Abstract
Background
Initial medication non-adherence is highly prevalent in primary care but no previous studies have evaluated its impact on the use of healthcare services and/or days on sick leave.
Aim
To estimate the impact of initial medication non-adherence on the use of healthcare services, days of sick leave, and costs overall and in specific medication groups.
Design and setting
A 3-year longitudinal register-based study of all primary care patients (a cohort of 1.7 million) who were prescribed a new medication in Catalonia (Spain) in 2012.
Method
Thirteen of the most prescribed and/or costly medication subgroups were considered. All medication and medication subgroups (chronic, analgesics, and penicillin) were analysed. The number of healthcare services used and days on sick leave were considered. Multilevel multivariate linear regression was used. Three levels were included: patient, GP, and primary care centre.
Results
Initially adherent patients made more use of medicines and some healthcare services than non-adherent and partially adherent patients. They had lower productivity losses, producing a net economic return, especially when drugs for acute diseases (such as penicillins) were considered. Initial medication non-adherence resulted in a higher economic burden to the system in the short term.
Conclusion
Initial medication non-adherence seems to have a short-term impact on productivity losses and costs. The clinical consequences and long-term economic consequences of initial medication non-adherence need to be assessed. Interventions to promote initial medication adherence in primary care may reduce costs and improve health outcomes.
Keywords: big data, database, health services research, medication adherence, primary health care, sick leave
INTRODUCTION
Non-adherence to medication is related to worsening health status and disease progression.1–4 Post-initiation medication non-adherence (discontinuation and/or suboptimal dosing) increases the use of healthcare services and costs.5–7 However, there is little evidence about initial medication non-adherence or primary non-adherence,8,9 that is, not filling the prescription for a newly-prescribed medication.10,11 Interest in initial medication non-adherence has grown recently.10 The prevalence of initial medication non-adherence in primary care ranges from 7% to 28%, depending on the definition of initial medication non-adherence, the medication, the country, and the population under consideration.8,12,13 To the authors’ knowledge, the economic consequences of initial medication non-adherence have not been explored, but they would be expected to be at least as high as for post-initiation medication non-adherence.5,6 The recent growth of real world evidence (‘big data’) in health care offers an opportunity to explore this issue in large systems and with highly representative samples.14–16
The aim of this study was to estimate the impact of initial medication non-adherence on the use of healthcare services, days on sick leave, and overall costs, and in specific relevant medication groups.
METHOD
This was a 3-year longitudinal register-based cohort study including all primary care patients who were prescribed a new medication in Catalonia (Spain) in 2012. The methods have been described in detail elsewhere.13
Setting
The Spanish public healthcare system provides universal coverage for citizens through a public system financed by taxes and is free at the point of use, with the sole exception of medicines. The system is decentralised, thus each of the 17 Spanish Autonomous Communities controls its own health planning, public health, and the management of health services.17 In Spain, primary care is the patient’s first point of contact with the public health system. Each individual has an assigned GP who issues all prescriptions, except when the consultation is done by a substitute or resident GP at the same primary care centre. In Catalonia, a Spanish region with over 7.5 million inhabitants, almost 300 of 371 publicly-funded primary care centres are managed by the Catalan Health Service (Institut Català de la Salut), which covers 80% of the population (5.8 million people).18 During the study period, two medication co-payment policies were introduced in Catalonia.19
How this fits in
The prevalence of initial medication non-adherence in primary care ranges from 7% to 28%. To date, only three articles have compared distinct medication groups in large representative samples and there is no published evidence on the economic impact of initial medication non-adherence. This study assessed the impact of initial medication non-adherence in primary care on the use of healthcare services and sick leave in a large representative sample of 1.7 million patients. The results suggest that initial medication non-adherence is not only highly prevalent but also has an impact on the use of services and costs. It might also imply a negative impact on health. Decision makers should consider these results and prioritise future actions to reduce initial medication non-adherence in order to improve the efficiency of primary care services.
Data source
Data were obtained from the System for the Development of Research in Primary Care database (SIDIAP)18,20 that includes information on primary care patients covered by the Catalan Health Service.18 Information is provided on patients’ sociodemographic and clinical data; including prescribed and dispensed medication; sociodemographic characteristics of the prescriber; and primary care centre characteristics. Information is also provided on healthcare services used and days on sick leave for all patients.
Cohort study
This study includes all patients aged >14 years old who were prescribed a new medication during 2012 that was included in 13 pharmacological subgroups. The selection of these medications was based on criteria of prevalence of use and cost to the public system, so that the 13 drugs were among the 10 most prescribed and the 10 most costly pharmacotherapeutic subgroups in primary care in Catalonia in 2014 (the most current data at the time of study design).13
As in previous studies, to ensure that only newly-prescribed medicines were considered, a 3-month pre-period was established so that patients who had been prescribed a medicine from the same pharmacotherapeutic subgroup in the 3 months prior to the prescription of interest were excluded from the study. An exception was made for the subgroup who were prescribed extended-spectrum penicillin where a 1-month pre-period was set (due to the pharmacotherapeutic characteristics of these drugs, that is two prescriptions issued in two consecutive months may be indicated for non-related events).13
Definition of initial medication non-adherence
Initial medication non-adherence was defined, following International Society for Pharmacoeconomics and Outcomes Research ISPOR recommendations, as not filling the prescription for a newly-prescribed medicine in the month of prescription or in the following month (follow-up period).10
Patients may have been prescribed more than one new treatment during the study period, leading to the classification of patients into three profiles of initial medication non-adherence-related behaviour:
initially adherent (patients that fill all prescriptions);
initially non-adherent (patients that fill no prescription); and
partially adherent (patients that fill some initial but not all prescriptions).
