Abstract
The literature on the contribution of kerosene lighting to indoor air particulate concentrations is sparse. In rural Uganda, kitchens are almost universally located outside the main home, and kerosene is often used for lighting. In this study, we obtained longitudinal measures of particulate matter 2.5 microns or smaller in size (PM2.5) from living rooms and kitchens of 88 households in rural Uganda. Linear mixed effects models with a random intercept for household were used to test the hypotheses that primary reported lighting source and kitchen location (indoor vs. outdoor) is associated with PM2.5 levels. During initial testing, households reported using the following sources of lighting: open wick kerosene (19.3%), hurricane kerosene (45.5%), battery powered (33.0%), and solar (1.1%) lamps. During follow-up testing these proportions changed to 29.5%, 35.2%, 18.2%, and 9.1%, respectively. Average ambient, living room, and kitchen PM2.5 levels were 20.2, 35.2, and 270.0 μg/m3. Living rooms using open wick kerosene lamps had the highest PM2.5 levels (55.3 μg/m3) compared to those using solar lighting (19.4 μg/m3; open wick vs. solar, p = 0.01). 27.6% of homes using open wick kerosene lamps met World Health Organization indoor air quality standards compared to 75.0% in homes using solar lighting.
INTRODUCTION
Indoor air pollution from solid fuel use leads to 3.9 million premature deaths a year globally1, and is one of the most important environmental risk factors contributing to the global burden of pulmonary, cardiovascular, and cerebrovascular disease2. In low and middle income countries like Uganda, over 95% of the population relies on biomass fuel for heating, cooking, and lighting3, with women and children disproportionately affected due to the time spent indoors during high exposure activities4, 5. Particulate matter, a component of indoor air pollution, is thought to be associated with adverse acute and long term respiratory effects including an increased risk of acute respiratory infections, chronic obstructive pulmonary disease, and lung cancer6, 7. For example, a dose-response relationship between indoor particulate levels and acute respiratory infections has been identified in rural Kenya8, whereas a recent cross-sectional study in rural Uganda has also identified a high prevalence of early onset chronic obstructive pulmonary disease in women, with exposure to biomass smoke being the major risk factor9.
However, attempts to reduce indoor air pollution in resource-limited settings by reducing emissions from cookstoves have not been successful. A randomized controlled trial in Guatemala10 of improved wood stoves with a chimney vs. traditional open fires did not show a statistically significant decrease in the primary outcome of physician-diagnosed pneumonia, although there were significant reductions in carbon monoxide levels (as a surrogate measure of particulate matter levels) and fieldworker assessed severe pneumonia. A recent large randomized controlled trial of cleaner cookstoves in Malawi also failed to demonstrate a reduction in childhood pneumonia11. Other randomized trials of improved cookstoves in Ghana12 and Rwanda13 did not find a significant reduction in indoor air pollution; one explanatory factor may be poor compliance with use of the improved cookstoves. A field test of improved cookstoves in rural India did find reductions in indoor particulate matter and carbon monoxide concentrations. However, no improved cookstove was able to achieve reductions in indoor air pollution to levels below 25 μg/m3.14 Although there is no clear “safe” threshold for PM2.5 exposure, 25 μg/m3 is an interim target for 24-hour averaged PM2.5 exposure deemed acceptable by the World Health Organization (WHO)15. This measure, however, does not accurately reflect PM2.5 levels at peak exposure that may be independently associated with acute health effects.
In contrast, kerosene used for lighting has not received significant attention as a contributor to indoor particulate levels. Studies in this area are limited, and particularly lacking when it comes to defining the contribution of kerosene lighting to indoor levels of fine particulate matter (particulate matter 2.5 microns and smaller in size, or PM2.5). A recent review of available studies in the literature16 found mostly experimental chamber studies which demonstrate that kerosene lamps, particularly simple wick lamps, often lead to emissions of indoor PM 2.5 that exceed WHO recommended standards17.
In rural Uganda, the kitchen is almost always located outside of the main home, typically in a separate structure or outdoors. Concurrently, there is a heavy reliance on kerosene for indoor lighting. The primary aim of this epidemiologic study was to determine whether reported primary lighting source was associated with indoor PM2.5 levels in the main home.
METHODS
Study population
We recruited women living in rural villages in Nyakabare Parish located in southwest Uganda. A survey of all households in Nyakabare parish was previously conducted as part of an ongoing population-based study evaluating the effect of different social, policy, and economic interventions. None of the households in this area are connected to the national electrical grid. For this sub-study, we first held a series of community meetings with the village health teams, district health officials, and village leaders in order to explain the purpose of the project and to demonstrate the air sampling equipment. Trained fieldworkers were then paired with research nurses and a member of the village health team to visit a subsample of homes and obtain informed consent to participate in this study. 88 women from distinct households located in 7 village cells were enrolled.
Indoor environment assessment
Trained research assistants first conducted a walk-through of each home. Characteristics of the home including location of the kitchen, type of fuel used, type of indoor lighting, and materials used in home construction were recorded on a standardized questionnaire. A kitchen was considered to be indoors if it was located in a structure that had at least three walls. Kerosene lamps were categorized as either open wick lamps or hurricane lamps (see Figure 1).
FIGURE 1.
