Abstract
Introduction: Prescription drug overdoses are the leading cause of accidental death in the United States. Alternatives to opioids for the treatment of pain are necessary to address this issue. Cannabis can be an effective treatment for pain, greatly reduces the chance of dependence, and eliminates the risk of fatal overdose compared to opioid-based medications. Medical cannabis patients report that cannabis is just as effective, if not more, than opioid-based medications for pain.
Materials and Methods: The current study examined the use of cannabis as a substitute for opioid-based pain medication by collecting survey data from 2897 medical cannabis patients.
Discussion: Thirty-four percent of the sample reported using opioid-based pain medication in the past 6 months. Respondents overwhelmingly reported that cannabis provided relief on par with their other medications, but without the unwanted side effects. Ninety-seven percent of the sample “strongly agreed/agreed” that they are able to decrease the amount of opiates they consume when they also use cannabis, and 81% “strongly agreed/agreed” that taking cannabis by itself was more effective at treating their condition than taking cannabis with opioids. Results were similar for those using cannabis with nonopioid-based pain medications.
Conclusion: Future research should track clinical outcomes where cannabis is offered as a viable substitute for pain treatment and examine the outcomes of using cannabis as a medication assisted treatment for opioid dependence.
Keywords: : opiates, pain, harm reduction, substitution, opioids, cannabis
Introduction
The Centers for Disease Control (CDC) and Prevention report that “[o]pioids (including prescription opioid pain relievers and heroin) killed more than 28,000 people in 2014, more than any year on record.” Unfortunately, this statistic has done little to curb the prescribing and consumption patterns for prescription opioids. The CDC estimates that, “since 1999, the amount of prescription opioids sold in the United States nearly quadrupled, yet there has not been an overall change in the amount of pain that Americans report. Deaths from prescription opioids—drugs like oxycodone, hydrocodone, and methadone—have also quadrupled since 1999.”1 Interestingly, Bachhuber et al. found that states with medical cannabis laws had significantly lower state-level opioid overdose mortality rates.2 Similarly, Bradford and Bradford evaluated data on all prescriptions filled by Medicare Part D patients from 2010 to 2013 and found that the use of prescription drugs for which cannabis could serve as a clinical alternative fell significantly, once a state medical cannabis law was implemented. They found that implementing an effective medical cannabis law led to a reduction of 1826 daily doses for opioid pain relief filled per physician per year.3
Patients who suffer with pain continue to use opioids for chronic pain conditions despite their limited long-term efficacy. The management of chronic pain impacts 11.2% of adults in the United States with about 3% to 4% of these patients receiving long-term opioid therapy.4 This translates to ∼100 million Americans and incurs costs of up to $635 billion dollars per year.5 Long-term opioid therapy is associated with a number of risks, including opioid use disorder, overdose, and death. In 2012 the National Institute of Drug Abuse estimated that there were ∼2.1 million people in the United States suffering from substance use disorders related to prescription opioid pain relievers and another half million addicted to heroin.6
Used in combination with opioid pain medications, cannabis can lower opioid side effects, cravings, and withdrawal severity, as well as enhance the analgesic effects of opioids, thereby allowing for lower doses and less risk of overdose.7,8 A previous study reported that their subjects' pain “was significantly decreased after the addition of vaporized cannabis” and suggested that cannabis treatment “may allow for opioid treatment at lower doses with fewer [patient] side effects.” The authors concluded that their results “demonstrate that inhaled cannabis safely augments the analgesic effects of opioids.”9 Research published last year found that 80% of medical cannabis users reported substituting cannabis for prescribed medications, particularly among patients with pain-related conditions.8
In an 1889 seminal article published in The Lancet, Dr. Edward A. Birch writes about his tremendous success in using cannabis to help patients who had become addicted to pain medications, including opioids. He wrote, “I prescribed the cannabis simply with a view to utilizing a well-known remedy for insomnia, but it did much more than procure sleep. I think it will be found that there need be no fear of peremptorily withdrawing the deleterious drug, if hemp be employed.” (p. 625).10 Birch's comments from 127 years ago predicted what we know to be true today, despite some controversy that continues to surround the topic of cannabis as medicine. Numerous scholarly studies have demonstrated the efficacy of cannabis for multiple conditions, including the management of pain, while concurrently reducing the reliance on opioid medications and nonopioid medications.5 In a 2010 pain study conducted in Canada, Ware et al. found that “a single inhalation of 25 mg of 9.4% tetrahydrocannabinol herbal cannabis three times daily for five days reduced the intensity of pain, improved sleep, and was well tolerated.”11
While the use of cannabis to treat pain is becoming more accepted in the United States, the Schedule I status of cannabis has made it difficult to conduct large-scale clinical trials on its efficacy. Recent clinical and systematic reviews have acknowledged the promise that cannabis might hold as a standardized pain treatment, while recognizing the limitations that come from small sample sizes and lack on controlled studies. While these reviews show moderate evidence for cannabis as a treatment for pain-related conditions, they also call for additional research in the form of standardized clinical trials.12,13 Meanwhile, in parallel, medical cannabis patients are reporting the use of cannabis to treat their pain in lieu of or in conjunction with opioid-based pain medications.