Use of health services and days on sick leave
The use of services registered in the SIDIAP database includes number and date of visits to primary care professionals (GP or nurse), specialist clinician visits, and laboratory or clinical tests (nuclear medicine and diagnostic imaging). Use of medication and sick leave are also registered. Sick leave is registered in the database when the GP issues a medical certificate. Days of sick leave and use of services were obtained for the 12 months before and the 24 months after the prescription.
Cost analysis
Unit costs were searched for the use of healthcare resources and productivity losses (details available from authors on request). Healthcare costs from a public sector perspective were valued in Euros (€) from the year 2014. The prices assigned to healthcare services were gathered from the Catalan Government Official Bulletin.21,22 The exact costs of publicly covered medicines and laboratory and medical tests were obtained from the SIDIAP database. To estimate the cost to the public sector, both the minimum23 and mean24 salary in Spain in 2014 were used to calculate productivity losses from the human capital perspective.
Patient, GP, and primary care centre characteristics
Patient characteristics included sex, age (at the time of the first initial prescription), socioeconomic status, nationality, comorbidities, and number of new prescriptions issued in the study period. Also collected were data about GPs’ sex, age, and GP type (assigned or substitute/resident), and type of primary care centre (resident-training centre or not).
Statistical analysis
Detailed information on data preprocessing is available from the authors on request. The differences in use of services, days on sick leave, and costs were analysed using multilevel multivariate linear regression with three levels: patient, GP, and primary care centre. Linear regression was used to analyse large datasets (>10 000 observations) with the average of the variables approximately normally distributed around the true mean.25 Robust standard errors were used to account for deviations from the normal distribution. Adjustment for costs incurred during the 12 months prior to the initial prescription was considered essential and all models were adjusted for previous use of services/costs. Other covariates were tested one at a time to select relevant covariates to adjust the multivariate model, using criteria of statistical and clinical significance. Categorical variables with P<0.05 which showed differences between their values >10% of the mean use of service or cost, and continuous variables with P<0.05 which showed differences >0.5% of the mean use of service or cost, for age, or 5% mean use/cost for comorbidities, were selected as adjustment variables.
Subgroup analysis
It was hypothesised that the impact on use of services and days on sick leave would differ between therapeutic groups. Considering the main indications of the 13 pharmacotherapeutic subgroups under study, medicines were classified into three subgroups: chronic medication, analgesics, and penicillin (for further details see Box 1).
Box 1. Medications included for each subgroup.
| Chronic medication |
| Insulins and analogues for injection, long acting (ATC code: A10AE; platelet aggregation inhibitors excluding heparin (B01AC); ACE inhibitors, plain (C09AA); HMG CoA reductase inhibitors (C10AA); other antiepileptics (N03AX); selective serotonin reuptake inhibitors (N06AB); adrenergics in combination with corticosteroids or other drugs, excluding anticholinergics (R03AK); and anticholinergics (R03BB). |
| Analgesics |
| Propionic acid derivatives (M01AE); and anilides (N02BE). |
| Penicillins |
| Extended-spectrum penicillin (A02BC). |
| All medication |
| Benzodiazepine derivatives (N05BA); and proton pump inhibitors (A02BC). |
ATC = Anatomical Therapeutic Chemical Classification System.
The same patient could be considered initially adherent in one medication subgroup analysis and initially non-adherent in another medication subgroup analysis. Analyses were performed with Stata MP (version 13.0) and MlwiN (version 2.33) using ‘runmlwin’ command.
RESULTS
A total of 1 678 941 patients from 291 primary care centres received an initial prescription for a considered medication in 2012 and fulfilled the inclusion criteria. The chronic medication group included 463 030 of these patients; the analgesics group, 1 110 664; and the penicillin group, 313 165 (Table 1). The characteristics of patients, GPs, and primary care centres overall and for each medication group are detailed in Table 2. Characteristics of patients for each initial medication non-adherence profile are available from authors on request).
Table 1.
Patients’ initial medication adherence status in Catalonia, Spain in 2012
| Subgroup analysis | Initially adherent, na (%) | Partially adherent, na (%) | Initially non-adherent, na (%) | Total patients in each group, Na |
|---|---|---|---|---|
| Chronic medication | 401 033 (86.61) | 13 123 (2.83) | 48 874 (10.56) | 463 030 |
| Analgesics | 816 215 (73.49) | 81 433 (7.33) | 213 016 (19.18) | 1 110 664 |
| Penicillins | 279 210 (89.16) | 5233 (1.67) | 28 722 (9.17) | 313 165 |
| All medicationb | 1 241 098 (73.92) | 215 685 (12.85) | 222 158 (13.23) | 1 678 941 |
Sample sizes in all medications are not the result of the sum of sample sizes of each medication group because the classification of patients as initially adherent, partially adherent, or initially non-adherent depends on the number of medications considered.
