Abstract
Background:
Infection-associated hemophagocytic syndrome (IAHS) is potentially a fatal disease caused by systemic infection complicated by hemophagocyticlymphohistiocytosis (HLH). Here, we report a case of HLH associated with dengue hemorrhagic fever (DHF) after a trip to Thailand.
Case summary:
A 33-year-old healthy female patient presented with 3 days of fever, myalgia, and skin rash. Serotype 3 dengue virus was isolated. Clinical and laboratory findings fulfilled the criteria of HLH. After the initiation of corticosteroid therapy, the patient recovered and laboratory findings were normalized.
Conclusion:
It would be important to differentially diagnose dengue-associated HLH from severe DHF. Early recognition and initiation of steroid treatment would be crucial for the successful treatment of dengue fever complicated by HLH.
Keywords: corticosteroid, dengue hemorrhagic fever, severe dengue, hemophagocyticlymphohistiocytosis
1. Introduction
Dengue infection is a mosquito-borne, endemic disease caused by dengue virus in tropical regions. After malaria, dengue fever is considered as the most serious public health problem worldwide. Since the first report in 1995, the number of imported cases has also been increasing with about 200 cases per a year in South Korea [1,2]. There are 4 distinct dengue virus serotypes, including DEN-1, DEN-2, DEN-3, and DEN-4. Primary dengue infection is generally mild, inducing life-long immunity to the virus serotype but not to the others. Dengue infection by different serotypes of dengue virus has been accepted as the predisposing factor of severe dengue hemorrhagic fever (DHF) and dengue shock syndrome (DSS). Here, we report a case of severe primary dengue hemorrhagic fever complicated by hemophagocyticlymphohistiocytosis.
2. Case report
A 33-year-old healthy female patient presented with fever, myalgia, and skin rash lasting 3 days before visiting Korea University Guro Hospital (Fig. 1). The patient had a history of trip to Thailand, and she came back to Koreaeight days ago. Except for conjunctiva hemorrhage and mild splenomegaly, the physical findings were unremarkable.
Figure 1.

Itchyerythematous rash on trunk, face, and both arms—white islands in a sea of red.
Initial laboratory tests showed mild neutropenia (1251/μL), thrombocytopenia (75,000/μL), elevated level of lactate dehydrogenase (LDH, 1775 IU/L), and elevated levels of alanine aminotransferase (ALT, 116 IU/L) and aspartate transaminase (AST,74 IU/L). Prothrombin time (PT, 13.1 sec) and activated partial thromboplastin time (aPTT, 33.3 sec) were within the normal range. Despite conservative treatment, sustained high fever was observed.
On hospital day 3, the patient appeared lethargic and fever persisted. With suspicion for secondary HLH after dengue infection, diagnostic tests were performed. Although bone marrow examination did not show typical findings of hemophagocytosis, diagnostic criteria of HLH were met: fever, splenomegaly, cytopenia, hypertriglyceridaemia (fasting TG 308 mg/dL), and hyperferritinaemia (ferritin 25,107 ng/mL) (Table 1). Intravenous dexamethasone (10 mg/m2) was initiated on day 3 (Fig. 2). Dengue virus PCR was positive and reported as a serotype 3 on hospital day 8. The dose of dexamethasone was tapered down after 2 weeks of treatment, and all results of blood tests were normalized (Fig. 2). The patient was discharged from the hospital on hospital day 18 without any sequelae.
Table 1.
Diagnostic criteria for hemophagocyticlymphohistiocytosis (HLH).
