Abstract
Introduction
Healthy volunteers are crucial for biomedical research. Inadvertent inclusion of subjects with non-alcoholic fatty liver disease (NAFLD) as controls can compromise study validity and subject safety. Given the rising prevalence of NAFLD in the general population, we sought to identify its prevalence and potential impact in volunteers for clinical trials.
Methods
Cross-sectional study of subjects with “Healthy Volunteer” diagnosis between 2011-2015 and no known liver disease. Subjects were defined presumed NAFLD (pNF, ALT≥20 for women or ≥31 for men and BMI>25), healthy non-NAFLD controls (HC, normal ALT and BMI), or indeterminate.
Results
3160 subjects participated as healthy volunteers in 149 clinical trials, (1-29 trials per subject). 1732 (55%) had BMI > 25 kg/m2 and 1382 (44%) had abnormal ALT. pNF was present in 881 subjects (27.9%) and these subjects were older than HC, and had higher triglycerides, LDL-C, and HbA1c and lower HDL-C (p<0.001 for all) . The 149 trials included 101 non-interventional, 33 interventional and 15 vaccine trials. The impact on study validity of recruiting NAFLD subjects as controls was estimated as likely, probable and unlikely in 10, 41 and 98 trials, respectively. The proportion of pNF subjects (28-29%) did not differ by impact. Only 14% of trials used both BMI and ALT for screening. ALT cut-offs for screening were based on local reference values. Grade 3-4 ALT elevations during the study period were rare but more common in pNF subjects than HC (4 vs. 1).
Conclusion
NAFLD is common and often overlooked in volunteers for clinical trials, despite its potential impact on subject safety and validity of study findings. Increased awareness of NAFLD prevalence and stricter ALT cut-offs may ameliorate this problem.
Introduction
Non-alcoholic fatty liver disease (NAFLD) is rapidly becoming the most common chronic liver disorder in the United States(1) with a reported prevalence of 10-46% in studies using different screening tests including laboratory results, hepatic imaging and histopathology(2). The NHANES III data suggests that as much as 23% of the population have unexplained liver enzyme elevations, which, in the absence of other identifiable causes, can be presumed to be NAFLD(3). The rise in NAFLD prevalence mirrors the rise of obesity and metabolic syndrome (MetS)(4). This is supported clinically as patients with NAFLD tend to be overweight or obese(5) and often exhibit additional components of the Metabolic syndrome (MetS) including insulin resistance, dyslipidemia and hypertension(6,7).
The rising prevalence of NAFLD has been described in population studies and in cohorts followed by hepatologists, such as in liver transplant candidates and in donor livers(8). However, NAFLD can also be present in groups of subjects that are not typically seen by hepatologists, where awareness of the disease may be lacking. One such cohort that may be affected by the increasing prevalence of NAFLD is that of healthy volunteers in biomedical research studies. Healthy volunteers play a crucial role in biomedical research and are generally considered healthy if they have no known disease as ascertained by medical history, physical examination and common laboratory tests. If the pool of seemingly healthy volunteers is actually “contaminated” by a prevalent disorder such as NAFLD, this could impact the validity of the clinical research and have consequences related to subject safety.
At the NIH Clinical Center (CC), approximately 2400 healthy volunteers are enrolled annually in clinical trials. These volunteers are recruited through flyers, advertisements, listserv messages and online searches. With the rising prevalence of NAFLD in the general population, we sought to evaluate its prevalence in the CC's pool of seemingly healthy volunteers and estimate its potential impact on the validity and safety of research.
Methods
Patient level data
Retrospective de-identified subject data were retrieved from medical records through the NIH clinical research repository, BTRIS(9). This study was exempted from the need to obtain individual subject consent by the NIH Office of Human Subjects Research Protections.
The study population comprised of adult (age ≥ 18) subjects with a diagnosis of “healthy control volunteer” who had been seen at the CC in a clinical trial between 2011-2015 and had body weight and serum alanine aminotransferase (ALT) measured on the same day during the study period. In total, 11765 subjects were seen as healthy volunteers at the CC during the study period, but only 4174 (36%) had simultaneous ALT and weight measurements and were considered further. Subjects with diagnoses of viral hepatitis or alcohol-related diagnoses were excluded, as well as subjects with positive serologies for HBV, HCV or HIV. Finally, we excluded subjects who did not participate in studies enrolling healthy volunteers during the study period (see below).
The index date for analysis was defined as the first occurrence of simultaneous weight and ALT measurement during the study period. For all subjects we retrieved race, gender and height, as well as additional laboratory data (within 3 months prior to the index date) including liver function tests, lipid panel, and hemoglobin A1c. In addition, we obtained all of the liver enzyme and weight measurements that were collected during the study period.
Normal ALT was defined as <31 U/L for males and <20 U/L for females (10); normal BMI was defined as <25 kg/m2. Subjects were stratified based on their ALT and BMI on the index date as healthy non-NAFLD (normal ALT and BMI), presumed NAFLD (elevated ALT and BMI≥25) and indeterminate (either elevated ALT or overweight). The NAFLD fibrosis score was calculated based on age, hyperglycemia, BMI, platelets, albumin and AST/ALT ratio as previously described (11).
Longitudinal analyses were conducted in subjects who had more than one visit with simultaneous ALT and BMI within the study period. Safety data were analyzed using the Common Terminology Criteria for Adverse Events (CTCAE)(12) using ALT as a surrogate for liver injury, and were limited to subjects with more than one visit. A conservative approach was chosen, using the laboratory upper limit of norm (ULN) for ALT, to minimize overestimation of toxicity. Specifically, grade 1 toxicity was defined as ULN < ALT < 3*ULN, grade 2 as 3-5*ULN, grade 3 as 5-20*ULN and grade 4 as ALT > 20*ULN. Subjects with elevated ALT at baseline were only considered to have an ALT-associated AE if there was a further rise in ALT within 90 days from the prior laboratory measurement that was greater than 35 U/L.
