Abstract
Epidemic increases in opioid use in the USA and globally highlight the need for effective adjunctive therapies to opioid-based analgesia. Given the shortcomings of behavioral adjuncts to opioid-based pain treatment, an urgent need exists for pain-related behavioral interventions that resonate with broad patient populations, can be delivered confidentially in any environment, and can incorporate new content automatically. Understanding the potential for automated behavioral therapies like music therapy in modulating the experience of pain may unlock methods to transition patients to lower doses of pharmacologic therapy or provide alternatives to opioids during acute exacerbations of pain. This manuscript describes the neurologic mechanism of action, theoretical basis, and potential applications of personalized music as a smartphone-based mHealth intervention for acute and chronic pain management.
Keywords: Music, Opioids, Pain, mHealth, Behavioral medicine
Introduction
Epidemic increases in opioid use highlight the need for effective adjunct therapies to opioid-based analgesia [1–4]. Behavioral therapies to improve analgesia are designed to reconfigure how individuals anticipate, perceive, and respond to pain. As an integral component of the multidisciplinary approach to pain, behavioral interventions address individual perceptions of pain, reinforce adherence to pharmacologic therapy, and frame pain in a more manageable context. Behavioral interventions for pain teach techniques to minimize psychosocial distress (e.g., catastrophizing, depression) while increasing pain acceptance through cognitive behavioral therapy (CBT) or mindfulness (MT) [5, 6]. These techniques have been demonstrated to be efficacious in decreasing chronic pain-related problems.
Unfortunately, existing behavioral interventions for pain suffer from several shortcomings. First, CBT and MT are time intensive techniques; even Internet or mobile-based adaptations of these therapies require that users learn behavioral techniques. Second, patients with chronic, unremitting pain may need lifelong interventions; behavioral therapy may need to be unending as well. CBT and MT interventions are skills that may denature over time. Given the lifelong nature of chronic pain, individuals may need periodic refreshers to ensure behavioral interventions persist. Finally, many of the behavioral interventions in current use suffer from limited content. For example, a “large” library of text messages to be used as behavioral supports may have limited messages especially considering the length of time a patient may need to use these behavioral supports; patients may quickly tire of receiving material drawn from this small group of content, a process known as “intervention fatigue.” Given the shortcomings of behavioral adjuncts to opioid-based pain treatment, an urgent need exists for pain-related behavioral interventions that resonate with broad patient populations, can be delivered confidentially in any environment, and can incorporate new content automatically. With its almost universal appeal, music may be an innovative adjunct to standard pharmacologic therapy for pain that is non-stigmatizing, can be delivered by mobile devices, requires little teaching, and may present an ever evolving yet personalized intervention to individuals suffering from chronic pain [7, 8]. This paper describes the neurologic mechanism of action, theoretical basis, and potential applications of music as a behavioral intervention for pain management.
Music as a Behavioral Intervention
Music, one of the most abstract of all art forms, can nonetheless depict places, people, or events through sound and serves several functions related to communication, social cohesion, and emotional reward [9, 10]. Synesthesia is the neurological phenomenon in which stimulation of one sensory or cognitive pathway leads to automatic, involuntary experiences in a second sensory or cognitive pathway encapsulates this, such as hearing music and seeing vivid colors (also known as chromesthesia). The anthropological history of music includes its incorporation into healing and medicine; every culture has described the importance of creating and listening to music. For example, the ancient Egyptians used song as a modality to heal the sick, while Hippocrates believed music as deeply intertwined with the medical arts [11, 12]. Music has emotive effects, including a near-universal ability to trigger pleasurable responses [13]. Music is expressive; individuals may trigger a variety of emotions through creating music in groups or individually. Via its ability to modify the affective or cognitive state of the listener, music can be adapted to function as a behavioral intervention for pain.