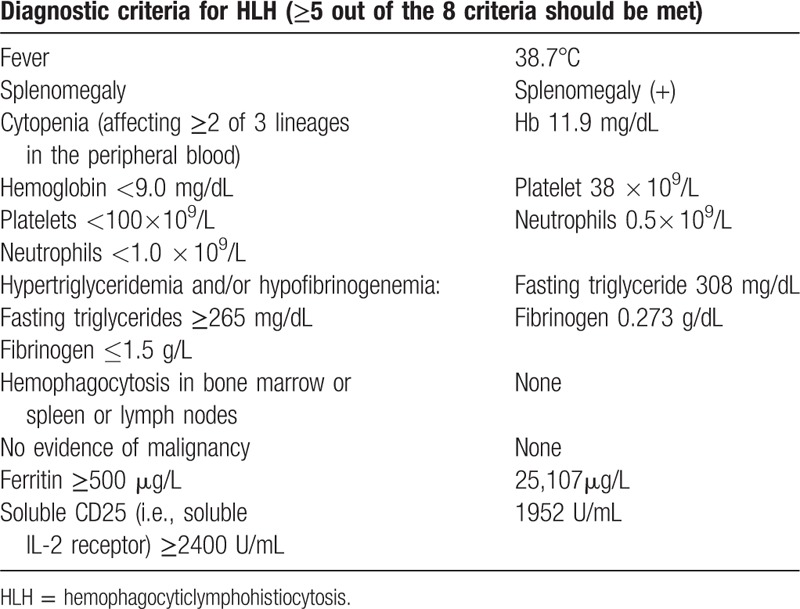
Figure 2.
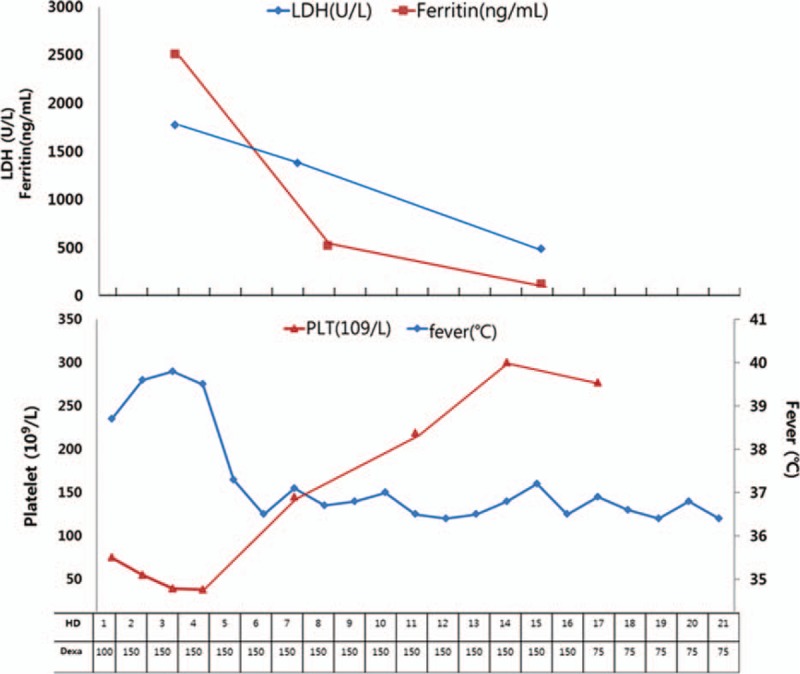
Trend of temperature and laboratory results in relation to dexamethasone treatment.
