Abstract
Lacrimal sac tumors are extremely rare but can be life threatening. Seventy percent of lacrimal sac tumors are of epithelial origin. Inverted transitional cell papilloma of the lacrimal sac is a rare epithelial sinonasal tumor of benign etiology with local invasion and malignant potential. These lesions may remain undiagnosed or may present with signs and symptoms of dacryocystitis or may transform to transitional cell carcinomas. Most lesions are diagnosed intra-operatively while performing a dacryocystorhinostomy. Biopsy and histopathological examination of mass lesions arising from the lacrimal sac helps in timely management of these rare tumors.
Keywords: Lacrimal sac, Papilloma, Transitional cell, Inverted, Tumors, Dacryocystorhinostomy
Introduction
Lacrimal sac tumors can be benign or malignant. These are rare tumors that have the potential to become malignant, and can be life threatening if treatment is delayed. They can be primary, secondary or metastatic. The majority of these tumors are primary and epithelial in origin (73%), and of these, 75% are malignant.1
Papillomas are benign epithelial tumors. They can be exophytic, endophytic or mixed. These can arise from squamous epithelium or transitional epithelium. Carcinomas are malignant epithelial tumors. These include adenocarcinomas, transitional cell carcinomas, squamous cell carcinomas or mixed carcinomas. These arise from papillomas or de novo.2
Patients with lacrimal sac tumors may present with epiphora and signs of nasolacrimal duct (NLD) obstruction. Presenting features of bloody discharge, epistaxis and a palpable mass in the lacrimal sac region are highly suggestive of malignancy. In the absence of these findings the diagnosis is intra-operative during a dacryocystorhinostomy.3
Case report
A 35-year-old lady, presented to us with complaints of right-sided epiphora of one-year duration, not associated with any pain or discharge. There were no prior episodes of swelling along the lacrimal sac area. There was no past history of trauma or spontaneous bleed from the nose. There was no regurgitation on pressure over the right lacrimal sac area. There was no palpable mass in the lacrimal sac area. On saline irrigation there was 100% clear regurgitation from the opposite punctum without lacrimal sac stasis and on probing there was a hard stop. The left lacrimal system was normal. Ocular examination of both the eyes was normal. A clinical impression of right primary acquired nasolacrimal duct obstruction was made and the patient was subjected to right external dacryocystorhinostomy by the standard surgical technique. As the lacrimal sac was incised a firm yellow globular friable mass was seen occupying the lacrimal sac below the common canaliculus. The mass seemed to be arising from the posterior sac flap and measured 5 × 6 × 3 mms. The common canaliculus looked normal with scattered black pigmentation around the inner ostium. There was no abnormal vascularity or bleeding from the lacrimal sac. The entire growth along with the posterior sac flap was excised and sent for histopathological examination. Mitomycin C was applied in a concentration of 0.04% at the ostium. Rest of the DCR surgery was completed as per standard protocol.
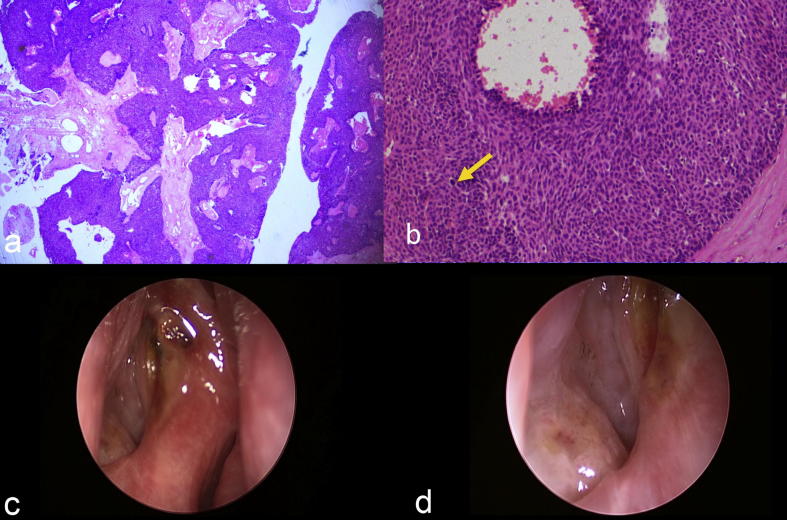
Histopathology (Fig. 1a and b).
Fig. 1.