Neurologic Basis of the Effect of Music on Affective States
Music is similar to other positively valenced stimuli such as money, sexual encounters, food, and psychoactive drugs that affect dopaminergic neurotransmission in the mesolimbic striatal system, the pathway implicated in reward, reinforcement, and motivation [9, 14–16].
The impact of music on the location and intensity of change in dopamine activity has been investigated by neuroimaging techniques. Functional magnetic resonance imaging (fMRI) studies have identified that the “wanting” phase (where a person wants to hear a pleasurable song) and “liking” phases (where the individual is rewarded with the pleasure of music) map to distinct brain regions within the caudate and nucleus accumbens [17, 18]. In these fMRI studies, the greatest dopamine response occurred immediately before peak emotional response [14, 15]. This spike in dopaminergic activity predominated in the striatum, a network of brain regions implicated in learned, reward-relevant, stimulus-response associations [14, 19]. Greater dopaminergic responses were initially observed in ventral striatal regions, but transitioned to more motor-oriented dorsal striatal areas as rewards become better predicted [14, 15]. These findings demonstrate that dopamine release in response to expectation, anticipation, and reward is triggered by music found desirable to the listener [20]. A recent resting-state fMRI study in patients with fibromyalgia who self-selected preferred and self-identified relaxing music correlated reduction of pain with increases in resting-state fMRI blood oxygen level-dependent signal amplitude in the left angular gyrus [21]. These data suggest that listening to well-liked pleasant music enhances functional connectivity between dorsal striatal structures and elements of the default mode network, potentially highlighting music’s role in influencing the valence and reward characteristics of multimodal sensory processing in patients with chronic pain [22]. Simply stated, pleasurable music changes neuronal pathways is patients suffering from painful conditions.
Exposure to music also produces beneficial effects on autonomic nervous system functioning, inducing adaptive changes in heart rate variability, electrodermal activity, skin temperature, and locomotion [18]. Continuous measurements of sympathetic nervous system activity in research participants listening to music demonstrated physiologic signs of emotional arousal; this sympathetic nervous system activity correlated strongly with real-time subjective ratings of pleasure [20, 23]. Conversely, participants who listened to songs that did not elicit subjective pleasure had no corresponding increase in physiologic measures of emotional arousal [18].
The experience of music as either “pleasurable” or “unpleasurable” may be partially mediated by the opioid receptor axis in the CNS. The emotion of “wanting” to hear a pleasurable song is associated with an increase in circulating endogenous opioids and an increased expression of the mu opioid receptor [22, 24]. Conversely, antagonism of mu opioid receptor function (e.g., with a competitive antagonist such as naltrexone) produces decreases in the subjective desirability of music and in the reported “thrill” of music listening [25]. Collectively, the ability of music to modulate affective state via its effects on circulating endogenous opioids and mu opioid receptor expression suggests that a tailored music-based behavioral intervention could be effectively used as an adjunct to pharmacologic therapy in treatments of pain [20, 24].
Theoretical Basis of Music as an Intervention for Pain
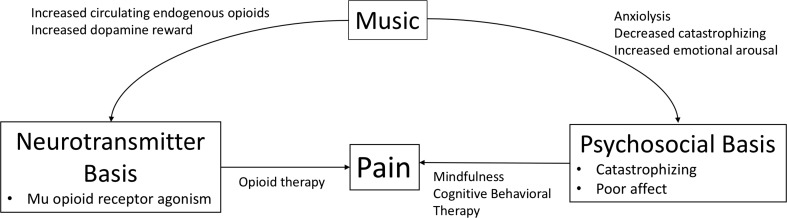
Music, with its abilities to improve affect and mood, intercalates well with gate-control theory of pain developed by Melzack and Wall as well as the subsequent neuromatrix theory of pain (Fig. 1) [26, 27]. These theories hold that pain is multimodal in origin, where physiological and psychosocial processes alter the perception and evaluation of pain. The confluence of these theories has altered approaches towards chronic pain from a monolithic focus on pharmacologic therapy to a multimodal strategy that integrates a variety of interventions addressing the broad array of biopsychosocial contributors to the experience of pain [28]. This biopsychosocial model of pain emphasizes a view of pain as a complex sensory and emotional experience. Broad endorsement of this biopsychosocial approach to pain has led to increasing interest in treatment strategies that are aimed at the self-management of chronic pain rather than its cure [28]. Psychologically based interventions as adjunct treatments for pain, the popularity of which has grown in recent years, have the aim of attenuating symptoms, one goal of which is to decrease reliance on pharmacologically based therapies. Music, with its ability to increase pleasure by activating dopaminergic reward circuitry in the central nervous system, has been demonstrated to blunt the pain response and therefore function as a neurobiology-based intervention that improves both acute and chronic pain [29, 30].