Protocol level data
As subjects may have participated in more than one study, we retrieved all research protocols under which each subject was recruited. For each protocol, we collected inclusion/exclusion criteria, use of liver enzymes and viral hepatitis serology for screening, exclusion of significant alcohol intake, and the description of all research arms. Subjects could have participated in some studies as healthy controls and in others as the diseased target population; as our focus was on the impact of NAFLD on the healthy volunteer population, we excluded studies that did not enroll healthy volunteers in any of their study arms. Some subjects carried a diagnosis of “healthy control volunteer” from participation prior to the study period, but during the study period participated only in trials that did not recruit healthy controls. These subjects were excluded.
Studies were categorized into vaccine trials, studies with pharmacological intervention, non-pharmacological intervention and non-interventional studies. Two authors (AN and VT) independently reviewed the inclusion-exclusion criteria and protocol précis for each study to assess the potential impact of recruiting NAFLD subjects on study validity. The studies were then divided into three groups of unlikely, possible and likely impact on outcomes, based on the research question and type of intervention. For example, a hypothetical study on the metabolism of lipid-lowering medication would be judged as likely impacted by inadvertent enrollment of NAFLD subjects as healthy controls, while a functional MRI study on motor function would be unlikely to be impacted. Any disagreement between the two reviewers was adjudicated in a group discussion including the senior author (YR).
Statistical Analysis
Descriptive statistics are shown as frequencies or described with appropriate measures of central tendency. All inferential analyses between the healthy non-NAFLD and presumed NAFLD groups were performed using parametric techniques, two-sample t-test and χ2 testing, where appropriate.
To quantify the association between ALT and weight, we performed a longitudinal analysis limited to subjects who had ≥3 separate visits during the study period (with a minimum of 4 weeks between visits) with concurrent ALT and BMI measurements. For each individual subject, a correlation coefficient r was calculated between ALT and BMI, and the distribution of individual r-values was compared between subjects according to their presumed NAFLD status. All statistical analysis was performed by SPSS® Statistics (IBM©, Version 21).
To ascertain the potential impact of undiagnosed NAFLD on clinical research protocols, the total number and percentage of presumed NAFLD subjects per protocol were calculated. Additionally, the mean number of studies per presumed NAFLD subject was also calculated. The percentage of clinical protocols that screened using BMI and ALT were also identified.
Results
Study population
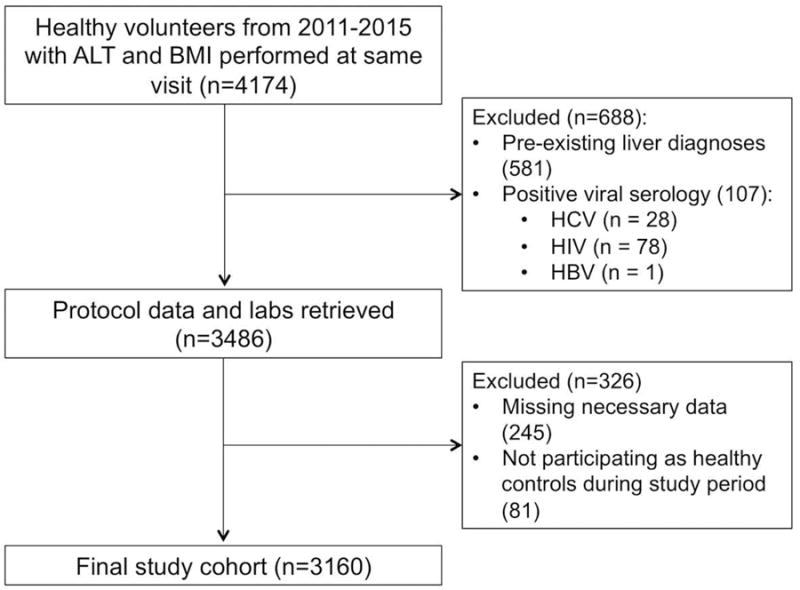
A total of 4174 subjects were enrolled as healthy volunteers in clinical trials at the NIH CC between 2011-2015 with ALT and BMI performed on the same day (Figure 1). 581 subjects were excluded from analysis as they had concomitant diagnoses of chronic liver disease, viral hepatitis, sickle cell disease, hemochromatosis or alcohol-related diseases. Another 107 were excluded for positive serologies for viral hepatitis or HIV and 245 were removed for missing data. Finally, 81 subjects were excluded for not participating as healthy volunteers during the study period. The final study population comprised of 3160 subjects.
Figure 1. Study Population.
The characteristics of the study cohort are listed in Table 1. Males comprised 54% of the subjects and the racial distribution was notable for 36% of African-American descent. 1732 subjects (55%) had BMI≥25 kg/m2 and 741 (23%) were obese (BMI≥30 kg/m2). ALT was elevated in 1382 (44%) of the subjects. There were no significant differences in age and BMI between genders but as expected, ALT was significantly higher for males at a median of 28 U/L (Inter quartile range [IQR] 12-45) compared to females at 19 U/L (8-30) (p<0.001).
