Abstract
Background
Many people who are not obese according to standard height and weight criteria may still display features of insulin resistance syndrome and thus be at high risk of ischemic heart disease. We sought to investigate the effect of cumulative features of insulin resistance syndrome on the risk of ischemic heart disease associated with variations in body mass index (BMI) among men who participated in the Québec Cardiovascular Study.
Methods
A cohort of 1824 nondiabetic men free of ischemic heart disease was evaluated at the 1985 baseline evaluation and followed for a period of 13 years, during which 284 first ischemic heart disease events were recorded. Relative hazards (RHs) of ischemic heart disease in 3 BMI groups (normal weight, overweight and obese) were estimated using Cox proportional hazards regression.
Results
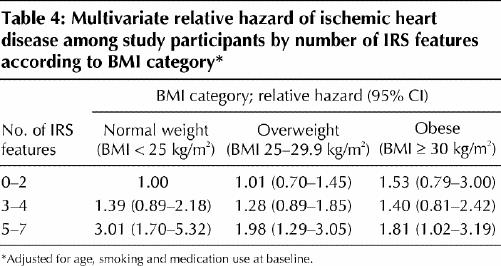
Although obese men (BMI ≥ 30 kg/m2) were the most likely to accumulate features of insulin resistance syndrome, the univariate risk of ischemic heart disease in this group was not significantly increased compared with normal-weight men (BMI < 25 kg/m2) (RH 1.26, 95% confidence interval [CI] 0.88–1.80). However, obese men who accumulated more than 4 features of insulin resistance syndrome were at increased risk of ischemic heart disease (RH 1.81, 95% CI 1.02–3.19) compared with normal-weight men who had fewer than 3 features of the syndrome. Conversely, having more than 4 features of insulin resistance syndrome was associated with a 3-fold increase in the risk of ischemic heart disease among normal-weight men (RH 3.01, 95% CI 1.70–5.32).
Interpretation
Although obesity is an important risk factor for ischemic heart disease, variations in BMI alone poorly reflect the risk of ischemic heart disease associated with features of insulin resistance syndrome.
In the late 1980s, Gerald Reaven proposed the concept of insulin resistance as the cornerstone of a plurimetabolic syndrome that included hypertriglyceridemia, low plasma high-density lipoprotein cholesterol concentrations, hypertension and hyperinsulinemia.1 This syndrome has been referred to as syndrome X, insulin resistance syndrome and the metabolic syndrome.2 Several other metabolic disturbances, such as an increase in the number of small, dense low-density lipoprotein particles, impaired fibrinolytic activity, a proinflammatory state, impaired postprandial lipoprotein metabolism and abdominal obesity, have been included as part of this syndrome over the years.3,4
Although obesity is an important component of insulin resistance syndrome, many people who are not obese according to standard height and weight criteria (i.e., body mass index [BMI]) may still display features of the syndrome. Indeed, studies have indicated that normal-weight subjects, whose BMI is less than 25 kg/m2, may have as much as 40% fat in the abdominal area, a level that correlates closely with decreased insulin sensitivity5 and an atherogenic dyslipidemic state. In that context, the risk of ischemic heart disease among normal-weight people with insulin resistance syndrome and among obese people without insulin resistance syndrome represents a major gap in the existing literature. We therefore sought to investigate how features of insulin resistance syndrome affected the risk of ischemic heart disease associated with variations in BMI in a cohort of 1824 men who participated in the Québec Cardiovascular Study.
Methods
The study population and follow-up methods have been described in detail elsewhere;6,7 the method of determining the participants of the present analysis is depicted in Fig. 1. The study cohort comprised 1824 nondiabetic men free of ischemic heart disease who were evaluated at the 1985 baseline evaluation and followed for a period of 13 years. The presence of diabetes at baseline was determined on the basis of self-report. In 1990/1991 and in 1998, participants were contacted by mail and invited to complete a short questionnaire, which asked for information on smoking habits (> 20 v. ≤ 20 cigarettes per day), medication use (use v. no use of β-blockers or diuretics or both), history of cardiovascular diseases and type 2 diabetes. Among the 1824 eligible men, none was lost to follow-up. Although 28 (1.5%) subjects could not be retraced between 1990 and 1998, their data were kept in the analysis because we had 5-year follow-up information for these participants.
