Abstract
Objective
To define the different breastfeeding interventions that promote breastfeeding exclusivity and duration in the late preterm infant and to synthesize findings from the published empirical literature on late preterm infant breastfeeding interventions.
Data Sources
The databases CINAHL, Scopus, and PubMed were searched for primary research articles on breastfeeding interventions for late preterm infants. Inclusion criteria included original research studies in which authors examined a breastfeeding intervention or second-line strategy in a sample inclusive of but not necessarily limited to the gestational age range of 34 to 36 6/7 weeks gestation, written in English, and published between 2005 and 2015.
Study Selection
Thirteen articles were identified, including five randomized controlled trials, three quasi-experimental studies, four descriptive studies, and one case study.
Data Extraction
Whittemore and Knafl’s methodology guided this integrative review. Data extraction and organization occurred under the following headings: author and year, study design, level of evidence, purpose, sample, setting, results, limitations, recommendations, and intervention.
Data Synthesis
Studies on breastfeeding interventions were synthesized under four concepts within the Late Preterm Conceptual Framework: Physiologic Functional Status, Care Practices, Family Role, and Care Environment.
Conclusions
The majority of the breastfeeding interventions within this integrative review had positive effects on exclusivity and duration of breastfeeding in the late preterm infant. However, second line strategies were equivocal on exclusivity but had positive effects on duration. Results highlight the positive effects of breastfeeding interventions on breastfeeding exclusivity and duration and points to the need for a focus on breastfeeding after the transition home for late preterm infants.
Keywords: Late preterm infant, breastfeeding intervention, integrative review
The rate of preterm births in the United States in 2015 increased to 9.62%, which was the first increase since 2007 (Hamilton, Martin & Osterman, 2016; March of Dimes, 2013). Late preterm infants born at 34 0/7 to 36 6/7 weeks gestation comprise 70% of this vulnerable population (Hamilton, 2014). The physiologic immaturities of late preterm infants place them at risk for respiratory distress, jaundice, hypoglycemia, hypothermia, and feeding difficulties (Kugelman & Colin, 2013). Many of these morbidities lead to readmission rates as high as 33%, which affect inpatient and outpatient health care costs (Berard, Le Tiec, & De Vera, 2012; Mally, Bailey, & Hendricks-Munoz, 2010; McLaurin, Hall, Jackson, Owens, & Mahadevia, 2009). In particular, feeding difficulties in late preterm infants who are breastfed place them at risk for inadequate intake, a significant predictor of re-hospitalization (Tomashek et al., 2006; Young, Korgenski, & Buchi, 2013). Infants who breastfeed successfully have fewer respiratory tract infections that require hospitalization, less otitis media, and fewer gastro-intestinal tract infections, as well as a long-term reduction in childhood diabetes (American Academy of Pediatrics [AAP], 2012). Moreover, breastfeeding mothers experience reduced risk of postpartum depression and certain cancers (Hamdan & Tamim, 2012; Stuebe, 2009).
Because breastmilk is a superior form of nutrition, it is important to examine interventions that promote adequate intake of breastmilk. Therefore, the purpose of this review, guided by the Late Preterm Conceptual Framework (Association of Women’s Health, Obstetric & Neonatal Nurses [AWHONN], 2013), was to integrate results from primary research studies examining the effect of breastfeeding promotion interventions for late preterm infants on breastfeeding exclusivity and duration.
Background
Breastfeeding is the leading influential factor for infant health (AAP, 2012). Researchers demonstrated that breastfeeding provides significant gastrointestinal, immunological, nutritional, and psychological benefits (Beattie & Weaver, 2011; Ip et al., 2007). In addition, breastfeeding provides maternal benefits, including a lower risk of maternal type 2 diabetes and reduced risk for the development of breast and ovarian cancer (Stuebe, 2009). The AAP (2012) and World Health Organization (2008) recommended exclusive breastfeeding for the first six months of life and continued breastfeeding (with addition of complementary foods) through the child ’s first or second years (World Health Organization [WHO], 2008).
Despite the reported benefits of breastfeeding, mothers of infants born at 35 to 36 weeks gestation are less likely to start breastfeeding and continue breastfeeding for six months than mothers of infants born at 37–39 weeks gestation (Ayton et al., 2012). The late preterm infant’s size and weight often resemble those of a term infant, which creates confusion among parents and health care professionals regarding the level of care needed during hospitalization after birth and unique feeding requirements caused by developmental differences. Thus, the late preterm infant is at a greater risk of morbidity than term counterparts.
Physical immaturities in late preterm infants can lead to severe respiratory distress, hypoglycemia, and hypothermia that require escalation of care and separation of the infant from the mother and delay initiation of breastfeeding (Boyle et al., 2015; Marrocchella et al., 2014). Additionally, in late preterm infants, neuronal immaturity affects oro-motor tone that causes poor suck-swallow coordination, decreased intraoral pressure, and an inadequate suck (AWHONN, 2010; Polin & Fox, 2010). Because the 34-week gestation mark is the point at which the suck, swallow, and breathe reflexes begins to develop and properly function, this lack of development contributes to the late preterm infant’s unique feeding challenges (Hallowell & Spatz, 2012).
Late preterm infants appear closer in size and weight to full-term infants, but because of their unique developmental and physiologic needs, they require adjusted day-to-day care. In addition, late preterm infants have difficulty maintaining a cycle of alertness and deep sleep, resulting in rapid fatigue and sleepiness during at-breast feeds, with subsequent detachment from the nipple (Meier, Patel, Wright, & Engstrom, 2013). These feeding immaturities result in inadequate emptying of the breast, which can lead to a decreased milk supply because breast milk production decreases to the level of demand (Meier et al., 2013). With inadequate milk intake and a decreasing milk supply, feeding-related morbidities, including dehydration, failure to thrive, and hyperbilirubinemia, can occur and cause re-hospitalization (Shapiro-Mendoza, et al., 2006).
Several maternal factors have also been associated with breastfeeding difficulties in the late preterm infant, including decreased self-efficacy and anxiety regarding feeding difficulties. Zanardo et al. (2011) found that maternal anxiety was one of the most significant independent risk factors for early breastfeeding failure in the late preterm population. Anxiety has the potential to affect milk supply and breastfeeding continuation through physiological and behavioral pathways (e.g., dampening of the milk ejection reflex and avoidance behavior that leads to infrequent breastfeeding or milk expression; Dewey, 2001).
The breastfeeding difficulties experienced by mothers of late preterm infants often result in the implementation of second line strategies to maintain at-breast feeds and the maternal milk supply. The use of nipple shields, cup feeding, triple feeding (breastfeeding, pumping, and bottle-feeding), bottle (formula) supplementation, supplemental nursing systems, and syringe feedings provide the infant with sufficient nutrition while maternal breastfeeding skills are improved (Meier et al., 2013). However, in some studies, the addition of syringe feedings, supplemental nursing systems, and nipple shields reduced breastfeeding self-efficacy and led to shorter duration of breastfeeding (Keemer, 2013; McQueen, Dennis, Stremler, & Norman, 2011; Nichols, Schutte, Brown, Dennis, & Price, 2009).