Table 1. Characteristics of the Study Cohort.
| Parameter | Total (N=3160) | Male (N=1709) | Female (N=1451) |
|---|---|---|---|
| Agea | 30 (18-86) | 30 (18-76) | 30 (19-86) |
| Race (N,%) | |||
| White | 1558 (49%) | 870 (51%) | 688 (47%) |
| Black | 1130 (36%) | 594 (35%) | 536 (37%) |
| Asian | 232 (7%) | 112 (7%) | 120 (8%) |
| Other | 240 (8%) | 133 (8%) | 107 (7%) |
| BMI (kg/m2)b | 26.9±5.9 | 26.8±4.9 | 27.0±6.8 |
| ALT (U/L)c | 23 (9-37) | 28 (12-44) | 19 (8-30) |
| AST (U/L)c | 19 (10-28) | 21 (12-30) | 17 (11-23) |
Median, range
Mean, standard deviation
Median, IQR
Non-NAFLD and Presumed NAFLD Healthy Volunteers
Using the previously defined classification, we identified 881 (27.9%) subjects with elevated ALT and BMI as presumed NAFLD (pNF), 929 (29.4%) with normal values as healthy non-NAFLD controls (HC) and 1350 (42.7%) as indeterminate. Within the indeterminate group, 850 (26.8%) subjects had BMI≥25 kg/m2 and normal ALT, while 500 (15.8%) had elevated ALT but normal BMI.
There were several significant differences between the pNF and HC cohort (Table 2). The pNF subjects were approximately 9 years older than the HC subjects and as expected, had more metabolic abnormalities including higher total cholesterol, LDL-C and serum triglycerides and lower HDL-C. There was also evidence for moderately increased insulin resistance in the pNF group with a Hemoglobin A1c of 5.6±0.9%. Thus, subjects in the pNF group clearly had the metabolic derangements typical of NAFLD.
Table 2. Characteristics of Presumed NAFLD and Healthy Non-NAFLD subjects.
| Parameter | Healthy (N=929) | Presumed NAFLD (N=881) | P-value |
|---|---|---|---|
| Age (years)a | 26 (18-86) | 35 (19-75) | <0.001 |
| Male Gender (N, %) | 518 (56%) | 516 (59%) | 0.24 |
| Race (N,%) | <0.001 | ||
| White | 502 (54%) | 396 (45%) | |
| Black | 260 (28%) | 372 (42%) | |
| Asian | 100 (11%) | 40 (5%) | |
| Other | 67 (7%) | 73 (8%) | |
| BMI (kg/m2)b | 22.3±1.8 | 31.2±5.6 | <0.001 |
| ALT (U/L)c | 17 (9-25) | 34 (20-48) | <0.001 |
| AST (U/L)c (N=1590) | 17 (11-23) | 22 (11-33) | <0.001 |
| Total Chol. (mg/dL)b (N=943) | 168±32 | 184±40 | <0.001 |
| HDL-C (mg/dL) b (N=940) | 63±17 | 52±16 | <0.001 |
| LDL-C (mg/dL) b (N=940) | 89±27 | 108±34 | <0.001 |
| Serum TG (mg/dL) b (N=940) | 78±38 | 117±77 | <0.001 |
| HbA1c (%)b (N=564) | 5.2±0.4 | 5.6±0.9 | <0.001 |
| Serum Glucose (mg/dL) b (N=1432) | 90±13 | 95±22 | <0.001 |
| Platelets (K/dL) b (N=1750) | 240±53 | 249±61 | <0.001 |
| Albumin (mg/dL) b (N=1331) | 4.4±0.3 | 4.1±0.4 | <0.001 |
| NAFLD Fibrosis Score b (N=1358) | -3.29±0.04 | -2.50±0.04 | <0.001 |
| < -1.455 | 661 (98.1%) | 573 (83.8%) | <0.001 |
| -1.455 – 0.675 | 12 (1.8%) | 105 (15.3%) | |
| > 0.675 | 1 (0.1%) | 6 (0.9%) | |
Total Chol.= Total Cholesterol, HDL-C= High density lipoprotein, LDL-C= Low density lipoprotein, Serum TG: serum triglycerides, HbA1c: Hemoglobin A1c
Median, range
Mean, standard deviation
Median, IQR
Within the indeterminate group, subjects with elevated BMI had an intermediate metabolic phenotype with glucose, HbA1c, cholesterol, LDL-C, HDL-C and triglyceride levels that were worse than HC but better than pNF. These subjects were also older than HC (Supplementary Table 1). Interestingly, subjects with high ALT but normal BMI had, for the most part, metabolic indices that were not different from HC.
To verify that elevated ALT at the index visit was not incidental, we evaluated the persistence of ALT elevation in subjects with more than one visit throughout the study period. In 205 pNF male and 145 pNF females with a median of 3 (range 2-52) visits, elevated ALT persisted in 79% and 81% of subjects, respectively. Furthermore, we calculated the correlation between ALT and BMI among 252 subjects who had ≥3 concurrent ALT and BMI measurements. ALT was positively correlated with BMI in the majority of the 154 pNF subjects (median individual r-value=0.28) and as expected, their r-values were significantly different from 0 (p<0.0001). On the other hand, in the 98 HC correlations did not differ from 0 (median r= 0.09, p=0.56, p=0.04 for the difference between groups) (Figure 2). Thus, in the pNF group ALT is clearly associated with weight.
Figure 2.
