Abstract
Background:
Obesity is one of the most prevalent chronic diseases associated with degenerative spinal disease. There is limited evidence regarding the short-term outcome of patients with elevated BMI following spinopelvic fixation surgery.
Methods:
We used the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) database from 2013 to 2014. Inclusion criteria included: adults, aged 18 and older, who underwent all-cause spinopelvic fixation surgery. Primary outcome measures were 30-day readmission, reoperation, and major complication rates. Logistic regression analysis was used to assess the effect of elevated body mass index (BMI) on 30-day outcome.
Results:
A total of 618 patients met inclusion criteria stratified into levels of BMI: 11.2% were Class 2 obese and 10.3% were Class 3 obese. Significant differences were found between the classes for the incidence of revision surgery, reoperations, and deep wound infections. However, there were no significant increases in readmissions and major complications rates, and only Class 3 obese patients had significantly higher odds of reoperation than those who were not obese.
Conclusion:
Significant differences between all classes of obesity regarding revision surgery, reoperation, and deep wound infection rates were found. Class 3 obese patients had significantly higher odds of reoperation, most likely attributed to the greater number/severity of preoperative comorbidities.
Keywords: Body mass index, spinopelvic fixation, NSQIP, complications, outcome
INTRODUCTION
Obesity is one of the most prevalent chronic diseases associated with higher rates of unfavorable outcomes, complications, and comorbidities in patients undergoing spinal surgery for degenerative disease.[3,7] Patients with lumbosacral spondylosis can develop degenerative scoliosis necessitating long segment fusion to the pelvis, which may further increase comorbidity.[1,6]
There are few studies that look at short-term outcomes for spinopelvic fixation in patients with high body mass index (BMI). Here, we analyzed the impact of increasing BMI on the 30-day outcomes of patients with different classes of obesity following spinopelvic fixation surgery.
MATERIALS AND METHODS
The American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) was queried (2013 to 2014) with the following inclusion criteria: all adults (18 and older) undergoing spinopelvic fixations (CPT code 22848). Multiple patient demographics were evaluated including age, sex, smoking status, number of spinal levels fused, type of surgery, BMI, American Society of Anesthesiologists Class (ASA Class), and numbers/types of comorbidities [Table 1]. Patients were then stratified into four classes of obesity (BMI as defined by the World Health Organization): No Obesity (BMI 18.5–29.9), Class 1 obesity (BMI 30–34.9), Class 2 obesity (BMI 35–39.9; note BMI 35 and greater with two major comorbidities is considered morbidly obese), and Class 3 morbid obesity (BMI 40+). The primary outcome measured the 30-day readmission/reoperation rates, intraoperative complications, and major complications. The latter were defined by mortality, coma, prolonged ventilation, reintubation, stroke, pulmonary embolism (PE), cardiac arrest, myocardial infarction (MI), renal failure, sepsis, shock, deep wound infection, and organ space infection.
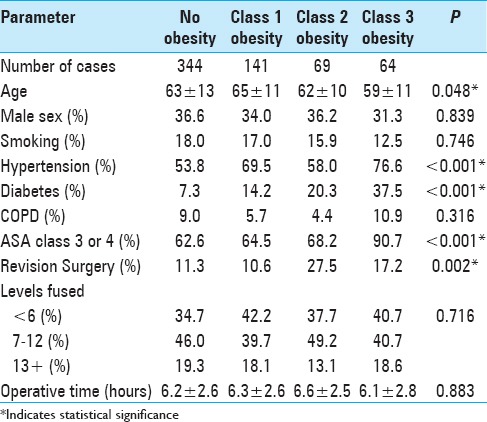
Table 1.
Patient and operative characteristics of 618 patients who underwent spinopelvic fixation
All statistical analyses were performed in Stata SE 12 (StataCorp, College Station, Texas) using student's t-tests and Chi-squared test or Fisher's exact test for frequencies. Multivariate logistic regression analysis was used to assess the independent effect of BMI on 30-day outcomes (complications, readmissions, and reoperations).
RESULTS
Significant differences were found between the obesity classes [Table 1]. Class 3 obese patients had the highest rates of medical comorbidities, ASA class 3 or 4, reoperation, and deep wound infection [Figure 1]. Class 2 obese patients had the highest rates of revision surgery. Class 1 obese patients had the lowest rate of deep wound infection among the different groups and the non-obese group of patients had the lowest rate of reoperation [Table 2 and Figure 2].