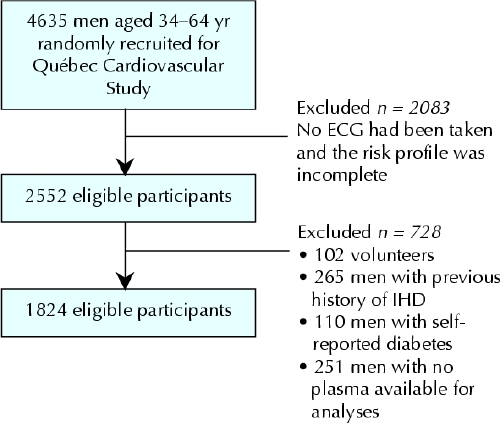
Fig. 1: Determination of the study population. The study population was originally screened from 7 towns in the Québec City metropolitan area in 1974 for the Québec Cardiovascular Study. Data collected in 1985 were used as the baseline characteristics for the present prospective study. Volunteers were men who asked to be part of the original study but were not selected among the randomly identified participants. ECG = electrocardiogram, IHD = ischemic heart disease.
Among the 1824 study participants who were free of clinical manifestations of ischemic heart disease in 1985, there were 284 first cases of ischemic heart disease during the 13-year follow-up. The diagnosis of a first ischemic heart disease event included angina on typical effort, coronary insufficiency, nonfatal myocardial infarction and coronary death, as has been described elsewhere.7,8 Coronary insufficiency was diagnosed using the nomenclature of the Framingham Heart Study for unstable angina presentation with electrocardiogram changes (changes in ST segment and T wave).
Twelve-hour fasting blood samples were obtained at the 1985 baseline evaluation, and lipid and apolipoprotein levels were measured immediately. The methods used to determine these levels have been detailed in previous publications.6,9 Plasma C-reactive protein levels,10 fasting insulin concentrations11 and low-density lipoprotein particle size6 were measured in plasma stored at –80°C. In the present analyses, low-density lipoprotein particles were characterized using the relative proportion of low-density lipoprotein particles having a diameter smaller than 255Å (termed LDL< 255Å), which was ascertained by computing the relative area of the densitometric scan on the gel using the 255Å cut-off point.6
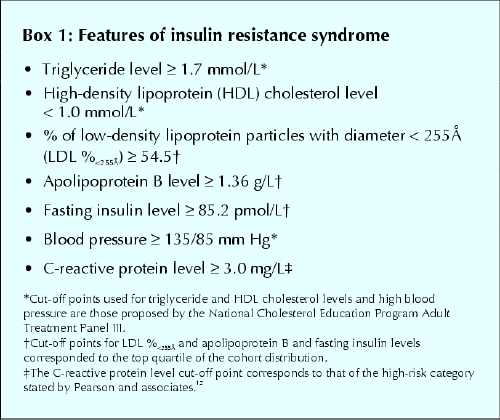
Features of insulin resistance syndrome were defined as outlined in Box 1. Participants were placed in 1 of 3 categories on the basis of BMI according to the 1998 clinical guidelines from the National Institutes of Health: normal weight (BMI < 25 kg/m2), overweight (25–29.9 kg/m2) and obese (≥ 30 kg/m2).13 Baseline characteristics of the normal-weight, overweight and obese men were compared using a general linear model with the Duncan post-hoc test to locate differences between the groups and by the Wilcoxon test for nonparametric variables. Duration of follow-up was calculated in person-years using the follow-up of each participant from the 1985 baseline evaluation until death, onset of ischemic heart disease or last contact. Cox proportional hazards models were used to estimate the relative hazard of ischemic heart disease events associated with the 3 BMI categories, individual and combined insulin resistance syndrome features, and confounding factors such as age, smoking habits and medication use at baseline. For each risk factor, assumptions of proportional hazards were tested and met. Estimated hazards of ischemic heart disease events were also estimated in normal-weight, overweight and obese participants having 2 or less, 3–4 or 5–7 features of insulin resistance syndrome. Adjustment for socioeconomic status using various standard approaches had no impact on the results (analysis not shown), and thus multivariate analyses did not include this covariable.