To address late preterm feeding challenges and reduce morbidities, the Academy of Breastfeeding Medicine (ABM, 2011) recommended the following: initiation of breastfeeding by a half hour after birth; rooming-in to facilitate skin-to-skin care and on-demand breastfeeding; support of a lactation specialist to educate mothers on techniques to facilitate adequate breastfeeding and alternative feeding methods, including second line strategies; and early and frequent follow-up in outpatient settings to monitor weight gain weekly until 40 weeks post conceptual age. Early and frequent follow-up are needed to track breastfeeding patterns, to assess the need for lactation support, and to adjust feedings as indicated to increase exclusive breastfeeding in late preterm infants (ABM, 2011). Although recommendations are in place for this population, research is lacking in regard to breastfeeding interventions for the unique needs of infants specifically born at 34 to 36 6/7 weeks gestation.
The Late Preterm Conceptual Framework
The Association of Women’s Health, Obstetric, and Neonatal Nurses (AWHONN, 2013) developed the Late Preterm Conceptual Framework to address developmental and physiologic disparities between the late preterm and infants born at term. The framework consists of four concepts: physiologic functional status, nursing care practices, care environment, and family role. These four concepts are interrelated and necessary to promote optimal, healthy outcomes in the late preterm infant within the newborn period and throughout the lifetime (Medoff Cooper et al., 2005; see Figure 1).
Figure 1.

Conceptual model for optimizing late preterm infant outcomes. From AWHONN Late Preterm Infant Initiative. http://www.awhonn.org/page/AWHONNLateInfant/AWHONN-Late-Preterm-Infant-Initiative.htm ©2013 Association of Women’s Health, Obstetric and Neonatal Nurses. Reprinted with permission.
Physiologic functional status includes physical and functional well-being determined by postmenstrual age, transition to extrauterine life, maternal-fetal health and history, timing and method of delivery, and location and quality of care (AWOHNN, 2013). The definition of nursing care practices includes the type and quality of care provided by registered or advanced practice nurses. A multidisciplinary approach is encouraged in the care of the late preterm infant including physicians, nurses, developmental specialists, lactation consultants, and social service professionals (AWOHNN, 2013). The care environment encompasses the location and social, cultural, political, and economic contexts of care provided to the late preterm infant. The family role is defined as the measure of family involvement in the care of the late preterm infant (AWOHNN, 2013).
Design
In order to provide the strongest rigor for this integrative review, we applied the Whittemore and Knafl’s (2005) integrative review method, which includes a systematic approach to problem identification, literature search, data evaluation, and data analysis. The initial step of the integrative review was to identify the problem and enable recognition of important variables to create a feasible scope for the literature search. The literature search included all relevant literature using multiple databases to provide optimal primary source retrieval and reduce bias. The data analysis stage required data reduction, display, and comparison. Interpretation of the data required reduction into subgroups, i.e. levels of evidence. Analysis continued with extraction of data into previously established criteria and subgroups based on the Late Preterm Conceptual Framework (Whittemore & Knafl, 2005). The results of the analysis are provided in table format to allow for comparison and contrast of studies and to facilitate synthesis. See Table 1 published with the online version of this article. The final step of this integrative review was to develop conclusions regarding represented data.
Table 1.
Late Preterm Breastfeeding Promotion Interventions That Affect Breastfeeding Exclusivity and Duration By Level of Evidence
| Author | Study Design | Level of Evidence | Study Purpose | Sample | Setting | Results | Limitations | Recommendations |
|---|---|---|---|---|---|---|---|---|
| Morelius, 2015 | Randomized controlled trial Continuous skin-to-skin care (SSC) versus general practice of SSC | 1a | To evaluate the effect of almost continuous skin-to-skin contact for late preterm infants, to study the concordance between the mothers’ and the preterm infants’ salivary cortisol levels at four moth corrected age, a third outcome was to study parental stress, depression, and breastfeeding | N = 42 Gestational age 32 to 35 6/7 weeks | NICU and post discharge | Exclusive and duration of breastfeeding: All infants n=18 in the SSC group were breastfeeding partly or exclusively at discharge compared to 16 out of 19 in the SC group but reported as not significant. More infants were breastfeeding partly or exclusively in the SSC group, compared to the SSC group at one and four months, but the differences did not reach significance. | Unable to provide a control group of no skin-to-skin | Rapid development of
regularity Facilitates spouse relationship No statistical significance in improving the rate of breastfeeding |
| Hayes Brook/2008 | Randomized controlled trial Kangaroo care versus standard care procedure (wrapped when being held) | 1b | To determine the effects of kangaroo care (KC)
on breastfeeding status in mother-preterm infant dyads from postpartum
through 18 months Hypothesis: Breastfeeding exclusivity would be greater and duration would be longer for dyads experiencing KC, than for control dyads experiencing standard care |
A subsample of 66 mothers and their preterm
infants (32–36 completed weeks gestation, 1,300–3,000 g,
5 minute Apgar > or = 6)who intended to breastfeed (n=36 in the KC group and n = 30 in the control group) |
NICU/post partum unit and post discharge |
Duration of Breastfeeding
: KC dyads, compared to control dyads, breastfed
significantly longer (5.08 months vs 2.05 months), p =
.003. Exclusive Breastfeeding: KC dyads also breastfed more exclusively from hospital discharge through 18 months (p = .047). At six months statistically the difference was statistically significant (p=.041) |
Duration and exclusivity during follow-up were
based entirely on self-report by the mothers. Control group did not receive the same attention from researchers as the intervention group (control group received care from staff versus the intervention group receiving care from researchers |
Kangaroo care is an effective way to
facilitate breastfeeding exclusivity and duration Need to look at amount and timing of kangaroo care Need to look at infants of other gestational ages |
| Rao et al/2008 | Prospective randomized controlled Trial (Kangaroo Care versus Conventional Method Care) |
1b | To assess the effect of Kangaroo Mother Care (KMC) on growth of infants weight <2000 g at birth | 206
singleton KMC 45(43.7%) 35 to 36 weeks Control 47(45.6%) 35 to 36 weeks |
NICU/post partum/post discharge | KMC babies achieved significantly better
growth at the end of the study Head circumference p = 0.02 |
Poor follow-up in the control | Examining the effect of implementation in the community |
| Ravn et al/2011 | Randomized controlled trial (Intervention group versus without intervention group) | 1b | Assess the effects of the Mother-Infant Transaction program on maternal depression and stress, breastfeeding and mothers’ perception of infant temperament and impact on preterm infant communication skills at 12 months | Gestational age of 30 to 36
weeks Intervention Group 19(33.9%) Control 17 (34%) |
Not identified | Breastfeeding duration: At 9 months 34.1% mothers in the intervention group were not breastfeeding their infants compared with 60% in the control group (p = .02). At 12 months (61.9%) versus (80%) (p=.07) | Results not broken down per gestational
age Limited to Norwegian background Small sample size |
Further follow-up of this cohort |
| Yilmaz et al/2014 | Randomized Controlled trial Cup (treatment) Versus Bottle (control) |
1b | Determine the effect of bottle and cup feeding
on breastfeeding rates in 32 to 35 week late preterm infants during
hospital stay, as well as upon discharge at 3 and 6
months Hypothesis: Cup feeding of late preterm infants could improve breastfeeding rates. |
Infants born between 32 to 35 week gestation
late preterm infants Cup feeding started at 35 week gestation Total = 522 Bottle = 268 Cup = 254 |
NICU and post discharge |
Exclusive
Breastfeeding: Infants randomized to the cup-feeding
versus bottle feeding method more like to be exclusively breastfed on
Discharge home (RR 1.58, 95% CI,
1.36–1.83) Duration of Breastfeeding 3 months (RR, 1.64, 95% CI, 1.42–1.89) 6 months (RR, 1.36, 95% CI, 1.14–1.63) No significance in weight gain at seven days between bottle and cup feedings (p=.64) |
Breastmilk and formula spillage were not
