rating or rated or score or scoring or rank or ranked or ranking).mp.
(control adj6 (assess* or test* or measur*)).mp.
(movement adj2 (screen* or assess* or quality or performance or observation or observe* or test*)).mp.
((performance or objective or observation* or quality) adj5 (measur* or test* or instrument* or method or methods or index or indices or assess* or screen*)).mp.
((deficit* or varus or valgus or asymmetr* or compensatory movement) and (measur* or test* or instrument* or method or methods or index or indices or assess* or screen*)).mp.
or 30–35
(((Lunge or Squat or Hop or jump or Reach or Cutting or Step-up or Balance or Push-up or Lift or Rotation or walk*) adj3 (test* or task* or assessment)) or gait analys* or gait evaluation*).mp.
(deep squat* or one leg squat* or mini-squat* or mini squat* or “in line lunge*” or inline lunge* or double leg drop vertical jump* or “hop and hold*” or Hurdle step* or single leg pickup or single leg pick-up or single leg land or single leg balance or leg raise or tuck jump or vertical jump or drop jump).mp.
(Functional movement screen* or PPM-16 or ((nine-test or movement or performance or function) adj3 screening battery) or landing error scoring system* or balance error scoring system*).mp.
or/37–39
(23 and 29 and 36 and 40)
predictive value.mp.
(predict* or associat* or correlat*).ti.
((predict* or correlat* or associat*) adj10 (injur* or pain* or tear or tears or sprain* or strain* or dislocation* or impingement* or instability)).mp.
(receiver operator curve* or ROC or likelihood ratio* or specificity or ((positive* or negative* or high* or low) adj4 correlat*)).mp.
validation studies/
Comparative Study/
“Outcome Assessment (Health Care)”/
observer variation/
Health Status Indicators/
exp “reproducibility of results”/
discriminant analysis/
(outcome assessment or outcome measure or observer variation or instrumentation or psychometr* or clinimetr* or clinometr* or reproducib* or reliab* or unreliab* or valid* or coefficient or homogeneity or homogeneous or internal consistency).mp.
((cronbach* adj2 alpha*) or (item adj5 (correlation* or selection* or reduction*)) or agreement or precision or imprecision or precise value* or test-retest or (test adj3 retest) or stability).mp.
(interrater or inter-rater or intrarater or intra-rater or intertester or inter-tester or intratester or intra-tester or interobserver or inter-observer or intraobserver or intraobserver or intertechnician or inter-technician or intratechnician or intra-technician or interexaminer or inter-examiner or intraexaminer or intra-examiner or interassay or inter-assay or intraassay or intra-assay or interindividual or inter-individual or intraindividual or intra-individual or interparticipant or interparticipant or intraparticipant or intra-participant).mp.
(kappa* or repeatab* or ((replicab* or repeated) adj6 (measure or measures or findings or result or results or test or tests)) or generaliza* or generalisa* or concordance or (intraclass and correlation*) or discriminative or known group or factor analysis or factor analyses or dimension* or subscale* or (multitrait adj6 scaling adj6 analys*) or item discriminant or interscale correlation* or error or errors or individual variability or (variability adj8 (analysis or values)) or (uncertainty adj6 (measurement or measuring)) or standard error of measurement or sensitiv* or responsive* or ((minimal or minimally or clinical or clinically or mall*) adj6 (important or significant or detectable or real) adj6 (change or difference)) or meaningful change or ceiling effect or floor effect or Item response model or IRT or Rasch or Differential item functioning or DIF or computer adaptive testing or item bank or cross-cultural equivalence).mp.
or/42–56
8 and 19 and 41 and 57
limit 58 to animals
limit 59 to humans
(mice or mouse or rat or rats or animal model* or bovine or rodent*).ti.
58 not ((59 not 60) or 61)
(arthroplast* or arthroscop* or TKA or THA or surgery or surgical).ti.
((after or undergoing) adj5 reconstruction).ti.
(paraplegi* or brain injur* or stroke or post-stroke or concussion or polyneuropath* or fibromyalgia or multiple sclerosis or arteriosclerosis or cancer or neoplasm* or malignanc* or degenerative).ti.
“return to sport”.ti.
(claudication or epidural or platelet-rich plasma or cadaver or spinal cord or spinal chord or vibration or arterial disease or caffeine or pregnan* or breast or breasts or steroid*).ti.
62 not (or/63–67)
limit 68 to “review articles”
68 not 69
case reports/
case report*.jw.
((case not (case control or case cohort or case crossover)) adj4 (series or study or report*)).ti.
70 not (or/71–73)
limit 74 to english language
b. Embase 1974 to 2015 December 31
sport injury/or battle injury/
exp sport/
athlete/
soldier/
rescue personnel/
(sport or sports or athlet* or runners or (run* adj2 (marathon* or competitive* or casual* or recreation*)) or joggers or police* or officer* or firefighter* or firem* or fire personnel or military or army or navy or air force or airforce or soldier* or armed forces or armed service* or active duty* or veteran* or paramedic or first responder* or (emergency adj2 responder*) or ambulance or emergency medical technician*).mp.
(active adj3 (individual* or population* or participant* or male* or female* or men or women or persons or students or adult* or patients or adolescent*)).mp.
or/1–7
sport injury/or battle injury/
exp leg pain/or exp leg injury/or femoroacetabular impingement/or ankle sprain/
injury/or injury prediction/or limb injury/or musculoskeletal injury/or soft tissue injury/or tissue injury/or sprain/or joint injury/or dislocation/or joint fracture/or joint instability/
((injur* or pain* or tear or tears or sprain* or strain* or dislocation* or impingement* or instability) adj6 (risk or risks or predict* or associat* or correlat* or screen* or prevent* or sport* or athletic or running)).mp.
((injur* or pain* or tear or tears or sprain* or strain* or dislocation* or impingement* or instability) adj8 (lower extremit* or lower limb* or hip or hips or thigh or thighs or leg or legs or knee or knees or ankle* or foot or foots or toe or toes or ACL or PCL or ((anterior or posterior) adj cruciate adj2 ligament*) or femoracetabular or femur or (menisc* adj3 (tibia* or lateral)) or patellofemoral)).mp.
or 9–13
exp leg pain/or exp leg injury/or femoroacetabular impingement/or ankle sprain/
hip/or exp leg/or exp “bones of the leg and foot”/or quadratus femoris muscle/or quadriceps femoris muscle/or sartorius muscle/or soleus muscle/or tibialis anterior muscle/or tibialis posterior muscle/or vastus lateralis muscle/or vastus medialis muscle/or ligament/or ankle lateral ligament/or exp knee ligament/or “ligament of head of femur”/or patella ligament/
(lower extremit* or lower limb* or hip or hips or thigh or thighs or leg or legs or knee or knees or ankle* or foot or foots or toe or toes or ACL or PCL or ((anterior or posterior) adj cruciate adj2 ligament*) or femoracetabular or femur or (menisc* adj3 (tibia* or lateral)) or patellofemoral).mp.
(run or running or jog* or squat* or minisquat* or balance or lunge or lunges or hop or jump or jumping or walk or walking or step-up or hurdle or gait).mp.
or/15–18
motor activity/or physical activity/or physical performance/or “physical activity, capacity and performance”/or motor performance/
(exercis* or (physical adj (activit* or perform* or function*))).mp.
