Abstract
Background:
Although studies involving intravenous (IV) ibuprofen are still limited, it has been shown to have a potential role in the treatment of postoperative pain. The primary objective of this study was to investigate the effects of preemptive IV ibuprofen on postoperative 24 hour opioid consumption and postoperative pain in patients undergoing laparoscopic cholecystectomy.
Methods:
Following ethical committee approval, 60 patients aged 18 to 65, American Society of Anesthesiology (ASA) I–II, and scheduled for laparoscopic cholecystectomy were included in this prospective, randomized, double-blinded study. Patients were randomly divided into 1 of 2 groups. The control group (n = 30) received 100 mL saline solution 30 minutes before surgery, while the ibuprofen group (n = 30) received 400 mg IV ibuprofen in 100 mL saline. The same general anesthesia protocol was applied in both groups, and all operations were performed by the same surgeon using the same technique. Postoperative analgesia was assessed using a visual analogue pain scale (VAS) with active and passive movements. Twenty-four hour postoperative fentanyl consumption with patient-controlled analgesia and additional analgesia requirements were recorded. Postoperative analgesia was established with 1000 mg paracetamol once every 6 hours and patient-controlled IV fentanyl.
Results:
Compared with the control group, VAS scores in the IV ibuprofen group were statistically lower at postoperative 30 minutes and 1, 2, 4, 8, 12, and 24 hours (P < 0.001). Twenty-four hour opioid consumption was statistically significantly higher in the control group compared to the ibuprofen group (553.00 ± 257.04 and 303.33 ± 132.08 μcq, respectively, P < 0.001). Additional analgesia use was statistically significantly higher in the control group than in the ibuprofen group (14/30 vs 5/30, respectively, P < 0.001). The rates of nausea and vomiting were higher in group control than in group ibuprofen (13/30 vs 5/30, respectively, P = 0.024). Other side-effects were similar between the groups.
Conclusion:
A preemptive single dose of IV ibuprofen in laparoscopic cholecystectomy reduced postoperative opioid consumption in the 1st 24 hours by 45%. It generated lower pain scores in the postoperative period compared with placebo.
Keywords: intravenous ibuprofen, laparoscopic cholecystectomy pain, postoperative analgesia, preemptive analgesia
1. Introduction
Cholecystectomy is the most common abdominal surgical procedure in developed countries, and is generally performed laparoscopically. Laparoscopic cholecystectomy is regarded as the gold standard surgical technique for gallstone diseases.[1] This procedure results in less postoperative pain, a better cosmetic outcome, shorter hospitalization faster healing, and earlier mobilization than open cholecystectomy.[2]
Several factors are involved in pain developing following laparoscopic cholecystectomy. This pain is quite complex and is generally regarded as visceral. Factors involved in the development of this pain include phrenic nerve irritation resulting from the insufflation of CO2 into the peritoneal cavity, abdominal distension, port-site incisions, trauma associated with removal of the gallbladder, sociocultural status, and individual factors.[3]
Postoperative pain is an acute sensation accompanied by an inflammatory process associated with surgical trauma and that decreases with tissue healing. Successful postoperative analgesia is known to prevent the majority of pain-related effects occurring in the patient, such as inability to breathe comfortably, increased workload in the cardiovascular system, thromboembolic events with delayed mobilization, and increased stress response with neuroendocrine and sympathetic nervous system activation.[4,5] Analgesic administration before surgical trauma has been shown in experimental and clinical studies to be capable of reducing posttraumatic sensitivity in the spinal cord and secondary hyperalgesia.[6] If analgesic treatment is started after a painful stimulus then difficulties may be experienced in the treatment of postoperative pain in such cases because peripheral hypersensitivity and central nervous system hyperexcitability may occur.[7]
Ibuprofen is a propionic acid derivative with antiinflammatory, antipyretic, and analgesic effects, like other NSAIDs. The oral form has for long been safely used, and it is one of the most commonly employed NSAIDs. The intravenous (IV) form of ibuprofen has been used in the treatment of mild and moderate pains and to treatment severe pain in combination with opioids since 2009 in the USA. Although there are still insufficient studies concerning IV ibuprofen, it has been shown to be capable of use in the treatment of postoperative pain.[8–10]
The purpose of this study was to investigate the effects of a single preemptive dose of IV ibuprofen on postoperative pain and opioid consumption in patients undergoing laparoscopic cholecystectomy.