Photomicrograph shows an exophytic tumor with ramifying fibrovascular core (Hematoxylin and Eosin stain, 4× magnification) (a). Photomicrograph shows hyperplastic epithelium with columnar cells, with patchy nuclear disarray. Occasional mitotic figure is noted (yellow arrow) (Hematoxylin and Eosin stain, 10× magnification) (b). Endoscopic view of the right nasal cavity showing a large and well epithelialized ostium (c). High magnification endoscopic view of the ostium showing a smooth base and without any evidence of intrasac papillomas (d).
On gross examination the tissue measured was 8 × 6 × 2 mm and was firm in consistency. Microscopic examination revealed an exophytic papillary growth with broad fronds and ramifying cores of connective tissue containing dilated capillaries (Fig. 1A). The hyperplastic epithelium displayed columnar cells with mild amount of eosinophilic cytoplasm and hyperchromatic elongated nuclei, although there was patchy nuclear disarray, there was no definite evidence of atypia. Occasional mitotic figure was noted (arrow marked, Fig. 1B). There was no evidence of keratinization, Periodic acid Schiff’s stain demonstrated few cells with mucin; however, there were no discrete goblet cells. These features were compatible with an exophytic transitional papilloma.
Endoscopic examination at one week showed a large, well epithelialized ostium with dynamic internal common opening and without any evidence of residual tumor (Fig. 1c and d). The sinonasal tract also showed no evidence of any growth. In view of the histopathological diagnosis, a close observation was planned for the patient involving quarterly endoscopic examinations for 1 year followed by half-yearly examinations. The patient has been under follow up for 25 months now and is symptom free without any endoscopic evidence of recurrence.
Discussion
Histologically, the canaliculi are lined by non keratinized, non mucin producing stratified squamous epithelium, which changes to stratified columnar epithelium with goblet cells in the lacrimal sac and in the nasolacrimal duct. This heterogeneous epithelial lining of the lacrimal drainage system gives rise to a variety of epithelial neoplasms. Transitional epithelium arises by metaplasia of the respiratory epithelium in response to chronic inflammation.4
The lacrimal excretory system has many similarities to the sinonasal tract where papillomas are more commonly seen.5, 6 Sinonasal papillomas were conventionally classified into three morphological types:
-
1.
Fungiform (exophytic) squamous papilloma
-
2.
Cylindrical cell (oncocytic, Schneiderian) papilloma
-
3.
Inverted (transitional cell) papilloma
Of these, the inverted papilloma is the most common type (70%).6
The exophytic papillomas consist of fingerlike fronds of proliferating epithelium growing in an outward direction. The inverted papillomas grow inward toward the underlying stroma, creating areas of invasive acanthosis.
In a small biopsy it maybe difficult for the pathologist to recognize the growth pattern leading to a misdiagnosis. It is important to correctly recognize transitional papillomas as they have a propensity to recur and have malignant transformation.7, 8
Harry and Ashton provided useful criteria for the diagnosis of benign and malignant transitional cell tumors.9 They divided the tumors into three categories on the basis of morphology and clinical behavior:Type I: Transitional papilloma
-
•
A papillary tumor with a stratified transitional epithelium
-
•
Marked but smooth infolding of epithelium into the stroma
-
•
Uniform cytomorphology
Type II: Intermediate transitional tumor
-
•
A papillary tumor with a stratified epithelium
-
•
More irregular invagination of the epithelium into the stroma
-
•
Mild cellular pleomorphism
-
•
Conspicuous squamous metaplasia
-
•
Readily recognizable mitotic figures
Type III: Transitional cell carcinoma
-
•
A neoplasm with irregular, stratified epithelium
-
•
Invasive growth
-
•
Marked cellular pleomorphism
-
•
Conspicuous squamous metaplasia
-
•
Conspicuous mitotic activity
These diagnostic criteria are of use to the practicing pathologist, particularly since an initial tissue sample may be a small biopsy obtained at dacryocystorhinostomy. Also these diagnostic criteria help in planning the management protocol. While transitional cell papillomas (type 1) warrant careful follow-up of the patient with frequent nasal endoscopic examinations, intermediate transitional tumor (type II) or transitional cell carcinoma (type II) in such a biopsy should prompt consideration of a subsequent dacryocystectomy with margin clearance to exclude a frankly invasive carcinoma. The role of adjuvant radiotherapy in the treatment of transitional cell carcinoma has been controversial. Recurrence of a Type 1 papilloma should be managed with a repeat biopsy under frozen section control for malignant transformation with PCR analysis to look for human papilloma virus DNA.10
Ancillary patient evaluation in cases of suspected lacrimal sac tumors would include peroperative CT scan. Merkonidis et al.11 published a prospective series and a literature review on the role of routine biopsy of the lacrimal sac wall during dacryocystorhinostomy. It was clearly shown that routine biopsy is not warranted and that the incidence of a malignant lesion was very low (0.08% of 1294 specimens).