(function* adj (activ* or perform*)).mp.
(motor or movement or motion or dynamic or moving).mp.
(run or running or jog* or squat* or minisquat* or balance or lunge or lunges or hop or jump or jumping or walk or walking or step-up or hurdle or gait).mp.
or/20–24
(functional test* or grade or grading or rating or rated or score or scoring or rank or ranked or ranking).mp.
(control adj6 (assess* or test* or measur*)).mp.
(movement adj2 (screen* or assess* or quality or performance or observation or observe* or test*)).mp.
((performance or objective or observation* or quality) adj5 (measur* or test* or instrument* or method or methods or index or indices or assess* or screen*)).mp.
((deficit* or varus or valgus or asymmetr* or compensatory movement) and (measur* or test* or instrument* or method or methods or index or indices or assess* or screen*)).mp.
or/26–30
(((Lunge or Squat or Hop or jump or Reach or Cutting or Step-up or Balance or Push-up or Lift or Rotation or walk*) adj3 (test* or task* or assessment)) or gait analys* or gait evaluation*).mp.
(deep squat* or one leg squat* or mini-squat* or mini squat* or “in line lunge*” or inline lunge* or double leg drop vertical jump* or “hop and hold*” or Hurdle step* or single leg pickup or single leg pick-up or single leg land or single leg balance or leg raise or tuck jump or vertical jump or drop jump).mp.
(Functional movement screen* or PPM-16 or ((nine-test or movement or performance or function) adj3 screening battery) or landing error scoring system* or balance error scoring system*).mp.
or/32–34
(19 and 25 and 31) or 35
predictive value.mp.
(predict* or associat* or correlat*).ti.
((predict* or correlat* or associat*) adj10 injur*).mp.
(receiver operator curve* or ROC or likelihood ratio* or specificity or ((positive* or negative* or high* or low) adj4 correlat*)).mp.
validation study/
comparative study/
outcome assessment/
observer variation/
health status indicator/
exp measurement precision/
statistical parameters/or exp reliability/or exp validity/
discriminant analysis/
(outcome assessment or outcome measure or observer variation or instrumentation or psychometr* or clinimetr* or clinometr* or reproducib* or reliab* or unreliab* or valid* or coefficient or homogeneity or homogeneous or internal consistency).mp.
((cronbach* adj2 alpha*) or (item adj5 (correlation* or selection* or reduction*)) or agreement or precision or imprecision or precise value* or test-retest or (test adj3 retest) or stability).mp.
(interrater or inter-rater or intrarater or intra-rater or intertester or inter-tester or intratester or intra-tester or interobserver or inter-observer or intraobserver or intraobserver or intertechnician or inter-technician or intratechnician or intra-technician or interexaminer or inter-examiner or intraexaminer or intra-examiner or interassay or inter-assay or intraassay or intra-assay or interindividual or inter-individual or intraindividual or intra-individual or interparticipant or interparticipant or intraparticipant or intra-participant).mp.
(kappa* or repeatab* or ((replicab* or repeated) adj6 (measure or measures or findings or result or results or test or tests)) or generaliza* or generalisa* or concordance or (intraclass and correlation*) or discriminative or known group or factor analysis or factor analyses or dimension* or subscale* or (multitrait adj6 scaling adj6 analys*) or item discriminant or interscale correlation* or error or errors or individual variability or (variability adj8 (analysis or values)) or (uncertainty adj6 (measurement or measuring)) or standard error of measurement or sensitiv* or responsive* or ((minimal or minimally or clinical or clinically or mall*) adj6 (important or significant or detectable or real) adj6 (change or difference)) or meaningful change or ceiling effect or floor effect or Item response model or IRT or Rasch or Differential item functioning or DIF or computer adaptive testing or item bank or cross-cultural equivalence).mp.
or/37–52
8 and 14 and 36 and 53
limit 54 to animals
(mice or mouse or rat or rats or animal model* or bovine or rodent*).ti.
54 not (55 or 56)
(arthroplast* or arthroscop* or TKA or THA or surgery or surgical).ti.
((after or undergoing) adj5 reconstruction).ti.
(paraplegi* or brain injur* or stroke or post-stroke or concussion or polyneuropath* or fibromyalgia or multiple sclerosis or arteriosclerosis or cancer or neoplasm* or malignanc* or degenerative).ti.
“return to sport”.ti.
(claudication or epidural or platelet-rich plasma or cadaver or spinal cord or spinal chord or vibration or arterial disease or caffeine or pregnan* or breast or breasts or steroid*).ti.
57 not (or/58–62)
limit 63 to (conference abstract or “conference review” or “review”)
63 not 64
case report/
case study/
case report*.jx.
((case not (case control or case cohort or case crossover)) adj4 (series or study or report*)).ti.
65 not (66 or 67 or 68)
limit 70 to english language
c. CINAHL Plus with Full Text
Search mode: Boolean/Phrase
-
S1
( (MH “Athletic Injuries+”) OR (MH “Sports+”) OR (MH “Military Personnel+”) ) OR ( sport or sports or athlet* or runners or (run* n2 (marathon* or competitive* or casual* or recreation*)) or joggers or police* or officer* or firefighter* or firem* or “fire personnel” or military or army or navy or “air force” or airforce or soldier* or “armed forces” or “armed service*” or “active duty*” or veteran* or paramedic or “first responder*” or (emergency n2 responder*) or ambulance or “emergency medical technician*” ) OR ( active n3 (individual* or population* or participant* or male* or female* or men or women or persons or students or adult* or patients or adolescent*) )
-
S2
( (MH “Leg Injuries+”) OR (MH “Knee Pain+”) OR (MH “Femoracetabular Impingement”) OR (MH “Wounds and Injuries”) OR (MH “Fractures”) OR (MH “Sprains and Strains”) OR (MH “Dislocations”) OR (MH “Athletic Injuries+”) OR (MH “Tendon Injuries”) OR (MH “Pain”) OR (MH “Joint Instability”) ) OR ( (injur* or pain* or tear or tears or sprain* or strain* or dislocation* or impingement* or instability) n6 (risk or risks or predict* or associat* or correlat* or screen* or prevent* or sport* or athletic or running) ) OR ( (injur* or pain* or tear or tears or sprain* or strain* or dislocation* or impingement* or instability) n8 (“lower extremit*” or “lower limb*” or hip or hips or thigh or thighs or leg or legs or knee or knees or ankle* or foot or foots or toe or toes or ACL or PCL or (cruciate n2 ligament*) or femoracetabular or femur or tibia* or patellofemoral or patella*) )
-
S3
( (MH “Leg Injuries+”) OR (MH “Knee Pain+”) OR (MH “Femoracetabular Impingement”) ) OR ( “lower extremit*” or “lower limb*” or hip or hips or thigh or thighs or leg or legs or knee or knees or ankle* or foot or foots or toe or toes or ACL or PCL or (cruciate n2 ligament*) or femoracetabular or femur or tibia* or patellofemoral or patella* ) OR ( run or running or jog* or squat* or minisquat* or balance or lunge or lunges or hop or jump or jumping or walk or walking or step-up or hurdle or gait )
