Abstract
Background:
Spinal intradural meningiomas that arise purely from a nerve root without dural attachments are extremely rare. Spinal meningiomas arise from arachnoidal cap cells in the spinal canal, and growth of these tumors exerts pressure on the spinal cord and nerve roots.
Case Description:
A patient presented with a lesion at the T3–T4 level that resembled a schwannoma on magnetic resonance imaging. During surgery, the tumor originated from a spinal nerve root. Pathologically, it was an angiomatous meningioma (AM).
Conclusions:
In a review of the literature, we discuss the pathogenesis and surgical strategy for diagnosing and treating these extremely rare AM lesions.
Keywords: Angiomatous meningioma, arachnoidal sheet, intradural meningioma, spinal nerve, spinal tumors
INTRODUCTION
Spinal intradural angiomatous meningiomas (AM) that arise purely from a nerve root, without any dural attachment, are extremely rare. Three intradural meningiomas (two AM) that arise from spinal nerves have been reported.[5,6,7] Here, we describe a fourth meningioma (third AM), which arose from a thoracic nerve root.
CASE REPORT
Over 8 months, a 40-year-old male presented with gait instability, numbness, progressive lower extremity weakness. His neurological examination revealed reduced sensation below the T10 level, and urinary hesitancy. A magnetic resonance image (MRI) of the thoracic spine demonstrated a 3 × 1.4 × 1.5cm lesion compressing the spinal cord at the T3–T4 level [Figure 1a]. It markedly enhanced with contrast, but showed no classical signs of a “dural tail.” It was presumed to be a spinal schwannoma.
Figure 1.
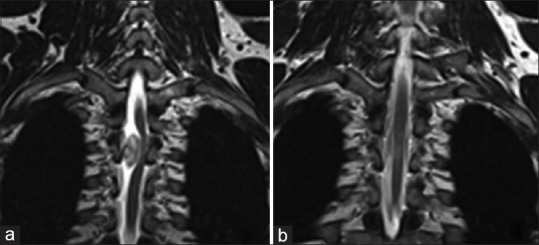
T2 MRIs of spinal tumor. (a) T3-T4 level shows a left-displaced spinal cord, due to an intradural lesion. No dural tail enhancement was observed. (b) Fourteen months after surgery: Normal spinal cord realignment and no enhancement with contrast medium
Surgery
A T3–T4 laminectomy was performed. Upon opening the dura, a reddish encapsulated tumor was observed [Figure 2]. Progressive debulking of the lesion showed no dural attachment, but firm adhesion of the lesion to the lateral aspect of a spinal nerve; the tumor resembled a schwannoma [Figure 3]. To avoid a neural deficit, a marginal resection was performed, leaving the spinal nerve intact. The postoperative course was uneventful, and the patient was discharged home on the 4th postoperative day. Fourteen months postoperatively, the patient remained asymptomatic, without any motor or radicular thoracic sensory impairment. The follow-up contrast enhanced MRI was normal, and there was no residual/recurrent tumor at the T3–T4 level [Figure 1b].
Figure 2.
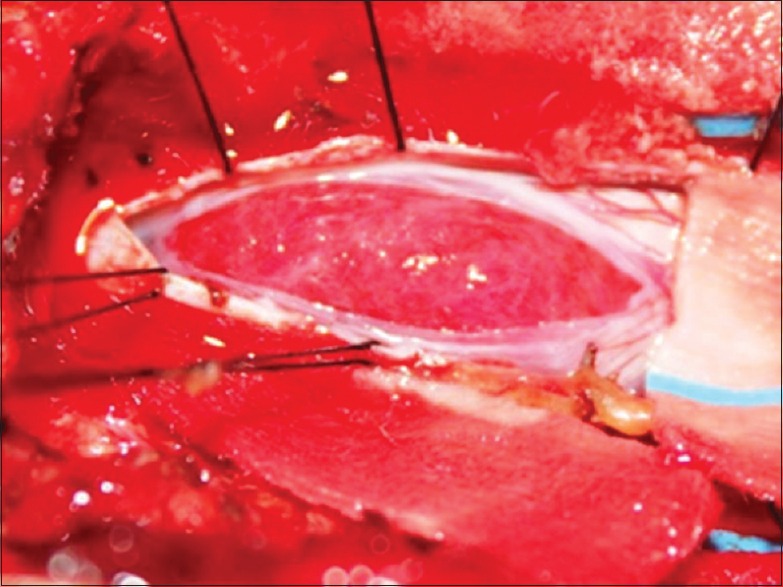
Intraoperative photograph shows the intradural (reddish) tumor, which displaced the spinal cord to the left
Figure 3.
