THE CASE: A 45-year-old right-handed man was admitted to hospital for evaluation of seizures that had begun when he was 10 years old but were not responding to treatment. The events were characterized by an initial butterfly sensation in his stomach, sometimes associated with a bad taste in his mouth, déjà vu and a diffuse tingling sensation lasting less than 30 seconds. About half the time, these symptoms would progress to loss of awareness, during which he would stare, smack his lips, drool, rub his leg with his right hand and flex his left arm in a rigid dystonic posture. These spells occurred 2 to 10 times a month and were more frequent during times of stress. The seizures were never completely controlled despite the use of numerous antiseizure medications, including phenytoin, phenobarbital, valproate, carbamazepine, primidone, topiramate, clobazam and levetiracetam. The patient was also taking paroxetine for depression related to the impact of his epilepsy on his ability to work and drive. He had had 2 brief febrile convulsions on the same day at 2 years of age but had no subsequent convulsions. His father had a history of grand mal seizures of unknown cause. The patient's physical examination was unremarkable, but he felt that his short-term memory was not as good as it had been at college.
Previous electroencephalograms (EEGs) over the years had demonstrated right temporal spikes, and previous MRI scans showed signs in the right hippocampus consistent with mesial temporal sclerosis (Fig. 1, arrow). Continuous EEG monitoring revealed seizures arising from the right temporal lobe. A formal neuropsychological evaluation was compatible with impaired memory mechanisms in the right mesial temporal structures but with notably intact memory in the left temporal lobe. Functional MRI for language localization indicated left hemisphere dominance (Fig. 2, arrows). A right temporal lobectomy in the form of a selective amygdalohippocampectomy was performed. The patient has been seizure-free since and continues to take low-dose carbamazepine therapy.
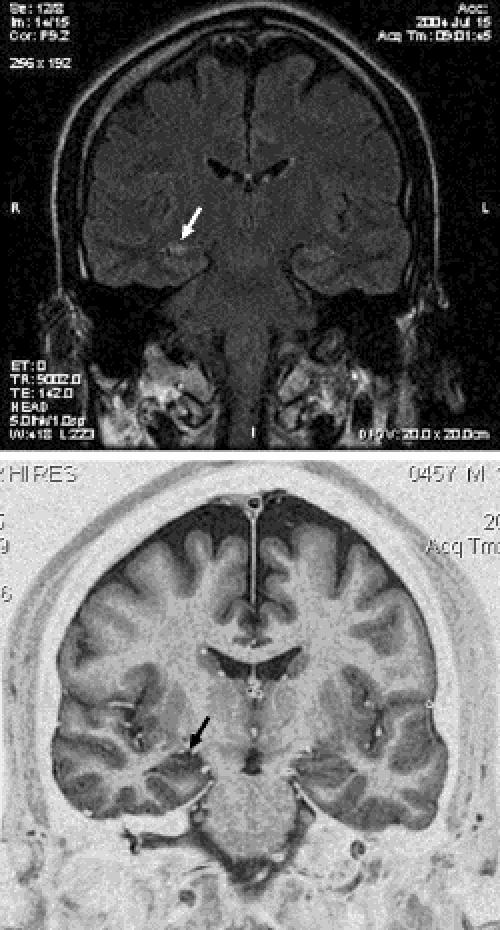
Fig. 1: Top: Coronal section of MRI of the brain on FLAIR (fluid-attenuated inversion recovery) sequence, showing high signal changes in the right hippocampus (arrow). Bottom: Coronal section of the same MRI on IR (inversion recovery) sequence, showing evidence of atrophy of the right hippocampus (arrow). The combination of these findings is diagnostic of mesial temporal sclerosis.
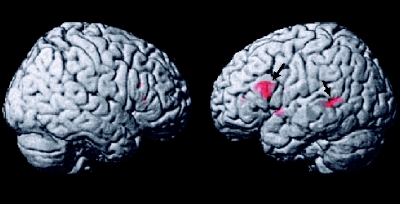
Fig. 2: Three-dimensional view of patient's brain. Areas of activation (Broca's area and Wernicke's area, arrows) for language are seen during mapping using functional MRI.
