Abstract
OBJECTIVES
To evaluate if the relationship of anthropometric measurements of obesity with mortality varies by age and race/ethnicity in older women.
DESIGN
A prospective cohort study of multiethnic post-menopausal women.
SETTING
The Women’s Health Initiative (WHI) observational study and clinical trials in 40 clinics.
PARTICIPANTS
A total of 161,808 postmenopausal women (age 50–79) participating in WHI.
MEASUREMENTS
Baseline height, weight and waist circumference (WC) were measured by trained staff, and body mass index (BMI) was calculated based on height and weight. Demographic, health, and lifestyle data from baseline questionnaire were used as covariates. The outcome was adjudicated death (n = 18,320) during a mean follow-up time of 11.4 ± 3.2 years.
RESULTS
Hazards ratios (HR) and 95% confidence interval (95% CI) indicated that ethnicity and age modified (p<0.01) the relationships between obesity measurements and mortality. While underweight was associated with a higher mortality rate, overweight or slightly obese was not a risk factor for mortality in most ethnic groups, except for Hispanic women in the obesity I category (HR = 1.42; 95%CI = 1.04–1.95). BMI was not or only weakly associated with mortality in the 70–79 age group; HR (95% CI) for death was 0.90 (0.85–0.95), 0.98 (0.92–1.06), 1.11 (1.00–1.23), and 1.08 (0.92–1.26) respectively in overweight and the three obesity categories compared to the normal BMI category. In contrast, higher central obesity measured by WC was consistently associated with higher mortality in all groups.
CONCLUSION
Underweight is a significant risk factor for mortality in older women and healthy BMI ranges may need to be age- and race/ethnic-specific. Finally, our findings support a consistent relationship between central obesity and mortality.
Keywords: body mass index, waist circumference, mortality, minority health, women
INTRODUCTION
Obesity is one of the major underlying causes of mortality. While there has been a large and growing body of evidence describing this link (1–3), uncertainties remain with respect to the utility of different measures of obesity, and variation with respect to different age and ethnic/racial groups.
Body mass index (BMI) is the most commonly used measure of obesity in both clinical practice and in population-based studies (2, 4), because of its low cost and relative ease of measurement. Waist circumference (WC) is another measure of obesity which reflects central adiposity, which may have a more detrimental impact on health (5), and mortality (6–11). Intuitively, WC may thus have greater clinical utility than BMI in predicting disease and mortality.
In order to provide public health recommendations defining a “healthy” BMI in different populations, it is critical to further investigate the extent to which the relationship of BMI with mortality varies by age and race/ethnicity. Previous studies have found considerable heterogeneity in the strength of this relationship, namely that it is weaker among older age-groups (12–14) and among African-Americans (13, 15–18).
In the Women’s Health Initiative (WHI) cohort, we examined the association of BMI with all-cause mortality across different age and racial/ethnic groups. We hypothesized that associations of obesity with mortality will vary across age and racial/ethnic groups. Secondarily, we evaluated these relationships using WC as the exposure of interest.
METHODS
Study participants and overview
Study participants came from the US WHI cohort which includes healthy multiethnic post-menopausal women (50–79 years old), enrolled in 4 clinical trials and one observational study. WHI recruitment was completed between 1993 and 1998. Questionnaires were used on baseline and follow-up health and lifestyle information. Women visited the clinic yearly or every three years for physical measurements. The institutional review boards at all 40 clinic sites approved the WHI study, and all WHI participants provided a written informed consent. The recruitment strategies (19), data collection (20) and baseline characteristics of the participants (21–27) have already been published.
Mortality
WHI participants who were lost to follow-up or who were known (through participants’ proxy) to be deceased were matched to the National Death Index to confirm death and to ascertain causes of death. For cause of death, hospitalization records from the time of death and the most recent relevant hospitalization before death, as well as autopsy records and death certificate diagnoses were used. For many out-of-hospital deaths, the only documentation available was the death certificate. In these cases, the immediate and underlying causes of death were abstracted from the death certificate (28). In this study, the latest WHI data on mortality were available through May, 2011.
Anthropometry
Weight was measured to the nearest 0.1 kg on a balance beam scale with the participant dressed in indoor clothing without shoes. Height was measured to the nearest 0.1 centimeter using a wall-mounted stadiometer. Body mass index (BMI) was calculated as: weight (kg)/height (m)2. Tape measures were used to measure waist circumference to the nearest 0.1 centimeter at the most narrow part of the waist region by trained staff at each WHI clinic (29). Only baseline anthropometric data were used in this study. BMI and waist circumference categories were created as below in the statistical analysis section.
Other covariates
Information on age, race/ethnicity, smoking, postmenopausal hormone use, physical activity (total MET-hrs/wk), medication uses, and medical history (such as depression, diabetes, cardiovascular disease, hypertension, arthritis, osteoporosis, cancer, asthma, and emphysema), were ascertained from baseline questionnaires. These questionnaires were either self-administered or interviewer-administered. “Don’t know” responses were coded as missing. Dietary alcohol consumption was assessed using a semi-quantitative food-frequency questionnaire (30).
Statistical Analysis
All-cause mortality was used in the main analysis. Descriptive analyses were performed based on baseline characteristics of the study participants and the results were presented as mean (95% CI), or frequencies (%) by BMI category (<18.5, 18.5–24.9, 25–29.9, 30–34.9, 35–39.9, ≥40 kg/m2) defined by the National Institute of Health, National Heart, Lung, and Blood Institute (31). T-tests or chi-square tests were conducted on selected baseline characteristics of the participants.
To better visualize the distribution of mortality rate by BMI and WC, BMI was categorized into multiple groups (≤18.4, 18.5–19.9, 20.0–22.4, 22.5–24.9, 25.0–27.4, 27.5–29.9, 30.0–34.9, 35.0–39.9, ≥40.0) which are similar to the ones presented by Berrington de Gonzalez et al (32), but without upper and lower limits for the two extreme ones. WC was also categorized into multiple groups (≤70, 71–75, 76–80, 81–85, 86–90, 91–95, 96–100, 101–105, 106–110, 111–115, 116–120, ≥121). Age-adjusted all-cause mortality rates, including 95% CI, were computed by categories of BMI and WC for all participants by race/ethnicity and by age group.