The act of substituting cannabis for opioids has also been documented in several studies of medical cannabis patients. Consistently, these studies saw substitution rates for prescription drugs over 50%, with less side effects from cannabis being a top reason for substitution across studies.14–16 Given the efficacy data on how cannabis assists patients' management of pain, while also mitigating the risks associated with long-term opioid therapy, the present study uses data gathered directly from the impressions of patients who have used cannabis. Patients were provided an opportunity to comment on how cannabis compared with their use of opioid and nonopioid-based pain medication for the treatment of pain.
Materials and Methods
This study utilized a cross-sectional survey to gather data about the use of cannabis as a substitute for opioid and nonopioid-based pain medication. This study was approved by the IRB at the University of California, Berkeley (Protocol No. 2016-08-9044). Drs. Welty and Reiman did not receive compensation from HelloMD to complete the study.
Instrument
The survey instrument (see Supplementary Appendix SA1 for a copy of the instrument) used for this study was a modified version of the survey used in the Tilray Observational Patient Survey (TOPS). The survey for this study included questions about demographic characteristics, conditions for which cannabis is used, and preferred method of cannabis ingestion. Participants were then asked about their use of cannabis as a substitute for opioid and nonopioid-based pain medication to create subsets of respondents who were engaging in substitution. An affirmative answer led participants to the sections that asked about their experiences using cannabis as a substitute. Questions in this section asked about perceived efficacy of cannabis compared to their other medications, perceived comparability of unwanted side effects, and how the stigma around cannabis impacts their decision to use it as a substitute.
Sampling
The survey was administered through e-mail to a database of 67,422 medical cannabis patients in the state of California using the HelloMD patient database. HelloMD is a digital cannabis health and wellness platform that also provides Telehealth evaluations for medical cannabis recommendations to patients in California. The members of the database received an invitation e-mail describing the study and the survey, along with a link to the survey. After clicking the link, respondents were taken to the Qualtrics survey site where they could complete the survey confidentially. A reminder e-mail with the link to the survey was sent out 2 weeks after the initial invitation was sent. The survey was closed 4 weeks after the reminder e-mail was sent. As an incentive for participating, upon completion of the survey, respondents were asked if they would like to enter a raffle for one of five Firefly vaporizers. If they wished to enter, they clicked on a link that directed them to a form where they could enter their name and e-mail address. At the completion of the sampling, five respondents were selected at random and awarded the vaporizer.
Results
Demographics
Of the 2897 participants, 55% were male. Eleven respondents identified as trans males and one identified as a trans female. Fifty-three percent of the sample was between the ages of 20 and 39, 29% being over the age of 50, and 15% over the age of 60. Sixty-four percent identified as White, 14% Latino(a), and 7% African American. Most patients had some college education or completed college (71%) with 14% having completed postgraduate work. There were some significant differences between the general sample and those reporting past 6 month use of opioid and nonopioid-based pain medications. Whites were significantly more likely to report past 6 month use of both types of pain medication (p<0.001). Age was also significantly related to past 6 month use of these medications (p<0.001). Other significant determinants were being a woman (p<0.001) and having a pain condition (p<0.001) (Table 1).
Table 1.