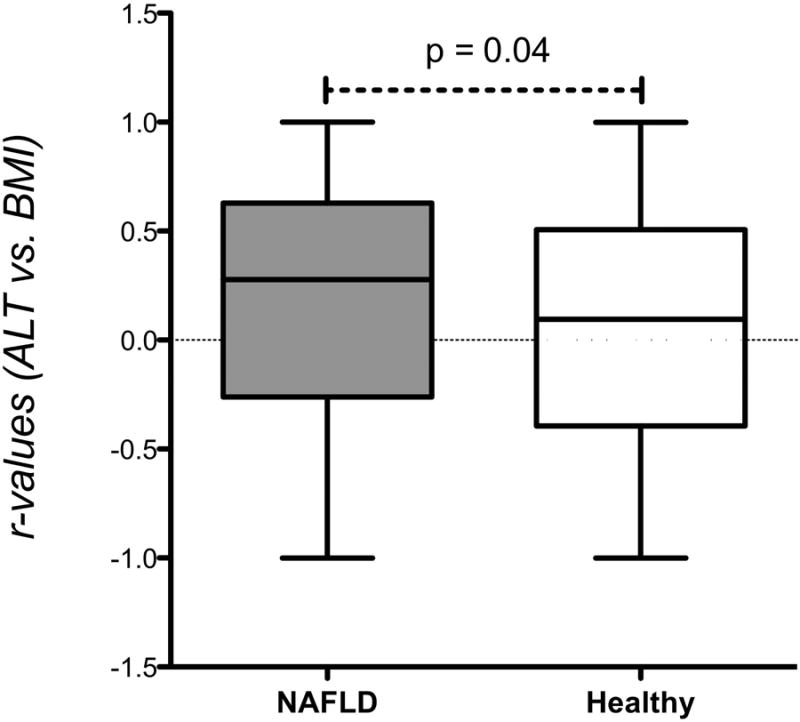
Distribution of individual correlation coefficients (r) for the association of ALT and weight in 252 subjects with at least 3 concurrent measurements (154 with presumed NAFLD and 98 healthy controls). P=0.04 for the difference between groups.
The NAFLD fibrosis score (NFS) was suggested as a non-invasive index to assess disease stage in patients with confirmed NAFLD (11,13). Data for its calculation were available in 684 subjects in the pNF group, of whom only 6 (0.9%) had NSF > 0.675, consistent with advanced fibrosis (Table 2).
Subjects could potentially participate in more than one trial. In fact 42% of the HC and 36% of the pNF subjects participated in 2 or more trials and the range was 1 to 29 trials per subject. The average number of clinical trials was 2.1±2.4 for pNF subjects and 1.9±1.6 for HC (p=0.43).
Clinical Trials and Effect of Presumed NAFLD
A total of 149 clinical trials enrolled healthy volunteers from our study population, and these trials were all reviewed in detail. 101 trials were non-interventional, 10 had a non-pharmacologic intervention, 23 included pharmacological intervention and 15 were vaccine development studies. Presumed NAFLD subjects comprised 31% of subjects enrolled in non-interventional studies, 24% of interventional study subjects and 25% of those enrolled in vaccine trials.
Only 51 of the trials required metabolic evaluation at screening, including baseline lipids and insulin sensitivity, and most were focused on comparing the healthy volunteers to patients with specific metabolic derangements, including diabetes mellitus and dyslipidemia. The primary study question was related to energy metabolism in 27 trials.
For each clinical trial, we reviewed the study précis, research question, inclusion/exclusion criteria and characteristics of non-healthy study groups, if relevant, and assessed the potential impact of inadvertently enrolling a subject with NAFLD as a presumably healthy control. We estimated that there would be no impact on 98 (66%) of the trials, a potential impact on 41 (28%) trials and a likely impact for 10 trials (7%). Examples of likely-impacted trials include studies that investigated the effect of nutritional or pharmacological interventions on lipid metabolism, studies assessing the effects of weight loss on inflammatory markers and studies associating bile acid secretion with energy metabolism. On average the percentage of control patients who met pNF criteria per trial was 29% and this did not differ between trials with predicted unlikely, possible or likely impact (Table 3). Overall, liver enzymes or BMI were evaluated as part of the exclusion criteria in only 26.2% and 25.6% of trials, respectively, and only 14% used both. Exclusion based on liver enzymes or BMI was more likely in trials with potential or likely impact (Table 3), but even within the trials likely to be impacted by enrollment of NAFLD, the utilization of liver enzymes at screening was only 70%. The cutoff value of liver enzymes used as an exclusion criterion was typically defined as 2 or 5 times the upper limit of the norm (ULN), without defining the ULN value. This type of cutoff was used in 36 trials for ALT and 26 trials for AST. Only 3 studies specified numeric cutoffs for ALT, two using an ALT of 41 U/L or AST of 34 U/L and one using an ALT of 80 U/L with no gender differentiation.
Table 3. Characteristics of Trials by Potential Impact of Enrolling NAFLD Subjects as Controls.
| All Trials | Unlikely Impacted Trials | Possibly Impacted Trials | Likely Impacted Trials | |
|---|---|---|---|---|
| Number of Trials | 149 | 98 | 41 | 10 |
| Number of Subjects per Trial (mean, range) | 42 (1-693) | 38 (1-693) | 57 (1-505) | 26 (2-77) |
| Percent pNF Subjects per Trial (mean, range) | 29% (0-100%) | 29% (0-100%) | 29% (0-88%) | 28% (0-50%) |
| Use of Liver Enzymes as Exclusion Criterion (n, %) | 39 (26%) | 24 (25%) | 11 (27%) | 4 (40%) |
| Use of BMI as Exclusion Criterion (n, %) | 38 (26%) | 13 (13%) | 18 (43%) | 7 (70%) |
Effect of Presumed NAFLD on Patient Safety
To determine whether pNF was associated with liver-related adverse events, we assessed subjects' ALT over time. Using the CTCAE criteria for adverse events (AEs), pNF had a total of 15 ALT-based AEs during the study period with three Grade 3-4 ALT elevations (Figure 3). These reflect a median rise in ALT of 59 U/L (range: 37-420) over a median of 15 days (1-74). In comparison, HC had only 4 AEs during this period with only one Grade 3-4 AE (p<0.06 for comparison with pNF) with a median ALT rise of 55 U/L (41-168) over a median of 18 days (7-86). The magnitude and timing of ALT increases that met the AE criteria did not differ between pNF and HC. Only one hepatology consultation was requested during the study period for a pNF subject with ALT elevation from 137 U/L to 177 U/L within a three-week period.