The Cox-proportional hazards model was used to test differences in the relative risk of mortality by different level of BMI and WC in the entire population, and in each race/ethnic or age group. A smaller number of categories were used for BMI (<18.5, 18.5–24.9, 25–29.9, 30–34.9, 35–39.9, ≥40) and WC (≤ 79, 80–89, 90–104, 105–114, ≥115) in this modeling stage to avoid sparse cells for the analyses. The following covariates were evaluated for confounding: study arm (intervention), baseline age (years), race/ethnicity physical activity (MET-hrs/wk), smoking status, alcohol use, medical conditions/diseases including arthritis ever, asthma ever, cancer ever, cardiovascular disease ever, diabetes, depression score (no depression: <0.06) (33), hormone use (never, past, current), family income, marital status, and highest education level from grade school to doctoral degree. Potential confounding factors were identified in the marginal analysis if the p-value was less than 0.2, and then examined one by one, and as a group in the Cox proportional hazards regression analysis to assess their independent and collective impacts on the relationship between obesity and mortality. If the inclusion of a variable significantly affected the hazards ratio (more than 10%), then it was treated as a confounding factor, and included in the final model. The covariates initially selected for consideration were previously reported risk factors for mortality and BMI (3, 32). Collinearities of covariates were examined. Interaction terms of race/ethnicity, age, smoking status, alcohol use, and physical activity with BMI and WC were tested for effect modifications in the association between BMI or WC and mortality. When significant interactions were detected, data were presented in different strata. We also examined the relationship of mortality with BMI and WC in the same Cox regression model, controlling for confounding factors. All analyses were performed with Stata Statistical Software (version 12.0, Statacorp, College Station, TX).
Sensitivity analysis
To examine whether pre-existing conditions confounded the association between mortality and anthropometric measurements, study participants were dropped from the analysis if their death occurred within 3 years after the baseline visit. To assess the impact of smoking on our findings, we also limited the analysis to non-smokers.
RESULTS
The results were based on 161,808 WHI participants. The mean follow-up time was 11.4±3.2 years, ranging from 26 days to 16.6 years. During the follow-up, 18,320 people died, and among them, 5,458 deaths were due to cardiovascular diseases (including cerebrovascular and pulmonary embolism), and 7,345 deaths were associated with any type of cancer.
The majority of the participants (82.9%) were non-Hispanic whites (Table 1). There were 14,618 African-American women (9% of total) and 6,484 Hispanic women (4%) in the study sample. An inverse relationship between age and BMI was observed at baseline. African-American women were more likely to be overweight (25.0–29.9) and obese (30.0 or above) based on BMI categories. Physical inactivity was more common among women classified as obese. There were more current smokers in the underweight categories. All other covariates, including alcohol intake, family income, diabetes ever, as well as study arms exhibited differences across BMI categories (p <0.001).
Table 1.
Characteristics of Study Participants by Body Mass Index Category
| Variables | Mean(SD) or N(%) by BMI Category | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Total | Underweight (<18.5) |
Normal (18.5– 24.9) |
Overweight (25.0–29.9) |
Obese I (30–34.9) |
Obese II (35–39.9) |
Obese III (≥40) |
P-value | |||
| Height(cm) | 161.76(6.66) | 162.17(6.87) | 162.35(6.42) | 161.72(6.35) | 161.41(6.26) | 161.27(6.53) | 160.38(8.31) | <0.001 | ||
| Age group(years) | ||||||||||
| 50–59 | 53559(33%) | 405(29%) | 18399(33%) | 17282(31%) | 9782(33%) | 4476(37%) | 2734(42%) | <0.001 | ||
| 60–69 | 72589(45%) | 555(40%) | 23579(43%) | 25300(45%) | 13836(47%) | 5735(47%) | 2944(46%) | |||
| 70–79 | 35660(22%) | 438(31%) | 12959(24%) | 13098(24%) | 6129(20%) | 1975(16%) | 755(12%) | |||
| Ethnicity | ||||||||||
| Native American | 713(<1%) | 5(<1%) | 166(<1%) | 208(1%) | 179(1%) | 85(1%) | 55(1%) | <0.001 | ||
| Asian | 4190(3%) | 148(11%) | 2291(4%) | 1275(2%) | 325(1%) | 92(1%) | 37(1%) | |||
