Abstract
Background
The primary objectives of the current prospective longitudinal study were to (a) describe social functioning outcomes and (b) identify childhood predictors of social functioning in young adults with 22q11.2 Deletion Syndrome (22q11.2DS).
Method
Childhood predictors of young adult social functioning were examined. Family environment and parental stress in adolescence were investigated as potential mediators between childhood variables and adult social functioning.
Results
Parent rated childhood internalizing symptoms significantly predicted young adult social functioning in 22q11.2DS, even after controlling for concurrent positive symptoms of psychosis, and problem behaviors contributing to parenting stress in adolescence partially mediated this relationship.
Conclusions
These findings highlight child internalizing symptoms and adolescent problem behaviors as potential targets for social functioning interventions in 22q11.2DS.
Keywords: social functioning, 22q11.2 Deletion Syndrome (22q11.2DS), developmental delay, internalizing, longitudinal
Childhood Predictors of Young Adult Social Functioning in 22q11.2 Deletion Syndrome
22q11.2 deletion syndrome (22q11.2DS) is caused by a deletion of approximately 40 genes at region q11.2 of chromosome 22. As the most common microdeletion syndrome, 22q11.2DS has a prevalence of approximately 1 in 1,000–5,950 live births (Botto et al., 2003; Grati et al., 2015). Some of the most characteristic phenotypic traits in 22q11.2DS include cardiac malformations, palatal abnormalities, and facial anomalies (Shprintzen, 2000). An increased risk for psychiatric disorders, including attention deficit / hyperactivity disorder (ADHD), anxiety disorders, mood disorders, autism spectrum disorder (ASD), and schizophrenia has been reported in this population (Antshel et al., 2007; Feinstein, Eliez, Blasey, & Reiss, 2002; Schneider et al., 2014). Notably, about one third of individuals with 22q11.2DS develop schizophrenia, which is much higher than the 0.3 – 0.7% prevalence rate in the general population (American Psychiatric Association, 2013; Drew et al., 2011). Despite the high prevalence of learning disabilities and mild intellectual disability in individuals with 22q11.2DS, the cognitive phenotype for 22q11.2DS consists of both relative strengths and weaknesses. Areas of relative strength include reading decoding, spelling, and rote auditory/verbal memory skills (Antshel, Fremont, & Kates, 2008). In contrast, mathematics, visual/spatial memory, attention and executive functions are areas of relative weakness (Antshel et al., 2008).
Executive Functions
Executive functions are an area of both relative and normative weakness for individuals with 22q11.2DS (Antshel et al., 2008). Using the theoretical framework with the most empirical support (Packwood et al., 2011), we operationalize executive functioning as a multiple component system characterized by separate but related cognitive processes that can be empirically measured using behavioral paradigms (Miyake & Friedman, 2012). This multi-component system includes (a) the ability to maintain and manipulate information from memory (working memory), (b) the ability to suppress impulses (response inhibition), (c) the ability to change behavior in response to new information (cognitive flexibility) and (d) the ability to formulate a strategy to achieve a goal (planning) (Miyake et al., 2000; Pennington & Ozonoff, 1996). These components of executive functioning (working memory, behavioral inhibition, cognitive flexibility, and planning) are necessary for effective social interactions (Altgassen & Kliegel, 2014; Miyake & Friedman, 2012).
Social Functioning
Just as there are a variety of ways to operationalize executive functioning, there are a variety of terms used to define social functioning (Cook & Oliver, 2011). Social functioning domains can include activities of daily living, recreational activities, friendships, intimate relationships, employment or occupation, social behaviors, and independence competency. One definition of social functioning is, “one’s ability to initiate, form and maintain social relationships with others” (e.g., making friends, playing with others on the playground, attending social events with others) (Campbell, McCabe, Melville, Strutt, & Schall, 2015). In contrast, social skills are defined as, “behaviors learned to facilitate awareness of one’s social environment and social contingencies, and to be able to solve social problems” (Gillis & Butler, 2007). Simply having the social skills does not guarantee that the skills will be deployed or lead to successful social relationships.
Social functioning is an important construct to study, yet has received scant attention by 22q11.2DS researchers. This is unfortunate as peer rejection or low acceptance among peers in childhood is related to a wide variety of negative outcomes, both concurrently and prospectively (Bagwell, Newcomb, & Bukowski, 1998; Boivin, Hymel, & Bukowski, 1995; Hodges, Malone, & Perry, 1997; Ladd, Kochenderfer, & Coleman, 1996; Parker & Asher, 1987). More specific to 22q11.2DS, given that poor social functioning in childhood is a predictor of psychosis in adulthood (Lauronen et al., 2007; Yuen, Chow, Silversides, & Bassett, 2013) and individuals with 22q11.2DS are at an increased risk for schizophrenia (Drew et al., 2011), social functioning seems an especially important variable to investigate in the 22q11.2DS population.
Social functioning in 22q11.2DS
Children with 22q11.2DS are significantly more socially inhibited and withdrawn than their peers (Schonherz et al., 2014; Swillen et al., 1997) and demonstrate more problem behaviors (e.g., internalizing behaviors) that interfere with social functioning than their peers (Shashi et al., 2012). Parents of children with 22q11.2DS do not report a delay in early social developmental milestones (Roizen et al., 2007). Instead, social challenges in 22q11.2DS manifest typically in early elementary school as problems with initiating and maintaining peer relationships (Campbell et al., 2011; Heineman-de Boer, Van Haelst, Cordia-de Haan, & Beemer, 1999).
While there are descriptive data on social functioning in youth with 22q11.2DS, to date, there are no longitudinal 22q11.2DS studies examining childhood predictors of social functioning outcomes in adulthood. Three cross-sectional research studies, however, have examined this research question. In each study, cognitive variables (executive functioning, intelligence) or internalizing behaviors were identified as being associated with social functioning. For example, parents of 24 adolescents with 22q11.2DS reported their children experiencing significantly more peer relationship problems compared to parent reports of 27 age-matched typically developing peers (Campbell et al. 2015). In the 22q11.2DS group, (a) working memory, (b) general intelligence, and (c) the ability to understand the emotions of others (emotion attribution) were each negatively associated with peer relationship problems.
Likewise, a cross-sectional study of 100 adults with 22q11.2DS also reported social functioning impairments in adults with 22q11.2DS (Butcher et al., 2012). In this study, a significant positive association between the full-scale IQ and social functioning outcomes was reported. A schizophrenia diagnosis was also a significant predictor of lower social functioning in this cross-sectional sample. Finally, in a cross-sectional study, Shashi et al. (2012) demonstrated that internalizing behaviors are associated with social functioning problems in children with 22q11.2DS.
Although these 3 cross sectional research studies in 22q11.2DS are useful for generating hypotheses, it does not permit the field to move forward in developing efficacious interventions designed to prevent/remediate social functioning impairments in this population.
Current Study Specific Aims / Hypotheses
This project investigates a clinically significant and novel research topic that has clear implications for intervention development and potentially prevention in 22q11.2DS. Given the high rate of schizophrenia in the 22q11.2DS population and the data suggesting that a lack of childhood social relationships are predictive of schizophrenia in the non-22q11.2DS population (Lauronen et al., 2007), prevention efforts could potentially be developed and tested in the 22q11.2DS population based upon any identified childhood predictors. In addition, since social abilities are related to quality of life (Tobin, Drager, & Richardson, 2014), identifying factors related to adult social functioning in 22q11.2DS may provide insight into guiding efforts to improve quality of life.
Considering that no previous studies 22q11.2DS included both self and parent reports, we include both in our study. Likewise, we included both siblings and community controls as comparison groups to (a) examine differences in social development, (b) control for environmental effects (e.g., socioeconomic status, home environment, etc.) shared by siblings, and (c) investigate if predictors in the 22q11.2DS group are specific to the population, as indicated by between group differences in childhood factors predicting social functioning. Our four specific aims and associated hypotheses are:
Specific aim 1: Describe social functioning outcomes in young adults with 22q11.2DS compared to siblings and community controls using both self- and parent-report measures. We hypothesize that young adults with 22q11.2DS will have lower self- and parent-reported social functioning when compared to both siblings and community controls.
Specific aim 2. Examine the relationship between concurrent positive symptoms of psychosis and social functioning in 22q11.2DS. Based upon a previous 22q11.2DS study (Butcher et al., 2012), we hypothesize that there will be a negative correlation between social functioning and positive symptoms of psychosis in young adulthood in 22q11.2DS. Given the very limited number of siblings and community controls expected to have positive symptoms of psychosis, this specific aim will only be considered in the 22q11.2DS group.
Specific aim 3: Identify potential childhood cognitive predictors of young adult social functioning in all three groups (22q11.2DS, siblings, community controls). Full scale IQ (Butcher et al., 2012; Campbell et al., 2015) and working memory (Campbell et al., 2015) was previously noted to be associated with social outcomes in 22q11.2DS cross-sectional studies. In the non-22q11.2DS literature, executive functioning skills including response inhibition, cognitive flexibility, working memory and planning have been documented to be associated with social functioning (Diamantopoulou, Rydell, Thorell, & Bohlin, 2007; Gilotty, Kenworthy, Sirian, Black, & Wagner, 2002; Lepage, Dunkin, Hong, & Reiss, 2013; Rinsky & Hinshaw, 2011; Rocca et al., 2009; Sánchez et al., 2009; Turkstra, Abbeduto, & Meulenbroek, 2014). Accordingly, we hypothesize that childhood Full Scale IQ (Specific Aim 3a) will significantly predict young adult social functioning in 22q11.2DS and executive functioning (Specific Aim 3b) will significantly predict young adult social functioning in all 3 groups.
Specific aim 4: Identify potential childhood behavioral / emotional predictors of young adult social functioning in all three groups (22q11.2DS, siblings, community controls). Factors related to social cognition, including emotion recognition, are associated with social functioning (Extremera & Fernández-Berrocal, 2006). In 22q11.2DS, internalizing behaviors are associated with social functioning (Shashi et al., 2012). In the non- 22q11.2DS literature, both internalizing behaviors (Jacob, Suveg, & Whitehead, 2014; Settipani & Kendall, 2013) and externalizing behaviors (Bongers et al., 2008; Chromik et al., 2015; Diamantopoulou et al., 2007) are associated with social funcitoning. Thus, we hypothesize that childhood emotion recognition, internalizing behaviors and externalizing behaviors will significantly predict young adult social functioning in all three groups.
Exploratory aim 1. For any significant childhood predictors in Specific Aim 3 or 4, we will explore adolescent family environment and parental stress as mediators of the relationship between any significant childhood variables and young adult social functioning in the 22q11.2DS group.
Parents/primary caregivers of youth with 22q11.2DS report three times higher stress levels compared to parents of typically developing children (Briegel, Schneider, & Schwab, 2008). Moreover, non-22q11.2DS research suggests that parental stress is significantly associated with the frequency of problem behaviors displayed by their children (Plant & Sanders, 2007), and negatively predicts the quality of peer-based social interactions in children with developmental delays (Guralnick, Hammond, Connor, & Neville, 2006). Accordingly, we will explore whether parental stress mediates the relationship between childhood variables and social functioning outcomes in young adulthood.
Parents of children with 22q11.2DS also report experiencing marital conflict and having lower than average expectancies for their children for functional independence and academic achievement, thereby requiring more close supervision (Allen et al., 2014; Prinzie et al., 2004). Moreover, family environment can influence social functioning (e.g., modeling how to resolve conflicts) in typically developing adolescents (Youngblade et al., 2007). Accordingly, we will also explore whether family environment mediates the relationship between childhood factors and young adult social functioning in individuals with 22q11.2DS.
Method
Participants
Recruitment
This study consists of a subsample of individuals who participated in a 9-year longitudinal study of risk factors for psychosis in 22q11.2DS. The current sample consists of 53 children with 22q11.2DS, 18 age and gender matched siblings of children with 22q11.2DS and 16 community controls (CC) who were each assessed at four time points (every three years). Participants with a fluorescence in situ hybridization-confirmed deletion of 22q11.2 and their age and gender matched siblings were recruited through local advertisements and from the 22q11.2DS Center at BLINDED FOR REVIEW. Age and gender matched community control participants were recruited from local public schools via advertisements. Neither group of control participants received formal molecular genetic screening, as 22q11.2DS is readily identifiable by a facial phenotype. In all three groups, children with an identifiable genetic disorder (other than 22q11.2DS) or children with an identifiable neurological condition (e.g., traumatic brain injury, pre-term birth) that is known to affect cognitive or psychiatric function were excluded from participation. Given the developmental delays that are associated with 22q11.2DS, no attempt was made to exclude community control participants with ADHD and learning disabilities (LD). Children in the community control group were excluded if they were not instructed in a general education classroom.