Figure 3.
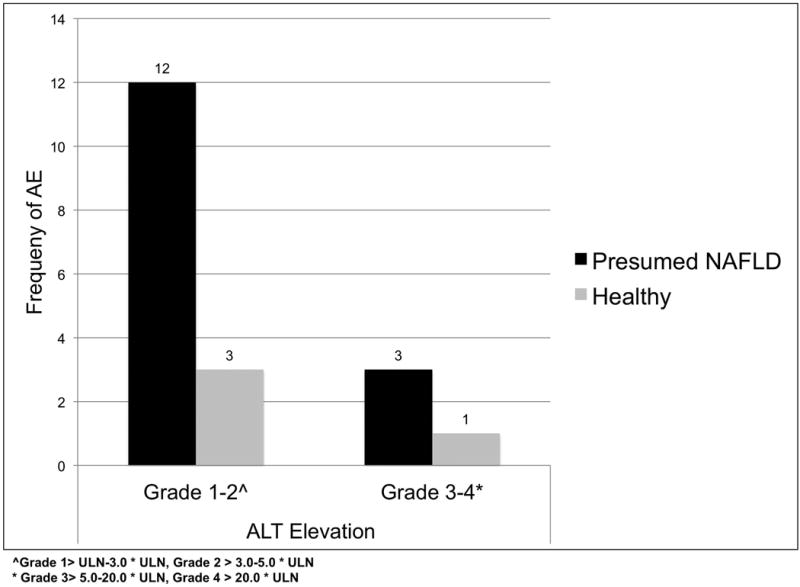
Frequency of Adverse Events (AE) for ALT in Healthy and Presumed NAFLD Volunteers during the study period
Discussion
Over the past 2 decades, the prevalence of obesity and NAFLD has substantially increased in United States(4,14,15). Therefore, it is not surprising that obese subjects are increasingly seen within the pool of volunteers to clinical research(16). In this manuscript we extend this finding by demonstrating that NAFLD as well is very prevalent in this population and is present in at least one-fourth of the subjects enrolled as healthy volunteers in clinical trials at the NIH Clinical Center, over a wide spectrum of trial designs.
Although we did not have radiographic or histologic confirmation of diagnosis, the vast majority of subjects we defined as presumed NAFLD are likely to indeed have an excess accumulation of liver fat for several reasons. First, our study population is reflective of the overall demographics of the Washington Metropolitan area as reported by the US Census(17) and the overall 28% prevalence of presumed NAFLD is in line with reported rates from other US-based population studies(3,4,18). Second, the presumed NAFLD cohort had, as expected from subjects with NAFLD, a significantly worse metabolic profile compared to subjects we classified as truly healthy and to the indeterminate subjects, with higher total cholesterol, higher serum triglycerides, higher LDL-C and lower HDL-C along with evidence of insulin resistance. Third, the majority of subjects demonstrated persistence of ALT elevation upon repeated testing, confirming that they were not diagnosed based on an isolated event, and further supported by an association of ALT with changes in BMI. And fourth, the definition we have used has been acceptable and used in other population studies in the past(19-24). In fact, it is likely that we are underestimating the prevalence of NAFLD in our population, as ALT is not a very sensitive marker. A more sensitive non-imaging based index would be the Fatty Liver Index (FLI) (25,26); however, to calculate the FLI, gamma-glutamyltransferase (GGT) and waist-to-hip circumference (WHC) values are needed, neither of which is routinely performed in the setting of a non-metabolic clinical trial. In fact, in our entire cohort, GGT and WHC together were available for fewer than 30 subjects. Thus, it is likely that most of the subjects we classified as pNF based on elevated enzymes and BMI truly had NAFLD as the underlying cause of their laboratory derangements, though it is possible that others, especially from the high BMI indeterminate group, also had NAFLD. Using the NAFLD fibrosis score, we estimate that the majority of subjects in the pNF group do not have advanced fibrosis, as expected in this cohort of seemingly healthy people.
Recruitment of subjects with NAFLD and obesity as controls in clinical trials can affect study validity in multiple ways. It is well known, and supported by our data, that subjects with NAFLD typically have features of insulin resistance, dyslipidemia and other components of metabolic syndrome. Thus, they would be inappropriate controls for studies assessing these features. Similarly, NAFLD is also inherently associated with alterations in energy metabolism(27) and with atherosclerosis(28,29), suggesting it should be considered when screening subjects to relevant trials.
The expression of hepatic uptake and efflux transporters, as well as that of xenobiotic-metabolizing Cyp450 enzymes is altered in NAFLD and NASH, and resultant alterations in drug disposition have been demonstrated in animal models(30-32) and human studies(33,34). In fact, even obesity by itself can affect drug metabolism and bioavailability(35). Thus, with any trials utilizing a medication or agent that undergoes hepatic metabolism, recruitment of subjects with obesity and/or NAFLD can affect the results.