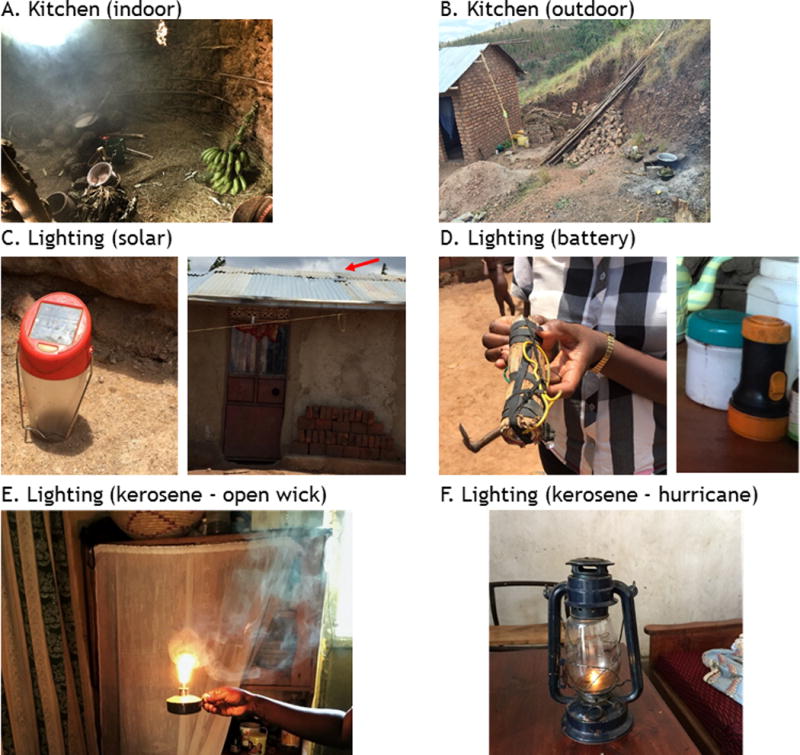
Sources of indoor air pollution in rural Ugandan home. A. Typical indoor kitchen. B. Typical outdoor kitchen. C. Solar lighting, with solar lantern (left) or solar panel (right), see red arrow. D. Battery-powered light. (left) Homemade flashlight composed of batteries wrapped in a banana leaf and rubber strip, with attached wiring and light bulb (left) vs. commercially available flashlight (right). E. Open wick kerosene lamp (locally referred to as a “tadooba”). F. Hurricane kerosene lamp.
Exposure assessment
Repeated measures of kitchen and living room PM2.5 levels were obtained from 88 homes during two different time periods: between July and October of 2015, and between March and July of 2016, during which time weather and daylight hours were similar. Of note, this area has two rainy seasons. The first runs from March to May and the second from September to November. In order to obtain measures of ambient air pollution, repeated measures of PM2.5 were also obtained during these periods from the public meeting places in each of the 7 villages, i.e., a centrally located outdoor location in each village.
24-hour integrated PM2.5 levels were obtained using a compact multistage cascade impactor18 with two 2.5 μm cutpoints. Particles larger than the cutpoint are collected onto polyurethane foam as an impaction substrate at each impactor stage, allowing for particles smaller than 2.5 μm to be collected onto a final 37 mm, 2.0 μm pore size Teflon filter (Pall Life Sciences; Teflo). The sampler was attached to a custom-built battery-powered pump operating at 5 liters per minute. Flow was measured by a flowmeter (Omron D6F-P), with flow and time of use data recorded onto a datalogger (HOBO UX120 4-Channel Analog Logger). Samplers were positioned 4 feet above ground level. In kitchens, samplers were placed one meter from the cooking fire. In living rooms, pumps were placed in the center of the room; because lighting sources such as lamps were moved by participants at night, we were unable to place samplers at a consistent distance from the lighting source. All collected environmental samples were labelled with a unique identifier, and details of sample collection were recorded onto a standardized field log.
Filters were conditioned in a temperature and humidity controlled environment for at 48 hours prior to weighing on an electronic microbalance (MT-5 Mettler Toledo) in Boston, Massachusetts. This was done prior to sample collection and after sample collection in order to calculate PM2.5 mass. The concentration of PM2.5 was calculated by dividing the change in filter weight by the volume of air sampled to give a final concentration in micrograms per cubic meter. Following gravimetric measurement, Teflon filters from living rooms were analyzed for indoor black carbon (BC) concentrations by measuring filter blackness using a smoke stain reflectometer (model EEL M43D, Diffusion Systems). We used the standard black-smoke index calculations of the absorption coefficients based on reflectance19. We assumed a factor of 1.0 for converting the absorption coefficient to BC mass20, 21, which was then divided by the sampled air volume to calculate average BC exposure concentration.
Field blanks were used to account for potential bias in filter weight due to sampling methods. Average net weights of field blank samples were negligible (mean 0.009 ± 0.005 mg), thus we did not blank correct our samples.
Questionnaire
To assess respiratory symptoms, trained research assistants administered a modified version of the American Thoracic Society Questionnaire in Runyankole, the local language. Additionally, questions regarding demographics, household assets, cooking practices, primary lighting source, time use, and health of children in the household were also obtained.
