Abstract
While many studies have explored the relationship between different eating disorder diagnoses and the familial social environment, current evidence does not support associations between distinct family interaction patterns (e.g., high enmeshment) and particular diagnoses (e.g., anorexia nervosa). The current study seeks to move beyond the current literature to explore whether empirically-derived subtypes of family environment are associated with clinical features within a transdiagnostic sample of youth seeking treatment for eating disorders (n =123). Latent class modeling of the Family Environment Scale (FES) identified three classes (i.e., different FES profiles): (1) Control-Oriented, (2) System Maintenance-Oriented, and (3) Conflict-Oriented. Data are presented to characterize the classes (e.g., age, gender, rates of different eating disorders, severity of eating disorder pathology, rates of comorbid disorders). These preliminary results suggest family interaction types may help personalize treatment for eating disorders and encourage future research to guide such efforts.
Keywords: anorexia nervosa, bulimia nervosa, atypical anorexia, family environment, transdiagnostic, latent class analysis
Patterns of family interactions (i.e., the social environment of families) have long been of interest in developing theories and treatments related to eating disorders. Early conceptualizations considered anorexia nervosa (AN) a psychosomatic disorder and hypothesized that family interaction patterns contributed to it’s development and maintenance. Minuchin, who developed a structural family model (Minuchin, Rosaman, & Baker, 1978), focused on targeting family interactions patterns such as enmeshment (high cohesion and low independence; high proximity and intensity in family interactions), overprotectiveness (high degree of family member concern for each other’s welfare), rigidity (commitment to maintaining status quo), and level of conflict. While these early theories were largely based on subjective clinical observations and mostly debunked (Dare, Le Grange, Eisler, & Rutherford, 1994), subsequent research has explored whether differences in family interactions characterize families of youth who develop eating disorders compared to those who do not, as well as whether there are patterns of interactions that are specific to certain eating disorders (e.g., AN versus bulimia nervosa [BN]). In much of the past research, youth and their parents are asked to report their perceptions of family interactions using validated assessments (e.g., Family Assessment Device [FAD](Epstein, Baldwin, & Bishop, 1983), Family Environment Scale [FES](R. H. Moos & B. S. Moos, 2009), Family Adaptability and Cohesion Evaluation Scale [FACES](Olson, Sprenkle, & Russell, 1979)). However, no pattern of family interactions is consistently associated with specific eating disorder diagnoses suggesting, for example that families with a child diagnosed with AN do not have higher enmeshment versus those with BN. Moreover, there are not clear patterns of family interactions related to the presence of an eating disorder. For example, research does not support that all families with a child diagnosed with any eating disorder have higher levels of enmeshment and conflict than those without (Cook-Darzens, Doyen, Falissard, & Mouren, 2005; Dare et al., 1994). Thus, work in this domain has not identified clear patterns of family interactions that would be useful in tailoring treatment for youth with eating disorders. Further, much of the research on family interaction patterns is not current, which suggests there is an opportunity for an updated approach.
Perhaps these results should not be surprising given the conceptual debates in the field regarding the classification of eating disorders into distinct diagnostic categories. With each revision of the Diagnostic and Statistical Manual, the number of diagnostic categories has increased and much debate has ensued regarding the optimal way of diagnosing maladaptive eating behaviors (Cachelin & Maher, 1998; Wonderlich, Crosby, Mitchell, & Engel, 2007; Wonderlich, Joiner, Keel, Williamson, & Crosby, 2007). This is not particular to eating disorders and, as a result, efforts are increasingly focused on transdiagnostic treatment approaches, which work across a number of diagnostic categories (Rohde, 2012) and attempts to identify variables other than diagnosis that are useful for personalizing treatment approaches, such as the NIMH’s Research Domain Criteria (Insel et al., 2010). Thus, treatment developers are moving to use similar approaches across the categories of eating disorders (Fairburn, Cooper, & Shafran, 2003; Loeb, Lock, Le Grange, & Greif, 2012) and exploring ways to personalize treatment using other variables (e.g., latent class modeling of personality Krug et al., 2011).
While contemporary approaches to eating disorder treatment in youth have moved away from viewing the family as the cause of an eating disorder (Le Grange & Eisler, 2009), family interaction patterns continue to be important in the context of treatment (Goddard et al., 2013) and may be an important variable to consider in personalizing transdiagnostic treatment approaches. The way in which a family interacts seems to be an important indicator of their strengths and/or weaknesses as research suggests that family interaction patterns are often associated with distress levels (Ciao, Accurso, Fitzsimmons-Craft, & Le Grange, 2015; Johnson & Flach, 1985) and symptom severity (Wisotsky et al., 2003). Moreover, family interaction patterns can significantly impact on the process and outcome of therapy (Hoste, Lebow, & Le Grange, 2015; Le Grange, Eisler, Dare, & Hodes, 1992; Le Grange, Hoste, Lock, & Bryson, 2011; ****North, Gowers, & Byram, 1997; Rienecke, Accurso, Lock, & Le Grange, 2016; Wewetzer, Deimel, Herpertz-Dahlmann, Mattejat, & Remschmidt, 1996). Interestingly, research has demonstrated similar negative family interaction patterns in anxiety and mood disorders compared with eating disorders(Erol, Yazici, & Toprak, 2007; Theinemann & Steiner, 1993; Woodside, 1996); thus, research on how family interaction patterns impact treatment for eating disorders may have implications for other common youth mental health problems.
