Abstract
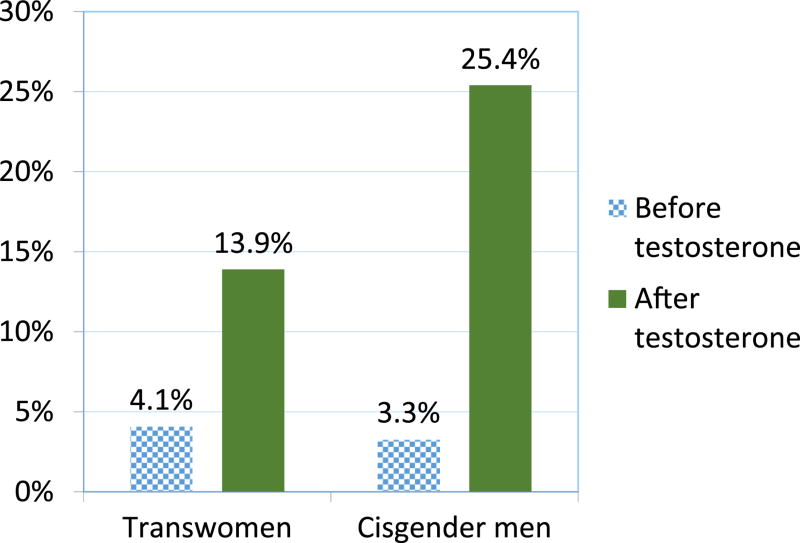
Little research has explored the link between the behavioural effects of testosterone use among transmen and HIV risk. We conducted a mixed methods study to explore testosterone use among transmen and the behavioural effects on HIV risk. A sample of 122 transmen from San Francisco participated in a cross-sectional quantitative survey and 14 transmen participated in 2 focus group discussions. Most participants (81.9%) were currently taking hormones. Participants attributed testosterone use to new sexual behaviours among 69% of transmen, changes in sexual attractions (49%), and increased frequency of sexual activity (72%). Among current testosterone users, 3.3% had cisgender men as partners before starting testosterone, whereas after starting testosterone, 25.4 % did. Similarly, 4.1% had a transgender woman as a sexual partner before starting testosterone and 13.9% after starting testosterone. Findings suggest that testosterone’s side effects were associated with transmen’s desires for sex with cisgender men who have sex with men. The reported increase in attraction to and sex with partners from populations with a high HIV prevalence may have important implications for HIV risk among transmen, especially as the availability of transgender health services may draw transmen to an area where HIV prevalence is high.
Keywords: Transmen, sexual practices, sexual risk, testosterone, USA
Introduction
Thirty years into the epidemic, HIV still disproportionately affects minority groups in the USA, especially men who have sex with men, racial and ethnic minorities, injection drug users, and transwomen (The Kaiser Family Foundation 2014). Less is understood about the burden of HIV among transmen. Studies of transmen have found HIV prevalence rates ranging from 0% (Kenagy and Bostwick 2005; Kenagy and Hsieh 2005; Conare, Cross, and Little 1997) to 3% (Xavier et al. 2005; Clements-Nolle et al. 2001). These findings, however, are limited by small sample sizes, non-probability based sampling techniques, and the inability to disaggregate trans-specific data in HIV surveillance data. In the USA, transgender status is not collected in national HIV/AIDS case surveillance data, a policy that masks HIV infection rates among transmen (Chen et al. 2011).
Investigators have expressed concern that transmen are at risk for HIV due to their sexual partnerships with cisgender men who have sex with men (Rowniak et al. 2011), who are disproportionately impacted by HIV. In addition, the high rates of substance use, mental health disorders, social isolation, economic marginalisation, and unmet healthcare needs, all known contributors to HIV risk behaviours, are disproportionately experienced by transmen (Herbst et al. 2008). Many of these factors reflect the health disparities of the broader LGBT population. Furthermore, the use of hormone therapy, particularly testosterone, to achieve medical transition has not been explored as a risk factor.