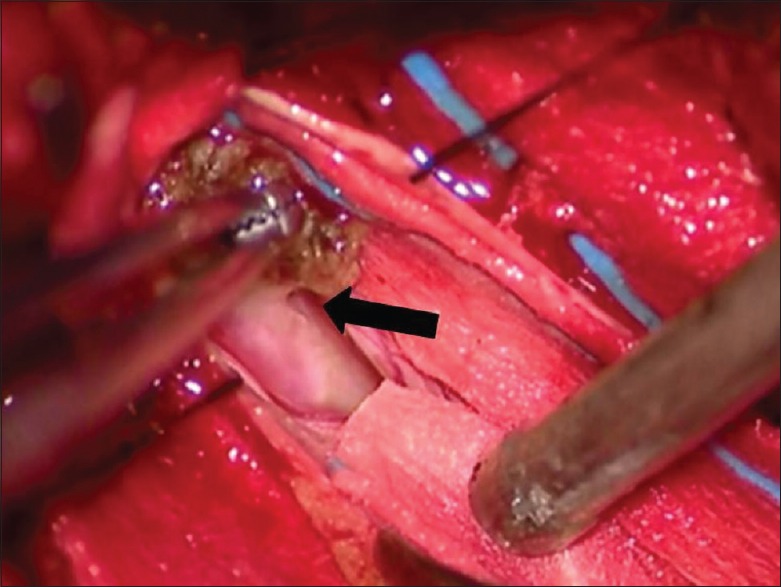
Intraoperative photograph with magnification shows tumor attachment. The forceps tumor lift a residual fragment, which shows firm attachment (black arrow) to the lateral aspect of a spinal nerve, resembling a schwannoma. The adherent fragment was coagulated but not excised
Histopathology
Histopathology of the tumor revealed proliferation of meningothelial cells characterized by round-to-oval nuclei, small nucleoli, occasional pseudoinclusions, and abundant eosinophilic cytoplasm. Cells were arranged in cords and small nests, and they appeared to grow around/intermingled with numerous blood vessels [Figure 4] that were of variable calibre. There was also marked hyalinization. Histologically, the tumor was considered an AM. Meningiomas are defined as “angiomatous” (vascular) when at least 50% of the tumor mass is composed of blood vessels. Mitotic figures were not found, and special studies were not needed to confirm the meningothelial nature of the neoplasia.
Figure 4.
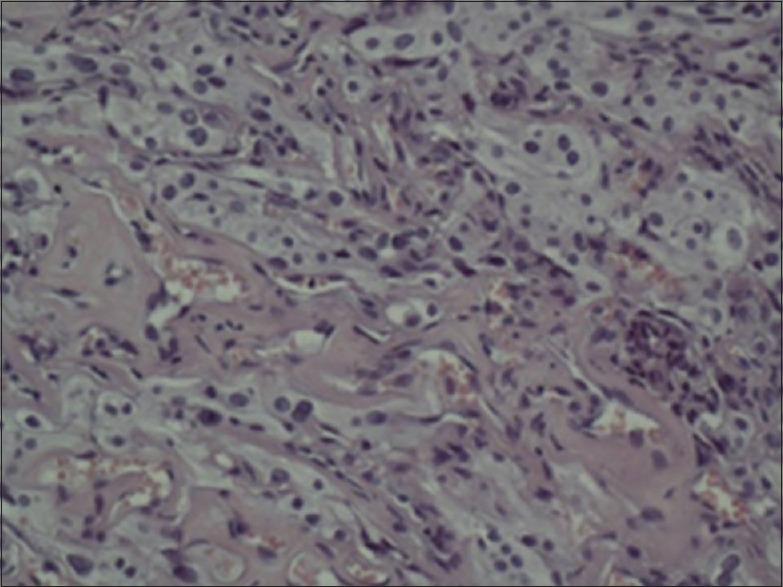
Micrograph of a hematoxylin and eosin-stained tumor specimen (200×) shows moderate cellularity. Meningothelial cells are arranged in small nests and cords. Numerous small blood vessels show marked hyalinization
DISCUSSION
In the vertebral canal, the parietal arachnoid membrane adheres to the dura mater, joins the visceral layer of the dura, and merges toward the spinal nerves near the root exit zones [Figure 5].[1] Spinal meningiomas arise from the arachnoidal cap cells in the spinal canal, and as they grow, they push against the spinal cord and nerve roots. Because the arachnoidal sheet may extend to the extraforaminal nerves, a few extracanalicular meningiomas are reported [Figure 5].[3,4] AMs account for only 1–2.7% of all intraspinal meningiomas.[2,7] In a previous series of 12 spinal AMs, no dural attachment was found in three cases. In one of the patients, the nerve root was connected to the tumor, and was sacrificed.[7] In the second patient, the L-5 sensory root lay within the tumor, and was sacrificed; the two ends were then approximated utilizing standard microsurgical techniques.[6] Here, we described a rare AM that was firmly adherent to a spinal nerve that presumably originated from the perineural visceral arachnoidal sheet.