Statistical analysis
Summary measures of PM2.5 by location were calculated. In unadjusted analyses, the Kruskal-Wallis test was used to determine differences in PM2.5 levels by location (outdoor, living room, kitchen) and by lighting source. In adjusted analyses, linear mixed effects models were used, with a random intercept for household to adjust for repeated measures of PM2.5 levels in the same home. PM2.5 level were natural log-transformed to account for the skewed distribution, and a categorical variable for sampling phase was used to adjust for seasonal trends. In order to adjust for household wealth as a potential confounder between lighting and indoor PM2.5 levels, we calculated an asset-based index for household wealth that has been validated for use in resource-limited settings.22 This index is based on a series of 19 survey questions regarding both household assets and housing characteristics (e.g., number of plots of land owned, whether a household member owns a radio, whether the home has a cement floor, etc.). In order to test the hypothesis that PM2.5 levels differed by location, a categorical variable for location (outdoor, living room, kitchen) was used. To test the hypothesis that kitchen PM2.5 levels differed between indoor and outdoor kitchens, the kitchen indicator variable was further subdivided by kitchen location (indoor vs. not indoor), adjusting for sampling phase. To test the hypothesis that living room PM2.5 and black carbon levels differed based on reported primary lighting source, the living room indicator variable was further subdivided by lighting source (solar, battery, hurricane lamp, open wick lamp). Sampling phase, use of a secondary stove in the main home, and household wealth were included as covariates. All statistical analyses were performed in R 3.3.0; the R packages nlme23 and ggplot224 were used for mixed effects models and plotting, respectively. Two-sided p-values of <0.05 were considered statistically significant.
Ethics
Written informed consent to participate in this study was obtained from all participants. The study was given ethical approval by the Research Ethics Committee of the Mbarara University of Science and Technology, the Partners Human Research Committee, and the Office of Human Research Administration at the Harvard T.H. Chan School of Public Health. Consistent with local guidelines, we also obtained clearance for the study from the Ugandan National Council for Science and Technology and the Research Secretariat in the Office of the President.
RESULTS
This study included 88 women from distinct households. The average age was 36.2 ± 9.0 years old, and 81 (92.0%) reported farming as their primary occupation. On average, participants spent 15.0 ± 2.8 hours indoors per day, of which 3.4 ± 1.4 hours were spent next to the cooking fire. Participants reported a history of the following healthcare worker diagnosed medical problems: allergies (27.3%), pneumonia (4.5%), and asthma (1.1%). The majority of participants reported cooking-related symptoms, with 84.5% reporting itchy eyes or runny nose, 48.8% reporting cough, 16.7% reporting wheezing, and 17.9% reporting difficulty breathing while cooking. There were on average 3.5 ± 1.3 children per household, and 93.2% of the children spent time in the kitchen. A substantial number of participants reported prior healthcare worker diagnosed medical problems in their children, with 15.9% reporting allergies, 4.5% reporting asthma, and 12.5% reporting pneumonia.
Only 5 kitchens were located outdoors. Of the indoor kitchens, most (89.8%) were located in a structure separate from the main home, with only 1 participant reporting cooking inside the main home, and only during the rainy season. The average distance between the kitchen and home was 6.2 meters. Most (98.9%) participants used firewood as the main fuel for cooking. Seven (8.0%) reported having a secondary stove inside the house that was used for tasks such as boiling water, rewarming food, or for heating the home. During baseline testing, participants reported the following primary lighting sources: open wick kerosene lamp (19.3%), hurricane lamp (45.5%), battery-powered lamp (33.0%), and solar-powered lamp (1.1% of). However, during follow-up testing, reported primary lighting sources changed as follows: open wick kerosene lamp (29.5%), hurricane lamp (35.2%), battery-powered light (18.2%), and solar lighting (9.1%).
A total of 14 outdoor, 110 living room, and 129 kitchen integrated 24-hour PM2.5 levels were obtained from 7 outdoor locations and 88 homes during the two sampling periods. In our first sampling period, we sampled 85 kitchens and 31 living rooms. In the second sampling period, we sampled 44 kitchens and 79 living rooms. Average 24-hour ambient PM2.5 levels in this rural location were 20.2 μg/m3. Indoor PM2.5 levels were higher and differed based on cooking vs. non-cooking environments, with average PM2.5 levels in living rooms measured at 35.2 μg/m3 as compared to kitchens measured at 270.0 μg/m3 (ambient vs. living room vs. kitchen, p < 0.0001, Kruskall-Wallis test; p < 0.0001, linear mixed effects models; see Table 3 and Figure 2). Only 36.4% of living room and 2.3% of kitchens had particulate levels that met the WHO criteria of having acceptable indoor PM2.5 levels of less than 25 μg/m3.
Table 3. PM2.5 levels by location.
Integrated 24-hour PM2.5 levels were measured by gravimetric methods from 88 distinct households over two time periods. WHO 24-hour PM2.5 standards refers to 24-hour PM2.5 levels less than 25 μg/m3.
| Location | N | Geometric Mean (Range), μg/m3 | Meets WHO 24-hour PM2.5 standards |
|---|---|---|---|
| Outdoor | 14 | 20.2 [6.8 – 57.0] | 10 (71.4%) |
| Living Room | 110 | 35.2 [6.8 – 4845.2] | 40 (36.4%) |
| Solar | 8 | 19.4 [6.8 – 43.7] | 6 (75.0%) |
| Battery | 29 | 30.6 [7.7 – 849.0] | 12 (41.4%) |
| Kerosene (hurricane) | 44 | 31.8 [9.1 – 145.9] | 14 (31.8%) |
| Kerosene (open wick) | 29 | 55.3 [14.7– 4,845.2] | 8 (27.6%) |
| Kitchen | 129 | 270.0 [11.6 – 5,241.1] | 3 (2.3%) |
| Outdoor | 5 | 181.3 [11.6 – 2,784.4] | 1 (20.0%) |
| Indoor | 124 | 274.4 [423.6 – 5,241.1] | 2 (1.6%) |
FIGURE 2. Fine particulate matter levels by location.