Demographics
For the current project, only participants who completed the parent-report outcome measure of social functioning at Time 4 and who also had Time 1 data were included in this study. As shown in Table 1, the 22q11.2DS, sibling, and CC groups did not differ significantly on age at Time 1, F (2, 84) = 1.80, p = .172, age at Time 4 F (2, 84) = 2.22, p = .115, gender distribution X2 (2, N = 87) = 1.51, p = .471, race, X2 (2, N = 86) = 5.95, p = .203, or ethnicity, X2 (2, N = 87) = .828, p = .661.
Table 1.
Sample Demographics
| Variable | 22q11.2DS (n = 53) | Siblings (n = 18) | Community Controls (n = 16) |
|---|---|---|---|
| Sex (% male) | 52.8 | 50.0 | 68.8 |
| T1 Age (years) | 11.9 (2.1) | 12.5 (2.0) | 11.2 (1.6) |
| Range | 8.9 to 16.0 | 9.2 to 15.8 | 8.5 to 15.8 |
| T4 Age (years) | 21.3 (2.2) | 21.9 (1.8) | 20.4 (1.5) |
| Range | 18.1 to 25.9 | 19.0 to 24.5 | 18.9 to 24.7 |
| Race (% percent) | |||
| White | 94.3 | 94.4 | 81.3 |
| Asian | 1.9 | 5.6 | 6.3 |
| American Indian/Alaska Native | 0 | 0 | |
| Black African American | 0 | 0 | |
| More than one race | 1.9 | 12.5 | |
| Unknown | 1.9 | ||
| Ethnicity (% percent) | |||
| Hispanic/Latino | 3.8 | 5.6 | 0 |
| Non-Hispanic/Latino | 96.2 | 94.4 | 100.0 |
Attrition
When comparing our study sample (i.e., participants who had both Time 1 and Time 4 data) to all individuals who participated at Time 1, we found no differences in attrition between the three groups X2 (2, N = 129) = .670, p = .715. Furthermore, participants lost at follow up sometime between Time 1 and Time 4 did not differ from those who followed-up on any relevant Time 1 socio-demographic measures including participant age, gender, and socioeconomic status (p > .05) or any relevant social and cognitive measures, including Time 1 Vineland Socialization scores, Time 1 FSIQ, and Time 1 Verbal IQ (p > .05). Thus, the participants in the current study appear to be representative of the larger study sample.
Young Adult Dependent Measures
Table 2 presents the timeline of when each measure was administered. Participants were assessed at four different time points; however, information from time 3 is not used in the current study.
Table 2.
Measures Used Across Time Points
| Instrument | Time 1 | Time 2 | Time 3 | Time 4 |
|---|---|---|---|---|
| Social Adjustment Scale- Self-Report | x | |||
| Vineland Adaptive Behavior Scales- 2nd edition (VABS-II) | x | x | ||
| Wechsler Intelligence Scale for Children- 3rd edition | x | |||
| Gordon Diagnostic System | x | |||
| Wisconsin Card Sorting Test | x | |||
| Stroop Color-Word Test | x | |||
| California Verbal Learning Test-Children’s version | x | |||
| Visual Span Test | x | |||
| Tower of London | x | |||
| Penn Emotion Recognition- 40 Test | x | |||
| Behavior Assessment System for Children- Parent Rating Scale | x | |||
| Family Environment Scale- 4th Edition | x | |||
| Parenting Stress Index- 3rd Edition | x |
Social Adjustment Scale - Self-Report (Weissman, 1999)
The Social Adjustment Scale - Self-Report (SAS-SR) is a 54-item self-report scale that measures social adjustment over the past two weeks. The SAS-SR identifies six social role areas, including work, social and leisure activities, relationships with extended family, role as a spouse or partner, parental role, and role within the family unit. For the present study, the standard score of Social and Leisure Domain was used as a self-report measure of social functioning, with higher scores indicating more social impairment. The SAS-SR Social and Leisure Domain includes questions such as, “how many friends have you been in contact with in the last 2 weeks” and “how many times in the last 2 weeks have you gone out socially with other people.”
Vineland Adaptive Behavior Scales, Second Edition (Sparrow et al., 2005)
The Vineland Adaptive Behavior Scales- 2nd edition (VABS-II) Parent/Caregiver Rating Form was used in the current study and is a 297-item questionnaire rated on a 3-point scale: 2 (usually), 1 (sometimes or partially), 0 (never). For the present study, only the standard score of the Socialization scale was used as a parent-report of social adaptive functioning, with higher scores indicating better functioning. Low to moderate associations were noted between parent- and self-report of social functioning (22q11.2DS r = −.44, siblings r = −.06, and community controls r = −.42) indicating that they are measuring somewhat different constructs.
Young Adult Predictor Measure
Structured Interview for Prodromal Symptoms (SIPS) (Miller et al., 2003)
The Structured Interview for Prodromal Symptoms (SIPS) is a commonly used structured interview that evaluates current symptoms and clinical risk of psychosis. In the current study, the full SIPS was administered to participants in young adulthood (Time 4), yet due to the conceptual overlap between negative symptoms and social functioning, only the Positive Symptom domain score was used in analyses. Higher scores on the SIPS indicate the presence of more positive symptoms of psychosis.
Childhood Cognitive Predictors
Wechsler Intelligence Scale for Children- 3rd edition (Wechsler, 1991)
The Wechsler Intelligence Scale for Children-3rd edition (WISC-III) FSIQ and Verbal IQ were used to assess general intellectual functioning and language abilities respectively. The Freedom from Distractibility index score (composite of Arithmetic and Digit Span subtests) was used to examine working memory. Construct validity for the Freedom from Distractibility as a measure of both working memory and attention has been adequately demonstrated in various studies (Mayes & Calhoun, 2006; Wechsler, 1991).
Gordon Diagnostic System (Gordon, McClure, & Aylward, 1989)
The Gordon Diagnostic System (GDS) is a continuous performance test (CPT) that objectively measures sustained attention and response inhibition, the latter a subdomain of executive functioning. For the present study, only the standardized commission errors score were used in the analyses.
Tower of London (Shallice, 1982)
The Tower of London (TOL) has demonstrated good construct validity as a measure of planning (Culbertson & Zillmer, 1998). The total number of moves was used in analyses.
Wisconsin Card Sorting Test (Heaton, Chelune, Talley, Kay, & Curtiss, 1993)
The Wisconsin Card Sorting Test (WCST) is a task that measures cognitive flexibility. We used the standard scores for perseverative errors and non-perseverative errors in our analyses.
Stroop Color-Word Test (Golden, 1978)
The Stroop Color-Word Test is a task that measures cognitive flexibility, selective attention and response inhibition. The interference T-score was used in the present study.
California Verbal Learning Test-Children’s version (Delis, Kramer, Kaplan, & Ober, 1994)
The California Verbal Learning Test-Children’s Version (CVLT-C) measures auditory/verbal learning and working memory. Scores for List A Trial 1 (recall after hearing the list once), List A Trial 5 (recall after hearing the list five times), and List B (interference) were used in analyses.
Visual Span Test (Davis, 1998)
The Visual Span Test is a computer-based test that assesses visual working memory abilities. The forward and backward span standardized z-scores were used in the current study.
Childhood Emotional / Behavioral Predictors
Penn Emotion Recognition - 40 Test (Gur et al., 2001)
The Penn Emotion Recognition-40 Test (Penn ER- 40) is a computerized test that assesses the ability to identify facial expressions of emotion. Total number of correct responses was used as a measure of emotion recognition in the current study. The Penn ER-40 demonstrates good test-retest reliability (Weiss et al., 2007) and adequate construct validity when correlated with other measures of social cognition (Pinkham, Penn, Green, & Harvey, 2016).
Behavior Assessment System for Children - Parent Rating Scale (Reynolds & Kamphaus, 1992)
The Behavior Assessment System for Children- Parent Rating Scale (BASC-PRS) is a measure of parent-reported behaviors of children and adolescents. For the present study, based upon our a priori hypotheses, only the Externalizing composite score, Internalizing composite score, and the Social Skills subscale score were used.
Exploratory Aim - Mediational Analyses Measures
Family Environment Scale-4th Edition (Moos & Moos, 1994)
The Family Environment Scale (FES) is a 90-item true/false scale used to assess a parent’s perception of the social environment of their family. For the current study, standard scores on the FES relationship domain subscales (Cohesion, Expressiveness, Conflict) were used, with higher scores indicating higher parent reported emphasis on that construct within the family.
Parenting Stress Index - 3rd Edition (Abidin, 1995)
The Parenting Stress Index–3rd edition (PSI-3) is a parent-report questionnaire designed to measure the amount of parental stress being experienced and to identify areas that are contributing to parental stress. The PSI-3 contains 101-items separated into two domains, parent characteristics and child characteristics. The Child Domain, Parent Domain, and Total Parent Stress composite scores were used as our parenting stress variables.
Procedures
Informed consent and assent was attained from parents and children. At all four time periods, a doctoral-level examiner administered all psychological tests to participants in a quiet room. Parents completed all parent-report rating scales in a separate room.
Planned Analyses
Data inspection
Before conducting analyses for each specific aim, outlier data points were truncated to 3 SDs above/below the group mean of each measure for each of the three groups (22q11.2DS, siblings, community controls) (Costa, 2014; Tabachnick & Fidell, 2007). In our sample, a total of 10 scores were truncated: 4 participants with 22q11.2DS, 3 siblings, and 3 controls. In addition, our data were examined for missing values and all analyses were treated using list-wise deletion (Peugh & Enders, 2004). Finally, considering our small group sample sizes and the likelihood that missing data would reduce statistical power, when conducting regression analyses, mean substitutions were used (Raaijmakers, 1999).
Specific aim 1
A one-way analysis of variance (ANOVA) was used to assess if mean differences existed in social functioning for individuals with 22q11.2DS, siblings and controls in young adulthood. A one-way ANOVA was also conducted using weighted means due to the uneven sample sizes between groups. Lastly, given the prevalence of cognitive delays among individuals with 22q11.2DS, an analysis of covariance (ANCOVA) was used to examine the mean differences in social functioning between groups while controlling for full-scale IQ. Tukey post-hoc tests identified the groups with significant mean differences. Homogeneity of variance was tested using Levene's Test for Equality of Variances for between subject comparisons.
Multicollinearity and Normal Distributions
Before conducting any regression analyses for specific aims 2, 3 and 4, multicollinearity was assessed by examining the correlation matrix between variables. A correlation coefficient of .80 was used as a cutoff (Tabachnick & Fidell, 2007). In addition, multicollinearity diagnostics were also conducted for every regression analysis using variance inflation factor (VIF). As suggested by (Montgomery, 2001) a predictor that has a VIF greater than 5 should be further investigated. Based on the correlation matrix and VIF (included in all regression tables), none of our models demonstrated multicollinearity. In addition, the skewness and kurtosis of Time 4 social functioning was evaluated. Using the criteria of West, Finch, and Curran (1995) all variables were normally distributed.
Specific aim 2
Specific aim 2 was examined in the 22q11.2DS group only. Zero-Inflated Poisson (ZIP) regression analyses (Lambert, 1992) were conducted using the SIPS Positive Symptoms Score to assess the relationship between Time 4 positive symptoms of psychosis and our Time 4 social functioning measures, the VABS-II Socialization and SAS-SR. A Vuong test was significant for both the VABS-II Socialization (z = 2.58, p = .005) and SAS-SR Social and Leisure Activities (z = 2.93, p = .002), indicating that the ZIP regression model was appropriate.
Specific aim 3
A multiple linear regression analysis was conducted separately for each study group to determine if childhood general intelligence (Specific Aim 3a) or childhood executive functioning abilities (Specific Aim 3b) predicted young adult social functioning.
Executive functioning composite scores
As noted in Figure 1, multiple instruments were used to assess response inhibition, cognitive flexibility, and working memory. To reduce the chance of Type I errors, composite scores for each of these 3 subdomains were created by averaging z-scores for each test variable. More specifically, the mean of z-scores for the Gordon Diagnostic System and the Stroop Color-Word Test were used to create an average z-score for response inhibition. Cognitive flexibility was assessed using the average z-score of the Stroop Color-Word Test and the Wisconsin Card Sorting Test. A mean working memory z-score was created using the California Verbal Learning Test, Visual Span Test, and the WISC-III Freedom from Distractibility Composite. By combining data from multiple measures of executive functions into a z-mean score instead of only using one instrument, the variance of non-executive functioning processes is reduced (Snyder et al., 2015). Since we only used the Tower of London scores to assess planning, however, an average z-score was not created for this domain.