Epilepsy is a chronic disease characterized by the risk of recurrent seizures that afflicts about 200 000 Canadians at any one time. In Canada the prevalence is 5.6 per 1000 population, with some variation depending on age.1 Seizures are completely controlled in about two-thirds of those with epilepsy,2 but an estimated 50 000 Canadians continue to have medically uncontrolled refractory seizures. According to the World Health Organization, disability due to epilepsy accounts for about 1% of the global burden of disease, as measured by disability-adjusted life-years, which ranks epilepsy just after some psychiatric problems such as affective disorders and alcohol dependence. The global burden of epilepsy is comparable to that of breast and lung cancer.
In about half the cases, epilepsy is considered idiopathic and is characterized by generalized seizures influenced primarily by genetic factors. The remainder involve focal seizures from a cortical lesion. Our case illustrates the most common form of intractable focal or partial epilepsy, mesial temporal lobe epilepsy (TLE). The cause was mesial temporal sclerosis, the usual pathological substrate of TLE. Although this type of epilepsy often responds poorly to treatment with antiepileptic medication, surgery offers an opportunity for complete seizure control in many instances.
TLE due to mesial temporal sclerosis is a well-defined epileptic syndrome of partial seizures, localized anteromesial temporal lobe abnormalities on EEG, memory dysfunction, and hippocampal atrophy or sclerosis on MRI. The mean age of seizure onset in patients with mesial temporal sclerosis is typically during the second or third decade of life. Patients often have a history of febrile seizures early in life. Ictal features characteristic of TLE include epigastric (rising sensation, nausea, butterflies), emotional (fear) or psychic (déjà vu) auras; decreased behavioural activity with unresponsiveness and staring; clouding of consciousness; oroalimentary (lip smacking, chewing) or manual (picking, rubbing, walking) automatisms; and autonomic (pallor) phenomena.
Because TLE with mesial temporal sclerosis is refractory to antiepileptic medications in more than 90% of patients with the condition, early surgical intervention is now advocated. No longer a treatment of last resort, surgical therapy after 1 or 2 antiseizure drugs have been tried will alleviate seizures in at least 70% of cases, as compared with no more than 5% of cases if another drug is added.
However, epilepsy surgery appears to be grossly underused. Our patient waited 35 years before referral to an epilepsy centre. In Canada, of an estimated 20 000 people with intractable epilepsy who are candidates for surgery, only 352 underwent surgical treatment during a recent 1-year survey.3 Similarly, in the United States, it is estimated that only 1500 patients undergo such surgical procedures each year. Many clinicians who care for patients with epilepsy are still uncertain about the efficacy and safety of surgical procedures and still view surgery as a last resort for patients with intractable epilepsy, even though the efficacy of surgery has been well demonstrated.
In addition to the many observational studies of the impact of surgical management, including those by Wilder Penfield and colleagues at the Montreal Neurological Institute more than 70 years ago, the only randomized, controlled trial of epilepsy surgery to date was done in London, Ont., by Wiebe and associates.4 The evidence from that study alleviated any doubt about the efficacy of surgical treatment in temporal lobe epilepsy both for controlling seizures and for improving quality of life. Furthermore, the extensive preoperative investigation now carried out in epilepsy surgery centres limits any unwanted impact of surgery on normal brain function. Concerns that surgery may result in adverse effects on memory, language, behaviour and emotion must be weighed against the potential consequences of continued disabling seizures on these functions. The disruption of the limbic system caused by recurrent temporal lobe seizures is often associated with both memory impairment and behavioural problems that in some cases may be progressive. Although hippocampal resection can impair memory, it has long been known that the memory deficits related to continued complex partial seizures may actually be reversed, and overall cognitive function improved, if seizure-induced dysfunction of the contralateral hippocampus is eliminated by temporal lobe surgery. In general, the psychological and social consequences of disabling complex partial seizures that develop over time in many people with epilepsy have a much more negative impact than any adverse effects of surgical treatment. This is clearly indicated by patients' own reports in the form of standardized, health-related quality-of-life measures. Finally, uncontrolled seizures are associated with a not inconsequential mortality far greater than that associated with any form of epilepsy surgery.