2. Materials and methods
Following ethical committee approval, 60 American Society of Anesthesiology (ASA) stage I–II patients aged 18 to 65 and scheduled for laparoscopic cholecystectomy were included in this prospective, randomized, double-blinded study. Written consent was obtained from all patients.
Patients graded ASA 3 or above, with allergies to the agent material, severe hepatic or renal failure, a history of long-term nonsteroid antiinflammatory and opioid analgesic use, a history of gastrointestinal bleeding, peptic ulcer or inflammatory bowel disease, diabetes or other neuropathic diseases, patients weighing less than 40 kg, patients incapable of using a patient-controlled analgesia (PCA) device, and those needing to discontinue the medication required in the study during surgery for any reason were excluded.
Patients were interviewed 1 day before surgery. The study protocol was explained to them, and information was provided about the visual analogue pain scale (VAS) and the PCA device to be used for analgesia after surgery. Written consent was obtained from all patients. Patients were assigned into 2 groups with a random computer program. The control group (n = 30) was administered 100 mL IV saline 30 minutes preoperatively, and the ibuprofen group (n = 30) received 400 mg ibuprofen (İntrafen 400 mg/4 mL, Gen İlaç, Istanbul, Turkey) intravenously in 100 mL saline. No premedication was performed. All patients were taken for surgery after receiving 6 mL/kg crystalloid, and crystalloid infusion (8 mL/kg/hour) was maintained during surgery. Standard ECG, peripheral oxygen saturation (SpO2), and noninvasive blood pressure monitoring were performed in all cases, and all measurements were recorded at 5-minute intervals during surgery.
Anesthesia in both groups was established with IV 2 mg/kg propofol (Propofol, Fresenius Kabi, Germany) and muscle relaxation with IV 0.6 mg/kg rocuronium (Esmeron, Glaxo Smith Kline, England). Following intubation, 0.1 mg/kg rocuronium was administered when necessary for muscle relaxation. Maintenance anesthesia was established with 1.5% sevoflurane (Sevorane, AbbVie, England), 50 μg/hour fentanyl, 50% N2O in oxygen, and 50% O2 in air (tidal volume = 6–8 mL/kg, frequency = 10/minute). Additional analgesia during surgery was provided with 1 μcg/kg fentanyl and 50% increase in sevoflurane concentration if heart rate and mean arterial pressure of the patient was raised above 20% of baseline. Depth of anesthesia was monitored by bispectral index (BIS) and the value of BIS was maintained between 40 and 60.
All operations were performed by the same surgical team using the same technique. At the end of the operation, 1.5 mg neostigmine (Neostigmin Ampoule 0.5 mg/mL, Adeka, Samsun, Turkey) and 0.5 mg atropine (Atropine Sulfate Ampoule 0.5 mg/mL, Galen, Istanbul, Turkey) were applied for the antagonism of the muscle relaxant. Tracheal extubation was performed when extubation criteria were fully met in the operating room, and the patient was then taken to the PACU.
2.1. Postoperative analgesia management
All patients received 1000 mg IV paracetamol (Perfalgan 10 mg/mL, Bristol-Myers Squibb, France) before the end of surgery, and this was repeated every 6 hour postoperatively. Patients were attached to a PCA device after surgery in the recovery room. The PCA device was set to a 10 mcq concentration, a 10-minute lockout and a 25 mcq bolus dose with no basal infusion, maintained for 24 hours.
Postoperative patient evaluation was performed by an anesthetist blinded to the drugs used and groups involved. Postoperative analgesia was assessed using a VAS, at rest and with active movements (VAS 0 = no pain, VAS 10 = the most severe pain possible). Active movement was defined as moving from a lying to a sitting position. Patients with a VAS score of 4 or above received rescue analgesia with 25 mg meperidine. Sedation levels were monitored using a 4-point sedation scale (0 – awake, eyes open; 1 – asleep but responding to verbal commands; 2 – asleep and difficult to arouse; and 3 – sleepy, cannot be aroused by shaking).