Despite the lack of population-based data, many experts believe that testosterone use among transmen is widespread, as it is both an affordable and effective method of gender transition (Sevelius 2010). Although some qualitative studies have suggested a link between testosterone and increased risk behaviour (Rowniak et al. 2011; Sevelius 2009; Reisner, Perkovich, and Mimiaga 2010), to date no quantitative research has explored this link and its possible mediators. Further research is needed to better understand the sexual behaviours of transmen, and whether testosterone affects risk via heightened sexual risks and increased desire for cisgender men who have sex with men sexual partners. To address gaps in the literature, we conducted a mixed methods study to explore testosterone use among transmen and to investigate whether testosterone affects risk for HIV among transmen in San Francisco.
Methods
This research is part of STRIPE, a larger study of transmen that was conducted between 2013 and 2015 by the San Francisco Department of Public Health’s Center for Public Health Research. The research aim of STRIPE was to estimate the population size, HIV prevalence, and HIV-risk behaviours of transmen in San Francisco. Data from focus group discussions and a cross-sectional survey with transmen were used for this analysis.
Formative Research
Prior to the focus groups and survey administration reported here, key informant interviews were conducted with members of the population and other community stakeholders to inform the development of the focus groups discussion guide, quantitative questionnaire, and to generate a universe of venues in San Francisco frequented by transmen.
Focus Group Discussions
Focus group discussion participants were recruited through referrals from San Francisco Department of Public Health (SFDPH) staff and members of the transmen community. Participants for the focus group discussion were recruited purposively to achieve demographic diversity (e.g. race/ethnicity, sexual orientation). The semi-structured focus group guide included a range of topics, including reasons for testosterone therapy initiation; effects of hormone therapy on emotions, physiology, and sexual behaviours; perceived HIV-risk; and sexual behaviours. Participants were invited to the San Francisco Department of Public Health to participate in focus group discussion. Focus groups were moderated by a student researcher, a cisgender gay man (RD). Both of the two focus groups lasted approximately 90 minutes.
Cross-sectional survey of transmen
Transmen were recruited to receive an HIV test and to take part in a cross-sectional survey using time location sampling (MacKellar et al. 2002; Valleroy, MacKellar, Karon, Rosen, McFarland, Shehan, Stoyanoff, LaLota, Celentano, and Koblin 2000). The universe of venues in San Francisco frequented by transmen generated from key informant interviews included bars, clubs, businesses, organisations, bathhouses, street locations, and other public venues. Recruitment venues were randomly selected from the list of venues. When the identified venues were no longer productive (specifically when no new individuals were identified during random recruitment times), the research team began recruitment from online venues (such as OK Cupid and Scruff). Subsequently transmen were invited to recruit peers from their social networks to participate in the survey. Eligibility criteria for the survey included: 1) being at least 18 years of age, 2) self-identifying as a transgender man, or as a gender other than female having been assigned a female sex at birth, 3) being English speaking, and 4) living working, or residing in San Francisco. Eligibility was determined using a brief screening interview (Valleroy, MacKellar, Karon, Rosen, McFarland, Shehan, Stoyanoff, LaLota, Celentano, Koblin, et al. 2000). Participants for the focus group discussions and survey received a list of referrals and resources as well as $50 as reimbursement for time spent. Participants who referred peers received $10 per eligible participant enrolled. The study protocol was approved by the Institutional Review Board at the University of California, San Francisco.
Quantitative Measures
The survey questionnaire was based on previous surveys used with groups at risk for HIV in San Francisco, including a study of transwomen, and further informed by the focus group and key informant data (Santos et al. 2014; Rapues et al. 2013). The survey included measures of socio-demographics, surgery and hormone use, reported side effects of testosterone, health care access, HIV and STI history, sexual behaviours, and drug and alcohol use.
Demographic variables included self-reported age, race/ethnicity, educational attainment, annual income, and employment status. Self-reported testosterone side effect variables included genital dryness, genital tears or fissures, changes in sexual behaviour, sexual attraction, and increased frequency of sex since starting testosterone (all yes/no). Health care access variables included health insurance status, number of visits to a health care provider in the prior 12 months, history of gynaecological care, history of mental health care, and comfort discussing transgender status with a health care provider. HIV and STI variables included history of HIV or STI infection and site of STI infection.