All medication includes chronic medication, analgesics, penicillins, and medicines not included in any of these groups (benzodiazepines and proton pump inhibitors).
Table 2.
Patient, GP, and primary healthcare centre characteristics for all medications and by medication groups
| Variable | All medications (N= 1 678 941) | Drugs for chronic diseases (N= 463 030) | Analgesics (N= 1 110 664) | Penicillins (N= 313 165) |
|---|---|---|---|---|
| Patient level | ||||
| Sex: female, n (%) | 967 593 (57.63) | 262 365 (56.66) | 653 788 (58.86) | 185 104 (59.11) |
| Age, mean (SD) | 52.66 (19.24) | 61.85 (16.69) | 50.23 (19.17) | 49.06 (19.71) |
|
| ||||
| Area socioeconomic status,an (%) | ||||
| Urban 1 | 233 152 (13.89) | 71 238 (15.39) | 142 558 (12.84) | 39 329 (12.56) |
| Urban 2 | 267 777 (15.95) | 75 316 (16.27) | 173 781 (15.65) | 48 081 (15.35) |
| Urban 3 | 280 554 (16.71) | 77 064 (16.64) | 187 324 (16.87) | 52 233 (16.68) |
| Urban 4 | 295 149 (17.58) | 79 093 (17.08) | 202 112 (18.20) | 55 825 (17.83) |
| Urban 5 | 294 369 (17.53) | 74 687 (16.13) | 208 831 (18.80) | 57 841 (18.47) |
| Rural | 307 940 (18.34) | 85 632 (18.49) | 196 058 (17.65) | 59 856 (19.11) |
|
| ||||
| Nationality, n (%) | ||||
| Spanish | 1 349 005 (80.35) | 417 930 (90.26) | 854 293 (76.92) | 251 006 (80.15) |
| Americanb | 134 965 (8.04) | 19 057 (4.12) | 102 827 (9.26) | 22 919 (7.32) |
| Asian/Oceanian | 35 055 (2.09) | 4090 (0.88) | 28 967 (2.61) | 6177 (1.97) |
| Other European | 59 196 (3.53) | 11 947 (2.58) | 40 198 (3.62) | 11 291 (3.61) |
| African | 100 720 (6.00) | 10 006 (2.16) | 84 379 (7.60) | 21 772 (6.95) |
| Number of comorbidities; grouped,c mean (SD) | 1.91 (1.46) | 2.49 (1.45) | 1.81 (1.45) | 1.84 (1.50) |
| Number of new prescriptions,d mean (SD) | 1.79 (1.07) | 1.19 (0.48) | 1.33 (0.59) | 1.11 (0.35) |
|
| ||||
| GP level, N | 6706 | 5835 | 6512 | 5919 |
| Sex: female, n (%) | 4681 (69.80) | 3990 (68.38) | 4517 (69.36) | 4046 (68.36) |
| Age, mean (SD) | 45.38 (11.35) | 45.68 (11.30) | 45.44 (11.34) | 45.64 (11.30) |
| Assigned GPs, n (%) | 5032 (75.04) | 4503 (77.17) | 4919 (75.54) | 4539 (76.69) |
|
| ||||
| PCC level, N | 291 | 287 | 290 | 288 |
| Training centre, n (%) | 72 (24.74) | 72 (25.09) | 72 (24.83) | 72 (25.00) |
Urban categories range from 1 to 5, quintiles of increasing socioeconomic status in urban areas, while rural refers to people who live in rural areas.
American covers North, Central and South-Americans.
Diseases were recorded according to the International Statistical Classification of Diseases and Related Health Problems (ICD-10) and grouped as follows: allergy, pain, respiratory, disability, cardiovascular, mental, neurological, diabetes mellitus, digestive, and thyroid-related diseases.
New prescriptions included in the same medication group. PCC = primary care centre.
Most patients initially adhered to medication (from 73% to 89%), between 9% and 19% were fully initially non-adherent patients, while 2% to 13% were partially adherent (Table 1). A total of 58 242 patients (3.5% of the sample) were initially adherent in one medication subgroup analysis and initially non-adherent in another medication subgroup analysis.
Use of healthcare services and days on sick leave
Table 3 shows the mean use of healthcare services and days of sick leave in the 2 years since the new prescription. The most frequently used services were GP visits to the primary care centre (11 to 13 mean visits) and medications prescribed by a healthcare system GP (9 to 16), while the least used services were home visits and nuclear medicine tests (mean ≤1). The mean number of days on sick leave was around 14.
Table 3.