Side-effects of the fentanyl and ibuprofen used were monitored and recorded. The presence of sedation, confusion, dizziness, headache, flatulence, nausea, vomiting, itching, dyspepsia, and urinary retention associated with the use of the drugs in the protocol was investigated.
2.2. Sample size
The primary outcome of the study was the total amount of fentanyl consumption in the 24-hour postoperative period. In our preliminary study, we determined standard deviation of 125.97 in the ibuprofen group and 233.13 in the placebo group. We intended to detect a difference in fentanyl consumption between the 2 groups of at least 150 μcg in the 24-hour postoperative period. Accordingly, we determined that the number of patients required in each group was 30, based on power of 85% and alpha error of 0.05 using Russ Lenth Piface Java module.
2.3. Statistical analysis
IBM SPSS 20.0 (SPSS Inc., Chicago, IL) software program was used to perform the statistical analysis. The distribution of the variables was evaluated for normality using the Kolmogorov–Smirnov and histogram tests. Descriptive statistics are expressed as the mean ± standard deviation (SD). Categorical variables were analyzed using the chi-square test. The normally distributed data comprising continuous variables were analyzed using Student t test. Otherwise, the Mann–Whitney U test was used. A value of P < 0.05 was considered statistically significant.
3. Results
Two patients in the ibuprofen group and 3 from the placebo group were excluded from the study due to being transferred to open surgery. Eligible patients for this study were analyzed for the primary outcomes and are presented in a Consolidated Standards of Reporting Trials (CONSORT) flow diagram (Fig. 1).
Figure 1.
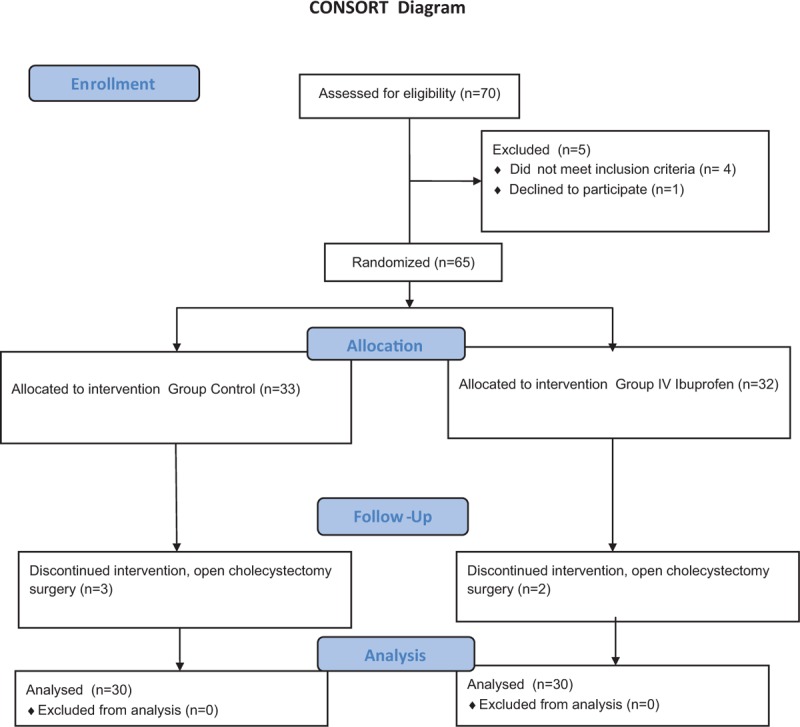
Consolidated Standards of Reporting Trials (CONSORT) flow diagram of study.