measured. No data on infant weight beyond day seven Analysis were not by intention to treat 85 infants were excluded because of noncompliance with the randomly assigned oral feeding protocol and development of a disease preventing oral feeding Inability to generalize results to all preterm infants as study participants were only late preterm infants |
Further studies recommended for those infants born more premature |
| Flacking/2010 | Prospective longitudinal | 2a | Rapid development of
regularity Facilitates spouse relationship No statistical significance in improving the rate of breastfeeding |
103 very preterm infants (<32
gestational weeks) NICU 197 preterm (32–36 weeks) |
NICU and post discharge |
Duration of
Breastfeeding: Very preterm infant dyads that breastfeed
experienced more time in kangaroo mother care than Very preterm infants
that did not breastfeed at 1 (p=.04), 2 (p=.04), 5
(p=.01), and 6 months (p=.04); no significant
differences could be detected at 3 (p=.08) or 4 months
(p=.06). In the preterm group, no differences were observed
between those dyads that breastfed and those that did
not. Exclusive breastfeeding: The association between duration of kangaroo mother care per day and exclusive versus partial breastfeeding at 1 and 6 months and were not significant at all gestational ages. |
Lack of study group identified as late preterm infant (34 to 36 6/7 week gestation) | All efforts should be made to keep mothers and infants together |
| Maastrup et al, 2014 | Prospective Observational (Questionnaires and structured telephone interviews) | 2a | To investigate the association between early breastmilk expression, early initiation of skin-to-skin contact, rooming-in, nipple shield use, test-weighting, and pacifier use, and the establishment of exclusive breastfeeding at discharge, as well as, at a predefined interval after discharge, in order to gain more evidence on which to base guidelines for mothers to preterm infants in the NICU | Total n = 1488 Extremely preterm (24 to 27 weeks) = 60 Very preterm (28–31 weeks) = 257 Moderate preterm (32–34 weeks) = 688 Late preterm (35–36) =483 |
NICU/post partum/post discharge |
Exclusive breastfeeding
66% of those mothers using a nipple shield were not exclusively
breastfeeding at discharge (p<0.0001) 61% of infants receiving skin-to-skin were exclusively breastfeeding at discharge (p<0.0001) Mother and infant admitted to NICU was significant with 31% exclusively breastfeeding at discharge compared to 22% not exclusively breastfeed (p<0.01) Duration of breastfeeding Use of nipple shields was associated with a higher OR for inadequate breastfeeding duration (OR 1.4 (95% CI 1.1–1.9). |
Results not broken down per gestational
age Findings based on mother’s self-report Results could not be generalized to all late preterm infants, as late preterm infants admitted to NICUs have more health problems than late preterm infants care for in maternity units. |
Restriction of nipple shields to preterm
infants. First time mothers, smokers, mothers with lower level of education, mothers of infants less than 32 weeks and mothers of multiples should be given special breastfeeding support and guidance |
| Mattsson et al/2015 | Prospective Comparative Study | 2a | To compare the influence of supplementary
artificial milk feeds on breast feeding and certain clinical parameters
among healthy late preterm infants given regular supplementary
artificial milk feeds with late preterm infants exclusively breastfed
from birth. Clinical parameters:
|
Postpartum/post discharge | Infants given artificial milk on a regular
basis had their first initial breast feeding later than infants who were
exclusively breastfed (p<0.01). Exclusive breastfeeding: Exclusively breastfed infants had a shorter duration of hospital stay (P<0.01). Duration of breastfeeding: 87% of infants exclusively breastfed from birth continued after discharge (p<0.001). |
Findings based on mother’s
self-report Alteration of WHO’s definition of exclusive breastfeeding |
Findings based on mother’s
self-report Alteration of WHO’s definition of exclusive breastfeeding |
Observation and self-reports would strengthen
results Longitudinal breastfeeding data would help to strengthen findings |
| Niela-Vilen et al./2013 | Structured Survey | 2a |
|
Finland Hospital A
N=76 Hospital B N – 94 Divided: < 32 weeks very preterm ≥32 to<37 weeks late preterm ≥ 37 sick full term |
NICU | Exclusive Breastfeeding: Hospital A – 47% of the late preterm infant who had had early physical contact with their mothers were fully or partially breast fed, while the same was true for 34% of the late preterm infants who had not had early physical contact with their mothers (p=0.49).. Hospital B were 82% and 36%. The strongest association between early contact and breast feeding was with the late preterm infants in Hospital B (p = 0.014). | Inadequate sample size (unable to reach
recommended sample size of 10 subjects for each item of the
instrument) Findings not generalizable due to the different populations of infants admitted between institutions |
Early physical contact essential for breastfeeding |
| Abouelfettoh/2009/Cairo Egypt | Quasi-experimental cohort Bottle (control) versus cup (intervention) |
2b |
|
Convenience sample of 60 late preterm infants
(30 in control and 30 in the intervention group) – at conclusion
of the study there were 25 mothers in the control group and 13 mothers
in the intervention group Mean gestational age of bottle group (35.3 weeks) Mean gestational age of cup group (34.9 weeks) |
NICU and post discharge | Medium effect size and a power of
80% PIBBS score higher in the cup feeding group (p=<0.01) Duration of Breastfeeding: At one week after discharge there was a higher proportion of breastfeeding in the cup feeding group than in the bottle feeding group (p=0.03). Exclusive Breastfeeding: No statistical differences between the two groups in relation to the type of breastfeeding (either exclusive or partial)p=0.29. |
A randomized experimental design not
used The principal investigator collected all of the data – not blinded Determination of breastfeeding practices should have continued longer after discharge (Low maternal education levels made long term documentation not feasible). Small sample size Gestational age reported in means |
Cup feeding preterm infants as a form of supplementation may support increased duration of breastfeeding. |
| Olson et al/2010 | Quasi-experimental (Peer counselor versus no peer counselor) | 2b | To estimate the effectiveness of a peer counselor breastfeeding program for low income women in Michigan | 336 women who requested services prenatally
and were contacted by a peer counselor (treatment)/6 54 women who
requested services prenatally but were not contacted by a peer counselor
(control) Treatment 36.4 weeks gestation Control 36.9 weeks gestation |
NICU or otherwise not identified/post discharge |
Breastfeeding duration:
The treatment group breastfed 2.6 weeks longer than the control group
(p<.001). Treatment group was 22.3% more likely to initiate breastfeeding (p<.001), 9% more like to breastfeed at 3 months (p=.002) and 6.2% more likely to breastfeed at 6 months (p=.008). |
A randomized controlled study would help to collaborate findings from this study due to how women were contacted | Cost benefit analysis for feasibility of implementation |
| Wataker, 2012 | Quasi-experimental design (Family Care program versus Traditional Care) | 2b | To investigate the effects of a Family Care Program in a NICU on maternal confidence and breastfeeding compared with mothers in a comparable NICU offering traditional care without such room facilities | Family Care Group (n=36)
(31.4–34.0) 32.7 weeks gestation Control Group (n= 30)(33.7–35.7) 34.7 weeks gestation. |
NICU/post discharge |
Duration of
breastfeeding: At 3 months: No
breastfeeding FC group 6(26%), Control group 12(57%)(p = .04) Partly breastfeeding FC Group 1(4%) Control 0(0%)(p = >.99) Full breastfeeding FC group 16(70%) Control 9(43%)(p = .07) |
Study had a small sample size No Randomization Fathers’ participation was not assessed. |
Further studies regarding maternal assessment of lactation support in both a FC environment and a traditional care environment. |
| Lucas et al/2014 | Case Presentation | 4 | Case presentation of a late preterm’s transition to full breastfeeding | 35 weeks | Not identified | Exclusive and Duration of breastfeeding Full breastfeeding achieved by 4 months | Need for further community based resources including lactation consultants, peer support groups and hospital grade pumps and scales |
Note. Levels of evidence: 1a: Systematic reviews of randomized controlled trials. 1b: Individual randomized controlled trials. 1c: All or none randomized controlled trials. 2a: Systematic reviews of cohort studies. 2b: Individual cohort study or low quality randomized controlled trials. 2c: “Outcomes” research; ecological studies. 3a: Systematic review of case-control studies. 3b: Individual case-control study. 4: Case-series. 5: Expert opinion with explicit critical appraisal, or based on physiology, bench research or first principles.