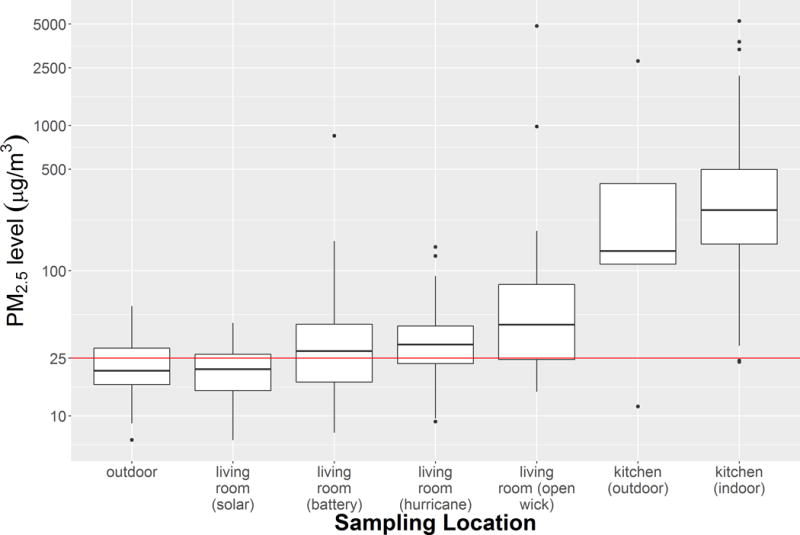
Boxplots of integrated 24-hour PM2.5 levels by sampling location. Horizontal red line is at PM2.5 concentration of 25 micrograms/m3, the World Health Organization (WHO) guideline level for acceptable indoor 24-hour PM2.5 concentrations.
When evaluating kitchens specifically, there were no statistically significant differences in PM2.5 levels between outdoor and indoor kitchens in both unadjusted (181.3 vs. 274.4 μg/m3, outdoor vs. indoor, p = 0.43, Kruskall-Wallis test) and adjusted comparisons (PM2.5 levels were 1.65 [0.63 – 4.33] times higher in indoor vs. outdoor kitchens, p = 0.30), although only 5 outdoor kitchens were sampled. In these mixed effects models, the only statistically significant predictor for kitchen PM2.5 levels was sampling phase (PM2.5 levels taken in March-July 2016 were 0.69 [0.49 – 0.98] times lower than those taken in July-October 2015, p = 0.04).
When evaluating living rooms PM2.5 levels, there were significant differences in PM2.5 levels based on type of lighting used in both unadjusted and adjusted analyses (p = 0.03, Kruskall-Wallis test; p = 0.02, mixed effects models). Most (75.0%) of the homes that reported using solar lighting met WHO-defined 24-hour PM2.5 standards, whereas only 27.6% of homes that reported using open wick kerosene lamps met WHO standards. In adjusted analyses, compared to solar lighting, homes using open wick lamps had 2.53 [1.14 – 5.64] times higher PM2.5 levels (p = 0.02). There were no statistically significant differences when comparing PM2.5 levels between homes using hurricane lamps vs. solar lighting, and battery-powered lighting vs. solar lighting. Reported use of an additional stove inside the home was not associated with differences in living room PM2.5 levels (p = 0.95), although we did not verify that the secondary stove was in use during the 24 hours in which we conducted environmental sampling. There was no statistically significant association between sampling phase and living room PM2.5 levels (p = 0.09). In a sensitivity analysis to determine whether very high living room PM2.5 levels drove the observed association between open wick lamps and PM2.5 levels, living room PM2.5 levels greater than or equal to 500 μg/m3 were excluded from the analysis. There was no significant change in the observed association between lighting source and measured PM2.5 levels, with homes using open wick kerosene lamps having 1.91 [1.07 – 3.42] times higher PM2.5 levels than homes using solar lighting (p = 0.01).
Similarly, when evaluating living room black carbon levels, there were significant differences in black carbon levels based on primary lighting source (p = 0.002, Kruskall-Wallis test). Average black carbon levels by lighting source were as follows (see Table 4): 0.75 (solar), 1.90 (battery), 2.71 (hurricane), 4.53 (open wick) μg/m3. In mixed effects models adjusting for sampling phase, use of a secondary stove, and household wealth, lighting source remained a significant predictor of indoor black carbon levels (p = 0.007), with black carbon levels being 4.72 [1.63 – 13.64] times higher in homes using open wick kerosene lamps compared to homes using solar lighting (p = 0.01).
Table 4. Black carbon levels in living rooms by primary lighting source.
Black carbon levels were measured over two time periods using reflectance to measure filter darkness. Primary reported source of lighting is a significant predictor of living room black carbon levels, with black carbon levels being 4.72 [1.63 – 13.64] times higher in homes using open wick kerosene lamps compared to homes using solar lighting (p = 0.01).
| Location | N | Geometric Mean (Range), μg/m3 |
|---|---|---|
| Outdoor | 14 | 1.19 [0.22 – 2.99] |
| Living Room | ||
| Solar | 8 | 0.75 [0.11 – 3.50] |
| Battery | 29 | 1.90 [0.24 – 35.49] |
| Kerosene (hurricane) | 44 | 2.71 [0.08 – 21.54] |
| Kerosene (open wick) | 29 | 4.53 [0.55 – 19.01] |
Correlation of measurements within the same kitchen between sampling phases was low (Spearman ρ = 0.38). Similar patterns were also observed in the same living rooms between sampling phases (Spearman ρ = 0.29).
