In 2016 an outbreak of Cryptosporidium potentially linked to swimming pools occurred in the West Midlands region in England. This highlighted the importance of prompt identification of Cryptosporidium by primary care and notification to Public Health England (PHE) to assist with patient management and outbreak control. This article outlines the epidemiology and processes to be followed should suspected Cryptosporidium cases present to primary care.
EPIDEMIOLOGY
Infection with the protozoan parasite Cryptosporidium results from ingestion of oocysts from faecally-contaminated water or food, direct person-to-person contact, or zoonotic spread. The incubation period (the time between exposure to Cryptosporidium and development of symptoms) varies but is on average between 5–7 days.1,2 Infection usually results in an acute illness lasting up to 3 weeks in otherwise healthy people, although asymptomatic infections are common and can be a source of infection for others.2 The symptoms are characterised by an abrupt onset of profuse watery diarrhoea with mucus (rarely blood) and abdominal cramping that may be associated with nausea, anorexia, and possibly fever. Although the infection is self-limiting in most patients, in the very young, older people, and in immunosuppressed individuals it can be a debilitating illness.
Cryptosporidium occurs worldwide and is the fourth most common cause of gastrointestinal infection in the UK.2 As gastrointestinal symptoms can result from a range of conditions, only some of which will be infectious, microbiological confirmation is required to confirm the diagnosis. Data available from PHE for 2000 to 2012 show that nationally the number of confirmed cases from samples ranges from 3000–6000 per year, with peaks in the spring and autumn.3
RISK OF OUTBREAKS
Ingestion of contaminated water has been responsible for large outbreaks of Cryptosporidium. The largest worldwide outbreak reported in Milwaukee in the US in 1993 resulted in an estimate of >400 000 people affected.4 In England, outbreaks have mainly been reported associated with public and private water supplies and swimming pools,5 with the Bouchier report providing recommendations on reducing such risks.6 Control of these outbreaks is challenging due to a) multiple transmission routes, b) the highly infectious nature of the parasite, and c) resistance of the oocysts to chlorine-based disinfectants at levels typically used in most swimming pools.7 Timely reporting of suspected cases by primary care can help public health colleagues identify whether they are connected by a source, such as swimming pools, in order to control a potential outbreak (as seen in the recent outbreak in the West Midlands).
MANAGEMENT OF PATIENTS
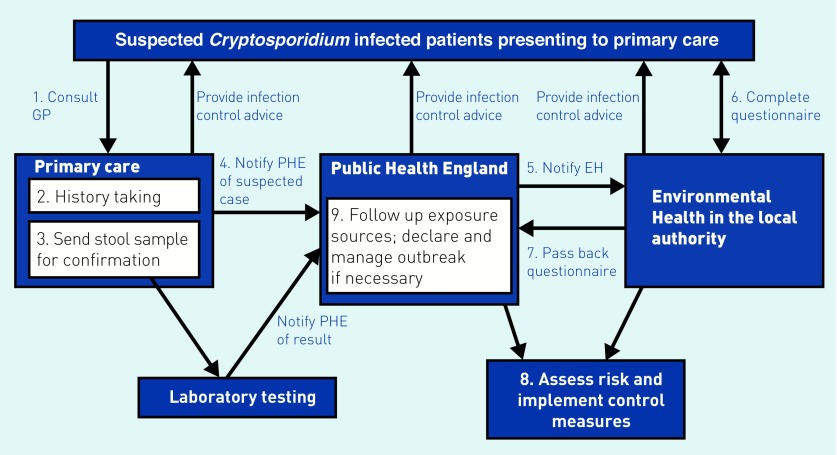
Figure 1 highlights the typical roles played by GPs, PHE, and associated organisations in managing a patient with suspected cryptosporidiosis.
Figure 1.
Management flowchart for a suspected Cryptosporidium patient presenting to primary care and the key roles played by each local agency. EH = environmental health. PHE = Public Health England.
Role of primary care
Clinical suspicion
As a busy GP with a limited time for consultations, history taking may help to identify patients at a higher risk of cryptosporidiosis presenting with gastrointestinal symptoms. Although infection occurs in all ages, it is most commonly seen in children <5 years old, with a decreasing infection rate with increasing age.3 Groups at particular risk of infection include contacts of confirmed cases, individuals with direct or indirect contact with a variety of farm and domestic animals, those who have travelled to less developed countries or been in contact with such travellers, who have recently visited a swimming pool, or have had contact with raw water.