In this integrative review, we examined and grouped studies according to the Late Preterm Conceptual Framework (AWHONN, 2013). The primary outcome measures reported in the reviewed articles and thus included in this review were breastfeeding duration and breastfeeding exclusivity. The aim of the review was to define the breastfeeding interventions that promote breastfeeding duration and exclusivity as written in the ABM guidelines in the late preterm infant.
Search Method
We conducted a review of the literature to examine breastfeeding interventions for the late preterm infant. We searched the databases CINAHL, Scopus, and PubMed for primary research articles that addressed breastfeeding interventions for late preterm infants. The search terms prematurity and breastfeeding, preterm and breastfeeding, early term and breastfeeding, and late preterm and breastfeeding were entered into each database, and duplicate research articles were removed. Inclusion criteria included original research studies on breastfeeding intervention or second-line strategy in a sample inclusive of but necessarily limited to the gestational age range of 34 to 36 6/7 weeks, written in English, and published between 2005 and 2015. We used these dates as a direct correlation to the development and publication in 2005 of the Late Preterm Conceptual Framework (AWHONN, 2013). All titles and abstracts were reviewed for pertinence to the study aims and inclusion/exclusion criteria including gestational ages between 34 to 36 6/7 weeks gestation. Subsequently, we reviewed all abstracts obtained from these articles for inclusion/exclusion criteria. The selection process is presented in Figure 2.
Figure 2.
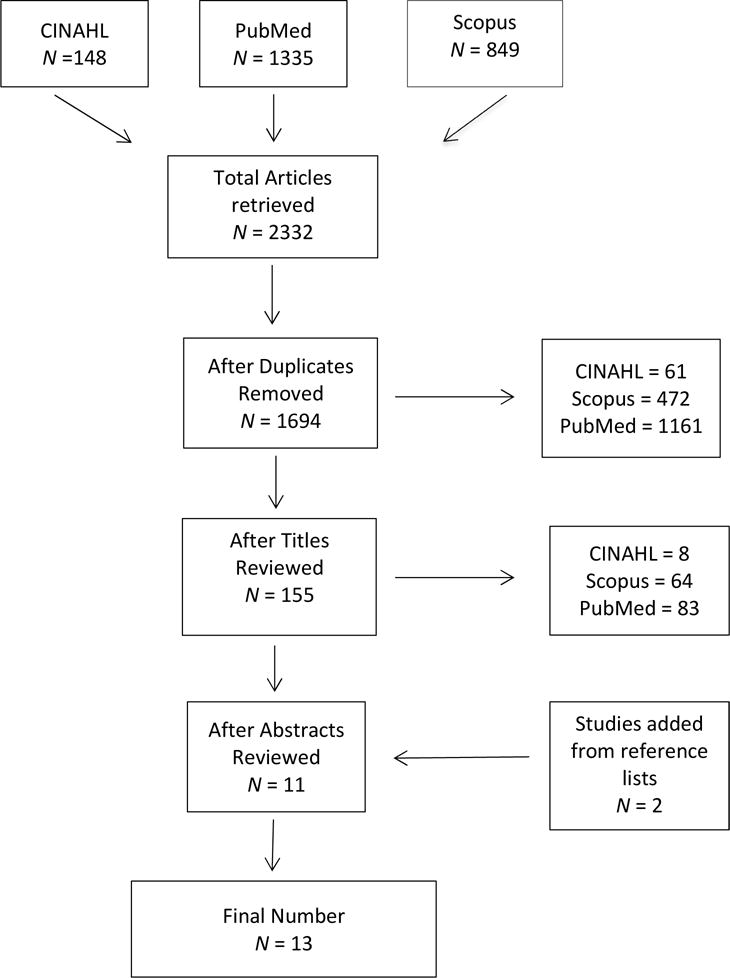
Flowchart of Literature Review
We used levels of evidence established by the Oxford Center for Evidence-Based Medicine (Centre for Evidence-Based Medicine, 2017) to evaluate the quality of the studies on a quick, concise, and uniform basis. Studies were grouped according to intervention content that affected exclusivity and duration of breastfeeding: interventions that support physiologic transition and feeding support; interventions that help to develop feeding practice guidelines to support those who provide care ; interventions that support feeding within different care environments: and interventions that educate and support the family in successful breastfeeding of their late preterm infant (AWOHNN, 2013).
Results
Initially, 1,694 articles were retrieved. After review of titles, 155 articles were retained. Our subsequent abstract review yielded 13 articles that are included in this review (Figure 2). The 13 articles included five randomized controlled trials, three quasi-experimental studies, four descriptive studies, and one case study. None of the studies that are included reported theoretical frameworks to guide research in the reviewed articles; however, the evidence from these articles collectively indicated that interventions supported exclusivity and increased duration of breastfeeding. The final 13 articles consisted of a total sample size of 3257 with a range of 1 to 990 participants. These studies were conducted in the United States, Norway, Turkey, Sweden, Finland, and India. The range of gestational ages was reported as 31.4 to 36 6/7 weeks with means reported as 32 to 36 weeks but only data pertinent to 34 to 36 6/7 week gestation from these articles was included. The sample included a range of mean hospital days as 3.3 to 25.96.