The goal of the current study is to explore whether family interaction patterns may be divided into classes, across eating disorder diagnoses, using latent variable modeling; this transdiagnostic approach moves beyond the current literature that has focused on differences based on diagnosis. While cross-sectional studies of this nature do not speak to whether challenging family interactions are a cause or consequence of an eating disorder, they may demonstrate utility in guiding future research aimed at understanding how families should be incorporated into transdiagnostic treatment for youth eating disorders. The current study is an initial step in this line of research; using latent class analysis, we examined whether youth with an eating disorder may be grouped by their perceptions of their family interactions, as reported on the Family Environment Scale (FES; R. Moos & B. Moos, 2009), and the clinical presentations of these classes (e.g., rates of comorbid diagnoses, demographic characteristics). To our knowledge, it is the first study to explore differences in family interaction patterns in relation to clinical presentations across different eating disorder diagnoses that may be useful for personalizing treatment.
METHODS
Sample/Procedures
The data analyzed in this manuscript are from a larger data collection effort: the initial pool of participants included 158 youth up to age 18 with a Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5) eating disorder diagnosis, and their caregiver(s), who presented to The University of Chicago Eating Disorders Program between May 2011 and June 2015 for standard clinical care (first episode of care; n = 92)(Vo, Accurso, Goldschmidt, & Le Grange, 2016), as well as between January 2009 to December 2012 for care in the context of a randomized clinical trial for BN (n = 66)(Le Grange, Lock, Agras, Bryson, & Jo, 2015). Data were collected from the initial clinical assessment, which included participant and caregiver interviews to assess diagnosis and demographic/clinical characteristics, as well as self-report questionnaires (described below). Of the 158 initial youth participants ages 10 to 18, 78% (n = 123) had complete data on the Family Environment Scale (FES) and were included in the primary analysis. Percent mBMI ranged 64.5 to 267.9. Duration of illness ranged from 1 month to 7 years and 3 months (see Table 1). There were no differences between youths who did or did not complete the FES by gender (X2 = 4.82, df = 1, p = 0.28, r = 0.20), race (white versus other; X2 = 1.69, df =1, p = 0.19, r = 0.12), ethnicity (Hispanic v. non-Hispanic; X2 = 1.03, df = 1, p = 0.31, r = 0.09), EDE Global score (t = −0.19, df = 29.64, p =0.85, d = 0.07), or duration of illness (t = −0.17, df = 147, p = 0.87, d = 0.03). Those who completed the FES had a lower mean age (t = −2.63, df = 43.85, p = 0.01, d = 0.75) and lower mean percent median body mass index (%mBMI; t = −2.70, df = 156, p = 0.01, d = 0.43) than those who did not. Participants provided written informed assent/consent, and the Institutional Review Boards at The University of Chicago and the University of California, San Francisco approved all protocols.
Table 1.
Demographic and clinical characteristics of sample
| Subsample who completed FES (N = 123) | ||
|---|---|---|
|
| ||
| Mean | SD | |
| Age (years) | 15.66 | 1.94 |
| %mBMI | 104.24 | 25.50 |
| Duration of illness (months) | 18.08 | 17.05 |
| EDE | 3.17 | 1.73 |
| BDI | 23.72 | 12.10 |
| CDI | 16.43 | 11.01 |
|
| ||
| f | % | |
|
| ||
| Gender (female) | 114 | 92.70 |
| Family Intact | 80 | 65.00 |
| Race | ||
| White | 106 | 86.20 |
| Black/African American | 8 | 6.50 |
| Asian | 3 | 2.40 |
| Mixed Race | 6 | 4.90 |
| Ethnicity (Hispanic) | 25 | 20.30 |
| Eating Disorder Diagnosis | ||
| Anorexia Nervosa | 23 | 19.32 |
| Bulimia Nervosa | 73 | 61.34 |
| Atypical AN | 15 | 12.60 |
| Other | 8 | 6.72 |
| Co-occurring Diagnosis | ||
| Mood | 41 | 33.30 |
| Anxiety | 32 | 26.00 |
%mBMI = Percent median body mass index; EDE = Eating Disorder Examination Global score; BDI = Beck Depression Inventory II; CDI = Children’s Depression Inventory; FES = Family Environment Scale; Atypical AN = Other Specified Feeding or Eating Disorder, Atypical Anorexia Nervosa
Measures
Participants’ height and weight were measured (without shoes in light indoor clothing) on a stadiometer and regularly recalibrated scale, respectively. Percent median body mass index (%mBMI) was calculated using the 50th Body Mass Index percentile according to Center for Disease Control norms for age and gender (Prevention, 2002).
Youth self-report measures
The Family Environment Scale (FES; R. Moos & B. Moos, 2009) was the main measure of interest for the current study; this 90 item measure of family social environment has good reliability and validity. The FES includes forms for parent and child report and can be used to assess actual, preferred, and expected family environments; the current study employed the actual form. Raw scores on the FES are averaged to calculate subscale scores grouped by three dimensions (relationship, personal growth, and system maintenance). The Relationship Dimensions are (1) cohesion: degree of commitment, help, and support; (2) expressiveness: extent to which family members encourage and express feeling directly; and (3) conflict: amount of openly expressed anger and conflict. The Personal Growth Dimensions are (1) independence: level of family members’ self-sufficiency and assertiveness; (2) achievement orientation: degree to which activities are cast in competitive framework; (3) intellectual: cultural orientation-level of interest in political, intellectual, or cultural activities; (4) active-recreational orientation: amount of participation in social and recreational activities; and (5) moral-religious emphasis: emphasis on ethical and religious issues and values. The System Maintenance Dimensions are (1) organization: the amount of structure and planning in family activities and responsibilities and (2) control: the degree to which rules run family life.
The Beck Depression Inventory (BDI-II; Beck, Steer, & Brown, 1996) is 21-item self-report measure of depression symptoms that is psychometrically valid for use with adolescents (Ambrosini, Metz, Bianchi, Rabinovich, & Undie, 1991). The Children’s Depression Inventory (CDI; Kovacs, 1992) is 27-item self-report measure developed to assess depression in children and adolescents. Due to changes in assessment protocol over the study period, some youth completed the BDI-II (n = 234 of total, n = 68 of those who completed the FES) and some completed the CDI (n = 150, n = 50 of those that completed the FES); see statistical analyses for how scores were analyzed.