DISCUSSION
In this epidemiologic study describing the contribution of cooking and lighting to household air pollution in a resource limited setting, we found that indoor PM2.5 levels were higher in cooking as compared to non-cooking environments. In non-cooking environments, reported primary lighting source was significantly associated with indoor PM2.5 levels, with homes relying on open wick kerosene lamps having higher indoor PM2.5 and black carbon levels compared with solar lighting. Our study has a number of practical implication. First, we identify primary lighting source as an important contributor to indoor particulate levels, and our findings suggest that in large epidemiologic studies where measurement of indoor pollutant levels is not possible, survey questions regarding lighting may identify individuals at risk of exposure to high indoor particulate levels. Average indoor particulate levels in homes using open wick kerosene lamps were 55.3 μg/m3, whereas levels in homes using primarily solar lighting were 19.4 μg/3. These differences in indoor PM2.5 levels is clinically significant, and suggests that the use of less-polluting forms of lighting such as solar lighting may be one strategy to reduce indoor air pollution in resource limited settings.
Several experimental chamber studies have examined kerosene-related combustion products. In one study, investigators described the particle size distribution and particle mass concentrations associated with diesel and kerosene lighting in a mock Kenyan market kiosk under high ventilation conditions17. They found that use of kerosene or diesel lighting was associated with PM2.5 levels that consistently exceeded 24-hour WHO guidelines. Consistent with our findings, open wick lamps were significantly more polluting than hurricane lamps. The investigators found average PM2.5 levels in this setting to be 500 μg/m3, whereas in our study, we report 24-hour integrated PM2.5 levels of 55.3 [14.7– 4,845.2] μg/m3 in homes primarily using open wick kerosene lamps. These differences may be explained by differences in study design. Apple et al measured PM2.5 levels only while the lamps were lit, with sampling occurring 0.6 meters away from the lamps, and they used light-scattering rather than gravimetric methods to estimate PM2.5 levels. In contrast, our study measured PM2.5 levels with samplers placed in the center of living rooms, and estimated average concentration over 24 hours using gravimetric methods. Lamps were likely lit only during the night, and may not have been as close as 0.6 meters from the samplers. It is possible that if we had used real-time monitoring of indoor particulate matter levels, or if we had used personal monitors on participants rather than area samplers in a fixed location, and restricted sampling to nighttime, we would have measured significantly higher PM2.5 levels than what we did observe. In another chamber study25, mean particulate emission rates from simple wick lamps were found to be lower than from cooking fires, although there was some overlap between the lower range of emissions for cooking fires and the higher range of emissions for open wick lamps. Taken together, this body of work highlights the need to focus on reductions in indoor air pollution from both cooking and lighting activities.
Other field and epidemiologic studies on kerosene based lighting have been performed, although few have specifically addressed indoor particulate levels. Lam et al measured emissions from open wick lamps in the field in Southwest Uganda, and combined these measurements with tests simulating field conditions in a controlled laboratory setting to demonstrate that kerosene lamps emit particulate matter largely in the form of black carbon26. We found a significant association between lighting source and both PM2.5 and black carbon levels, further supporting the idea that lighting rather than other combustion sources are an important contributor to indoor particulate concentrations inside the main home. In a case control study, Pokhrel et al found that use of kerosene based lighting was associated with a striking 9.43 increased odds of active tuberculosis27, highlighting the emerging literature on potential adverse health effects associated with kerosene-based lighting. Other studies on the use of kerosene either as a cooking fuel or for lighting have focused on acute health impacts such as reduced risk of burns from accidental fire, accidental poisoning from kerosene ingestion, or economic outcomes16, 28.
A strength of our study is that it is an epidemiologic study conducted in a large number of residential homes. Another strength is the longitudinal design, which allowed us to adjust for the effect of seasonality on both lighting source and particulate concentrations in our analysis. We note that choice of lighting source for the same participant changed over our sampling period, and may have reflected a spike in fuel prices between our first and second sampling phases. An additional strength is that rather than using carbon monoxide as a surrogate for PM2.5, we directly measured PM2.5. Although direct measurement of PM2.5 is more labor-intensive, some studies have shown that carbon monoxide does not serve as a reliable proxy for PM2.5 levels29. Finally, while other studies from Uganda have focused on ambient air pollution in urban locations30, 31, the issue of indoor air pollution from combustion sources is likely more relevant to most populations in low and middle income countries, who live predominantly in rural areas32.
Our study does have limitations. PM2.5 levels were measured as integrated levels over 24 hours rather than with real-time monitoring; it is likely that the magnitude of peak exposure may be predictive of health effects as well. We did not measure air exchange rates limiting comparability with other studies. However, in rural Africa, homes are unsealed and therefore highly ventilated – tracer gases would be removed quickly and so it would be difficult to measure air exchange rates. We did not perform triplicate measures of the same location at the same time to demonstrate the potential variability of our sampling strategy. Living room and personal PM2.5 levels were likely underestimated. This is because we performed environmental assessment over a 24 hour period, while the home did not require lighting during the daytime, indicating that measured values do not reflect peak values. Area sampling is also not a good surrogate for personal measures, particularly since kerosene lamps are often carried from room to room at night. Furthermore, we did not use thermal monitors to verify that stoves in kitchens, secondary stoves inside homes, or kerosene lighting was used during the period in which we conducted environmental sampling. Although research assistants instructed participants to carry on with their daily activities as per usual, our study team was informed that in a few cases, participants were initially afraid to cook near the area samplers for fear of damaging them. This likely explains why some indoor kitchens had measured PM2.5 levels that approximated ambient levels, and also suggests that the overall PM2.5 levels in our study were likely underestimates. Due to budget limitations as well as initial concerns from the community regarding placing samplers inside the main home, we were unable to sample all living rooms and all kitchens in both sampling periods. However, we used mixed effects models to analyze the resulting unbalanced data. Finally, we focused on PM2.5 and black carbon, while kerosene has other combustion products such as carbon monoxide and nitrogen oxides.33, 34 However, PM2.5 remains an important pollutant with well-documented health effects and recommended exposure standards.15 Despite the limitations noted above, our study does demonstrate that primary lighting source is associated with indoor PM2.5 levels.