| African-American | 14618(9%) | 72(5%) | 2255(4%) | 4711(8%) | 3898(13%) | 2084(17%) | 1465(23%) | |||
| Hispanic | 6484(4%) | 23(2%) | 1572(3%) | 2443(5%) | 1500(5%) | 592(5%) | 284(4%) | |||
| Non-Hispanic white | 133541(83%) | 1136(81%) | 47952(88%) | 46241(83%) | 23395(79%) | 9168(75%) | 4486(70%) | |||
| Other | 1849(1%) | 10(1%) | 549(1%) | 660(1%) | 379(1%) | 144(1%) | 91(1%) | |||
| Family income | ||||||||||
| Less than $34,999 | 62101(40%) | 530(40%) | 17227(33%) | 21505(40%) | 13127(46%) | 5907(50%) | 3241(52%) | <0.001 | ||
| $35,000 to $99,999 | 74423(48%) | 588(44%) | 26942(51%) | 25820(48%) | 12959(45%) | 4981(42%) | 2544(41%) | |||
| $100,000 up | 14360(9%) | 145(11%) | 6830(13%) | 4714(9%) | 1722(6%) | 554(5%) | 257(4%) | |||
| Don't know | 4384(3%) | 61(5%) | 1494(3%) | 1446(3%) | 857(3%) | 308(3%) | 179(3%) | |||
|
Recreational physical activity (mets/wk) |
||||||||||
| 0–3.79 | 52577(34%) | 414(30%) | 12376(23%) | 17045(32%) | 12300(44%) | 6136(53%) | 3767(60%) | <0.001 | ||
| 3.8–14.2 | 51233(33%) | 417(30%) | 17640(33%) | 18436(35%) | 9329(33%) | 3362(29%) | 1635(26%) | |||
| 14.3–142.3 | 50587(33%) | 541(40%) | 22734(44%) | 17417(33%) | 6553(23%) | 2006(18%) | 826(14%) | |||
| Smoking status | ||||||||||
| never smoked | 81430(51%) | 718(52%) | 27874(51%) | 27859(51%) | 15105(51%) | 6073(50%) | 3116(49%) | <0.001 | ||
| past smoker | 67110(42%) | 454(33%) | 22066(41%) | 23293(42%) | 12439(42%) | 5362(45%) | 2882(46%) | |||
| current smoker | 11142(7%) | 203(15%) | 4297(8%) | 3796(7%) | 1801(7%) | 604(5%) | 335(5%) | |||
| Alcohol intake | ||||||||||
| none | 17652(11%) | 225(16%) | 5279(10%) | 5863(10%) | 3615(12%) | 1581(13%) | 937(15%) | <0.001 | ||
| past drinker | 30148(19%) | 275(20%) | 8080(15%) | 9750(18%) | 6623(22%) | 3176(26%) | 1981(31%) | |||
| <1 drink per week | 52863(33%) | 338(24%) | 15970(29%) | 18314(33%) | 10762(37%) | 4651(39%) | 2379(37%) | |||
| 1–6 drinks per week | 41173(25%) | 330(24%) | 16562(30%) | 14894(27%) | 6160(21%) | 2006(17%) | 859(13%) | |||
| 7+ drinks per week | 18748(12%) | 215(16%) | 8677(16%) | 6470(12%) | 2319(8%) | 654(5%) | 231(4%) | |||
| Diabetes ever | ||||||||||
| no | 152080(94%) | 1355(97%) | 53613(98%) | 52948(95%) | 26992(91%) | 10493(86%) | 5337(83%) | <0.001 | ||
| yes | 9618(6%) | 39(3%) | 1279(2%) | 2702(5%) | 2732(9%) | 1690(14%) | 1093(17%) | |||
| Study arms | ||||||||||
| Observation | 93676(58%) | 1107(79%) | 36689(67%) | 31462(56%) | 14580(50%) | 5451(45%) | 3282(51%) | <0.001 | ||
| CT controls | 26515(16%) | 109(8%) | 7270(13%) | 9473(17%) | 5788(19%) | 2529(21%) | 1216(19%) | |||
| DM intervention | 13664(9%) | 50(4%) | 3687(7%) | 4855(9%) | 3018(10%) | 1377(11%) | 618(10%) | |||
| HRT intervention | 9777(6%) | 47(3%) | 2631(5%) | 3414(6%) | 2200(7%) | 979(8%) | 458(7%) | |||
| CAD intervention | 18176(11%) | 85(6%) | 4660(8%) | 6476(12%) | 4161(14%) | 1850(15%) | 859(13%) | |||
Mortality rates by age and ethnicity
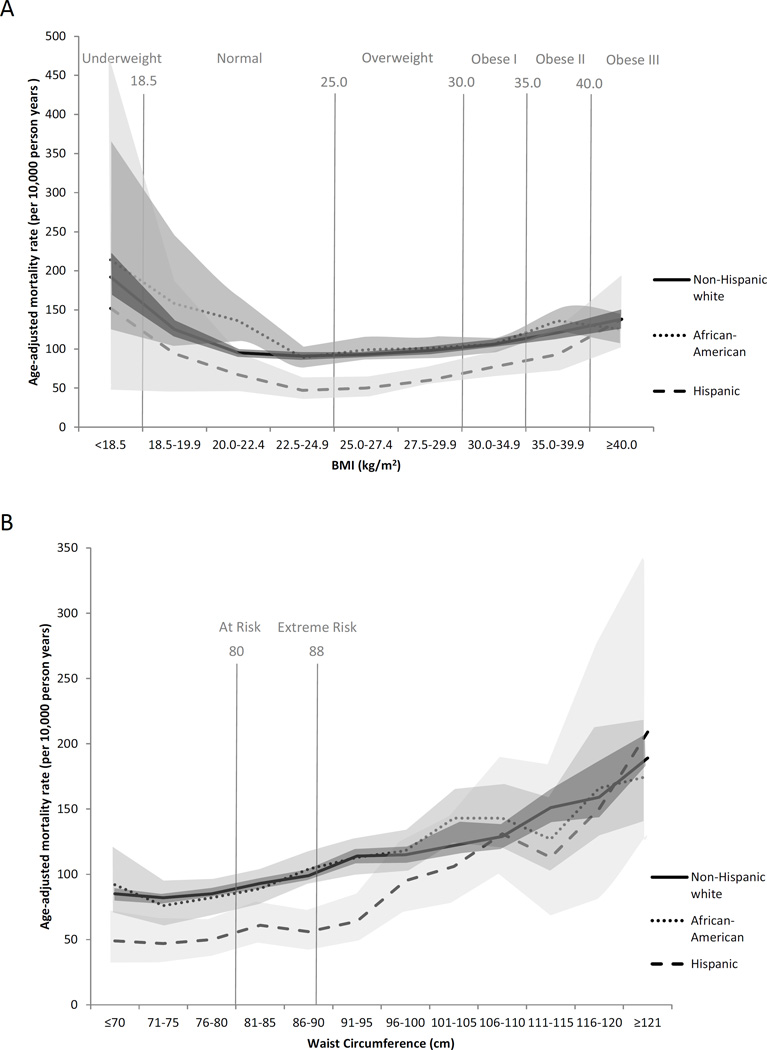
Figure 1 shows the mean age-adjusted mortality rates (95% CI in shade) for BMI and WC by ethnic group. A larger number of categories for BMI (9 categories) and WC (12 categories) were used to help better illustrate the relationships of mortality with BMI or WC. For any given cell, the minimal number of death was 5 or greater. While a U-shaped curve was observed in each ethnic group for BMI, the relationship between WC and mortality was more linear. The age-adjusted mortality rate appears to generally increase with larger WC in different ethnic groups. Interestingly, Hispanic women appear to have lower mortality rates at any given level of WC or BMI in comparison to African-American and Non-Hispanic white women.
Figure 1.
Age-Adjusted All-cause Mortality Rate with BMI (top panel) and WC (bottom panel) by Ethnicity
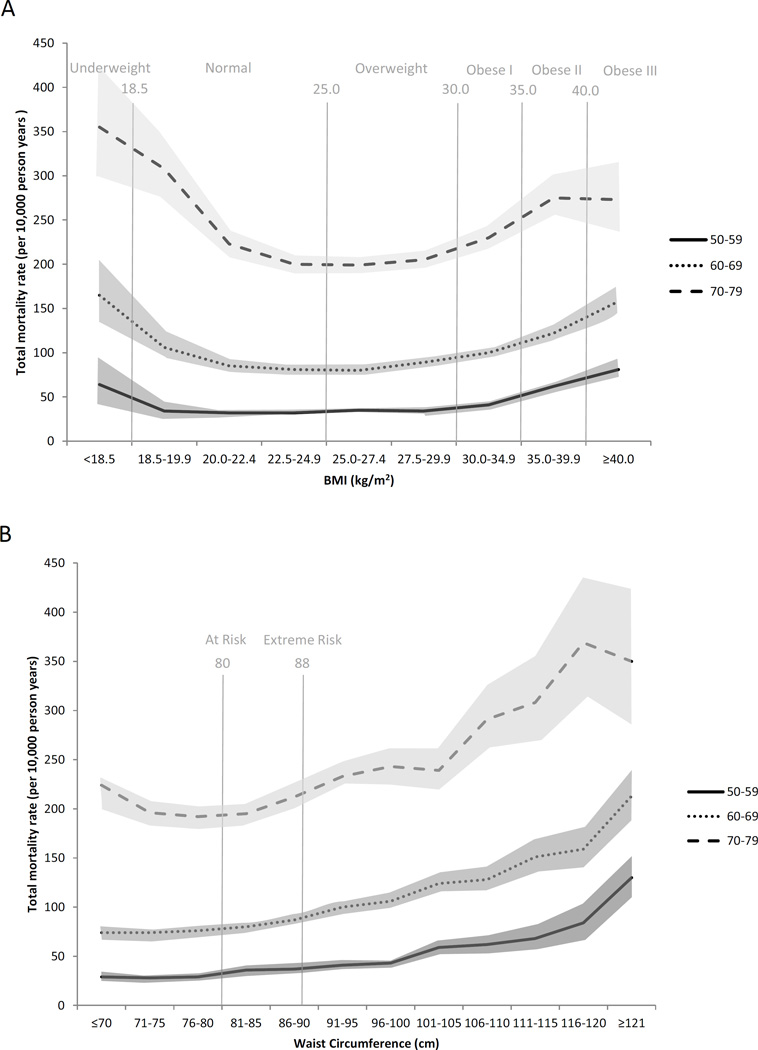
Figure 2 shows the mortality rate across different BMI and WC categories by age group. A clear U-shaped curve was observed for the BMI and mortality relationship in all age groups, especially in the oldest age group (70 – 79). A low mortality rate as observed across the range of BMIs from 20 to 29. For example, in age group 70–79, we observed an age-adjusted mortality rate of 223 (95% CI 209–237), 200 (95% CI 190–210), 199 (95% CI 190–209), and 205 (95% CI 194–217) per 10,000 person years for the BMI category of 20–22.4, 22.5–24.9, 25.0–27.4, 27.5–29.9 respectively.