Structured interviews
The Eating Disorder Examination (EDE, version 12.0; Fairburn & Cooper, 1993) is a structured diagnostic interview for assessing eating disorder diagnosis and eating disorder psychopathology that has good reliability and validity (Cooper, Cooper, & Fairburn, 1989; Rizvi, Peterson, Crow, & Stewart Agras, 2000; Rosen, Vara, Wendt, & Leitenberg, 1990). The global score was used in this study. A semi-structured diagnostic interview was used to assess for current Diagnostic and Statistical Manual of Mental Disorders, 4th Edition, Text Revision psychiatric disorders. For analytic purposes, co-occurring diagnoses were combined into major categories (e.g., mood, anxiety, disruptive behavior disorder, PTSD, OCD). Due to low numbers of other categories, only mood (i.e., major depressive disorder, dysthymia, bipolar disorder I, and bipolar disorder II) and anxiety disorder (i.e., generalized anxiety disorder and specific phobia) status were included in the analyses.
Statistical Analyses
Descriptive statistical analyses were conducted using SPSS version 19. T-tests and chi-square analyses were used to compare youth who had completed the FES to those who did not on age, gender, race (white versus other), ethnicity (Hispanic v. non-Hispanic), %mBMI, duration of illness, and EDE Global score. MPlus version 7.1 was used for latent variable modeling (Muthén, K., & Muthén, 1998). Significance level for all analyses was set at p < 0.05.
Depression z-scores
In order to use the data from both the BDI-II and CDI, individual depression scores from each of these measures were converted to z-scores using published, nonclinical population data, based on methods used in benchmarking studies to compare depression scores across psychotherapy trials (Weersing & Weisz, 2002). For the BDI-II, we used population mean μ = 7.17 and standard deviation σ = 7.50(Roberts, Lewinsohn, & Seeley, 1991); for the CDI, we used a population mean μ = 9.09 and standard deviation σ = 7.04 (Smucker, Craighead, Craighead, & Green, 1986).
Latent class analyses
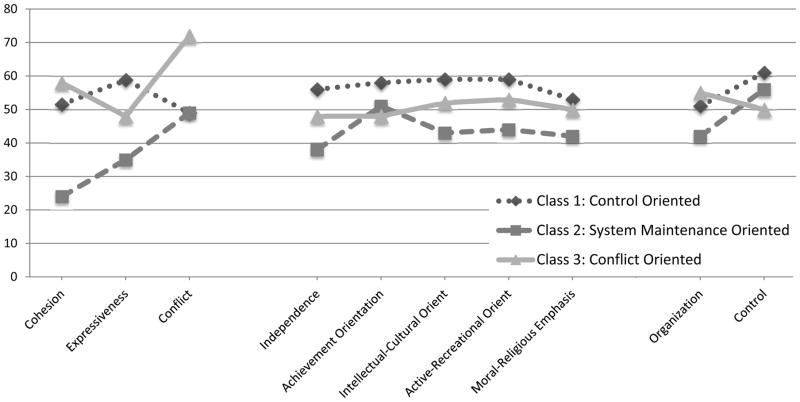
Models with 2–5 classes were fit to the FES subscale scores. The Bayesian Information Criterion and results of the Lo, Mendel, and Rubin likelihood ratio test were used to determine the number of classes to retain (Loehlin, 2004). Specifically, the lowest Bayesian Information Criterion and a significant likelihood ratio test (p < 0.05) were used to indicate good fit. If these criteria left the model choice unclear, the clinical interpretability of the solutions was examined (i.e., if clinically relevant patterns distinguished the classes in one solution but not another). Individuals were assigned to their most likely class based on posterior probabilities and the mean T score of each FES subscale was calculated per class and graphed; this is similar to how an individual’s FES profile is interpreted (i.e., subscale T-scores are graphed). The classes were labeled following the hierarchical classification system provided in the FES manual used to characterized profiles based on patterns of subscale T-scores in relationship to average scores (i.e., T-score = 50); profiles are labeled considering elevations in Personal Growth dimensions first, then Relationship dimensions, and then System Maintenance dimensions.
Using the auxiliary variable function of MPlus, we compared the classes based on age, %mBMI, duration of illness, global EDE scores, depression scores, and rates of different eating disorder and other co-occurring psychiatric diagnoses. The auxiliary variable function tests the equality of means across classes using posterior probability-based multiple imputations; it is used to compare classes on both continuous and categorical variables and results are reported as chi-square statistics.
RESULTS
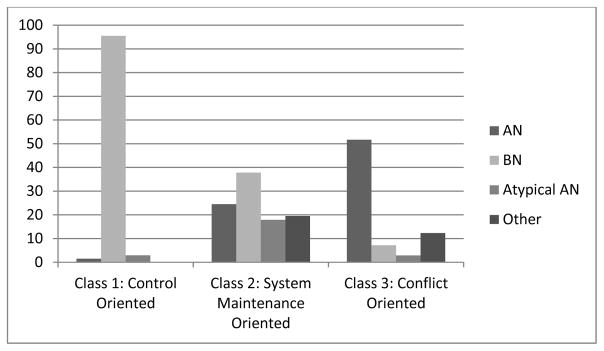
The best fitting latent class model was the 3-class solution (see Table 2; BIC decreased with each additional class, LMR test was not significant for the 4 or 5 class solutions). The FES profiles that best match the class profiles are (1) Control-Oriented, (2) System Maintenance-Oriented, and (3) Conflict-Oriented (see Figure 1). The first class did not match identified profiles from the FES manual. This class can best be described as Control-Oriented; these families had elevated mean control subscale score (>60) and several personal growth mean subscales scores approached 60. The System Maintenance-Oriented class was characterized by low cohesion, expression, and independence mean subscales scores (< 40). An elevated mean conflict subscale score (>60) was present for the Conflict-Oriented class. Overall tests, using the auxiliary variable function that accounts for uncertainty of class membership, indicated significant differences between the classes on age (χ2 = 33.57, df = 2, p < 0.001), %mBMI (χ2 = 48.61, df = 2, p < 0.001), duration of illness (χ2 = 23.88, df = 2, p < 0.001), EDE global score (χ2 = 30.22, df = 2, p < 0.001), depression score (χ2 = 30.70, df = 2, p < 0.001), eating disorder diagnosis (χ2 = 119.09, df = 6, p < 0.001), and co-occurring mood diagnosis (χ2 = 7.57, df = 2, p = 0.02). Classes did not differ based on whether families were intact or not (χ2 = 3.15, df = 2, p = 0.21) or rates of co-occurring anxiety diagnosis (χ2 = 5.99, df = 2, p = 0.05).