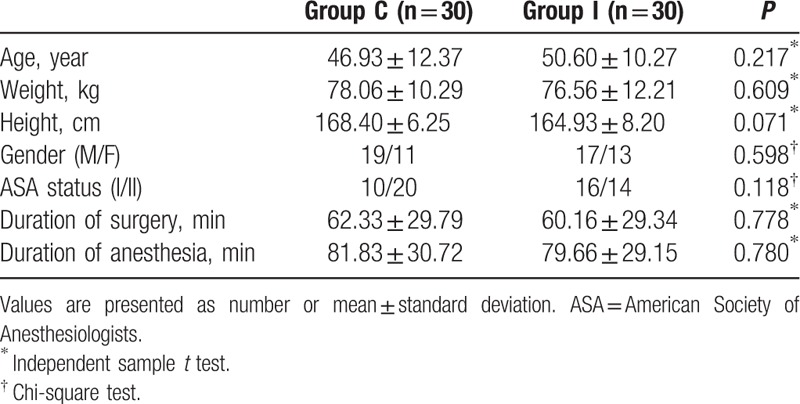
Demographic data for the patients are shown in Table 1. No differences were determined between the 2 groups in terms of age, height, weight, ASA classification, length of surgery, or duration of anesthesia (P > 0.05).
Table 1.
Demographic characteristic of study patients.
Mean blood pressure, heart rate, SPO2, and respiration numbers were similar between the 2 groups at all measurement times (P > 0.05).
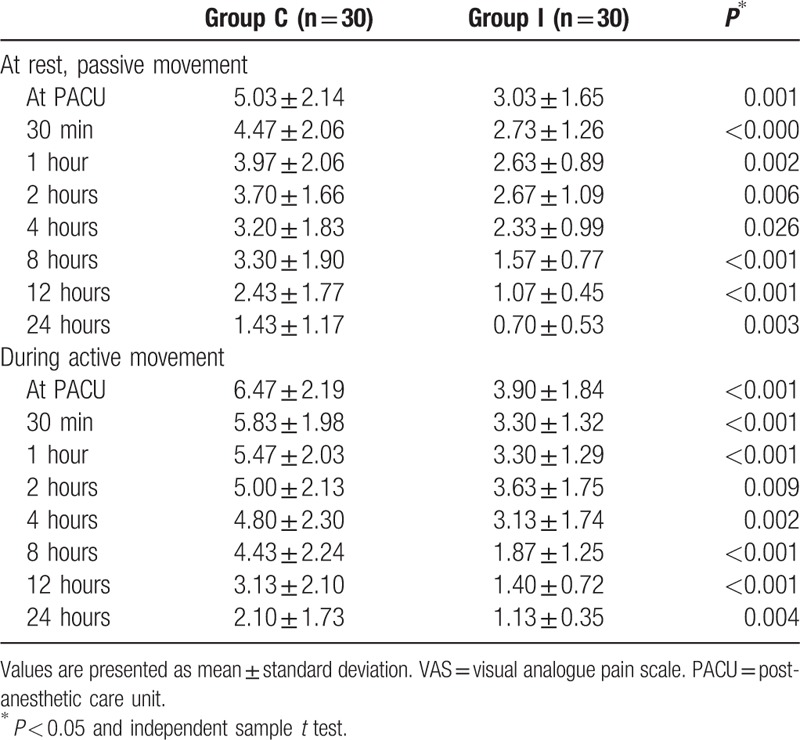
VAS scores were assessed both at rest and with active movements. VAS scores at rest and with active movement at 30 minutes and 1, 2, 4, 8, 12, and 24 hours were lower in the ibuprofen group (P < 0.05) (Table 2).
Table 2.
Comparison of VAS scores at postoperative time points.
Fentanyl consumption was lower in the ibuprofen group compared to the placebo group at all time periods (0–4, 4–8, and 8–24 hours) (P < 0.001). In terms of total fentanyl consumption, 24-hour consumption was lower in the ibuprofen group compared to the placebo group (553.00 ± 257.04 and 303.33 ± 132.08 μcq, respectively) (P < 0.001) (Fig. 2).
Figure 2.
