Reason for posting: Many patients with eczema, or atopic dermatitis, are prescribed the topical immunomodulators tacrolimus and pimecrolimus. The drugs are often given to people for whom the potential side effects of topical corticosteroids (e.g., systemic absorption, skin thinning, telangiectasia) are a concern. However, the US Food and Drug Administration (FDA) recently reviewed the safety of these agents and warned that they may be associated with a risk of cancer.1
The drugs: Tacrolimus and pimecrolimus bind and inactivate calcineurin (a calcium- and calmodulin-dependent serine and threonine phosphatase) and may act by inhibiting T-lymphocyte activation, down-regulating numerous interleukins, interferon-γ, granulocyte-macrophage colony-stimulating factor and tumour necrosis factor-α, and affecting the function of mast cells, basophils and Langerhans cells.
Both agents are more effective than placebo in treating atopic dermatitis. Tacrolimus (0.03% and 0.1% preparations) is more effective than mild topical steroids, and the 0.1% preparation is as effective as more potent topical steroids.2 In contrast, pimecrolimus is less effective than potent steroids (0.1% betamethasone valerate), but its efficacy relative to mild corticosteroids is unclear.2
Common adverse effects include mild, local, temporary burning or pruritus, and users may have increased risk of local varicella-zoster virus infection, herpes simplex infection and eczema herpeticum. Children under the age of 2 receiving topical pimecrolimus had higher rates of respiratory tract infections than children receiving the placebo.1
Lymphadenopathy, usually transient and related to underlying infections, has been reported. However, patients taking systemic tacrolimus (as an immunosuppressive agent after liver and organ transplantation) have reported lymphomas and solid organ tumours, possibly because their defences against cancer have been suppressed.3Only small amounts of the drugs are usually absorbed through the skin; however, some children given topical tacrolimus have blood levels of the drug similar to those given its systemic form.1
Animals (mice, rats, monkeys) given high doses of the drugs topically or orally have a risk of cancer that is dependent on both the duration and dose of the drug.1,3 Long-term safety trials involving humans have not been done.
Causative associations are uncertain, but the FDA is also reporting the cases of several patients in whom cancer developed after drug use. For tacrolimus, 19 cases of cancer were reported, involving 16 adults and 3 children under the age of 16. The cancers were diagnosed 21–790 days after the start of therapy (the median time to diagnosis was 150 days). Nine cases involved lymphomas, and 10 involved skin tumours (7 at the site of the drug application). Tumour types included squamous cell carcinoma, cutaneous sarcoma and malignant melanoma. For pimecrolimus, 10 postmarketing cases of cancer were reported, involving 4 children (3 less than 6 years of age) and 6 adults. Of the 10 cases, 6 involved cutaneous tumours and 4 were lymphomas. Diagnoses were made 7–300 days after treatment was started (median time to diagnosis was 90 days).
What to do: As second-line agents, these drugs should be used only if other therapies (topical corticosteroids, emollients) are ineffective or inappropriate. They should not be used by patients with weakened or compromised immune systems, by children under the age of 2 or by patients with active viral skin infections. Short-term or intermittent use is advised. Unfortunately, atopic dermatitis is an uncomfortable, common and chronic condition. Patients should be warned of the potential cancer risk and carefully monitored clinically when taking the drugs. Any patient with nonresolving lymphadenopathy should be appropriately investigated. The lowest concentration of the drugs needed to control a patient's symptoms should be used. Unnecessary and potentially harmful ultraviolet exposure (from the sun and tanning beds) should be avoided.
Eric Wooltorton Associate Editor, CMAJ
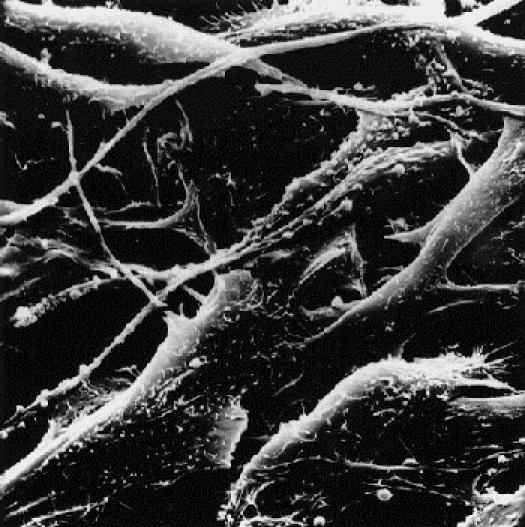
Figure. Melanoma Photo by: Timothy Triche, National Cancer Institute
Footnotes
Published at www.cmaj.ca on Apr. 7, 2005.
References
- 1.US Food and Drug Administration. FDA Public Health Advisory: Elidel (pimecrolimus) cream and Protopic (tacrolimus) ointment. 2005 Mar 10. Available at: www.fda.gov/medwatch/SAFETY/2005/safety05.htm#Elidel (accessed 2005 Mar 30).
- 2.Ashcroft DM, Dimmock P, Garside R, Stein K, Williams HC. Efficacy and tolerability of topical pimecrolimus and tacrolimus in the treatment of atopic dermatitis: meta-analysis of randomized controlled trials. BMJ 2005;330:516-22. [DOI] [PMC free article] [PubMed]
- 3.Niwa Y, Terashima T, Sumi H. Topical application of the immunosuppressant tacrolimus accelerates carcinogenesis in mouse skin. Br J Dermatol 2003;149:960-7. [DOI] [PubMed]