Table 2.
Fit statistics and class sizes for latent class analyses
| 2 Classes | 3 Classes | 4 Classes | 5 Classes | |
|---|---|---|---|---|
| BIC | 4928.99 | 4883.47 | 4874.55 | 4865.37 |
| Entropy | 0.89 | 0.91 | 0.92 | 0.88 |
| LMR p value | 0.01 | 0.01 | 0.13 | 0.71 |
| n class 1 | 29 | 64 | 11 | 12 |
| n class 2 | 94 | 22 | 65 | 21 |
| n class 3 | 37 | 22 | 28 | |
| n class 4 | 25 | 25 | ||
| n class 5 | 37 |
BIC = Bayesian Information Criterion
LMR = Lo, Mendel, and Rubin parametric likelihood ratio test
Note: Bold lettering indicates best fitting solution based on low BIC, significant LMR results, and clinically interpretable classes
Figure 1.
Family Environment Scale standard (T) subscale scores for three classes
Youths in Control-Oriented families (Class 1) had significantly greater eating disorder psychopathology (EDE global scores), and were more likely to have a diagnosis of BN compared to the other two classes, but least likely to have a co-occurring anxiety disorder (see Table 3 for between class comparisons). Youths in System Maintenance-Oriented families (Class 2) were more likely to have a co-occurring mood disorder. They also had the highest estimated rate of co-occurring anxiety disorders across classes, but the overall test for this comparison was not significant. Youths in Conflict-Oriented families (Class 3) were younger with a shorter duration of illness, lower %mBMI, and lower depression scores compared to the other classes.
Table 3.
Characterizing classes
| Class 1: Control-Oriented | Class 2: System Maintenance-Oriented | Class 3: Conflict-Oriented | Class 1 vs 2 | Class 1 vs. 3 | Class 2 vs. 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| Mean | SE | Mean | SE | Mean | SE | X2 | p | X2 | p | X2 | p | |
| Age (years) | 16.40 | 0.20 | 15.78 | 0.37 | 14.28 | 0.31 | 7.57 | 0.02 | 0.18 | 0.006 | 4.41 | 0.04 |
| %mBMI | 112.89 | 3.49 | 103.35 | 3.68 | 87.54 | 1.79 | 3.54 | 0.06 | 41.74 | <0.001 | 14.92 | <0.001 |
| Duration of illness | 22.81 | 2.40 | 17.35 | 3.59 | 9.82 | 1.32 | 1.60 | 0.21 | 22.43 | <0.001 | 3.88 | 0.049 |
| EDE | 3.67 | 0.15 | 2.66 | 0.33 | 2.17 | 0.24 | 7.95 | 0.005 | 27.44 | <0.001 | 1.47 | 0.23 |
| Depression | 2.14 | 0.20 | 2.12 | 0.35 | 0.55 | 0.23 | 0.01 | 0.91 | 27.12 | <0.001 | 15.35 | <0.001 |
|
| ||||||||||||
| Rate | SE | Rate | SE | Rate | SE | |||||||
|
| ||||||||||||
| Eating Disorder Diagnosis | 24.34 | <0.001 | 86.65 | <0.001 | 5.74 | 0.13 | ||||||
| Anorexia Nervosa | 1.5 | 1.5 | 24.8 | 12.9 | 51.7 | 9.7 | ||||||
| Bulimia Nervosa | 95.5 | 2.8 | 37.8 | 11.5 | 7.2 | 9.0 | ||||||
| Atypical AN | 2.9 | 2.4 | 17.9 | 9.6 | 28.8 | 9.0 | ||||||
| Other | 0 | 0 | 19.5 | 10.0 | 12.3 | 6.1 | ||||||
| Intact family | 60.3 | 6.2 | 72.5 | 10.3 | 77.2 | 7.5 | - | - | - | |||
| Mood Disorder | 26.1 | 5.6 | 60.9 | 11.3 | 30.4 | 8.4 | 7.54 | 0.006 | 0.18 | 0.67 | 4.41 | 0.036 |
| Anxiety Disorder | 18.1 | 4.8 | 46.7 | 11.2 | 28.8 | 8.0 | - | - | - | |||
%mBMI = Percent median body mass index; EDE = global Eating Disorders Examination score; Atypical AN = Other Specified Feeding or Eating Disorder, Atypical Anorexia Nervosa
Note: Did not present tests between classes for variables where overall test was not significant. Degrees of freedom for each chi-square test between classes = 1.