Definitions of Interventions
Skin-to-skin contact is often referred to as kangaroo care and is defined as care of an unclothed infant, unwrapped and placed against the mother’s bare chest (Nyqvist et al., 2013). Skin-to-skin care is advantageous because it significantly increases milk production and promotes longer breastfeeding duration (Hake-Brooks & Anderson, 2008; Renfrew, Craig & Dyson, et al., 2009). Cup feeding and triple feeding were the only second line strategies studied in the reviewed literature. Cup feedings entail the use of a soft, small flexible cup to feed the late preterm infant (Lawrence & Lawrence, 2011). Triple feeding is the process of breastfeeding at-breast, bottle feeding expressed breastmilk and/or formula to the infant, and pumping or expressing milk from one or both breasts to achieve adequate nutrition while preserving at-breast feeds and milk supply (Meier, 2010). Rooming-in, an element of family-centered care, gives the parents unrestricted access in the NICU so they can have 24-hour presence at the infant’s beside (Griffin, 2006). Rooming-in is also integrated in the care of the clinically stable late preterm infant remaining in the postpartum/newborn environment.
Physiologic Functional Status
One of the major interventions identified to promote exclusivity of breastfeeding was skin-to-skin care (Flacking et al., 2011; Hake-Brooks, 2008; Morelius et al., 2015). Skin-to-skin care helps to establish breastfeeding exclusivity and duration by enabling a smoother transition to extrauterine life by promoting temperature and heart rate regulation. Mature sleep organization, improved sleep cycling that resulted in less energy expenditure, and increased increase oxytocin release that stimulated increased milk production were observed with the use of skin-to-skin care (Ludington-Hoe, Johnson, & Morgan et al., 2006). The duration of skin-to-skin care did correlate with breastfeeding exclusivity and/or duration in 4 of 9 studies in which the practice was used (Flacking et al., 2011; Hake-Brooks et al., 2008; Lucas et al., 2013; Morelius et al., 2015).
The late preterm mother-infant dyads with more skin-to-skin time per day breastfed significantly longer, and the infants were given breast milk by breast only more often from discharge to 18 months of age (Flacking et al., 2011; Hake-Brooks et al., 2008). Of those studies including skin-to-skin care as an intervention, five studies lacked information on the effect on breastfeeding exclusivity and/or duration (Abouelfettoh et al., 2008; Maastrup et al., 2014; Mattsson et al., 2015; Niela-Vilen et al., 2013; Rao et al., 2008). Niela-Vilen et al. (2013) found that late preterm infants who experiences skin-to-skin care shortly after birth were more likely to display early feeding cues to begin breastfeeding than those infants not offered this care. In two studies, the late preterm infant had “better” growth, weight, length, and head circumference with the use of kangaroo care (Lucas et al., 2013; Rao et al., 2008).
Many late preterm infants require assistive devices to feed adequately, and second line strategies are innovative approaches to achieve exclusive breastfeeding. Three studies addressed successful breastfeeding outcomes with the use of second line strategies (Abouelfettoh et al., 2008, Lucas, et al., 2014; Yilmaz et al., 2014). In contrast, Maastrup et al. (2014) and Mattson et al. (2015) reported a decrease in exclusive breastfeeding and an increase in weight loss with the use of nipple shields as the second line strategy.
Researchers examined the use of cup feeding in the late preterm infants in two studies (Abouelfettoh et al., 2008; Yilmaz et al., 2014). In each of these studies, implementation of cup feeding rather than bottle-feeding helped to transition an increased number of late preterm infants to exclusive breastfeeding compared to control groups. Post-intervention, the cup feeding groups demonstrated more mature breastfeeding behaviors and an increased likelihood of being exclusively breastfed from discharge to 6 months compared to those who were bottle fed during the birth hospitalization (Abouelfettoh et al., 2008; Yilmaz et al., 2014).
Triple feeding and limited use of a nipple shield enabled a preterm infant to establish and maintain breastfeeding for 4 months in one case study (Lucas et al., 2014). Although Lucas et al. (2014) successfully increased breastfeeding duration using a combination of second line strategies, Maastrup et al., (2014) found that the use of nipple shields alone failed to contribute to exclusivity at discharge or an increase in the duration of breastfeeding.
Care Practices
Nursing care practices were represented in our review by the effectiveness of who delivered the breastfeeding educational interventions to the mothers of the late preterm infant. Nurses, peer counselors, and lactation consultants are important providers of breastfeeding education. Research in the effectiveness of nurses, peer counselors, and lactation consultants in breastfeeding education is an important tool in development of educational resources and evidence based clinical practice guidelines for the late preterm infant (Medoff-Cooper et al., 2005). Two studies addressed educational effectiveness, including a peer-supported educational intervention and an educational intervention provided by nurses in the intensive care setting (Olson et al., 2010; Ravn et al., 2012). In the Ravn et al. (2012) study, mothers who received instructions from neonatal nurses regarding their late preterm infant’s temperament and developmental potential, including feeding cues, were more likely still to be breastfeeding or providing breastmilk at 9 and 12 months than mothers who did not receive the intervention (Ravn et al., 2012). Olson et al. (2010) found that education and support for low-income mothers of late preterm infants using community peer counselors contributed to earlier initiation of breastfeeding after birth and a higher likelihood of breastfeeding at 3 and 6 months.
Care Environment
Mothers who room in with their infants have greater milk supply, breastfeed longer, and are more likely to breastfeed exclusively due to the increased physical contact (Bystrova, 2009). In our review, the relationship of rooming in to breastfeeding duration and exclusivity with implementation of family centered care was examined in one study. Wataker et al. (2012) encouraged mothers to room in with their late preterm infant and reported an increase in the mothers’ understanding of infants’ feeding cues, development of increased confidence, and increased duration and exclusivity of breastfeeding at 3 months (Wataker et al., 2012).
Family Role
Preparing parents to care for a late preterm infant involves establishing confidence and competence in their ability to care for their late preterm infant (Medoff-Cooper et al., 2005). In two studies, the effects on family role were investigated through two different interventions. As noted above, Wataker et al., (2012) encouraged mothers to room in with their infants, optimizing close contact. This extended period of close physical contact provided the ability of mothers to experience greater empowerment and confidence in taking care of the infant. In another study, targeting recognition of infants’ behavioral cues, Ravn et al., (2012) implemented an educational intervention that sensitized the mother to the recognition of feeding cues thus affecting the nutritional needs of her late preterm infant. In both of these investigations, breastfeeding duration and exclusivity increased.
Discussion
Examination of breastfeeding interventions in the late preterm infant have occurred only in a small number of studies. Our findings indicate that implementation of the three types of breastfeeding interventions increased exclusivity and duration of breastfeeding in this vulnerable population. Second line strategies were found to have an equivocal effect on exclusivity but a positive effect on duration of breastfeeding. Examination of outcomes when interventions were used in combination found either no effect or equivocal results in regards to exclusivity and duration of breastfeeding.