An additional concern is subject safety. Although animal models suggested increased susceptibility of fatty livers to various noxious stimuli, to date no human study demonstrated increased incidence of drug-induced liver injury (DILI) in subjects with pre-existing NAFLD(28,36). However, if patients with chronic liver diseases like NAFLD do develop DILI, they are likely to have worse outcomes(36-38). We did detect an increased rate of markedly elevated liver enzymes (CTCAE grade 3-4) in subjects with presumed NAFLD, and these typically occurred over a relatively short time period (medians of 14-18 days). These could reflect an association with study interventions but could also be independent of the studies the subjects participated in and reflect other, unrelated causes (i.e. acute infection, alcohol consumption etc). Our study design and the use of deidentified data did not allow for definitive differentiation between the two possibilities; however, the short time frame does suggest an association with study procedures, as we would expect non-study related causes to be spread over a longer time period. Notably, these rises in liver enzymes did not elicit the need for hepatology consultation in most subjects, suggesting the subjects were asymptomatic. Given the inherent limitations, we cannot infer that pNF subjects are at a higher risk for liver injury in clinical trials, but awareness and careful monitoring seem to be warranted.
The ALT cut-off we used in our study is based on the 95th percentile of healthy volunteers with normal BMI, lipids and blood glucose(10), is consistent with recent guidelines from the American College of Gastroenterology(39) and was used by other studies(20). The ULN reported by clinical laboratories is typically higher than this cutoff, varies widely between facilities, is not affected by assay methodology or device, and is dependent predominantly on the selection of “healthy” subjects to define the reference range at each facility(40). ALT levels that are greater than the cut-off we used have been shown to be associated with abnormal metabolic and atherogenic profiles, even when lower than a common laboratory ULN of 40 U/L (41). Approximately one-quarter of the clinical trials we evaluated attempted to avoid recruiting patients with liver disease, typically by using a cutoff of 2-5 times the laboratory ULN for inclusion into studies. Obviously, this has resulted in inadvertent inclusion of a large proportion of subjects with NAFLD. None of the trials have used the strict and gender-specific normal ALT cut-off, suggesting poor awareness on the part of clinical investigators of the impact of the accurate reference range.
The main limitations of our study, as discussed above, are the use of de-identified data without actual chart review and the reliance on indirect measures (anthropomorphic and laboratory) to define NAFLD. In addition, although we have data on racial distribution, ethnicity was not accurately captured in our database, limiting our ability to assess the impact of Hispanic origin in our study population, given the increased prevalence of NAFLD in Hispanic-Americans (4,18). Finally, our study only encompasses healthy volunteers who had simultaneous liver transaminases and BMI measurements and can only be assumed to represent the whole population of healthy volunteers.
Overall, the significance of this study is to increase awareness and vigilance among clinical researchers. Subjects with NAFLD should be included in trials that aim to reflect the general population, both for practical purposes (given the high prevalence of NAFLD) and for generalizability. However, strictly speaking, these subjects should not be considered “healthy” and are inappropriate controls for trials assessing metabolic pathways or drugs and devices that could be affected by hepatic dysfunction or NAFLD. Our data is not necessarily aimed at investigators designing a trial with NAFLD as the research question, as hepatologists are likely to be aware of the high prevalence of NAFLD, the proper liver enzyme cut-offs, the poor sensitivity of ALT, and the potential impact of NAFLD. Non-hepatologists on the other hand, are far less aware of the disease and its features, and tend to erroneously rely on marked elevations in liver enzymes as a trigger for evaluation and referral (42,43). Increasing awareness among the broad community of non-hepatologist clinical investigators to the stricter ALT thresholds is crucial in this regard.
In conclusion, NAFLD is a common and an often-overlooked disease in subjects recruited as healthy control volunteers to clinical trials. Use of a strict ALT cut-off of 19 U/L in females and 30 U/L in males may help overcome concerns for the presence of NAFLD in seemingly healthy controls and improve research validity.
Supplementary Material
Acknowledgments
Funding: The Intramural Research Program of the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK)
Abbreviations
- NAFLD
non-alcoholic fatty liver disease
- NASH
non-alcoholic steatohepatitis
- MetS
metabolic syndrome
- NHANES
National Health and Nutrition Examination Survey
- NIH
National Institutes of Health
- CC
Clinical Center
- BMI
body mass index
- BTRIS
Biomedical Translational Research Information System
- ALT
alanine aminotransferase
- AST
aspartate aminotransferase
- HBV
hepatitis B virus
- HCV
hepatitis C virus
- HIV
human immunodeficiency virus
- pNF
presumed non-alcoholic fatty liver disease
- HC
healthy controls
- MRS
magnetic resonance spectroscopy
- ULN
upper limit of the norm
Footnotes
Authors' Contributions: Study concept and design: Rotman, Takyar
Acquisition of data: Takyar, Beri, Nath, Rotman, Gharib
Analysis and interpretation of data: Takyar, Nath, Rotman
Drafting of the manuscript: Takyar, Nath, Rotman
Critical revision of the manuscript for important intellectual content: Takyar, Rotman, Gharib
Statistical Analysis: Takyar, Rotman
Study supervision: Rotman
Guarantor of Data: Rotman
Conflicts of interest: None of the authors has any financial interest or conflict of interest related to this research.