DISCUSSION
This study investigated differences in youth perceptions of their family interaction patterns among families presenting to an outpatient eating disorders clinic. The goal was to explore whether differences in perceived family functioning might be useful for personalizing transdiagnostic eating disorder treatment. While the cross sectional methods employed do not have direct implications for treatment utility, they can be used to generate hypotheses for future research. Latent class modeling identified three classes of family environments: 1) Control-Oriented, 2) System Maintenance-Oriented, and 3) Conflict-Oriented. Importantly, these classes were not driven solely by diagnosis (i.e., not all youth diagnosed with AN were present in one class) or severity (i.e., low functioning and high functioning classes), which would preclude potential clinical utility of the results (i.e., classes of family functioning would not have provided information beyond assessment of symptoms and diagnosis). Although these results are preliminary, the differences between the classes, as detailed below, highlight areas of interest for future research regarding modifications to youth eating disorders treatment.
Control-Oriented families were high on the control subscale of the FES System Maintenance Dimension, indicating that these youths perceived their families as using many rules and procedures to run family life. Youths from Control-Oriented families had more severe eating disorder psychopathology and were also more likely to have a diagnosis of BN than the other two classes of families. As the onset of an eating disorder is likely to impact a family environment; the finding that many families were perceived as using rules to run family life may be a reflection of this in that families in this class may have implemented rules and procedures to cope with the eating disorder. If so, they may be well positioned to begin family based treatment (FBT; Lock & Le Grange, 2013), which starts with implementing structure to support healthy eating behaviors, and further adaptations may not be necessary for families in this class that are already empowered to implement structure. While the majority of this class had a diagnosis of BN (95.5%), almost 40% of the System Maintenance-Oriented class had a diagnosis of BN as well; thus, these classes are providing information above what can be learned from diagnosis or research that focuses on one diagnostic category. Additionally, the finding in the current study that the majority of youth diagnosed with BN did not perceive higher than average levels of conflict within their families was surprising as previous research has associated a BN diagnosis or bulimic symptoms with higher perceived family conflict, from both the patient and caregiver’s perspective.(Humphrey, 1986; Johnson & Flach, 1985; Strober, 1981)
System Maintenance-Oriented families were characterized by low Relationship scores, meaning that the youths in these families experience little cohesion and expressiveness, with average levels of conflict compared to youths in other family classes. These youths also had lower independence scores, suggesting they perceived more enmeshment within their family, or felt less encouraged to be assertive and self-reliant. This finding is similar to recent qualitative findings about youths’ perceptions of low emotional connectedness (Huemer et al., 2012; Karwautz et al., 2002) and may have implications for how treatment might aim to change family interactions in order to promote the youth’s independence, possibly with additional youth-focused interventions and/or family interventions focused on increasing the youth’s independence within the family system. This class also had high FES control scores, indicating that System Maintenance-Oriented youths perceived family life as being governed by more rules and procedures. Of note, youths in this class had a variety of different eating disorder diagnoses and the distribution was not significantly different from Conflict-Oriented families.
Conflict-Oriented families (i.e., families that youths perceived as more openly hostile toward each other), were characterized by youths who were more likely to be younger, have a shorter duration of illness, lower %mBMI, and lower depression scores. Notably, about 50% of the participants in this class had a diagnosis of AN, which is interesting given that previous research has often associated restrictive symptoms with enmeshment (Steiger, Puentes-Neuman, & Leung, 1991; Strober & Humphrey, 1987) rather than family conflict. Anecdotally, however, it is not uncommon to witness high levels of conflict in families of youth with AN, particularly around issues related to eating and weight-related issues.
Taken together, findings from this study highlight differences in clinical characteristics across family social environments in youth with eating disorders that do not solely map on to diagnostic differences. Future research should investigate whether transdiagnostic treatment for adolescent eating disorders modified based on a specific family’s FES profile improves treatment outcome. For instance, some families might benefit from skills taken from dialectical behavior therapy (DBT; Linehan, 1993; Miller, Rathus, & Linehan, 2007) or the Collaborative Care Skill Training workshops (Treasure, Smith, & Crane, 2007). Conflict-Oriented families may be taught distress tolerance skills in order to help them better cope with conflict in the short term, while also learning interpersonal effectiveness skills to improve communication around emotional topics. System Maintenance-Oriented families may benefit from learning validation strategies to encourage and support emotional expression. Results from a pilot trial that integrated FBT and DBT provides preliminary evidence for the feasibility and efficacy of treatment that integrates coping strategies and FBT(Murray et al., 2015), which paves the way for future exploration of how and when to integrate these approaches.
The current study offers evidence that differences in family social environment profiles are associated with the clinical presentation of youth with eating disorders. Importantly, this study, in parallel with other cross-sectional studies of family interaction patterns, does not speak to the etiology of eating disorders. While changes in the family social environment may facilitate recovery from an eating disorder, the relationship between the family interaction patterns and the presence of an eating disorder is likely complex and transactional. The current study aimed to identify differences in family interaction patterns that may indicate ways to adapt treatment and facilitate eating disorder recovery.
It should also be noted that the current study relied solely on youth report of the family social environment. Future research is needed to assess whether family profiles differ based on the respondent (i.e., caregivers’ views of interaction patterns), as some previous research has found discrepancies between youth versus parent reports of family interactions, which may be clinically meaningful (Bonne et al., 2003; Weinstock, Wenze, Munroe, & Miller, 2013). For instance, if a youth’s perception of family cohesion and expressiveness is low, while a parent’s perception of these variables is high, treatment could be modified to address this discrepancy through improved communication skills. Alternatively, if a youth experiences their family as high in conflict, but their parents do not, the therapist might include distress tolerance or emotion regulation skills in treatment. The current results should also be considered with caution given the modest sample size, differences in severity of age and expected body weight between those that did and did not complete the FES, and potential limits of generalizability due to sample demographics (92.68% female, and 86.2% white).