Figure 1.
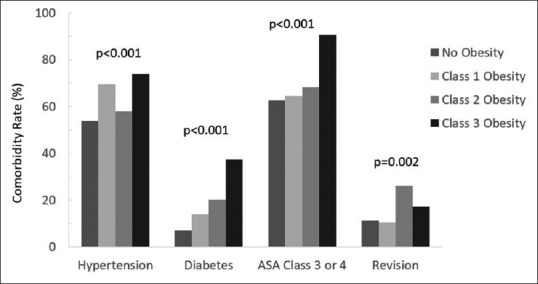
Patient comorbidity rates (left to right: hypertension, diabetes, ASA Class 3 or 4, and Revision) at each class of obesity
Table 2.
The 30-day outcomes of 618 patients who underwent spinopelvic fixation
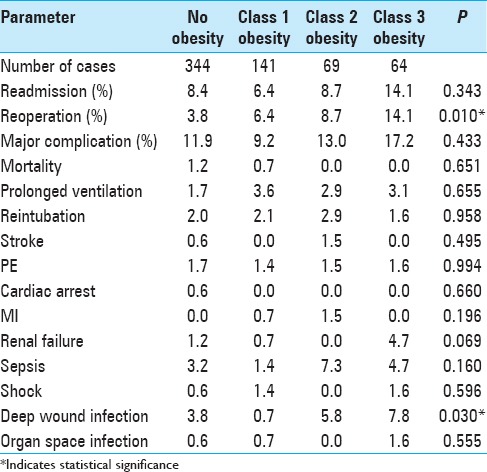
Figure 2.
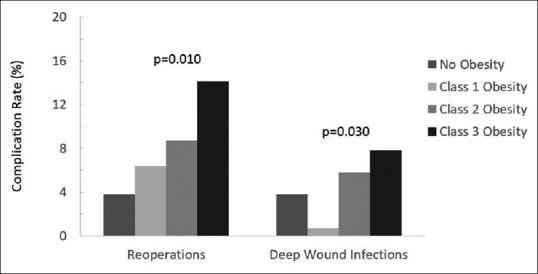
The 30-day reoperations (left) and 30-day deep wound infections (right) at each class of obesity
On multivariate analysis, Class 1, 2, or 3 obesity did not significantly increase the risk of readmission. Class 1 and Class 2 obesity did not increase the odds of reoperation, but Class 3 obese patients did have significantly higher odds of reoperation. Of interest, the severity of obesity did not increase the odds of developing a major complication.
DISCUSSION
Lumbosacral fusion with supplemental spinopelvic fixation has become increasingly common practice in the treatment of long-segment lumbar degenerative disease with deformity.[1,5,6] The increased incidence of such degenerative lumbar disease has been linked to increasing BMI.[3] However, limited data exists on the effect of obesity on 30-day outcomes after spinopelvic fixation surgery.[4] Previous studies have shown that complication development increases with increasing BMI in patients undergoing surgery for degenerative spinal disease. Buerba et al. showed that increased BMI results in increased risk for urinary tract infections (UTI), wound complications, operative time, length of stay, and pulmonary complications after lumbar spine surgery.[3]
We found a significant difference between the different classes of obesity. Class 3 obese patients had the highest rates of medical comorbidities, ASA class 3 or 4, reoperation, and deep wound infection. This fits the hypothesis of a sicker population being at higher risk than the normal control population.[9]
The multivariate analysis attempted to control for these comorbidities. Class 3 obese patients did have significantly higher odds of reoperation. However, the odds of readmission or developing a major complication was not significantly different between the groups. Other unmeasured covariates such as spinal alignment or deformity, degree of spondylosis, presence or absence of ossified ligament, and others may have contributed to this.
Limitations of this study include coding and information bias since data identification and procurement in NSQIP is done through codes, regardless of quality controls maintained by NSQIP. Also, NSQIP is a surgical database not specific to spine surgery patients, thus limiting acquisition of in-depth information about specific patients and procedures being studied. Lastly, this study corresponds to level three evidence. The non-blinded and retrospective nature of this evidence can lead to recall or selection biases, which could skew the gathered data. Nonetheless, NSQIP is a widely used, highly accurate, and reproducible database.[2,8]
CONCLUSION
Lumbosacral fusion with spinopelvic fixation is increasingly being used to treat long-segment lumbosacral degenerative disease. Significant differences between all classes of obesity were seen and a higher incidence of postoperative issues were associated with Class 3 obese patient. Through patient education and preoperative weight reduction and optimization, these risks may be better mitigated.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Footnotes
Contributor Information
Niketh Bhashyam, Email: nbhashya@mail.einstein.yu.edu.