Sexual behaviour variables included questions about participants’ three most recent sexual partners in the prior six months from the following groups: cisgender women, cisgender men, transwomen, and transmen. Participants were also asked to report the sexual orientation of each partner. In addition, for each partner, participants were asked about frequency of insertive and receptive vaginal sex, insertive and receptive anal sex, and insertive and receptive oral sex in the prior six months, including whether the sex was protected or unprotected. Drug and alcohol use variables included frequency of alcohol and marijuana use in the last six months, frequency of injection drug use in the last 12 months, history of sharing needles or syringe, frequency of non-injection drug use in the last 12 months, and history of drug or alcohol treatment.
Surveys were interviewer-administered and took up to 90-minutes to complete. Participants provided verbal informed consent and completed the survey anonymously. HIV testing was conducted using Insti rapid tests (bioLytical, Vancouver, CA) with results available within one minute.
Data Analysis
Focus group discussions were audiotaped and transcribed. The transcriptions were analysed employing a thematic approach. Transcripts were coded independently by the student researcher (RD) and a study collaborator (CA). The researchers read and discussed subsections of the material corresponding to specific codes or intersections of codes, and summarised findings in analytic memos. Memos were analysed to describe the themes presented below.
Quantitative data were analyzed with Stata version 12.1 (StataCorp, College Station, TX). Primary outcomes of interest included testosterone use and HIV risk behaviours. We used descriptive statistics to examine sample characteristics, prevalence of hormone therapy, and HIV risk behaviours. Prevalence was calculated with 95% confidence intervals (CIs).
We first present our quantitative results. We then contextualise the findings with our qualitative data to illustrate the possible influence of testosterone on HIV-risk among transmen in San Francisco.
Results – Quantitative findings
We recruited 122 transmen over 14 months. Eleven were recruited in the venue only phase, 10 in the venue and online venue phase and 101 in the venue, online venue and social network phase. Of note, only 32 participants were recruited through social networks during the final phase of recruitment (Figure 1).
Figure 1.
Recruitment process, transmen, San Francisco, 2014–2015.
Of the 122 transmen, 77.1% reported being White, while 6.6%, 3.3%, 4.9%, and 8.2% reported being Black, Latino, Asian, and Other race/ethnicity, respectively. Ages ranged from 18 to 56 years old, with a median of 28.0 years. A majority (86.1%) had some college education or greater. The median annual income was $26,000 (IQR, $10,000–$45,000). Over half of respondents (52.5%) reported sex with a cisgender woman in the prior 6 months, while 36.9%, 22.1%, and 32.8% reported sex with a cisgender men, transgender man, and transgender woman, respectively. Only 17.2% of participants thought transmen were low risk for HIV. No participants tested positive for HIV in the study.
Almost half of participants (49.2%) reported any surgical procedures, most of whom were using testosterone (97%). The most common surgery was top surgery (n=58), with two people reporting having a phalloplasty. Most participants (86.1%) reported ever using hormones, while 81.9% of participants were currently taking hormones. Two-thirds (66.4%) of those who had ever used hormones obtained a prescription for hormone therapy from a primary care provider (Table 1). Among the 100 participants currently using testosterone, 30% said that testosterone had caused genital dryness and 14% said they experienced genital tearing due to dryness. Eighty-nine percent (89%) of participants reported that testosterone increased their libido. In terms of testosterone’s perceived effect on sexual behaviour, 49% of participants reported that their sexual attractions changed after taking testosterone. Sixty-nine percent (69%) reported that testosterone led to new sexual behaviours. Seventy-two percent reported that testosterone had increased the frequency of their sexual activity. (Table 2). Before starting testosterone, 3.3% of transmen currently using testosterone had cisgender men as partners whereas after starting testosterone, 25.4 % did. Similarly, 4.1% of transmen currently using testosterone had a transgender woman as a sexual partner before starting testosterone, whereas after starting testosterone, this percentage increased to 13.9% (Figure 2).
Table 1.