This study offers preliminary evidence for the relationship between family social environment and the clinical presentation of adolescent eating disorders. Future work should further examine the utility of using differences in perceptions of family interactions to personalize care for youth and families presenting to eating disorders clinics and ultimately improve outcomes.
Figure 2.
Estimated rates of eating disorder diagnoses per class
AN = Anorexia Nervosa, BN= Bulimia Nervosa, Atypical AN = Other Specified Feeding or Eating Disorder, Atypical Anorexia Nervosa
Acknowledgments
Dr. Le Grange receives royalties from Guilford Press and Routledge, and is co-director of the Training Institute for Child and Adolescent Eating Disorders, LLC. Dr. Goldschmidt was supported by NIH grant (K23-DK105234, PI: Goldschmidt).
References
- Ambrosini PJ, Metz C, Bianchi MD, Rabinovich H, Undie A. Concurrent validity and psychometric properties of the Beck Depression Inventory in outpatient adolescents. J Am Acad Child Adolesc Psychiatry. 1991;30(1):51–57. doi: 10.1097/00004583-199101000-00008. [DOI] [PubMed] [Google Scholar]
- Beck A, Steer R, Brown G. Manual for the Beck Depression Inventory-II. San Antonio, Tx: Psychological Corporation; 1996. [Google Scholar]
- Bonne O, Lahat S, Kfir R, Berry E, Katz M, Bachar E. Parent-daughter discrepancies in perception of family function in bulimia nervosa. Psychiatry. 2003;66(3):244–254. doi: 10.1521/psyc.66.3.244.25154. [DOI] [PubMed] [Google Scholar]
- Cachelin FM, Maher BA. Restricters who purge: Implications of purging behavior for psychopathology and classification of anorexia nervosa. Eating Disorders: The Journal of Treatment & Prevention. 1998;6(1):51–63. doi: http://dx.doi.org/10.1080/10640269808249247. [Google Scholar]
- Ciao AC, Accurso EC, Fitzsimmons-Craft EE, Le Grange D. Predictors and moderators of psychological changes during the treatment of adolescent bulimia nervosa. Behav Res Ther. 2015;69:48–53. doi: 10.1016/j.brat.2015.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook-Darzens S, Doyen C, Falissard B, Mouren MC. Self-perceived family functioning in 40 French families of anorexic adolescents: implications for therapy. European Eating Disorders Review. 2005;13(4):223–236. doi: 10.1002/erv.628. [DOI] [Google Scholar]
- Cooper Z, Cooper PJ, Fairburn CG. The validity of the Eating Disorder Examination and its subscales. The British Journal of Psychiatry. 1989;154:807–812. doi: 10.1192/bjp.154.6.807. doi: http://dx.doi.org/10.1192/bjp.154.6.807. [DOI] [PubMed] [Google Scholar]
- Dare C, Le Grange D, Eisler I, Rutherford J. Redefining the psychosomatic family: Family process of 26 eating disorder families. International Journal of Eating Disorders. 1994;16(3):211–226. doi: 10.1002/1098-108x(199411)16:3<211::aid-eat2260160302>3.0.co;2-x. doi: http://dx.doi.org/10.1002/1098-108X(199411)16:3<211::AID-EAT2260160302>3.0.CO;2-X. [DOI] [PubMed] [Google Scholar]
- Epstein NB, Baldwin LM, Bishop DS. The McMaster Family Assessment Device. Journal of Marital and Family Therapy. 1983;9(2):171–180. doi: http://dx.doi.org/10.1111/j.1752-0606.1983.tb01497.x. [Google Scholar]
- Erol A, Yazici F, Toprak G. Family functioning of patients with an eating disorder compared with that of patients with obsessive compulsive disorder. Compr Psychiatry. 2007;48(1):47–50. doi: 10.1016/j.comppsych.2006.05.004. [DOI] [PubMed] [Google Scholar]
- Fairburn CG, Cooper Z. The eating disorder examination (12.0D) In: Fairburn CG, Wilson GT, editors. Binge eating: Nature, assessment and treatment. New York, NY: Guilford Press; 1993. [Google Scholar]
- Fairburn CG, Cooper Z, Shafran R. Cognitive behaviour therapy for eating disorders: a “transdiagnostic” theory and treatment. Behaviour research and therapy. 2003;41(5):509–528. doi: 10.1016/s0005-7967(02)00088-8. [DOI] [PubMed] [Google Scholar]
- Goddard E, Salerno L, Hibbs R, Raenker S, Naumann U, Arcelus J, … Treasure J. Empirical examination of the interpersonal maintenance model of anorexia nervosa. International Journal of Eating Disorders. 2013;46(8):867–874. doi: 10.1002/eat.22172. doi: http://dx.doi.org/10.1002/eat.22172. [DOI] [PubMed] [Google Scholar]
- Hoste RR, Lebow J, Le Grange D. A bidirectional examination of expressed emotion among families of adolescents with bulimia nervosa. International Journal of Eating Disorders. 2015;48(2):249–252. doi: 10.1002/eat.22306. doi: http://dx.doi.org/10.1002/eat.22306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huemer J, Haidvogl M, Mattejat F, Wagner G, Nobis G, Fernandez-Aranda F, … Karwautz AFK. Perception of autonomy and connectedness prior to the onset of anorexia nervosa and bulimia nervosa: A retrospective study in sister pairs discordant for an eating disorder. Zeitschrift für Kinder- und Jugendpsychiatrie und Psychotherapie. 2012;40(1):61–68. doi: 10.1024/1422-4917/a000150. doi: http://dx.doi.org/10.1024/1422-4917/a000150. [DOI] [PubMed] [Google Scholar]