To support physiologic functional status, breastfeeding experts recommend tools to address feeding challenges and assist with breastfeeding late preterm infants (Meier et al., 2013). Kangaroo care, patient educational interventions, and rooming in are an effective means to promote breastfeeding exclusivity and duration in the late preterm infant. However, in our review interventions involving second line strategies were inconsistently associated with improvement in exclusivity and duration of breastfeeding in late preterm infants. Nevertheless, ABM (2012) recommends second line strategies and increased lactation support for late preterm infants, both during the birth hospitalization and after discharge, to ensure the adequacy of breastfeeding and optimal growth parameters. Moreover, the use of second line strategies is an effective way of assisting in milk transfer in late preterm infants (Meier, Furman, & Degenhardt, 2007). Findings from our integrative review are inconclusive about whether the use of second line strategies supports breastfeeding duration and exclusivity.
Findings from our review support the practice of rooming-in and family centered care and the positive effect on breastfeeding outcomes, and the opportunity for cue based feedings. Remaining with her infant during hospitalization provided the mother increased opportunities for kangaroo care, and gives health care professionals a convenient platform to educate and support feedings increasing exclusivity and duration of breastfeeding in the late preterm infant. Successful breastfeeding in this population depends in part on parental knowledge of the infant’s feeding readiness cues and developmental needs and limitations (Walker, 2008); this knowledge is likely to be enhanced by prolonged and close proximity to the infant, which is achieved through rooming in and kangaroo care practices.
Our findings support the view that breastfeeding educational interventions improve breastfeeding exclusivity and duration in late preterm infants. Providing education for parents to help them understand the infant’s physical characteristics assists them in establishing feeding success and may increase duration and exclusivity of breastfeeding (Ravn et al., 2012; Wataker et al., 2012).
Although breastfeeding interventions in our review addressed combinations of concepts within the Late Preterm Conceptual Framework (AWHONN, 2013), none assessed interventions in all four concepts as a whole. Incorporating all four concepts of the framework into breastfeeding interventions may better support exclusive long-term breastfeeding and health outcomes in late preterm infants.
Limitations
Although multiple authors reviewed the manuscript, a single reviewer compiled the literature creating the potential to influence the outcome of this integrative review of literature. Establishment of specific inclusion and exclusion criteria and mapping of article selection minimized bias. Search criteria included English language references published between 2005 to 1015 as the period correlating with publication of the Late Preterm Conceptual Framework, a framework that significantly affected care of the late preterm infant. Finally, the definition of late preterm infant varies in published literature from 32 weeks to 37 weeks. Variation in gestational age for the late preterm infant prevents clear comparison of outcomes.
One problematic issue in the literature reviewed is a lack of specificity concerning gestational age. Gestational ages ranging from 32 weeks to 36 6/7 weeks were included in several studies, making it difficult to identify findings pertinent to the late preterm infant exclusively (Flacking et al., 2011; Hake-Brooks & Anderson, 2008; Wataker et al., 2012; Yilmaz et al., 2014). Engle et al. (2007) defined late preterm infants as those with a gestational age of 34 weeks to 36 6/7 weeks. The degree of physical immaturities increases as gestational age decreases; therefore, studies that include infants of age < 34 weeks may not provide accurate accounts of effective interventions for the late pre-term population. Consistency of gestational age parameters with standard late preterm infant definitions can provide accurate evaluations of the effectiveness of breastfeeding interventions.
Implications for Practice and Research
Although there are detailed feeding guidelines for late preterm infants, many recommendations have not been empirically studied in the target population. There is a need for additional research to test these recommendations and additional unexamined post-hospitalization interventions designed to facilitate the transition to direct breastfeeding (e.g., nipple shields, triple feeding). Breastfeeding plans specifically designed to assist the late preterm infant in transitioning to home and ultimately increasing the duration and exclusivity are needed to reduce feeding related morbidities in this vulnerable population. In addition, because breastfeeding readiness occurs along a gestational continuum, with evidence that physiological maturity supporting successful breastfeeding is not complete until 39 weeks, future researchers should include an early term infants group (37–38 6/7 weeks) in studies of breastfeeding interventions.
Conclusion
The increase in the late preterm infant birth rate along with their unique physiological needs demonstrates why it is crucial to support and encourage breastfeeding in the hospital setting and after discharge. The Late Preterm Conceptual Framework provides a model for making a successful transition to home and healthy long-term outcomes. Without effective breastfeeding interventions to address the feeding challenges in this vulnerable population, the late preterm infant will continue to lag in breastfeeding exclusivity and duration when compared to the term population. Closing this gap requires implementation of interventions that address both infant and maternal factors that affect breastfeeding. In our integrative review, we highlighted the positive effects of breastfeeding interventions on breastfeeding exclusivity and duration concluding the need for a focus on interventions after the transition home. The support of breastfeeding success in the late preterm population will enable improved health outcomes from infancy and throughout the life span.
Callouts.
Infants with various gestational ages were included in several studies, which made it difficult to identify findings pertinent to the late preterm infant exclusively.
Findings from this review supported the view that breastfeeding educational interventions improve breastfeeding exclusivity and duration in late preterm infants.
Future studies on breastfeeding interventions should include early term infants (37 to 38 6/7 weeks gestation).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure
The authors report no conflict of interest or relevant financial relationships.
Supplementary Material
Note: To access the supplementary material that accompanies this article, visit the online version of the Journal of Obstetric, Gynecologic, & Neonatal Nursing at http://jognn.org.
Contributor Information
JoAnna Cartwright, Neonatal nurse practitioner, WakeMed Health and Hospitals, Raleigh, NC.
Teresa Atz, Assistant professor in the School of Nursing, Medical University of South Carolina, Charleston, SC.
Susan Newman, Director of the PhD Program and an associate professor in the School of Nursing, Medical University of South Carolina, Charleston, SC.
Martina Mueller, Associate professor in the School of Nursing, Medical University of South Carolina, Charleston, SC.
Jill Radtke Demirci, Postdoctoral fellow, in the Department of Medicine, University of Pittsburgh, Pittsburgh, PA.