Figure 2.
All-cause Mortality Rate with BMI (top panel) and WC (bottom panel) by Age
Relative risk of mortality with different BMI and WC level
In the total sample, we found significant increased risk for mortality in the underweight group (BMI <18.5) and all the obesity categories (BMI >30), and continuously higher mortality risk with increased WC (data not shown). Age and ethnicity exhibited significant interactions with BMI and WC (pinteraction<0.01), so the results from Cox models were presented for each racial/ethnic and age strata.
Table 2 presents the results of hazards ratios (HR) and 95% CI of BMI, WC, and BMI plus WC models in each racial/ethnic group. Consistent with the findings from the total sample, the results from the crude and age-adjusted models showed that underweight and obesity were associated with an increased risk of mortality in African-Americans, Hispanics, and non-Hispanic whites in comparison to the normal BMI category (BMI = 18.5–24.9). However, the magnitude of these associations appeared to be the greatest among Hispanics, and smallest among African-Americans. Being in the obesity categories II or III (BMI>34.9) was associated with increased mortality risk in all three racial/ethnic groups. In contrast, a significantly elevated mortality rate in the obesity I category (BMI = 30.0–34.9) was only observed in Hispanic women in the further adjusted model. Being overweight (BMI = 25.0 –29.9) was not associated with an increased mortality rate in any of the racial/ethnic groups. A monotonic relationship between increased WC and mortality rate was observed in African-Americans, Hispanics and non-Hispanic whites using WC group of 80–89 as the reference. The increased mortality risk associated with larger WC was strongest in Hispanics but showed no differences between African-Americans and non-Hispanic whites. In all racial/ethnic groups, when BMI and WC were included in the same model, BMI was no longer a significant risk factor for mortality (instead, it seemed to be a protective factor in African-American and non-Hispanic whites), while larger WC still showed a significant association with higher mortality, when BMI was included in the model (data not shown).
Table 2.
BMI and Waist Circumference Cox Model for All-Cause Mortality Stratified by Ethnicity Group
| Model | Model 1* | Model 2** | Model 3*** | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Ethnicity | African- American |
Hispanic | Non-Hispanic white |
African- American |
Hispanic | Non-Hispanic white |
African- American |
Hispanic | Non-Hispanic white |
| BMI(kg/m2) | HR(95%CI) | HR(95%CI) | HR(95%CI) | ||||||
| (< 18.5) | 1.98(1.13–3.45) | 3.10(1.14–8.46) | 2.09(1.83–2.38) | 1.89(1.08–3.30) | 3.15(1.16–8.57) | 1.94(1.70–2.21) | 1.68(0.96–2.95) | 3.52(1.28–9.65) | 1.67(1.45–1.92) |
| (18.5 – 24.9) | ref | ref | ref | ref | ref | ref | ref | ref | ref |
| (25.0 – 29.9) | 0.98(0.83–1.13) | 0.97(0.74–1.26) | 1.01(0.98–1.05) | 1.00(0.86–1.16) | 0.99(0.75–1.29) | 0.98(0.94–1.02) | 1.02(0.87–1.20) | 0.97(0.72–1.31) | 0.94(0.90–0.98) |
| (30.0 – 34.9) | 1.02(0.87–1.19) | 1.42(1.08–1.88) | 1.13(1.08–1.18) | 1.10(0.94–1.38) | 1.55(1.17–2.04) | 1.14(1.08–1.19) | 1.10(0.93–1.31) | 1.42(1.04–1.95) | 1.02(0.97–1.07) |
| (35.0 – 39.9) | 1.31(1.11–1.55) | 1.69(1.20–2.39) | 1.30(1.23–1.39) | 1.50(1.26–1.78) | 2.00(1.42–2.83) | 1.42(1.33–1.51) | 1.37(1.14–1.66) | 1.99(1.36–2.91) | 1.21(1.13–1.29) |
| (≥ 40) | 1.22(1.01–1.48) | 2.50(1.70–3.69) | 1.50(1.39–1.63) | 1.54(1.27–1.86) | 2.89(1.96–4.26) | 1.83(1.69–1.99) | 1.36(1.10–1.68) | 2.41(1.57–3.70) | 1.44(1.32–1.57) |
| WC(cm) | HR(95%CI) | HR(95%CI) | HR(95%CI) | ||||||
| ≤79 | 0.87(0.74–1.02) | 0.87(0.66–1.14) | 0.87(0.84–0.91) | 0.87(0.74–1.02) | 0.86(0.66–1.13) | 0.94(0.90–0.98) | 0.88(0.74–1.05) | 0.96(0.71–1.30) | 0.98(0.93–1.02) |
| 80–89 | ref | ref | ref | ref | ref | ref | ref | ref | ref |
| 90–104 | 1.28(1.13–1.45) | 1.40(1.10–1.79) | 1.21(1.16–1.26) | 1.31(1.16–1.48) | 1.41(1.10–1.81) | 1.21(1.16–1.26) | 1.18(1.03–1.35) | 1.40(1.06–1.85) | 1.11(1.06–1.16) |
| 105–114 | 1.51(1.28–1.77) | 2.49(1.80–3.44) | 1.45(1.37–1.54) | 1.67(1.42–1.96) | 2.74(1.98–3.78) | 1.57(1.48–1.67) | 1.36(1.14–1.62) | 2.66(1.86–3.80) | 1.36(1.27–1.45) |
| ≥115 | 1.77(1.47–2.13) | 3.09(2.05–4.68) | 1.89(1.75–2.03) | 2.16(1.80–2.61) | 3.15(2.08–4.76) | 2.24(2.08–2.41) | 1.72(1.41–2.10) | 2.30(1.43–3.69) | 1.74(1.61–1.88) |
Model 1: Crude Model
Model 2: Adjusted for age group
BMI Model 3: Adjusted for age group, annual income, alcohol intake, physical activity, smoking status, diabetes, and study arms (interventions)
WC Model 3: Adjusted for age group, height, annual income, alcohol intake, physical activity, smoking status, diabetes, study arms (interventions)
Table 3 shows the Cox regression results for BMI and WC on mortality in different age groups. Being underweight (BMI < 18.5) or obese II or III (BMI >35.9) was significantly associated with a higher mortality rate in all three age groups. In contrast, being overweight (BMI = 25.0–29.9) or obese I (BMI = 25.0 –29.9) was not associated with any increased risk of mortality. Instead, being overweight was protective in the oldest age group (>70 yrs) in this study. It was found that higher WC was always a significant risk factor in all age groups.