Box 1.
Results
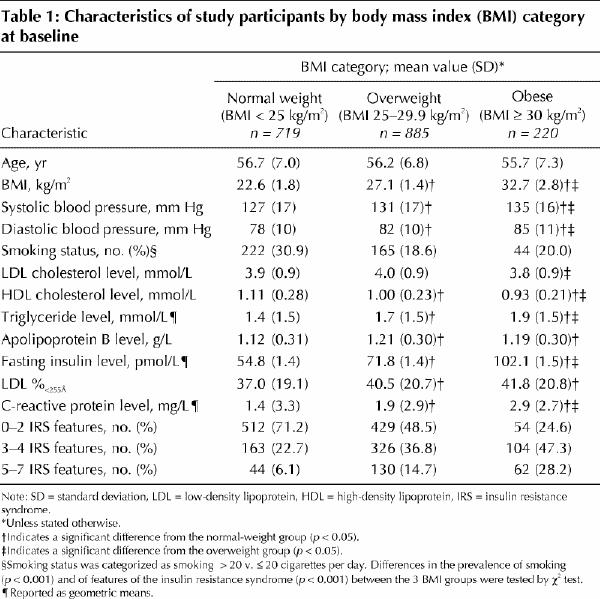
As expected, obese men had in general a higher risk profile compared with overweight and normal-weight men (Table 1). Indeed, 75.5% of obese men accumulated more than 2 features of insulin resistance syndrome. However, almost one-third (28.8%) of normal-weight men also accumulated more than 2 features of the syndrome.
Table 1
The risk of ischemic heart disease among overweight and obese men was computed using normal-weight men as the low-risk reference group. Despite having a deteriorated risk profile, overweight men were not at increased long-term risk of ischemic heart disease compared with normal-weight men (RH 0.99, 95% confidence interval [CI] 0.76–1.28) after adjustment for nonmetabolic risk factors (age, systolic blood pressure, smoking habits and medication use at baseline). Obese men showed a slightly increased risk of ischemic heart disease compared with normal-weight men, but the difference did not achieve significance in either univariate (RH 1.26, 95% CI 0.88–1.80) or multivariate (RH 1.12, 95% CI 0.78–1.62) analyses (analyses not shown).
Analyses of individual features of insulin resistance syndrome revealed that only high blood pressure (≥ 135/85 mm Hg) and high apolipoprotein B levels (≥ 1.36 g/L) were independently associated with an increased risk of ischemic heart disease (RH 1.32, 95% CI 1.03–1.70 and RH 1.72, 95% CI 1.32–2.24 respectively) (Table 2). However, the cumulative number of features modulated the risk of ischemic heart disease in an almost linear fashion (Table 3). Thus, the predicted risk of ischemic heart disease among subjects with several features of insulin resistance syndrome appeared greater than what would be expected on the basis of the individual nonsignificant contribution of most risk factors.