Sample Demographics
| N (%) | |
|---|---|
| Male | 1593 (55) |
| 20–29 | 898 (31) |
| 30–39 | 666 (23) |
| 40–49 | 406 (14) |
| 50–59 | 406 (14) |
| 60+ | 435 (15) |
| White (not Hispanic) | 1854 (64) |
| Hispanic/Latino(a) | 406 (14) |
| African American | 203 (7) |
| Asian | 145 (5) |
| Pacific Islander | 29 (1) |
| American Indian | 58 (2) |
| Other ethnicity | 203 (7) |
| High school | 435 (15) |
| Some college | 1130 (39) |
| College graduate | 927 (32) |
| Graduate school | 406 (14) |
Condition and cannabis use
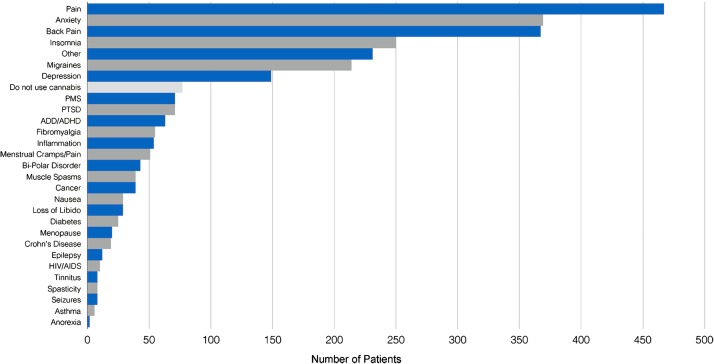
Pain was the most common condition for which respondents reported using cannabis with 16% reporting that as their primary condition. However, when accounting for all pain-related conditions (menstrual cramps, fibromyalgia, back pain and arthritis, etc.) that rises to 63%. Common mental health conditions for which respondents used cannabis included anxiety (13%), insomnia (9%), and depression (5%) (Fig. 1). Smoking was the most common method of ingestion with 50% of the sample reporting using cannabis in that way. Thirty-one percent report vaporizing their cannabis, and 10% use edibles. Three percent reported that they do not currently use medical cannabis.
FIG. 1.
Primary conditions.
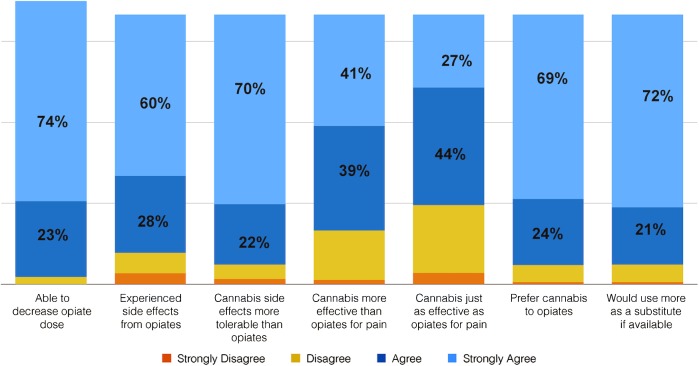
Cannabis and opioids
Thirty percent of the sample (N=841) reported using an opioid-based pain medication currently or in the past 6 months. Of those who have used opioids, 61% reported using them with cannabis. Ninety-seven percent of the sample “strongly agreed/agreed” that they are able to decrease the amount of opioids they consume when they also use cannabis. In addition, 89% “strongly agreed/agreed” that taking opioids produces unwanted side effects such as constipation and nausea. Ninety-two percent of the sample “strongly agreed/agreed” that cannabis has more tolerable side effects than the opioid-based medications they have taken. Eighty-one percent “strongly agreed/agreed” that taking cannabis by itself was more effective at treating their condition than taking cannabis with opioids. When asked if cannabis produces the same amount of pain relief as their opioid-based medications, 71% “strongly agreed/agreed” with that fact. Ninety-two percent of the sample “strongly agreed/agreed” that they prefer cannabis to opioids for the treatment of their condition and 93% “strongly agreed/agreed” that they would be more likely to choose cannabis to treat their condition if it were more readily available (Fig. 2).
FIG. 2.
Use of cannabis as a substitute/in conjunction with opioid-based pain medication (n=828).
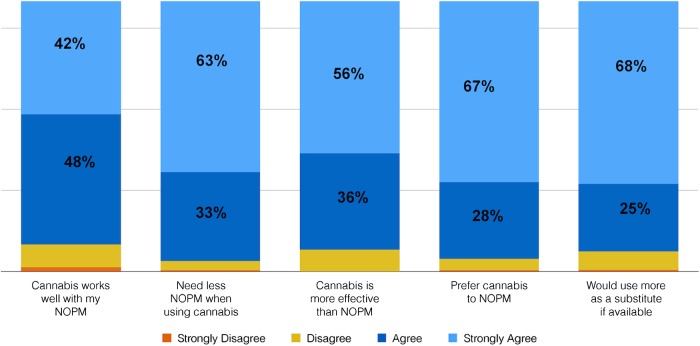
Cannabis and nonopioid-based medications
Sixty-four percent of the sample (N=1751) reported taking a nonopioid-based pain medication (e.g., Tylenol) for their condition currently or in the past 6 months. Seventy-six percent of the sample reported taking a nonopioid-based pain medication along with cannabis currently or in the past 6 months. Ninety-six percent “strongly agreed/agreed” that they do not need to take as much of their nonopioid-based pain medication when they use cannabis and 92% “strongly agreed/agreed” that cannabis works better for their condition than a nonopioid-based pain medication.