Figure 5.
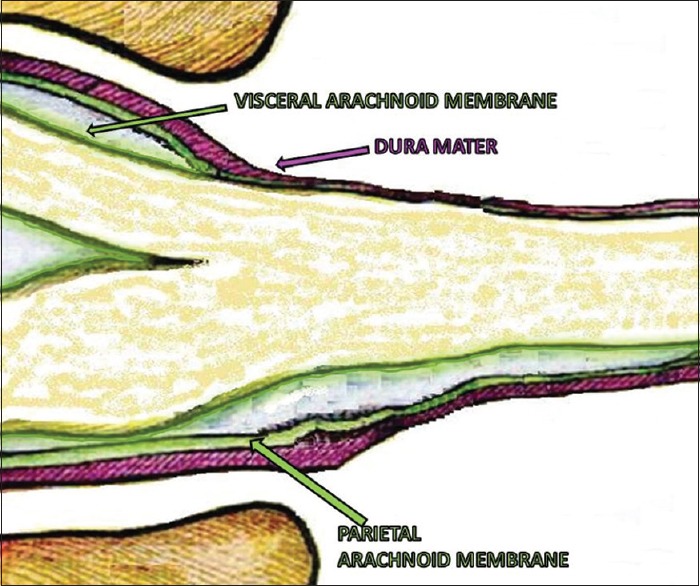
The parietal layer of the arachnoid membrane adheres to the dura mater and the visceral layer of the arachnoid membrane adheres to the pia mater of the spinal cord and nerves. Both join at the intervertebral foramina, but part of the arachnoidal sheet may extend into the extraforaminal space
Surgery
It is not essential to preserve the nerve roots involved in spinal schwannomas, as in most cases, radical resection is possible without causing a neurological deficit. Here, we opted for a marginal resection of the AM tumor from an unidentified thoracic nerve root. The residual small fragment did not show any sign of recurrence on the follow-up MR 14 months later. In conclusion, spinal AMs can resemble schwannomas and may form firm attachments to a specific nerve root. Removal of these lesions can be accomplished without any nerve iatrogenic injury.
Financial support and sponsorship
Nil.
Conflicts of interest
The authors declare that they received no funding, and the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Footnotes
Contributor Information
Paolo Missori, Email: missorp@yahoo.com.
Valeria Palmarini, Email: valeria.palmarini@virgilio.it.
Maria Grazia Elefante, Email: grazia.elefante@gmail.com.
Marco Scapeccia, Email: marcoscapeccia@live.it.
Maurizio Domenicucci, Email: m.domenicucci@gmail.com.
Sergio Paolini, Email: srgpaolini@gmail.com.
REFERENCES
- 1.Benzel EC. Saunders Company WB. Spine Surgery Techniques, Complication Avoidance, and Management. 3rd. Philadelphia: Elsevier/Saunders; 2012. Intradural extramedullary spinal lesions. Meningiomas; pp. 991–98. [Google Scholar]
- 2.Hasselblatt M, Nolte KW, Paulus W. Angiomatous meningioma: A clinicopathologic study of 38 cases. Am J Surg Pathol. 2004;28:390–3. doi: 10.1097/00000478-200403000-00013. [DOI] [PubMed] [Google Scholar]
- 3.Krishnan KL, Narayanan R, Kalyanaraman S, Ramamurthi B. Spinal epidural meningioma. Int Surg. 1978;63:42–3. [PubMed] [Google Scholar]
- 4.Kumar S, Kaza RC, Maitra TK, Chandra M. Extradural spinal meningioma arising from a nerve root. Case report. J Neurosurg. 1980;52:728–9. doi: 10.3171/jns.1980.52.5.0728. [DOI] [PubMed] [Google Scholar]
- 5.Mizutani J, Fukuoka M, Tsubouchi S, Otsuka T, Tono Y, Shimizu S, et al. A rare case of lumbosacral meningioma: Nondural attachment and possible enlargement by orally administered sex steroid. Spine (Phila Pa 1976) 2002;27:E377–81. doi: 10.1097/00007632-200208150-00025. [DOI] [PubMed] [Google Scholar]
- 6.Ng TH, Chan KH, Mann KS, Fung CF. Spinal meningioma arising from a lumbar nerve root. Case report. J Neurosurg. 1989;70:646–8. doi: 10.3171/jns.1989.70.4.0646. [DOI] [PubMed] [Google Scholar]
- 7.Wu L, Yang T, Yang C, Deng X, Fang J, Xu Y. Surgical treatment of intraspinal angiomatous meningiomas from a single center. Neurol Med Chir (Tokyo) 2015;55:328–35. doi: 10.2176/nmc.oa.2014-0274. [DOI] [PMC free article] [PubMed] [Google Scholar]