References
- 1.Chalasani N, Younossi Z, Lavine JE, et al. The diagnosis and management of non-alcoholic fatty liver disease: practice guideline by the American Gastroenterological Association, American Association for the Study of Liver Diseases, and American College of Gastroenterology. Gastroenterology. 2012;142:1592–609. doi: 10.1053/j.gastro.2012.04.001. [DOI] [PubMed] [Google Scholar]
- 2.Vernon G, Baranova A, Younossi ZM. Systematic review: the epidemiology and natural history of non-alcoholic fatty liver disease and non-alcoholic steatohepatitis in adults. Alimentary pharmacology & therapeutics. 2011;34:274–85. doi: 10.1111/j.1365-2036.2011.04724.x. [DOI] [PubMed] [Google Scholar]
- 3.Lazo M, Hernaez R, Eberhardt MS, et al. Prevalence of nonalcoholic fatty liver disease in the United States: the Third National Health and Nutrition Examination Survey, 1988-1994. American journal of epidemiology. 2013;178:38–45. doi: 10.1093/aje/kws448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Williams CD, Stengel J, Asike MI, et al. Prevalence of nonalcoholic fatty liver disease and nonalcoholic steatohepatitis among a largely middle-aged population utilizing ultrasound and liver biopsy: a prospective study. Gastroenterology. 2011;140:124–31. doi: 10.1053/j.gastro.2010.09.038. [DOI] [PubMed] [Google Scholar]
- 5.Ruhl CE, Everhart JE. Determinants of the association of overweight with elevated serum alanine aminotransferase activity in the United States. Gastroenterology. 2003;124:71–9. doi: 10.1053/gast.2003.50004. [DOI] [PubMed] [Google Scholar]
- 6.Chan WK, Tan AT, Vethakkan SR, Tah PC, Vijayananthan A, Goh KL. Non-alcoholic fatty liver disease in diabetics--prevalence and predictive factors in a multiracial hospital clinic population in Malaysia. Journal of gastroenterology and hepatology. 2013;28:1375–83. doi: 10.1111/jgh.12204. [DOI] [PubMed] [Google Scholar]
- 7.Portillo Sanchez P, Bril F, Maximos M, et al. High Prevalence of Nonalcoholic Fatty Liver Disease in Patients with Type 2 Diabetes Mellitus and Normal Plasma Aminotransferase Levels. The Journal of clinical endocrinology and metabolism. 2014 doi: 10.1210/jc.2014-2739. [DOI] [PubMed] [Google Scholar]
- 8.Marcos A, Fisher RA, Ham JM, et al. Selection and outcome of living donors for adult to adult right lobe transplantation. Transplantation. 2000;69:2410–5. doi: 10.1097/00007890-200006150-00034. [DOI] [PubMed] [Google Scholar]
- 9.Cimino JJ, Ayres EJ, Remennik L, et al. The National Institutes of Health's Biomedical Translational Research Information System (BTRIS): design, contents, functionality and experience to date. Journal of biomedical informatics. 2014;52:11–27. doi: 10.1016/j.jbi.2013.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Prati D, Taioli E, Zanella A, et al. Updated definitions of healthy ranges for serum alanine aminotransferase levels. Annals of internal medicine. 2002;137:1–10. doi: 10.7326/0003-4819-137-1-200207020-00006. [DOI] [PubMed] [Google Scholar]
- 11.Angulo P, Hui JM, Marchesini G, et al. The NAFLD fibrosis score: a noninvasive system that identifies liver fibrosis in patients with NAFLD. Hepatology. 2007;45:846–54. doi: 10.1002/hep.21496. [DOI] [PubMed] [Google Scholar]
- 12.NCI. Common Terminology Criteria for Adverse Events (CTCAE) National Cancer Institute; 2010. https://evs.nci.nih.gov/ftp1/CTCAE/CTCAE_4.03_2010-06-14_QuickReference_5×7.pdf: [Google Scholar]
- 13.Musso G, Gambino R, Cassader M, Pagano G. Meta-analysis: natural history of non-alcoholic fatty liver disease (NAFLD) and diagnostic accuracy of non-invasive tests for liver disease severity. Ann Med. 2011;43:617–49. doi: 10.3109/07853890.2010.518623. [DOI] [PubMed] [Google Scholar]
- 14.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999-2010. Jama. 2012;307:491–7. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- 15.Li C, Ford ES, McGuire LC, Mokdad AH. Increasing trends in waist circumference and abdominal obesity among US adults. Obesity. 2007;15:216–24. doi: 10.1038/oby.2007.505. [DOI] [PubMed] [Google Scholar]
- 16.Courville AB, DiVito M, Moyer L, et al. Increase in body mass index from normal weight to overweight in a cross-sectional sample of healthy research volunteers. Nutrition research. 2014;34:1052–7. doi: 10.1016/j.nutres.2014.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bureau USC. American Community Survey 1-year estimates- Census Reporter Profile page for Washington-Arlington-Alexandria, DC-VA-MD-WV Metro Area. 2014: US Federal Government. 2014 [Google Scholar]
- 18.Browning JD, Szczepaniak LS, Dobbins R, et al. Prevalence of hepatic steatosis in an urban population in the United States: impact of ethnicity. Hepatology. 2004;40:1387–95. doi: 10.1002/hep.20466. [DOI] [PubMed] [Google Scholar]
- 19.Younossi ZM, Stepanova M, Afendy M, et al. Changes in the prevalence of the most common causes of chronic liver diseases in the United States from 1988 to 2008. Clin Gastroenterol Hepatol. 2011;9:524–530 e1. doi: 10.1016/j.cgh.2011.03.020. quiz e60. [DOI] [PubMed] [Google Scholar]
- 20.Dunn W, Xu R, Wingard DL, et al. Suspected nonalcoholic fatty liver disease and mortality risk in a population-based cohort study. The American journal of gastroenterology. 2008;103:2263–71. doi: 10.1111/j.1572-0241.2008.02034.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pendino GM, Mariano A, Surace P, et al. Prevalence and etiology of altered liver tests: a population-based survey in a Mediterranean town. Hepatology. 2005;41:1151–9. doi: 10.1002/hep.20689. [DOI] [PubMed] [Google Scholar]