-
S4
( motor or movement or motion or dynamic or moving ) OR ( exercis* or (physical n1 (activit* or perform* or function*)) ) OR ( (function* n1 (activ* or perform*)) ) OR ( run or running or jog* or squat* or minisquat* or balance or lunge or lunges or hop or jump or jumping or walk or walking or step-up or hurdle or gait )
-
S5
(MH “Task Performance and Analysis”) OR ( “functional test*” or grade or grading or rating or rated or score or scoring or rank or ranked or ranking ) OR ( movement n2 (screen* or assess* or quality or performance or observation or observe* or test*) ) OR ( (performance or objective or observation* or quality or control) n5 (measur* or test* or instrument* or method or methods or index or indices or assess* or screen*) ) OR (( deficit* or varus or valgus or asymmetr* or “compensatory movement”) and (measur* or test* or instrument* or method or methods or index or indices or assess* or screen* ))
-
S6
( (Lunge or Squat or Hop or jump or Reach or Cutting or Step-up or Balance or Push-up or Lift or Rotation or walk*) n3 (test* or task* or assessment) ) OR ( “gait analys*” or “gait evaluation*” or “deep squat*” or “one leg squat*” or mini-squat* or “mini squat*” or “in line lunge*” or “inline lunge*” or “double leg drop” or “hop and hold*” or “Hurdle step*” or “single leg pickup” or “single leg pick-up” or “single leg land” or “single leg balance” or “leg raise” or “tuck jump” or “vertical jump” or “drop jump” ) OR ( “functional movement screen*” or “landing error scoring system*” or “balance error scoring system*” or ppm-16 ) OR ( (nine-test or movement or performance or function) n3 “screening battery” )
-
S7
(S3 AND S4 AND S5) OR S6
-
S8
TI (predict* or associat* or correlat*)
-
S9
(MH “Discriminant Analysis”) or (MH “Health Status Indicators”) or (MH “Comparative Studies”)
-
S10
( “predictive value” or “receiver operator curve*” or ROC or “likelihood ratio*” or specificity ) OR ( (predict* or correlat* or associat*) n10 (injur* or pain* or tear or tears or sprain* or strain* or dislocation* or impingement* or instability) ) OR ( (positive* or negative* or high* or low) n4 correlat*) ) OR ( “outcome assessment” or “outcome measure*” or “observer variation*” or instrumentation or psychometr* or clinimetr* or clinometr* or reproducib* or reliab* or unreliab* or valid* or coefficient or homogeneity or homogeneous or “internal consistency”)
-
S11
( (item n5 (correlation* or selection* or reduction*) ) OR ( “cronbach* alpha” or agreement or precision or imprecision or “precise value*” or test-retest or (test n3 retest) or stability ) OR ( interrater or inter-rater or intrarater or intra-rater or intertester or inter-tester or intratester or intra-tester or interobserver or inter-observer or intraobserver or intraobserver or intertechnician or inter-technician or intratechnician or intra-technician or interexaminer or inter-examiner or intraexaminer or intra-examiner or interassay or inter-assay or intraassay or intra-assay or interindividual or inter-individual or intraindividual or intra-individual or interparticipant or interparticipant or intraparticipant or intra-participant )
-
S12
( (replicab* or repeated) n6 (measure or measures or findings or result or results or test or tests) ) OR ( kappa* or repeatab* or generaliza* or generalisa* or concordance or (intraclass and correlation*) or discriminative or “known group” or “factor analysis” or “factor analyses” or dimension* or subscale* ) OR (multitrait n6 scaling n6 analys*) OR ( “item discriminant” or “interscale correlation*” or error or errors or “individual variability” or “standard error of measurement” or sensitiv* or responsive* ) OR ( variability n8 (analysis or values) ) OR ( uncertainty n6 (measurement or measuring) ) OR ( (minimal or minimally or clinical or clinically or mall*) n6 (important or significant or detectable or real) n6 (change or difference) ) OR ( “meaningful change” or “ceiling effect” or “floor effect” or “item response model” or IRT or Rasch or “Differential item functioning” or DIF or “computer adaptive testing” or “item bank” or “crosscultural equivalence” )
-
S13
S8 OR S9 OR S10 OR S11 OR S12
-
S14
S1 AND S2 AND S7 AND S13
-
S15
TI ( ice or mouse or rat or rats or animal model* or bovine or rodent* ) OR TI ( arthroplast* or arthroscop* or TKA or THA or surgery or surgical or paraplegi* or brain injur* or stroke or post-stroke or concussion or polyneuropath* or fibromyalgia or multiple sclerosis or arteriosclerosis or cancer or neoplasm* or malignanc* or degenerative or “return to sport” or claudication or epidural or platelet-rich plasma or cadaver or spinal cord or spinal chord or vibration or arterial disease or caffeine or pregnan* or breast or breasts or steroid* ) OR TI ( (after or undergoing) n5 reconstruction )
-
S16
PT review
-
S17
(MH “Case Studies”)
-
S18
TI ((case NOT (case control or case cohort or case crossover)) n4 (series or study or report*))
-
S19
SO case report*
-
S20
S14 NOT ( (S15 OR S16 OR S17 OR S18 OR S19) )
-
S21
S20 Limiters - Language: English
d. SPORTDiscus
Search mode: Boolean/Phrase
-
S1
AB ( ( athlet* or players or sport or sports or rugby or netball* or basketball* or hockey or volleyball or skiers or snowboard* or soccer or football* or lacrosse or rowers or gymnasts or “figure skaters” or dancers or tennis or badminton ) OR ( runners or (run* n2 (marathon* or competitive* or casual* or recreation*)) or joggers or police* or officer* or firefighter* or firem* or “fire personnel” or military or army or navy or “air force” or airforce or soldier* or “armed forces” or “armed service*” or “active duty*” or veteran* or paramedic or “first responder*” or (emergency n2 responder*) or ambulance or “emergency medical technician*” ) OR ( active n3 (individual* or population* or participant* or male* or female* or men or women or persons or students or adult* or patients or adolescent*) ) ) OR KW ( ( athletes or players or sport or sports or rugby or netball* or basketball* or hockey or volleyball or skiers or snowboard* or soccer or football* or lacrosse or rowers or gymnasts or “figure skaters” or dancers or tennis or badminton ) OR ( runners or (run* n2 (marathon* or competitive* or casual* or recreation*)) or joggers or police* or officer* or firefighter* or firem* or “fire personnel” or military or army or navy or “air force” or airforce or soldier* or “armed forces” or “armed service*” or “active duty*” or veteran* or paramedic or “first responder*” or (emergency n2 responder*) or ambulance or “emergency medical technician*” ) OR ( active n3 (individual* or population* or participant* or male* or female* or men or women or persons or students or adult* or patients