- Humphrey L. Family relations in bulimic-anorexic and nondistressed families. International Journal of Eating Disorders. 1986;5(2):223–232. [Google Scholar]
- Insel T, Cuthbert B, Garvey M, Heinssen R, Kozak M, Pine DS, … Wang P. Research Domain Criteria (RDoC): toward a new classification framework for research on mental disorders. Am J Psychiat. 2010:167. doi: 10.1176/appi.ajp.2010.09091379. [DOI] [PubMed] [Google Scholar]
- Johnson C, Flach A. Family characteristics of 105 patients with bulimia. Am J Psychiatry. 1985;142(11):1321–1324. doi: 10.1176/ajp.142.11.1321. [DOI] [PubMed] [Google Scholar]
- Karwautz A, Haidvogl M, Wagner G, Nobis G, Wöber-Bingöl Ç, Friedrich MH. Subjektives Familienbild bei Anorexia nervosa und Bulimia nervosa um Jugendalter: Eine kontrollierte Studie. [Subjective family image in adolescents with anorexia nervosa and bulimia nervosa] Zeitschrift für Kinder- und Jugendpsychiatrie und Psychotherapie. 2002;30(4):251–259. doi: 10.1024/1422-4917.30.4.251. doi: http://dx.doi.org/10.1024/1422-4917.30.4.251. [DOI] [PubMed] [Google Scholar]
- Kovacs M. Children’s Depression Inventory manual. North Tonawanda, NY: Multi-Health Systems; 1992. [Google Scholar]
- Krug I, Root T, Bulik C, Granero R, Penelo E, Jiménez-Murcia S, Fernández-Aranda F. Redefining phenotypes in eating disorders based on personality: A latent profile analysis. Psychiatry Research. 2011;188(3):439–445. doi: 10.1016/j.psychres.2011.05.026. doi: http://dx.doi.org/10.1016/j.psychres.2011.05.026. [DOI] [PubMed] [Google Scholar]
- Le Grange D, Eisler I. Family interventions in adolescent anorexia nervosa. Child and Adolescent Psychiatric Clinics of North America. 2009;18(1):159–173. doi: 10.1016/j.chc.2008.07.004. doi: http://dx.doi.org/10.1016/j.chc.2008.07.004. [DOI] [PubMed] [Google Scholar]
- Le Grange D, Eisler I, Dare C, Hodes M. Family criticism and self-starvation: a study of expressed emotion. Journal of Family Therapy. 1992;14:177–192. [Google Scholar]
- Le Grange D, Hoste RR, Lock J, Bryson SW. Parental expressed emotion of adolescents with anorexia nervosa: Outcome in family-based treatment. International Journal of Eating Disorders. 2011;44(8):731–734. doi: 10.1002/eat.20877. doi: http://dx.doi.org/10.1002/eat.20877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le Grange D, Lock J, Agras WS, Bryson SW, Jo B. Randomized Clinical Trial of Family-Based Treatment and Cognitive-Behavioral Therapy for Adolescent Bulimia Nervosa. J Am Acad Child Adolesc Psychiatry. 2015;54(11):886–894. e882. doi: 10.1016/j.jaac.2015.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linehan M. Cognitive-behavioral treatment of borderline personality disorder. New York, NY: Guilford Press; 1993. [Google Scholar]
- Lock J, Le Grange D. Treatment manual for anorexia nervosa: A family-based approach. 2. New York: Guilford Press; 2013. [Google Scholar]
- Loeb KL, Lock J, Le Grange D, Greif R. Transdiagnostic Theory and Application of Family-Based Treatment for Youth with Eating Disorders. Cogn Behav Pract. 2012;19(1):17–30. doi: 10.1016/j.cbpra.2010.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loehlin JC. Goodness of Fit Indices: Latent Variable Models. 4. Mahwah, NJ: Lawrence Erlbaum Associates; 2004. [Google Scholar]
- Miller AL, Rathus JH, Linehan M. Dialectical behavior therapy for suicidal adolescents. New York, NY: Guilford Press; 2007. [Google Scholar]
- Minuchin S, Rosaman BL, Baker L. Psychosomatic families: Anorexia nervosa in context. Cambridge: Harvard University Press; 1978. [Google Scholar]
- Moos R, Moos B. Family Environment Scale Manual: Development, Applications, and Research. Palo Alto, CA: Mind Garden, Inc; 2009. [Google Scholar]
- Moos RH, Moos BS. Family Environment Scale Manual: Development, Applications, and Research. Palo Alto, CA: Mind Garden, Inc; 2009. [Google Scholar]
- Murray SB, Anderson LK, Cusack A, Nakamura T, Rockwell R, Griffiths S, Kaye WH. Integrating Family-Based Treatment and Dialectical Behavior Therapy for Adolescent Bulimia Nervosa: Preliminary Outcomes of an Open Pilot Trial. Eat Disord. 2015;23(4):336–344. doi: 10.1080/10640266.2015.1044345. [DOI] [PubMed] [Google Scholar]
- Muthén KL, Muthén BO. Mplus User’s Guide. 7. Los Angeles, CA: Muthén & Muthén; 1998. [Google Scholar]
- North C, Gowers S, Byram V. Family functioning and life events in the outcome of adolescent anorexia nervosa. Br J Psychiatry. 1997;171:545–549. doi: 10.1192/bjp.171.6.545. [DOI] [PubMed] [Google Scholar]
- Olson DH, Sprenkle DH, Russell CS. Circumplex model of marital and family systems: I. Cohesion and adaptability dimensions, family types, and clinical applications. Family Process. 1979;18(1):3–28. doi: 10.1111/j.1545-5300.1979.00003.x. doi: http://dx.doi.org/10.1111/j.1545-5300.1979.00003.x. [DOI] [PubMed] [Google Scholar]
- Prevention, C. f. D. C. a. CDC growth charts for the United States: Development and methods. Atlanta, GA: Centers for Disease Control and Prevention; 2002. [Google Scholar]