References
- Abouelfettoh AM, Dowling DA, Dabash SA, Elguindy SR, Seoud IA. Cup versus bottle feeding for hospitalized late preterm infants in Egypt: a quasi-experimental study. International Breastfeeding Journal. 2008;3:27. doi: 10.1186/1746-4358-3-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Academy of Breastfeeding Medicine. ABM clinical protocol #10: Breastfeeding the late preterm infant (34 0/7 to 36 6/7 weeks gestation) Breastfeeding Medicine. 2011;6(3):151–156. doi: 10.1089/bfm.2011.9990. [DOI] [PubMed] [Google Scholar]
- American Academy of Pediatrics. Breastfeeding and the use of human milk. Pediatrics. 2012;129(3):e827–e841. doi: 10.1542/peds.2011-3552. [DOI] [PubMed] [Google Scholar]
- Association of Women’s Health, Obstetric and Neonatal Nurses. Assessment and care of the late preterm infant: Evidence-based clinical practice guidelines. Washington, DC: Author; 2010. [Google Scholar]
- Association of Women’s Health, Obstetric and Neonatal Nurses. Assessment & care—late preterm infant implementation toolkit. Washington, DC: Author; 2013. [Google Scholar]
- Ayton J, Hansen E, Quinn S, Nelson M. Factors associated with initiation and exclusive breastfeeding at hospital discharge: late preterm compared to 37 week gestation mother and infant cohort. International Breastfeeding Journal. 2012;7(1):16. doi: 10.1186/1746-4358-7-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beattie LM, Weaver LT. Mothers, babies and friendly bacteria. Archives of Disease in Childhood: Fetal and Neonatal Edition. 2011;96(3):F160–F163. doi: 10.1136/adc.2010.189639. [DOI] [PubMed] [Google Scholar]
- Berard A, Le Tiec M, De Vera MA. Study of the costs and morbidities of late-preterm birth. Archives of Disease in Childhood: Fetal and Neonatal Edition. 2012;97(5):F329–F334. doi: 10.1136/fetalneonatal-2011-300969. [DOI] [PubMed] [Google Scholar]
- Boyle EM, Johnson S, Manktelow B, Seaton SE, Draper ES, Smith LK, Field DJ. Neonatal outcomes and delivery of care for infants born late preterm or moderately preterm: a prospective population-based study. Archives of Disease in Childhood: Fetal and Neonatal Edition. 2015;100(6) doi: 10.1136/archdischild-2014-307347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bystrova K, Ivanova V, Edhborg M, Matthiesen AS, Ransjo-Arvidson AB, Mukhamedrakhimov R, Widstrom AM. Early contact versus separation: effects on mother-infant interaction one year later. Birth. 2009;36(2):97–109. doi: 10.1111/j.1523-536X.2009.00307.x. [DOI] [PubMed] [Google Scholar]
- Centre for Evidence-Based Medicine. Explanation of the OCEBM 2011 levels of evidence. 2017 Retrieved from http://www.cebm.net/explanation-2011-ocebm-levels-evidence/
- Dewey K. Maternal and fetal stress are associated with impaired lactogenesis in humans. Journal of Nutrition. 2001;131(11):3012S–3015S. doi: 10.1093/jn/131.11.3012S. [DOI] [PubMed] [Google Scholar]
- Engle W, Tomahsek K, Wallman C, Committee on Fetus and Newborn Late preterm infants: A population at risk. Pediatrics. 2007;120:1390–1401. doi: 10.1542/pes.2007-2952. [DOI] [PubMed] [Google Scholar]
- Flacking R, Ewald U, Wallin L. Positive effect of kangaroo mother care on long-term breastfeeding in very preterm infants. Journal of Obstetric, Gynecologic, & Neonatal Nursing. 2011;40(2):190–197. doi: 10.1111/j.1552-6909.2011.01226.x. [DOI] [PubMed] [Google Scholar]
- Griffin T. Family-centered care in the NICU. Journal of Perinatal and Neonatal Nursing. 2006;20(1):98–102. doi: 10.1097/00005237-200601000-00029. [DOI] [PubMed] [Google Scholar]
- Hake-Brooks SJ, Anderson GC. Kangaroo care and breastfeeding of mother-preterm infant dyads 0–18 months: a randomized, controlled trial. Neonatal Network. 2008;27(3):151–159. doi: 10.1891/0730-0832.27.3.151. [DOI] [PubMed] [Google Scholar]
- Hallowell SG, Spatz DL. The relationship of brain development and breastfeeding in the late-preterm infant. Journal of Pediatric Nursing. 2012;27(2):154–162. doi: 10.1016/j.pedn.2010.12.018. [DOI] [PubMed] [Google Scholar]
- Hamdan A, Tamim H. The relationship between postpartum depression and breastfeeding. International Journal of Psychiatry Medicine. 2012;43(3):243–259. doi: 10.2190/PM.43.3.d. [DOI] [PubMed] [Google Scholar]
- Hamilton B, Martin J, Osterman M. Births: Preliminary data for 2015. National Vital Statistics Reports. 2014;65(3) [PubMed] [Google Scholar]
- Ip S, Chung M, Raman G, Chew P, Magula N, Devine D, Lau J. (Evidence report/technology assessment no. 153).Breastfeeding and maternal and infant health outcomes in developed countries. 2007 Retrieved from https://archive.ahrq.gov/downloads/pub/evidence/pdf/brfout/brfout.pdf. [PMC free article] [PubMed]
- Keemer F. Breastfeeding self-efficacy of women using second-line strategies for healthy term infants in the first week postpartum: an Australian observational study. International Breastfeeding Journal. 2013;8(1):18. doi: 10.1186/1746-4358-8-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kugelman A, Colin A. Late preterm infants: near term but still in a critical developmental time period. Pediatrics. 2013;132(4):741–751. doi: 10.1542/peds.2013-1131. [DOI] [PubMed] [Google Scholar]
- Lawrence RA, Lawrence RM. Breastfeeding: A guide for the medical profession. 7th. Maryland Heights, MO: Mosby/Elsevier; 2011. [Google Scholar]
- Lucas R, Gupton S, Holditch-Davis D, Brandon D. A case study of a late preterm infant’s transition to full at-breast feedings at 4 months of age. Journal of Human Lactation. 2013;30(1):28–30. doi: 10.1177/0890334413495973. [DOI] [PubMed] [Google Scholar]
- Ludington-Hoe S, Johnson M, Morgan K, Lewis R, Gutman J, Wilson D, Scher M. Neurophysiologic assessment of neonatal sleep organization: Preliminary results of a randomized controlled trial of skin contact with preterm infants. Pediatrics. 2006;112:e909–e923. doi: 10.1542/peds.2004-1422. [DOI] [PubMed] [Google Scholar]
- Maastrup R, Hansen BM, Kronborg H, Bojesen SN, Hallum K, Frandsen A, Hallstrom I. Factors associated with exclusive breastfeeding of preterm infants. Results from a prospective national cohort study. PloS One. 2014;9(2):e89077. doi: 10.1371/journal.pone.0089077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mally PV, Bailey S, Hendricks-Munoz KD. Clinical issues in the management of late preterm infants. Current Problems in Pediatric and Adolescent Health Care. 2010;40(9):218–233. doi: 10.1016/j.cppeds.2010.07.005. [DOI] [PubMed] [Google Scholar]
- March of Dimes. U.S. Preterm birth rate drops to 15 year low. 2013 Retrieved from Http://www.marchofdimes.org/news/us-preterm-birth-rate-drops-to-15-year-low.aspx#.