Fig. 1.
The neuromatrix theory of pain describes the effect of neurotransmitters and psychosocial basis of pain. Treatment of pain therefore incorporates both bases for pain by providing pharmacologic therapy (opioids) and behavioral interventions (CBT/MT). Music can address both the neurotransmitter and psychosocial basis of pain through regulation of endogenous opioid circulation, increasing dopamine reward pathways, increasing positively valenced emotions, and decreasing catastrophizing
Music reduces the considerable postoperative pain observed in thoracic or spine surgery as well as minor operative procedures [29, 31, 32]. Music therapy also decreases perioperative opioid use as well as the overall amount of opioids delivered by IV-PCA to surgical patients [32]. Music has an anxiolytic effect as well. Anxiety and other signs of stress also decrease in response to music [30, 33]. For example, music effectively reduces catastrophizing about burn dressing changes, epidural catheter placement, and bone marrow biopsies [7, 34, 35]. Decreases in indices of stress and sympathetic nervous system activation, as well as pain, occur when music is used in the time surrounding surgery; the effect size is the greatest when music is administered preoperatively, when anxiety is the highest. Music played during general anesthesia is, unsurprisingly, less effective than conscious listening [29, 36, 37]. Some analyses identified that these effects were most prominent when patients could select which music they could listen [29].
Despite this promising evidence of music to modulate the psychological and physiologic response to pain, important questions remain about the timing and choice of music and how to maximize its potential as an adjunct behavioral intervention in pain. For instance, the tailoring of music to a patient’s preferences or memories, or even in response to real-time detection of opioid ingestion or stressful events, might improve the music’s efficacy in reducing pain. Locus of control (e.g., whether the music is self- or experimenter-selected) may alter adherence to and efficacy of a music intervention, although studies have demonstrated benefit of both patient self-selection and experimenter-selected music [38–40]. Overall, we hypothesize that patient self-selection of desirable songs may improve retention in longitudinal interventions, and facilitate the optimization of “dosing” including duration, settings, and volume of music interventions, which may in turn maximize the efficacy of music-based analgesic treatments.
Innovative Strategies for Tailoring Music to Improve Pain
Ideally, music therapy can be tailored to both individual preference and indices of pain level. Three existing methods to curate digital music content could potentially be used to achieve this real-time, individualized tailoring: (1) active personal curation (e.g., individual searching for music and adding it to a personalized playlist), (2) professional curation (an authority in music curating content), and perhaps most appealing, (3) automated discovery. Techniques of active personal curation, professional curation, and automated discovery form the basis for commercial delivery of music. Most music interventions describe active personal curation (participant locus of control) or professional curation (experimenter locus of control). The use of automated discovery to deliver music interventions has yet to be investigated.
Automated discovery, commercialized by popular online music providers like Spotify and Pandora, offers an intriguing solution to intervention fatigue. It can, in theory, provide endlessly novel, but appropriate, music choices to behavioral interventions. Automated discovery consists of two parts—collaborative filtering and content-based modeling. Collaborative filtering is a process in which users with similar music preferences are matched, playlists indexed, and unique songs that a user may not possess highlighted—resulting in new content that is likely to be accepted by the user. Content-based modeling utilizes machine learning to assign specific attributes to phrases of music (i.e., musical “genes”) [41]. An algorithm then searches libraries of music across genres and periods to find matching musical genes, thereby creating a list of new songs recommended to the user.