Figure 1.
Instruments used to Measure Executive Functions
Covariates
VABS scores at time 1 were entered as a covariate in regression models predicting to parent reported–social functioning (VABS-II) outcomes in adulthood, to account for the potential effects of childhood social functioning. We did not covary for time 1 self-reported social functioning in regression models predicting to Time 4 SAS-SR Social and Leisure Activities scores since we did not collect a self-reported measure of social functioning at Time 1.
Since language skills are related to social functioning (Gillespie-Lynch et al., 2012; Howlin, Moss, Savage, & Rutter, 2013; Liss et al., 2001), Verbal IQ was also entered into the model to account for the variance verbal abilities may have on an individual’s ability to make or maintain relationships with others.
Specific aim 4
Multiple linear regression analyses were conducted separately for each study group to determine if young adult social functioning could be predicted from childhood behavioral functioning or emotion recognition constructs. We again entered social functioning at Time 1 and Verbal IQ as covariates to account for the variance that childhood social functioning and verbal abilities may have on social functioning outcomes in young adulthood, in order to identify what other behavioral/emotional variables may be contributing to parent reported social functioning.
Exploratory aim 1
Based on the significant childhood predictors of young adult social functioning that emerged from analyses in Specific Aims 3 and 4, mediation analyses were conducted to examine if adolescent (Time 2) family environment or parental stress mediated the relationship. To test the proposed indirect effect model suggesting that the association between the identified cognitive, behavioral, or emotional predictors and social functioning may be due, at least in part, to family environment or parenting stress, a mediation approach of bootstrapping the indirect effect was used (Preacher & Hayes, 2004, 2008). Bootstrapping is considered one of the more powerful and valid methods of testing mediation (Williams & MacKinnon, 2008). For these analyses, the SPSS-23 mediation PROCESS macro described in (Hayes, 2013) was used.
Statistical power
Before conducting our analyses, we ran a power analysis using our cognitive regression model with the most variables (Specific Aim 3), an effect size of 0.25 and alpha as 0.05 in G power. Results indicated that our sample size (53 participants) is adequate to achieve .80 statistical power in 22q11.2DS, yet not in the other two groups.
Results
Specific Aim 1
Young adult social functioning group differences
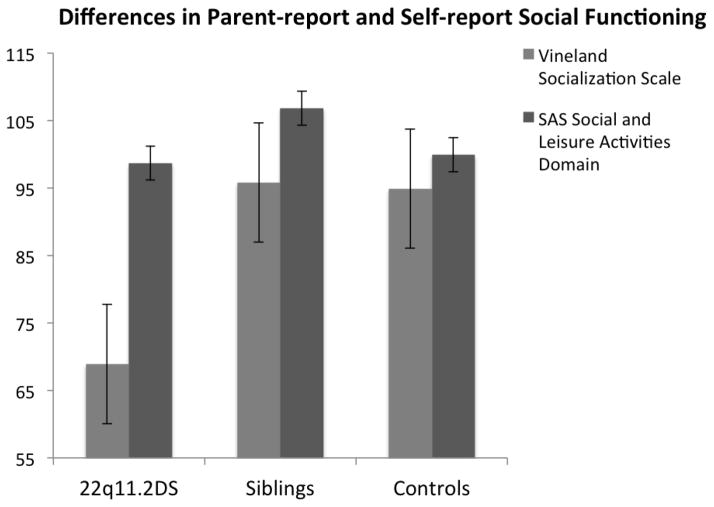
There was a statistically significant difference in the parent-reported VABS-II Socialization scale at Time 4, F(2,84) = 38.2, p < 0.001. Tukey post-hoc tests suggest that parents of participants with 22q11.2DS reported significantly lower social functioning than both the sibling and CC groups. The siblings and CC groups did not differ from each other (See Figure 2).
Figure 2.
Social Functioning Outcome Variables Between Groups
When a one-way ANOVA was conducted using weighted means to control for unequal sample sizes, there was still a statistically significant difference in the parent-reported VABS-II Socialization scale at Time 4 among the three groups, F(2,134) = 57.6, p < 0.001. Likewise, there was still a group effect on parent reported social functioning after controlling for FSIQ, F(2,83) = 8.47, p < 0.001, suggesting that general cognitive abilities do not explain the differences in social functioning as reported by parents.
Conversely, a one-way ANOVA comparing the self-report SAS-SR social and leisure activities across the 22q11.2DS, sibling, and CC groups revealed that there were no significant differences between the three groups (p > .05). Paired samples t-tests were conducted to examine if significant differences existed between parent-report and self-report measures within each group. There was a significant difference between the parent-reported VABS-II Socialization scale and the self-report SAS-SR social and leisure activities domain within the 22q11.2DS group t(50) = −14.623, p = .0001 and sibling group t(16) = −2.442, p = .027, but not the community control group (p > .05).
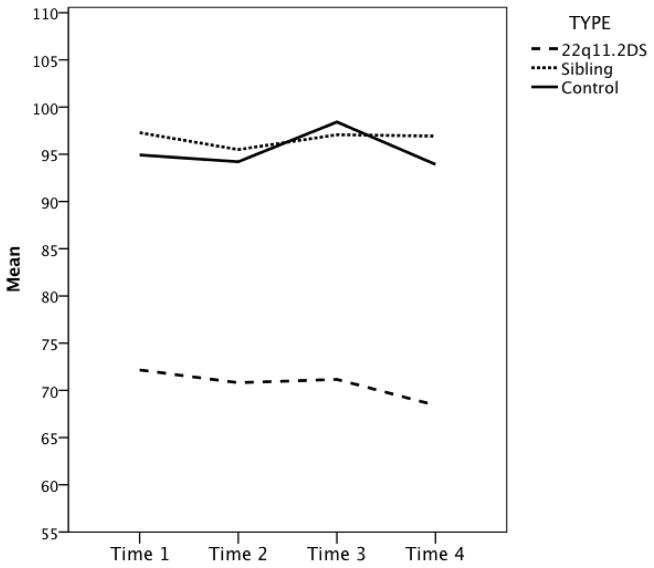
Finally, a repeated measures ANOVA was conducted to examine the effect of time on the parent-reported VABS-II Socialization scale. The interaction between time and group failed to reach statistical significance, F(6, 204) = .339, p = .898 (See Figure 3). There was also no significant effect of time on the parent reports of social functioning, F(3, 204) = .671, p = .553. Thus, parent reported socialization ratings were relatively constant across time in all three groups.
Figure 3.
Vineland Socialization Scale Across Time
Specific Aim 2
Psychosis and social functioning
The ZIP regression conducted for the 22q11.2DS group that examined the association between Time 4 parent-reported VABS-II Socialization ratings and Time 4 SIPS Positive Symptoms Score was significant (z = −4.49, p = .0001). In 22q11.2DS, the model examining if SAS-SR social and leisure activities were associated with SIPS Positive Symptoms Score was also significant (z = 4.27, p = .0001). Thus, from both parent and self-report, higher levels of Time 4 positive psychotic symptoms were associated with lower Time 4 social functioning. Given these relationships, if any significant findings emerge in Specific Aims 3 and 4 in the 22q11.2DS group, the possible role of positive symptoms of psychosis will be considered as a possible explanatory variable for the significant findings.
Specific Aim 3
Childhood cognitive variable group differences
A multivariate analysis of variance (MANOVA) was conducted using childhood cognitive variables. There was a significant multivariate effect, F(26,84) = 4.145, p < .001; Wilk's λ = 0.192, partial η2 = 0.56. As shown in Table 3, univariate results showed significantly lower performance for the 22q11.2DS group than both the sibling group and CC group for most cognitive variables.
Table 3.
Time 1 Cognitive Variable Means
| Variable | 22q11.2DS (n = 53) | Siblings (n = 18) | Community Controls (n = 16) | Significant main effects |
|---|---|---|---|---|
| WISC-III Full Scale IQ Standard score | 69.6 (12.5)*** | 102.7 (16.3) | 98.3 (12.7) | 22q11.2DS < sibling, control |
| WISC-III Freedom From Distractibility Index Standard score | 78.7 (13.2)*** | 100.4 (13.3) | 93.3 (13.4) | 22q11.2DS < sibling, control |
| WISC-III Verbal IQ Standard score | 73.1 (13.6)*** | 100.4 (14.5) | 96.5 (13.6) | 22q11.2DS < sibling, control |
| GDS Commission Errors z-score | −2.9 (5.0)* | 0.0 (1.2) | −2.2 (2.7) | 22q11.2DS < sibling |
| TOL Total moves Raw score | 136.0 (35.6)* | 105.6 (20.1) | 116.3 (22.3) | 22q11.2DS > sibling |
| WCST Perseverative Errors Standard score | 71.4 (15.5)*** | 94.7 (16.5) | 95.9 (17.1) | 22q11.2DS < sibling, control |
| WCST Non-perseverative errors Standard score | 82.3 (15.1) | 89.2 (16.0) | 91.8 (16.2) | None |
| Stroop Interference Score T-score | 47.0 (9.8) | 53.8 (12.2) | 46.8 (7.4) | None |
| CVLT-C List A Trial 1 Score z-score | −0.9 (1.0)** | −0.1 (1.0) | −0.2 (0.6) | 22q11.2DS < sibling, control |
| CVLT-C List A Trial 5 Score z-score | −1.1 (1.3)** | 0.3 (1.2) | 0.0 (0.8) | 22q11.2DS < sibling, control |
| CVLT-C List B Score z-score | −0.7 (1.1) | −0.4 (0.8) | −0.3 (0.8) | None |
| Visual Span Test Forward Span z-score | −0.9 (0.6)*** | 0.4 (0.6) | −0.2 (0.8) | 22q11.2DS < sibling, control |
| Visual Span Test Backward Span z-score | −1.3 (1.0)*** | −0.1 (1.0) | −0.5 (1.3) | 22q11.2DS < sibling, control |
Note. WISC-III = Wechsler Intelligence Scale for Children- 3rd edition, GDS = Gordon Diagnostic System, TOL = The Tower of London, WCST = Wisconsin Card Sorting Test, Stroop = The Stroop Color-Word Test, CVLT-C = California Verbal Learning Test-Children’s version
P < 0.05.
P < 0.01,
P < 0.001.
Specific Aim 3a - Regression analyses of childhood general intelligence
Linear regression analyses examining the relationships between FSIQ and social functioning were conducted for each group separately controlling for Time 1 social functioning in step one. In the 22q11.2DS group, the majority of the variance explained in the model was accounted for in step 1 (Time 1 parent-reported VABS-II Socialization; r2 = .307, F(1,51) = 22.61, p < .0001). Step 2 (Time 1 FSIQ) was not significant after controlling for the effects of Time 1 Vineland Socialization. See Table 4 for 22q11.2DS results.
Table 4.
| General Intelligence Predicting Parent-reported Social Functioning 22q11.2DS
| |||||||
|---|---|---|---|---|---|---|---|
| Variable | β | t | R | R2 | ΔR2 | Sig. | VIF |
| Step 1 | .554 | .307 | .294 | .000* | |||
| Time 1 Vineland Socialization | .554 | 4.76 | .000* | 1.00 | |||
| Step 2 | .558 | .312 | .284 | .569 | |||
| Time 1 Vineland Socialization | .590 | 4.43 | .000* | 1.29 | |||
| FSIQ | −.076 | −.573 | .569 | 1.29 | |||
| Cognitive Predictors of Parent-reported Social Functioning in 22q11.2DS
| |||||||
|---|---|---|---|---|---|---|---|
| Variable | β | t | R | R2 | ΔR2 | Sig. | VIF |
| Step 1 | .554 | .307 | .307 | .000* | |||
| Time 1 Vineland Socialization | .554 | 4.76 | .000* | 1.00 | |||
| Step 2 | .555 | .308 | .001 | .794 | |||
| Time 1 Vineland Socialization | .537 | 3.98 | .000* | 1.32 | |||
| WISC-III Verbal IQ | .035 | .26 | .794 | 1.32 | |||
| Step 3 | .640 | .410 | .102 | .112 | |||
| Time 1 Vineland Socialization | .604 | 4.37 | .000* | 1.49 | |||
| WISC-III Verbal IQ | .206 | 1.36 | .180 | 1.78 | |||
| Working Memory Composite | −.293 | −1.92 | .062 | 1.83 | |||
| Response Inhibition Composite | .000 | .001 | 1.00 | 1.18 | |||
| Cognitive Flexibility Composite | .031 | .218 | .829 | 1.59 | |||
| Planning score | .237 | 2.01 | .050 | 1.09 | |||
Note. WISC-III = Wechsler Intelligence Scale for Children- 3rd edition. FSIQ = Full Scale IQ. VIF = Variance Inflation Factor.