Use of healthcare services and productivity losses for all medications and medication groups for 2 years after new prescription
| Variable | All medications, mean n (SD) | Drug for chronic diseases, mean n (SD) | Analgesics, mean n (SD) | Penicillins, mean n (SD) |
|---|---|---|---|---|
| Use of servicesa | ||||
| GP visit in PCC | 10.60 (9.13) | 13.04 (10.32) | 10.65 (9.20) | 11.40 (10.03) |
| Home GP visit | 0.26 (1.56) | 0.47 (2.17) | 0.21 (1.34) | 0.21 (1.35) |
| Nurse visit in PCC | 5.86 (10.34) | 8.12 (12.60) | 5.62 (10.07) | 6.17 (10.65) |
| Home nurse visit | 0.46 (4.22) | 0.87 (5.71) | 0.35 (3.67) | 0.34 (3.49) |
| Specialist consultation | 1.44 (1.88) | 1.73 (2.12) | 1.47 (1.89) | 1.52 (1.95) |
| Laboratory test | 1.54 (1.59) | 1.94 (1.69) | 1.48 (1.56) | 1.50 (1.59) |
| Nuclear medicine test | 0.01 (0.11) | 0.01 (0.13) | 0.01 (0.11) | 0.01 (0.11) |
| Diagnostic imaging test | 1.02 (1.54) | 1.10 (1.66) | 1.08 (1.59) | 1.11 (1.61) |
| Dispensed medicinesb | 10.26 (9.00) | 15.63 (8.11) | 9.13 (8.75) | 9.54 (8.80) |
|
| ||||
| Productivity losses | ||||
| Days on sick leave | 13.78 (53.64) | 16.34 (63.54) | 14.08 (53.33) | 12.02 (48.54) |
2 years from prescription date.
Refers to medication prescribed by a GP in the primary care public health system. PCC = primary care centre.
Table 4 shows differences in the use of healthcare services and sick leave between initially adherent (reference group), partially adherent, and initially non-adherent patients based on adjusted multilevel multivariate analysis. The results from unadjusted analysis are available from authors on request.
Table 4.
Difference in use of healthcare services and days on sick leave (2012–2014) for each medication group for partially adherent and non-adherent patients in comparison with initially adherent patients based on adjusted multilevel regression analysis
| Variable | All medications, mean (95% CI) | Chronic, mean (95% CI) | Analgesics, mean (95% CI) | Penicillins, mean (95% CI) | ||||
|---|---|---|---|---|---|---|---|---|
| Partially adherent | Initially non-adherent | Partially adherent | Initially non-adherent | Partially adherent | Initially non-adherent | Partially adherent | Initially non-adherent | |
| GP visit in PCC | 0.06a (0.02 to 0.10) | −0.16a (−0.19 to −0.13) | −0.12 (−0.29 to 0.05) | −0.62a (−0.69 to −0.54) | 0.23a (0.17 to 0.29) | −0.13a (−0.16 to −0.10) | −0.17 (−0.10 to 0.07) | −0.09 (−0.18 to 0.01) |
| Home GP visit | 0.01 (−0.01 to 0.01) | 0.03a (0.02 to 0.03) | −0.04 (−0.09 to 0.01) | −0.04a (−0.06 to −0.02) | 0.01 (−0.01 to 0.01) | 0.01a (0.01 to 0.02) | 0.03 (−0.01 to 0.07) | 0.02a (0.01 to 0.03) |
| Nurse visit in PCC | −0.21a (−0.25 to −0.17) | −0.22a (−0.25 to −0.19) | −0.17 (−0.40 to 0.05) | −0.37a (−0.47 to −0.26) | −0.17a (−0.23 to −0.10) | −0.24a (−0.28 to −0.21) | −0.13 (−0.39 to 0.13) | −0.16a (−0.25 to −0.06) |
| Home nurse visit | 0.01 (−0.01 to 0.02) | 0.05a (0.03 to 0.06) | −0.06 (−0.18 to 0.06) | 0.10a (0.06 to 0.14) | 0.01 (−0.01 to 0.03) | 0.01 (−0.01 to 0.02) | 0.01 (−0.07 to 0.08) | 0.07a (0.03 to 0.11) |
| Specialist visit | 0.05a (0.04 to 0.06) | −0.01 (−0.01 to 0.01) | −0.01 (−0.04 to 0.04) | −0.06a (−0.08 to −0.04) | 0.07a (0.06 to 0.09) | 0.01 (−0.01 to 0.01) | 0.06a (0.01 to 0.12) | 0.01 (−0.01 to 0.04) |
| Laboratory test | −0.03a (−0.04 to −0.02) | −0.09a (−0.09 to −0.08) | −0.10a (−0.13 to −0.07) | −0.15a (−0.16 to −0.13) | −0.02a (−0.03 to −0.01) | −0.06a (−0.07 to −0.06) | −0.03 (−0.07 to 0.01) | −0.06a (−0.08 to −0.05) |
| Nuclear medicine test | 0.001 (−0.001 to 0.001) | −0.001 (−0.001 to 0.001) | −0.001 (−0.004 to 0.001) | −0.001 (−0.002 to 0.001) | 0.001 (−0.001 to 0.001) | −0.001 (−0.001 to 0.001) | 0.003 (−0.001 to 0.007) | 0.001 (−0.001 to 0.001) |
| Diagnostic imaging test | 0.06a (0.05 to 0.07) | 0.01a (0.01 to 0.02) | 0.03a (0.01 to 0.06) | −0.01 (−0.03 to 0.01) | 0.05a (0.04 to 0.06) | −0.02a (−0.03 to −0.02) | 0.02 (−0.03 to 0.07) | −0.02a (−0.04 to −0.01) |
| Dispensed medicines (boxes)b | −1.77a (−1.80 to −1.75) | −2.17a (−2.20 to −2.15) | −2.55a (−2.67 to −2.43) | −4.22a (−4.29 to −4.16) | −1.41a (−1.45 to −1.37) | −1.43a (−1.45 to −1.41) | −1.46a (−1.59 to −1.33) | −1.27a (−1.33 to −1.22) |
| Days on sick leave | 3.78a (3.44 to 4.12) | 2.49a (2.26 to 2.73) | 1.87a (0.57 to 3.18) | 2.11a (1.44 to 2.78) | 3.81a (3.33 to 4.31) | 2.71a (2.42 to 2.99) | 3.07a (1.56 to 4.58) | 3.96a (3.27 to 4.65) |
Statistically significant differences (95%)
Medication prescribed by GP in the primary care public healthcare system. PCC = primary care centre.