or adolescent*) ) ) OR TI ( ( athletes or players or sport or sports or rugby or netball* or basketball* or hockey or volleyball or skiers or snowboard* or soccer or football* or lacrosse or rowers or gymnasts or “figure skaters” or dancers or tennis or badminton ) OR ( runners or (run* n2 (marathon* or competitive* or casual* or recreation*)) or joggers or police* or officer* or firefighter* or firem* or “fire personnel” or military or army or navy or “air force” or airforce or soldier* or “armed forces” or “armed service*” or “active duty*” or veteran* or paramedic or “first responder*” or (emergency n2 responder*) or ambulance or “emergency medical technician*” ) OR ( active n3 (individual* or population* or participant* or male* or female* or men or women or persons or students or adult* or patients or adolescent*) ) ) OR SU ( ( athletes or players or sport or sports or rugby or netball* or basketball* or hockey or volleyball or skiers or snowboard* or soccer or football* or lacrosse or rowers or gymnasts or “figure skaters” or dancers or tennis or badminton ) OR ( runners or (run* n2 (marathon* or competitive* or casual* or recreation*)) or joggers or police* or officer* or firefighter* or firem* or “fire personnel” or military or army or navy or “air force” or airforce or soldier* or “armed forces” or “armed service*” or “active duty*” or veteran* or paramedic or “first responder*” or (emergency n2 responder*) or ambulance or “emergency medical technician*” ) OR ( active n3 (individual* or population* or participant* or male* or female* or men or women or persons or students or adult* or patients or adolescent*) ) )
-
S2
SU (injur* or pain* or tear or tears or sprain* or strain* or dislocation* or impingement* or instability )
-
S3
( (injur* or pain* or tear or tears or sprain* or strain* or dislocation* or impingement* or instability) n6 (risk or risks or predict* or associat* or correlat* or screen* or prevent* or sport* or athletic or running) ) OR ( (injur* or pain* or tear or tears or sprain* or strain* or dislocation* or impingement* or instability) n8 (“lower extremit*” or “lower limb*” or hip or hips or thigh or thighs or leg or legs or knee or knees or ankle* or foot or foots or toe or toes or ACL or PCL or (cruciate n2 ligament*) or femoracetabular or femur or tibia* or patellofemoral or patella*) )
-
S4
S2 OR S3
-
S5
( “lower extremit*” or “lower limb*” or hip or hips or thigh or thighs or leg or legs or knee or knees or ankle* or foot or foots or toe or toes or ACL or PCL or (cruciate n2 ligament*) or femoracetabular or femur or tibia* or patellofemoral or patella* ) OR ( run or running or jog* or squat* or minisquat* or balance or lunge or lunges or hop or jump or jumping or walk or walking or step-up or hurdle or gait )
-
S6
( motor or movement or motion or dynamic or moving or exercise ) OR ( (physical n1 (activit* or perform* or function*)) ) OR ( (function* n1 (activ* or perform*)) ) OR ( run or running or jog* or squat* or minisquat* or balance or lunge or lunges or hop or jump or jumping or walk or walking or step-up or hurdle or gait )
-
S7
( “functional test*” or grade or grading or rating or rated or score or scoring or rank or ranked or ranking ) OR ( movement n2 (screen* or assess* or quality or performance or observation or observe* or test*) ) OR ( (performance or objective or observation* or quality or control) n5 (measur* or test* or instrument* or method or methods or index or indices or assess* or screen*) ) OR ( ( deficit* or varus or valgus or asymmetr* or “compensatory movement”) and (measur* or test* or instrument* or method or methods or index or indices or assess* or screen* ) )
-
S8
( (Lunge or Squat or Hop or jump or Reach or Cutting or Step-up or Balance or Push-up or Lift or Rotation or walk*) n3 (test* or task* or assessment) ) OR ( “gait analys*” or “gait evaluation*” or “deep squat*” or “one leg squat*” or mini-squat* or “mini squat*” or “in line lunge*” or “inline lunge*” or “double leg drop” or “hop and hold*” or “Hurdle step*” or “single leg pickup” or “single leg pick-up” or “single leg land” or “single leg balance” or “leg raise” or “tuck jump” or “vertical jump” or “drop jump” or “functional movement screen*” or “landing error scoring system*” or “balance error scoring system*” or ppm-16 ) OR ( (nine-test or movement or performance or function) n3 “screening battery” )
-
S9
(S5 AND S6 AND S7) OR S8
-
S10
TI(predict* or associat* or correlat*)
-
S11
(“discriminant analys*” or “health status indicators” or “health indicators” or “predictive value” or “receiver operator curve*” or ROC or “likelihood ratio*” or specificity ) OR ( (predict* or correlat* or associat*) n10 (injur* or pain* or tear or tears or sprain* or strain* or dislocation* or impingement* or instability) ) OR ( (positive* or negative* or high* or low) n4 correlat*) ) OR ( “outcome assessment” or “outcome measure*” or “observer variation*” or instrumentation or psychometr* or clinimetr* or clinometr* or reproducib* or reliab* or unreliab* or valid* or coefficient or homogeneity or homogeneous or “internal consistency”)
-
S12
(item n5 (correlation* or selection* or reduction*) ) OR ( “cronbach* alpha” or agreement or precision or imprecision or “precise value*” or test-retest or (test n3 retest) or stability ) OR ( interrater or inter-rater or intrarater or intra-rater or intertester or inter-tester or intratester or intra-tester or interobserver or inter-observer or intraobserver or intraobserver or intertechnician or inter-technician or intratechnician or intra-technician or interexaminer or inter-examiner or intraexaminer or intra-examiner or interassay or inter-assay or intraassay or intra-assay or interindividual or inter-individual or intraindividual or intra-individual or interparticipant or interparticipant or intraparticipant or intra-participant )
-
S13
( (replicab* or repeated) n6 (measure or measures or findings or result or results or test or tests) ) OR ( kappa* or repeatab* or generaliza* or generalisa* or concordance or (intraclass and correlation*) or discriminative or “known group” or “factor analysis” or “factor analyses” or dimension* or subscale* ) OR (multitrait n6 scaling n6 analys*) OR ( “item discriminant” or “interscale correlation*” or error or errors or “individual variability” or “standard error of measurement” or sensitiv* or responsive* ) OR ( variability n8 (analysis or values) ) OR ( uncertainty n6 (measurement or measuring) ) OR ( (minimal or minimally or clinical or clinically or mall*) n6 (important or significant or detectable or real) n6 (change or difference) ) OR ( “meaningful change” or “ceiling effect” or “floor effect” or “item response model” or IRT or Rasch or “Differential item functioning” or DIF or “computer adaptive testing” or “item bank” or “cross-cultural equivalence” )
-
S14
S10 OR S11 OR S12 OR S13
-
S15