In the sibling group, step 1 (Time 1 parent-reported VABS-II Socialization) was non-significant and the model remained non-significant in Step 2 (FSIQ) p > .05. Lastly, in the CC group, the majority of the variance explained was accounted for in step 1 (Time 1 parent-reported VABS-II Socialization; r2 = .366, F(1,14) = 8.10, p = .013). Step 2 (FSIQ) was not significant after controlling for the effects of Time 1 VABS-II Socialization. Thus, in all 3 groups, childhood FSIQ did not predict young adult social functioning after controlling for Time 1 social functioning.
When Time 4 VABS-II Socialization was used as the outcome variable, but Time 1 social functioning was not included as a covariate, the models for child FSIQ predicting young adult social functioning in the 22q11.2DS group, sibling group, and CC groups were non-significant (p > .05). This suggests that childhood FSIQ does not independently predict social functioning outcomes in young adulthood. Time 1 FSIQ was not significantly correlated with the Time 4 parent-reported socialization scale of the VABS-II for the 22q11.2DS (r = .20), sibling (r = .27) or community control (r = .38) groups.
When the self-reported SAS-SR social and leisure activities domain was used as the outcome variable, the FSIQ models described above were non-significant for all three groups (p > .05).
Specific Aim 3b - Executive functioning composite variables
22q11.2DS group executive functioning
In the 22q11.2DS group, when using the Time 4 parent-reported VABS-II Socialization Scale as the outcome variable, the majority of the variance explained was accounted for in step 1 (Time 1 VABS-II Socialization; r2 = .307, F(1,51) = 22.61, p < .0001). Step 2 (Verbal IQ) and step 3 (Executive Function mean z-score scores) were not significant after controlling for the effects of Time 1 VABS-II Socialization (p > .05). In the 22q11.2DS group, using the self-reported social functioning measure (SAS-SR social and leisure activities domain) as the outcome variable, neither Step 1 (Verbal IQ) nor Step 2 (Executive Function mean z-score scores) were significant predictors of Time 4 self-ratings (p > .05) (See Table 4).
Sibling group executive functioning
In the sibling group, when using Time 4 parent reported VABS-II Socialization as the outcome variable, step 1 (Time 1 VABS-II Socialization), step 2 (Verbal IQ) and step 3 (Executive Function mean z-score scores) were each not significant (p > .05) The regression analysis for siblings including the self-reported SAS-SR social and leisure activities domain as the outcome variable indicated that step one (Verbal IQ) was not significant (p > .05). Step 2 (Executive Function mean z-score scores; r2 = .533, F(4,12) = 3.43, p = .043) was significant. Of the executive functioning variables examined in step 2, only Time 1 planning made a unique contribution to predicting time 4 self-reported SAS-SR social and leisure activities (β = .88, p = .009).
Community control group executive functioning
In the CC group, when using Time 4 parent-reported VABS-II Socialization as the outcome variable, the majority of the variance explained was accounted for in step 1 (Time 1 VABS-II Socialization; r2 = .366, F(1,14) = 8.10, p = .013). Step 2 (Verbal IQ) and step 3 (Executive Function mean z-score scores) were not significant after controlling for the effects of Time 1 VABS-II Socialization (p > .05). Using the self-reported social functioning measure (SAS-SR social and leisure activities domain) as the outcome variable, neither step 1 (Verbal IQ) nor step 2 (Executive Function mean z-score scores) were significant predictors of Time 4 self-ratings (p > .05)
Specific Aim 4
Childhood behavioral / emotional variable group differences
A MANOVA was conducted using childhood behavioral and emotional predictors. There was a significant multivariate effect (F(8,150) = 5.07, p < .001; Wilk's λ = 0.590, partial η2 = .23). As shown in Table 5, univariate results showed significantly lower scores for the 22q11.2DS group than both the sibling group and CC group on the Penn Emotion Recognition Test (F(2,78) = 9.43, p < .001 partial η2 = .20), indicating poorer abilities to accurately recognize emotions in others. Significantly lower scores for the 22q11.2DS group than both the sibling group and CC group was also found on the BASC social skills composite (F(2,78) = 13.13, p < .001, partial η2 = .25), which indicates a lower parent reported frequency of socially skilled behaviors in childhood. On the BASC-PRS Internalizing composite, the 22q11.2DS group had significantly higher scores than both the sibling group and CC group (F(2,78) = 11.25, p < .001, partial η2 = .22), which indicates more parent reported internalizing symptoms in childhood. Lastly, the 22q11.2DS group had significantly higher scores when compared to the CC group, but not the sibling group on the BASC Externalizing composite (F(2,78) = 4.46, p = .015, partial η2 = .10).
Table 5.
Time 1 Emotional and Behavioral Variable Means
| Variable | 22q11.2DS (n = 53) | Siblings (n = 18) | Community Controls (n = 16) | Significant main effects |
|---|---|---|---|---|
| Penn Emotion Recognition Test Raw Score | 31.6 (7.2)*** | 38.3 (2.0) | 37.0 (3.9) | 22q11.2DS < sibling, control |
| BASC-PRS Externalizing Composite T-score | 55.4 (12.3)* | 47.7 (8.0) | 47.3 (8.9) | 22q11.2DS > control |
| BASC-PRS Internalizing Composite T-score | 60.3 (15.2)*** | 43.9 (5.4) | 50.1 (9.3) | 22q11.2DS > sibling, control |
| BASC-PRS Social Skills T-score | 40.7 (9.7)*** | 51.7 (10.4) | 52.3 (8.5) | 22q11.2DS < sibling, control |
Note. BASC-PRS = The Behavior Assessment System for Children-Parent Rating Scale
P < 0.05.
P < 0.001.
Regression analyses of childhood behavioral / emotional variables
22q11.2DS group behavioral/emotional models
In the 22q11.2DS group, when using Time 4 parent-reported VABS-II Socialization as the outcome variable, the majority of the variance explained was accounted for in step 1 (Time 1 VABS-II Socialization; r2 = .307, F(1,51) = 22.61, p < .0001). Step 2 (Verbal IQ) was not significant. Step 3 (Time 1 Behavioral and Emotional scores; r2 = .153, F(4,46) = 3.26, p = .019) made a significant contribution to predicting Time 4 VABS-II Socialization. The overall model accounted for 46.1% of the variance in Time 4 VABS-II Socialization. Of the behavioral/ emotional variables included, only BASC internalizing behaviors (β = −.38, p = .005) significantly predicted young adult social functioning in 22q11.2DS (See Table 6).
Table 6.
Emotional/Behavioral Predictors of Parent-reported Social Functioning in 22q11.2DS
| Variable | β | t | R | R2 | ΔR2 | Sig. | VIF |
|---|---|---|---|---|---|---|---|
| Step 1 | .554 | .307 | .307 | .000* | |||
| Time 1 Vineland Socialization | .554 | 4.76 | .000* | 1.00 | |||
| Step 2 | .555 | .308 | .001 | .794 | |||
| Time 1 Vineland Socialization | .537 | 3.98 | .000* | 1.32 | |||
| WISC-III Verbal IQ | .035 | .26 | .794 | 1.32 | |||
| Step 3 | .679 | .461 | .153 | .019* | |||
| Time 1 Vineland Socialization | .499 | 3.09 | .003* | 2.23 | |||
| WISC-III Verbal IQ | .001 | .01 | .991 | 1.39 | |||
| BASC-PRS Internalizing Behaviors | −.381 | −2.99 | .005* | 1.39 | |||
| BASC-PRS Externalizing Behaviors | −.047 | −.36 | .717 | 1.44 | |||
| BASC-PRS Social Skills | −.064 | −.44 | .666 | 1.82 | |||
| Penn ER-40 | −.099 | −.82 | .417 | 1.24 |
Note. Penn ER-40 = Penn Emotion Recognition- 40 Test, BASC-PRS = Behavior Assessment System for Children- Parent Rating Scale.
P < 0.05.
In the 22q11.2DS group, using the self-reported social functioning measure (SAS-SR social and leisure activities domain) as the outcome variable, neither Step 1 (Verbal IQ) nor Step 2 (Behavioral and Emotional scores) were significant predictors of Time 4 self-ratings (p > .05).
Follow up analyses
Since a significant relationship was previously demonstrated between Time 4 SIPS Positive symptoms and Time 4 VABS-II Socialization (Specific Aim 2), and Time 1 BASC internalizing symptoms seem to be making a significant contribution to Time 4 VABS-II Socialization in the 22q11.2DS group, we sought to further examine the relationship between Time 1 BASC internalizing symptoms and Time 4 SIPS Positive Symptoms. The ZIP regression conducted within the 22q11.2DS group that examined if Time 1 BASC internalizing symptoms predicted Time 4 SIPS Positive Symptoms Score was not significant (z = −1.46, p = .144). Thus, childhood parent reported internalizing symptoms were not a significant predictor of positive symptoms of psychosis in adulthood.
To further understand any contributions of concurrent positive symptoms of psychosis to our longitudinal findings, a second regression analysis was then used to examine the extent to which childhood internalizing symptoms predict young adult social functioning, after controlling for young adult positive symptoms of psychosis. In this stepwise regression, when using Time 4 VABS-II Socialization Scale as the outcome variable, step 1 was significant (Time 1 VABS-II Socialization; r2 = .339, F(1,45) = 23.13, p < .0001). Step 2 (Verbal IQ) was not significant. Step 3 (Time 4 SIPS Positive Symptoms; r2 = .108, F(1,43) = 8.52, p = .006) was significant and step 4 was also significant (Time 1 BASC internalizing symptoms; r2 = .071, F(1,42) = 6.28, p = .016). The overall model accounted for 47.9% of the variance in Time 4 VABS-II Socialization. Therefore, even after controlling for positive symptoms of psychosis at time 4, parent reported childhood internalizing symptoms continue to make a significant contribution to explaining young adult social functioning in the 22q11.2DS group.
Sibling group behavioral/emotional models
In the sibling group, when using the Time 4 parent-reported VABS-II Socialization Scale as the outcome variable, neither step 1 (Time 1 VABS-II Socialization), step 2 (Verbal IQ) nor step 3 (Time 1 Behavioral and Emotional scores) predicted Time 4 parent-ratings (p > .05). When the self-reported SAS-SR was used as the outcome measure, step 1 (Verbal IQ) was not significant (p > .05). Step 2 (Time 1 Behavioral and Emotional scores; r2 = .153, F(4,46) = 3.26, p = .021) made a significant contribution to predicting the Time 4 SAS-SR social and leisure activities domain. Of the behavioral and emotional variables examined, only parent reported BASC social skills in childhood were a significant predictor of Time 4 self-reported social functioning (β = .83, p = .015).
Community control group behavioral/emotional models
In the CC group, when using Time 4 parent-reported VABS-II Socialization Scale as the outcome variable, the majority of the variance explained was accounted for in step 1 (Time 1 VABS-II Socialization; r2 = .366, F(1,14) = 8.10, p = .013). Neither Step 2 (Verbal IQ) nor step 3 (Time 1 Behavioral and Emotional scores) was significant after controlling for the effects of Time 1 VABS-II Socialization (p > .05). When the self-reported SAS-SR social and leisure activities domain was used as the outcome measure, neither step 1 (Verbal IQ) nor step 2 (Time 1 Behavioral and Emotional scores) were significant (p > .05).
Exploratory Aim 1 - Mediation Analyses
Given our significant findings in Specific Aim 4 for the 22q11.2DS group for Time 1 BASC internalizing behaviors, our exploratory aim was investigated for this variable.
Family environment and parent stress group differences
A MANOVA was conducted comparing Time 2 (adolescence) family environment and parenting stress between the three groups. There was a significant multivariate effect (F(12,116) = 3.646, p < .001; Wilk's λ = 0.527, partial η2 = .25). As shown in Table 7, univariate results showed significantly higher scores for the 22q11.2DS group than the CC group, but not the sibling group on PSI Total Parent Stress score (F(2,59) = 6.60, p = .002, partial η2 = .18) and higher scores for the 22q11.2DS group than both the sibling and CC group on the PSI Child score (F(2,59) = 15.81, p < .001, partial η2 = .36). These results indicate that the parents of youth with 22q11.2DS report that their children have problematic behaviors that make parenting stressful. There were no significant differences between groups for the PSI Parent score and all domains of the Family Environment Scale–4th Edition (cohesion, conflict, and expressiveness).
Table 7.