When all medications were considered, partially adherent patients made the greatest use of GP visits in the primary care centre, specialist visits, and diagnostic imaging tests; while initially non-adherent patients made the most frequent use of GP and nurse visits at home. Initially adherent patients generated the highest costs in terms of medicines and laboratory tests. In the analysis of medication for chronic diseases, initially non-adherent patients showed the lowest use of all types of services, except for home nurse visits.
Initially adherent patients had fewer days on sick leave in all medication group analyses, with mean days on sick leave differences of between 1.9 and 4.0 days shorter than partially and initially non-adherent patients (Table 4).
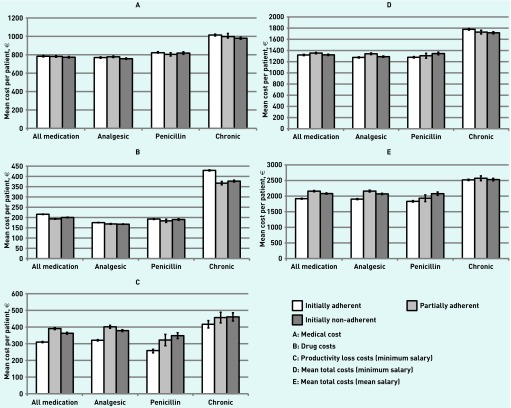
Differences in costs
Figure 1 shows the 2-year adjusted mean differences in costs for each medication group in initially adherent, partially adherent, and initially non-adherent patients in Catalonia (Spain) in 2012. The multilevel adjusted model for mean differences in costs is shown in Table 5. The multilevel unadjusted model is available from authors on request.
Figure 1.
Mean costs per patient (in €, 2012–2014) based on multilevel adjusted analysis for every medication group for initially adherent, partially adherent, and initially non-adherent patients in Catalonia (Spain) in 2012.
Table 5.
Difference in costs (in €, 2012–2014) for each medication group for partially adherent and non-adherent patients in comparison with initially adherent patients based on adjusted multilevel regression analysis
| Cost, € | All medications, mean (95% CI) | Chronic, mean (95% CI) | Analgesics, mean (95% CI) | Penicillins, mean (95% CI) | ||||
|---|---|---|---|---|---|---|---|---|
| Partially adherent | Initially non-adherent | Partially adherent | Initially non-adherent | Partially adherent | Initially non-adherent | Partially adherent | Initially non-adherent | |
| Medical cost | −2.02 (−4.79 to 0.76) | −10.54a (−12.62 to −8.46) | −16.35a (−31.22 to −1.47) | −34.51a (−40.84 to −28.18) | 8.07a (3.60 to 12.57) | −12.54a (−14.82 to −10.26) | −12.51 (−29.56 to 4.54) | −6.84a (−13.42 to −0.27) |
| Drug cost | −22.59a (−24.21 to −20.97) | −15.38a (−16.41 to −14.35) | −62.03a (−73.17 to −50.89) | −55.75a (−55.75 to −48.60) | −6.40a (−8.29 to −4.52) | −7.49a (−8.48 to −6.49) | −10.99a (−19.17 to −3.47) | −3.21a (−6.04 to −0.38) |
| Sick leave cost (minimum salary) | 80.90a (73.54 to 88.26) | 52.99a (47.68 to 58.31) | 39.97a (11.87 to 68.05) | 44.30a (29.90 to 58.70) | 80.62a (70.00 to 91.26) | 57.91a (51.81 to 64.02) | 67.20a (32.13 to 102.27) | 85.20a (70.42 to 99.97) |
| Sick leave cost (mean salary) | 244.89a (222.61 to 267.17) | 160.42a (144.32 to 176.50) | 120.96a (35.93 to 205.99) | 134.10a (90.50 to 177.69) | 244.05a (211.88 to 276.23) | 175.30a (156.81 to 193.79) | 203.42a (97.26 to 309.58) | 257.89a (213.16 to 302.61) |
| Total cost (minimum salary for sick leave) | 34.56a (25.48 to 43.63) | 2.58 (−3.82 to 8.98) | −49.55a (−85.90 to −13.20) | −61.76a (−79.65 to −43.86) | 65.21a (52.47 to 77.96) | 14.15a (6.89 to 21.41) | 9.86 (−36.42 to 56.15) | 56.86a (38.05 to 75.67) |
| Total cost (mean salary for sick leave) | 242.12a (218.33 to 265.91) | 164.71a (147.70. to 181.71) | 52.30 (−37.43 to 142.03) | 10.74 (−35.61 to 57.10) | 256.59a (222.78 to 290.40) | 166.60a (149.85 to 186.34) | 144.99a (30.35 to 259.64) | 229.99a (182.60 to 277.37) |
Statistically significant differences. PCC = primary care centre.