S1 AND S4 AND S9 AND S14
-
S16
TI ( mice or mouse or rat or rats or animal model* or bovine or rodent* ) OR TI ( arthroplast* or arthroscop* or TKA or THA or surgery or surgical or paraplegi* or brain injur* or stroke or post-stroke or concussion or polyneuropath* or fibromyalgia or multiple sclerosis or arteriosclerosis or cancer or neoplasm* or malignanc* or degenerative or “return to sport” or claudication or epidural or platelet-rich plasma or cadaver or spinal cord or spinal chord or vibration or arterial disease or caffeine or pregnan* or breast or breasts or steroid* ) OR TI ( (after or undergoing) n5 reconstruction)
-
S17
PT review OR PT (conference proceeding)
-
S18
SO “case report*” or “case stud*”
-
S19
TI ((case NOT (case control or case cohort or case crossover)) n4 (series or study or report*))
-
S20
S15 NOT (S16 OR S17 OR S18 OR S19)
e. Scopus
( ( ( ( ( TITLE-ABS-KEY ( athlet* OR players OR sport OR sports OR rugby OR netball* OR basketball* OR hockey OR volleyball OR skiers OR snowboard* OR soccer OR football* OR lacrosse OR rowers OR gymnasts OR “figure skaters” OR dancers OR tennis ) OR TITLE-ABS-KEY ( runners OR marathoners OR joggers OR police* OR officer* OR firefighter* OR firem* OR “fire personnel” OR military OR army OR navy OR “air force” OR airforce OR soldier* OR “armed forces” OR “armed service*” OR “active duty*” OR veteran* OR paramedic* ) OR TITLE-ABS-KEY ( “first responder*” OR ambulance OR “emergency medical technician*” ) OR TITLE-ABS-KEY ( ( active W/3 ( individual* OR population* OR participant* OR male* OR female* OR men OR women OR persons OR students OR adult* OR patients OR adolescent* ) ) ) ) ) AND ( ( TITLE-ABS-KEY ( ( ( injur* OR pain* OR tear OR tears OR sprain* OR strain* OR dislocation* OR impingement* OR instability ) W/6 ( risk OR risks OR predict* OR associat* OR correlat* OR screen* OR prevent* OR sport* OR athletic OR running ) ) ) OR TITLE-ABS-KEY ( ( ( injur* OR pain* OR tear OR tears OR sprain* OR strain* OR dislocation* OR impingement* OR instability ) W/8 ( “lower extremit*” OR “lower limb*” OR hip OR hips OR thigh OR thighs OR leg OR legs OR knee OR knees OR ankle* OR foot OR foots OR toe OR toes ) ) ) OR TITLE-ABS-KEY ( ( ( injur* OR pain* OR tear OR tears OR sprain* OR strain* OR dislocation* OR impingement* OR instability ) W/8 ( acl OR pcl OR “cruciate ligament*” OR femoracetabular OR femur OR tibia* OR patellofemoral OR patella ) ) ) ) ) AND ( ( ( ( TITLE-ABS-KEY ( “lower extremit*” OR “lower limb*” OR hip OR hips OR thigh OR thighs OR leg OR legs OR knee OR knees OR ankle* OR foot OR foots OR toe OR toes OR acl OR pcl OR “cruciate ligament*” OR femoracetabular OR femur OR tibia* OR patell* ) OR TITLE-ABS-KEY ( run OR running OR jog* OR squat* OR lunge OR lunges OR hop OR jump OR jumping OR walk OR walking OR step-up OR hurdle OR gait ) ) ) AND ( ( TITLE-ABS-KEY ( motor OR movement OR motion OR dynamic OR moving OR exercise ) OR TITLE-ABS-KEY ( ( physical W/1 ( activit* OR perform* OR function* ) ) ) OR TITLE-ABS-KEY ( ( function* W/1 ( activ* OR perform* ) ) ) OR TITLE-ABS-KEY ( run OR running OR jog* OR squat* OR minisquat* OR balance OR lunge OR lunges OR hop OR jump OR jumping OR walk OR walking OR step-up OR hurdle OR gait ) ) ) AND ( ( TITLE-ABS-KEY ( “functional test*” OR grade OR grading OR rating OR rated OR score OR scoring OR RANK OR ranked OR ranking ) OR TITLE-ABS-KEY ( movement W/2 ( screen* OR assess* OR quality OR performance OR observation OR observe* OR test* ) ) OR TITLE-ABS-KEY ( ( performance OR objective OR observation* OR quality OR control ) W/5 ( measur* OR test* OR instrument* OR method OR methods OR INDEX OR indices OR assess* OR screen* ) ) OR TITLE-ABS-KEY ( ( deficit* OR varus OR valgus OR asymmetr* OR “compensatory movement” ) AND ( measur* OR test* OR instrument* OR method OR methods OR INDEX OR indices OR assess* OR screen* ) ) ) ) ) OR ( ( TITLE-ABS-KEY ( ( lunge OR squat OR hop OR jump OR reach OR cutting OR step-up OR balance OR push-up OR lift OR rotation OR walk* ) W/3 ( test* OR task* OR assessment ) ) OR TITLE-ABS-KEY ( “gait analys*” OR “gait evaluation*” OR “deep squat*” OR “one leg squat*” OR mini-squat* OR “mini squat*” OR “in line lunge*” OR “inline lunge*” OR “double leg drop” OR “hop and hold*” OR “Hurdle step*” ) OR TITLE-ABS-KEY ( “single leg pickup” OR “single leg pick-up” OR “single leg land” OR “single leg balance” OR “leg raise” OR “tuck jump” OR “vertical jump” OR “drop jump” OR “functional movement screen*” OR “landing error scoring system*” ) OR TITLE-ABS-KEY ( “balance error scoring system*” OR ppm-16 ) OR ( ( nine-test OR movement OR performance OR function ) n3 “screening battery” ) ) ) ) ) AND ( ( ( TITLE ( predict* OR associat* OR correlat* ) OR TITLE-ABS-KEY ( “discriminant analys*” OR “health status indicators” OR “health indicators” OR “predictive value” OR “receiver operator curve*” OR roc OR “likelihood ratio*” OR specificity ) OR TITLE-ABS-KEY ( ( predict* OR correlat* OR associat* ) W/10 ( injur* OR pain* OR tear OR tears OR sprain* OR strain* OR dislocation* OR impingement* OR instability ) ) OR TITLE-ABS-KEY ( ( positive* OR negative* OR high* OR low ) W/4 correlat* ) OR TITLE-ABS-KEY ( “observer variation*” OR instrumentation OR psychometr* OR clinimetr* OR clinometr* OR reproducib* OR reliab* OR unreliab* OR valid* OR coefficient OR homogeneity OR homogeneous OR “internal consistency” ) ) ) OR ( ( TITLE-ABS-KEY ( item W/5 ( correlation* OR selection* OR reduction* ) ) OR TITLE-ABS-KEY ( “cronbach* alpha” OR agreement OR precision OR imprecision OR “precise value*” OR test-retest OR ( test W/3 retest ) ) OR TITLE-ABS-KEY ( interrater OR inter-rater OR intrarater OR intra-rater OR intertester OR inter-tester OR intratester OR intra-tester OR interobserver OR inter-observer OR intraobserver OR intraobserver OR intertechnician OR intertechnician OR intratechnician ) OR TITLE-ABS-KEY ( intra-technician OR interexaminer OR inter-examiner OR intraexaminer OR intra-examiner OR interassay OR inter-assay OR intraassay OR intra-assay OR interindividual OR inter-individual OR intraindividual ) OR TITLE-ABS-KEY ( intra-individual OR interparticipant OR inter-participant OR intraparticipant OR intra-participant ) ) ) OR ( ( TITLE-ABS-KEY ( ( replicab* OR repeated ) W/6 ( measure OR measures OR findings OR result OR results OR test OR tests ) ) OR TITLE-ABS-KEY ( kappa* OR repeatab* OR generaliza* OR generalisa* OR concordance OR ( intraclass AND correlation* ) ) OR TITLE-ABS-KEY ( discriminative OR “known group” OR “factor analysis” OR “factor analyses” OR dimension* OR subscale* ) OR TITLE-ABS-KEY ( multitrait W/6 scaling W/6 analys* ) OR TITLE-ABS-KEY ( “item discriminant” OR “interscale correlation*” OR “individual variability” OR “standard error of measurement” OR sensitiv* OR responsive* ) OR TITLE-ABS-KEY ( ( minimal OR minimally OR clinical OR clinically OR mall* ) W/6 ( important OR significant OR detectable OR real ) W/6 ( change OR difference ) ) OR TITLE-ABS-KEY ( “meaningful change” OR “ceiling effect” OR “floor effect” OR “item response model” OR irt OR rasch OR “Differential item functioning” OR dif OR “computer adaptive testing” OR “item bank” OR “cross-cultural equivalence” ) ) ) ) ) AND NOT ( ( TITLE ( mice OR mouse OR rat OR rats OR animal model* OR bovine OR rodent* ) OR TITLE ( arthroplast* OR arthroscop* OR tka OR tha OR surgery OR surgical OR paraplegi* OR brain injur* OR stroke OR post-stroke OR concussion OR polyneuropath* OR fibromyalgia OR “multiple sclerosis” ) OR TITLE ( arteriosclerosis OR cancer OR neoplasm* OR malignanc* OR degenerative OR “return to sport” OR claudication OR epidural OR platelet-rich plasma OR cadaver OR spinal cord OR spinal chord OR vibration OR arterial disease OR caffeine OR pregnan* OR breast ) OR TITLE ( ( after OR undergoing ) n5 reconstruction ) ) ) ) AND NOT ( ( TITLE ( “case report” OR “case study” OR “case series” ) AND KEY ( “case report” OR “case study” OR “case series” ) AND SRCTITLE ( “case report*” OR “case stud*” ) ) ) AND ( LIMIT-TO ( LANGUAGE, “English” ) ) AND ( EXCLUDE ( DOCTYPE, “re” ) OR EXCLUDE ( DOCTYPE, “cp” ) OR EXCLUDE ( DOCTYPE, “cr” ) )
RESULTS
| Database | Date searched | # of results |
|---|---|---|
| Medline | Jan 5, 2016 | 1716 |
| CINAHL | Jan 5, 2016 | 1329 |
| EMBASE | Jan 5, 2016 | 1505 |
| SportDiscus | Jan 5, 2016 | 1497 |
| Scopus | Jan 5, 2016 | 2172 |
| Total | 8219 |
APPENDIX 2: DOWN’S AND BLACK QUALITY ASSESSMENT CRITERIA SCORED FOR INCLUDED STUDIES
| Item | Score | |
|---|---|---|
| 1 | Is the hypothesis/aim/objective of the study clearly described? | yes=1; no=0 |
| 2 | Are the main outcomes to be measured clearly described in the Introduction or Methods section? | yes=1; no=0 |
| 3 | Are the characteristics of the patients included in the study clearly described? | yes=1; no=0 |
| 4 | * Are the interventions of interest clearly described? | yes=1; no=0 |
| 5 | Are the distributions of principal confounders in each group of subjects to be compared clearly described? | yes=2; partially=1; no=0 |
| 6 | Are the main findings of the study clearly described? | yes=1; no=0 |
| 7 | Does the study provide estimates of the random variability in the data for the main outcomes? | yes=1; no=0 |
| 8 | * Have all important adverse events that may be a consequence of the intervention been reported? | yes=1; no=0 |
| 9 | Have the characteristics of patients lost to follow-up been described? | yes=1; no=0 |
| 10 | Have actual probability values been reported (e.g. 0.035 rather than <0.05) for the main outcomes except where the probability value is less than 0.001? | yes=1; no=0 |
| 11 | Were the subjects asked to participate in the study representative of the entire population from which they were recruited? | yes=1; no=0 |
| 12 | Were those subjects who were prepared to participate representative of the entire population from which they were recruited? | yes=1; no=0 |
| 13 | Were the staff, places, and facilities where the patients were treated, representative of the treatment the majority of patients receive? | yes=1; no=0 |
| 14 | * Was an attempt made to blind study subjects to the intervention they have received? | yes=1; no=0 |
| 15 | Was an attempt made to blind those measuring the main outcomes of the intervention? | yes=1; no=0 |
| 16 | If any of the results of the study were based on “data dredging”, was this made clear? | yes=1; no=0 |
| 17 | In trials and cohort studies, do the analyses adjust for different lengths of follow-up of patients, or in case-control studies, is the time period between the intervention and outcome the same for cases and controls? | yes=1; no=0 |
| 18 | Were the statistical tests used to assess the main outcomes appropriate? | yes=1; no=0 |
| 19 | * Was compliance with the intervention/s reliable? | yes=1; no=0 |
| 20 | Were the main outcome measures used accurate (valid and reliable)? | yes=1; no=0 |
| 21 | Were the patients in different intervention groups (trials and cohort studies) or were the cases and controls (case-control studies) recruited from the same population? | yes=1; no=0 |
| 22 | Were study subjects in different intervention groups (trials and cohort studies) or were the cases and controls (case-control studies) recruited over the same period of time? | yes=1; no=0 |
| 23 | * Were study subjects randomized to intervention groups? | yes=1; no=0 |
| 24 | * Was the randomized intervention assignment concealed from both patients and health care staff until recruitment was complete and irrevocable? | yes=1; no=0 |
| 25 | Was there adequate adjustment for confounding in the analyses from which the main findings were drawn? | yes=1; no=0 |
| 26 | Were losses of patients to follow-up taken into account? | yes=1; no=0 |
| 27 | * Did the study have sufficient power to detect a clinically important effect where the probability value for a difference being due to chance is less than 5%? | Size of smallest intervention group: <n1=0; n1-n2=1; n3-n4=2; n5-n6=3; n7-n8=4; n8+=5 |
Items 1–10 = reporting, 11–13 = external validity, 14–20 = internal validity (bias), 21–26 = internal validity (confounding) and 27 = power.
not applicable to observational studies.
APPENDIX 3: LEVELS OF EVIDENCE ADAPTED FROM THE OXFORD CENTRE FOR EVIDENCE-BASED MEDICINE MODEL 200916
| Level | Description | |
|---|---|---|
| 1 | a | Systematic reviews (with homogeneity) of randomized controlled trials |
| b | Individual randomized controlled trials (with narrow confidence intervals) | |
| c | All or none randomized controlled trials | |
| 2 | a | Systematic reviews (with homogeneity) of cohort studies |
| b | Individual cohort study or low quality randomized controlled trials (e.g. <80% follow-up) | |
| c | “Outcomes” research; ecological studies | |
| 3 | a | Systematic review (with homogeneity) of case-control studies |
| b | Individual case-control study | |
| c | Cross-sectional studies | |
| 4 | Case-series (and poor quality cohort and case-control studies) | |
| 5 | Expert opinion without explicit critical appraisal, or based on physiology, bench research or “first principles” | |
Footnotes
AUTHORS CONTRIBUTIONS
JW, CE, NB and DW were responsible for the conception of the study while all authors were involved in study design. LD designed and executed the extensive search strategy. All authors (except LD) independently reviewed the literature, participated in rating the literature and extracted data. JW was the primary author in preparing the manuscript however all authors contributed to the interpretation of the findings, critical revision of the manuscript and reviewed the document prior to submission.
COMPETING INTERESTS
The authors acknowledge that they have no conflicts of interest that are directly relevant to the contents of this systematic review.
