Abstract
Trichilemmal carcinomas are rare malignant adnexal tumors which can involve the head and, rarely, the eyelid. Accurate diagnosis and differentiation from basal cell carcinoma or trichoepithelioma are dependent on histopathological and immunohistochemical analysis. We report a case of an eyelid mass, initially diagnosed by incisional biopsy as a trichoepithelioma, later found on excisional biopsy to be a trichilemmal carcinoma and present a review of the literature of the histopathology, differential diagnosis and management. Consideration of these entities will be useful to the histopathologist and clinician to better identify and treat these challenging lesions.
Keywords: Trichilemmal carcinoma, Trichoepithelioma, Basal cell carcinoma, Eyelid
Introduction
Trichilemmal carcinomas are rare malignant adnexal tumors derived from keratinocytes of the outer root sheath of hair follicles. It is usually found in sun-exposed areas of elderly patients. We report a case of an eyelid mass, initially diagnosed by incisional biopsy as a trichoepithelioma, later found on excisional biopsy to be a trichilemmal carcinoma.
Case report
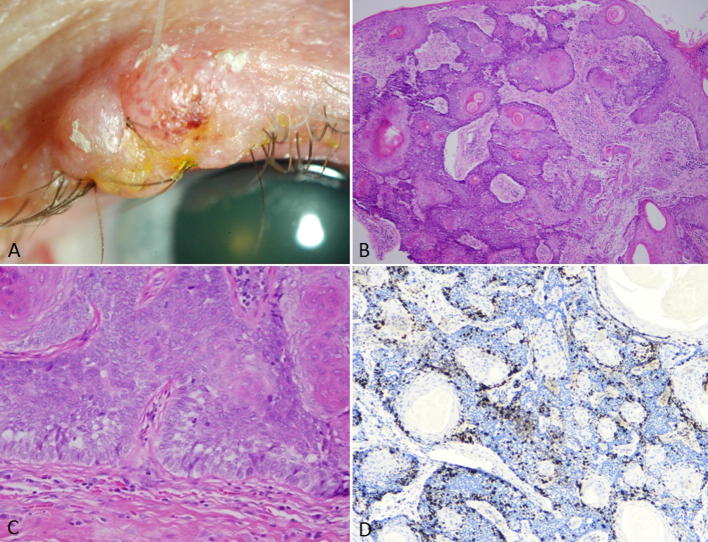
A 71-year-old man presented with a left upper eyelid mass, which he noticed two days prior to visiting our clinic. He denied any bleeding, discharge or pain. On examination, the lesion was a firm, exophytic nodule measuring 7.1 mm in width and 5.2 mm in height located on his medial eyelid, arising anterior to the gray line. The lesion exhibited madarosis. Multiple telangiectatic vessels were seen deep to the surface. No ulceration, discharge or lipid deposits were found within the mass and it was non-tender to palpation (Fig. 1A). His vision and intraocular examination were normal.
Fig. 1.
(A) External photograph: 7.1 mm × 5.2 mm firm, nodular mass of the medial left upper eyelid, arising anterior to the gray line, with madarosis and telangiectasias on the surface. (B) Excisional biopsy revealing blue basaloid cells with multiple pink epithelial islands recapitulating immature hair follicles (few lumens filled with concentric laminated keratin). Malignant cells at the bottom right of the image show invasion into dermis (H&E, 10x). (C) Basaloid cells with clear cytoplasm, nuclear atypia, prominent nucleoli and atypical mitoses. Tumor cells form immature pilosebaceous units with trichilemmal keratinization and exhibit peripheral palisading (H&E, 40x). (D) Intermediate Ki67 positivity (Immunohistochemical stain, 20x).
Patient underwent incisional biopsy. Histopathological examination revealed islands of blue basaloid cells, as well as multiple horn cysts containing concentric laminae of keratin, which represent immature hair follicles. A few areas of peripheral palisading cells around the basaloid islands were noted. No mucinous stroma was seen. Ki67 was mildly positive. Based on these findings, the initial diagnosis was trichoepithelioma versus low grade neoplasm.
One week later, the mass was completely excised via a full-thickness pentagonal wedge of the left upper eyelid. Margins were determined to be tumor-free by frozen section control, and the eyelid was reconstructed by direct closure of the eyelid defect after release of the superior crux of the lateral canthal tendon. Final pathology showed deeply invasive cells with clear cytoplasm, prominent nucleoli, nuclear atypia with multiple mitoses, recapitulating immature hair follicles and peripheral palisading cells (Fig. 1B and C). The cells which invaded the stroma showed surrounding desmoplastic reaction. Immunohistochemical staining showed intermediate Ki67 positivity and Ber-EP4 negativity, consistent with trichilemmal differentiation (Fig. 1D). The final diagnosis was trichilemmal carcinoma.