- Marrocchella S, Sestilli V, Indraccolo U, de Rosario F, Castellana L, Mastricci AL, Matteo M. Late preterm births: a retrospective analysis of the morbidity risk stratified for gestational age. Springerplus. 2014;3:114. doi: 10.1186/2193-1801-3-114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattsson E, Funkquist E, Wickstrom M, Nyqvist K, Volgsten H. Healthy late preterm infants and supplementary artifical milk feeds: effects on breastfeeding and associated clinical parameters. Midwifery. 2015;31(4):426–431. doi: 10.1016/j.midw.2014.12.004. [DOI] [PubMed] [Google Scholar]
- McLaurin KK, Hall CB, Jackson EA, Owens OV, Mahadevia PJ. Persistence of morbidity an cost differences between late-preterm and term infants during the first year of life. Pediatrics. 2009;123(2):653–659. doi: 10.1542/peds.2008-1439. [DOI] [PubMed] [Google Scholar]
- McQueen KA, Dennis CL, Stremler R, Norman CD. A pilot randomized controlled trial of a breastfeeding self-efficacy intervention with primiparous mothers. Journal of Obstetric, Gynecologic, and Neonatal Nursing. 2011;40(1):35–46. doi: 10.1111/j.1552-6909.2010.01210.x. [DOI] [PubMed] [Google Scholar]
- Medoff-Cooper B, Bakewell-Sachs S, Buus-Frank M, Santa-Donato A, Near-Term Infant Advisory Panel The AWHONN Near-Term Infant Initiative: A conceptual frameworkd for optimizing health for near-term infants. Journal of Obstetric, Gynecologic, & Neonatal Nurses. 2005;34(6):666–671. doi: 10.1177/0884217505281873. doi:20.1177/0884217505281873. [DOI] [PubMed] [Google Scholar]
- Meier P. Breastfeeding your late preterm infant. McHenry, IL: Medela, Inc.; 2010. [Google Scholar]
- Meier P, Furman L, Degenhardt M. Increased lactation risk for late preterm infants and mothers: evidence and management strategies to protect breastfeeding. Journal of Midwifery & Women ’s Health. 2007;52(6):579–587. doi: 10.1016/j.jmwh.2007.08.003. [DOI] [PubMed] [Google Scholar]
- Meier P, Patel AL, Wright K, Engstrom JL. Management of breastfeeding during and after the maternity hospitalization for late preterm infants. Clinics in Perinatology. 2013;40(4):689–705. doi: 10.1016/j.clp.2013.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morelius E, Ortenstrand A, Theodorsson E, Frostell A. A randomised trial of continuous skin-to-skin contact after preterm birth and the effects on salivary cortisol, parental stress, depression, and breastfeeding. Early Human Development. 2015;91(1):63–70. doi: 10.1016/j.earlhumdev.2014.12.005. [DOI] [PubMed] [Google Scholar]
- Nichols J, Schutte NS, Brown RF, Dennis CL, Price I. The impact of a self-efficacy intervention on short-term breast-feeding outcomes. Health Education and Behavior. 2009;36(2):250–258. doi: 10.1177/1090198107303362. [DOI] [PubMed] [Google Scholar]
- Niela-Vilen H, Axelin A, Salantera S, Lehtonen L, Tammela O, Salmelin R, Latva R. Early physical contact between a mother and her NICU-infant in two university hospitals in Finland. Midwifery. 2013;29(12):1321–1330. doi: 10.1016/j.midw.2012.12.018. [DOI] [PubMed] [Google Scholar]
- Nyqvist KH, Haggkvist AP, Hansen MN, Kylberg E, Frandsen AL, Maastrup R, Baby-Friendly Hospital Initiative Expert, G. Expansion of the baby-friendly hospital initiative ten steps to successful breastfeeding into neonatal intensive care: expert group recommendations. Journal of Human Lactation. 2013;29(3):300–309. doi: 10.1177/0890334413489775. [DOI] [PubMed] [Google Scholar]
- Olson BH, Haider SJ, Vangel L, Bolton TA, Gold JG. A quasi-experimental evaluation of a breastfeeding support program for low income women in Michigan. Maternal Child Health Journal. 2010;14(1):86–93. doi: 10.1007/s10995-008-0430-5. [DOI] [PubMed] [Google Scholar]
- Polin RA, Fox WW. Fetal and Neonatal Physiology. 4th. Philadelphia, PA: Saunders; 2010. [Google Scholar]
- Rao S, Udani R, Nanavati R. Kangaroo mother care for low birth weight infants: A randomized controlled trial. Indian Pediatrics. 2008;45:17–23. [PubMed] [Google Scholar]
- Ravn IH, Smith L, Smeby NA, Kynoe NM, Sandvik L, Bunch EH, Lindemann R. Effects of early mother-infant intervention on outcomes in mothers and moderately and late preterm infants at age 1 year: a randomized controlled trial. Infant Behavior & Development. 2012;35(1):36–47. doi: 10.1016/j.infbeh.2011.09.006. [DOI] [PubMed] [Google Scholar]
- Renfrew M, Craig D, Dyson L, McCormick F, Rice S, King S, Williams A. Breastfeeding promotion for infants in neonatal units: A systematic review and economic analysis. Health Technology Assessment. 2009;13(40):1–146. doi: 10.3310/hta13400. [DOI] [PubMed] [Google Scholar]
- Shapiro-Mendoza C, Tomahsek K, Kotelchuck M, Barfield W, Weiss J, Evans S. Risk factors for neonatal morbidity and mortality among “healthy” late preterm newborns. Seminars in Perinatology. 2006;30(2):54–60. doi: 10.1053/j.semperi.2006.02.002. [DOI] [PubMed] [Google Scholar]
- Spong C, Mercer B, D’alton M, Kilpatrick S, Blackwell S, Saade G. Timing of indicated late-preterm and early-term birth. Obstetrics & Gynecology. 2011;118(2):323–333. doi: 10.1097/AOG.0b013e3182255999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stuebe A. The risks of not breastfeeding for mothers and infants. Review in Obstetrics & Gynecology. 2009;2(4):222–231. [PMC free article] [PubMed] [Google Scholar]
- Tomashek K, Shapiro-Mendoza C, Weiss J, Kotelchuck M, Barfield W, Evans S, Declercq E. Early discharge among late preterm and term newborns and risk of neonatal mobridity. Seminars in Perinatology. 2006;30(2):61–68. doi: 10.1053/j.semperi.2006.02.003. [DOI] [PubMed] [Google Scholar]
- Wataker H, Meberg A, Nestaas E. Neonatal family care for 24 hours per day: effects on maternal confidence and breast-feeding. Journal of Perinatal and Neonatal Nursing. 2012;26(4):336–342. doi: 10.1097/JPN.0b013e31826d928b. [DOI] [PubMed] [Google Scholar]
- Whittemore R, Knafl K. The integrative review: updated methodology. Journal of Advanced Nursing. 2005;52(5):546–553. doi: 10.1111/j.1365-2648.2005.03621.x. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Indicators for assessing infant and young child feeding practices. Geneva, Switzerland: Author; 2008. [Google Scholar]
- Yilmaz G, Caylan N, Karacan CD, Bodur I, Gokcay G. Effect of cup feeding and bottle feeding on breastfeeding in late preterm infants: a randomized controlled study. Journal of Human Lactation. 2014;30(2):174–179. doi: 10.1177/0890334413517940. [DOI] [PubMed] [Google Scholar]
- Young PC, Korgenski K, Buchi KF. Early readmission of newborns in a large health care system. Pediatrics. 2013;131(5):e1538–1544. doi: 10.1542/peds.2012-2634. [DOI] [PubMed] [Google Scholar]
- Zanardo V, Gambina I, Begley C, Litta P, Cosmi E, Giustardi A, Trevisanuto D. Psychological distress and early lactation performance in mothers of late preterm infants. Early Human Development. 2011;87(4):321–323. doi: 10.1016/j.earlhumdev.2011.01.035. [DOI] [PubMed] [Google Scholar]