Contributor Information
Jackie L Whittaker, Department of Physical Therapy, Faculty of Rehabilitation Medicine, University of Alberta, 2-50 Corbett Hall, 8205-114 Street, Edmonton, Canada T6G 2G4. Glen Sather Sports Medicine Clinic, University of Alberta, Edmonton, Canada.
Nadine Booysen, Faculty of Health Sciences, University of Southampton, Southampton, UK. Arthritis Research UK Centre for Exercise, Sport and Osteoarthritis.
Sarah de la Motte, Constortium for Health and Military Performance, Uniformed Services University of the Health Sciences, Bethesda, Maryland, USA.
Liz Dennett, John W. Scott Health Sciences Library, University of Alberta.
Cara L. Lewis, Department of Physical Therapy and Athletic Training, College of Health and Rehabilitation Sciences, Sargent College, Boston University, Boston, Massachusetts, USA.
Dave Wilson, Faculty of Health Sciences, University of Southampton, Southampton, UK. Arthritis Research UK Centre for Exercise, Sport and Osteoarthritis.
Carly McKay, Department for Health, Bath University, Bath UK. Arthritis Research UK Centre for Exercise, Sport and Osteoarthritis.
Martin Warner, Faculty of Health Sciences, University of Southampton, Southampton, UK. Arthritis Research UK Centre for Exercise, Sport and Osteoarthritis.
Darin Padua, Department of Exercise and Sport Science, University of North Carolina, Chapel Hill NC, USA.
Carolyn A Emery, Sport Injury Prevention Research Centre, Faculty of Kinesiology, Alberta Children’s Hospital Research Institute, Department of Pediatrics and Department of Community Health Sciences, Cumming School of Medicine, University of Calgary, Calgary, Canada.
Maria Stokes, Faculty of Health Sciences, University of Southampton, Southampton, UK. Arthritis Research UK Centre for Exercise, Sport and Osteoarthritis.
References
- 1.Roos EM, Arden NK. Strategies for the prevention of knee osteoarthritis. Nat Rev Rheumatol. 2016;12(2):92–101. doi: 10.1038/nrrheum.2015.135. [DOI] [PubMed] [Google Scholar]
- 2.Pons-Villanueva J, Segui-Gomez M, Martinez-Gonzalez MA. Risk of injury according to participation in specific physical activities: a 6-year follow-up of 14 356 participants of the SUN cohort. Int J Epidemiol. 2010;39(2):580–7. doi: 10.1093/ije/dyp319. [DOI] [PubMed] [Google Scholar]
- 3.Andersen KA, Grimshaw PN, Kelso RM, et al. Musculoskeletal Lower Limb Injury Risk in Army Populations. Sports Med Open. 2016;2:22. doi: 10.1186/s40798-016-0046-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Songer TJ, LaPorte RE. Disabilities due to injury in the military. Am J Prev Med. 2000;18(3 Suppl):33–40. doi: 10.1016/s0749-3797(00)00107-0. [DOI] [PubMed] [Google Scholar]
- 5.van Mechelen W, Hlobil H, Kemper HC. Incidence, severity, aetiology and prevention of sports injuries. A review of concepts. Sports Med. 1992;14(2):82–99. doi: 10.2165/00007256-199214020-00002. published Online First: 1992/08/01. [DOI] [PubMed] [Google Scholar]
- 6.Finch C. A new framework for research leading to sports injury prevention. J Sci Med Sport. 2006;9(1–2):3–9. doi: 10.1016/j.jsams.2006.02.009. discussion 10. [DOI] [PubMed] [Google Scholar]
- 7.Meeuwisse WH, Tyreman H, Hagel B, et al. A dynamic model of etiology in sport injury: the recursive nature of risk and causation. Clin J Sport Med. 2007;17(3):215–9. doi: 10.1097/JSM.0b013e3180592a48. [DOI] [PubMed] [Google Scholar]
- 8.Bahr R, Holme I. Risk factors for sports injuries--a methodological approach. Br J Sports Med. 2003;37(5):384–92. doi: 10.1136/bjsm.37.5.384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bahr R. Why screening tests to predict injury do not work-and probably never will: a critical review. Br J Sports Med. 2016;50(13):776–80. doi: 10.1136/bjsports-2016-096256. [DOI] [PubMed] [Google Scholar]
- 10.Hegedus EJ, McDonough S, Bleakley C, et al. Clinician-friendly lower extremity physical performance measures in athletes: a systematic review of measurement properties and correlation with injury, part 1. The tests for knee function including the hop tests. Br J Sports Med. 2015;49(10):642–8. doi: 10.1136/bjsports-2014-094094. [DOI] [PubMed] [Google Scholar]
- 11.Hegedus EJ, McDonough SM, Bleakley C, et al. Clinician-friendly lower extremity physical performance tests in athletes: a systematic review of measurement properties and correlation with injury. Part 2—the tests for the hip, thigh, foot and ankle including the star excursion balance test. Br J Sports Med. 2015 doi: 10.1136/bjsports-2014-094341. [DOI] [PubMed] [Google Scholar]
- 12.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-Aanalyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Med. 2009;6(7):1–28. doi: 10.1371/journal.pmed.1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kroman SL, Roos EM, Bennell KL, et al. Measurement properties of performance-based outcome measures to assess physical function in young and middle-aged people known to be at high risk of hip and/or knee osteoarthritis: a systematic review. Osteoarthritis Cartilage. 2014;22(1):26–39. doi: 10.1016/j.joca.2013.10.021. [DOI] [PubMed] [Google Scholar]
- 14.VonVille HM. [accessed January 1, 2016];Excel Workbooks for Systematic Reviews. 2015 [Available from: http://libguides.sph.uth.tmc.edu/excel_workbook_home.