As for preferring cannabis over nonopioid pain medication, 95% “strongly agreed/agreed” with this statement.
Similarly to the opioid pain medication group, 93% reported that they would be more likely to use cannabis as a substitute if it were more readily available and easier to access (Fig. 3).
FIG. 3.
Use of cannabis as a substitute/in conjunction with nonopioid based medication (n=1684).
Discussion
Supporting the results of previous research, this study can conclude that medical cannabis patients report successfully using cannabis along with or as a substitute for opioid-based pain medication. Echoing the results of Ware et al. and Abrams et al., patients in this study who are using cannabis and opioids report that they are able to use less opioids and that cannabis presents less unwanted side effects than their opioid-based medication.9,11 In addition, 80% of patients reported that cannabis by itself was more effective than their opioids. It is possible that the variability of individual endocannabinoid and endo-opioid systems results in varying levels of efficacy between the two treatments. For example, a recent review released by the National Academy of Sciences reports conclusive evidence cannabis' efficacy in treating chronic pain, but localized versus neuropathic pain might demand different approaches.17 Cannabis has been found to be very useful in treating neuropathic pain specifically.11
This study found a similar pattern of results when looking at substituting cannabis for nonopioid-based pain medication like Tylenol and Advil. Research suggests that long-term use of these remedies might lead to organ damage.18 With cannabis not only becoming more accepted in the mainstream but also coming in a variety of preparations, some of which are nonintoxicating, more people are looking at cannabis as a viable treatment for everyday ailments such as muscle soreness and inflammation. The results of this study support that not only is this practice common but also medical cannabis patients who choose to use cannabis as a substitute for these medicines report better outcomes with fewer unwanted side effects with cannabis compared to their other medications.
Participants in this study overwhelmingly supported the notion that they would be more likely to use cannabis as a substitute for pain medication if it were less stigmatized and more available, suggesting that there are populations of people who could benefit from this practice but are shying away due to the stigma and legal restrictions related to cannabis use. If cannabis laws continue to change across the country, it will be important to assess how changes in these laws might impact other public health behaviors and outcomes, such as opioid overdose, dependence, risky behaviors, and spending on prescription medications.
Limitations
This is a study of patient self-report through online survey. The data for analyses are based on patient perception and not on objective measure of cannabis and opioid use. Furthermore, there is no comparison group of pain patients who only have access to opioid-based medications or individuals solely using over-the-counter medications for pain. Finally, the solicitation e-mail sent to potential participants included the title of the study which relates to cannabis use for pain. This may have biased the respondents toward those using for pain versus other conditions.
Response rate
The survey yielded responses from 2897 participants, which is a response rate of 4.3%. Since the survey was sent to the HelloMD total patient database, including those not using cannabis for pain, this could reflect in the response rate. Other reasons for nonresponse, besides lack of interest, include people who are no longer patients and those who chose not to participate for other reasons such as privacy concerns.
Amount of cannabis consumed
One of the major limitations of cannabis research is the difficulty in determining how much cannabis participants are using. Variations in strength of product, size of vessel, and social use patterns all impact the reliability and validity of consumption measures. This survey did not ask participants to estimate their amount of consumption and therefore cannot comment on reported effective doses.
Prescription status of opioids
This study did not ask participants if the opioids they consumed were from a prescription or by self-medication. The study also did not inquire as to the specific types of opioids being consumed.
Conclusions
The results of this study provide implications from both a micro and macro level. First, from the macro level, there have been three previously published indicators of public health changes in states that permit medical cannabis: decreases in opioid related mortality, decreases in spending on opioids, and a decrease in traffic fatalities.2,3,19 While none of these studies shows a cause and effect relationship, they do suggest public health related population based changes in localities where cannabis can be accessed to treat pain. Given that the participants in this study reported a greater likelihood of using cannabis as a substitute in a less stigmatized and easily accessible environment, it makes sense why we would see these changes in locations where medical cannabis is sanctioned versus places where it is illegal.
At the micro level, there is a great deal of individual risk associated with prolonged use of opioids and perhaps even nonopioid-based pain medications. The prescribing of opioids has not been curbed in the United States, despite the growing number of fatal overdoses and reported dependence. Providing the patient with the option of cannabis as a method of pain treatment alongside the option of opioids might assist with pain relief in a safer environment with less risk. A society with less opioid dependent people will result in fewer public health harms.