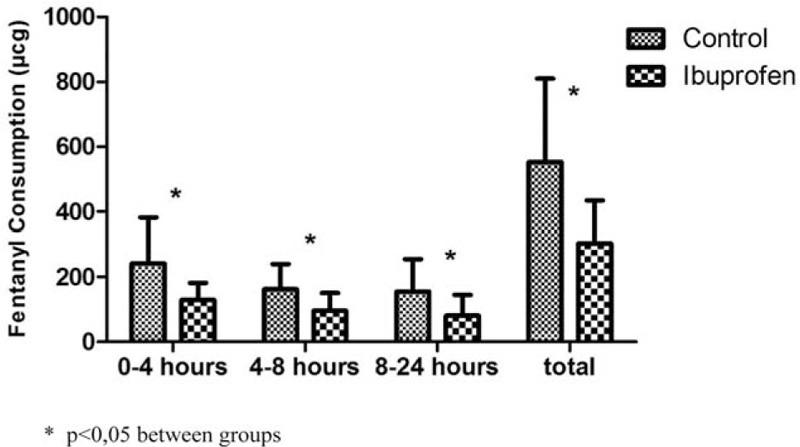
Fentanyl consumption of groups at postoperative time points.
Postoperative rescue analgesic use was statistically significantly higher in the placebo group (n = 14) (350 mg meperidine) compared to the ibuprofen group (n = 5) (125 mg meperidine) (P = 0.012).
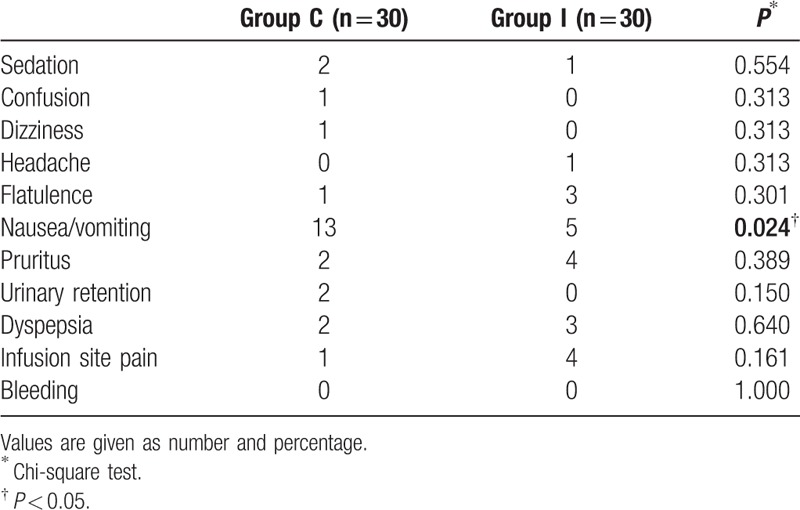
The incidence of nausea/vomiting in the 1st 24 hours was higher in the control group (n = 13) than in the ibuprofen group (n = 5) (P = 0.024). Other side-effects are shown in Table 3. No statistically significant difference was determined between the groups.
Table 3.
Incidence of adverse events.
4. Discussion
This study showed that a single preemptive dose of IV ibuprofen reduced 24-hour opioid consumption and was effective in the emergence of lower pain scores in the postoperative period. In addition, IV ibuprofen significantly reduced rescue analgesic use. In addition IV ibuprofen has played a key role with opioid sparing effect.
Early mobilization, a shortened hospital stay, lower hospital costs, and increased patient satisfaction can be achieved with effective postoperative pain management. One method of postoperative pain management is preemptive analgesia. This represents analgesic application before onset of painful stimuli.[11] Central sensitization, hyperalgesia, and allodynia can thus be reduced. Although various studies have emphasized that the timing of preoperative analgesia is unimportant in terms of postoperative pain and opioid consumption,[12] several other studies have shown the effectiveness of preemptive analgesia. Several systemic and local agents are used for preemptive analgesia. Bupivacaine, lidocaine, clonidine, ketorolac, oral ibuprofen, gabapentin, and pregabalin are drugs used for this purpose.[13–15] The number of studies of IV ibuprofen use is still limited.