3. Discussion
Most dengue fever cases reported in South Korea are imported from endemic areas such as Southeast and southern Asia. During 2006–2010, all dengue fever cases reported in South Korea were travel associated. The disease spectrum of dengue infection can range from asymptomatic infection to severe dengue in the form dengue hemorrhagic fever (DHF) and dengue shock syndrome (DSS).[3] Looking at the pathogenesis of dengue infection, even though primary infection confers durable protection against re-infection by a homologous DENV serotype, secondary infection by viruses of a heterologous DENV serotype occurs frequently in endemic areas and is the single most important risk factor for severe disease.[4]
This case was about dengue virus-associated HLH presenting with typical feature such as fever, splenomegaly, cytopenia, coagulopathy, and ferritinemia, meeting 5 of 8 HLH diagnostic criteria. Bone marrow biopsy showed increased number of histiocytes, although typical hemophagocytosis was not observed. It is important to clinically suspect IAHS based on the diagnostic criteria in the HLH-2004 guidelines (Table 1). Early recognition and diagnosis of HLH might enable physicians to start the steroid treatment in optimal time, leading to better clinical outcome.[5] Although the mechanism of HLH remains unclear, current accepted theory suggests that inappropriately proliferating and activated T-cells may induce macrophage activation with inadequate intracellular killing of phagocytes.[6] Many studies suggested the important roles of perforin and natural killer (NK) cells in the HLH subtypes.[7–9] Perforin deficiency may impair defenses against intracellular pathogens as demonstrated in animal models, whereas decreased NK cell activity results in increased T-cell activation and expansion with production of large quantities of cytokines (IFN-γ, TNF–α and GM-CSF), thereby causing sustained macrophage activation. During a virus infection, if the NK cell response cannot control the virus, T cells become more important, and the increased disease load promotes more inflammatory cytokine production by the T cells which activates more macrophages. Although the macrophages phagocytize infected white blood cells, they are inefficient in killing them. Activated T cells and the abundance of activated macrophage produce more inflammatory cytokines to enhance the inflammation causing more tissue damage even in the bone marrow. In the case of dengue infection, the NK cell activity was significantly increased in the early disease stage, but significantly decreased in the febrile shock stages.[10] In addition, invariant natural killer T (iNKT) cells are known to be activated during acute dengue infection.[11] iNKT cells are polyfunctional, as demonstrated by their ability to proliferate and secrete IFN-γ and GM-CSF following stimulation.[12] Further studies are required to better clarify the pathogenesis of HLH-associated with dengue virus infection.
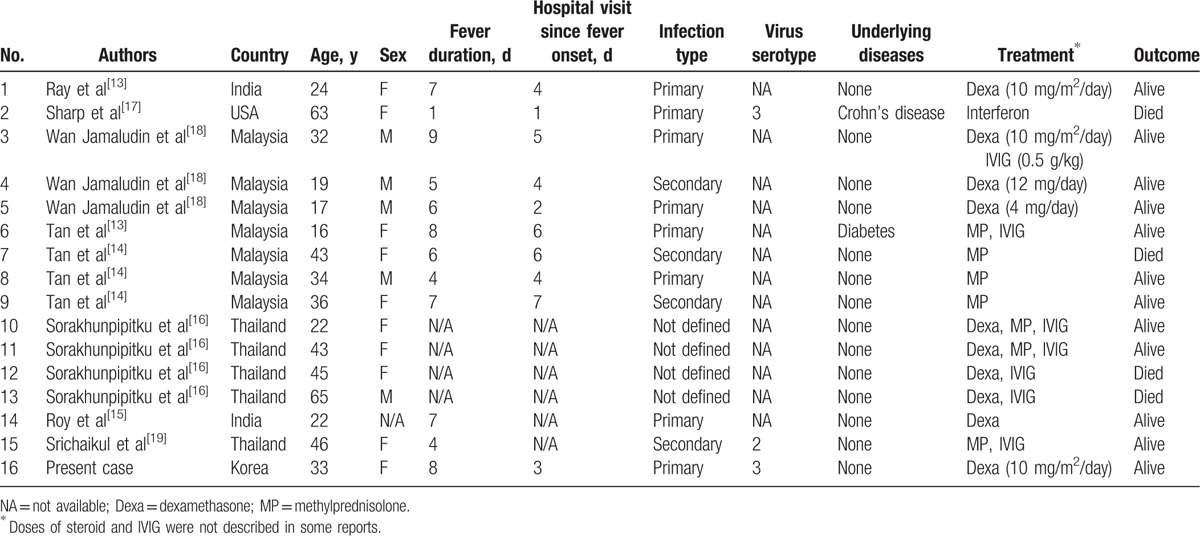
Table 2 shows 16 cases of dengue-associated HLH, including the present case.[13–19] The data was acquired from case reports in PubMed. The average age of the 16 patients was 35.1 years and the survival rate was 75% (12 alive out of 16cases). The youngest patient was 16 years old, and the oldest was 63 years. Eighty-seven percent (14 out of 16 patients) of patients were healthy individuals without underlying disease. The 63-year old female was the only patient who had many underlying diseases including Crohn's disease, hysterectomy state (uterine cancer), and chronic renal failure. The 43-year old female in Tans’ case had diabetes mellitus with HbA1C 7.4%.[14] Among the 16 reported cases, dengue-associated HLH was twice more common in female compared to male. As for the ethnicity, there were 7 Malays, 5 Thai, 2 Indians, 1 American, and 1 Korean. With respect to the infection types (primary or secondary), data were available in limited cases. Except for 4 DHF cases, 8 cases were primary, and 4 cases were secondary infection. Also, not all of the data evaluated the serotype of the dengue virus. Many studies found that primary dengue infections could be associated with severe DHF and dengue-associated hemophagocytic syndrome.[13–15,20,21] In the previous studies, primary dengue infection with serotype 1 or 3 and secondary infection with serotype 2 led to severe DHF.[22] Further studies are required to better clarify the relation between dengue-associated HLH and infection types/viral serotypes. Among the 4 fatal cases, underlying disease, multiple organ dysfunction (MOD), old age, dengue secondary infection, late diagnosis, and delayed treatment were related to poor prognosis. MOD is more common in adult than child DHF which signifies the different pathogenesis of DHF between adults and children.[16]
Table 2.