- 22.Suzuki A, Angulo P, Lymp J, et al. Chronological development of elevated aminotransferases in a nonalcoholic population. Hepatology. 2005;41:64–71. doi: 10.1002/hep.20543. [DOI] [PubMed] [Google Scholar]
- 23.Kotronen A, Yki-Jarvinen H, Mannisto S, et al. Non-alcoholic and alcoholic fatty liver disease - two diseases of affluence associated with the metabolic syndrome and type 2 diabetes: the FIN-D2D survey. BMC Public Health. 2010;10:237. doi: 10.1186/1471-2458-10-237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dunn W, Xu R, Schwimmer JB. Modest wine drinking and decreased prevalence of suspected nonalcoholic fatty liver disease. Hepatology. 2008;47:1947–54. doi: 10.1002/hep.22292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bedogni G, Bellentani S, Miglioli L, et al. The Fatty Liver Index: a simple and accurate predictor of hepatic steatosis in the general population. BMC Gastroenterol. 2006;6:33. doi: 10.1186/1471-230X-6-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ruhl CE, Everhart JE. Fatty liver indices in the multiethnic United States National Health and Nutrition Examination Survey. Alimentary pharmacology & therapeutics. 2015;41:65–76. doi: 10.1111/apt.13012. [DOI] [PubMed] [Google Scholar]
- 27.Koliaki C, Roden M. Do mitochondria care about insulin resistance? Mol Metab. 2014;3:351–3. doi: 10.1016/j.molmet.2014.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pais R, Giral P, Khan JF, et al. Fatty liver is an independent predictor of early carotid atherosclerosis. Journal of hepatology. 2016;65:95–102. doi: 10.1016/j.jhep.2016.02.023. [DOI] [PubMed] [Google Scholar]
- 29.Zeb I, Li D, Budoff MJ, et al. Nonalcoholic Fatty Liver Disease and Incident Cardiac Events: The Multi-Ethnic Study of Atherosclerosis. J Am Coll Cardiol. 2016;67:1965–6. doi: 10.1016/j.jacc.2016.01.070. [DOI] [PubMed] [Google Scholar]
- 30.Buechler C, Weiss TS. Does hepatic steatosis affect drug metabolizing enzymes in the liver? Current drug metabolism. 2011;12:24–34. doi: 10.2174/138920011794520035. [DOI] [PubMed] [Google Scholar]
- 31.Li P, Robertson TA, Thorling CA, et al. Hepatic pharmacokinetics of cationic drugs in a high-fat emulsion-induced rat model of nonalcoholic steatohepatitis. Drug metabolism and disposition: the biological fate of chemicals. 2011;39:571–9. doi: 10.1124/dmd.110.036806. [DOI] [PubMed] [Google Scholar]
- 32.Canet MJ, Cherrington NJ. Drug disposition alterations in liver disease: extrahepatic effects in cholestasis and nonalcoholic steatohepatitis. Expert Opin Drug Metab Toxicol. 2014;10:1209–19. doi: 10.1517/17425255.2014.936378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Barshop NJ, Capparelli EV, Sirlin CB, Schwimmer JB, Lavine JE. Acetaminophen pharmacokinetics in children with nonalcoholic fatty liver disease. J Pediatr Gastroenterol Nutr. 2011;52:198–202. doi: 10.1097/MPG.0b013e3181f9b3a0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ferslew BC, Johnston CK, Tsakalozou E, et al. Altered morphine glucuronide and bile acid disposition in patients with nonalcoholic steatohepatitis. Clin Pharmacol Ther. 2015;97:419–27. doi: 10.1002/cpt.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Brill MJ, Diepstraten J, van Rongen A, van Kralingen S, van den Anker JN, Knibbe CA. Impact of obesity on drug metabolism and elimination in adults and children. Clinical pharmacokinetics. 2012;51:277–304. doi: 10.2165/11599410-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 36.Chalasani N, Bonkovsky HL, Fontana R, et al. Features and Outcomes of 899 Patients With Drug-Induced Liver Injury: The DILIN Prospective Study. Gastroenterology. 2015;148:1340–52 e7. doi: 10.1053/j.gastro.2015.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kaplowitz N, DeLeve L. Drug-Induced Liver Disease- Risk Factors for Drug-Induced Liver Disease. 3. Philadelphia: Lippincott Williams & Wilkins; 1999. [Google Scholar]
- 38.FDA. Guidance for Industry- Drug-Induced liver injury: Premarketing Clinical Evaluation. US Federal Government. 2009:2. [Google Scholar]
- 39.Kwo PY, Cohen SM, Lim JK. ACG Clinical Guideline: Evaluation of Abnormal Liver Chemistries. The American journal of gastroenterology. 2017;112:18–35. doi: 10.1038/ajg.2016.517. [DOI] [PubMed] [Google Scholar]
- 40.Dutta A, Saha C, Johnson CS, Chalasani N. Variability in the upper limit of normal for serum alanine aminotransferase levels: a statewide study. Hepatology. 2009;50:1957–62. doi: 10.1002/hep.23200. [DOI] [PubMed] [Google Scholar]
- 41.Siddiqui MS, Sterling RK, Luketic VA, et al. Association between high-normal levels of alanine aminotransferase and risk factors for atherogenesis. Gastroenterology. 2013;145:1271–9. e1–3. doi: 10.1053/j.gastro.2013.08.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Blais P, Husain N, Kramer JR, Kowalkowski M, El-Serag H, Kanwal F. Nonalcoholic fatty liver disease is underrecognized in the primary care setting. The American journal of gastroenterology. 2015;110:10–4. doi: 10.1038/ajg.2014.134. [DOI] [PubMed] [Google Scholar]
- 43.Armstrong MJ, Houlihan DD, Newsome PN. NAFLD is underrecognized in the primary care setting: UK experience. The American journal of gastroenterology. 2014;109:1500–1. doi: 10.1038/ajg.2014.207. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