Although it is more advantageous than open surgery, acute pain after laparoscopic cholecystectomy is common. In a study by Kandil and El Hefnawy,[16] patients who underwent laparoscopic cholecystectomy reported VAS 5.46 + 2.67 and 3.08 + 1.38 at 12 and 24 hours postoperatively, respectively. In our study in placebo group pain scores are as high as previous study. A VAS score of 3 or more evaluated as moderate pain.[17] Peak of pain intensity is during the early postoperative hours, especially in the 1st 8th hour and usually reduces after 2 or 3 days from laparoscopic cholecystectomy.[18] Patients generally complain of the back, shoulder pain, and port site incisions. Sympathetic pain occurs in approximately 30% to 50% of patients following cholecystectomy, and this pain is difficult to overcome.[19] Since high-level acute postoperative pain that can occur weeks or months after surgery can also trigger chronic pain, the overcoming of acute pain is very important.[19,20]
The multimodal analgesia approach to postoperative pain in recent years is thought to be more effective than the traditional approach. Studies have reported that IV ibuprofen can be used safely as a component of multimodal analgesia.[21] We also administered multimodal analgesia by adding paracetamol and fentanyl as an opioid in the postoperative period to preemptive IV ibuprofen.
Ibuprofen is a well-known analgesic, antiinflammatory, and antipyretic NSAID, the oral form of which has been used for some 40 years. The IV form entered the market in America in 2009. The analgesic efficacy of ibuprofen is associated with cyclooxygenase enzyme inhibition. Ibuprofen administration causes rapid reversible and competitive inhibition of the isoenzymes COX-1 and COX-2. COX-2 inhibition is responsible for the analgesic, antipyretic, and antiinflammatory effects of ibuprofen, while COX-1 causes undesirable side-effects.[22,23]
The only study in the literature in which a single preemptive dose of IV ibuprofen was used by Moss et al[10] and involved pediatric tonsillectomies. In that study, IV ibuprofen reduced postoperative fentanyl use. However, the fact that corticosteroid use exhibited a synergistic effect with ibuprofen may be regarded as a limitation of that study. In contrast to that study, we employed no steroid agent and assessed the postoperative efficacy of IV ibuprofen alone. IV ibuprofen at a dose of 800 mg has been used and its effectiveness discussed in the management of postoperative pain in different operations.[8,9,24] In studies to analyze efficacy of IV ibuprofen for acute postoperative pain who underwent orthopedic and abdominal surgery, IV ibuprofen was administered with wound closure. Compared with placebo 800 mg IV ibuprofen resulted in significant decrease morphine consumption 1st 24 hours. In these studies, 800 mg IV ibuprofen was started perioperatively and was administered once every 6 hours postoperatively. It significantly reduced opioid consumption compared to placebo administration. In contrast to these studies, a single dose of 400 mg was used only preemptively, and postoperative analgesia was maintained with IV paracetamol in our study. This resulted in a 45% decrease in 24-hour opioid requirements compared to the control group. Additional opioid requirement was also lower in the IV ibuprofen group. Another study that used a 400 mg dose, in contrast to our study, reported no statistically significant change, despite a lower morphine requirement and lower pain scores.[25] Studies in the literature have also reported that the combined effect of IV ibuprofen and IV paracetamol reduced opioid consumption and opioid-related side-effects compared to ibuprofen alone. In the study concerned, ibuprofen was administered during induction and maintained postoperatively.[26] In another study, the authors reported that the administration of preoperative IV ibuprofen modulated stress and inflammatory response by reducing catecholamine, cortisol, and cytokine levels following laparoscopic cholecystectomy.[27]
IV ibuprofen is rapidly absorbed (reaching a peak plasma concentration for 400 mg in 0.5 hours). It has an elimination half-life of 60 minutes and bioavailability of approximately 100%. An initial dose of 400 mg is recommended.[22,23] In our study, we used IV ibuprofen in a single dose, 30 minutes before surgery. Our purpose here was for the drug to reach a peak plasma concentration at the start of surgical stimulus and that fewer side-effects would be seen at a dose of 400 mg. Although greater nausea and vomiting were observed in association with opioid use in the control group, no statistical significance was determined in terms of other side-effects between the control and ibuprofen groups. IV ibuprofen also reduced opioid-related side-effects.