With few exceptions, initially adherent patients generated higher medical and drug-related costs than non-adherent and partially adherent patients. On the other hand, in all cases, initially adherent patients generated lower costs than non-adherent and partially adherent patients in terms of productivity losses. When total costs were considered, higher costs in use of healthcare services and drugs were offset by lower productivity losses in all scenarios, with the exception of chronic conditions. Patients who initially adhered to chronic medication incurred the highest total costs but only when the minimum salary for sick leave was used to calculate their total costs (Figure 1).
DISCUSSION
Summary
The results of the study show that, overall, initially non-adherent patients made less use of: GP and nurse consultations at a primary care centre, medicines, and laboratory and nuclear medicine tests. However, they made more use of home GP and nurse consultations, which are more expensive, and had more days on sick leave. Partially adherent patients used fewer medicines, had fewer nurse consultations at primary care centres, and required fewer laboratory tests than initially adherent patients, but made greater use of GP and specialist consultations, and diagnostic imaging tests, and had more days on sick leave.
When services and sick leave were translated into costs, it was observed that initially non-adherent patients generate higher costs for the government than adherent patients. The only exceptions were patients who did not initiate a drug for a chronic disease, although this was only true if the minimum salary in Spain was assumed for cost of sick leave calculation.
It is important to note that costs for chronic diseases were only evaluated in the short-term (2 years). With exceptions, such as depression, chronic diseases have the greatest impact on health and use of services in the long term and a peak in demand for healthcare services at the moment of diagnosis.26 Given the volume of patients who are initially non-adherent to medication and the effect of applying the mean impact of initial medication non-adherence on costs in all medication analysis, the range of the total economic impact for the government in Catalonia could be between €8 million (minimum salary for sick leave) and almost €89 million (mean salary for sick leave).
Strengths and limitations
This is the first study to assess the economic consequences of initial medication non-adherence and among the first to estimate the economic consequences of a medication non-adherence event in almost an entire population. Big data provide high representativeness, which increases the validity of the results.
Regarding limitations in the database registries, it was not possible to assess differences in hospital admissions and interventions between adherent and non-adherent patients. These costs have been shown to be higher in patients who display post-initiation medication non-adherence.6,7 Furthermore, it was not possible to evaluate the clinical impact of non-adherence and, as mentioned above, only the short-term impact of non-adherence to chronic medication could be evaluated. In the future, clinical indicators should be searched in the database for specific diseases and economic models constructed to evaluate the long-term consequences of initial medication non-adherence.
Another database limitation is that emergency primary care centre visits cannot be distinguished from regular visits. However, as stated above, home visits are usually emergency visits so could indicate the impact of initial medication non-adherence on emergency visits.
Until July 2014, employees were allowed to take up to 3 consecutive days sick leave before they had to take a medical certificate to their employer. Although patients could get a medical certificate for short sick leave (27% of database-registered sick leave was for no more than 3 days), it is possible that productivity losses were underestimated. Furthermore, there was no information about the reason for the sick leave, therefore it is not possible to conclude that it was linked to the treatment that was not initiated.
Primary care electronic databases may contain some errors or missing data in their registries. Missing data were dealt with by using imputation techniques. Thus, 3% of patients received a new prescription without registration of the GP consultation. These could be due to phone consultations, prescriptions made out to the person accompanying the patient (typically the partner), or prescriptions issued during a nurse visit. To minimise bias, an extra GP consultation was imputed to these patients.
Finally, it is not certain that patients who filled a prescription initiated the treatment or that patients who did not fill the prescription are non-adherent (for example, they may have used the medicine cabinet effect, accessing remaining pills at home from previous use of over-the-counter medicines).13 However, this is very unlikely for most of the drugs evaluated (penicillin or chronic).
Comparison with existing literature
To the best of the authors’ knowledge, this is the first study to evaluate the impact of initial medication non-adherence on the use of healthcare services and days on sick leave. Studies examining the economic consequences of post-initiation medication non-adherence also reported adherent patients making greater use of services than non-adherent patients in some pharmacologic groups.5,6 On the one hand, this could be due to the need for followup visits for the assessment of treatment effectiveness in adherent patients and, in some cases, to deal with changes in treatment and/or side-effects. On the other hand, non-adherent patients might miss appointments because they did not take the medication.27 Previous post-initiation medication non-adherence studies also showed how higher drug costs were offset by savings in other medical services,28 while higher absenteeism was also observed in non-adherent patients.29
In the framework of health economics, health consequences need to be taken into account when deciding whether improving initial medication adherence is an efficient strategy in primary care. Home visits are mainly emergencies. The greater use of home visits by non-adherent patients, together with longer periods of sick leave, could indicate that these patients have worse health outcomes as a consequence of non-adherence. This is supported by the fact that more home visits are observed specifically in patients prescribed penicillins and analgesics, which are prescribed for diseases with shorter-term impact on health than chronic diseases.
In this regard, post-initiation medication non-adherence seems highly influenced by modifiable factors,13,30 and initial medication non-adherence seems to be similar.