Table 2
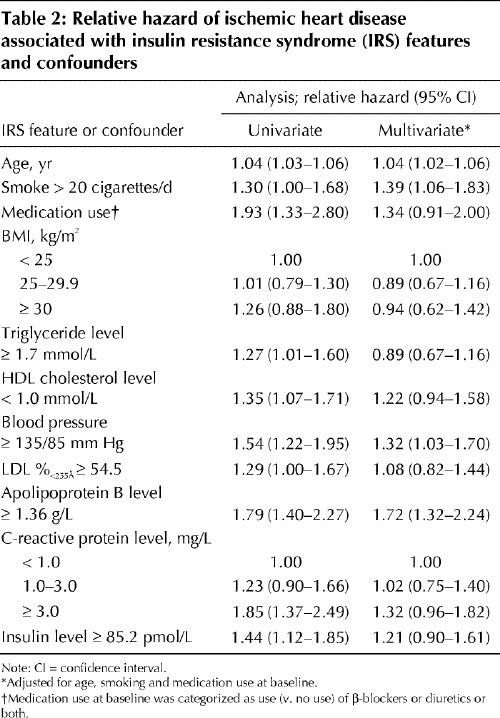
Table 3
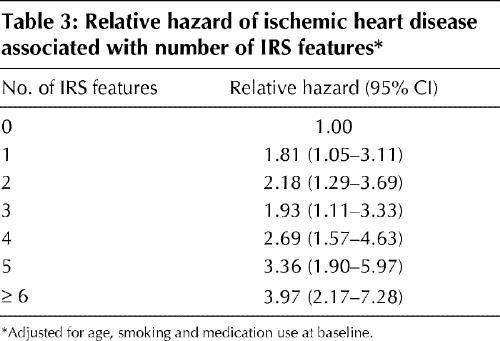
Table 4 shows the combined impact of BMI and the cumulative number of insulin resistance syndrome features on the risk of ischemic heart disease. The reference group for the relative hazards estimates is the group of normal-weight men with fewer than 3 features of insulin resistance syndrome. Obese men with fewer than 3 features of the syndrome were not at increased risk of ischemic heart disease. Having more than 4 features of the syndrome was associated with a 3-fold increase in risk among normal-weight men. The mean BMI among normal-weight men was 22.6 (standard deviation 1.8) kg/m2. Finally, the presence of more than 4 features of insulin resistance syndrome in obese men was associated with an almost 2-fold increase in risk (RH 1.81, 95% CI 1.02–3.19). There was no interaction between number of syndrome features and BMI categories (p = 0.68) in modulating the long-term risk of ischemic heart disease. We performed additional analyses using only hard endpoints (i.e., nonfatal myocardial infarction and death from coronary artery disease [N = 187]), and the results were virtually identical (analyses not shown).
Table 4
Interpretation
The results of this prospective population-based study indicate that the risk of ischemic heart disease associated with a high BMI depended entirely on whether features of insulin resistance syndrome were simultaneously present. Thus, although obese men were more susceptible to developing features of the syndrome, their risk of ischemic heart disease was elevated only when more than 4 of the 7 features were present. Interestingly, the risk of ischemic heart disease among normal-weight men was also increased in the subgroup displaying more than 4 of the 7 syndrome features.
Increased body weight and BMI have been associated with an increased risk of ischemic heart disease in several populations, but this has not been a consistent finding. The authors of the Framingham Offspring Study reported an approximate 2-fold increase in the 10-year risk of coronary artery disease in subjects with a BMI of 30 kg/m2 or more compared with those with a BMI less than 21 kg/m2 after adjustment for age.14 On the other hand, the results of the Prospective Cardiovascular Munster Study indicated that BMI did not independently contribute to cardiovascular risk in multiple logistic regression analysis.15 Stevens and associates suggested that, among men aged 30–74 years, higher body weight increased the risk of death from cardiovascular disease over a 12-year period among subjects aged 44 years or less but not among men older than 65 years.16 Because our cohort included only men 6–76 years of age, the high-risk age group (30–44 years) in the study by Stevens and associates was absent from our study, which may explain why the association between increased BMI was not significantly associated with an increased risk of ischemic heart disease in our study. The National Cholesterol Education Program Adult Treatment Panel III (NCEP III) has recently recognized the metabolic syndrome as an important risk factor for ischemic heart disease among both men and women.17 It has been estimated, on the basis of results of the Third National Health and Nutrition Examination Survey, that more than 1 in 5 adults in the United States have the metabolic syndrome,17 with almost a doubling of this prevalence (43%) among people older than 60 years.17 Our study results show that the risk of ischemic heart disease increased as a function of the cumulative number of insulin resistance syndrome features, with 3 or more metabolic features resulting in a 2–4-fold increase in the risk of ischemic heart disease. These results are consistent with data from previous studies that suggested that the prevalence of unstable angina pectoris and history of myocardial infarction were highest among patients with 5 insulin resistance syndrome features as defined by the NCEP III.18
The results of our study suggest that the risk attributable to obesity largely depends on the concomitant presence of features of insulin resistance syndrome. Thus, among obese men, who would generally be considered to be at high risk of ischemic heart disease, those who accumulated fewer than 5 features of the syndrome were not at increased risk. This subgroup represented 71.9% of all obese men. Conversely, normal-weight men with 5 or more features of insulin resistance syndrome had a risk of ischemic heart disease 3.01 times higher than of those presenting with fewer than 3 features. About 6% of all normal-weight men had 5 or more features of insulin resistance syndrome. These results confirm that insulin resistance syndrome is more prevalent among obese men. Yet, BMI appears to be a poor atherogenic index for characterizing the risk of ischemic heart disease associated with insulin resistance syndrome. We therefore believe that clinicians should not use BMI to assess the long-term risk of ischemic heart disease attributable to obesity. Other measures of adiposity, such as waist circumference, which reflects total adiposity by regional deposition of fat as well, may be a more useful and adequate clinical tool for predicting risk of ischemic heart disease. In that regard, Janssen and associates have demonstrated that, after adjustment for waist circumference as a continuous variable, the likelihood of insulin resistance syndrome was similar in all BMI groups.19 Future studies will have to demonstrate that a combination of risk factors, and more particularly a combination of insulin resistance syndrome features and indices of obesity such as waist girth, has a greater clinical utility.