Hurricane lamps are likely less polluting than open wick kerosene lamps because the flame in a hurricane lamp is shielded from ventilation, leading to more efficient combustion. While we were surprised to find that there were no statistically significant differences in PM2.5 levels between indoor and outdoor kitchens, a major limitation is that only 5 of the participants used outdoor kitchens during our study period, and thus we likely were underpowered to detect a difference.
One-fifth of the global population lacks access to electricity, and most rely on kerosene for lighting.16 Our findings highlight the important contribution of kerosene lighting to indoor air pollution. This has been a neglected area of research, as most epidemiologic surveys of indoor air pollution have focused on solid fuels used in cooking. Our findings suggest that in population-based health surveys conducted in rural resource-limited settings without access to a steady supply of electricity, it would be prudent to add questions targeted to lighting source, with a distinction made between open wick and hurricane lamps. Furthermore, our observational findings suggest that solar lighting has the potential to reduce household air pollution. Studies performed in other resource limited settings such as rural Malawi have demonstrated that introduction of solar lamps dramatically reduced reliance on kerosene lighting.35 Solar lighting is already being used in some rural communities in Uganda, and community uptake may be higher than the use of improved cookstoves due to convenience and cost savings on fuel, although solar uptake will likely by limited by the high initial cost.36
In conclusion, we have demonstrated in this field study that reported primary lighting source is significantly associated with indoor PM2.5 levels, with significantly higher PM2.5 levels in homes relying on open-wick kerosene lamps compared to homes relying on solar lighting. A solar lighting intervention has the potential to reduce exposure to indoor air particulate exposure in resource limited settings, and should be further studied.
Table 1.
Baseline characteristics of household members
| Characteristic | Mean ± SD or n (%) |
|---|---|
| Female, n (%) | 88 (100%) |
| Age, years | 36.2 ± 9 |
| Occupation | |
| Farming (without animals), n (%) | 54 (61.4%) |
| Farming (with animals), n (%) | 27 (30.7%) |
| Other, n (%) | 7 (7.9%) |
| Time use, hours | |
| Indoors | 15.0 ± 2.8 |
| Cooking | 3.4 ± 1.4 |
| Cooking-related symptoms, n (%) | |
| Itchy eyes or runny nose | 71 (84.5%) |
| Cough | 41 (48.8%) |
| Wheezing | 14 (16.7%) |
| Difficulty breathing | 15 (17.9%) |
| Physician diagnosed problems, n (%) | |
| Allergies | 24 (27.3%) |
| Asthma | 1 (1.1%) |
| Tuberculosis | 3 (3.4%) |
| Pneumonia | 4 (4.5%) |
| Number of children in household, n | 3.5 ± 1.3 |
| Children spend time in kitchen, n (%) | 82 (93.2%) |
| Children with physician diagnosed problems, n (%) | |
| Allergies | 14 (15.9%) |
| Asthma | 4 (4.5%) |
| Pneumonia | 11 (12.5%) |
Table 2. Baseline characteristics of homes.
Note that during follow-up testing the primary lighting source changed as follows: open wick kerosene lamp (29.5%), hurricane lamp (35.2%), battery-powered light (18.2%), and solar lighting (9.1%).
| Characteristic | |
|---|---|
| Homes, n | 88 |
| Kitchen location, n (%) | |
| Outdoors | 5 (5.7%) |
| Structure attached to house | 3 (3.4%) |
| Structure separate from house | 79 (89.8%) |
| Inside house | 1 (1.1%) |
| Distance between kitchen and house, meters | 6.2 ± 11.1 |
| Primary fuel for cooking, n (%) | |
| Firewood | 87 (98.9%) |
| Charcoal | 1 (1.1%) |
| Kitchen with chimney, n (%) | 5 (5.7%) |
| Kitchen roof composition, n (%) | |
| Iron or tin | 64 (70.5%) |
| Grass, banana fibers, leaves | 19 (21.6%) |
| Other | 5 (5.7%) |
| Secondary stove used inside house, n (%) | 7 (8.0%) |
| Primary lighting source, n (%) | |
| Solar lamp or light | 1 (1.1%) |
| Battery powered light | 29 (33.0%) |
| Covered kerosene lamp | 40 (45.5%) |
| Traditional kerosene lamp (“tadooba”) | 17 (19.3%) |
Practical Implications.
In this epidemiologic study examining the contribution of lighting to household air pollution, we demonstrate that primary lighting source is associated with indoor particulate levels, with the highest levels detected in homes using open wick kerosene lamps. Our findings suggest that in population-based health surveys conducted in rural resource-limited settings without access to a steady supply of electricity, it would be prudent to add questions targeted to lighting source, with a distinction made between open wick and hurricane lamps. Solar lighting to reduce kerosene use may be one future strategy to reduce indoor air pollution in resource limited settings.