Implications for research and practice
Initial medication non-adherence seems to have an impact on productivity losses and costs, and the data suggest that it could also have a negative impact on health because this behaviour is associated with greater use of home health visits. Savings in use of medicines are offset by increased use of other services and more days off work. It is recommended that future research focuses on designing and developing interventions to reduce the prevalence of initial medication non-adherence in primary care.31
Future studies also need to confirm whether there are negative consequences of initial medication non-adherence on health, and evaluate the long-term consequences in terms of costs and health of initial medication non-adherence in chronic diseases. Specific policies and interventions addressed to reduce non-adherence should be implemented in Spanish primary care to reduce the impact of this behaviour on the system.
Acknowledgments
The authors thank Mr Christopher Charlton from University of Bristol for his help in command ‘runmlwin’ configuration to develop multilevel linear regression analysis and Mr Stephen Kelly for his editorial help.
Funding
This research was funded by the project ‘The problem of non-initiation of pharmacological treatment: mixed-methods evaluation’ (PI14/00052) included in the Spanish National Plan for R&D cofounded by Institute of Health Carlos III (ISCIII) and the European Fund for Regional Development (FEDER). Maria Rubio-Valera received a research contract from the Institute of Health Carlos III (Red RD12/0005/008).
Ethical approval
Approval for the study was obtained from the authors’ institutions (P14/140; PIC-111-14).
Provenance
Freely submitted; externally peer reviewed.
Competing interests
The authors have declared no competing interests.
Discuss this article
Contribute and read comments about this article: bjgp.org/letters
REFERENCES
- 1.Ismaila A, Corriveau D, Vaillancourt J, et al. Impact of adherence to treatment with tiotropium and fluticasone propionate/salmeterol in chronic obstructive pulmonary diseases patients. Curr Med Res Opin. 2014;30(7):1427–1436. doi: 10.1185/03007995.2014.908828. [DOI] [PubMed] [Google Scholar]
- 2.Chang PY, Chien LN, Lin YF, et al. Nonadherence of oral antihyperglycemic medication will increase risk of end-stage renal disease. Medicine (Baltimore) 2015;94(47):e2051. doi: 10.1097/MD.0000000000002051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Modi A, Siris ES, Tang J, Sen S. Cost and consequences of noncompliance with osteoporosis treatment among women initiating therapy. Curr Med Res Opin. 2015;31(4):757–765. doi: 10.1185/03007995.2015.1016605. [DOI] [PubMed] [Google Scholar]
- 4.Marks DF, Murray M, Evans B, Estacio EV. Health psychology: theory, research and practice. 3rd edn. London: SAGE Publications; 2011. Medicine taking: adherence and resistance. pp. 410–436. [Google Scholar]
- 5.Dragomir A, Côté R, White M, et al. Relationship between adherence level to statins, clinical issues and health-care costs in real-life clinical setting. Value Health. 2010;13(1):87–94. doi: 10.1111/j.1524-4733.2009.00583.x. [DOI] [PubMed] [Google Scholar]
- 6.Roebuck MC, Liberman JN, Gemmill-Toyama M, Brennan TA. Medication adherence leads to lower health care use and costs despite increased drug spending. Health Aff (Millwood) 2011;30(1):91–99. doi: 10.1377/hlthaff.2009.1087. [DOI] [PubMed] [Google Scholar]
- 7.Katon W, Cantrell CR, Sokol MC, et al. Impact of antidepressant drug adherence on comorbid medication use and resource utilization. Arch Intern Med. 2005;165(21):2497–2503. doi: 10.1001/archinte.165.21.2497. [DOI] [PubMed] [Google Scholar]
- 8.Pottegård A, Christensen RD, Houji A, et al. Primary non-adherence in general practice: a Danish register study. Eur J Clin Pharmacol. 2014;70(6):757–763. doi: 10.1007/s00228-014-1677-y. [DOI] [PubMed] [Google Scholar]
- 9.Raebel MA, Schmittdiel J, Karter AJ, et al. Standardizing terminology and definitions of medication adherence and persistence in research employing electronic databases. Med Care. 2013;51(8 Suppl 3):S11–S21. doi: 10.1097/MLR.0b013e31829b1d2a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hutchins DS, Zeber JE, Roberts CS, et al. Initial medication adherence: review and recommendations for good practices in outcomes research: an ISPOR medication adherence and persistence special interest group report. Value Health. 2015;18(5):690–699. doi: 10.1016/j.jval.2015.02.015. [DOI] [PubMed] [Google Scholar]
- 11.Zeber JE, Manias E, Williams AF, et al. A systematic literature review of psychosocial and behavioral factors associated with initial medication adherence: a report of the ISPOR medication adherence & persistence special interest group. Value Health. 2013;16(5):891–900. doi: 10.1016/j.jval.2013.04.014. [DOI] [PubMed] [Google Scholar]