There were a number of limitations to our study. Unfortunately, we could not use the NCEP III definition of the metabolic syndrome in our cohort because data on waist girth and fasting plasma glucose levels were not collected in the study cohort in 1985. Our intent was not to propose a new definition of the metabolic syndrome but, rather, to examine how specific features of this syndrome modify the risk of ischemic heart disease attributable to variations in BMI. Physical activity was not assessed as thoroughly in 1985, and thus the extent to which adjustment for physical activity would have modified the interrelation between BMI, features of insulin resistance syndrome and risk of ischemic heart disease could not be analyzed. Our 1985 data on diet are also fragmentary, and thus they were not added to the multivariate. Finally, it must be stressed that much of the medical history (e.g., diabetes, medication use) was by self-report and was not further validated.
Our results indicate that the risk of ischemic heart disease associated with an elevated BMI was significantly modulated by features of insulin resistance syndrome. These data challenge the concept that the clinical definition of obesity, based on weight and height, is adequate as a clinical tool for the primary prevention of ischemic heart disease. Alternative measures such as waist circumference should be considered and thoroughly investigated.
β See related article page 1315
Acknowledgments
This study was supported in part by an operating grant from the Canadian Institute for Health Research (MOP 14475) and by an unrestricted Medical School Grant from Merck-Frosst. Benoît Lamarche is the recipient of a Canada Research Chair in Nutrition, Functional Foods and Cardiovascular Health. Annie St-Pierre is the recipient of a training fellowship from the Heart and Stroke Foundation of Canada. Jean Bergeron is a Research Clinical Scholar from the Fonds de la Recherche en santé du Québec.
Footnotes
This article has been peer reviewed.
Contributors: Annie St-Pierre contributed substantially to the acquisition, analysis and interpretation of data and drafted the article. Bernard Cantin, Gilles Dagenais and Jean-Pierre Després contributed significantly to the conception and design of the study. Pascale Mauriège and Jean Bergeron contributed significantly to the acquisition of data. Benoît Lamarche contributed significantly to the conception and design of the study and to the acquisition, analysis and interpretation of data. All of the authors revised the article critically for important intellectual content and gave final approval of the version to be published.
Competing interests: None declared.