Discussion
Our case presented a diagnostic challenge. The patient's age and the lesion's appearance suggested malignancy; however, the incisional biopsy revealed predominately benign features, such as the lack of deep invasion by tumors cells, and only a few malignant features, such as intermediate Ki67 staining. We will discuss trichoepitheliomas briefly, with a focus on differentiating between trichoepithelioma, basal cell carcinoma and trichilemmal carcinoma.
Trichoepitheliomas are benign tumors of immature hair follicles.1, 2, 3 These tumors are most commonly found on the face; the eyelid is a rare location. One review by Simpson et al. reported only 18 cases of eyelid trichoepithelioma over a 30 year period. The average age of presentation was 46.8 years old, with a 2:1 male to female ratio. Most cases were located on the upper lid and only 2 of the 18 experienced local recurrence.1
In contrast, trichilemmal carcinomas are locally invasive malignant tumors of the outer sheath of hair follicles. The entity was first described by Headington in 1976.4 Trichilemmal carcinomas are found on sun-exposed areas such as the face and scalp, but rarely appear on the eyelid.5, 6, 7, 8 In a review by Hamman and Jiang, of the 82 cases in the literature that reported demographic information, 42 cases (51%) were found on the face, while only 3 cases (4%) were found on the eyelid. The most common locations were scalp, ears, and neck accounting for 13%, 9%, and 9% of the cases, respectively. Mean age was 70 years (range 9–93) with a 3:2 male to female ratio. Only a total of 4 cases were found in patients younger than 40 years of age. Trichilemmal carcinoma usually presents as a exophytic, nodular or papular mass and can be associated with ulcerations, telangiectasias and conjunctival erosions.6, 7, 8, 9 Thus, the differential also includes basal cell carcinoma, squamous cell carcinoma and keratoacanthoma.8 It is thought that UV radiation may play an important role in the pathogenesis of the disease because most lesions are found on sun-exposed regions of elderly patients.8 Other possible risk factors include ionizing radiation,10 previous trauma or burns,11 and genetic disorders such as xeroderma pigmentosa and Cowden disease.6, 12, 13
Histopathologically, trichoepitheliomas, basal cell carcinomas and trichilemmal carcinomas may be difficult to distinguish from each other. Trichoepitheliomas are composed of multiple horn cysts containing concentrically laminated keratin with basaloid cells arranged in a cord or lacy pattern. The cells are without mitotic figures and are found within a dense fibromyxomatous stroma without much mucin.2, 3 This is in contrast to basal cell carcinoma, which generally shows epidermal ulceration, mucinous stroma and few keratin cysts. Additionally, basal cell carcinoma shows retraction artifact and peripheral palisading cells within the basaloid islands.
In contrast, trichilemmal carcinomas show malignant cells with clear cytoplasm with prominent nucleoli, nuclear atypia and high mitotic rate. The cells form immature pilosebaceous units, with multiple horn cysts containing laminated keratin. Importantly, the cells show trichilemmal keratinization, where is a lack of the granular layer between the spinosum and keratin layer, which is normally seen in epidermal keratinization. Similar to basal cell carcinoma, peripheral palisading cells can be seen within the basaloid islands.4, 10, 14 Cells which invade deeper have a desmoplastic reaction from the surrounding stroma. Cells usually exhibit increased proliferative activity and are Ber-EP4 negative, unlike basal cell carcinoma, which are usually Ber-EP4 positive and lack hair follicle differentiation.
The treatment for trichilemmal carcinoma is local excision with tumor-free margins which is curative in most cases.6, 7, 10, 15 Local recurrence can be aggressive, especially if the initial lesion is incompletely excised, and regular monitoring is prudent. Distant metastasis is extremely rare.
In our case, the provisional diagnosis of trichoepithelioma upon incisional biopsy was changed to the final diagnosis of trichilemmal carcinoma after the full-thickness specimen was examined to review the depth of tumor invasion. This case highlights the overlapping and unique histopathological features of three clinically similar entities: basal cell carcinoma, trichoepithelioma, and trichilemmal carcinoma.
Conflict of interest
The authors declared that there is no conflict of interest.