Supplementary Material
Abbreviations Used
- CDC
Centers for Disease Control
- TOPS
Tilray Observational Patient Survey
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Centers for Disease Control. Injury prevention and control: opioid overdose. www.cdc.gov/drugoverdose/epidemic (Accessed February1, 2017)
- 2.Bachhuber MA, Saloner B, Cunningham CO, et al. Medical cannabis laws and opioid analgesic overdose mortality in the United States, 1999–2010. JAMA. 2014;174:1668–1673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bradford AC, Bradford WD. Medical cannabis laws reduce prescription medication use in Medicare Part D. Health Aff. 2016;35:1230–1236 [DOI] [PubMed] [Google Scholar]
- 4.Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain—United States, 2016. JAMA. 2016;315:1624–1645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Boehnke KF, Litinas E, Clauw DJ. Medical cannabis associated with decreased opiate medication use in retrospective cross-sectional survey of chronic pain patients. J Pain. 2016; DOI: 10.1016/j.jpain.2016.03.002 [DOI] [PubMed] [Google Scholar]
- 6.Volkow ND. America's addiction to opioids: heroin and prescription drug abuse. 2014. www.drugabuse.gov/about-nida/legislative-activities/testimony-to-congress/2016/americas-addiction-to-opioids-heroin-prescription-drug-abuse (last accessed March27, 2017)
- 7.Degenhardt L, Lintzeris N, Campbell G, et al. Experience of adjunctive marijuana use for chronic non-cancer pain: findings from the Pain and Opioids IN Treatment (POINT) study. Drug Alcohol Depend. 2015;147:44–150 [DOI] [PubMed] [Google Scholar]
- 8.Haroutounian S, Ratz Y, Ginosar Y, et al. The effect of medicinal marijuana on pain and quality of life outcomes in chronic pain: a prospective open-label study. Clin J Pain. 2016;32:1036–1043 [DOI] [PubMed] [Google Scholar]
- 9.Abrams D, et al. Cannabinoid-opioid interaction in chronic pain. Clin Pharmacol Ther. 2011;90:844–851 [DOI] [PubMed] [Google Scholar]
- 10.Birch EA. The use of Indian hemp in the treatment of chronic chloral and chronic opium poisoning. Lancet. 1889;625 [Google Scholar]
- 11.Ware MA, Wang T, Shapiro S, et al. Smoked cannabis for chronic neuropathic pain: a randomized controlled trial. CMAJ. 2010;182:E694–E701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hill K. Medical marijuana for the treatment of chronic pain and other medical and psychiatric problems: a clinical review. JAMA. 2015;313:2474–2483 [DOI] [PubMed] [Google Scholar]
- 13.Whiting P, Wolff R, Deshpande S, et al. Cannabinoids for medical use: a systematic review and meta-analysis. JAMA. 2015;313:2456–2473 [DOI] [PubMed] [Google Scholar]
- 14.Reiman A. Cannabis as a substitute for alcohol and other drugs. Harm Reduct J. 2009;6:3–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lucas P. Cannabis as an adjunct to or substitute for opioids in the treatment of chronic pain. J Psychoactive Drugs. 2012;44:125–133 [DOI] [PubMed] [Google Scholar]
- 16.Lucas P, Reiman A, Earleywine M. Cannabis as a substitute for alcohol and other drugs: a dispensary-based survey of substitution effect in Canadian medical cannabis patients. Addict Res Theory. 2013; DOI: 10.3109/16066359.2012.7334 [DOI] [Google Scholar]
- 17.Institute of Medicine. The health effects of cannabis and cannabinoids: the current state of evidence and recommendations for research. National Academies Press, 2017. www.nap.edu/24625 (last accessed March27, 2017) [PubMed] [Google Scholar]
- 18.Food and Drug Administration. Acetaminophen and liver damage: Q and A for consumers. 2017. www.fda.gov/ForConsumers/ConsumerUpdates/ucm168830.htm (last accessed March27, 2017)
- 19.Santaella Tenorio J, Mauro C, Wall M, et al. US traffic fatalities, 1985–2014, and their relationship to medical marijuana laws. Am J Public Health. 2016;107:336–342 [DOI] [PMC free article] [PubMed] [Google Scholar]
References
Cite this article as: Reiman A, Welty M, Solomon P (2017) Cannabis as a substitute for opioid-based pain medication: patient self-report, Cannabis and Cannabinoid Research 2:1, 160–166, DOI: 10.1089/can.2017.0012.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.