Automated discovery is appealing because it provides a method to provide ever-new content to a patient managing a chronic disease (e.g., chronic pain); it also permits patients to manage the “dosage” of music they require in response to pain. An additional feature of automated discovery is that recommendation accuracy improves with use by the individual and with greater numbers of users. For example, a group of patients managed by a chronic pain service who use automated discovery to access songs that improve positive affect and decrease opioid use will then receive improved recommendations that parallel increased patient participation, leading to persistence of the intervention. At the same time, groups of patients with pain may curate desired songs among themselves, creating a library of music interventions that respond to the affective cues of a specific group. As new songs are written and digitized, they increase the potential library providing automated, novel content for users, thereby mitigating intervention fatigue.
In addition to facilitating automated discovery, musical genes can also be used to create songs de novo. By understanding the musical genes that improve a patient’s affect through automated discovery, affect-improving phrases of music can be stitched together to create novel passages of music that modulate pain. This concept of tailoring music based on automated discovery provides an innovative and unique approach compared to existing music behavioral interventions.
Roles of the Toxicologist in Music and Pain Management
Medical toxicologists have a growing experience using innovative mobile technologies in substance abuse investigations [42–46]. Understanding the ability of music to modulate pain may provide alternatives to opioids. An improved understanding of the relationship between pain, stress, anxiety, and the neurotransmitters which modulate these states will help investigators tailor music as a personalized therapy for individuals with chronic pain or substance abuse. Toxicologists may apply their expertise in medication adherence and substance abuse to create models where music enhances adherence to non-opioid analgesics by improving an individual’s perception of their pain. Finally, any condition which responds to improvements in positive affect is potentially amenable to music as an intervention.
Potential Research Avenues
At present, a single behavioral intervention does not apply broadly across conditions; a behavioral theory (e.g., the Theory of Reasoned Action) might serve as a grounding for a wide number of interventions, but each single intervention applies to a unique condition (e.g., Life Steps rooted in Cognitive Behavioral Theory supports antiretroviral adherence in HIV+ men who have sex with men, while Motivational Interviewing supports cannabis abstinence in cannabis-dependent individuals) [47]. This odd situation is analogous to inventing a unique antibiotic for each type of infection, at the time the infection appears. Treatments based on music—as a universal art form—have the potential to revolutionize behavioral intervention development by eliminating the need to recreate a new, unique behavioral intervention for each disease state that responds to positive affect. Because of the nearly universal use of music across cultures and socioeconomic status, additionally, understanding what the features of music that modulate affect in the context of real-life events is unknown. Our proposed line of investigation, therefore, is first to assess the acceptability and usability of music in an outpatient pain clinic (Table 1). Next, once acceptability is established, the assessment of endpoints such as decreased pain, changes in psychosocial distress, and the degree of pharmacologic therapy needed in conjunction with music interventions should be considered. Delivery of music interventions can be scheduled around times when individuals ingest opioids; alternatively, music interventions could be available at all times, allowing individuals to tailor the timing as well as dose of music intervention. Finally, understanding the correct dosing and duration of music behavioral interventions is important. Whether music interventions can be delivered in a fashion similar to CBT—initial bursts of intervention followed by “refresher” sessions—or whether music can be delivered in response to increasing pain or escalating opioid use should be another important line of investigation.
Table 1.