Cases of dengue-associated hemophagocyticlymphohistiocytosis in adults.
Across the decades, switch in the predominant circulating serotype has been related to several dengue outbreaks in endemic areas.[23] At the beginning of 2013, switch from DENV2 to DENV1 caused outbreak in Singapore.[23] In neighboring Malaysia, DENV2 became dominant other than pre-existing DENV3 and DENV4.[23] Considering frequent re-infections and complicated cases as reported here, vaccine development has been requested. Currently, a licensed dengue vaccine (Dengvaxia, Sanofi-Pasteur) is available in some endemic countries, and several vaccine candidates are in clinical development: TV003/TV005 (United States National Institutes of Health), TDV (Takeda), TDENV-PIV DPIV (GSK/Fiocruz/Walter Reed Army Institute of Research), V180 (Merck), and TVDV (United States Naval Medical Research Center).[24]
In conclusion, it would be important to differentially diagnose dengue-associated HLH from severe dengue hemorrhagic fever. Early recognition and initiation of steroid would be crucial for the successful treatment of dengue fever complicated by HLH. Dengue virus needs to be investigated as an important triggering factor for IAHS.
Footnotes
Abbreviations: ALT = alanine aminotransferase, AST = aspartate transaminase, DHF = dengue hemorrhagic fever, DSS = dengue shock syndrome, HLH = hemophagocyticlymphohistiocytosis, IAHS = infection-associated hemophagocytic syndrome, LDH = lactate dehydrogenase.
The patient provided written permission for publication of this case report.
This work was supported by the National Research Foundation of Korea(NRF) Grant funded by the Korean Government(MSIP)(NRF-2016R1A5A1010148).
The authors have no conflicts of interest to disclose.