Demographics, sexual behaviour, hormone use, and HIV prevalence among transmen, San Francisco, 2014–2015 (N = 122)
| Variable | N (%) |
|---|---|
| Age | Median 28.0 y.o.; Range 18–56 |
| 18–25 | 43 (35.3) |
| 26–35 | 60 (49.2) |
| 36–45 | 8 (6.6) |
| 46+ | 11 (9.1) |
| Race/Ethnicity* | |
| White | 94 (77.1) |
| Black | 8 (6.6) |
| Latino | 4 (3.3) |
| Asian | 6 (4.9) |
| Other / mixed race | 10 (8.2) |
| Highest Level of Education Attained | |
| Below High School | 4 (3.3) |
| High School or GED | 10 (8.2) |
| Some College | 48 (3.93) |
| Bachelor’s | 44 (36.1) |
| Post-Graduate | 16 (13.1) |
| Income | Median $26,000, IQR ($10,000–$45,000) |
| Sexual Behaviours in the Last 6 Months* | |
| Cis-female partners | 64 (52.5) |
| Cis-male partners | 45 (36.9) |
| Transgender female partners | 27 (22.1) |
| Transgender male partners | 40 (32.8) |
| Are Transmen at Low-Risk for HIV? | |
| Yes | 21 (17.2) |
| Health Care | |
| Ever Hormone Use | 105 (86.1) |
| Prescribed by primary care provider | 81 (66.4) |
| Currently Using Hormones | 100 (81.9) |
| Currently Using Testosterone | 100 (81.9) |
| HIV Infected, by testing data | 0 (0) |
Table 2.
Testosterone Use and Side Effects among transmen on testosterone therapy, San Francisco, 2014. (n= 100)
| Variable | N (%) |
|---|---|
| As a side effects of testosterone, did you experience… | |
| Increased libido | 89 (89.0) |
| Genital dryness | 30 (30.0) |
| Genital tearing | 14 (14.0) |
| Changes in sexual attraction | 49 (49.0) |
| New sexual behaviours | 69 (69.0) |
| Increased frequency of sexual activity | 72 (72.0) |
Figure 2.
Proportion of participants reporting cisgender men who have sex with men and transwomen sexual partners before and after testosterone use, San Francisco, 2014–2015.
The 27 participants who reported sex with a transgender woman in the prior 6 months reported a total of 1062 sex acts (oral, anal or vaginal) with 39 partners. Of the 1062 acts, 101 (9.5%) and 26 (2.4%) were unprotected receptive vaginal and unprotected receptive anal sex acts, respectively. The 45 participants who had sex with cisgender male partners in the last 6 months reported a total of 856 sex acts (oral, anal or vaginal) with 97 partners (two-thirds of which were men who have sex with men). Of these acts, 118 (13.8%) and 7 (0.8%) were unprotected receptive vaginal and unprotected receptive anal sex acts, respectively (Figure 3).
Figure 3.
Sexual acts, unprotected receptive vaginal acts, unprotected receptive anal acts, transmen, San Francisco, 2014–2015.
Results – Qualitative findings
Fourteen transmen, 20 to 44 years of age, participated in two focus groups. Fifty-seven (57%) percent identified as White, 21% as Black, 14% as Latino, and 8% as Asian/Pacific-Islander. Our analysis of the focus group data identified four major themes about the relationship between testosterone and sexual behaviours: 1) increased libido, 2) emotional changes and detachment, 3) unwelcome physiologic changes, and 4) more attraction and availability of cisgender men as sexual partners.
Increased Libido
Participants in the focus groups reported that for many transmen, initiating testosterone was accompanied by a marked increase in libido. One participant expressed not feeling prepared for the frequency and intensity of his sexual urges:
I didn’t know what to do with my libido. There wasn’t an off button.
(J, 31 y.o.)
Another participant likened his reaction to testosterone as a second puberty, which was a time when his libido was also very high.
I was 20 or 21 but it’s like being 12 or 13 again. I was jerking off multiple times a day. (B, 26 y.o.)
Changes in Sexual Partnerships
Many participants described a new attraction to cisgender male partners.
A lot of trans guys are sleeping with men and no one’s acknowledging that. There’s even a lot of straight-identified trans guys who sleep with men because their sexual attractions change. Or they come to a different sense of themselves and they’re like, “Oh, this might be fun” or “I’m curious to try this.” ? (K, 36 y.o.)