There are a number of limitations to this study. First, only a single drug dose of 400 mg dose was used of the drug, which has 2 forms, irrespective of patients’ weights. Different results and a different side-effect profile might have been obtained with a dose of 800 mg. The 2nd limitation is that the 400 mg was used only preoperatively and was not maintained postoperatively. Our purpose was to evaluate the efficacy of a single dose. Third, no local anesthetic injection was applied to the port site incision areas. Pain scores might have been reduced still further with port site injection. Studies might be performed combining local anesthetic infiltration. Fourth, cost-effectiveness of the study and duration of hospital stay was not evaluated. Fifth, on the postoperative period paracetamol was used, this influenced the VAS scores. Finally, the sample size was determined on the basis of opioid requirement, the primary aim. IV ibuprofen-related side-effects may not emerge fully with a small sample size. Further studies with a larger sample size may be needed.
In conclusion, a single preemptive dose of 400 mg resulted in better pain scores by reducing postoperative opioid use in the 1st 24 hours in patients undergoing laparoscopic cholecystectomy by 45%. It also reduced rescue analgesic use in the postoperative period and opioid-related side-effects such as nausea-vomiting.
We recommended preemptive administration of IV ibuprofen 400 mg before 30 minutes in laparoscopic cholecystectomy with advantages of reduces opioid consumption, pain scores, and rescue analgesics usage.
Footnotes
Abbreviations: ASA = American Society of Anesthesiology, IV = intravenous, PCA = patient-controlled analgesia, VAS = visual analogue pain scale.
The authors have no funding and conflicts of interest to disclose.
References
- [1].Soper NJ, Stockmann PT, Dunnegan DL, et al. Laparoscopic cholecystectomy. The new ‘gold standard’? Arch Surg 1992;127:917–21. discussion 921–913. [DOI] [PubMed] [Google Scholar]
- [2].Johansson M, Thune A, Nelvin L, et al. Randomized clinical trial of open versus laparoscopic cholecystectomy in the treatment of acute cholecystitis. Br J Surg 2005;92:44–9. [DOI] [PubMed] [Google Scholar]
- [3].Protic M, Veljkovic R, Bilchik AJ, et al. Prospective randomized controlled trial comparing standard analgesia with combined intra-operative cystic plate and port-site local anesthesia for post-operative pain management in elective laparoscopic cholecystectomy. Surg Endosc 2017;31:704–13. [DOI] [PubMed] [Google Scholar]
- [4].Kehlet H, Holte K. Effect of postoperative analgesia on surgical outcome. Brish J Anaesth 2001;87:62–72. [DOI] [PubMed] [Google Scholar]
- [5].American Society of Anesthesiologists Task Force on Acute Pain Management Practice guidelines for acute pain management in the perioperative setting: an updated report by the American Society of Anesthesiologists Task Force on Acute Pain Management. Anesthesiology 2012;116:248–73. [DOI] [PubMed] [Google Scholar]
- [6].Woolf CJ. Somatic pain – pathogenesis and prevention. Br J Anaesth 1995;75:169–76. [DOI] [PubMed] [Google Scholar]
- [7].Woolf CJ, Chong MS. Preemptive analgesia – treating postoperative pain by preventing the establishment of central sensitization. Anesth Analg 1993;77:362–79. [DOI] [PubMed] [Google Scholar]
- [8].Gago Martinez A, Escontrela Rodriguez B, Planas Roca A, et al. Intravenous ibuprofen for treatment of post-operative pain: a multicenter, double blind, placebo-controlled, randomized clinical trial. PLoS One 2016;11:e0154004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Kroll PB, Meadows L, Rock A, et al. A multicenter, randomized, double-blind, placebo-controlled trial of intravenous ibuprofen (i.v.-ibuprofen) in the management of postoperative pain following abdominal hysterectomy. Pain Pract 2011;11:23–32. [DOI] [PubMed] [Google Scholar]