- 12.Raebel MA, Ellis JL, Carroll NM, et al. Characteristics of patients with primary non-adherence to medications for hypertension, diabetes, and lipid disorders. J Gen Intern Med. 2012;27(1):57–64. doi: 10.1007/s11606-011-1829-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Aznar-Lou I, Fernández A, Gil-Girbau M, et al. Initial medication non-adherence: prevalence and predictive factors in a cohort of 1.6 million primary care patients. Br J Clin Pharmacol. 2017;83(6):1328–1340. doi: 10.1111/bcp.13215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Roski J, Bo-Linn GW, Andrews TA. Creating value in health care through big data: opportunities and policy implications. Health Aff (Millwood) 2014;33(7):1115–1122. doi: 10.1377/hlthaff.2014.0147. [DOI] [PubMed] [Google Scholar]
- 15.Bates DW, Saria S, Ohno-Machado L, et al. Big data in health care: using analytics to identify and manage high-risk and high-cost patients. Health Aff (Millwood) 2014;33(7):1123–1131. doi: 10.1377/hlthaff.2014.0041. [DOI] [PubMed] [Google Scholar]
- 16.Collins B. Big data and health economics: strengths, weaknesses, opportunities and threats. Pharmacoeconomics. 2016;34(2):101–106. doi: 10.1007/s40273-015-0306-7. [DOI] [PubMed] [Google Scholar]
- 17.García-Armesto S, Begoña Abadía-Taira MB, Durán A, et al. Spain: Health system review. Health Syst Transit. 2010;12(4):1–295. [PubMed] [Google Scholar]
- 18.García-Gil Mdel M, Hermosilla E, Prieto-Alhambra D, et al. Construction and validation of a scoring system for the selection of high-quality data in a Spanish population primary care database (SIDIAP) Inform Prim Care. 2011;19(3):135–145. doi: 10.14236/jhi.v19i3.806. [DOI] [PubMed] [Google Scholar]
- 19.Puig-Junoy J, Rodríguez-Feijoó S, Lopez-Valcarcel BG. Paying for formerly free medicines in Spain after 1 year of co-payment: changes in the number of dispensed prescriptions. Appl Health Econ Health Policy. 2014;12(3):279–287. doi: 10.1007/s40258-014-0097-6. [DOI] [PubMed] [Google Scholar]
- 20.Bolíbar B, Fina Avilés F, Morros R, et al. SIDIAP database: electronic clinical records in primary care as a source of information for epidemiologic research. [In Spanish] Med Clin (Barc) 2012;138(14):617–621. doi: 10.1016/j.medcli.2012.01.020. [DOI] [PubMed] [Google Scholar]
- 21.Catalonia Government. Health Department. Orden SLT/106/2013. The Official Journal of the Government of Catalonia. [In Spanish]. http://portaldogc.gencat.cat/utilsEADOP/PDF/6387/1302585.pdf (accessed 17 Jul 2017)
- 22.Catalonia Government. Health Department. Orden SLT/79/2014. The Official Journal of the Government of Catalonia. [In Spanish]. http://portaldogc.gencat.cat/utilsEADOP/PDF/6589/1345713.pdf (accessed 17 Jul 2017)
- 23.Spanish Ministry of Employment and Social Security. Royal decree 1046/2013. Official State Gazette. [In Spanish]. https://www.boe.es/boe/dias/2013/12/30/pdfs/BOE-A-2013-13764.pdf (accessed 17 Jul 2017)
- 24.Spanish Statistics National Institute. Economically Active Population Survey (EAPS). Year 2014. Madrid, Spain. [In Spanish]. http://www.ine.es/prensa/np939.pdf (accessed 17 Jul 2017)
- 25.Lumley T, Diehr P, Emerson S, Chen L. The importance of the normality assumption in large public health data sets. Annu Rev Public Health. 2002;23:151–169. doi: 10.1146/annurev.publhealth.23.100901.140546. [DOI] [PubMed] [Google Scholar]
- 26.Løkke A, Hilberg O, Tønnesen P, et al. Direct and indirect economic and health consequences of COPD in Denmark: a national register-based study: 1998–2010. BMJ Open. 2014;4(1):e004069. doi: 10.1136/bmjopen-2013-004069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brown MT, Bussell J, Dutta S, et al. Medication adherence: truth and consequences. Am J Med Sci. 2016;351(4):387–399. doi: 10.1016/j.amjms.2016.01.010. [DOI] [PubMed] [Google Scholar]
- 28.Sokol MC, McGuigan KA, Verbrugge RR, Epstein RS. Impact of medication adherence on hospitalization risk and healthcare cost. Med Care. 2005;43(6):521–530. doi: 10.1097/01.mlr.0000163641.86870.af. [DOI] [PubMed] [Google Scholar]
- 29.Carls GS, Roebuck MC, Brennan TA, et al. Impact of medication adherence on absenteeism and short-term disability for five chronic diseases. J Occup Environ Med. 2012;54(7):792–805. doi: 10.1097/JOM.0b013e31825463e9. [DOI] [PubMed] [Google Scholar]
- 30.Gil M, Aznar I, Peñarrubia MT, et al. The problem of non-initiation of pharmacological treatment: preliminary results from a qualitative study. [In Spanish]. Farmacéuticos Comunitarios. 2016;8(Suppl 1) [Google Scholar]
- 31.Conn VS, Ruppar TM, Enriquez M, Cooper PS. Patient-centered outcomes of medication adherence interventions: systematic review and meta-analysis. Value Health. 2016;19(2):277–285. doi: 10.1016/j.jval.2015.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]