Collection of stool samples for microbiological confirmation supplements epidemiological and environmental data, and can help to determine the source of the outbreak. Genotyping analysis can also help to identify the species and origin; C. hominis (genotype 1) is a human-adapted species and responsible for most cases, whereas C. parvum (genotype 2) has many animal hosts.7
Notifying public health
Infection with Cryptosporidium is notifiable; notification to PHE should occur as soon as possible when infection is suspected without waiting for microbiological confirmation to allow PHE to monitor potential outbreaks and apply control measures.2 If the affected individual is a food handler or works with vulnerable groups (such as older people, the young, or those in poor health) they may need to inform their employer. Public health can assist with this.
Clinical advice
There is no specific treatment available. Replacing fluids is important to avoid dehydration. Advice on infection control measures should be provided to further help prevent the spread of infection. As Cryptosporidium and the affected stools are highly infectious, the household should follow strict handwashing after contact with faeces, nappies, and animals, with safe disposal of contaminated waste. Separate towels and hot machine washes should also be used. The individual should not return to work or school until free from symptoms for 48 hours. This guidance includes food handlers (microbiological clearance is not required). Swimming should be advised against until the patient is clear of diarrhoea for at least 2 weeks. Key prevention steps to avoid re-infection include washing hands thoroughly when preparing food and going to the toilet, washing fruit and vegetables before use, avoiding contact with infected farm animals and humans, and not drinking raw water.
Response coordinated by PHE
Following notification by primary care, PHE will inform the local authority Environmental Health Officers (EHOs) who will then get in touch with the patient to complete a standard questionnaire, the aim of which is to: assess an individual patient’s circumstances, identify risk factors, identify a source of infection, and check for epidemiological links to other cases to identify any clusters. PHE also receives laboratory notifications on confirmed cases that may have presented elsewhere, for example, accident and emergency or secondary care.
EHOs will then send the completed questionnaire back to PHE who will conduct a risk assessment based on potential exposure sources and the epidemiology of the patient. If infection with Cryptosporidium is confirmed and a common source of infection has been identified with other cases, PHE will lead outbreak investigations with the help of multidisciplinary teams involving microbiologists, epidemiologists, local authority colleagues, communications officers, and water company representatives as appropriate. If a hazard is identified, then it is followed up with environmental health to implement specific control measures.
Provenance
Freely submitted; externally peer reviewed.
Competing interests
The authors have declared no competing interests.
Discuss this article
Contribute and read comments about this article: bjgp.org/letters
REFERENCES
- 1.Heyman DL, editor. Control of communicable diseases manual. 19th edn. Washington, DC: American Public Health Association; 2008. [Google Scholar]
- 2.Hawker J, Begg N, Blair I, et al. Communicable disease control and health protection handbook. 3rd edn. Oxford: Wiley-Blackwell; 2012. [Google Scholar]
- 3.Public Health England Cryptosporidium: statistics 2000 to 2012. 2013. https://www.gov.uk/government/publications/cryptosporidium-statistics-2000-to-2012 (accessed 13 Jun 2017)
- 4.MacKenzie WR, Hoxie NJ, Proctor ME, et al. A massive outbreak in Milwaukee of cryptosporidium infection transmitted through the public water supply. N Engl J Med. 1994;331(3):161–167. doi: 10.1056/NEJM199407213310304. [DOI] [PubMed] [Google Scholar]
- 5.Coetzee N, Edeghere O, Orendi J, et al. A swimming pool-associated outbreak of cryptosporidiosis in Staffordshire, England, October to December 2007. Euro Surveill. 2008;13(45) pii: 19028. [PubMed] [Google Scholar]
- 6.Bouchier I. Cryptosporidium in water supplies; Third report of the group of experts. London: Department of the Environment, Transport and the Regions, Department of Health; 1998. http://www.dwi.gov.uk/research/bouchier/ (accessed 28 Jul 2017) [Google Scholar]
- 7.Chalmers RM, Giles M. Zoonotic cryptosporidiosis in the UK — challenges for control. J Appl Microbiol. 2010;109(5):1487–1497. doi: 10.1111/j.1365-2672.2010.04764.x. [DOI] [PubMed] [Google Scholar]