Table 3.
BMI and Waist Circumference Cox Model for All-Cause Mortality Stratified by Age Group
| Model | Model 1* | Model 2** | Model 3*** | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Age Group | 50–59 | 60–69 | 70–79 | 50–59 | 60–69 | 70–79 | 50–59 | 60–69 | 70–79 |
| BMI(kg/m2) | HR(95%CI) | HR(95%CI) | HR(95%CI) | ||||||
| (< 18.5) | 1.87(1.28–2.73) | 1.98(1.62–2.43) | 1.81(1.54–2.14) | 1.89(1.30–2.76) | 2.01(1.64–2.46) | 1.83(1.55–2.16) | 1.47(0.98–2.19) | 1.86(1.51–2.29) | 1.57(1.31–1.88) |
| (18.5 – 24.9) | ref | ref | ref | ref | ref | ref | ref | ref | ref |
| (25.0 – 29.9) | 1.11(1.00–1.23) | 1.01(0.95–1.07) | 0.94(0.90–0.99) | 1.08(0.97–1.19) | 1.00(0.94–1.06) | 0.94(0.89–0.99) | 1.02(0.91–1.14) | 0.97(0.92–1.04) | 0.90(0.85–0.95) |
| (30.0 – 34.9) | 1.27(1.13–1.43) | 1.22(1.14–1.30) | 1.09(1.03–1.17) | 1.21(1.07–1.36) | 1.19(1.11–1.27) | 1.08(1.01–1.15) | 1.08(0.95–1.23) | 1.07(0.99–1.15) | 0.98(0.92–1.06) |
| (35.0 – 39.9) | 2.06(1.81–2.35) | 1.48(1.36–1.61) | 1.32(1.21–1.45) | 1.93(1.69–2.20) | 1.43(1.32–1.55) | 1.30(1.18–1.43) | 1.61(1.39–1.87) | 1.24(1.13–1.35) | 1.11(1.00–1.23) |
| (≥ 40) | 2.61(2.26–3.02) | 2.00(1.82–2.21) | 1.36(1.18–1.58) | 2.40(2.07–2.78) | 1.91(1.73–2.11) | 1.34(1.16–1.54) | 1.82(1.55–2.15) | 1.52(1.36–1.69) | 1.08(0.92–1.26) |
| WC(cm) | HR(95%CI) | HR(95%CI) | HR(95%CI) | ||||||
| ≤79 | 0.80(0.72–0.89) | 0.91(0.86–0.97) | 0.99(0.94–1.04) | 0.82(0.74–0.92) | 0.92(0.86–0.98) | 0.99(0.94–1.05) | 0.89(0.79–1.00) | 0.95(0.88–1.01) | 1.03(0.97–1.10) |
| 80–89 | ref | ref | ref | ref | ref | ref | ref | ref | ref |
| 90–104 | 1.27(1.14–1.41) | 1.28(1.21–1.36) | 1.18(1.11–1.25) | 1.25(1.12–1.39) | 1.27(1.19–1.35) | 1.18(1.11–1.24) | 1.18(1.05–1.33) | 1.13(1.06–1.21) | 1.10(1.04–1.17) |
| 105–114 | 1.83(1.59–2.11) | 1.72(1.58–1.86) | 1.48(1.35–1.62) | 1.78(1.55–2.06) | 1.69(1.56–1.83) | 1.47(1.34–1.61) | 1.48(1.27–1.73) | 1.40(1.28–1.53) | 1.31(1.19–1.44) |
| ≥115 | 3.09(2.68–3.57) | 2.32(2.11–2.55) | 1.85(1.63–2.10) | 2.98(2.58–3.45) | 2.27(2.06–2.49) | 1.86(1.64–2.10) | 2.22(1.89–2.61) | 1.72(1.55–1.91) | 1.50(1.31–1.72) |
Model 1: Crude model
Model 2: Adjusted for ethnicity
BMI Model 3: Adjusted for ethnicity, annual income, alcohol intake, physical activity, smoking status, diabetes, and study arms (interventions)
WC Model 3: Adjusted for ethnicity, height, annual income, alcohol intake, physical activity, smoking status, diabetes, study arms (interventions)
Again, in all age groups, higher BMI was no longer a significant risk factor when WC was added, but a larger WC was associated with a higher mortality rate regardless of whether BMI was included in the models (data not shown).
Sensitivity analysis
The sensitivity analysis results were not significantly different from the results in the primary analysis. Upon excluding all smokers, the increased HR in the underweight group was attenuated (slightly reduced), but it did not significantly change the overall findings (data not shown).
DISCUSSION
Findings from this large and multiethnic cohort demonstrate that being overweight or slightly obese is not associated with a significantly increased mortality rate in postmenopausal women. Similar to most published studies (34, 35), a U-shaped curve for the relationship between BMI and mortality, and a close to linear relationship between WC and mortality were observed across each racial/ethnic and age group, as well as in the entire WHI sample. This study also supports previous studies showing a higher mortality rate among underweight women. However, some of our findings from Hispanic women are different from findings in other studies.
Hispanic paradox
Our study shows that Hispanic women in the WHI enjoyed a lower mortality rate at any given BMI and WC compared to non-Hispanic whites or African-Americans. This finding is consistent with previous reports showing that in spite of a lower socioeconomic standing, Hispanics have a lower total age-adjusted mortality rate in comparison to their non-Hispanic white and African-American counterparts after age 45 (36). Healthy immigrants (37) and the healthy aging population due to earlier selection by other diseases in infanthood and younger adulthood are some possible explanations (38). However, Hispanics show higher cause-specific mortality rates in certain conditions, such as liver disease, cervical cancer, AIDs, homicides and diabetes according to published studies (39–41).