Acknowledgments
Funding for this study was provided by NIH grants K23 ES023700, P30 00002, and K23 MH096620, American Lung Association Biomedical Research Grant RG-346990, Harvard Catalyst (UL1 TR001102) Early Clinical Data Support Pilot Grant, and Friends of a Healthy Uganda. The content is solely the responsibility of the authors and does not necessarily represent the official views of Harvard Catalyst, Harvard University and its affiliated academic healthcare centers, the National Institutes of Health, or the American Lung Association.
We wish to thank the members of the “Clean Air Study” team: S. Kobugyenyi, R. Twinamasiko, J.B. Oribakiriho, C. Agaba, J. Karakire, and C. Komugisha.
Footnotes
Conflict of interest: The authors have no conflicts of interest to declare.
LITERATURE CITED
- 1.Smith KR, Bruce N, Balakrishnan K, Adair-Rohani H, Balmes J, Chafe Z, Dherani M, Hosgood HD, Mehta S, Pope D, Rehfuess E, Group, H.C.R.E. Millions dead: how do we know and what does it mean? Methods used in the comparative risk assessment of household air pollution. Annual review of public health. 2014;35:185–206. doi: 10.1146/annurev-publhealth-032013-182356. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization. Burden of disease from Household Air Pollution for 2012–2014. Geneva, World Health Organization: World Health Organization; 2012. [Google Scholar]
- 3.World Health Organization. Indoor air pollution: national burden of disease estimates 2007 [Google Scholar]
- 4.Ezzati M, Saleh H, Kammen DM. The contributions of emissions and spatial microenvironments to exposure to indoor air pollution from biomass combustion in Kenya. Environ Health Perspect. 2000;108:833–839. doi: 10.1289/ehp.00108833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dionisio KL, Howie SRC, Dominici F, Fornace KM, Spengler JD, Adegbola RA, Ezzati M. Household Concentrations and Exposure of Children to Particulate Matter from Biomass Fuels in The Gambia. Environ Sci Technol. 2012;46:3519–3527. doi: 10.1021/es203047e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Smith KR, Samet JM, Romieu I, Bruce N. Indoor air pollution in developing countries and acute lower respiratory infections in children. Thorax. 2000;55:518–532. doi: 10.1136/thorax.55.6.518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bose S, Hansel N, Tonorezos E, Williams D, Bilderback A, Breysse P, Diette G, Mccormack MC. Indoor Particulate Matter Associated with Systemic Inflammation in COPD. Journal of Environmental Protection. 2015;6:566. [Google Scholar]
- 8.Ezzati M, Kammen DM. Indoor air pollution from biomass combustion and acute respiratory infections in Kenya: an exposure-response study. The Lancet. 2001;358:619–624. doi: 10.1016/s0140-6736(01)05777-4. [DOI] [PubMed] [Google Scholar]
- 9.Van Gemert F, Kirenga B, Chavannes N, Kamya M, Luzige S, Musinguzi P, Turyagaruka J, Jones R, Tsiligianni I, Williams S, De Jong C, Van Der Molen T. Prevalence of chronic obstructive pulmonary disease and associated risk factors in Uganda (FRESH AIR Uganda): a prospective cross-sectional observational study. The Lancet Global health. 2015;3:e44–51. doi: 10.1016/S2214-109X(14)70337-7. [DOI] [PubMed] [Google Scholar]
- 10.Smith KR, Mccracken JP, Weber MW, Hubbard A, Jenny A, Thompson LM, Balmes J, Diaz A, Arana B, Bruce N. Effect of reduction in household air pollution on childhood pneumonia in Guatemala (RESPIRE): a randomised controlled trial. Lancet. 2011;378:1717–1726. doi: 10.1016/S0140-6736(11)60921-5. [DOI] [PubMed] [Google Scholar]
- 11.Mortimer K, Ndamala CB, Naunje AW, Malava J, Katundu C, Weston W, Havens D, Pope D, Bruce NG, Nyirenda M, Wang D, Crampin A, Grigg J, Balmes J, Gordon SB. A cleaner burning biomass-fuelled cookstove intervention to prevent pneumonia in children under 5 years old in rural Malawi (the Cooking and Pneumonia Study): a cluster randomised controlled trial. Lancet. 2017;389:167–175. doi: 10.1016/S0140-6736(16)32507-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Burwen J, Levine DI. A rapid assessment randomised-controlled trial of improved cookstoves in rural Ghana. Energy for Sustainable Development. 2012;16:328–338. [Google Scholar]
- 13.Rosa G, Majorin F, Boisson S, Barstow C, Johnson M, Kirby M, Ngabo F, Thomas E, Clasen T. Assessing the impact of water filters and improved cook stoves on drinking water quality and household air pollution: a randomised controlled trial in Rwanda. PLoS ONE. 2014;9:e91011. doi: 10.1371/journal.pone.0091011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Muralidharan V, Sussan TE, Limaye S, Koehler K, Williams DL, Rule AM, Juvekar S, Breysse PN, Salvi S, Biswal S. Field testing of alternative cookstove performance in a rural setting of western India. International journal of environmental research and public health. 2015;12:1773–1787. doi: 10.3390/ijerph120201773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.World Health Organization. WHO Indoor Air Quality Guidelines: Household Fuel Combustion. Geneva: 2014. [PubMed] [Google Scholar]