Adolescent Variables used for Mediation Model Means
| Variable | 22q11.2DS (n = 53) | Siblings (n = 18) | Community Controls (n = 16) | Significant main effects |
|---|---|---|---|---|
| Time 2 FES Cohesion Standard score | 52.4 (16.9) | 54.1 (16.3) | 59.2 (6.6) | None |
| Time 2 FES Expressiveness Standard score | 53.2 (12.7) | 53.6 (15.1) | 57.0 (12.2) | None |
| Time 2 FES Conflict Standard score | 47.5 (12.2) | 48.4 (14.4) | 42.8 (9.7) | None |
| Time 2 PSI Total Parent Stress Standard score | 238.0 (39.6)** | 208.3 (43.3) | 195.2 (35.2) | 22q11.2DS > control |
| Time 2 PSI Parent Domain Standard score | 109.9 (22.0) | 113.3 (26.9) | 102.8 (17.8) | None |
| Time 2 PSI Child Domain Standard score | 127.2 (23.3)*** | 94.7 (18.8) | 92.5 (22.1) | 22q11.2DS > sibling, control |
Note. FES = Family Environment Scale-4th Edition, PSI = Parenting Stress Index-3rd Edition
P < 0.01,
P < 0.001.
Mediational analyses
In the 22q11.2DS group, mediation analyses were performed to investigate the hypotheses that various domains of family environment (Time 2 cohesion, expressiveness, conflict) and parenting stressors in adolescence (Time 2 total parent stress, child domain, parent domain) mediate the relationship between Time 1 BASC internalizing behaviors and parent-reported young adult social functioning (Time 4 VABS-II Socialization scale). The indirect effect was tested using a bootstrap estimation approach with 1000 samples.
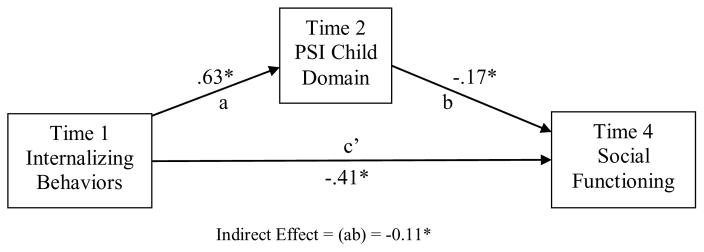
Results showed that parent reported BASC internalizing behaviors were a significant predictor of the PSI child score (β = .63, SE = .23, p = .008) and that the PSI child score approached significance as a predictor of VABS-II Socialization (β = −.17, SE = .09, p = .053). BASC internalizing behaviors were a significant predictor of VABS-II Socialization (β = −.41, SE = .13, p = .004). The indirect coefficient was significant (β = −.11, SE = .09, 95% CI = −.3705, –.0048) (See Figure 4); these results support a partial mediational hypothesis. Therefore, parents of youth with 22q11.2DS report increases in internalizing behaviors in childhood (T1) and increased problematic behaviors that cause parenting stress in adolescence (T2), which in turn lower parent-report social functioning scores in young adulthood (T4).
Figure 4.
Mediation model for Childhood Internalizing Behaviors on Young Adult Parent-reported Social Functioning: (1)
Total Effect (c) and (2) Direct Effect (c’) and Indirect Effect (ab)
Note. *Significant at the 0.05 level
Using the VABS-II Socialization scale as the outcome variable, FES cohesion, FES expressiveness, FES conflict, PSI parent stress, and PSI total stress were not significant mediators. Likewise, there were also no significant mediators in analyses conducted with self-reported SAS-SR social and leisure activities domain as the outcome variable.
Discussion
The present study is, to our knowledge, the first longitudinal study to identify childhood factors that may contribute to poor social functioning outcomes in young adulthood for individuals with 22q11.2DS. In summary, childhood internalizing symptoms prospectively predicted social functioning outcomes in young adulthood in 22q11.2DS, even after controlling for the influences of poor social functioning in childhood, verbal abilities in childhood, and positive symptoms of psychosis in young adulthood. Interestingly, general intelligence and executive functioning in childhood did not significantly predict social functioning outcomes indicating that symptoms of anxiety, depression and somatization in childhood better predict social difficulties in 22q11.2DS in young adulthood. High parenting stress from problematic behaviors displayed by adolescents with 22q11.2DS mediated the relationship between elevated internalizing symptoms in childhood and lower social functioning in young adulthood.
Specific Aim 1: Parent and Child Perceptions of Social Functioning
Overall, parents rated individuals with 22q11.2DS as having more social difficulties than siblings and community controls across all four time points from childhood to young adulthood. This is consistent with previous 22q11.2DS research suggesting that children with 22q11.2DS exhibit poor social functioning when compared to same-age peers (Shashi et al., 2012; Swillen et al., 1997). Parents of participants with 22q11.2DS described their children as having more difficulty with interpersonal relationships, seeking out social activities, and demonstrating proper coping skills in social settings during all developmental periods. Our results are also similar to those reported by Butcher et al. (2012), with both studies reporting that parent reported social functioning in young adults with 22q11.2DS is greater than 2 standard deviations below the mean (< 1st percentile).
Within groups, parent and child report of child social functioning were moderately associated with each other in the 22q11.2DS and community control groups (r’s = −.4 range), yet not related in the sibling group. Despite these moderate relationships in the 22q11.2DS group, individuals with 22q11.2DS reported having statistically comparable social functioning levels with the other two groups. While parent and child reports of child functioning are not collinear (Kolko & Kazdin, 1993), the lack of a self-report group difference (despite significant group differences in parent report) is interesting. Our data suggest that unlike their parents, individuals with 22q11.2DS do not perceive themselves as experiencing social difficulties when compared to their same aged peers.
One possible explanation for the lack of self-report differences between the three groups may be related to cognitive immaturity (Milich, 1994), which has been forwarded as a hypothesis to explain the commonly noted positive self-perceptions that exist in individuals with ADHD (Owens, Goldfine, Evangelista, Hoza, & Kaiser, 2007). Given the cognitive abilities of individuals with 22q11.2DS in our sample (mean FSIQ = 70), and the lack of a significant difference in self-reported social functioning among groups when controlling for FSIQ, the cognitive immaturity hypothesis suggests that developmental delays may explain these findings. Without a developmentally-matched control group, it is not possible to ascertain to what extent this finding is specific to 22q11.2DS. Just as others in the ADHD literature (Swanson, Owens, & Hinshaw, 2012) have encouraged researchers not to consider that parents are correct (and children are incorrect), future research should continue to investigate how parent- and self-report of social functioning in 22q11.2DS are related and how best to understand any differences that may exist between reporters.
Specific Aim 2: Psychosis and Social Functioning in Young Adulthood
Given that approximately one third of individuals with 22q11.2DS develop schizophrenia (Drew et al., 2011) and a prodromal period of social withdrawal and isolation typically precedes the onset of psychotic symptoms in schizophrenia, we examined how symptoms of psychosis were related to the social impairments exhibited in young adults with 22q11.2DS. Within our sample, approximately 48% of individuals with 22q11.2DS endorsed positive symptoms of psychosis, and elevated positive symptoms of psychosis in young adulthood (Time 4) were related to lower parent-report and self-report of social functioning (Time 4). These results supported our hypothesis and are a finding consistent with previous research in 22q11.2DS (Butcher et al., 2012) and schizophrenia literature (Burns & Partick, 2007). The relationship between poor social premorbid adjustment and psychosis has also been identified in 22q11.2DS, both cross-sectionally (Yuen et al., 2013) and, in our sample, longitudinally (Radoeva, Fremont, Antshel, & Kates, 2016).
Specific Aim 3: Childhood Cognitive Predictors of Young Adult Social Functioning
Stability of social functioning
Childhood social functioning was a significant predictor of young adulthood social functioning, when entered into the model as a covariate, for both the 22q11.2DS group and community controls. This suggests that social difficulties begin in childhood and these difficulties remain constant across a 9-year period. Our results are consistent with longitudinal studies in ASD (Howlin et al., 2013), suggesting stability of social difficulties across time. Similarly, our findings support previous 22q11.2DS studies suggesting that social difficulties are already present in elementary school for children with 22q11.2DS (Campbell et al., 2011; Heineman-de Boer et al., 1999). It is possible that peer reputations developed when children begin elementary school (middle childhood) are having a lasting impact on social functioning, a finding noted in typically developing populations (Bagwell et al., 1998; Morison & Masten, 1991). Children with 22q11.2DS are rejected by their peers in childhood (Campbell et al., 2011; Heineman-de Boer et al., 1999) and these problems with interpersonal relationships, social leisure activities and coping with social experiences appear to persist across time.
Unlike the community control and 22q11.2DS groups, childhood social functioning was not a significant predictor of young adult social functioning in siblings. One possible explanation for this finding may be statistical and related to a restricted range of scores in the sibling group. A second possible explanation for this lack of an association between childhood and young adult social functioning relates to having a sibling with 22q11.2DS and the great variability that exists in psychiatric functioning in youth with 22q11.2DS. Via changes in psychiatric functioning in the proband with 22q11.2DS, the sibling’s social development may be less consistent across time. Future research should continue to explore how best to understand our finding that childhood social functioning was not a significant predictor of young adult social functioning in siblings
General intellectual abilities
Childhood full-scale IQ was not a significant predictor of young adult social functioning outcomes in all three groups. This did not support our hypothesis and suggests that global cognitive impairment does not predict social outcomes in individuals with 22q11.2DS. These findings differ from cross sectional studies conducted in 22q11.2DS in which general intelligence was associated with peer relationship problems in adolescence (Campbell et al., 2015) and the VABS Socialization scale in adulthood (Butcher et al., 2012). Our study was the first to examine this relationship longitudinally in 22q11.2DS. While it is possible that general intelligence impacts social functioning cross sectionally at various developmental time points (adolescence, adulthood) in 22q11.2DS, global cognitive impairments in childhood do not predict social functioning impairments in young adulthood. The discrepancy between our findings and previous cross-sectional studies in 22q11.2DS (Butcher et al., 2012; Campbell et al., 2015) may be related to differences in measures used to examine these constructs. Another possible explanation is that when examining this relationship longitudinally, there are other childhood variables specific to 22q11.2DS (e.g., parent reported internalizing symptoms) that better explain social functioning difficulties later in life.
Executive functions
Childhood executive functions (working memory, cognitive flexibility, response inhibition, and planning) did not longitudinally predict young adult social functioning in the 22q11.2DS and community control groups. These findings did not support our hypothesis and were inconsistent with previous cross-sectional 22q11.2DS studies (Campbell et al., 2015), longitudinal studies in ADHD (Diamantopoulou et al., 2007; Rinsky & Hinshaw, 2011) and schizophrenia (Sánchez et al., 2009) and cross-sectional studies in schizophrenia (Rocca et al., 2009), ASD (Gilotty et al., 2002), Turner syndrome (Lepage et al., 2013) and Fragile X syndrome (Turkstra et al., 2014). Unlike the non-significant 22q11.2DS and community control findings, childhood planning abilities was a significant predictor of self-reported social functioning in the sibling group; better planning abilities prospectively predicted higher social functioning. This finding is consistent with those reported by Rinsky and Hinshaw (2011). In their study, planning abilities in childhood longitudinally predicted social functioning in girl adolescents with ADHD. Future research should continue to explore why these predicted associations were not observed in the 22q11.2DS and community control groups.
Our results suggest that within 22q11.2DS, there are other childhood factors that better predict social functioning difficulties in adulthood than executive functions. The lack of a significant longitudinal relationship between executive functions and social functioning outcomes may be related to differences in measures employed in our study compared to previous research. Other possible explanations for these discrepancies include the specificity of executive functioning problems as a function of the disorder examined, with some executive functioning deficits being more related to social abilities than others. However, our results were consistent with cross-sectional studies in adults with schizophrenia (Addington et al., 1998) and ADHD (Biederman et al., 2004; Øie et al., 2011) that found no significant relationship between executive functions and social functioning. Rather than executive skills, within 22q11.2DS, social difficulties already present in childhood better explain social functioning outcomes in adulthood.
Specific Aim 4: Childhood Behavioral/Emotional Predictors of Adult Social Functioning
Internalizing symptoms are prevalent in 22q11.2DS (Jansen et al., 2007; Shashi et al., 2012; Stephenson, Beaton, Weems, Angkustsiri, & Simon, 2015; Wray, Shashi, Schoch, Curtiss, & Hooper, 2013). Our data suggest that not only are these symptoms common, parent reported internalizing symptoms in children with 22q11.2DS also predict parent reported poor social functioning in young adulthood. Even after controlling for poor social functioning already present in childhood, parent reported elevated childhood internalizing symptoms explained problems with interpersonal relationships, social leisure activities and coping with social experiences in young adulthood. The model explained 46.1% of the variance in social functioning for the 22q11.2DS group. Given that this finding was only present within the 22q11.2DS group, the impact of childhood internalizing symptoms to social functioning outcomes may be more specific to 22q11.2DS.