While previous findings among Hispanic populations (42, 43) show no association of obesity with all-cause mortality, our study suggests that obesity is associated with increased risk of all-cause mortality in Hispanic women. Furthermore, this association may be even stronger in Hispanic women than in African-American or non-Hispanic white women, even after adjusting for diabetes. The discrepancy between previous studies and our study may be related to levels of acculturation, or sex differences. Indeed, in a large analysis of the association of WC with mortality, a stronger association of WC with mortality was found among Hispanic women as compared to men (17). These results suggest that obesity, especially central obesity, has a significant negative impact on older Hispanic women’s survival, and highlight an important area deserving further research.
Older age paradigm
Being overweight or slightly obese (BMI between 25 and 34.9) was not a significant risk factor for an increased mortality rate after adjusting for ethnicity and some confounding factors. Our results agreed with most of studies in older people. A review on 28 published studies in people 65 or older (2) suggests that normal healthy BMI level may be higher for the elderly, as elderly with BMI between 25 and 30 kg/m2 did not show significantly increased mortality. In contrast, another review of 57 studies on people from 35 to 89 years old showed that people with BMI in the ‘normal weight’ range had a significant survival advantage (3). It is likely that the different conclusions from the two reviews are due to age differences in the study samples. Overweight may indicate metabolic disorder in the younger age group. However, in the elderly it may reflect better nutrition status or a result of survivorship from earlier cardiovascular death associated with obesity. A recent review on BMI by Flegal and colleagues (44) found that overweight is protective for all-cause premature death, and grade I obese is not associated with an increased mortality risk in adult individuals. Interestingly, in Flegal’s review for older people (65 and up), BMI over 35 was not even associated with a significantly increased risk of mortality, which is supported by our study.
While obesity may significantly increase people’s risk for multiple diseases and mortality, collectively, there is convincing evidence showing that overweight individuals, especially elderly individuals, do not show an increased mortality rate. Importantly, being underweight is a significant risk for premature death even after excluding the impact of smoking. Poor nutrition may be one explanation. A recent publication from frail women in WHI cohort also found a strong association between underweight and mortality, especially in frail women without cancer, emphysema, cardiovascular disease, diabetes mellitus or a history of smoking; in contrast, women with BMI larger than 25 kg/m2 had a lower mortality rate (35). These cumulative findings send an important public health message for managing a healthy body weight in aging women, suggesting that a healthy BMI should be higher than 25 kg/m2 for women over age 50.
In this study, a WC larger than 80– 89 cm was significantly correlated with an increased mortality risk in all age and BMI categories. This result is in agreement with other studies (12, 45). We have also found that the survival benefit may extend to women with a WC lower than 79 cm. In contrast to the findings from general obesity as measured by BMI, central obesity measured by WC is more consistently related to mortality in all age and ethnic groups in our study. Interestingly, when WC and BMI were both included in the models, BMI was no longer a risk factor for mortality, or in some cases, was protective. However, larger WC was still significantly associated with increased risk of mortality. This finding further supports the importance of central fat (as measured by WC) rather than general obesity (as measured by BMI) for health.
Visceral fat is a known risk factor for cardiometabolic disease (46). Larger WC reflects higher visceral fat content, likely explaining the stronger and consistent positive association of WC with mortality (11). However, WC is not routinely measured in clinical settings because of technical difficulties, especially in older and obese people. Furthermore losing height may bias BMI calculations.
Our study is strengthened by the large sample, resulting in more precise estimates of relative risk. The high rate of complete follow-up (99% with at least one follow up) as well as the prospective design decreased the chance of recall bias or bias as a result of loss to follow-up. Furthermore, anthropometric measurements were directly taken by our trained staff instead of self-reports. The comprehensive WHI data allowed controlling for potential confounding factors. Analyzing data by race/ethnicity and age, as well as combining the effects of BMI and WC are some of the unique features of this study which were not present, or not possible, in previous studies. Finally, there are few large longitudinal studies evaluating the relationship between obesity and all-cause mortality in Hispanic or African-American postmenopausal women, so our study contributes to our understanding in this area. However, because the study participants came from the WHI, our results may only apply to older postmenopausal women who self-select to participate in research. Taking these strengths and limitations into consideration, our findings on the similarities and differences across ethnic/racial groups may contribute to our understanding of human variation and health disparities, and help towards fine-tuning clinical guidelines and public health policies.
In conclusion, this large and multiethnic study in older women provides additional evidence for the need to use different healthy BMI ranges in older women, and further supports the more important role of central obesity rather than general obesity in mortality risk. The ethnic differences among Hispanic women in the magnitude of the association between BMI and mortality are intriguing and not consistent with previous findings, and thus deserving of further research.
Acknowledgments
Funding Source: This work was supported by the Women's Health Initiative (WHI), which is funded by the National Heart, Lung, and Blood Institute through contracts HHSN268201100046C, HHSN268201100001C, HHSN268201100002C, HHSN268201100003C, HHSN268201100004C, and HHSN271201100004C.
Footnotes
| Elements of Financial/Personal Conflicts |
* Zhao Chen |
Yann C. Klimentidis |
Jennifer W. Bea |
Kacey C. Ernst |
Chengcheng Hu |
Rebecca Jackson |