For some participants, presenting physically as male meant negotiating sexual interest from cisgender men who have sex with men for the first time.
There’s this old adage that testosterone makes you gay. I don’t know if that’s necessarily true, but you’re kind of queer-identified to begin with and then your sex drive goes way up, and you’re getting sexual attention from people you maybe weren’t getting it from before. And so it can be relieving to suddenly have an outlet for that sex drive. (T, 40 y.o.)
Emotional changes and detachment
Participants reported that initiating hormone therapy precipitated changes in mood and emotional processing that were as tangible as the physical changes associated with transition.
Testosterone changes the chemistry of your brain. Everything you’re experiencing physically is also happening inside your skull. (B., 26 y.o.)
Some participants spoke of a newfound “emotional detachment,” which they described as an ability to filter out emotions that would otherwise compete with their desires. For some participants, this emotional detachment allowed them to engage in casual sex without feelings of remorse or ambivalence.
After transitioning, I can say, ‘There’s a hot guy” and we can just have sex. And then peace out. That doesn’t happen when you’re a female. And that’s from my ability to detach, to filter emotionally. That came after I started testosterone. (L., 22 y.o.)
Another participant described emotional detachment as a kind of male privilege:
Testosterone gave me a level of armour, and I want to say male armour. And I think of stereotypical guys who are just like “whatever.” But that helped me cope and gave me skills, because it was a level of detachment. (Z., 25 y.o.)
Unwelcome physiological changes
In addition to emotional changes that accompanied transition, participants spoke of unwelcome physiological changes, such as vaginal dryness or tearing, phenomena that could interfere with sex or even lead to anxiety about STI risks.
We have to worry about the other biological effects of testosterone, like our junk changing. Fissures during sex or tearing because of the testosterone thinning the vaginal walls. All of these new things I never had to consider before transitioning. (R., 23 y.o.)
For gay-identified transmen who have not transitioned surgically, being a receptive partner may lead to differential risks relative to their men who have sex with men peers due to differences in internal anatomy.
My doctor told me my anatomy was putting me at higher risk. She said, ‘You’ve been doing the same thing that cisgender guys are doing but your [vaginal] anatomy puts you at higher risk for bacterial infections. And I think that’s something that we don’t talk about. What is our risk for STIs compared to our cisgender gay male peers that are doing the exact same things? (K., 36 y.o.)
Other participants spoke of a change in their orgasms after starting testosterone, which sometimes led to new sexual behaviours and practices.
My orgasms changed, and not for the better. I was like, ‘I have to figure out new ways to have sex because my orgasms aren’t as fulfilling.’ (B., 26 y.o.)
Discussion
Our study represents the first to quantitatively examine the effects of testosterone on sexual behaviours in a community-based sample of transmen. Our participants reported that initiating testosterone was associated with increased libido and frequency of sex, increased interest in casual sexual partnerships, and a change in sexual partner preferences, an important constellation of factors that can inform future HIV prevention efforts. Furthermore, increased genital dryness and genital fissures attributed to testosterone by participants may represent novel routes for sexual transmission of HIV.
An overwhelming majority of participants in the sample had ever used hormones as part of their physical transition, and roughly 4 in 5 were currently taking testosterone. Rates of other methods of physical transition, like gender confirmation surgery, were much lower, suggesting that hormone therapy is the primary method by which most transmen in San Francisco accomplish and maintain gender transition.