- [10].Moss JR, Watcha MF, Bendel LP, et al. A multicenter, randomized, double-blind placebo-controlled, single dose trial of the safety and efficacy of intravenous ibuprofen for treatment of pain in pediatric patients undergoing tonsillectomy. Paediatr Anaesth 2014;24:483–9. [DOI] [PubMed] [Google Scholar]
- [11].Kelly DJ, Ahmad M, Brull SJ. Preemptive analgesia I: physiological pathways and pharmacological modalities. Can J Anaesth 2001;48:1000–10. [DOI] [PubMed] [Google Scholar]
- [12].Moiniche S, Kehlet H, Dahl JB. A qualitative and quantitative systematic review of preemptive analgesia for postoperative pain relief: the role of timing of analgesia. Anesthesiology 2002;96:725–41. [DOI] [PubMed] [Google Scholar]
- [13].Mixter CG, 3rd, Meeker LD, Gavin TJ. Preemptive pain control in patients having laparoscopic hernia repair: a comparison of ketorolac and ibuprofen. Arch Surg 1998;133:432–7. [DOI] [PubMed] [Google Scholar]
- [14].Fassoulaki A, Patris K, Sarantopoulos C, et al. The analgesic effect of gabapentin and mexiletine after breast surgery for cancer. Anesth Analg 2002;95:985–91. table of contents. [DOI] [PubMed] [Google Scholar]
- [15].Ahiskalioglu EO, Ahiskalioglu A, Aydin P, et al. Effects of a single-dose preemptive pregabalin on acute and chronic pain after inguinal hernia repair with mesh under spinal anaesthesia: a randomised controlled trial. Eur J Anaesthesiol 2016;33:605–7. [DOI] [PubMed] [Google Scholar]
- [16].Kandil TS, El Hefnawy E. Shoulder pain following laparoscopic cholecystectomy: factors affecting the incidence and severity. J Laparoendosc Adv Surg Tech A 2010;20:677–82. [DOI] [PubMed] [Google Scholar]
- [17].Collins SL, Moore RA, McQuay HJ. The visual analogue pain intensity scale: what is moderate pain in millimetres? Pain 1997;72:95–7. [DOI] [PubMed] [Google Scholar]
- [18].Saadati K, Razavi MR, Nazemi Salman D, et al. Postoperative pain relief after laparoscopic cholecystectomy: intraperitoneal sodium bicarbonate versus normal saline. Gastroenterol Hepatol Bed Bench 2016;9:189–96. [PMC free article] [PubMed] [Google Scholar]
- [19].Blichfeldt-Eckhardt MR, Ording H, Andersen C, et al. Early visceral pain predicts chronic pain after laparoscopic cholecystectomy. Pain 2014;155:2400–7. [DOI] [PubMed] [Google Scholar]
- [20].Kehlet H, Jensen TS, Woolf CJ. Persistent postsurgical pain: risk factors and prevention. Lancet (London, England) 2006;367:1618–25. [DOI] [PubMed] [Google Scholar]
- [21].Southworth SR, Woodward EJ, Peng A, et al. An integrated safety analysis of intravenous ibuprofen (Caldolor®) in adults. J Pain Res 2015;8:753–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Scott LJ. Intravenous ibuprofen: in adults for pain and fever. Drugs 2012;72:1099–109. [DOI] [PubMed] [Google Scholar]
- [23].Smith HS, Voss B. Pharmacokinetics of intravenous ibuprofen: implications of time of infusion in the treatment of pain and fever. Drugs 2012;72:327–37. [DOI] [PubMed] [Google Scholar]
- [24].Singla N, Rock A, Pavliv L. A multi-center, randomized, double-blind placebo-controlled trial of intravenous-ibuprofen (IV-ibuprofen) for treatment of pain in post-operative orthopedic adult patients. Pain Med 2010;11:1284–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Southworth S, Peters J, Rock A, et al. A multicenter, randomized, double-blind, placebo-controlled trial of intravenous ibuprofen 400 and 800 mg every 6 hours in the management of postoperative pain. Clin Ther 2009;31:1922–35. [DOI] [PubMed] [Google Scholar]
- [26].Gupta A, Abubaker H, Demas E, et al. A randomized trial comparing the safety and efficacy of intravenous ibuprofen versus ibuprofen and acetaminophen in knee or hip arthroplasty. Pain Physician 2016;19:349–56. [PubMed] [Google Scholar]
- [27].Le V, Kurnutala L, SchianodiCola J, et al. Premedication with intravenous ibuprofen improves recovery characteristics and stress response in adults undergoing laparoscopic cholecystectomy: a randomized controlled trial. Pain Med 2016;17:1163–73. [DOI] [PubMed] [Google Scholar]