Cynthia A. Thomson |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Yes | No | Yes | No | Yes | No | Yes | No | Yes | No | Yes | No | Yes | No | |
| Employment or Affiliation |
x | x | X | x | x | X | X | |||||||
| Grants/Funds | x | x | X | x | x | X | X | |||||||
| Honoraria | x | x | X | x | x | X | X | |||||||
| Speaker Forum | x | x | X | x | x | X | X | |||||||
| Consultant | x | x | X | x | x | X | X | |||||||
| Stocks | x | x | X | x | x | X | X | |||||||
| Royalties | x | x | X | x | x | X | X | |||||||
| Expert Testimony | x | x | X | x | x | X | X | |||||||
| Board Member | x | x | X | x | x | X | X | |||||||
| Patents | x | x | X | x | x | X | X | |||||||
| Personal Relationship |
x | x | X | x | x | X | X | |||||||
Author Contributions:
Zhao Chen: study design; data collection; data analysis; interpretation of data; drafting, reviewing, and revising, and final approval of the manuscript
Yann C. Klimentidis: interpretation of data; reviewing, and revising, and final approval of the manuscript
Jennifer W. Bea: interpretation of data; reviewing, and revising, and final approval of the manuscript
Kacey C. Ernst: interpretation of data; reviewing, and revising, and final approval of the manuscript
Chengcheng Hu: data analysis; interpretation of data; reviewing, and revising, and final approval of the manuscript
Rebecca Jackson: study design; data collection; interpretation of data; reviewing, and revising, and final approval of the manuscript
Cynthia A. Thomson: study design; data collection; interpretation of data; reviewing, and revising, and final approval of the manuscript
REFERENCES
- 1.Bales CW, Buhr G. Is obesity bad for older persons? A systematic review of the pros and cons of weight reduction in later life. J Am Med Dir Assoc. 2008;9(5):302–312. doi: 10.1016/j.jamda.2008.01.006. [DOI] [PubMed] [Google Scholar]
- 2.Janssen I, Mark AE. Elevated body mass index and mortality risk in the elderly. Obes Rev. 2007;8(1):41–59. doi: 10.1111/j.1467-789X.2006.00248.x. [DOI] [PubMed] [Google Scholar]
- 3.Prospective Studies C. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009 doi: 10.1016/S0140-6736(09)60318-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Strain GW, Zumoff B. The relation of weight-height indices of boesity to body fat content. J Am Coll Nutr. 1991;11:715–718. doi: 10.1080/07315724.1992.10718272. [DOI] [PubMed] [Google Scholar]
- 5.Hartz A, He T, Rimm A. Comparison of adiposity measures as risk factors in postmenopausal women. J Clin Endocrinol Metab. 2012;97(1):227–233. doi: 10.1210/jc.2011-1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Folsom AR, Kushi LH, Anderson KE, Mink PJ, Olson JE, Hong CP, et al. Associations of general and abdominal obesity with multiple health outcomes in older women: the Iowa Women's Health Study. Arch Intern Med. 2000;160(14):2117–2128. doi: 10.1001/archinte.160.14.2117. [DOI] [PubMed] [Google Scholar]
- 7.Katzmarzyk PT, Craig CL, Bouchard C. Adiposity, adipose tissue distribution and mortality rates in the Canada Fitness Survey follow-up study. Int J Obes Relat Metab Disord. 2002;26(8):1054–1059. doi: 10.1038/sj.ijo.0802057. [DOI] [PubMed] [Google Scholar]
- 8.Lahmann PH, Lissner L, Gullberg B, Berglund G. A prospective study of adiposity and all-cause mortality: the Malmo Diet and Cancer Study. Obes Res. 2002;10(5):361–369. doi: 10.1038/oby.2002.50. [DOI] [PubMed] [Google Scholar]
- 9.Pischon T, Boeing H, Hoffmann K, Bergmann M, Schulze MB, Overvad K, et al. General and abdominal adiposity and risk of death in Europe. N Engl J Med. 2008;359(20):2105–2120. doi: 10.1056/NEJMoa0801891. [DOI] [PubMed] [Google Scholar]
- 10.Simpson JA, MacInnis RJ, Peeters A, Hopper JL, Giles GG, English DR. A comparison of adiposity measures as predictors of all-cause mortality: the Melbourne Collaborative Cohort Study. Obesity (Silver Spring) 2007;15(4):994–1003. doi: 10.1038/oby.2007.622. [DOI] [PubMed] [Google Scholar]
- 11.Visscher TL, Seidell JC, Molarius A, van der Kuip D, Hofman A, Witteman JC. A comparison of body mass index, waist-hip ratio and waist circumference as predictors of all-cause mortality among the elderly: the Rotterdam study. Int J Obes Relat Metab Disord. 2001;25(11):1730–1735. doi: 10.1038/sj.ijo.0801787. [DOI] [PubMed] [Google Scholar]
- 12.Cerhan JR, Moore SC, Jacobs EJ, Kitahara CM, Rosenberg PS, Adami HO, et al. A pooled analysis of waist circumference and mortality in 650,000 adults. Mayo Clin Proc. 2014;89(3):335–345. doi: 10.1016/j.mayocp.2013.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fontaine KR, Redden DT, Wang C, Westfall AO, Allison DB. Years of life lost due to obesity. JAMA. 2003;289(2):187–193. doi: 10.1001/jama.289.2.187. [DOI] [PubMed] [Google Scholar]
- 14.Reis JP, Macera CA, Araneta MR, Lindsay SP, Marshall SJ, Wingard DL. Comparison of overall obesity and body fat distribution in predicting risk of mortality. Obesity (Silver Spring) 2009;17(6):1232–1239. doi: 10.1038/oby.2008.664. [DOI] [PubMed] [Google Scholar]
- 15.Cohen SS, Signorello LB, Cope EL, McLaughlin JK, Hargreaves MK, Zheng W, et al. Obesity and all-cause mortality among black adults and white adults. Am J Epidemiol. 2012;176(5):431–442. doi: 10.1093/aje/kws032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Katzmarzyk PT, Mire E, Bray GA, Greenway FL, Heymsfield SB, Bouchard C. Anthropometric markers of obesity and mortality in white and African American adults: the pennington center longitudinal study. Obesity (Silver Spring) 2013;21(5):1070–1075. doi: 10.1002/oby.20151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Koster A, Leitzmann MF, Schatzkin A, Mouw T, Adams KF, van Eijk JT, et al. Waist circumference and mortality. Am J Epidemiol. 2008;167(12):1465–1475. doi: 10.1093/aje/kwn079. [DOI] [PubMed] [Google Scholar]
- 18.Stevens J, Keil JE, Rust PF, Tyroler HA, Davis CE, Gazes PC. Body mass index and body girths as predictors of mortality in black and white women. Arch Intern Med. 1992;152(6):1257–1262. [PubMed] [Google Scholar]
- 19.Hays J, Hunt JR, Hubbell FA, Anderson GL, Limacher M, Allen C, et al. The Women's Health Initiative recruitment methods and results. Ann Epidemiol. 2003;13(9 Suppl):S18–S77. doi: 10.1016/s1047-2797(03)00042-5. [DOI] [PubMed] [Google Scholar]
- 20.Prentice R, Rossouw JE, Furberg C, Johnson S, Henderson M, Cummings S, et al. Design of the WHI Clinical Trial and Observational Study. Control Clin Trials. 1998;19:61–109. doi: 10.1016/s0197-2456(97)00078-0. [DOI] [PubMed] [Google Scholar]
- 21.Beresford SA, Johnson KC, Ritenbaugh C, Lasser NL, Snetselaar LG, Black HR, et al. Low-fat dietary pattern and risk of colorectal cancer: the Women's Health Initiative Randomized Controlled Dietary Modification Trial. JAMA. 2006;295(6):643–654. doi: 10.1001/jama.295.6.643. [DOI] [PubMed] [Google Scholar]