- Rienecke RD, Accurso EC, Lock J, Le Grange D. Expressed emotion, family functioning, and treatment outcome for adolescents with anorexia nervosa. European Eating Disorders Review. 2016;24(1):43–51. doi: 10.1002/erv.2389. doi: http://dx.doi.org/10.1002/erv.2389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rizvi SL, Peterson CB, Crow SJ, Stewart Agras W. Test-retest reliability of the Eating Disorder Examination. International Journal of Eating Disorders. 2000;28(3):311–316. doi: 10.1002/1098-108x(200011)28:3<311::aid-eat8>3.0.co;2-k. doi: http://dx.doi.org/10.1002/1098-108X(200011)28:3<311::AID-EAT8>3.0.CO;2-K. [DOI] [PubMed] [Google Scholar]
- Roberts RE, Lewinsohn PM, Seeley JR. Screening for adolescent depression: a comparison of depression scales. J Am Acad Child Adolesc Psychiatry. 1991;30(1):58–66. doi: 10.1097/00004583-199101000-00009. [DOI] [PubMed] [Google Scholar]
- Rohde P. Applying transdiagnostic approaches to treatments with children and adolescents: Innovative models that are ready for more systematic evaluation. Cognitive and Behavioral Practice. 2012;19(1):83–86. doi: http://dx.doi.org/10.1016/j.cbpra.2011.06.006. [Google Scholar]
- Rosen JC, Vara L, Wendt S, Leitenberg H. Validity studies of the eating disorder examination. International Journal of Eating Disorders. 1990;9(5):519–528. doi: http://dx.doi.org/10.1002/1098-108X(199009)9:5<519::AID-EAT2260090507>3.0.CO;2-K. [Google Scholar]
- Smucker MR, Craighead WE, Craighead LW, Green BJ. Normative and reliability data for the Children’s Depression Inventory. J Abnorm Child Psychol. 1986;14(1):25–39. doi: 10.1007/BF00917219. [DOI] [PubMed] [Google Scholar]
- Steiger H, Puentes-Neuman G, Leung FYK. Personality and family features of adolescent girls with eating disorder symptoms: Evidence for restricter/binger differences in a nonclinical population. Addictive Behaviors. 1991;16:303–314. doi: 10.1016/0306-4603(91)90023-b. [DOI] [PubMed] [Google Scholar]
- Strober M. The significance of bulimia nervosa in juvenile anorexia nervosa: An exploration of possible etiologic factors. International Journal of Eating Disorders. 1981;1:28–43. [Google Scholar]
- Strober M, Humphrey LL. Familial contributions to the etiology and course of anorexia nervosa and bulimia. J Consult Clin Psychol. 1987;55(5):654–659. doi: 10.1037//0022-006x.55.5.654. [DOI] [PubMed] [Google Scholar]
- Theinemann M, Steiner H. Family environment of eating disordered and depressed adolescents. Int J Eat Disord. 1993;(14):43–48. doi: 10.1002/1098-108x(199307)14:1<43::aid-eat2260140106>3.0.co;2-7. [DOI] [PubMed] [Google Scholar]
- Treasure J, Smith G, Crane A. Skills-based learning for caring for a loved one with an eating disorder: The new Maudsley method. Routledge/Taylor & Francis Group; New York, NY: 2007. [Google Scholar]
- Vo M, Accurso EC, Goldschmidt AB, Le Grange D. The impact of dsm-5 on eating disorder diagnoses. International Journal of Eating Disorders. 2016 doi: 10.1002/eat.22628. doi: http://dx.doi.org/10.1002/eat.22628. [DOI] [PMC free article] [PubMed]
- Weersing VR, Weisz JR. Community clinic treatment of depressed youth: benchmarking usual care against CBT clinical trials. J Consult Clin Psychol. 2002;70(2):299–310. doi: 10.1037//0022-006x.70.2.299. [DOI] [PubMed] [Google Scholar]
- Weinstock LM, Wenze SJ, Munroe MK, Miller IW. Concordance between patient and family reports of family functioning in bipolar I disorder and major depressive disorder. J Nerv Ment Dis. 2013;201(5):377–383. doi: 10.1097/NMD.0b013e31828e1041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wewetzer C, Deimel W, Herpertz-Dahlmann B, Mattejat F, Remschmidt H. Follow-up investigation of family relations in patients with anorexia nervosa. Eur Child Adolesc Psychiatry. 1996;5(1):18–24. doi: 10.1007/BF00708210. [DOI] [PubMed] [Google Scholar]
- Wisotsky W, Dancyger I, Fornari V, Katz J, Wisotsky WL, Swencionis C. The relationship between eating pathology and perceived family functioning in eating disorder patients in a day treatment program. Eat Disord. 2003;11(2):89–99. doi: 10.1080/10640260390199280. [DOI] [PubMed] [Google Scholar]
- Wonderlich SA, Crosby RD, Mitchell JE, Engel SG. Testing the validity of eating disorder diagnoses. International Journal of Eating Disorders. 2007;40(Supl):S40–S45. doi: 10.1002/eat.20437. doi: http://dx.doi.org/10.1002/eat.20437. [DOI] [PubMed] [Google Scholar]
- Wonderlich SA, Joiner TE, Jr, Keel PK, Williamson DA, Crosby RD. Eating disorder diagnoses: Empirical approaches to classification. American Psychologist. 2007;62(3):167–180. doi: 10.1037/0003-066X.62.3.167. doi: http://dx.doi.org/10.1037/0003-066X.62.3.167. [DOI] [PubMed] [Google Scholar]
- Woodside DBS, Kuch RP, Heinmaa KM. Family functioning in anxiety an eating disorders—a comparative study. Compr Psychiatry. 1996;37:139–143. doi: 10.1016/s0010-440x(96)90575-1. [DOI] [PubMed] [Google Scholar]