Potential concepts and study designs to assess music as a behavioral intervention for pain
| Potential research concept | Study design | Outcome |
|---|---|---|
| Locus of control | Randomized participants to participant centered versus experimented centered locus of control in music selection | • User preference for locus of control • Adoption of intervention |
| Dosing of music intervention | Investigating the timing of music interventions scheduled around opioid administration, painful events versus participant-initiated music | • Uptake of participant-initiated dosing • Learned used of music interventions by participants |
| Pharmacologic therapy | Dosed music as an adjunct to opioid use in chronic pain | • Opioid ingestion patterns • Increased dosing of music in response to escalating opioid ingestion patterns |
| Music as a behavioral intervention | Implementing a tailored, automatic discovery music intervention used by participants with chronic pain | • Changes in pain scales • Changes in psychosocial phenotypes • Sustainability of a music intervention |
Pitfalls in Music Therapy for Pain
Despite the promising ability of music to temper the perception of pain, multiple limitations exist in its deployment. Methods through which individuals experience pain are highly variable, and the exact point at which a music intervention may modulate the development of chronic pain remains unknown. Designing studies that assess the efficacy of music are complicated by variations in methods of music delivery (headphones with noise canceling, delivery at home, or during clinic visits), degree of control in song selection, and the appropriate timing of music interventions. Although we focus on the passive listening of music in this paper, evidence suggests that the effects of music may be augmented during the active generation of music—whether through rhythmic drum circles, singing, or instrumental ensembles [20]. These concepts may alter the efficacy of music in substance abuse treatment if deployed as a part of group therapy in comparison to individual therapy sessions. Similarly, the locus of control may alter the efficacy of music. Although it may seem intuitive that a user-centered locus of control in a music intervention would increase its use and acceptability, shifting the locus of control to the investigator or therapist may allow for standardized music delivered to study participants. Finally, the timing and method of music interventions—whether music is delivered immediately prior to scheduled pharmaceutical therapy in pain, or in response to medication ingestion, and the use of smartphone apps or text message prompts to listen to music—remain to be investigated.
Conclusions
Digitized music, delivered via mobile devices such as smartphones, can be innovatively combined with automated discovery algorithms to generated tailored music lists designed to modulate pain and decrease opioid use. Music augments positive reward pathways in the brain and functions to reinforce healthy engagement with disease states, including chronic pain. By leveraging automatic discovery through vast libraries of songs across multiple users or the stitching of music genes to create continuously novel songs, music interventions can continue to provide novel content to users as they develop personalized self-management approaches to reduce acute and chronic pain.
Acknowledgements
Dr. Boyer is supported by the National Institutes of Health 1K24DA037109. Dr. Carreiro is supported by the National Institutes of Health KL2 TR001455-01. Ketki Karanam and Marko Ahtisaari are co-founders of the Sync Project.
Compliance with Ethical Standards
Conflicts of Interest
None.
Sources of Funding
None.
References