- 22.Howard BV, Van Horn L, Hsia J, Manson JE, Stefanick ML, Wassertheil-Smoller S, et al. Low-fat dietary pattern and risk of cardiovascular disease: the Women's Health Initiative Randomized Controlled Dietary Modification Trial. JAMA. 2006;295(6):655–666. doi: 10.1001/jama.295.6.655. [DOI] [PubMed] [Google Scholar]
- 23.Jackson RD, LaCroix AZ, Gass M, Wallace RB, Robbins J, Lewis CE, et al. Calcium plus vitamin D supplementation and the risk of fractures. N Engl J Med. 2006;354(7):669–683. doi: 10.1056/NEJMoa055218. [DOI] [PubMed] [Google Scholar]
- 24.Prentice RL, Caan B, Chlebowski RT, Patterson R, Kuller LH, Ockene JK, et al. Low-fat dietary pattern and risk of invasive breast cancer: the Women's Health Initiative Randomized Controlled Dietary Modification Trial. JAMA. 2006;295(6):629–642. doi: 10.1001/jama.295.6.629. [DOI] [PubMed] [Google Scholar]
- 25.The Women's Health Initiative Steering Committee. Effects of Conjugated Equine Estrogen in Postmenopausal Women With Hysterectomy. The Women’s Health Initiative Randomized Controlled Trial. JAMA. 2004;291:1701–1712. doi: 10.1001/jama.291.14.1701. [DOI] [PubMed] [Google Scholar]
- 26.The Writing Group for the Women's Health Initiative Investigators. Risks and Benefits of Estrogen Plus Progestin in Healthy Postmenopausal WomenPrincipal Results From the Women's Health Initiative Randomized Controlled Trial. JAMA. 2002;288(3):321–333. doi: 10.1001/jama.288.3.321. [DOI] [PubMed] [Google Scholar]
- 27.Wactawski-Wende J, Kotchen JM, Anderson GL, Assaf AR, Brunner RL, O'Sullivan MJ, et al. Calcium plus vitamin D supplementation and the risk of colorectal cancer. N Engl J Med. 2006;354(7):684–696. doi: 10.1056/NEJMoa055222. [DOI] [PubMed] [Google Scholar]
- 28.Curb JD, McTiernan A, Heckbert SR, Kooperberg C, Stanford J, Nevitt M, et al. Outcomes ascertainment and adjudication methods in the Women's Health Initiative. Ann Epidemiol. 2003;13(9 Suppl):S122–S128. doi: 10.1016/s1047-2797(03)00048-6. [DOI] [PubMed] [Google Scholar]
- 29.Cauley JA, Wu L, Wampler NS, Barnhart JM, Allison M, Chen Z, et al. Clinical risk factors for fractures in multi-ethnic women: the Women's Health Initiative. J Bone Miner Res. 2007;22(11):1816–1826. doi: 10.1359/jbmr.070713. [DOI] [PubMed] [Google Scholar]
- 30.Kristal AR, Feng Z, Coates RJ, Oberman A, George V. Associations of race/ethnicity, education, and dietary intervention with the validity and reliability of a food frequency questionnaire: the Women's Health Trial Feasibility Study in Minority Populations. Am J Epidemiol. 1997;146(10):856–869. doi: 10.1093/oxfordjournals.aje.a009203. [DOI] [PubMed] [Google Scholar]
- 31.Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults--The Evidence Report. National Institutes of Health. Obes Res. 1998;6(Suppl 2):51S–209S. [PubMed] [Google Scholar]
- 32.Berrington de Gonzalez A, Hartge P, Cerhan JR, Flint AJ, Hannan L, MacInnis RJ, et al. Body-mass index and mortality among 1.46 million white adults. N Engl J Med. 2010;363(23):2211–2219. doi: 10.1056/NEJMoa1000367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bertone-Johnson ER, Powers SI, Spangler L, Larson J, Michael YL, Millen AE, et al. Vitamin D supplementation and depression in the women's health initiative calcium and vitamin D trial. Am J Epidemiol. 2012;176(1):1–13. doi: 10.1093/aje/kwr482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Winter JE, MacInnis RJ, Wattanapenpaiboon N, Nowson CA. BMI and all-cause mortality in older adults: a meta-analysis. Am J Clin Nutr. 2014;99(4):875–890. doi: 10.3945/ajcn.113.068122. [DOI] [PubMed] [Google Scholar]
- 35.Zaslavsky O, Rillamas-Sun E, LaCroix AZ, Woods NF, Tinker LF, Zisberg A, et al. Association Between Anthropometric Measures and Long-Term Survival in Frail Older Women: Observations from the Women's Health Initiative Study. J Am Geriatr Soc. 2016;64(2):277–284. doi: 10.1111/jgs.13930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Turra CM, Goldman N. Socioeconomic differences in mortality among U.S. adults: insights into the Hispanic paradox. J Gerontol B Psychol Sci Soc Sci. 2007;62(3):S184–S192. doi: 10.1093/geronb/62.3.s184. [DOI] [PubMed] [Google Scholar]
- 37.Abraido-Lanza AF, Dohrenwend BP, Ng-Mak DS, Turner JB. The Latino mortality paradox: a test of the "salmon bias" and healthy migrant hypotheses. Am J Public Health. 1999;89(10):1543–1548. doi: 10.2105/ajph.89.10.1543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hummer RA, Powers DA, Pullum SG, Gossman GL, Frisbie WP. Paradox found (again): infant mortality among the Mexican-origin population in the United States. Demography. 2007;44(3):441–457. doi: 10.1353/dem.2007.0028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chen NE, Gallant JE, Page KR. A systematic review of HIV/AIDS survival and delayed diagnosis among Hispanics in the United States. J Immigr Minor Health. 2012;14(1):65–81. doi: 10.1007/s10903-011-9497-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lariscy JT, Nau C, Firebaugh G, Hummer RA. Hispanic-White Differences in Lifespan Variability in the United States. Demography. 2015 doi: 10.1007/s13524-015-0450-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Siegel R, Naishadham D, Jemal A. Cancer statistics for Hispanics/Latinos, 2012. CA Cancer J Clin. 2012;62(5):283–298. doi: 10.3322/caac.21153. [DOI] [PubMed] [Google Scholar]
- 42.Fontaine KR, McCubrey R, Mehta T, Pajewski NM, Keith SW, Bangalore SS, et al. Body mass index and mortality rate among Hispanic adults: a pooled analysis of multiple epidemiologic data sets. Int J Obes (Lond) 2012;36(8):1121–1126. doi: 10.1038/ijo.2011.194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mehta T, McCubrey R, Pajewski NM, Keith SW, Allison DB, Crespo CJ, et al. Does obesity associate with mortality among Hispanic persons? Results from the National Health Interview Survey. Obesity (Silver Spring) 2013;21(7):1474–1477. doi: 10.1002/oby.20105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Flegal KM, Kit BK, Orpana H, Graubard BI. Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA. 2013;309(1):71–82. doi: 10.1001/jama.2012.113905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jacobs EJ, Newton CC, Wang Y, Patel AV, McCullough ML, Campbell PT, et al. Waist circumference and all-cause mortality in a large US cohort. Arch Intern Med. 2010;170(15):1293–1301. doi: 10.1001/archinternmed.2010.201. [DOI] [PubMed] [Google Scholar]
- 46.Chiba Y, Saitoh S, Takagi S, Ohnishi H, Katoh N, Ohata J, et al. Relationship between visceral fat and cardiovascular disease risk factors: the Tanno and Sobetsu study. Hypertens Res. 2007;30(3):229–236. doi: 10.1291/hypres.30.229. [DOI] [PubMed] [Google Scholar]