Correspondence to: Dr. Benoît Lamarche, Institute on Nutraceuticals and Functional Foods, Pavillon Paul-Comtois, Laval University, Ste-Foy QC G1K 7P4; fax 418 656-5877; benoit.lamarche@inaf.ulaval.ca
References
- 1.Reaven GM. Role of insulin resistance in human disease. Diabetes 1988;37:1495- 507. [DOI] [PubMed]
- 2.Despres JP. Abdominal obesity as important component of insulin-resistance syndrome. Nutrition 1993;9(5):452-9. [PubMed]
- 3.Reaven GM. The insulin resistance syndrome. Curr Atheroscler Rep 2003;5(5):364-71. [DOI] [PubMed]
- 4.Despres JP. Inflammation and cardiovascular disease: Is abdominal obesity the missing link? Int J Obes Relat Metab Disord 2003;27(Suppl 3):S22-24. [DOI] [PubMed]
- 5.Carey DG, Jenkins AB, Campbell LV, Freund J, Chisholm DJ. Abdominal fat and insulin resistance in normal and overweight women: Direct measurements reveal a strong relationship in subjects at both low and high risk of NIDDM. Diabetes 1996;45(5):633-8. [DOI] [PubMed]
- 6.St-Pierre AC, Ruel IL, Cantin B, Dagenais GR, Després JP, Lamarche B. Comparison of various electrophoretic characteristics of LDL particles and their relationship to the risk of ischemic heart disease. Circulation 2001;104:2295-9. [DOI] [PubMed]
- 7.Lamarche B, Despres JP, Moorjani S, Cantin B, Dagenais GR, Lupien PJ. Prevalence of dyslipidemic phenotypes in ischemic heart disease (prospective results from the Quebec Cardiovascular Study). Am J Cardiol 1995;75(17):1189-95. [DOI] [PubMed]
- 8.Dagenais GR, Robitaille NM, Lupien PJ, Christen A, Gingras S, Moorjani S, et al. First coronary heart disease event rates in relation to major risk factors: Québec cardiovascular study. Can J Cardiol 1990;6:274-80. [PubMed]
- 9.Lamarche B, Tchernof A, Dagenais GR, Cantin B, Lupien PJ, Després JP. Small, dense LDL particles and the risk of ischemic heart disease. Prospective results from the Québec Cardiovascular Study. Circulation 1997;95(1):69-75. [DOI] [PubMed]
- 10.Pirro M, Bergeron J, Dagenais GR, Bernard PM, Cantin B, Despres JP, et al. Age and duration of follow-up as modulators of the risk of ischemic heart desease associated with high plasma C-reactive protein levels in men. Arch Intern Med 2001;161:2474-80. [DOI] [PubMed]
- 11.Despres JP, Lamarche B, Mauriege P, Cantin B, Dagenais GR, Moorjani S, et al. Hyperinsulinemia as an independent risk factor for ischemic heart disease. N Engl J Med 1996;334(15):952-7. [DOI] [PubMed]
- 12.Pearson TA, Mensah GA, Alexander RW, Anderson JL, Cannon RO III, Criqui M, et al. Markers of inflammation and cardiovascular disease: application to clinical and public health practice: A statement for healthcare professionals from the Centers for Disease Control and Prevention and the American Heart Association. Circulation 2003;107(3):499-511. [DOI] [PubMed]
- 13.Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults —The Evidence Report. National Institutes of Health. Obes Res 1998;6(Suppl 2):51S-209S. [PubMed]
- 14.Lamon-Fava S, Wilson PW, Schaefer EJ. Impact of body mass index on coronary heart disease risk factors in men and women. The Framingham Offspring Study. Arterioscler Thromb Vasc Biol 1996;16(12):1509-15. [DOI] [PubMed]
- 15.Schulte H, von Eckardstein A, Cullen P, Assmann G. [Obesity and cardiovascular risk]. Herz 2001;26(3):170-7. [DOI] [PubMed]
- 16.Stevens J, Cai J, Pamuk ER, Williamson DF, Thun MJ, Wood JL. The effect of age on the association between body-mass index and mortality. N Engl J Med 1998;338(1):1-7. [DOI] [PubMed]
- 17.Ford ES, Giles WH, Dietz WH. Prevalence of the metabolic syndrome among US adults: findings from the third National Health and Nutrition Examination Survey. JAMA 2002;287(3):356-9. [DOI] [PubMed]
- 18.Solymoss BC, Bourassa MG, Campeau L, Sniderman A, Marcil M, Lesperance J, et al. Effect of increasing metabolic syndrome score on atherosclerotic risk profile and coronary artery disease angiographic severity. Am J Cardiol 2004;93(2):159-64. [DOI] [PubMed]
- 19.Janssen I, Katzmarzyk PT, Ross R. Waist circumference and not body mass index explains obesity-related health risk. Am J Clin Nutr 2004;79(3):379-84. [DOI] [PubMed]