- 1.Rudd RA, Aleshire N, Zibbell JE, Gladden RM. Increases in drug and opioid overdose deaths—United States, 2000–2014. MMWR Morb Mortal Wkly Rep. 2016;64:1378–1382. doi: 10.15585/mmwr.mm6450a3. [DOI] [PubMed] [Google Scholar]
- 2.Chang H-Y, Daubresse M, Kruszewski SP, Alexander GC. Prevalence and treatment of pain in EDs in the United States, 2000 to 2010. Am J Emerg Med. 2014;32:421–431. doi: 10.1016/j.ajem.2014.01.015. [DOI] [PubMed] [Google Scholar]
- 3.Dart RC, Severtson SG, Bucher-Bartelson B. Trends in opioid analgesic abuse and mortality in the United States. N Engl J Med. 2015;372:1573–1574. doi: 10.1056/NEJMsa1406143. [DOI] [PubMed] [Google Scholar]
- 4.Gilson AM, Ryan KM, Joranson DE, Dahl JL. A reassessment of trends in the medical use and abuse of opioid analgesics and implications for diversion control: 1997–2002. J Pain Symptom Manag. 2004;28:176–188. doi: 10.1016/j.jpainsymman.2004.01.003. [DOI] [PubMed] [Google Scholar]
- 5.Cherkin DC, Sherman KJ, Balderson BH, Cook AJ, Anderson ML, Hawkes RJ, et al. Effect of mindfulness-based stress reduction vs cognitive behavioral therapy or usual care on back pain and functional limitations in adults with chronic low back pain: a randomized clinical trial. JAMA. 2016;315:1240–1249. doi: 10.1001/jama.2016.2323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Turner JA, Anderson ML, Balderson BH, Cook AJ, Sherman KJ, Cherkin DC. Mindfulness-based stress reduction and cognitive behavioral therapy for chronic low back pain: similar effects on mindfulness, catastrophizing, self-efficacy, and acceptance in a randomized controlled trial. Pain. 2016;157:2434–2444. doi: 10.1097/j.pain.0000000000000635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Drzymalski DM, Tsen LC, Palanisamy A, Zhou J, Huang C-C, Kodali BS. A randomized controlled trial of music use during epidural catheter placement on laboring parturient anxiety, pain, and satisfaction. Anesth Analg. 2017;124:542–547. doi: 10.1213/ANE.0000000000001656. [DOI] [PubMed] [Google Scholar]
- 8.De Silva AP, Niriella MA, Nandamuni Y, Nanayakkara SD, Perera KRP, Kodisinghe SK, et al. Effect of audio and visual distraction on patients undergoing colonoscopy: a randomized controlled study. Endosc Int Open. 2016;4:E1211–E1214. doi: 10.1055/s-0042-117630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dubé L, Le Bel J. The content and structure of laypeople’s concept of pleasure. Cognit Emot. 2003;17:263–295. doi: 10.1080/02699930302295. [DOI] [PubMed] [Google Scholar]
- 10.Mas-Herrero E, Zatorre RJ, Rodriguez-Fornells A, Marco-Pallarés J. Dissociation between musical and monetary reward responses in specific musical anhedonia. Curr Biol. 2014;24:699–704. doi: 10.1016/j.cub.2014.01.068. [DOI] [PubMed] [Google Scholar]
- 11.Babikian T, Zeltzer L, Tachdjian V, Henry L, Javanfard E, Tucci L, et al. Music as medicine: a review and historical perspective. Altern Complement Ther. 2013;19:251–254. doi: 10.1089/act.2013.19510. [DOI] [Google Scholar]
- 12.West ML. The Babylonian musical notation and the Hurrian melodic texts. Music Lett. 1994;75:161–179. doi: 10.1093/ml/75.2.161. [DOI] [Google Scholar]
- 13.Conrad C. Music for healing: from magic to medicine. Lancet. 2010;376:1980–1981. doi: 10.1016/S0140-6736(10)62251-9. [DOI] [PubMed] [Google Scholar]
- 14.Salimpoor VN, Benovoy M, Larcher K, Dagher A, Zatorre RJ. Anatomically distinct dopamine release during anticipation and experience of peak emotion to music. Nat Neurosci. 2011;14:257–262. doi: 10.1038/nn.2726. [DOI] [PubMed] [Google Scholar]
- 15.Menon V, Levitin DJ. The rewards of music listening: response and physiological connectivity of the mesolimbic system. NeuroImage. 2005;28:175–184. doi: 10.1016/j.neuroimage.2005.05.053. [DOI] [PubMed] [Google Scholar]