Choi et al.12 have described the preoperative CT scan findings in cases scheduled to undergo DCR surgery. Their study shows that though in cases of routine DCR, preoperative CT scans adds to the findings, almost all of them are innocuous and do not play a role in changing the management plan. In general we recommend performing preoperative CT scan imaging in cases with a blood-stained discharge, a palpable firm mass in the lacrimal sac area or if examination/history suggest a secondary cause of a nasolacrimal duct obstruction like trauma or a tumor.Our patient had a type I papilloma and has been disease-free on endoscopic examinations for a 25 month follow-up period.
To conclude, transitional papillomas have a propensity to recur as invasive carcinomas. Good prognostic factors include cells with uniform nuclear morphology, rare mitotic figures, and an intact basement membrane. These are usually accidentally diagnosed during a dacryocystorhinostomy and require frequent endonasal endoscopic examinations to rule out recurrences and to look for co-existent sinonasal papillomas. Histopathology plays a pivotal role in the diagnosis and management of these tumors.
Conflict of interest
The authors declared that there is no conflict of interest.
Footnotes
Peer review under responsibility of Saudi Ophthalmological Society, King Saud University.
Contributor Information
Tarjani Vivek Dave, Email: tvdeye@gmail.com.
Dilip Mishra, Email: mishra_dk29@yahoo.co.in.
Ruchi Mittal, Email: drrmittal@gmail.com.
Mohammad Javed Ali, Email: javed007@gmail.com.
References
- 1.Ryan S.J., Font R.L. Primary epithelial neoplasms of the lacrimal sac. Am J Ophthalmol. 1973;76:73–88. doi: 10.1016/0002-9394(73)90014-7. [DOI] [PubMed] [Google Scholar]
- 2.Karcioglu Z.A., Caldwell D.R., Reed H.T. Papillomas of lacrimal drainage system: a clinicopathologic study. Ophthalmic Surg. 1984;15:670–676. [PubMed] [Google Scholar]
- 3.Anderson N.G., Wojno T.H., Grossniklaus H.E. Clinicopathologic findings from lacrimal sac biopsy specimens obtained during dacryocystorhinostomy. Ophthal Plast Reconstr Surg. 2003;19:173–176. doi: 10.1097/01.iop.0000066646.59045.5a. [DOI] [PubMed] [Google Scholar]
- 4.Heathcote G.J. Transitional neoplasms of the nasolacrimal system: A review of the histopathology and histogenesis. Saudi J Ophthalmol. 2012;26:125–131. doi: 10.1016/j.sjopt.2012.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Snyder R.N., Perzin K.H. Papillomatosis of nasal cavity and paranasal sinuses (inverted papilloma, squamous papilloma). A clinicopathologic study. Cancer. 1972;30:668–690. doi: 10.1002/1097-0142(197209)30:3<668::aid-cncr2820300315>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 6.Hyams V.J. Papillomas of the nasal cavity and paranasal sinuses. A clinicopathological study of 315 cases. Ann Otol Rhinol Laryngol. 1971;80:192–206. doi: 10.1177/000348947108000205. [DOI] [PubMed] [Google Scholar]
- 7.Anderson K.K., Lessner A.M., Hood I. Invasive transitional cell carcinoma of the lacrimal sac arising in an inverted papilloma. Arch Ophthalmol. 1994;112:306–307. doi: 10.1001/archopht.1994.01090150036014. [DOI] [PubMed] [Google Scholar]
- 8.Karim R., Ghabrial R., Lin B. Transitional cell carcinoma of the nasolacrimal sac. Clin Ophthalmol. 2009;3:587–591. doi: 10.2147/opth.s7706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Harry J., Ashton N. The pathology of tumours of the lacrimal sac. Trans Ophthalmol Soc UK. 1968;87:19–35. [PubMed] [Google Scholar]
- 10.Orura H., Fukushima K., Watanabe S. A high prevalence of human papilloma virus DNA in recurrent nasal papillomas. J Med Micriobiol. 1996;45:162–166. doi: 10.1099/00222615-45-3-162. [DOI] [PubMed] [Google Scholar]
- 11.Merkonidis C., Brewis C., Yung M., Nussbaumer M. Is routine biopsy of the lacrimal sac wall indicated at dacryocystorhinostomy? A prospective study and literature review. Br J Ophthalmol. 2005;89:1589–1591. doi: 10.1136/bjo.2005.072199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Choi S.C., Lee S., Choi H.S., Jang J.W., Kim S.J., Lee J.H. Kor J Ophthalmol. 2016;30:2430250. [Google Scholar]