Footnotes
Peer review under responsibility of Saudi Ophthalmological Society, King Saud University.
Contributor Information
Michael K. Chai, Email: mchai@nyee.edu.
Phillip Tenzel, Email: ptenzel@nyee.edu.
Codrin Iacob, Email: ciacob@nyee.edu.
Adrienne Jordan, Email: ajordan@nyee.edu.
Harsha S. Reddy, Email: hreddy@nyee.edu.
References
- 1.Simpson W., Garner A., Collin J.R.O. Benign hair-follicle tumours in the differential diagnosis of basal-cell carcinoma of the eyelids: a clinicopathological comparison. Br J Ophthalmol. 1989;73:347–353. doi: 10.1136/bjo.73.5.347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gupta A., Ali M.J., Misha D.K., Naik M.N. Solitary trichoepithelioma of the eyelid: a clinico-pathological correlation. Int J Trichol. 2015;7(2):80–81. doi: 10.4103/0974-7753.160119. Apr-Jun. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shields JA, Shields CL. Eyelid, conjunctival, and orbital tumors: an atlas and textbook, Volume 1. LWW; 2008.
- 4.Headington J.T. Tumour of the hair follicle: a review. Am J Pathol. 1976;85:479–514. [PMC free article] [PubMed] [Google Scholar]
- 5.Dailey J.R., Helm K.F., Goldberg S.H. Tricholemmal carcinoma of the eyelid. Am J Ophthalmol. 1993;115:118–119. doi: 10.1016/s0002-9394(14)73540-8. [DOI] [PubMed] [Google Scholar]
- 6.Reis J.P., Tellechea O., Cunha M.F., Baptista A.P. Trichilemmal carcinoma: review of 8 cases. J Cutan Pathol. 1993;20:44–49. doi: 10.1111/j.1600-0560.1993.tb01248.x. [DOI] [PubMed] [Google Scholar]
- 7.Boscaino A., Terracciano L.M., Donofrio V., Ferrara G. Tricholemmal carcinoma: a study of seven cases. J Cutan Pathol. 1992;19:94–99. doi: 10.1111/j.1600-0560.1992.tb01349.x. [DOI] [PubMed] [Google Scholar]
- 8.Hamman M.S., Brian Jiang S.I. Management of trichilemmal carcinoma: An update and comprehensive review of the literature. Dermatol Surg. 2014;40(7):711–717. doi: 10.1111/dsu.0000000000000002. [DOI] [PubMed] [Google Scholar]
- 9.Lee J.H., Shin Y.W., Oh Y.H., Lee Y.J. Trichilemmal carcinoma of the upper eyelid: A case report. Korean J Ophthalmol. 2009;23:301–305. doi: 10.3341/kjo.2009.23.4.301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chan K.O., Lim I.J., Baladas H.G., Tan W.T. Multiple tumour presentation of trichilemmal carcinoma. Br J Plast Surg. 1999;52:665–667. doi: 10.1054/bjps.1999.3180. [DOI] [PubMed] [Google Scholar]
- 11.Ko T., Tada H., Hatoko M., Muramatsu T. Trichilemmal carcinoma developing in a burn scar: a report of two cases. J Dermatol. 1996;23:463–468. [PubMed] [Google Scholar]
- 12.Mane D.R., Kale A.D., Hallikerimath S., Angadi P. Trichilemmal carcinoma associated with xeroderma pigmentosa: report of a rare case. J Oral Sci. 2010;52:505–507. doi: 10.2334/josnusd.52.505. [DOI] [PubMed] [Google Scholar]
- 13.O’Hare A.M., Cooper P.H., Parlette H.L. Trichilemmomal carcinoma in a patient with Cowden’s disease (multiple hamartoma syndrome) J Am Acad Dermatol. 1997;36:1021–1023. doi: 10.1016/s0190-9622(97)80295-2. [DOI] [PubMed] [Google Scholar]
- 14.Swanson P.E., Marrogi A.J., Williams D.J., Cherwitz D.L. Tricholemmal carcinoma: clinicopathologic study of 10 cases. J Cutan Pathol. 1992;19:100–109. doi: 10.1111/j.1600-0560.1992.tb01350.x. [DOI] [PubMed] [Google Scholar]
- 15.Lai T.F., Huilgol S.C., James C.L. Trichilemmal carcinoma of the upper eyelid. Acta Ophthalmol Scand. 2003;81:536–538. doi: 10.1034/j.1600-0420.2003.00132.x. [DOI] [PubMed] [Google Scholar]