The reported increased attraction to cisgender men who have sex with men who have a high population prevalence of HIV in San Francisco (SFDPH 2014), may have important implications for understanding the HIV-risk of transmen. This is particularly relevant in our study of transmen in San Francisco since its robust transgender health services may serve to draw transmen to the city. There was a convergence in our qualitative and quantitative findings that transmen associate testosterone’s side effects with increased interest in sex with cisgender men who have sex with. Reisner et al. found that transmen who had sex with men only were more likely to have engaged in sexual risk behaviour in the prior three months. (Reisner, Perkovich, and Mimiaga 2010) Researchers have recently documented that in San Francisco nearly 1 in 4 men who have sex with men are HIV-positive (Raymond et al. 2013). White men make up the majority of new HIV cases among men who have sex with men (45% in 2014), followed by Latinos, Asian, African Americans and multi-race men. (SFDPH 2014) Given the high risk cisgender gay and other men who have sex with men face in San Francisco, transmen in this sample with such partners may be also be at elevated risk for HIV. Participants also reported a shift in sexual attraction to transwomen partners. Transwomen in San Francisco are also disproportionately affected by HIV. Researchers have also recently reported that 39% of trans women in San Francisco are living with HIV, only half of whom are virologically suppressed.(Santos et al. 2014) Our findings regarding sexual partners and behaviours on testosterone in this population warrant further longitudinal research.
We found no cases of HIV among transmen, perhaps speaking to the fact that the vast majority of sex acts reported by participants were while using condoms. Yet without HIV incidence or prevalence data, particularly at the population level, it is difficult to fully assess the HIV-risk of transmen in San Francisco. Future research is needed to determine whether the susceptibility to HIV among transmen is similar to that of other marginalised groups, and if it is not, what factors might explain the resiliency of this community. Systematic inclusion of transmen in surveillance data nationally is also needed.
While this study advances our understanding of a group that has been largely invisible in the HIV prevention literature, there are several limitations to our results. First, though their income was low, respondents to the quantitative survey were largely young, white and well-educated. Many may have been students or recent graduates with potential upward mobility. We have no benchmark for the racial/ethnic and educational composition of the transmen population in San Francisco. Future studies could expand this inquiry by purposefully recruiting a sample of transmen with more diversity in regard to race/ethnicity and educational background. Second, our cross-sectional survey design limits our ability to make causal inferences about the relationship between testosterone therapy and HIV-risk. The influence of testosterone on HIV-risk may be confounded by the experience of gender transition more broadly. Third, the high prevalence of hormone use among the sample also limited our statistical ability to compare hormone users to non-users. Fourth, our sampling may have over-represented gay-identified transmen given the relative dearth of transgender spaces in general and the prominence of gay culture in San Francisco. Finally, given the uniqueness of the HIV epidemic in San Francisco as well as the breadth and quality of its transgender services, we recommend caution before generalising our findings to other cities.
Despite these limitations, these data point to important associations between of testosterone and changes in sexual behaviour observed among transmen, especially with regard to increased sexual behaviour with cisgender men who have sex with men and transwomen. Providers can play an important role in HIV prevention by explaining to patients that hormone therapy could result in changes in their sexual behaviours, desires, experiences, and needs. With further longitudinal research, accurate sexual health information, HIV prevention messaging and programmes for this population, we have an opportunity to prevent an HIV epidemic among transmen in San Francisco and nationally.
References
- Chen S, McFarland W, Thompson HM, Raymond HF. Transmen in San Francisco: what do we know from HIV test site data? AIDS Behavior. 2011;15(3):659–62. doi: 10.1007/s10461-010-9859-9. [DOI] [PubMed] [Google Scholar]