- 16.Lam NL, Smith KR, Gauthier A, Bates MN. Kerosene: a review of household uses and their hazards in low- and middle-income countries. Journal of toxicology and environmental health. Part B, Critical reviews. 2012;15:396–432. doi: 10.1080/10937404.2012.710134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Apple J, Vicente R, Yarberry A, Lohse N, Mills E, Jacobson A, Poppendieck D. Characterization of particulate matter size distributions and indoor concentrations from kerosene and diesel lamps. Indoor Air. 2010;20:399–411. doi: 10.1111/j.1600-0668.2010.00664.x. [DOI] [PubMed] [Google Scholar]
- 18.Lee, Demokritou, Koutrakis Development and evaluation of personal respirable particulate sampler (PRPS) Atmos Environ. 2006;40:13–13. [Google Scholar]
- 19.International Organization for Standardization (Iso) ISO: ISO 9835, Ambient air - Determination of a black smoke index. Geneva: 1993. [Google Scholar]
- 20.Kinney PL, Aggarwal M, Northridge ME, Janssen NA, Shepard P. Airborne concentrations of PM(2.5) and diesel exhaust particles on Harlem sidewalks: a community-based pilot study. Environ Health Perspect. 2000;108:213–218. doi: 10.1289/ehp.00108213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Janssen N, Van Vliet P, Aarts F, Harssema H, Brunekree B. Assessment of exposure to traffic related air pollution of children attending schools near motorways. Atmospheric Environment. 2001;35:3875–3884. [Google Scholar]
- 22.Filmer D, Pritchett LH. Estimating wealth effects without expenditure data–or tears: an application to educational enrollments in states of India. Demography. 2001;38:115–132. doi: 10.1353/dem.2001.0003. [DOI] [PubMed] [Google Scholar]
- 23.Pinheiro J, Bates D, Debroy S, Sarkar D, R Core Team (2016) nlme: Linear and Nonlinear Mixed Effects Models. R package version 3.1–128. 2016;2016 [Google Scholar]
- 24.Wickham H. ggplot2: Elegant Graphics for Data Analysis. New York: Springer-Verlag; 2009. [Google Scholar]
- 25.Schare S, Smith K. Particulate emission rates of simple kerosene lamps. Energy Sustain Dev. 1995;2:32–35. [Google Scholar]
- 26.Lam L, Chen Y, Weyant C, Venkataraman C, Sadavarte P, Johnson MA, Smith KR, Brem BT, Arineitwe J, Ellis JE, Bond TC. Household light makes global heat: high black carbon emissions from kerosene wick lamps. Environ Sci Technol. 2012;46:13531–13538. doi: 10.1021/es302697h. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pokhrel AK, Bates MN, Verma SC, Joshi HS, Sreeramareddy CT, Smith KR. Tuberculosis and indoor biomass and kerosene use in Nepal: a case-control study. Environ Health Perspect. 2010;118:558–564. doi: 10.1289/ehp.0901032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mills E. Light for Life: Identifying and Reducing the Health and Safety Impacts of Fuel-based Lighting. Paris: United Nations, Environment Programme (UNEP) en.lighten initiative; 2014. pp. 1–20. [Google Scholar]
- 29.Klasen EM, Wills B, Naithani N, Gilman RH, Tielsch JM, Chiang M, Khatry S, Breysse PN, Menya D, Apaka C, Carter EJ, Sherman CB, Miranda JJ, Checkley W, Group, C.T.W. Low correlation between household carbon monoxide and particulate matter concentrations from biomass-related pollution in three resource-poor settings. Environmental research. 2015;142:424–431. doi: 10.1016/j.envres.2015.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kirenga BJ, Meng Q, Van Gemert F, Aanyu-Tukamuhebwa H, Chavannes N, Katamba A, Obai G, Molen TVD, Schwander S, Mohsenin V. The State of Ambient Air Quality in Two Ugandan Cities: A Pilot Cross-Sectional Spatial Assessment. International journal of environmental research and public health. 2015;12:8075–8091. doi: 10.3390/ijerph120708075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schwander S, Okello CD, Freers J, Chow JC, Watson JG, Corry M, Meng Q. Ambient particulate matter air pollution in Mpererwe District, Kampala, Uganda: a pilot study. Journal of environmental and public health. 2014;2014:763934. doi: 10.1155/2014/763934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.World Bank. Rural population (% of total population) World Bank Staff estimates based on United Nations. World Urbanization Prospects. 2015;2016 [Google Scholar]
- 33.Fan C, Zhang J. Characterization of emissions from portable household combustion devices: particle size distributions, emission rates and factors, and potential exposures. Atmos Environ. 2001;35:1281–1290. [Google Scholar]
- 34.Chen LW, Moosmuller H, Arnott WP, Chow JC, Watson JG, Susott RA, Babbitt RE, Wold CE, Lincoln EN, Hao WM. Emissions from laboratory combustion of wildland fuels: emission factors and source profiles. Environ Sci Technol. 2007;41:4317–4325. doi: 10.1021/es062364i. [DOI] [PubMed] [Google Scholar]
- 35.Adkins E, Eapen S, Kaluwile F, Nair G, Modi V. Off-grid energy services for the poor: Introducing LED lighting in the Millennium Villages Project in Malawi. Energy Policy. 2010;38:1087–1097. [Google Scholar]
- 36.Mills E, Jacobson A. From carbon to light: a new framework for estimating greenhouse gas emissions reductions from replacing fuel-based lighting with LED systems. Energy Efficiency. 2011;4:523–546. [Google Scholar]