We found that childhood internalizing symptoms (Time 1) were not related to positive symptoms of psychosis in young adulthood (Time 4). These results differ from Gothelf et al. (2007) who indicated that anxiety and depression in childhood longitudinally predicted a schizophrenia diagnosis in adulthood. It is possible that negative symptoms of psychosis are more related to internalizing behaviors and when examining this relationship using only positive symptoms of psychosis this relationship is no longer present. Interestingly, even after controlling for psychosis, childhood internalizing symptoms still significantly explained poor social functioning in young adulthood. Previous work from our group suggested that a composite comprised of parent reported child symptoms of anxiety, depression, somatization, withdrawal and atypicality on the BASC predicted to late adolescent psychosis (Kates et al., 2014). The present results differ, possibly due to (a) the different follow-up periods (late adolescence in previous work, young adulthood in current work) and (b) the inclusion of withdrawal and atypicality symptoms, which may be driving the relationship with psychosis. Future research should continue to investigate how best to predict psychosis in the 22q11.2DS population.
The link between internalizing symptoms and social functioning has been made in previous research in 22q11.2DS, such that internalizing symptoms and problematic social behaviors that interfere with the ability to make and maintain friends in childhood were associated cross-sectionally (Shashi et al., 2012). Our study is the first to identify this relationship longitudinally. Butcher et al. (2012) did not find a significant association between a lifetime history of a mood/anxiety disorder diagnosis and social functioning in adults with 22q11.2DS. One possible explanation of these divergent results is that we measured internalizing symptoms dimensionally while Butcher et al. (2012) used a categorical approach.
It is also possible that this longitudinal relationship emerges because children with 22q11.2DS experience medical and emotional stressors early in life that may contribute to early experiences of anxiety, depression or somatization, and these symptoms influence later social functioning impairments. This is a well-documented finding in non-22q11.2DS research which has indicated that early symptoms of internalizing behaviors related to anxiety and depression in childhood have a negative impact on social outcomes in adolescence (Korhonen et al., 2014) and adulthood (Essau, Lewinsohn, Olaya, & Seeley, 2014; Maughan, Collishaw, & Stringaris, 2013). Internalizing symptoms have also been identified as related to functional outcomes (not specific to social functioning) in 22q11.2DS. In a cross-sectional sample, Angkustsiri et al. (2012) found higher symptoms of anxiety were related to lower adaptive functioning in children with 22q11.2DS. Likewise, in children with 22q11.2DS, a cross-sectional association was found between elevated symptoms of depression and poor adaptive functioning (again, not specific to social functioning) (Fabbro, Rizzi, Schneider, Debbane, & Eliez, 2012).
However, due to the relative variance for which childhood internalizing symptoms alone predict poor social functioning outcomes in young adulthood (15.3% of the variance) in the 22q11.2DS population, it is likely that there are other childhood factors explaining social functioning outcomes that have not yet been considered in 22q11.2DS. For example, constructs specific to the clinical phenotype of individuals with 22q11.2DS, such as facial anomalies and speech and language delays (Shprintzen, 2000) may also be related to impairments in the ability to make and maintain friendships. Since we measured only one aspect of social cognition (emotion recognition), deficits in other domains of social cognition such as theory of mind may also explain poor social functioning outcomes in 22q11.2DS, a finding noted in schizophrenia literature (Green, Horan, & Lee, 2015). While there are likely other factors that explain adult social functioning, our data suggest that internalizing symptoms in childhood are clinically relevant and provide possible avenues for intervention.
Parent-reported social skills did not predict adult social functioning in the 22q11.2DS or community control groups. This is interesting, especially when one considers that social skills training interventions are a widely used intervention to improve social outcomes. Our findings highlight the importance of treating internalizing symptoms in children with 22q11.2DS. This finding suggests that a potential research topic to explore would be the relative efficacy of interventions that include treatment of internalizing symptoms versus those that only target social skills.
Exploratory Aim 1: Child Behaviors Causing Parental Stress in Adolescence
Parents of the 22q11.2DS group reported higher child behavior problems that cause parental stress than both of the control groups and also higher total stress than the community control group. This is consistent with previous literature suggesting that parents of children with 22q11.2DS report three times higher stress levels compared to parents of typically developing children (Briegel et al., 2008). Stress experienced by parents has been linked to the frequency of problem behaviors displayed by children in previous 22q11.2DS studies (Briegel, Schneider, & Schwab, 2007; Briegel et al., 2008).
Our results take this line of research a step further and indicate that parent reported child behavior problems in mid-adolescence contributing to parenting stress (Time 2) were a mediator of the relationship between childhood internalizing symptoms (Time 1) and parent-reported social functioning in young adulthood (Time 4). This suggests that child-related stresses such as child distractibility/hyperactivity, low adaptability, low acceptability, high demandingness, negative mood, and low ability to reinforce parents, may be a mechanism by which internalizing behaviors may negatively impact social outcomes.
According to the transactional model, continuous reciprocal interactions between an individual and their environment are important to social development (Ollendick & Hirshfeld-Becker, 2002; Sameroff, 1995). Therefore, the interpersonal interactions between children with 22q11.2DS and their parents may contribute to the enduring effects of childhood internalizing symptoms and problematic behaviors in adolescence on social functioning later in life. It is possible that evidence based interventions for internalizing symptoms will improve social outcomes in 22q11.2DS by teaching parents how best to respond to child problematic behaviors. For example, training parents in how to emphasize autonomy and reduce reliance upon parents is emphasized in some child anxiety treatment programs (Rapee, Wignall, Spence, Cobham, & Lyneham, 2008). Future studies should examine the extent to which internalizing symptom focused treatments such as the cognitive behavioral therapy (CBT) Coping Cat (Kendall & Hedtke, 2006) delivered in childhood can improve social functioning, both proximally in childhood and distally in adulthood (Beidas, Benjamin, Puleo, Edmunds, & Kendall, 2010). Due to cognitive impairments experienced by individuals with 22q11.2DS, it is quite likely that the CBT will need to be adapted (Fjermestad, Vatne, & Gjone, 2015).
Limitations
Results of the current study should be interpreted in the context of potential limitations. First, due to the discrepancy between parent-report and self-report measures of social functioning, it may be more valid to observe participants in their natural environment using a behavioral measure or sociometric surveys, to assess social functioning of participants with 22q11.2DS relative to their age matched peers. Second, we did not consider the possible influences of social skills training or any previous treatment that may impact social functioning (e.g., CBT, pharmacotherapy) on our results. It remains unknown how many individuals with 22q11.2DS received social skills training or other social functioning-based interventions before participating in the current study. Thus, before concluding that internalizing interventions are more likely than social skills training to have positive yields, future studies should control for the impact of interventions. Third, while our 22q11.2DS analyses were adequately powered and the 22q11.2DS analyses were our primary interest, the sample size of our other two groups is a limitation. Low statistical power may have increased our Type II error rates and hindered the ability for statistically significant effects to be detected in our sibling and community control groups. Also, we did not adjust alpha level when examining the relationship between the childhood variables and young adult social functioning because correcting for multiple comparisons may have masked true statistical significance and increased the likelihood of null findings, which would not have provided useful leads for future studies. However, future studies should consider correcting for alpha level to decrease the risk for Type 1 error within analyses. Lastly, while 22q11.2DS can be readily identifiable by facial features, due to the genetic risk in 22q11.2DS, future studies should consider the use of genetic testing to confirm the absence of a genetic disorder in sibling samples.
Conclusions
In summary, the present study suggests parent reported symptoms of anxiety, depression, and somatization in childhood may have a long-term negative impact on social functioning in young adulthood, and may be mediated by the expression of problem behaviors that cause parental stress in adolescence. These results are important as social functioning was consistently rated as more impaired across developmental periods (Time 1 to 4) for individuals with 22q11.2DS relative to their siblings and age matched peers. This highlights the need for intervention in early childhood in this vulnerable population and suggests that targeting internalizing symptoms and associated parental responses may be a viable research agenda to investigate.
Acknowledgments
Funding: This study was funded by NIH / MH064824 (to Wendy R. Kates).
This research is supported by a grant from the NIH in affiliation with SUNY-Upstate Medical University.
Footnotes
Compliance with Ethical Standards
Ethical Approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent: Informed consent was obtained from all individual participants included in the study.
Conflict of Interest: The authors declare they have no conflicts of interest.
References
- Abidin RR. Parenting Stress Index - 3rd edition. Lutz, FL: Psychological Assessment Resources (PAR) Inc; 1995. [Google Scholar]
- Addington J, McCleary L, Munroe-Blum H. Relationship between cognitive and social dysfunction in schizophrenia. Schizophrenia Research. 1998;34(1–2):59–66. doi: 10.1016/s0920-9964(98)00079-6. [DOI] [PubMed] [Google Scholar]
- Allen TM, Hersh J, Schoch K, Curtiss K, Hooper SR, Shashi V. Association of the family environment with behavioural and cognitive outcomes in children with chromosome 22q11.2 deletion syndrome. J Intellect Disabil Res. 2014;58(1):31–47. doi: 10.1111/jir.12054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5. Washington, DC: 2013. [Google Scholar]
- Angkustsiri K, Leckliter I, Tartaglia N, Beaton EA, Enriquez J, Simon TJ. An examination of the relationship of anxiety and intelligence to adaptive functioning in children with chromosome 22q11.2 deletion syndrome. Journal of Developmental and Behavioral Pediatrics. 2012;33(9):713. doi: 10.1097/DBP.0b013e318272dd24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antshel KM, Aneja A, Strunge L, Peebles J, Fremont WP, Stallone K, … Kates WR. Autistic spectrum disorders in velo-cardio facial syndrome (22q11.2 deletion) Journal of Autism and Developmental Disorders. 2007;37(9):1776–1786. doi: 10.1007/s10803-006-0308-6. [DOI] [PubMed] [Google Scholar]
- Antshel KM, Fremont W, Kates WR. The neurocognitive phenotype in velo-cardio-facial syndrome: a developmental perspective. Developmental Disabilities Research Reviews. 2008;14(1):43–51. doi: 10.1002/ddrr.7. [DOI] [PubMed] [Google Scholar]