- Clements-Nolle K, Marx R, Guzman R, Katz M. HIV prevalence, risk behaviors, health care use, and mental health status of transgender persons: implications for public health intervention. American Journal of Public Health. 2001;91(6):915–21. doi: 10.2105/ajph.91.6.915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conare K, Cross L, Little M. Needs assessment of transgendered people in Philadelphia for HIV/AIDS and other health and social services. Philadelphia, PA: ActionAIDS; 1997. [Google Scholar]
- Herbst JH, Jacobs ED, Finlayson TJ, McKleroy VS, Neumann MS, Crepaz N. Estimating HIV prevalence and risk behaviors of transgender persons in the United States: a systematic review. AIDS Behavior. 2008;12(1):1–17. doi: 10.1007/s10461-007-9299-3. [DOI] [PubMed] [Google Scholar]
- Kenagy GP, Hsieh CM. The risk less known: female-to-male transgender persons' vulnerability to HIV infection. AIDS Care. 2005;17(2):195–207. doi: 10.1080/19540120512331325680. [DOI] [PubMed] [Google Scholar]
- Kenagy Gretchen P, Bostwick Wendy B. Health and social service needs of transgender people in Chicago. International Journal of Transgenderism. 2005;8(2–3):57–66. [Google Scholar]
- MacKellar Duncan A, Valleroy Linda A, Secura Gina M, Bartholow Brad N, McFarland William, Shehan Douglas, Ford Wesley, LaLota Marlene, Celentano David D, Koblin Beryl A. Repeat HIV testing, risk behaviors, and HIV seroconversion among young men who have sex with men: a call to monitor and improve the practice of prevention. Journal of Acquired Immune Deficiency Syndromes. 2002;29(1):76–85. doi: 10.1097/00042560-200201010-00011. [DOI] [PubMed] [Google Scholar]
- Rapues J, Wilson EC, Packer T, Colfax GN, Raymond HF. Correlates of HIV infection among transfemales, San Francisco, 2010: results from a respondent-driven sampling study. American Journal of Public Health. 2013;103(8):1485–92. doi: 10.2105/AJPH.2012.301109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raymond HF, Bereknyei S, Berglas N, Hunter J, Ojeda N, McFarland W. Estimating population size, HIV prevalence and HIV incidence among men who have sex with men: a case example of synthesising multiple empirical data sources and methods in San Francisco. Sexually Transmitted Infections. 2013;89(5):383–7. doi: 10.1136/sextrans-2012-050675. [DOI] [PubMed] [Google Scholar]
- Reisner SL, Perkovich B, Mimiaga MJ. A mixed methods study of the sexual health needs of New England transmen who have sex with nontransgender men. AIDS Patient Care STDS. 2010;24(8):501–13. doi: 10.1089/apc.2010.0059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rowniak S, Chesla C, Rose CD, Holzemer WL. Transmen: the HIV risk of gay identity. AIDS Education and Prevention. 2011;23(6):508–20. doi: 10.1521/aeap.2011.23.6.508. [DOI] [PubMed] [Google Scholar]
- Santos GM, Wilson EC, Rapues J, Macias O, Packer T, Raymond HF. HIV treatment cascade among transgender women in a San Francisco respondent driven sampling study. Sexually Transmitted Infections. 2014;90(5):430–3. doi: 10.1136/sextrans-2013-051342. [DOI] [PubMed] [Google Scholar]
- Sevelius J. "There's no pamphlet for the kind of sex I have": HIV-related risk factors and protective behaviors among transgender men who have sex with nontransgender men. J Assoc Nurses AIDS Care. 2009;20(5):398–410. doi: 10.1016/j.jana.2009.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sevelius J. What are transgender men’s HIV prevention needs? UCSF Center for AIDS Prevention Studies Fact Sheet 67 2010 [Google Scholar]
- SFDPH. HIV Epidemiology Annual Report. San Francisco, CA: San Francisco Department of Public Health, Population Health Division, Applied Research, Community Health Epidemiology, and Surveillance Branch (ARCHES); 2014. [Google Scholar]
- The Kaiser Family Foundation. The HIV/AIDS Epidemic in the United States. http://kfforg/hivaids/fact-sheet/the-hivaids-epidemic-in-the-united-states/
- Valleroy LA, MacKellar DA, Karon JM, Rosen DH, McFarland W, Shehan DA, Stoyanoff SR, et al. HIV prevalence and associated risks in young men who have sex with men. Young Men's Survey Study Group. JAMA. 2000;284(2):198–204. doi: 10.1001/jama.284.2.198. [DOI] [PubMed] [Google Scholar]
- Valleroy Linda A, MacKellar Duncan A, Karon John M, Rosen Daniel H, McFarland William, Shehan Douglas A, Stoyanoff Susan R, LaLota Marlene, Celentano David D, Koblin Beryl A. HIV prevalence and associated risks in young men who have sex with men. JAMA. 2000;284(2):198–204. doi: 10.1001/jama.284.2.198. [DOI] [PubMed] [Google Scholar]
- Xavier Jessica M, Bobbin Marilyn, Singer Ben, Budd Earline. A needs assessment of transgendered people of color living in Washington, DC. International Journal of Transgenderism. 2005;8(2–3):31–47. [Google Scholar]