- 16.Knutson B, Burgdorf J, Panksepp J. Ultrasonic vocalizations as indices of affective states in rats. Psychol Bull. 2002;128:961–977. doi: 10.1037/0033-2909.128.6.961. [DOI] [PubMed] [Google Scholar]
- 17.Mantione M, Figee M, Denys D. A case of musical preference for Johnny Cash following deep brain stimulation of the nucleus accumbens. Front Behav Neurosci. 2014;8:152. doi: 10.3389/fnbeh.2014.00152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.van den Bosch I, Salimpoor VN, Zatorre RJ. Familiarity mediates the relationship between emotional arousal and pleasure during music listening. Front Hum Neurosci. 2013;7:534. doi: 10.3389/fnhum.2013.00534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Blum K, Chen TJH, Chen ALH, Madigan M, Downs BW, Waite RL, et al. Do dopaminergic gene polymorphisms affect mesolimbic reward activation of music listening response? Therapeutic impact on Reward Deficiency Syndrome (RDS) Med Hypotheses. 2010;74:513–520. doi: 10.1016/j.mehy.2009.10.008. [DOI] [PubMed] [Google Scholar]
- 20.Chanda ML, Levitin DJ. The neurochemistry of music. Trends Cogn Sci. 2013;17:179–193. doi: 10.1016/j.tics.2013.02.007. [DOI] [PubMed] [Google Scholar]
- 21.Garza-Villarreal EA, Jiang Z, Vuust P, Alcauter S, Vase L, Pasaye EH, et al. Music reduces pain and increases resting state fMRI BOLD signal amplitude in the left angular gyrus in fibromyalgia patients. Front Psychol. 2015;6:1051. doi: 10.3389/fpsyg.2015.01051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stefano GB, Zhu W, Cadet P, Salamon E, Mantione KJ. Music alters constitutively expressed opiate and cytokine processes in listeners. Med Sci Monit. 2004;10:MS18–MS27. [PubMed] [Google Scholar]
- 23.Lee JH. The effects of music on pain: a meta-analysis. J Music Ther. 2016;53:430–477. doi: 10.1093/jmt/thw012. [DOI] [PubMed] [Google Scholar]
- 24.Mallik A, Chanda ML, Levitin DJ. Anhedonia to music and mu-opioids: evidence from the administration of naltrexone. Sci Rep. 2017;7:41952. doi: 10.1038/srep41952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Goldstein A. Thrills in response to music and other stimuli. Physiol Psychol. 1980;8:126–129. doi: 10.3758/BF03326460. [DOI] [Google Scholar]
- 26.Melzack R, Wall PD. Pain mechanisms: a new theory. Science. 1965;150:971–978. doi: 10.1126/science.150.3699.971. [DOI] [PubMed] [Google Scholar]
- 27.Melzack R. Stress-induced analgesia. Pain. 1985;22:101. doi: 10.1016/0304-3959(85)90154-X. [DOI] [Google Scholar]
- 28.Roditi D, Robinson ME. The role of psychological interventions in the management of patients with chronic pain. Psychol Res Behav Manag. 2011;4:41–49. doi: 10.2147/PRBM.S15375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hole J, Hirsch M, Ball E, Meads C. Music as an aid for postoperative recovery in adults: a systematic review and meta-analysis. Lancet. 2015;386:1659–1671. doi: 10.1016/S0140-6736(15)60169-6. [DOI] [PubMed] [Google Scholar]
- 30.Bradt J, Dileo C, Shim M. Music interventions for preoperative anxiety. In: Bradt J, editor. The Cochrane database of systematic reviews. Chichester: Wiley; 2013. p. CD006908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Liu Y, Petrini MA. Effects of music therapy on pain, anxiety, and vital signs in patients after thoracic surgery. Complement Ther Med. 2015;23:714–718. doi: 10.1016/j.ctim.2015.08.002. [DOI] [PubMed] [Google Scholar]
- 32.Wang Y, Tang H, Guo Q, Liu J, Liu X, Luo J, et al. Effects of intravenous patient-controlled sufentanil analgesia and music therapy on pain and hemodynamics after surgery for lung cancer: a randomized parallel study. J Altern Complement Med. 2015;21:667–672. doi: 10.1089/acm.2014.0310. [DOI] [PubMed] [Google Scholar]