- 15.Viera AJ, Garrett JM. Understanding interobserver agreement: the kappa statistic. Family Med. 2005;37(5):360–3. [PubMed] [Google Scholar]
- 16.Downs S, Black N. The feasibility of creating a checklist for the assessment of the methodolical quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52:377–84. doi: 10.1136/jech.52.6.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Howick J, Phillips B, Ball C, et al. [accessed June 23 2014];Oxford Centre for Evidence-based Medicine: Levels of evidence. 2009 [Available from: http://www.cebm.net/oxford-centre-evidence-based-medicine-levels-evidence-march-2009/
- 18.Azzam MG, Throckmorton TW, Smith RA, et al. The Functional Movement Screen as a predictor of injury in professional basketball players. Curr Orthop Pract. 2015;26:619–23. [Google Scholar]
- 19.Bardenett SM, Micca JJ, DeNoyelles JT, et al. Functional Movement Screen Normative Values and Validity in High School Athletes: Can the Fmstm Be Used as a Predictor of Injury? Int J Sports Phys Ther. 2015;10:303–08. [PMC free article] [PubMed] [Google Scholar]
- 20.Bushman TT, Grier TL, Canham-Chervak M, et al. Pain on Functional Movement Screen Tests and Injury Risk. J Strength Cond Res. 2015;29(Suppl 11):S65–70. doi: 10.1519/JSC.0000000000001040. [DOI] [PubMed] [Google Scholar]
- 21.Butler RJ, Contreras M, Burton LC, et al. Modifiable risk factors predict injuries in firefighters during training academies. Work. 2013;46:11–17. doi: 10.3233/WOR-121545. [DOI] [PubMed] [Google Scholar]
- 22.Chorba RS, Chorba DJ, Bouillon LE, et al. Use of a functional movement screening tool to determine injury risk in female collegiate athletes. N Am J Sports Phys Ther. 2010;5:47–54. [PMC free article] [PubMed] [Google Scholar]
- 23.Garrison M, Westrick R, Johnson MR, et al. Association between the functional movement screen and injury development in college athletes. Int J Sports Phys Ther. 2015;10:21–28. [PMC free article] [PubMed] [Google Scholar]
- 24.Kiesel K, Plisky PJ, Voight ML. Can Serious Injury in Professional Football be Predicted by a Preseason Functional Movement Screen? N Am J Sports Phys Ther. 2007;2:147–58. [PMC free article] [PubMed] [Google Scholar]
- 25.Kiesel KB, Butler RJ, Plisky PJ. Prediction of injury by limited and asymmetrical fundamental movement patterns in american football players. J Sport Rehabil. 2014;23(2):88–94. doi: 10.1123/jsr.2012-0130. [DOI] [PubMed] [Google Scholar]
- 26.Knapik JJ, Cosio-Lima L, Reynolds KL, et al. Efficacy of functional movement screening for predicting injuries in coast guard cadets. J Strength Cond Res. 2015;29:1157–62. doi: 10.1519/JSC.0000000000000704. [DOI] [PubMed] [Google Scholar]
- 27.Lisman P, O’Connor FG, Deuster PA, et al. Functional movement screen and aerobic fitness predict injuries in military training. Med Sci Sports Exer. c2013;45(4):636–43. doi: 10.1249/MSS.0b013e31827a1c4c. [DOI] [PubMed] [Google Scholar]
- 28.Padua DA, DiStefano LJ, Beutler AI, et al. The Landing Error Scoring System as a Screening Tool for an Anterior Cruciate Ligament Injury-Prevention Program in Elite-Youth Soccer Athletes. J Athl Train. 2015;50(6):589–95. doi: 10.4085/1062-6050-50.1.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Warren M, Smith CA, Chimera NJ. Association of the Functional Movement Screen with injuries in division I athletes. J Sport Rehabil. 2015;24(2):163–70. doi: 10.1123/jsr.2013-0141. [DOI] [PubMed] [Google Scholar]
- 30.Wiese BW, Boone JK, Mattacola CG, et al. Determination of the Functional Movement Screen to Predict Musculoskeletal Injury in Intercollegiate Athletics. Athl Train Sports Health Care. 2014;6:161–69 9p. doi: 10.3928/19425864-20140717-01. [DOI] [Google Scholar]
- 31.Dossa K, Cashman G, Howitt S, et al. Can injury in major junior hockey players be predicted by a pre-season functional movement screen - a prospective cohort study. J Can Chiropr Assoc. 2014;58:421–27. [PMC free article] [PubMed] [Google Scholar]
- 32.Shojaedin SS, Letafatkar A, Hadadnezhad M, et al. Relationship between functional movement screening score and history of injury and identifying the predictive value of the FMS for injury. Int J Inj Contr Saf Promot. 2014;21:355–60. doi: 10.1080/17457300.2013.833942. [DOI] [PubMed] [Google Scholar]
- 33.Hotta T, Nishiguchi S, Fukutani N, et al. Functional Movement Screen for Predicting Running Injuries in 18- to 24-Year-Old Competitive Male Runners. J Strength Cond Res. 2015;29:2808–15. doi: 10.1519/JSC.0000000000000962. [DOI] [PubMed] [Google Scholar]
- 34.Smith HC, Johnson RJ, Shultz SJ, et al. A prospective evaluation of the Landing Error Scoring System (LESS) as a screening tool for anterior cruciate ligament injury risk. Am J Sports Med. 2012;40:521–26. doi: 10.1177/0363546511429776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kazman JB, de la Motte S, Gribbin TC, et al. Improving physical performance tests: time to include a psychologist. Br J Sports Med. 2016 doi: 10.1136/bjsports-2015-095407. [DOI] [PubMed] [Google Scholar]
- 36.Cook G, Burton L, Hoogenboom B. Pre-participation screening: the use of fundamental movements as an assessment of function - part 2. N Am J Sports Phys Ther. 2006;1(3):132–9. [PMC free article] [PubMed] [Google Scholar]
- 37.Dossa K, Cashman G, Howitt S, et al. Can injury in major junior hockey players be predicted by a pre-season functional movement screen - a prospective cohort study. J Can Chiropr Assoc. 2014;58:421–27 7p. [PMC free article] [PubMed] [Google Scholar]
- 38.Engebretsen AH, Myklebust G, Holme I, et al. Prevention of injuries among male soccer players: a prospective, randomized intervention study targeting players with previous injuries or reduced function. Am J Sports Med. 2008;36(6):1052–60. doi: 10.1177/0363546508314432. [DOI] [PubMed] [Google Scholar]
- 39.Holmich P, Larsen K, Krogsgaard K, et al. Exercise program for prevention of groin pain in football players: a cluster-randomized trial. Scand J Med Sci Sports. 2010;20(6):814–21. doi: 10.1111/j.1600-0838.2009.00998.x. [DOI] [PubMed] [Google Scholar]
- 40.Frohm A, Heijne A, Kowalski J, et al. A nine-test screening battery for athletes: a reliability study. Scand J Med Sci Sports. 2012;22(3):306–15. doi: 10.1111/j.1600-0838.2010.01267.x. [DOI] [PubMed] [Google Scholar]
- 41.Mischiati CR, Comerford M, Gosford E, et al. Intra and inter-rater reliability of screening for movement impairments: movement control tests from the foundation matrix. J Sports Sci Med. 2015;14(2):427–40. [PMC free article] [PubMed] [Google Scholar]
- 42.Ageberg E, Bennell KL, Hunt MA, et al. Validity and inter-rater reliability of medio-lateral knee motion observed during a single-limb mini squat. BMC Musculoskelet Disord. 2010;11:265. doi: 10.1186/1471-2474-11-265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Junge T, Balsnes S, Runge L, et al. Single leg mini squat: an inter-tester reproducibility study of children in the age of 9–10 and 12–14 years presented by various methods of kappa calculation. BMC Musculoskelet Disord. 2012;13:203. doi: 10.1186/1471-2474-13-203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Botha NWW, Gimpel M, Mottram S, Comerford M, Stokes M. Movement patterns during a small knee bend test in academy footballers with femoroacetabular impingement (FAI) Working Paper Health Sci. 2014;1(10):1–10. [Google Scholar]
- 45.McCunn R, Aus der Funten K, Fullagar HH, et al. Reliability and Association with Injury of Movement Screens: A Critical Review. Sports Med. 2016;46(6):763–81. doi: 10.1007/s40279-015-0453-1. [DOI] [PubMed] [Google Scholar]
- 46.Fuller CW, Ekstrand J, Junge A, et al. Consensus statement on injury definitions and data collection procedures in studies of football (soccer) injuries. Br J Sports Med. 2006;40(3):193–201. doi: 10.1136/bjsm.2005.025270. [DOI] [PMC free article] [PubMed] [Google Scholar]