Rafael De la Garza Ramos, Email: rafdelag@gmail.com.
Jonathan Nakhla, Email: jonathan.nakhla@gmail.com.
Jane Jacob, Email: janepjacob@gmail.com.
Murray Echt, Email: murrayecht@gmail.com.
Adam Ammar, Email: adam.e.ammar@gmail.com.
Rani Nasser, Email: rani.nasser@gmail.com.
Reza Yassari, Email: ryassari@montefiore.org.
Merritt D. Kinon, Email: mkinon@montefiore.org.
REFERENCES
- 1.Baek SW, Park YS, Ha KY, Suh SW, Kim C. The analysis of spinopelvic parameters and stability following long fusions with S1, S2 or iliac fixation. Int Orthop. 2013;37:1973–80. doi: 10.1007/s00264-013-2000-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bhashyam N, De la Garza Ramos R, Nakhla J, Nasser R, Jada A, Purvis TE, et al. Thirty-day readmission and reoperation rates after single-level anterior cervical discectomy and fusion versus those after cervical disc replacement. Neurosurg Focus. 2017;42:E6. doi: 10.3171/2016.11.FOCUS16407. [DOI] [PubMed] [Google Scholar]
- 3.Buerba RA, Fu MC, Gruskay JA, Long WD, 3rd, Grauer JN. Obese Class III patients at significantly greater risk of multiple complications after lumbar surgery: An analysis of 10,387 patients in the ACS NSQIP database. Spine J. 2014;14:2008–18. doi: 10.1016/j.spinee.2013.11.047. [DOI] [PubMed] [Google Scholar]
- 4.Hyun SJ, Rhim SC, Kim YJ, Kim YB. A mid-term follow-up result of spinopelvic fixation using iliac screws for lumbosacral fusion. J Korean Neurosurg Soc. 2010;48:347–53. doi: 10.3340/jkns.2010.48.4.347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kelly PD, Sivaganesan A, Chotai S, Parker SL, McGirt MJ, Devin CJ. Matched-pair cohort study of 1-year patient-reported outcomes following pelvic fixation. Spine J. 2016;16:742–7. doi: 10.1016/j.spinee.2016.01.191. [DOI] [PubMed] [Google Scholar]
- 6.Lehman RA, Jr, Kuklo TR, Belmont PJ, Jr, Andersen RC, Polly DW., Jr Advantage of pedicle screw fixation directed into the apex of the sacral promontory over bicortical fixation: A biomechanical analysis. Spine (Phila Pa 1976) 2002;27:806–11. doi: 10.1097/00007632-200204150-00006. [DOI] [PubMed] [Google Scholar]
- 7.Sebastian A, Huddleston P, 3rd, Kakar S, Habermann E, Wagie A, Nassr A. Risk factors for surgical site infection after posterior cervical spine surgery: An analysis of 5,441 patients from the ACS NSQIP 2005-2012. Spine J. 2016;16:504–9. doi: 10.1016/j.spinee.2015.12.009. [DOI] [PubMed] [Google Scholar]
- 8.Sellers MM, Merkow RP, Halverson A, Hinami K, Kelz RR, Bentrem DJ, et al. Validation of new readmission data in the American College of Surgeons National Surgical Quality Improvement Program. J Am Coll Surg. 2013;216:420–7. doi: 10.1016/j.jamcollsurg.2012.11.013. [DOI] [PubMed] [Google Scholar]
- 9.Su AW, Habermann EB, Thomsen KM, Milbrandt TA, Nassr A, Larson AN. Risk Factors for 30-Day Unplanned Readmission and Major Perioperative Complications After Spine Fusion Surgery in Adults: A Review of the National Surgical Quality Improvement Program Database. Spine (Phila Pa 1976) 2016;41:1523–34. doi: 10.1097/BRS.0000000000001558. [DOI] [PMC free article] [PubMed] [Google Scholar]