- 33.Beaulieu-Boire G, Bourque S, Chagnon F, Chouinard L, Gallo-Payet N, Lesur O. Music and biological stress dampening in mechanically-ventilated patients at the intensive care unit ward—a prospective interventional randomized crossover trial. J Crit Care. 2013;28:442–450. doi: 10.1016/j.jcrc.2013.01.007. [DOI] [PubMed] [Google Scholar]
- 34.Eckhouse DR, Hurd M, Cotter-Schaufele S, Sulo S, Sokolowski M, Barbour L. A randomized controlled trial to determine the effects of music and relaxation interventions on perceived anxiety in hospitalized patients receiving orthopaedic or cancer treatment. Orthop Nurs. 2014;33:342–351. doi: 10.1097/NOR.0000000000000098. [DOI] [PubMed] [Google Scholar]
- 35.Fauerbach JA, Lawrence JW, Haythornthwaite JA, Richter L. Coping with the stress of a painful medical procedure. Behav Res Ther. 2002;40:1003–1015. doi: 10.1016/S0005-7967(01)00079-1. [DOI] [PubMed] [Google Scholar]
- 36.Nilsson U, Unosson M, Rawal N. Stress reduction and analgesia in patients exposed to calming music postoperatively: a randomized controlled trial. Eur J Anaesthesiol. 2005;22:96–102. doi: 10.1017/S0265021505000189. [DOI] [PubMed] [Google Scholar]
- 37.Liu Y, Bartlett N, Li L, Lv X, Zhang Y, Zhou W. Attitudes and knowledge about naloxone and overdose prevention among detained drug users in Ningbo, China. Subst Abuse Treat Prev Policy. 2012;7:6. doi: 10.1186/1747-597X-7-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wang S-M, Kulkarni L, Dolev J, Kain ZN. Music and preoperative anxiety: a randomized, controlled study. Anesth Analg. 2002;94:1489–1494. doi: 10.1097/00000539-200206000-00021. [DOI] [PubMed] [Google Scholar]
- 39.Wallston KA. The validity of the multidimensional health locus of control scales. J Health Psychol. 2005;10:623–631. doi: 10.1177/1359105305055304. [DOI] [PubMed] [Google Scholar]
- 40.Leardi S, Pietroletti R, Angeloni G, Necozione S, Ranalletta G, Del Gusto B. Randomized clinical trial examining the effect of music therapy in stress response to day surgery. Br J Surg. 2007;94:943–947. doi: 10.1002/bjs.5914. [DOI] [PubMed] [Google Scholar]
- 41.Meymandi A. Music, medicine, healing, and the genome project. Psychiatry (Edgmont) 2009;6:43–45. [PMC free article] [PubMed] [Google Scholar]
- 42.Chai PR, Babu KM, Boyer EW. The feasibility and acceptability of Google Glass for teletoxicology consults. J Med Toxicol. 2015;11:283–287. doi: 10.1007/s13181-015-0495-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chai PR, Carreiro S, Innes BJ, Rosen RK, O’Cleirigh C, Mayer KH, et al. Digital pills to measure opioid ingestion patterns in emergency department patients with acute fracture pain: a pilot study. J Med Internet Res. 2017;19:e19. doi: 10.2196/jmir.7050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Carreiro S, Fang H, Zhang J, Wittbold K, Weng S, Mullins R, et al. iMStrong: deployment of a biosensor system to detect cocaine use. J Med Syst. 2015;39:186. doi: 10.1007/s10916-015-0337-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Carreiro S, Wittbold K, Indic P, Fang H, Zhang J, Boyer EW. Wearable biosensors to detect physiologic change during opioid use. J Med Toxicol. 2016;12:255–262. doi: 10.1007/s13181-016-0557-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Skolnik AB, Chai PR, Dameff C, Gerkin R, Monas J, Padilla-Jones A, et al. Teletoxicology: patient assessment using wearable audiovisual streaming technology. J Med Toxicol. 2016;12:358–364. doi: 10.1007/s13181-016-0567-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Carroll KM, Onken LS. Behavioral therapies for drug abuse. Am J Psychiatry. 2005;162:1452–1460. doi: 10.1176/appi.ajp.162.8.1452. [DOI] [PMC free article] [PubMed] [Google Scholar]