There are 2 main surgical treatments for TLE with seizures arising from mesial temporal structures. Standard anterior temporal resection includes resection of up to 6.5 cm of the anterior nondominant (usually right) temporal lobe and 4.5 cm of the dominant temporal lobe, sparing the language area. Usually such resections encompass the amygdala and at least 1.0–3.0 cm of the hippocampus, where short-term memory resides. The second procedure is selective amygdalohippocampectomy, as was used in our patient. It is a limited removal of the hippocampal formation and amygdala, sparing the anterior and lateral temporal neocortex. Although no definitive comparative studies have been done of these 2 operations, they are likely equally effective in controlling seizures, and there is evidence that suggests the more limited procedure may have less impact on neuropsychological function.
Although TLE with mesial temporal sclerosis is the most common surgically treated seizure disorder, there are other focal epilepsy syndromes amenable to surgical management. More accurate diagnosis through multidisciplinary assessments in epilepsy monitoring units and improvements in neuroimaging have allowed more patients to be considered for surgical treatment. An example of improved neuroimaging is high-resolution MRI techniques that detect subtle malformations of cortical development. A variety of other functional techniques may help to locate areas of epileptogenesis in patients without visible structural lesions. Among these techniques are functional MRI, single photon emission computed tomography (SPECT) scanning, and magnetic source imaging (MSI). Localization of seizure activity using continuous EEG recording from the scalp or from implanted intracranial electrodes, however, remains the mainstay of investigation of potential candidates for surgery.
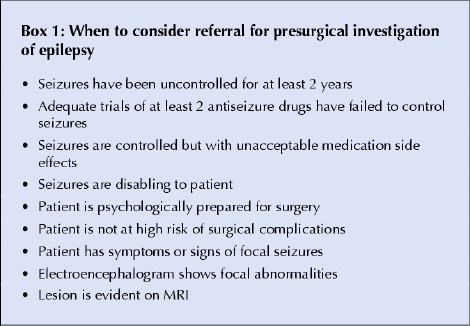
This case highlights the lack of an early adequate referral of a patient with intractable or refractory epilepsy.5 Box 1 outlines some general considerations for surgical management and referral to an epilepsy centre. Patients with seizures whose condition does not improve after 2 to 3 adequate trials of antiseizure medications may benefit from referral to an epilepsy centre, especially if there are signs that the patient has a surgically treatable condition such as temporal lobe epilepsy.
Box 1.
Jorge G. Burneo Richard S. McLachlan Epilepsy Program London Health Sciences Centre University of Western Ontario London, Ont.
References
- 1.Tellez-Zenteno JF, Pondal-Sordo M, Matijevic S, Wiebe S. National and regional prevalence of self-reported epilepsy in Canada. Epilepsia 2004;45(12):1623-9. [DOI] [PubMed]
- 2.Kwan P, Brodie MJ. Early identification of refractory epilepsy. N Engl J Med 2000;342(5):314-9. [DOI] [PubMed]
- 3.McLachlan RS. Commentary on epilepsy surgery in Canada. Can J Neurol Sci 2001;28(1):4-5. [DOI] [PubMed]
- 4.Wiebe S, Blume WT, Girvin JP, Eliasziw M; Effectiveness and Efficiency of Surgery for Temporal Lobe Epilepsy Study Group. A randomized, controlled trial of surgery for temporal-lobe epilepsy. N Engl J Med 2001;345(5):311-8. [DOI] [PubMed]
- 5.Trevathan E, Gilliam F. Lost years: delayed referral for surgically treatable epilepsy. Neurology 2003;61(4): 432-3. [DOI] [PubMed]