- Bagwell CL, Newcomb AF, Bukowski WM. Preadolescent Friendship and Peer Rejection as Predictors of Adult Adjustment. Child Development. 1998;69(1):140–153. doi: 10.1111/j.1467-8624.1998.tb06139.x. [DOI] [PubMed] [Google Scholar]
- Beidas RS, Benjamin CL, Puleo CM, Edmunds JM, Kendall PC. Flexible applications of the Coping Cat program for anxious youth. Cognitive and Behavioral Practice. 2010;17(2):142–153. doi: 10.1016/j.cbpra.2009.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biederman J, Monuteaux MC, Doyle AE, Seidman LJ, Wilens TE, Ferrero F, … Faraone SV. Impact of executive function deficits and attention-deficit/hyperactivity disorder (ADHD) on academic outcomes in children. Journal of Consulting and Clinical Psychology. 2004;72(5):757–766. doi: 10.1037/0022-006X.72.5.757. [DOI] [PubMed] [Google Scholar]
- Boivin M, Hymel S, Bukowski WM. The roles of social withdrawal, peer rejection, and victimization by peers in predicting loneliness and depressed mood in childhood. Development and Psychopathology. 1995;7(4):765–785. doi: 10.1017/S0954579400006830. [DOI] [Google Scholar]
- Bongers IL, Koot HM, van der Ende J, Verhulst FC. Predicting young adult social functioning from developmental trajectories of externalizing behaviour. Psychological Medicine. 2008;38(7):989–999. doi: 10.1017/S0033291707002309. [DOI] [PubMed] [Google Scholar]
- Botto LD, May K, Fernhoff PM, Correa A, Coleman K, Rasmussen SA, … Campbell RM. A population-based study of the 22q11.2 deletion: phenotype, incidence, and contribution to major birth defects in the population. Pediatrics. 2003;112(1):101–107. doi: 10.1542/peds.112.1.101. [DOI] [PubMed] [Google Scholar]
- Briegel W, Schneider M, Schwab KO. 22q11.2 deletion syndrome: behaviour problems of children and adolescents and parental stress. Child Care Health Dev. 2008;34(6):795–800. doi: 10.1111/j.1365-2214.2008.00850.x. [DOI] [PubMed] [Google Scholar]
- Burns T, Partick D. Social functioning as an outcome measure in schizophrenia studies. Acta Psychiatrica Scandinavica. 2007;116(6):403–418. doi: 10.1111/j.1600-0447.2007.01108.x. [DOI] [PubMed] [Google Scholar]
- Butcher NJ, Chow EW, Costain G, Karas D, Ho A, Bassett AS. Functional outcomes of adults with 22q11.2 deletion syndrome. Genetics in Medicine. 2012;14(10):836–843. doi: 10.1038/gim.2012.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell LE, McCabe KL, Melville JL, Strutt PA, Schall U. Social cognition dysfunction in adolescents with 22q11.2 deletion syndrome (velo-cardio-facial syndrome): relationship with executive functioning and social competence/functioning. Journal of Intellectual Disability Research. 2015 doi: 10.1111/jir.12183. [DOI] [PubMed] [Google Scholar]
- Campbell LE, Stevens AF, McCabe K, Cruickshank L, Morris RG, Murphy DGM, Murphy KC. Is theory of mind related to social dysfunction and emotional problems in 22q11.2 deletion syndrome (velo-cardio-facial syndrome)? Journal of Neurodevelopmental Disorders. 2011;3(2):152–161. doi: 10.1007/s11689-011-9082-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chromik LC, Quintin EM, Lepage JF, Hustyi KM, Lightbody AA, Reiss AL. The influence of hyperactivity, impulsivity, and attention problems on social functioning in adolescents and young adults with fragile x syndrome. Journal of Attention Disorders. 2015;1(8) doi: 10.1177/1087054715571739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook F, Oliver C. A review of defining and measuring sociability in children with intellectual disabilities. Research in Developmental Disabilities. 2011;32(1):11–24. doi: 10.1016/j.ridd.2010.09.021. [DOI] [PubMed] [Google Scholar]
- Costa PJ. Truncated outlier filtering. Journal of biopharmaceutical statistics. 2014;24(5):1115–1129. doi: 10.1080/10543406.2014.926366. [DOI] [PubMed] [Google Scholar]
- Culbertson WC, Zillmer EA. The construct validity of the Tower of LondonDX as a measure of the executive functioning of ADHD children. Assessment. 1998;5(3):215. doi: 10.1177/107319119800500302. [DOI] [PubMed] [Google Scholar]
- Davis HR. Colorado assessment tests - Visual Span Test. Boulder, CO: Colorado Assessment Tests; 1998. [Google Scholar]
- Delis D, Kramer JH, Kaplan E, Ober BA. California Verbal Learning Test - Children's Version. San Antonio, TX: The Psychological Corporation; 1994. [Google Scholar]
- Diamantopoulou S, Rydell A, Thorell LB, Bohlin G. Impact of executive functioning and symptoms of attention deficit hyperactivity disorder on children's peer relations and school performance. Developmental Neuropsychology. 2007;32(1):521–542. doi: 10.1080/87565640701360981. [DOI] [PubMed] [Google Scholar]
- Drew LJ, Crabtree GW, Markx S, Stark KL, Chaverneff F, Xu B, … Karayiorgou M. The 22q11.2 microdeletion: Fifteen years of insights into the genetic and neural complexity of psychiatric disorders. International Journal of Developmental Neuroscience. 2011;29(3):259–281. doi: 10.1016/j.ijdevneu.2010.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Essau CA, Lewinsohn PM, Olaya B, Seeley JR. Anxiety disorders in adolescents and psychosocial outcomes at age 30. J Affect Disord. 2014;163:125–132. doi: 10.1016/j.jad.2013.12.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Extremera N, Fernández-Berrocal P. Emotional Intelligence as Predictor of Mental, Social, and Physical Health in University Students. The Spanish Journal of Psychology. 2006;9(1):45–51. doi: 10.1017/s1138741600005965. [DOI] [PubMed] [Google Scholar]
- Fabbro A, Rizzi E, Schneider M, Debbane M, Eliez S. Depression and anxiety disorders in children and adolescents with velo-cardio-facial syndrome (VCFS) Eur Child Adolesc Psychiatry. 2012;21(7):379–385. doi: 10.1007/s00787-012-0273-x. [DOI] [PubMed] [Google Scholar]
- Feinstein C, Eliez S, Blasey C, Reiss AL. Psychiatric disorders and behavioral problems in children with velocardiofacial syndrome: usefulness as phenotypic indicators of schizophrenia risk. Biological Psychiatry. 2002;51(4):312–318. doi: 10.1016/s0006-3223(01)01231-8. [DOI] [PubMed] [Google Scholar]
- Fjermestad KW, Vatne TM, Gjone H. Cognitive behavioral therapy for adolescents with 22q11.2 deletion syndrome. Advances in Mental Health and Intellectual Disabilities. 2015;9(1):30–39. [Google Scholar]
- Gillespie-Lynch K, Sepeta L, Wang Y, Marshall S, Gomez L, Sigman M, Hutman T. Early childhood predictors of the social competence of adults with autism. Journal of Autism and Developmental Disorders. 2012;42(2):161–174. doi: 10.1007/s10803-011-1222-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillis JM, Butler RC. Social skills interventions for preschoolers with autism spectrum disorder: A description of single-subject design studies. Journal of Early and Intensive Behvaior Intervention. 2007;4(3):532–547. [Google Scholar]
- Gilotty L, Kenworthy L, Sirian L, Black DO, Wagner AE. Adaptive skills and executive function in autism spectrum disorders. Child Neuropsychology. 2002;8(4):241–248. doi: 10.1076/chin.8.4.241.13504. [DOI] [PubMed] [Google Scholar]
- Golden JC. Stroop Color and Word Test. Chicago, IL: Stoelting Company; 1978. [Google Scholar]
- Gordon M, McClure FD, Aylward GP. Gordon Diagnostic System. Dewitt, NY: Gordon Diagnostic Systems; 1989. [Google Scholar]
- Gothelf D, Feinstein C, Thompson T, Gu E, Penniman L, Van Stone E, … Reiss AL. Risk Factors for the Emergence of Psychotic Disorders in Adolescents With 22q11.2 Deletion Syndrome. American Journal of Psychiatry. 2007;164(4):663–669. doi: 10.1176/ajp.2007.164.4.663. [DOI] [PubMed] [Google Scholar]
- Grati FR, Molina Gomes D, Ferreira JC, Dupont C, Alesi V, Gouas L, … Vialard F. Prevalence of recurrent pathogenic microdeletions and microduplications in over 9500 pregnancies. Prenat Diagn. 2015 doi: 10.1002/pd.4613. [DOI] [PubMed] [Google Scholar]
- Green MF, Horan WP, Lee J. Social cognition in schizophrenia. Nature Reviews, Neuroscience. 2015;16(10) doi: 10.1038/nrn4005. [DOI] [PubMed] [Google Scholar]
- Gur RC, Ragland JD, Moberg PJ, Turner TH, Bilker WB, Kohler C, … Gur RE. Computerized neurocognitive scanning: I. Methodology and validation in healthy people. Neuropsychopharmacology. 2001;25(5):766–776. doi: 10.1016/S0893-133X(01)00278-0. [DOI] [PubMed] [Google Scholar]
- Guralnick MJ, Hammond MA, Connor RT, Neville B. Stability, Change, and Correlates of the Peer Relationships of Young Children With Mild Developmental Delays. Child Development. 2006;77(2):312–324. doi: 10.1111/j.1467-8624.2006.00872.x. [DOI] [PubMed] [Google Scholar]
- Hayes AF. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. Guilford Press; 2013. [Google Scholar]
- Heaton RK, Chelune GJ, Talley JL, Kay GG, Curtiss G. Wisconsin Card Sorting Test Manual: Revised and expanded. Odessa, FL: Psychological Assessment Resources Inc; 1993. [Google Scholar]
- Heineman-de Boer JA, Van Haelst MJ, Cordia-de Haan M, Beemer FA. Behavior problems and personality aspects of 40 children with velo-cardio-facial syndrome. Genetic Counseling. 1999;10(1):89–93. [PubMed] [Google Scholar]
- Hodges EVE, Malone MJ, Perry DG. Individual Risk and Social Risk as Interacting Determinants of Victimization in the Peer Group. Developmental Psychology. 1997;33(6):1032–1039. doi: 10.1037/0012-1649.33.6.1032. [DOI] [PubMed] [Google Scholar]
- Howlin P, Moss P, Savage S, Rutter M. Social outcomes in mid- to later adulthood among individuals diagnosed with autism and average nonverbal IQ as children. Journal of the American Academy of Child & Adolescent Psychiatry. 2013;52(6):572–581. doi: 10.1016/j.jaac.2013.02.017. [DOI] [PubMed] [Google Scholar]
- Jacob ML, Suveg C, Whitehead MR. Relations between emotional and social functioning in children with anxiety disorders. Child Psychiatry & Human Development. 2014;45:519–532. doi: 10.1007/s10578-013-0421-7. [DOI] [PubMed] [Google Scholar]
- Jansen PW, Duijff Sn, Beemer FA, Vorstman JAS, Klaassen PWJ, Morcus MEJ, Heineman-de Boer JA. Behavioral problems in relation to intelligence in children with 22q11.2 deletion syndrome: a matched control study. American Journal of Medical Genetics. 2007;143(6):574–580. doi: 10.1002/ajmg.a.31623. [DOI] [PubMed] [Google Scholar]
- Kates WR, Russo N, Wood WM, Antshel KM, Faraone SV, Fremont WP. Neurocognitive and familial moderators of psychiatric risk in velocardiofacial (22q11.2 deletion) syndrome: a longitudinal study. Psychol Med. 2014:1–11. doi: 10.1017/S0033291714002724. [DOI] [PubMed] [Google Scholar]
- Kendall PC, Hedtke K. Cognitive-behavioral therapy for anxious children: Therapist manual. Ardmore, PA: Workbook Publishing; 2006. [Google Scholar]
- Kolko DJ, Kazdin AE. Emotional/behavioral problems in clinic and nonclinic children: correspondence among child, parent and teacher reports. Journal of Child Psychology and Psychiatry. 1993;34(6):991–1006. doi: 10.1111/j.1469-7610.1993.tb01103.x. [DOI] [PubMed] [Google Scholar]
- Korhonen M, Luoma I, Salmelin RK, Helminen M, Kaltiala-Heino R, Tamminen T. The trajectories of child's internalizing and externalizing problems, social competence and adolescent self-reported problems in a Finnish normal population sample. School Psychology International. 2014;35(6):561–579. doi: 10.1177/0143034314525511. [DOI] [Google Scholar]
- Ladd GW, Kochenderfer BJ, Coleman CC. Friendship Quality as a Predictor of Young Children's Early School Adjustment. Child Development. 1996;67(3):1103–1118. doi: 10.1111/j.1467-8624.1996.tb01785.x. [DOI] [PubMed] [Google Scholar]
- Lambert D. Zero-inflated Poisson regression, with an application to defects in manufacturing. Technometrics. 1992;34:1–14. [Google Scholar]
- Lauronen E, Miettunen J, Veijola J, Karhu M, Jones PB, Isohanni M. Outcome and its predictors in schizophrenia within the Northern Finland 1966 Birth Cohort. European Psychiatry. 2007;22(2):129–136. doi: 10.1016/j.eurpsy.2006.07.001. [DOI] [PubMed] [Google Scholar]
- Lepage JF, Dunkin B, Hong DS, Reiss AL. Impact of cognitive profile on social functioning in prepubescent females with turner syndrome. Child Neuropsychology. 2013;19(2):161–172. doi: 10.1080/09297049.2011.647900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liss M, Harel B, Fein D, Allen D, Dunn M, Feinstein C, … Rapin I. Predictors and Correlates of Adaptive Functioning in Children with Developmental Disorders. Journal of Autism and Developmental Disorders. 2001;31(2):219–230. doi: 10.1023/A:1010707417274. [DOI] [PubMed] [Google Scholar]