References
- [1].Park S. Results of the National Infectious Diseases Surveillance, 2013. Public Health Weekly Rep 2014;7:881–7. [Google Scholar]
- [2].Park JH, Lee DW. Dengue fever in South Korea, 2006–2010. Emerg Infect Dis 2012;18:1525–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Ghosh A, Dar L. Dengue vaccines: challenges, development, current status and prospects. Indian J Med Microbiol 2015;33:3–15. [DOI] [PubMed] [Google Scholar]
- [4].Halstead SB. Dengue. Lancet 2007;370:1644–52. [DOI] [PubMed] [Google Scholar]
- [5].Henter JI, Horne A, Aricó M, et al. HLH-2004: diagnostic and therapeutic guidelines for hemophagocytic lymphohistiocytosis. Pediatr Blood Cancer 2007;48:124–31. [DOI] [PubMed] [Google Scholar]
- [6].Imashuku S, Ueda I, Teramura T, et al. Occurrence of haemophagocytic lymphohistiocytosis at less than 1 year of age: analysis of 96 patients. Eur J Pediatr 2005;164:315–9. [DOI] [PubMed] [Google Scholar]
- [7].Risma KA, Frayer RW, Filipovich AH, et al. Aberrant maturation of mutant perforin underlies the clinical diversity of hemophagocytic lymphohistiocytosis. J Clin Invest 2006;116:182–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Katano H, Cohen JI. Perforin and lymphohistiocytic proliferative disorders. Br J Haematol 2005;128:739–50. [DOI] [PubMed] [Google Scholar]
- [9].Rieux-Laucat F, Le Deist F, De Saint Basile G. Autoimmune lymphoproliferative syndrome and perforin. N Engl J Med 2005;352:306–7. author reply -7. [DOI] [PubMed] [Google Scholar]
- [10].Homchampa P, Sarasombath S, Suvatte V, et al. Natural killer cells in dengue hemorrhagic fever/dengue shock syndrome. Asian Pac J Allergy Immunol 1988;6:95–102. [PubMed] [Google Scholar]
- [11].Matangkasombut P, Chan-In W, Opasawaschai A, et al. Invariant NKT cell response to dengue virus infection in human. PLoS Negl Trop Dis 2014;8:e2955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Sun W, Wang Y, East JE, et al. Invariant natural killer T cells generated from human adult hematopoietic stem-progenitor cells are poly-functional. Cytokine 2015;72:48–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Ray S, Kundu S, Saha M, et al. Hemophagocytic syndrome in classic dengue fever. J Glob Infect Dis 2011;3:399–401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Tan LH, Lum LC, Omar SF, et al. Hemophagocytosis in dengue: comprehensive report of six cases. J Clin Virol 2012;55:79–82. [DOI] [PubMed] [Google Scholar]
- [15].Roy M, Bandyopadhyay D, Saha K, et al. Hemophagocytosis in dengue. Assam J Int Med 2013;3:27–9. [Google Scholar]
- [16].Sorakhunpipitkul L, Punyagupta S, Srichaikul T, et al. Thai adult dengue hemorrhagic fever during 2008–2010: seven cases presented with severe multiorgan failure and successfully treated with high dose of corticosteroids and intravenous immunoglobulin G. J Infect Dis Antimicrob Agents 2011;28:99–103. [Google Scholar]
- [17].Sharp TM, Gaul L, Muehlenbachs A, et al. Fatal hemophagocytic lymphohistiocytosis associated with locally acquired dengue virus infection - New Mexico and Texas, 2012. MMWR Morb Mortal Wkly Rep 2014;63:49–54. [PMC free article] [PubMed] [Google Scholar]
- [18].Wan Jamaludin WF, Periyasamy P, Wan Mat WR, et al. Dengue infection associated hemophagocytic syndrome: Therapeutic interventions and outcome. J Clin Virol 2015;69:91–5. [DOI] [PubMed] [Google Scholar]
- [19].Srichaikul T, Punyagupta S, Kanchanapoom T, et al. Hemophagocytic syndrome in Dengue hemorrhagic fever with severe multiorgan complications. J Med Assoc Thai 2008;91:104–9. [PubMed] [Google Scholar]
- [20].Mitra S, Bhattacharyya R. Hemophagocytic syndrome in severe dengue fever: a rare presentation. Indian J Hematol Blood Transfus 2014;30:97–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Ribeiro E, Kassab S, Pistone T, et al. Primary dengue fever associated with hemophagocytic syndrome: a report of three imported cases, Bordeaux, France. Intern Med 2014;53:899–902. [DOI] [PubMed] [Google Scholar]
- [22].Lei HY. Transient hemophagocytic activity in dengue immunopathogenesis. J Formos Med Assoc 2009;108:595–8. [DOI] [PubMed] [Google Scholar]
- [23].Ng LC, Chem YK, Koo C, et al. 2013 dengue outbreaks in Singapore and Malaysia caused by different viral strains. Am J Trop Med Hyg 2015;92:1150–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Lim SK, Lee YS, Namkung S, et al. Prospects for dengue vaccines for travelers. Clin Exp Vaccine Res 2016;5:89–100. [DOI] [PMC free article] [PubMed] [Google Scholar]