- Maughan B, Collishaw S, Stringaris A. Depression in childhood and adolescence. Journal of the Canadian Academy of Child and Adolescent Psychiatry. 2013;22(1):35. [PMC free article] [PubMed] [Google Scholar]
- Mayes SD, Calhoun SL. WISC-IV and WISC-III Profiles in Children With ADHD. Journal of Attention Disorders. 2006;9(3):486–493. doi: 10.1177/1087054705283616. [DOI] [PubMed] [Google Scholar]
- Milich R. The response of children with ADHD to failure: If at first you don't succeed, do you try, try again? School Psychology Review. 1994;23:11–28. [Google Scholar]
- Miller TJ, McGlashan TH, Rosen JL, Cadenhead K, Ventura J, McFarlane W, … Woods SW. Prodromal Assessment With the Structured Interview for Prodromal Syndromes and the Scale of Prodromal Symptoms: Predictive Validity, Interrater Reliability, and Training to Reliability. Schizophrenia Bulletin. 2003;29(4):703–715. doi: 10.1093/oxfordjournals.schbul.a007040. [DOI] [PubMed] [Google Scholar]
- Miyake A, Friedman NP. The Nature and Organization of Individual Differences in Executive Functions: Four General Conclusions. Current Directions in Psychological Science. 2012;21(1):8–14. doi: 10.1177/0963721411429458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miyake A, Friedman NP, Emerson MJ, Witzki AH, Howerter A, Wager TD. The Unity and Diversity of Executive Functions and Their Contributions to Complex “Frontal Lobe” Tasks: A Latent Variable Analysis. Cognitive Psychology. 2000;41(1):49–100. doi: 10.1006/cogp.1999.0734. http://dx.doi.org/10.1006/cogp.1999.0734. [DOI] [PubMed] [Google Scholar]
- Montgomery DC. Introduction to linear regression analysis. 3. New York: Wiley; 2001. [Google Scholar]
- Moos RH, Moos BS. Family Environment Scale Manual. Consulting Psychologists Press; 1994. [Google Scholar]
- Morison P, Masten AS. Peer Reputation in Middle Childhood as a Predictor of Adaptation in Adolescence: A Seven-Year Follow-up. Child Development. 1991;62(5):991–1007. doi: 10.1111/j.1467-8624.1991.tb01585.x. [DOI] [PubMed] [Google Scholar]
- Ollendick TH, Hirshfeld-Becker DR. The developmental psychopathology of social anxiety disorder. Biological Psychiatry. 2002;51(1):44–58. doi: 10.1016/S0006-3223(01)01305-1. [DOI] [PubMed] [Google Scholar]
- Owens JS, Goldfine ME, Evangelista NM, Hoza B, Kaiser NM. A critical review of self-perceptions and the positive illusory bias in children with ADHD. Clinical Child and Family Psychology Review. 2007;10(4):335–351. doi: 10.1007/s10567-007-0027-3. [DOI] [PubMed] [Google Scholar]
- Packwood S, Hodgetts HM, Tremblay S. A multiperspective approach to the conceptualization of executive functions. Journal of Clinical and Experimental Neuropsychology. 2011;33(4):456–470. doi: 10.1080/13803395.2010.533157. [DOI] [PubMed] [Google Scholar]
- Parker JG, Asher SR. Peer Relations and Later Personal Adjustment: Are Low-Accepted Children At Risk? Psychological Bulletin. 1987;102(3):357–389. doi: 10.1037/0033-2909.102.3.357. [DOI] [PubMed] [Google Scholar]
- Pennington BF, Ozonoff S. Executive functions and developmental psychopathology. J Child Psychol Psychiatry. 1996;37(1):51–87. doi: 10.1111/j.1469-7610.1996.tb01380.x. [DOI] [PubMed] [Google Scholar]
- Peugh JL, Enders CK. Missing data in educational research: A review of reporting practices and suggestions for improvement. Review of Educational Research. 2004;74:525–556. [Google Scholar]
- Pinkham AE, Penn DL, Green MF, Harvey PD. Social cognition psychometric evaluation: Results of the initial psychometric study. Schizophrenia Bulletin. 2016;42(2):494–504. doi: 10.1093/schbul/sbv056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plant KM, Sanders MR. Predictors of care-giver stress in families of preschool-aged children with developmental disabilities. Journal of Intellectual Disability Research. 2007;51(2):109–124. doi: 10.1111/j.1365-2788.2006.00829.x. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior Research Methods, Instruments & Computers. 2004;36:717–731. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in mutliple mediator models. Behavior Research Methods. 2008;40:879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Prinzie P, Swillen A, Maes B, Onghena P, Vogels A, Van Hooste A, … Fryns JP. Parenting, family contexts, and personality characteristics in youngsters with VCFS. Genetic Counseling. 2004;15(2):141–157. [PubMed] [Google Scholar]
- Raaijmakers QAW. Effectiveness of Different Missing Data Treatments in Surveys with Likert-Type Data: Introducing the Relative Mean Substitution Approach. Educational and Psychological Measurement. 1999;59(5):725–748. doi: 10.1177/0013164499595001. [DOI] [Google Scholar]
- Radoeva PD, Fremont W, Antshel KM, Kates WR. Longitudinal study of premorbid adjustment in 22q11.2 deletion (velocardiofacial) syndrome and association with psychosis. Development and Psychopathology. 2016;11:1–14. doi: 10.1017/S0954579416000018. [DOI] [PubMed] [Google Scholar]
- Rapee RM, Wignall A, Spence SH, Cobham V, Lyneham H. Helping your anxious child: a step-by-step guide for parents. 2. Vol. 2. Oakland, CA: New Harbinger Publications; 2008. [Google Scholar]
- Reynolds CR, Kamphaus RW. Behavior Assessment System for Children: Manual. Circle Pines, MN: American Guidance Service, Inc; 1992. [Google Scholar]
- Rinsky JR, Hinshaw SP. Linkages between childhood executive functioning and adolescent social functioning and psychopathology in girls with ADHD. Child Neuropsychology. 2011;17(4):368–390. doi: 10.1080/09297049.2010.544649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rocca P, Montemagni C, Castagna F, Giugiario M, Scalese M, Bogetto F. Relative contribution of antipsychotics, negative symptoms and executive functions to social functioning in stable schizophrenia. Progress in Neuro-Psychopharmacology & Biological Psychiatry. 2009;33(2):373–379. doi: 10.1016/j.pnpbp.2009.01.002. [DOI] [PubMed] [Google Scholar]
- Roizen NJ, Antshel KM, Fremont W, AbdulSabur N, Higgins AM, Shprintzen RJ, Kates WR. 22q11.2DS deletion syndrome: developmental milestones in infants and toddlers. Journal of Developmental and Behavioral Pediatrics. 2007;28(2):119–124. doi: 10.1097/01.DBP.0000267554.96081.12. [DOI] [PubMed] [Google Scholar]
- Sameroff AJ. General systems theories and developmental psychopathology. In: Cicchetti D, Cohen DJ, Cicchetti D, Cohen DJ, editors. Developmental psychopathology, Vol. 1: Theory and methods. Oxford, England: John Wiley & Sons; 1995. pp. 659–695. [Google Scholar]
- Schneider M, Debbane M, Bassett AS, Chow EWC, Fung WLA, van den Bree MBM … Behavior in 22q11.2 Deletion S. Psychiatric Disorders From Childhood to Adulthood in 22q11.2 Deletion Syndrome: Results From the International Consortium on Brain and Behavior in 22q11.2 Deletion Syndrome. American Journal of Psychiatry. 2014;171(6):627–639. doi: 10.1176/appi.ajp.2013.13070864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schonherz Y, Davidov M, Knafo A, Zilkha H, Shoval G, Zalsman G, … Gothelf D. Shyness discriminates between children with 22q11.2 deletion syndrome and williams syndrome and predicts emergence of psychosis in 22q11.2 deletion syndrome. Journal of Neurodevelopmental Disorders. 2014;6:3. doi: 10.1186/1866-1955-6-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Settipani CA, Kendall PC. Social functioning in youth with anxiety disorders: association with anxiety severity and outcomes from cognitive-behavioral therapy. Child Psychiatry & Human Development. 2013;44:1–18. doi: 10.1007/s10578-012-0307-0. [DOI] [PubMed] [Google Scholar]
- Shallice T. Specific impairments of planning. Philosophical Transactions of the Royal Society of London Series B, Biological Sciences. 1982;298(1089):199–209. doi: 10.1098/rstb.1982.0082. [DOI] [PubMed] [Google Scholar]
- Shashi V, Veerapandiyan A, Schoch K, Kwapil T, Keshavan M, Ip E, Hooper S. Social skills and associated psychopathology in children with chromosome 22q11.2 deletion syndrome: Implications for interventions. Journal of Intellectual Disability Research. 2012;56(9):865–878. doi: 10.1111/j.1365-2788.2011.01477.x. [DOI] [PubMed] [Google Scholar]
- Shprintzen RJ. Velo-cardio-facial syndrome: A distinctive behavioral phenotype. Mental Retardation and Developmental Disabilities Research Reviews. 2000;6(2):142–147. doi: 10.1002/1098-2779(2000)6:2<142::AID-MRDD9>3.0.CO;2-H. [DOI] [PubMed] [Google Scholar]
- Snyder HR, Miyake A, Hankin BL. Advancing understanding of executive function impairments and psychopathology: bridging the gap between clinical and cognitive approaches. Frontiers in Psychology. 2015;6(e190):328. doi: 10.3389/fpsyg.2015.00328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sparrow S, Cicchetti DV, Balla DA. Vineland Adaptive Behavior Scales. 2. Circle Pines, MN: American Guidance Service; 2005. [Google Scholar]
- Stephenson DD, Beaton EA, Weems CF, Angkustsiri K, Simon TJ. Identifying patterns of anxiety and depression in children with chromosome 22q11.2 deletion syndrome: comorbidity predicts behavioral difficulties and impaired functional communications. Behavioural brain research. 2015;276:190–198. doi: 10.1016/j.bbr.2014.05.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swanson EN, Owens EB, Hinshaw SP. Is the Positive Illusory Bias Illusory? Examining Discrepant Self-Perceptions of Competence in Girls with ADHD. Journal of Abnormal Child Psychology. 2012;40(6):987–998. doi: 10.1007/s10802-012-9615-x. [DOI] [PubMed] [Google Scholar]
- Swillen A, Devriendt K, Legius E, Eyskens B, Dumoulin M, Gewillig M, Fryns JP. Intelligence and psychosocial adjustment in velocardiofacial syndrome: a study of 37 children and adolescents with VCFS. Journal of Medical Genetics. 1997;34(6):453–458. doi: 10.1136/jmg.34.6.453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tabachnick BG, Fidell LS. Using Multivariate Statistics. 5. Boston, MA: Allyn & Bacon; 2007. [Google Scholar]
- Thorndike RL, Hagen EP, Sattler JM. Stanford-Binet Intelligence Scale: Fourth Edition. Itasca, IL: Riverside Publishing; 1986. [Google Scholar]
- Tobin MC, Drager KDR, Richardson LF. A systematic review of social participation for adults with autism spectrum disorders: Support, social functioning, and quality of life. Research in Autism Spectrum Disorders. 2014;8(3):214–229. [Google Scholar]
- Turkstra LS, Abbeduto L, Meulenbroek P. Social cognition in adolescent girls with fragile x syndrome. Am J Intellect Dev Disabil. 2014;119(4):319–339. doi: 10.1352/1944-7558-119.4.319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler D. Wechsler Intelligence Scale for Children. 3. San Antonio, TX: Psychological Corporation; 1991. [Google Scholar]
- Weiss EM, Stadelmann E, Kohler CG, MBC, Nolan KA, Oberacher H, … Marksteiner J. Differential effect of catechol-o-methyltransferase Val158Met genotype on emotional recognition abilities in healthy men and women. Journal of the International Neuropsychological Society. 2007;13(5):881–887. doi: 10.1017/S1355617707070932. [DOI] [PubMed] [Google Scholar]
- Weissman MM. Social Adjustment Scale- Self-report (SAS-SR) User’s Manual. North Tonawanda, NY: Multi-Health Systems, Inc; 1999. [Google Scholar]
- West SG, Finch JF, Curran PJ. Structural equation models with nonnormal variables: Problems and remedies. 1995. [Google Scholar]
- Williams J, MacKinnon DP. Resampling and Distribution of the Product Methods for Testing Indirect Effects in Complex Models. Structural Equation Modeling: A Multidisciplinary Journal. 2008;15(1):23–51. doi: 10.1080/10705510701758166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wray E, Shashi V, Schoch K, Curtiss K, Hooper SR. Discrepancies in parent and teacher ratings of social-behavioral functioning of children with chromosome 22q11.2 deletion syndrome: implications for assessment. Am J Intellect Dev Disabil. 2013;11(5):339–352. doi: 10.1352/1944-7558-118.5.339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Youngblade LM, Theokas C, Schulenberg J, Curry L, Huang IC, Novak M. Risk and Promotive Factors in Families, Schools, and Communities: A Contextual Model of Positive Youth Development in Adolescence. Pediatrics. 2007;119(Supplement):S47–S53. doi: 10.1542/peds.2006-2089H. [DOI] [PubMed] [Google Scholar]
- Yuen T, Chow EWC, Silversides CK, Bassett AS. Premorbid adjustment and schizophrenia in individuals with 22q11.2 deletion syndrome. Schizophrenia Research. 2013;151(1–3):221–225. doi: 10.1016/j.schres.2013.10.041. [DOI] [PubMed] [Google Scholar]